Clorhexidina vaginal durante el trabajo de parto para la prevención de la infección neonatal por estreptococos del grupo B de inicio temprano
Información
- DOI:
- https://doi.org/10.1002/14651858.CD003520.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 14 diciembre 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Arne Ohlsson: design of review; editing text of protocol; evaluation of methodologic quality of included trials; and editing text of review.
Vibhuti Shah: design of review; editing text of protocol; identification of trials for inclusion; evaluation of methodologic quality of included trials; abstraction of data; and editing text of review.
Brenda Stade: design of review; writing text of protocol; literature search and identification of trials for inclusion; evaluation of methodologic quality of included trials;abstraction of data; verifying and entering data into Review Manager; and writing text of review.
All three review authors contributed to the 2004 update of this review (Stade 2004).
For the 2014 update, all three review authors assessed the identified trials for inclusion or exclusion. Arne Ohlsson became the contact author; revised the background and methods sections. Arne Ohlsson and Vibhuti Shah extracted data from all included trials and completed the 'Risk of bias' tables. Vibhuti Shah developed the 'Summary of findings' table. Vibhuti Shah and Brenda Stade edited the text and checked the 'Risk of bias' table and the 'Summary of findings' table for accuracy.
Sources of support
Internal sources
-
St. Michael's Hospital, Toronto, Canada.
-
Mount Sinai Hospital, Toronto, Canada.
External sources
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Arne Ohlsson, Vibhuti Shah and Brenda Stade have no conflicts of interest to declare.
Acknowledgements
Marianne Bracht, RN: translation of articles from Spanish into English.
We would like to thank Erika Ota for her support in the creation of the 'Summary of findings' table for this update. Erika Ota's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication.
Dr. Anna‐Karin Dykes provided additional information regarding the Christensen 1987 study.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Dec 14 | Vaginal chlorhexidine during labour to prevent early‐onset neonatal group B streptococcal infection | Review | Arne Ohlsson, Vibhuti S Shah, Brenda C Stade | |
| 2004 Jul 19 | Vaginal chlorhexidine during labour to prevent early‐onset neonatal group B streptococcal infection | Review | Brenda C Stade, Vibhuti S Shah, Arne Ohlsson | |
| 2002 Jan 21 | Vaginal chlorhexidine during labour to prevent neonatal group B streptococcal infection | Protocol | Brenda C Stade, Vibhuti Shah, Arne Ohlsson | |
Differences between protocol and review
For this update GBS pneumonia within the first seven days of life was added as a non‐prespecified outcome.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Streptococcus agalactiae;
- Administration, Intravaginal;
- Anti‐Infective Agents, Local [*administration & dosage];
- Chlorhexidine [*administration & dosage];
- Labor, Obstetric;
- Randomized Controlled Trials as Topic;
- Streptococcal Infections [*prevention & control];
- Vaginal Creams, Foams, and Jellies [administration & dosage];
Medical Subject Headings Check Words
Female; Humans; Infant, Newborn; Pregnancy;
PICO

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment, Outcome 1 Early onset GBS disease (sepsis and/or meningitis within the first seven days of life)).
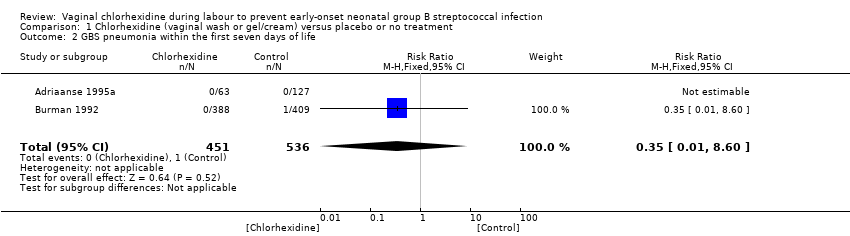
Comparison 1 Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment, Outcome 2 GBS pneumonia within the first seven days of life.

Comparison 1 Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment, Outcome 3 Neonatal colonization with GBS within the first seven days of life.

Comparison 1 Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment, Outcome 4 Neonatal mortality due to early‐onset GBS infection.

Comparison 1 Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment, Outcome 5 Adverse (mild) effects in the mother.

Comparison 1 Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment, Outcome 6 Adverse (mild) effects in the neonate.

Comparison 2 Chlorhexidine vaginal wash versus mechanical washing with placebo or no treatment, Outcome 1 Early onset GBS disease (sepsis and/or meningitis) within the first seven days of life.

Comparison 2 Chlorhexidine vaginal wash versus mechanical washing with placebo or no treatment, Outcome 2 GBS pneumonia within in the first seven days of life.

Comparison 2 Chlorhexidine vaginal wash versus mechanical washing with placebo or no treatment, Outcome 3 Neonatal colonization with GBS within the first seven days of life.

Comparison 2 Chlorhexidine vaginal wash versus mechanical washing with placebo or no treatment, Outcome 4 Adverse effects (mild) in the mother.

Comparison 2 Chlorhexidine vaginal wash versus mechanical washing with placebo or no treatment, Outcome 5 Adverse effects (mild) in the neonate.

Comparison 3 Chlorhexidine digluconate gel or cream versus placebo or no treatment, Outcome 1 Early onset GBS disease (sepsis and/or meningitis within the first seven days of life).

Comparison 3 Chlorhexidine digluconate gel or cream versus placebo or no treatment, Outcome 2 GBS pneumonia within the first seven days of life.

Comparison 3 Chlorhexidine digluconate gel or cream versus placebo or no treatment, Outcome 3 Neonatal colonization with GBS within the first seven days of life.

Comparison 3 Chlorhexidine digluconate gel or cream versus placebo or no treatment, Outcome 4 Neonatal mortality due to early‐onset GBS infection.

Comparison 3 Chlorhexidine digluconate gel or cream versus placebo or no treatment, Outcome 5 Adverse (mild) effects in the mother.

Comparison 3 Chlorhexidine digluconate gel or cream versus placebo or no treatment, Outcome 6 Adverse (mild) effects in the neonate.
| Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment | ||||||
| Population: women with vaginal or rectal colonization with GBS during labour and their preterm/term infants | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Chlorhexidine (vaginal wash or gel/cream) versus placebo or no treatment | |||||
| Early onset GBS disease (sepsis and/or meningitis within the first seven days of life)) | Study population | RR 2.32 | 987 | ⊕⊝⊝⊝ | ||
| 2 per 1000 | 4 per 1000 | |||||
| Moderate | ||||||
| 1 per 1000 | 2 per 1000 | |||||
| GBS pneumonia within the first seven days of life | Study population | RR 0.35 | 987 | ⊕⊝⊝⊝ | ||
| 2 per 1000 | 1 per 1000 | |||||
| Moderate | ||||||
| 1 per 1000 | 0 per 1000 | |||||
| Neonatal colonization with GBS within the first seven days of life | Study population | RR 0.64 | 328 | ⊕⊝⊝⊝ | ||
| 225 per 1000 | 144 per 1000 | |||||
| Moderate | ||||||
| 333 per 1000 | 213 per 1000 | |||||
| Neonatal mortality due to early‐onset GBS infection | See comment | See comment | Not estimable | 190 | See comment | The outcome was reported with no events. |
| Adverse (mild) effects in the mother | Study population | RR 8.5 | 1066 | ⊕⊝⊝⊝ | ||
| 2 per 1000 | 15 per 1000 | |||||
| Moderate | ||||||
| 0 per 1000 | 0 per 1000 | |||||
| Adverse (mild) effects in the neonate | See comment | See comment | Not estimable | 1066 | See comment | The outcome was reported with no events. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most studies contributing data had design limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Early onset GBS disease (sepsis and/or meningitis within the first seven days of life)) Show forest plot | 2 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.32 [0.34, 15.63] |
| 2 GBS pneumonia within the first seven days of life Show forest plot | 2 | 987 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.60] |
| 3 Neonatal colonization with GBS within the first seven days of life Show forest plot | 3 | 328 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.36, 1.18] |
| 4 Neonatal mortality due to early‐onset GBS infection Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Adverse (mild) effects in the mother Show forest plot | 3 | 1066 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.50 [1.60, 45.28] |
| 6 Adverse (mild) effects in the neonate Show forest plot | 3 | 1066 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Early onset GBS disease (sepsis and/or meningitis) within the first seven days of life Show forest plot | 1 | 797 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.07, 16.79] |
| 2 GBS pneumonia within in the first seven days of life Show forest plot | 1 | 797 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.60] |
| 3 Neonatal colonization with GBS within the first seven days of life Show forest plot | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.12, 0.90] |
| 4 Adverse effects (mild) in the mother Show forest plot | 2 | 876 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.50 [1.60, 45.28] |
| 5 Adverse effects (mild) in the neonate Show forest plot | 2 | 876 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Early onset GBS disease (sepsis and/or meningitis within the first seven days of life) Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.25, 145.22] |
| 2 GBS pneumonia within the first seven days of life Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Neonatal colonization with GBS within the first seven days of life Show forest plot | 2 | 249 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.48, 1.35] |
| 4 Neonatal mortality due to early‐onset GBS infection Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Adverse (mild) effects in the mother Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Adverse (mild) effects in the neonate Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

