Tiefe Querfriktionen zur Behandlung von Sehnenentzündungen (Tendinitiden) an der Außenseite des Ellbogens oder Knies
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Study design: randomized, assessor‐blinded trial Sample size at entry: 20 | |
| Participants | Setting: visitors to a sports injury clinic with unilateral chronic (> 4 weeks) iliotibial band syndrome causing pain severe enough to restrict running distance or speed (grade 3), or to prevent it altogether (grade 4) Inclusion criteria:
Exclusion criteria: < 18 years old, history of previous knee surgery, concomitant medical therapy | |
| Interventions | Deep transverse friction massage: applied on days 3, 5, 7 and 10 Treated anatomical area (most tender area) with constant pressure, such that discomfort was experienced, but not severe pain; 2 minutes of light friction, then 8 minutes of harder friction Technique: Pressure was applied with the index finger and reinforced with the ring finger, with the thumb acting as a pivot; brisk motion was initiated from the therapist's shoulder, with the wrist flexible and the hand stiff Concurrent treatment:
| |
| Outcomes | Mean pain daily recall, total pain while running, % max pain experienced while running (VAS 0 to 10; 0 = no pain) for 3 treatment periods (days 0 to 2, 3 to 6, 7 to 14) | |
| Notes | One participant was excluded for refusal to comply with the treatment group. Two participants were not accounted for in the control group (reasons not provided) Per‐protocol analysis Source of funding: "This research project was generously supported financially by Johnson and Johnson Pty Ltd" Declarations of interest of primary researchers not provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: ''patients were divided into two treatment groups on a random basis'' Comments: method not described |
| Allocation concealment (selection bias) | Unclear risk | Comments: Investigators state that they divided the 17 athletes into 2 groups without explaining the method of allocation |
| Blinding of participants and personnel (performance bias) | High risk | Comment: Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Quote: ''the efficacy of the treatment was assessed by a different therapist who was blind to the treatment group of the patient'' Comments: Insufficient information available to judge whether not blinding the participants had an impact on patient‐reported outcomes. More likely at 'high risk' for self‐reported subjective outcomes (eg, pain) |
| Incomplete outcome data (attrition bias) | High risk | Comments: This study had a 15% dropout rate (even across treatment groups). Duration of follow‐up was mentioned, but investigators did not perform an intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Comments: The trial presented planned outcomes whether or not the result was significant. No selective reporting was found to be present |
| Other bias | High risk | Comment: Baseline imbalance was reported; mean age and duration of symptoms were different across groups |
| Methods | Study design: randomized controlled trial, parallel group, combination of interventions Sample size at entry: 40 Treatment duration: 9 sessions within 5 weeks Follow‐up: 5 weeks | |
| Participants | Setting: patients attending a community sports injuries clinic Inclusion criteria: those who complained of discomfort at or about the lateral epicondyle; pain at the lateral aspect of the elbow during resisted wrist extension; radial deviation during complete elbow extension; tenderness in palpation over, or at, one of the following areas: (1) origin of extensor carpi radialis longus tendon, (2) origin of extensor carpi radialis brevis tendon, (3) extensor carpi radialis brevis at tendon body, and (4) extensor carpi radialis brevis tendon with tenderness extending from origin to the tendon body Age (mean in years (± SD)) Disease duration (months: mean (± SD)) Exclusion criteria: combined lesions; bilateral elbow problems at initial assessment; history of prior surgery; history of an injection to the elbow within the past 6 months | |
| Interventions | Deep transverse friction massage Concurrent treatment for group 1 and group 2: ultrasound and placebo ointment Concurrent treatment for groups 3 and 4: phonophoresis | |
| Outcomes | Pain
Grip strength
Function
Functional status (success or failure to perform pain‐free strengthening program for the wrist extensor muscles, with the elbow extended, without subsequent regression within 2 weeks of follow‐up) | |
| Notes | We extracted the outcome of pain on VAS (0 to 100), not pain‐free function, for the review Source of funding: "This work was supported by the Physiotherapy Foundation of Canada" Declarations of interest of primary researchers not provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''The study design was a two by two factorial design. The subjects were randomly assigned using a balanced blocked randomization table'' |
| Allocation concealment (selection bias) | Unclear risk | Comments: Method of allocation concealment was not described |
| Blinding of participants and personnel (performance bias) | High risk | Comment: Participants and personnel were not blinded to treatment |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: ''Decision was made by the assessor who was blind to both interventions'' Comments: Insufficient information was available on which to base judgement if not blinding participants had an impact on patient‐reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comments: No description of withdrawals and dropouts was mentioned. However, all randomly assigned participants were accounted for in the results |
| Selective reporting (reporting bias) | Low risk | Comments: The trial presented all planned outcomes whether or not the result was significant. No selective reporting was found to be present |
| Other bias | High risk | Comments: Baseline imbalance was reported; the duration of symptoms was different across groups |
DTFM: Deep transverse friction massage.
SD: Standard deviation.
SE: Standard error.
VAS: Visual analog scale.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not tendinitis | |
| Combination of interventions; co‐interventions not applied to the control group | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Healthy participants | |
| Healthy participants | |
| Not tendinitis | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Study was not a randomized controlled trial | |
| Study was not a randomized controlled trial | |
| No control group | |
| No control group | |
| No control group | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| No control group | |
| Combination of interventions: Cyriax and Mill's manipulation; co‐intervention not applied to the control group | |
| Pilot study | |
| Combination of Interventions; co‐interventions not applied to the control group | |
| Not tendinitis | |
| No control group | |
| Combination of interventions: Cyriax and Mill's manipulation; co‐intervention not applied to the control group | |
| Not tendinitis | |
| Study was not a randomized controlled trial |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain (VAS 0‐100, 0 = worst) (change from baseline) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 1 Pain (VAS 0‐100, 0 = worst) (change from baseline). | ||||
| 2 Grip strength (ratio index, higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 2 Grip strength (ratio index, higher is better). | ||||
| 3 Function (VAS 0‐100, 0 = worst) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 3 Function (VAS 0‐100, 0 = worst). | ||||
| 4 Function (pain‐free function; average number of pain‐free items; higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4 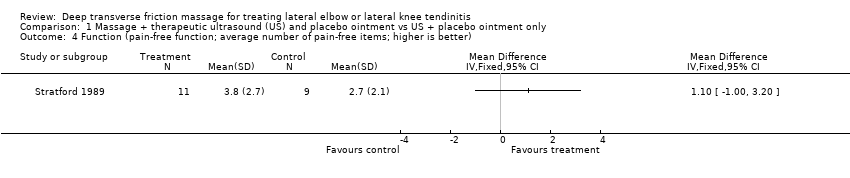 Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 4 Function (pain‐free function; average number of pain‐free items; higher is better). | ||||
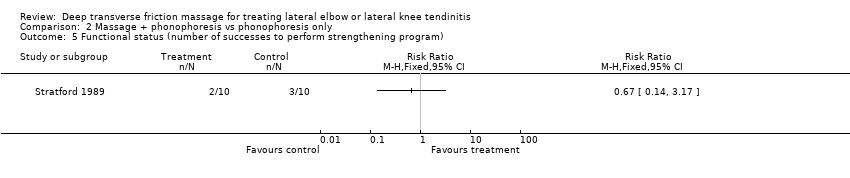
| 5 Functional status (number of successes to perform strengthening program) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 5 Functional status (number of successes to perform strengthening program). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain (VAS 0‐100, 0 = worst) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 1 Pain (VAS 0‐100, 0 = worst). | ||||
| 2 Grip strength (ratio index, higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2 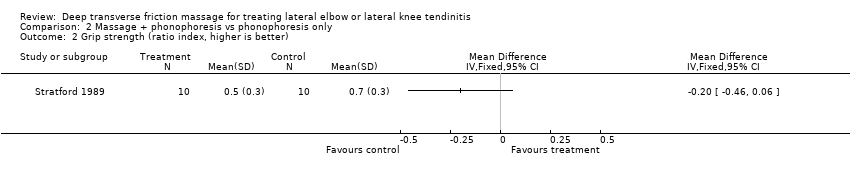 Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 2 Grip strength (ratio index, higher is better). | ||||
| 3 Function (VAS 0‐100, 0 = worst) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 3 Function (VAS 0‐100, 0 = worst). | ||||
| 4 Function (pain‐free function; average number of pain‐free items; higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4 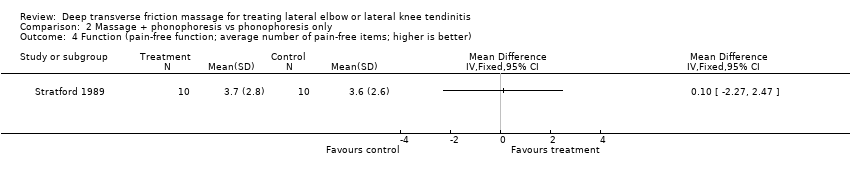 Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 4 Function (pain‐free function; average number of pain‐free items; higher is better). | ||||
| 5 Functional status (number of successes to perform strengthening program) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.5  Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 5 Functional status (number of successes to perform strengthening program). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1 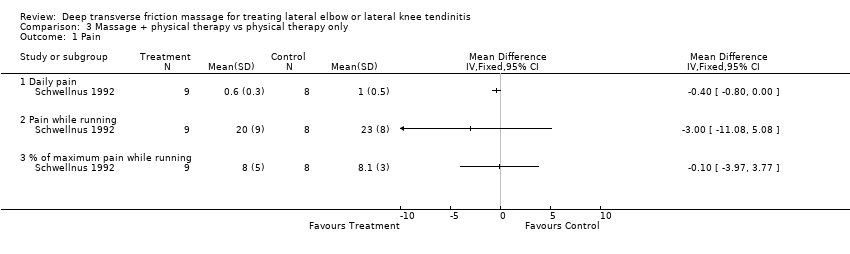 Comparison 3 Massage + physical therapy vs physical therapy only, Outcome 1 Pain. | ||||
| 1.1 Daily pain | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Pain while running | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 % of maximum pain while running | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
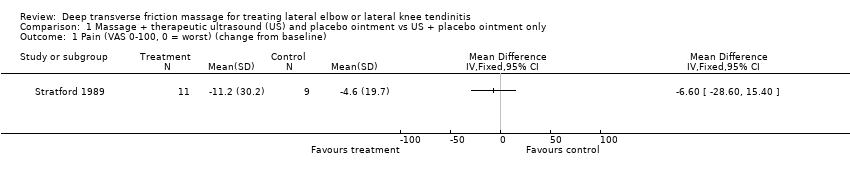
Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 1 Pain (VAS 0‐100, 0 = worst) (change from baseline).

Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 2 Grip strength (ratio index, higher is better).

Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 3 Function (VAS 0‐100, 0 = worst).
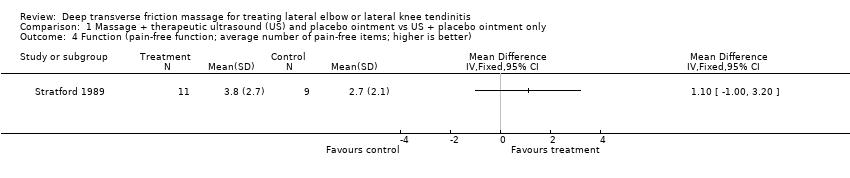
Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 4 Function (pain‐free function; average number of pain‐free items; higher is better).

Comparison 1 Massage + therapeutic ultrasound (US) and placebo ointment vs US + placebo ointment only, Outcome 5 Functional status (number of successes to perform strengthening program).

Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 1 Pain (VAS 0‐100, 0 = worst).

Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 2 Grip strength (ratio index, higher is better).

Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 3 Function (VAS 0‐100, 0 = worst).

Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 4 Function (pain‐free function; average number of pain‐free items; higher is better).
Comparison 2 Massage + phonophoresis vs phonophoresis only, Outcome 5 Functional status (number of successes to perform strengthening program).

Comparison 3 Massage + physical therapy vs physical therapy only, Outcome 1 Pain.
| Massage + therapeutic ultrasound and placebo ointment compared with ultrasound + placebo ointment only (follow‐up 2 weeks) for treating tendinitis | ||||||
| Patient or population: patients with extensor carpi radialis tendinitis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (US + placebo ointment only) | Massage + US and placebo ointment | |||||
| Pain Scale from 0 to 100 (lower is better) | Mean change in pain in the control groups was | Mean change in pain in the intervention groups was | 20 | ⊕⊝⊝⊝ | MD = ‐6.60 (‐28.60 to 15.40) Absolute improvement = ‐7% (‐29% to ‐15%) Relative percentage change = 8% (‐24% to 37%) Not statistically significant | |
| Proportion reporting pain relief of 30% or greater not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Function Scale from 0 to 100 (higher is better) | Mean function (vas 0 to 100, 0 = worst) in the control groups was | Mean function (VAS 0‐100, 0 = worst) in the intervention groups was | 20 | ⊕⊝⊝⊝ | MD = ‐1.80 (‐18.64 to 15.04) Absolute improvement = 2% (‐19% to 15%) Relative percentage change = ‐3% (‐28% to 23%) Not statistically significant | |
| Quality of life—not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Patient global assessment of success not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Adverse events not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Withdrawals due to adverse events not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aAllocation concealment was unclear. Only assessors were blinded. Baseline imbalance was reported. | ||||||
| Massage + phonophoresis compared with control (phonophoresis only) (follow‐up 2 weeks) for treating tendinitis | ||||||
| Patient or population: patients with extensor carpi radialis tendinitis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (phonophoresis only) (follow‐up 2 weeks) | Massage + phonophoresis | |||||
| Pain Scale from 0 to 100 (lower is better) | Mean change in pain in the control groups was | Mean change in pain in the intervention groups was | 20 | ⊕⊝⊝⊝ | MD = ‐1.2 (‐20.24 to 17.84) Absolute improvement = ‐1% Relative percentage change = 6% (‐86% to 97%) Not statistically significant | |
| Proportion reporting pain relief of 30% or greater not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Function Scale from 0 to 100 (higher is better) | Mean function in the control groups was | Mean function in the intervention groups was | ‐ | 20 | ⊕⊝⊝⊝ | MD = 3.70 (‐14.13 to 21.53) Absolute improvement = 4% (‐14% to 22%) Relative percentage change = 5% (‐18% to 28%) Not statistically significant |
| Quality of life not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Patient global assessment of success not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Adverse events not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Withdrawals due to adverse events not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aAllocation concealment was unclear. Only assessors were blinded. Baseline imbalance was reported. | ||||||
| Deep transverse friction massage + physical therapy compared with physical therapy alone | ||||||
| Patient or population: patients with iliotibial band friction syndrome (knee tendinitis) Settings: community sports injury clinic in South Africa Intervention: deep transverse massage and physical therapy Comparison: physical therapy alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Deep transverse massage | |||||
| Daily pain Follow‐up mean 2 | Mean daily pain | Mean daily pain in the intervention groups was | 17 | ⊕⊝⊝⊝ | MD = ‐0.4 (‐0.8 to 0) Absolute improvement = ‐4% (‐8% to 0%) Relative percentage change = ‐40% (‐80% to 0%) Not statistically significant | |
| Proportion reporting pain relief of 30% or greater not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Function not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Quality of life not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Patient global assessment not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Adverse events not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Withdrawals due to adverse events | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aRandomization and allocation concealment were unclear. Only assessors were blinded. No intention‐to‐treat analysis was done, and baseline imbalance was reported. | ||||||
| Inclusion | Exclusion |
| Participants/Population (P)
| Participants/Population (P)
|
| Interventions (I)
| Interventions (I)
|
| Comparisons (C) Studies were included if they compared an intervention group (eg, deep transverse frictions techniques combined with modalities, exercises) with a comparison group (eg, placebo, no treatment, active treatment such as modalities, exercises) | Comparisons (C) Studies were excluded if they did not compare the intervention group with a comparison group (eg, placebo, no treatment, active treatment such as modalities, exercises) |
| Outcomes (O)
| Outcomes (O)
|
| Period of time (P) Studies were included if the intervention period lasted longer than 1 week or 1 treatment session, with or without a follow‐up period | Period of time (P) Studies were excluded if the intervention period lasted less than 1 week or 1 treatment session |
| Study designs (S)
*English and French articles only. | Study designs (S)
|
| BMI: Body mass index. | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain (VAS 0‐100, 0 = worst) (change from baseline) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Grip strength (ratio index, higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Function (VAS 0‐100, 0 = worst) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Function (pain‐free function; average number of pain‐free items; higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Functional status (number of successes to perform strengthening program) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain (VAS 0‐100, 0 = worst) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Grip strength (ratio index, higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Function (VAS 0‐100, 0 = worst) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Function (pain‐free function; average number of pain‐free items; higher is better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Functional status (number of successes to perform strengthening program) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Daily pain | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Pain while running | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 % of maximum pain while running | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

