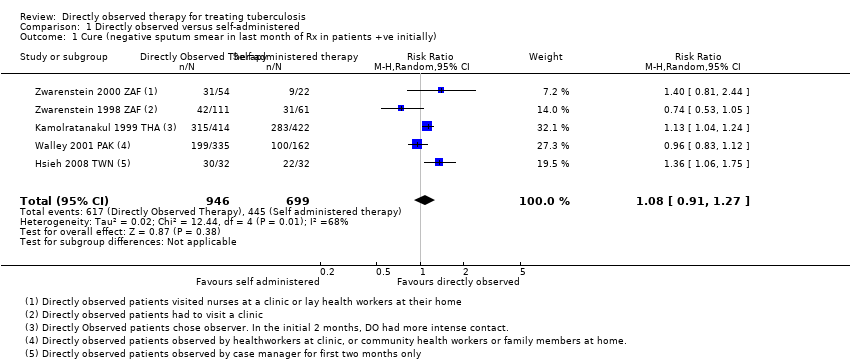
| 1 Cure (negative sputum smear in last month of Rx in patients +ve initially) Show forest plot | 5 | 1645 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.27] |
|
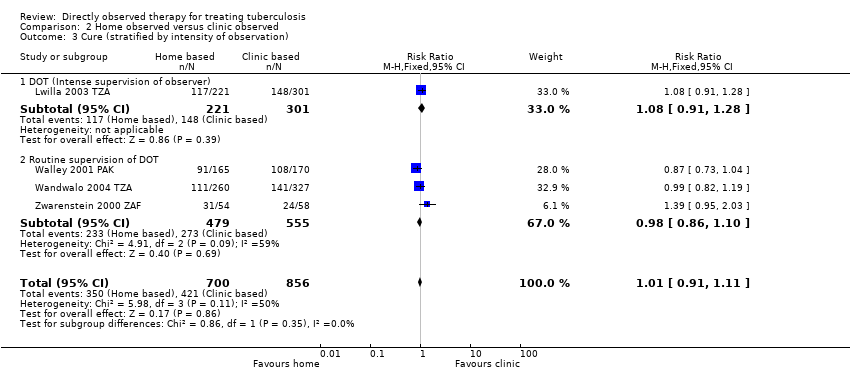
| 2 Cure (by intensity of monitoring in control group) Show forest plot | 5 | 1645 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.15] |
|
| 2.1 Monthly monitoring of patients in self administered group | 2 | 900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [1.06, 1.25] |
| 2.2 Once every two weeks monitoring of patients in self‐administered group | 1 | 497 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.83, 1.12] |
| 2.3 Weekly monitoring of patients in self‐administered group | 2 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.68, 1.21] |
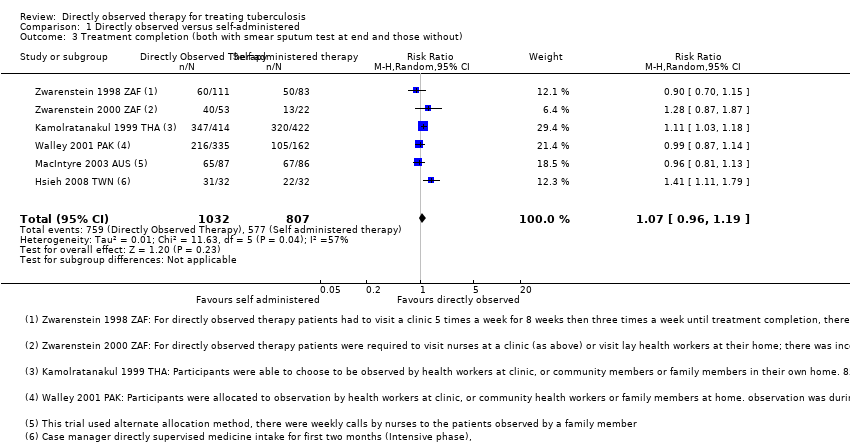
| 3 Treatment completion (both with smear sputum test at end and those without) Show forest plot | 6 | 1839 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.96, 1.19] |
|
| 4 Treatment completion (grouped by frequency of monitoring in the self‐administered therapy group) Show forest plot | 6 | 1839 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.96, 1.19] |
|
| 4.1 Monthly monitoring of self‐administered treatment | 3 | 1073 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.95, 1.31] |
| 4.2 Once every two weeks monitoring of self‐administered treatment | 1 | 497 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.87, 1.14] |
| 4.3 Weekly monitoring of self‐administered treatment | 2 | 269 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.74, 1.46] |