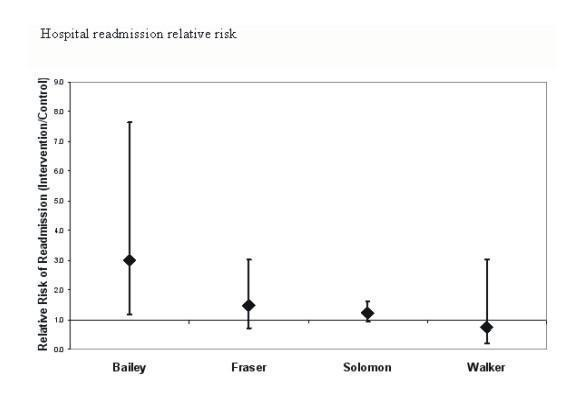
| Study | Intervention | Design | Outcome | Difference (Int‐Con)1 | CI (Lower‐Upper)2 | p Value | Relative Risk | CI (Lower‐Upper)2 | Effect |
| Bailey 1997 | Persuasive, Pharmacist | RCT | Switch to oral in 24h (Intended direction: +ve, increase) | +9.8% | ‐7.6% to +27.2% | >0.1 | 1.15 | 0.90 to 1.47 | No |
| Burton 1991 | Structural, Bayesian dosing program | RCT | Trough aminoglycoside level <2mg/l (Intended direction: +ve, increase) | +4.5% | ‐6.2% to +15.2% | >0.1 | 1.05 | 0.93 to 1.19 | No |
| Cordova 1986 | Persuasive, Pharmacist | CBA | Cefazolin dosing 8hrly or more (Intended direction: +ve, increase) | +54.9% | +33.4% to +76.5% | <0.001 | 3.93 | 1.40 to 10.99 | Yes |
| Dranitsaris 2001 | Persuasive, Pharmacist | RCT | Appropriate cefotaxime indication+dosing (Intended direction: +ve, increase) | +5.9% | ‐4.1% to +15.9% | >0.1 | 1.09 | 0.94 to 1.25 | No |
| Appropriate cefotaxime indication (Intended direction: +ve, increase) | +1.9% | ‐7.0% to +10.7% | >0.1 | 1.02 | 0.92 to 1.14 | No |
| Appropriate cefotaxime dosing (Intended direction: +ve, increase) | +8.1% | +1.4% to +14.9% | <0.05 | 1.09 | 1.01 to 1.18 | Yes |
| Fraser 1997 | Persuasive, ID fellow and pharmacist | RCT | Mean daily doses of IV antibiotics per patient (Intended direction: ‐ve, decrease) | ‐3.43 | Not calculable from data in the paper | 0.09 | Continuous variable | Trend |
| Mean antibiotic charges per patient (Intended direction: ‐ve, decrease) | ‐$387 | Not calculable from data in the paper | 0.05 | Yes |
| Gums 1999 | Persuasive, antimicrobial management team | RCT | Median antibiotic costs (Intended direction: ‐ve, decrease) | ‐$605 | ‐$662 to ‐$548 | <0.001 | Continuous variable | Yes |
| Median of total costs (Intended direction: ‐ve, decrease | ‐$3,054 | ‐$3,280 to ‐$2,828 | <0.001 | Yes |
| Herfindal 1983 | Persuasive, Pharmacist | CBA | Mean antibiotic cost per patient day (Intended direction: ‐ve, decrease) | ‐$2.35 | ‐$3.08 to ‐$1.62 | <0.001 | Continuous variable | Yes |
| Mean antibiotic doses per patient day (Intended direction: ‐ve, decrease) | ‐0.98 | ‐1.28 to ‐0.68 | <0.001 | Yes |
| Mean antibiotic courses per patient day (Intended direction: ‐ve, decrease) | ‐0.35 | ‐0.46 to ‐0.24 | <0.001 | Yes |
| Landgren 1988 | Persuasive, Pharmacist | CBA | % appropriate timing of prophylaxis (Intended direction: +ve, increase) | +13.0% | ‐4.0% to +30.0% | 0.12 | Relative risk cannot be calculated from data in paper | No |
| % appropriate duration of prophylaxis (Intended direction: +ve, increase) | +20.0% | +1.0% to +40.0% | 0.04 | Yes |
| Parrino 1989 | Persuasive, Feedback letter | CBA | Mean quarterly antibiotic expenditure per physician (Intended direction: ‐ve, decrease) | +$3,818 | +$603 to +$7,033 | >0.5 | Continuous variable | No |
| Pastel 1992 | Persuasive, Pharmacist | CCT | Appropriate modification based on C&S results, all physicians (Intended direction: +ve, increase) | +11.1% | ‐5.3% to +27.5% | >0.1 | 1.16 | 0.93 to 1.45 | No |
| Same, private physicians only (Intended direction: +ve, increase) | +34.7% | +4.2% to +65.1% | <0.05 | 1.97 | 0.94 to 4.15 | Yes |
| Shojania 1998 | Persuasive, reminder via computer screen | RCT | Mean vancomycin orders per prescriber (Intended direction: ‐ve, decrease) | ‐5.40 | ‐10.34 to ‐0.46 | <0.05 | Continuous variable | Yes |
| Mean vancomycin days per prescriber (Intended direction: ‐ve, decrease) | ‐14.70 | ‐27.31 to ‐2.09 | <0.05 | Yes |
| Singh 2000 | Restrictive, Stop order | RCT | Patients receiving > 3 days antibiotics for suspected pneumonia in the ICU (Intended direction: ‐ve, decrease) | ‐69.2% | ‐84.2% to ‐54.3% | <0.05 | 0.29 | 0.17 to 0.48 | Yes |
| Solomon 2001 | Persuasive, Multi‐disciplinary team | RCT | Mean days unnecessary levofloxacin or ceftazidime (Intended direction: ‐ve, decrease) | ‐3.30 | ‐3.81 to ‐2.79 | <0.001 | Continuous variable | Yes |
| Trenholme 1989 | Structural, Rapid culture | RCT | Patients changed to less expensive antibiotics (Intended direction: +ve, increase) | +16.4% | +5.1% to +27.8% | <0.01 | 1.91 | 1.20 to 3.04 | Yes |
| Walker 1998 | Persuasive, Reminder | RCT | Patients switched to oral antibiotics (Intended direction: +ve, increase) | +52.0% | +29.3% to +74.7% | <0.001 | 2.44 | 1.42 to 4.20 | Yes |