La manipulation fœtale pour faciliter les tests du bien‐être du fœtus
Referencias
References to studies included in this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomisation method: randomised by odd or even hospital numbers with its attendant bias. Effectiveness of randomisation was assessed by comparison of various indications within the 2 groups. | |
| Participants | Women of gestation ages ranging from < 30 weeks to > 42 weeks. Majority of the tests were done because of suspected postdate pregnancy, diabetes and suspected intrauterine growth retardation. Country: USA, California. 790 women randomised. | |
| Interventions | Women randomised to manual stimulation group underwent manual stimulation of the fetus for 60 seconds prior to the beginning of 20 minutes of non‐stress CTG test. Women randomised to non‐manual stimulation group did not undergo manual manipulation prior to the beginning of 20‐minute of non‐stress CTG test. | |
| Outcomes | Primary outcome: FHR reactivity. This was defined as the presence of 2 accelerations of greater than 15 beats/minute and of 15 seconds' duration or more within a 20‐minute period. | |
| Notes | Manual manipulation involved grasping both poles of the fetus and moving the fetus back and forth in a rocking motion. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequence generated by even or odd hospital number. |
| Allocation concealment (selection bias) | High risk | Allocation based on hospital number. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Probably not done. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Probably not done. |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up 100%. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | No evidence of other forms of bias. |
| Methods | Randomisation: randomised by draw of sealed envelopes. Effectiveness of randomisation was assessed by comparisons of several parameters within the 2 groups which include maternal ages, parities, gestational ages and primary indications. | |
| Participants | Women of at least 34 weeks' gestation. Exclusion criteria ‐ no contraindications to contraction stress tests. Country: Western Australia. 300 women randomised. | |
| Interventions | Women randomised to fetal acoustic stimulation group were monitored for an initial 5 minutes. If the pattern was non‐reactive, a 3‐second vibratory acoustic stimulation was applied to the maternal abdomen in the region of the fetal head. The stimulus was repeated a second and a third time, also at 1‐minute intervals, if satisfactory FHR accelerations had not occurred. | |
| Outcomes | Primary outcome: FHR reactivity. This was defined as the presence of 2 accelerations of greater than 15 beats/minute and of 15 seconds' duration or more within a 20‐minute period. In tests in which accelerations had been provoked by fetal acoustic stimulation, the definition of reactivity required 1 of the 2 accelerations to have been unprovoked. | |
| Notes | All tests were performed with Corometrics 115 monitors using Doppler FHR transducers. The tests were performed by specially trained fetal intensive care midwives with a nurse: patient ratio of 1:1. The vibratory acoustic stimulus had an audio frequency of 75 Hz, a sound intensity of 74 db at 1 m in air and a stimulation duration of 3 seconds. Randomisation was performed after informed consent. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation done by draw of sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Randomisation done by draw of sealed envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up 100%. |
| Selective reporting (reporting bias) | Unclear risk | Not clear. |
| Other bias | Low risk | No evidence of other form of bias. |
| Methods | Randomisation: 308 patients were included for 540 FHR testings, assigned to either non‐stress test or manual stimulation test using blocked randomisation, 270 in each group. | |
| Participants | Singleton pregnant women with gestational age of 28 or more weeks. Country: Thailand. | |
| Interventions | In the MST group, the presenting part of the fetus was held through the maternal abdomen by the operator with 1 hand and the upper pole of the fetus with the other hand. After 3‐minute baseline recording of the FHR tracing, the fetus was then gently shaken left‐and‐right, up‐and‐down and forward‐and‐backward each procedure twice, making 6 manipulations. The procedure was repeated up to 3 times (4 times in total) if no qualifying acceleration was observed within 15 seconds. A new cycle of stimulation was carried out if no reactive criteria were fulfilled in 10 minutes. The same procedure was extended for another 30 minutes if no reactive criteria were achieved within 20 minutes for both MST and NST. All FHR tracings were read blindly by 1 independent perinatologist. | |
| Outcomes | Tests were interpreted as reactive when there were 2 or more FHR accelerations of at least 14 beats/minute lasting at least 15 seconds in any 20‐minute period. 1 prolonged FHR acceleration of at least 15 beats/minute lasting 2 or more minutes was also interpreted as reactive. The test was diagnosed as non‐reactive when these criteria were not met within 40 minutes of monitoring and contraction stress test, biophysical profile, Doppler velocity or delivery determination was conducted as the hospital standard practice guideline. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were assigned to either non‐stress test or manual stimulation test using blocked randomisation, 270 in each group. |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unclear. |
| Blinding of outcome assessment (detection bias) | Low risk | All FHR tracings were read blindly by 1 independent perinatologist. |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up rate 100%. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the methods section have been reported on. |
| Other bias | Low risk | No evidence of other forms of bias. |
| Methods | Randomisation: randomised by draw of sealed envelopes. | |
| Participants | 10 healthy nulliparous women with normal pregnancies of 37 to 40 weeks. | |
| Interventions | 10 envelopes were prepared, half of which indicated that shaking procedure should be performed during the first observed FHR low variation episode and the remainder indicated that the procedure should be postponed until the second low variation episode. For each participant, an envelope was opened after the first non‐reactive trace lasting 10 minutes. Shaking was performed immediately thereafter or postponed until the second such occasion. In this way 2 episodes of low variation were examined in each fetus, 1 serving as control and the other as an experimental observational period. | |
| Outcomes | Primary outcome: FHR reactivity. | |
| Notes | Manual manipulation involved external stimulation over a 20‐second period by the same investigators in all participants. The stimulation consisted of strong shaking movements of the uterus, from 1 side to the other. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation done by draw of sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Randomisation done by draw of sealed envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unclear. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unclear. |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up 100%. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the methods section have been reported on. |
| Other bias | Low risk | No evidence of other forms of bias. |
CTG: cardiotocography
FHR: fetal heart rate
MST: manual stimulation test
NST: non‐stress test
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Non‐reactive cardiotocography Show forest plot | 2 | 2350 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.02, 6.20] |
| Analysis 1.1 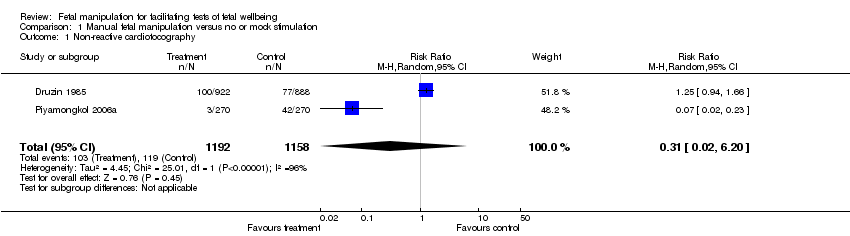 Comparison 1 Manual fetal manipulation versus no or mock stimulation, Outcome 1 Non‐reactive cardiotocography. | ||||
| 2 Perinatal deaths | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal anxiety | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Mean time of fetal heart rate remaining unreactive Show forest plot | 2 | 560 | Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐9.61, 5.03] |
| Analysis 1.5  Comparison 1 Manual fetal manipulation versus no or mock stimulation, Outcome 5 Mean time of fetal heart rate remaining unreactive. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Non‐reactive cardiotocography Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.83, 2.61] |
| Analysis 2.1  Comparison 2 Manual fetal manipulation versus vibroacoustic stimulation, Outcome 1 Non‐reactive cardiotocography. | ||||
| 2 Need for contraction‐stress test Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.67 [0.72, 9.86] |
| Analysis 2.2 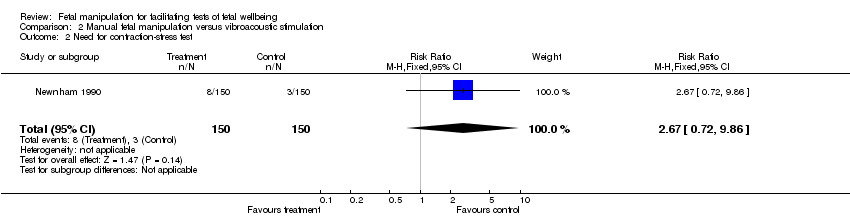 Comparison 2 Manual fetal manipulation versus vibroacoustic stimulation, Outcome 2 Need for contraction‐stress test. | ||||

.'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
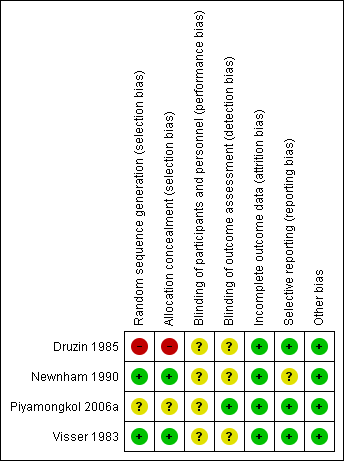
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Manual fetal manipulation versus no or mock stimulation, Outcome 1 Non‐reactive cardiotocography.

Comparison 1 Manual fetal manipulation versus no or mock stimulation, Outcome 5 Mean time of fetal heart rate remaining unreactive.
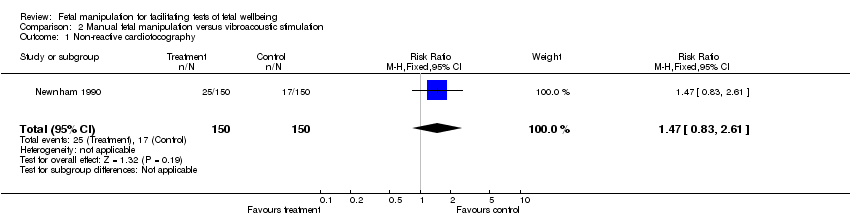
Comparison 2 Manual fetal manipulation versus vibroacoustic stimulation, Outcome 1 Non‐reactive cardiotocography.
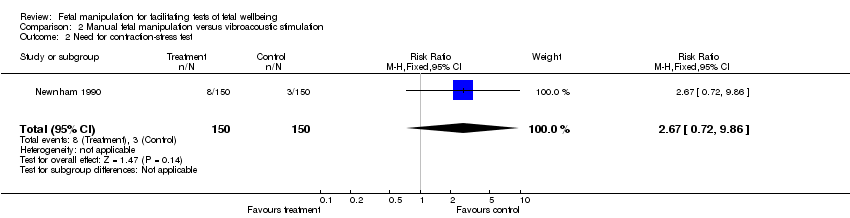
Comparison 2 Manual fetal manipulation versus vibroacoustic stimulation, Outcome 2 Need for contraction‐stress test.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Non‐reactive cardiotocography Show forest plot | 2 | 2350 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.02, 6.20] |
| 2 Perinatal deaths | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Maternal anxiety | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Mean time of fetal heart rate remaining unreactive Show forest plot | 2 | 560 | Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐9.61, 5.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Non‐reactive cardiotocography Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.83, 2.61] |
| 2 Need for contraction‐stress test Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.67 [0.72, 9.86] |

