Akupunktura po przebytym udarze mózgu
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 35, control: 41 Health conditions before stroke: without severe mental disease, dementia, Parkinson's disease, heart failure, hepatic failure, or severe renal dysfunction | |
| Interventions | Treatment group: 2 scalp acupoints, manual twirling stimulation, 40 minutes/session for 2 weeks, but total number of sessions not stated | |
| Outcomes | Change in MESSS score at 14 days | |
| Notes | FU: 14 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated random number list | |
| Participants | Country: China (Hong Kong) Treatment: 10, control: 8 Health conditions before the stroke: not stated | |
| Interventions | Treatment group: 3 motor‐implicated acupoints (LI4, PC6, LI11), unilaterally on the paretic hand of the participants, manual twirling and electrical stimulation, Both groups: routine, inpatient stroke rehabilitation program including physical and occupational therapy | |
| Outcomes | Motricity Index, BI, FMA, and grip power before and after treatment Adverse events Number of deaths | |
| Notes | FU: 8 weeks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number list |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of patients |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | High risk | 1 in treatment group and 4 in control group did not finish predetermined treatment and evaluation schedules. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, using random number table Blinding: not stated | |
| Participants | Country: China Treatment: 95, control: 72 Health conditions before stroke: not stated | |
| Interventions | Treatment group: 2 acupoints (ST 9), manual twirling stimulation, 10 minutes/session, once a day for 20 days | |
| Outcomes | Number of participants with improvement (MESSS score decrease > 18%) at 20 days | |
| Notes | FU: 20 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table used |
| Allocation concealment (selection bias) | Low risk | Random number list read by doctor not entering participants into the trial |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 40, control: 40 Health conditions before stroke: without severe medical disease, such as heart failure, hepatic failure, severe renal dysfunction, infection, or shock Comparability: age, sex, MESSS similar | |
| Interventions | Treatment group: 4 areas of main acupoints (bilateral upper and lower energizer) and 6 areas of auxiliary acupoints (hepatic area, cardiac area, renal area, spleen area, bile area, and middle energizer) according to clinical symptoms, manual stimulation, 30 minutes/session, 5 sessions a week for 3 months | |
| Outcomes | SSS, BI, and FMA before and after treatment Number of BI < 60 points after treatment Number of deaths | |
| Notes | FU: 3 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 100, control: 100 Health conditions before stroke: without consciousness disturbance, neurological signs caused by brain tumor, trauma or cerebral parasitic disease, heart failure, hepatic failure, or severe renal dysfunction | |
| Interventions | Treatment group: acupoints in upper and lower limbs including LI11, LI10, PC6, SJ5, SP6 etc., manual stimulation, 30 minutes/session, once a day for 30 days | |
| Outcomes | FMA and BI evaluated before and after treatment Presence of adverse events | |
| Notes | FU: 30 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, randomization computer generated by independent research staff using software | |
| Participants | Country: China Treatment: 125, control: 125 Health conditions before stroke: without serious heart, liver, or kidney‐related disease; blood coagulation dysfunction; or congenital disabilities; for women, this study excluded those who were pregnant or breastfeeding | |
| Interventions | Treatment group: 2 to 3 needles penetrated through the top midline, MS‐6, MS‐7 of the lesion side for scalp acupuncture. Acupoints in upper and lower limbs included LI15, LI11, LI10, TE5, ST34, ST36, GB34, SP6, etc., manual stimulation, 30 minutes/session, 6 days per week for 3 weeks | |
| Outcomes | NIHSS and FMA evaluated at baseline, week 1, week 3, and week 7 Presence of adverse events | |
| Notes | FU: 7 weeks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization computer generated by independent research staff using software |
| Allocation concealment (selection bias) | Low risk | Generated list of random numbers placed into sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | High risk | 2 in acupuncture group and 3 in control group lost to follow‐up; 3 in acupuncture group and 1 in control group discontinued intervention |
| Selective reporting (reporting bias) | Low risk | Outcomes in this trial in accordance with those in the protocol |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated randomization | |
| Participants | Country: China Health conditions before stroke: without serious heart, lung, liver, or kidney‐related disease; coagulation‐related intracerebral hemorrhage; subarachnoid hemorrhage; primary ventricular hemorrhage; mental disease | |
| Interventions | Treatment group: 2 acupoints (DU20, EX‐HN5), manual twirling stimulation, 30 minutes/session, once a day for 28 days | |
| Outcomes | BI before and after treatment Number of deaths | |
| Notes | FU: 28 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Health conditions before stroke: not stated | |
| Interventions | Treatment group: 2 acupoints (DU20, GB7), manual twirling stimulation, 24 minutes/session, once per day for 30 days | |
| Outcomes | Change in MESSS score at 30 days | |
| Notes | FU: 30 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated random number list stratified according to side of cerebral lesion, diabetes, and hospital | |
| Participants | Country: Sweden < 7 days from stroke onset 100% CT scan before entry Health conditions before stroke: without severe aphasia, unconsciousness, an earlier cerebral lesion (with a documented need of care), or treatment with a cardiac pacemaker | |
| Interventions | Treatment group: 10 acupoints (DU20, LI11, ST38, EX mob, SJ5), manual or electrical stimulation, 30 minutes/session, twice per week for 10 weeks | |
| Outcomes | Change in SSS score at 3, 12 months | |
| Notes | FU: 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number |
| Allocation concealment (selection bias) | Low risk | Central randomization by telephone |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | For BI, 1 in deep acupuncture group and 1 in superficial acupuncture group lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, simple randomization via coin tossing | |
| Participants | Country: China Health conditions before stroke: without subarachnoid hemorrhage; serious heart, liver, or kidney‐related disease; mental disease; for women, this study excluded those who were pregnant or breastfeeding | |
| Interventions | Treatment group: eye, scalp, and body acupoints including LI4, LI10 PC6, B12 ST40, PC6, ST36, LR3, etc., manual or electrical stimulation, 30 minutes/session, 6 times a week for 2 weeks | |
| Outcomes | Change in MESSS score before and after treatment | |
| Notes | FU: 14 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence generated via simple randomization |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Low risk | No participants withdrawn or lost to FU |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated random number list stratified with BI Numbers of losses to FU: 2 in acupuncture group, 4 in control group | |
| Participants | Country: UK Treatment: 47, control: 45 Health conditions before stroke: without previous stroke or TIA, serious comorbidity, cardiac pacemaker | |
| Interventions | Treatment group: 10 acupoints on paralyzed side, manual (GB20, GB31, GB43, etc.) or electrical stimulation (LI10, SJ5, GB34), 30 minutes/session, 3 times per week for 4 weeks Both groups: drug therapy, routine physiotherapy, and occupational therapy | |
| Outcomes | BI, Motricity Index, NHP at entry, 3, 6, 12, 24, and 52 weeks Adverse events | |
| Notes | FU: 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number list stratified with BI |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants not blinded to treatment |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | 13 in acupuncture group and 12 in control group lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, stratified randomization with envelopes, following the principle of simple block randomization | |
| Participants | Country: Taiwan, Republic of China Treatment: 30, control: 33 Within 2 weeks from stroke onset Health conditions before stroke: without acute life‐threatening illness, significant systemic disease, or hemodynamic instability | |
| Interventions | Treatment group: 9 acupoints (GV20, bilateral GB20, and LI15, LI11, LI4, GB31, GB34, St36 on paralyzed side), electrical stimulation, 20 minutes/session, 2 courses per week, with a total of 8 sessions in 1 month | |
| Outcomes | Number requiring institutional care after discharge | |
| Notes | FU: 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomization with envelopes, following the principle of simple block randomization |
| Allocation concealment (selection bias) | Low risk | Concealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessor |
| Incomplete outcome data (attrition bias) | High risk | 5, 6, 8, 10 participants (at 2 weeks, 4 weeks, 3 months, and 6 months, respectively) in acupuncture group, corresponding figures for control group 2, 3, 9, 11 Rate of loss to FU over 30% |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, methods of randomization not stated | |
| Participants | Country: China (Taiwan) Treatment: 15, control: 15 Health conditions before stroke: without history of previous stroke, coma, any other acute life‐threatening disease, significant systemic disease, or anticoagulant therapy Comparability: age, sex, risk factors, and location of stroke similar, more hemispheric stroke and less lacunar stroke in acupuncture group | |
| Interventions | Treatment group: more than 24 acupoints (scalp motor area, GB21, LI11, GB34, EX‐UE7, BL60, and LR3 selected routinely), electrical stimulation (9.4 Hz), 30 to 60 minutes/session, every other day for 4 weeks | |
| Outcomes | Change in SSS score at 28, 90 days | |
| Notes | FU: 90 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Health conditions before stroke: without unconsciousness, peptic ulcer, infective endocarditis, atrial fibrillation, or severe renal dysfunction | |
| Interventions | Treatment group: 4 to 6 acupoints, pricking blood therapy, once a day for 7 days | |
| Outcomes | Change in MESSS score at 7 days | |
| Notes | FU: 7 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 60, control: 60 Health conditions before stroke: not stated | |
| Interventions | Treatment group: more than 14 acupoints (DU20, DU23, and DU26 selected routinely), manual twirling or electrical stimulation, 60 minutes/session, 5 times a week for 40 days | |
| Outcomes | Number of participants with improvement (MESSS score decrease > 8) at 40 days | |
| Notes | FU: 40 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, stratified randomization with envelopes | |
| Participants | Country: Sweden Health conditions before stroke: without pacemaker treatments | |
| Interventions | Treatment group: 10 acupoints (DU20, ST40, ST36, GB34, LI4, LI11, SJ5, etc.), manual and electrical stimulation, 30 minutes/session, twice a week for 10 weeks | |
| Outcomes | Motor function score at 1, 3 months | |
| Notes | FU: 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomization with envelopes |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes but not sequentially numbered or opaque |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated randomization | |
| Participants | Country: Sweden Health conditions before stroke: without previous neurological, psychiatric, or other disorder, making it difficult to pursue treatment or evaluation | |
| Interventions | Treatment group: 9 to 10 acupoints (LI4, ST36, DU20, LI11, ST40, EX28:21, EX36:1, GB34), manual and/or electrical stimulation, 30 minutes/session, twice a week for 10 weeks | |
| Outcomes | Motor function (RMI, walk speed, ability to walk 10 meters) at 3, 12 months | |
| Notes | FU: 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | For BI, 6 in acupuncture group, 6 in control group lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Health conditions before stroke: not stated | |
| Interventions | Treatment group: 8 acupoints (DU20, ST36, PC6, LI4, etc.), manual twirling stimulation, 20 minutes/session, once a day for 12 days | |
| Outcomes | Change in MESSS at 12 days | |
| Notes | FU: 12 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, randomized via an online random number generator Numbers with incomplete outcome data: 2 in the acupuncture group, 5 in the control group | |
| Participants | Country: Taiwan, Republic of China Health conditions before stroke: without a history of stroke or hemorrhage after ischemic stroke, cerebellar infarction, seizures, serious medical disease, cancer, or bleeding tendency; for women, this study excluded those who were pregnant or breastfeeding | |
| Interventions | Treatment group: 3 arm points, 3 leg points, 7 scalp points (LI11, TE5, LI4, ST36, SP6, LR3, etc.), manual twirling stimulation, 15 to 20 minutes/session, once a day for 2 weeks | |
| Outcomes | Changes in FMA and FIM at 4 weeks, as well as changes in NIHSS score, daily quality of life, and independence at 12 weeks | |
| Notes | FU: 12 weeks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomized via an online random number generator |
| Allocation concealment (selection bias) | Low risk | Generated code sealed in an envelope |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of assessors |
| Incomplete outcome data (attrition bias) | High risk | 7 of 38 participants did not complete the study. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China. 60 participants (40 men, mean age 69.5 ± 7.1 years in treatment group, mean age 66.5 ± 8.8 years in control group) with acute ischemic stroke Treatment: 30, control: 30 2 to 14 days from stroke onset Health conditions before stroke: without liver or kidney‐related disease, neurological signs caused by brain tumor, trauma or cerebral parasitic disease, or mental disease | |
| Interventions | Treatment group: 3 to 5 acupoints, manual twirling stimulation, treated for 20 days | |
| Outcomes | Change in MESSS at end of FU | |
| Notes | FU: 20 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 53, control: 52 Within 2 weeks from stroke onset Health conditions before stroke: without intracerebral hemorrhage; subarachnoid hemorrhage; history of hypertension, diabetes mellitus, severe heart, liver, lung, or kidney‐related disease or mental disease; women who were pregnant or breastfeeding excluded | |
| Interventions | Treatment group: scalp acupuncture (bilateral DU20 and GB7; EX‐HN1 and GB6 at lesion side) and body acupuncture (LI11, HT3, LI4, etc.), manual twirling stimulation, 30 minutes/session, once per day for 14 days | |
| Outcomes | Change in MESSS and FIM scores at end of follow‐up | |
| Notes | FU: 14 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated C: unclear | |
| Participants | Country: China Health conditions before stroke: without heart, liver, lung, or kidney‐related disease; or dysfunction of coagulation function | |
| Interventions | Treatment group: 2 areas of main acupoints (upper energizer and lower energizer), 3 areas of auxiliary acupoints (hepatic area, cardiac area, and renal area) according to clinical symptoms; manual twirling stimulation, 30 minutes/session, once a day for 8 days then rest 2 days, repeated 4 times | |
| Outcomes | BI before and after treatment | |
| Notes | FU: mean 40 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, stratified by baseline NIHSS score < 20 or ≥ 20, age < 70 years or ≥ 70 years, and whether affected side was dominant or non‐dominant | |
| Participants | Country: England 116 participants (60 men, mean age 74.8 ± 10.0 years in treatment group, mean age 74.1 ± 10.2 years in control group) with acute ischemic or hemorrhagic stroke ≤ 4 weeks from stroke onset All had CT scan before entry. Health conditions before stroke: without preexisting disability leading to modified Rankin score ≥ 3, or recent history of other serious diseases Comparability: sex, age, previously disabled, dominance of affected side similar | |
| Interventions | Treatment group: 10 acupoints (BL66, LI1, HT3, HT4, GB43, etc.), manual stimulation, ≥ 20 minutes/session, received between 9 and 12 sessions of real acupuncture during 2 weeks | |
| Outcomes | Change in Barthel ADL score, NIHSS score, Motoricity Index at end of treatment QOL score (EQ‐5D and EQ‐VAS) at end of treatment Death Adverse events | |
| Notes | FU: 2 weeks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified by baseline NIHSS score < 20 or ≥ 20, age < 70 years or ≥ 70 years, and whether affected side was dominant or non‐dominant |
| Allocation concealment (selection bias) | Low risk | Sequential, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | 2 in acupuncture group and 0 in control group lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer software used to allocate participants stratified according to hospital | |
| Participants | Country: China Treatment: 50, control: 50 Within 14 days from stroke onset Health conditions before stroke: without severe hepatic or renal dysfunction, unconsciousness, mental disease, or dementia | |
| Interventions | Treatment group: 3 main acupoints (DU26, PC6, SP6) and 2 auxiliary acupoints (HT1, BL40), manual twirling stimulation, 30 minutes per session, once per day for 2 weeks | |
| Outcomes | Change in FMA and BI after treatment BI score ≤ 60 at 3 months | |
| Notes | FU: 3 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer software used to allocate participants stratified according to hospital |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated sequence | |
| Participants | Country: China Treatment: 145, control: 145 Health conditions before stroke: without history of rheumatoid arthritis or any other illness or injury that could interfere with participation in the study Comparability: age, sex, NIHSS score, and duration of symptoms similar between 2 groups | |
| Interventions | Treatment group: resuscitating acupuncture, 6 main acupoints (PC6, DU26, SP6, HT1, BL40, LU5) and auxiliary acupoints according to clinical symptoms, manual twirling stimulation, 7 times a week for 4 weeks | |
| Outcomes | NIHSS at 2, 4 weeks, CSS at 4 weeks, and SS‐QOL at 6 months BI, relapse, and death up to 6 months Adverse events | |
| Notes | FU: 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Low risk | 1 in acupuncture group and 2 in control group lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, stratified randomization with random permuted blocks of 4 | |
| Participants | Country: China (Hong Kong) Health conditions before stroke: without hemodynamic instability, history of dementia, impaired cognition or receptive aphasia | |
| Interventions | Treatment group: 10 main acupoints and 6 auxiliary acupoints on the paretic side, manual twirling stimulation and/or electrical stimulation, 30 minutes/session, 3 times a week for 8 weeks then 2 times a week for 2 weeks | |
| Outcomes | FMA at 10 weeks | |
| Notes | FU: 10 weeks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomization with random permuted blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | 14 participants dropped out the trial. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 60, control: 60 Within 7 days from stroke onset Health conditions before stroke: without severe heart, liver, or kidney‐related disease; or bone‐joint diseases that influence recovery of motor function | |
| Interventions | Treatment group: 2 areas of main acupoints (upper energizer and lower energizer) and other areas of auxiliary acupoints (hepatic area, cardiac area, renal area, gastric area, etc.) according to clinical symptoms, manual twirling stimulation, once a day for 14 days | |
| Outcomes | Change in MESSS at end of follow‐up | |
| Notes | FU: 14 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China 104 participants (66 men, mean age 64.16 ± 9.91 years in treatment group, mean age 67.82 ± 10.64 in control group) with acute ischemic stroke and hemorrhagic stroke Treatment: 52, control: 52 Health conditions before stroke: without unconsciousness, severe medical disease, brain tumor, brain injury, or parasitic disease | |
| Interventions | Treatment group: 6 main acupoints and more than 6 auxiliary acupoints, manual twirling stimulation, 30 minutes/session, 5 times a week until discharge from hospital | |
| Outcomes | Change in MESSS and BI at end of FU | |
| Notes | FU: mean 24 to 25 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of assessors |
| Incomplete outcome data (attrition bias) | Low risk | 2 participants in acupuncture group lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, with random number table | |
| Participants | Country: China Health conditions before stroke: without severe medical disease | |
| Interventions | Treatment group: 2 acupoints (DU20, GB7), manual twirling stimulation, 16 to 19 minutes/session, once a day for 15 days | |
| Outcomes | Change in mobility index at 15 days | |
| Notes | FU: 15 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Random number list read by doctor entering participants into trial |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, computer‐generated random number C: sequentially numbered, sealed, opaque envelopes | |
| Participants | Country: China 100 participants (60 men, mean age 65.3 ± 8.7 years in treatment group, mean age 65.5 ± 10.1 years in control group) with acute ischemic stroke Treatment: 51, control: 49 Health conditions before stroke: without history of paralysis, infection around acupoints, coma, shock, or severe medical diease | |
| Interventions | Treatment group: 4 main acupoints and more than 7 auxiliary acupoints, manual twirling stimulation, 30 minutes/session, 6 times a week for 3 weeks | |
| Outcomes | Numbers of deaths or cases of dependency (trial authors' own definition) at 6 months Numbers of deaths from all causes at 6 months Adverse events | |
| Notes | FU: 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 30, control: 30 Health conditions before stroke: without cognitive decline, heart or lung failure, or limb fracture | |
| Interventions | Treatment group: 10 to 15 acupoints (LI11, LI10, LU5, etc.), electrical stimulation, 20 minutes/session, once a day for 20 days | |
| Outcomes | Change in FMA at end of follow‐up | |
| Notes | FU: 20 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, centrally by computer‐generated random numbers, stratified by participating centre | |
| Participants | Country: China Treatment: 427, control: 435 Between 3 and 10 days from stroke onset Health conditions before stroke: without dependency in ADLs before present stroke, infection in acupuncture sites, severe aphasia or unconsciousness, other severe complications or comorbidities such as heart/renal function failure | |
| Interventions | Treatment group: 5 main acupoints (DU26 and PC6 at both sides, SP6 at paretic side) and 9 auxiliary acupoints (DU20, ST36, ST40, LK3, LL5, etc.), manual and/or electrical stimulation, 30 minutes/session, 5 times per week for 3 to 4 weeks (in the pilot study) or 3 weeks (in the main study) | |
| Outcomes | Numbers of deaths/cases of disability according to BI at 6 months Numbers of death/need for institutional care at 6 months Case fatality and changes in neurological deficit score at end of treatment periods or at discharge Severe adverse events and adverse events directly related to acupuncture | |
| Notes | FU: 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centrally by computer‐generated random numbers, stratified by participating center |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | 40 (9.4%) participants in acupuncture group and 39 (9.0%) in control group at 6 months lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Outcomes in this trial were in accordance with those in the protocol. |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Methods | RCT, method of randomization not stated | |
| Participants | Country: China Treatment: 35, control: 35 Health conditions before stroke: without severe medical disease such as heart/liver/renal function failure | |
| Interventions | Treatment group: 2 main acupoints (HT1, Ex‐UE) and 2 auxiliary acupoints, electrical stimulation, 20 minutes/session, once a day for 30 days | |
| Outcomes | Change in FMA at 30 days | |
| Notes | FU: 30 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
acup: acupuncture.
ADL: activity of daily living.
BI: Barthel Index.
C: concealment of allocation.
CSS: Chinese Stroke Scale.
CT: computed tomography.
EQ‐5D: EuroQoL–5‐Dimensional forma.
EQ‐VAS: EuroQoL–Visual Analog Scale.
FIM: Functional Independence Measurement.
FMA: Fugl‐Meyer Assessment of Physical Performance.
fMRI: functional magnetic resonance imaging.
FU: follow‐up.
ITT: intention‐to‐treat.
MESSS: modified Edinburgh‐Scandinavian Stroke Scale.
MMSE: Mini Mental State Examination.
MRI: magnetic resonance imaging.
NHP: Nottingham Health Profile.
NIHSS: National Institutes of Health Stroke Scale.
QOL: quality of life.
RCT: randomized controlled trial.
RMI: Rivermead Mobility Index.
SS‐QOL: Stroke‐Specific Quality of Life scale.
SSS: Scandinavian Stroke Scale.
TENS: transcutaneous electrical nerve stimulation.
TIA: transient ischemic attack.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Questionable randomization (patients in 5 hospitals were included, but patients in only 1 hospital were allocated into the control group) | |
| It was not possible to include data from this trial in the analysis (NIHSS and BI were evaluated before and after treatment, but mean change in NIHSS and BI were not available). | |
| Data from this trial were questionable (data were inconsistent in full text of published paper). | |
| It was not possible to include data from this trial in the analysis (BI was assessed before and after treatment, but number of participants independent after treatment was not available). | |
| It was not possible to include data from this trial in the analysis (MESSS was assessed before and after treatment, but mean change in MESSS was not available). | |
| Confounded trial (clinical treatment plus dynamic acupuncture vs clinical treatment plus traditional acupuncture vs no acupuncture) | |
| Confounded to the course of included patients with stroke | |
| It was not possible to include data from this trial in the analysis (BI was reported as mean ± SD, so data on death or dependency were not available). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| Questionable inclusion criteria (> 14 days from stroke onset included); types of participants questionable | |
| Trial aimed to assess effects of 2 kinds of acupuncture on acute stroke (acupuncture involving Du15 and Du16 in addition to other acupoints vs acupuncture involving other acupoints alone). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| Quasi‐randomised trials. The scale used to evaluate neurological function did not include a detailed description or reference, so reliability was uncertain. | |
| It was not possible to include data from this trial in the analysis (data on outcomes were not available). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis. Motor function and BI were assessed before and after treatment, but mean change in motor function score and number of participants independent after treatment were not available. | |
| It was not possible to include data from this trial in the analysis. MESSS scores, motor function, and BI were assessed before and after treatment, but mean change in neurological score and number of participants independent after treatment were not available. | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was unclear when acupuncture treatment was started after stroke onset; types of participants were questionable. | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| This trial did not define the course of acute stroke in inclusion criteria. | |
| It was not possible to include data from this trial in the analysis. Motor function was assessed before and after treatment, but mean change in motor function score after treatment was not available. | |
| Confounded (acupuncture vs nimodipine), questionable randomization (68 cases in acupuncture group and 30 cases in control group) | |
| Confounded (clinical treatment plus electro‐acupuncture vs clinical treatment plus active and/or passive functional exercise) | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Liu 2015). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| Quasi‐randomized trial | |
| Confounded (combined therapy of scalp cluster acupuncture and constraint‐induced movement therapy vs combined therapy of body acupuncture and traditional rehabilitation therapy) | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis. Neurological score was assessed by a scoring system based on principles of Traditional Chinese Medicine, but mean change in score after treatment was not available. | |
| Questionable inclusion criteria (participants within 3 days after stroke onset were included in abstract, and participants within 7 days were included in the main text; 120 participants were enrolled and randomized in this study in the main text, whereas only 90 participants were described in the results section and no information was provided on the remaining 30 participants) | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| Lack of information on acupoints, how to stimulate, how long per session, and how many sessions. In addition, it was not possible to obtain usable data for analysis. | |
| It was not possible to include data from this trial in the analysis (BI was evaluated before and after treatment, but mean change in BI was not available). | |
| Acupuncture points were stimulated by an adhesive surface electrode. | |
| This study included participants with subarachnoid hemorrhage. | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis. BI was assessed before and after treatment, but the number of participants independent at end of treatment was not available. | |
| It was not possible to include data from this trial in the analysis. MESSS scores, motor function, and BI were assessed before and after treatment, but mean change in neurological score and number of participants independent after treatment were not available. | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| Quasi‐randomized trial | |
| Questionable randomization (300 cases were randomly divided into 5 groups: control, 24‐hour acupuncture, 72‐hour acupuncture, 1‐week acupuncture, and 2‐week acupuncture from stroke onset) | |
| Data in this trial were questionable. Participants with acute ischemic stroke and BI < 70 were included and randomised in outpatient department. It was difficult to perform this trial in China, so the type of study selected was questionable. | |
| Confounded: acupuncture plus defibrase (5 U) vs defibrase (10 U) | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| Questionable randomization (145 cases in acupuncture group and 96 cases in control group) and no useful data available for analysis | |
| It was not possible to include data from this trial in the analysis (FMA was evaluated before and after treatment, but mean change in FMA score was not available). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis (BI and FMA were evaluated before and after treatment, but mean changes in BI and FMA were not available). | |
| Confounded (acupuncture vs routine drug treatment); questionable quasi‐randomization via alternate allocation (40/30) | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Guo 2006a). | |
| It was not possible to include data from this trial in the analysis. Motor function of limbs was assessed via Yishangtian Scale, but mean changes in scores for each group were not available. | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Liu 2015). | |
| It was not possible to include data from this trial in the analysis (see reason for exclusion of Zhen 2011). |
BI: Barthel Index.
FMA: Fugl‐Meyer Assessment of Physical Performance.
MESSS: modified Edinburgh‐Scandinavian Stroke Scale.
NIHSS: National Institutes of Health Stroke Scale.
SD: standard deviation.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Acupuncture for acute stroke: study protocol for a multicenter, randomized, controlled trial |
| Methods | RCT, computer‐generated by independent research staff using software |
| Participants | Country: China |
| Interventions | Treatment group: scalp acupuncture and electro‐acupuncture, manual twirling stimulation and electrical stimulation, 30 minutes per session, 6 times per week for 3 weeks |
| Outcomes | Changes in NIHSS score at the 1, 3, 4‐week follow‐up FMA, MMSE, Montreal Cognitive Assessment Videofluoroscopic swallowing study for swallowing ability Incidence of adverse events |
| Starting date | Started March 1, 2012 |
| Contact information | Correspondence: [email protected], Department of Acupuncture, The Third Affiliated Hospital of Zhejiang Chinese Medical University, No. 219 Moganshan Road, XiHu District, Hangzhou, Zhejiang Province 310005, China |
| Notes | FU: 4 weeks after treatment |
| Trial name or title | Acupuncture treatment for ischemic stroke in young adults: protocol for a randomized, sham‐controlled clinical trial |
| Methods | RCT: computer generated by independent research staff using SAS 9.3 software |
| Participants | Country: China |
| Interventions | Treatment group: motor area and sensory area of the lesion side for scalp acupuncture; IL15, LI11, ST31, GB34, etc., for body acupuncture; CV12, CV10, etc., for abdominal acupuncture; manual stimulation, 30 minutes per session, 3 times per week for 8 weeks |
| Outcomes | BI, FMA, and QOL at week 9 and week 20 Incidence of adverse events, mortality and recurrence rates, and QOL at 10 years, 30 years after stroke |
| Starting date | Not stated |
| Contact information | Correspondence to Professor Jianqiao Fang, Department of Acupuncture and Moxibustion, The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou City, Zhejiang Province, China; [email protected] |
| Notes | FU: 30 years |
| Trial name or title | Acupuncture for acute moderate thalamic hemorrhage: randomized controlled trial protocol |
| Methods | RCT: computer generated via Package for Encyclopaedia Medical Statistics 3.1 (PEMS 3.1) software C: generated list of random numbers to be placed into opaque sealed envelopes |
| Participants | Country: China |
| Interventions | Treatment group: scalp and body acupuncture (LI15, LI11, SJ5, LI4, ST34, ST36, etc.), manual stimulation, 30 minutes per session, once a day, 6 times per week for 6 weeks Control group: no acupuncture |
| Outcomes | Change in NIHSS score at 30 and 90 days Death or major disability at 90 days, need for surgery at 30 days, Glasgow Outcome Scale score at 90 days after thalamic hemorrhage |
| Starting date | January 2017 |
| Contact information | Correspondence: [email protected]. Department of Integrated Traditional and Western Medicine, West China Hospital, Sichuan University, Chengdu, China |
| Notes | FU: 90 days |
BI: Barthel Index.
C: concealment of allocation.
FMA: Fugl‐Meyer Assessment of Physical Performance.
FU: follow‐up.
MMSE: Mini Mental State Examination.
NIHSS: National Institutes of Health Stroke Scale.
QOL: quality of life.
RCT: randomized controlled trial.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependency at end of follow‐up Show forest plot | 11 | 1582 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.46, 0.79] |
| Analysis 1.1 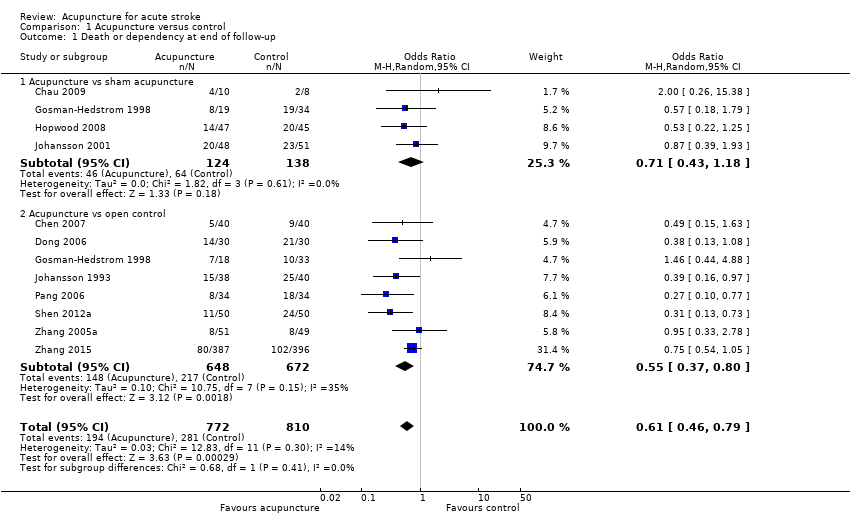 Comparison 1 Acupuncture versus control, Outcome 1 Death or dependency at end of follow‐up. | ||||
| 1.1 Acupuncture vs sham acupuncture | 4 | 262 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.43, 1.18] |
| 1.2 Acupuncture vs open control | 8 | 1320 | Odds Ratio (M‐H, Random, 95% CI) | 0.55 [0.37, 0.80] |
| 2 Death or dependency at end of follow‐up (> 3 months) Show forest plot | 8 | 1436 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.53, 0.85] |
| Analysis 1.2  Comparison 1 Acupuncture versus control, Outcome 2 Death or dependency at end of follow‐up (> 3 months). | ||||
| 2.1 Acupuncture vs sham acupuncture | 3 | 244 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.40, 1.12] |
| 2.2 Acupuncture vs open control | 6 | 1192 | Odds Ratio (M‐H, Random, 95% CI) | 0.62 [0.42, 0.93] |
| 3 Death or institutional care at end of follow‐up Show forest plot | 5 | 1120 | Odds Ratio (M‐H, Random, 95% CI) | 0.78 [0.54, 1.12] |
| Analysis 1.3  Comparison 1 Acupuncture versus control, Outcome 3 Death or institutional care at end of follow‐up. | ||||
| 3.1 Acupuncture vs sham acupuncture | 2 | 145 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.23, 0.96] |
| 3.2 Acupuncture vs open control | 4 | 975 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.61, 1.42] |
| 4 Change in global neurological deficit score at end of treatment period Show forest plot | 12 | 1086 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.36, 1.32] |
| Analysis 1.4 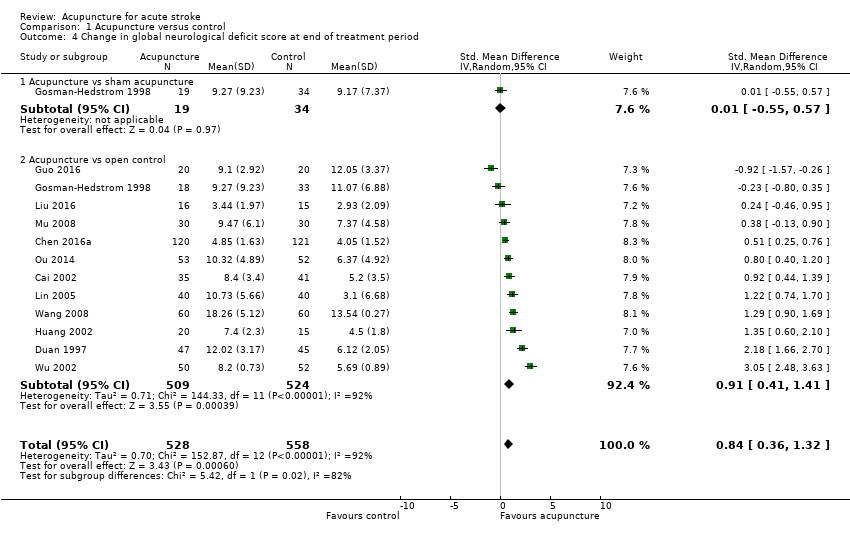 Comparison 1 Acupuncture versus control, Outcome 4 Change in global neurological deficit score at end of treatment period. | ||||
| 4.1 Acupuncture vs sham acupuncture | 1 | 53 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.55, 0.57] |
| 4.2 Acupuncture vs open control | 12 | 1033 | Std. Mean Difference (IV, Random, 95% CI) | 0.91 [0.41, 1.41] |
| 5 Motor function at end of acupuncture treatment period Show forest plot | 11 | 895 | Std. Mean Difference (IV, Random, 95% CI) | 1.08 [0.45, 1.71] |
| Analysis 1.5 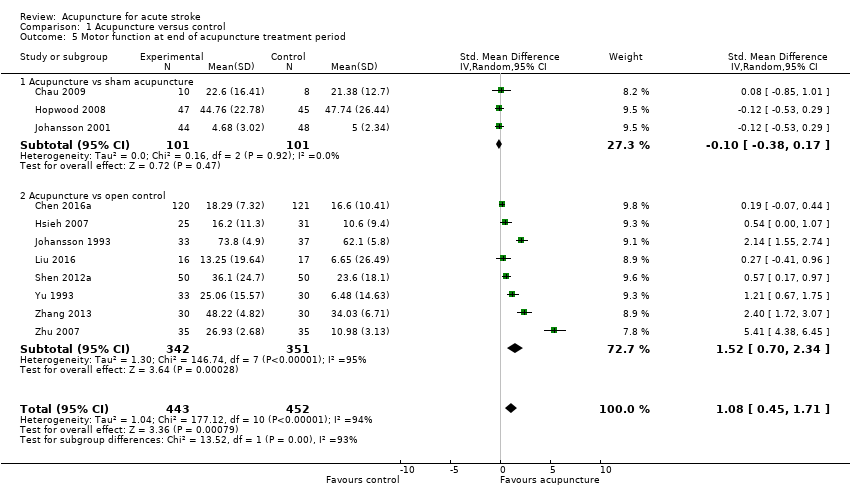 Comparison 1 Acupuncture versus control, Outcome 5 Motor function at end of acupuncture treatment period. | ||||
| 5.1 Acupuncture vs sham acupuncture | 3 | 202 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.38, 0.17] |
| 5.2 Acupuncture vs open control | 8 | 693 | Std. Mean Difference (IV, Random, 95% CI) | 1.52 [0.70, 2.34] |
| 6 Motor function at end of follow‐up (> 3 months) Show forest plot | 3 | 186 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.21, 0.37] |
| Analysis 1.6  Comparison 1 Acupuncture versus control, Outcome 6 Motor function at end of follow‐up (> 3 months). | ||||
| 6.1 Acupuncture vs sham acupuncture | 2 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.35, 0.31] |
| 6.2 Acupuncture vs open control | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [‐0.18, 1.05] |
| 7 Death within first 2 weeks Show forest plot | 18 | 1612 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.33, 2.55] |
| Analysis 1.7 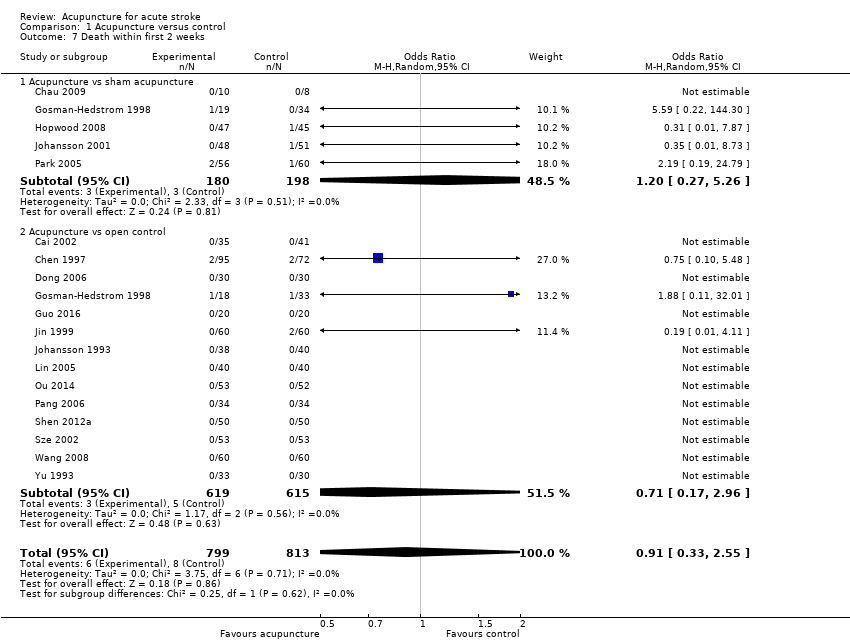 Comparison 1 Acupuncture versus control, Outcome 7 Death within first 2 weeks. | ||||
| 7.1 Acupuncture vs sham acupuncture | 5 | 378 | Odds Ratio (M‐H, Random, 95% CI) | 1.20 [0.27, 5.26] |
| 7.2 Acupuncture vs open control | 14 | 1234 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.17, 2.96] |
| 8 Death during whole follow‐up period Show forest plot | 22 | 2865 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.74, 1.58] |
| Analysis 1.8 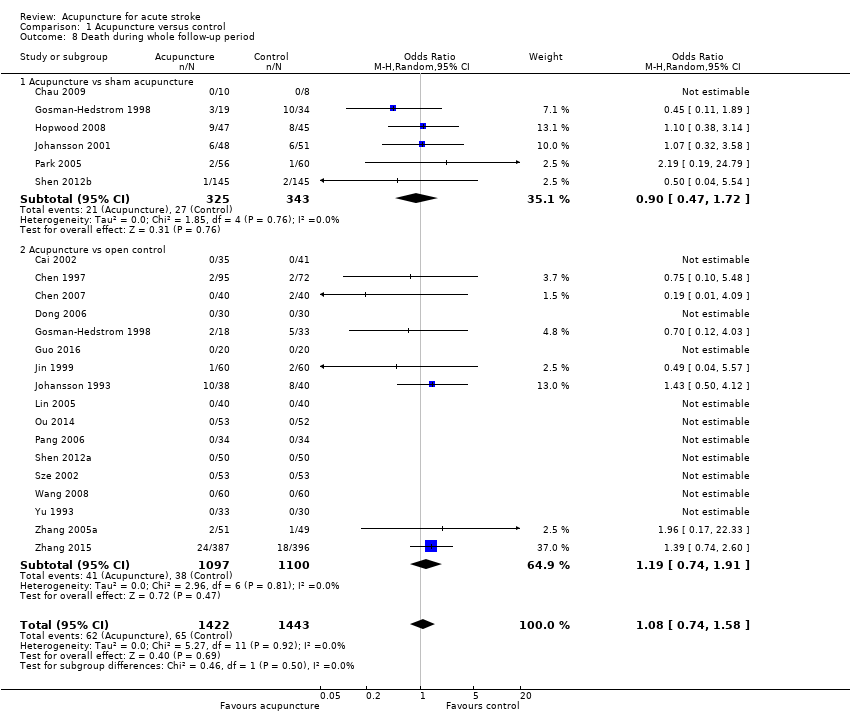 Comparison 1 Acupuncture versus control, Outcome 8 Death during whole follow‐up period. | ||||
| 8.1 Acupuncture vs sham acupuncture | 6 | 668 | Odds Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.72] |
| 8.2 Acupuncture vs open control | 17 | 2197 | Odds Ratio (M‐H, Random, 95% CI) | 1.19 [0.74, 1.91] |
| 9 Adverse events during treatment period Show forest plot | 5 | 576 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.29, 1.16] |
| Analysis 1.9  Comparison 1 Acupuncture versus control, Outcome 9 Adverse events during treatment period. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependency at end of follow‐up Show forest plot | 6 | 1094 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.54, 0.94] |
| Analysis 2.1  Comparison 2 Ischemic stroke versus hemorrhagic stroke, Outcome 1 Death or dependency at end of follow‐up. | ||||
| 1.1 Death or dependency in hemorrhagic stroke | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.13, 1.08] |
| 1.2 Death or dependency in ischemic stroke | 5 | 1034 | Odds Ratio (M‐H, Random, 95% CI) | 0.75 [0.56, 1.00] |

Funnel plot of comparison: 1 Acupuncture versus control, outcome: 1.1 Death or dependency at end of follow‐up.
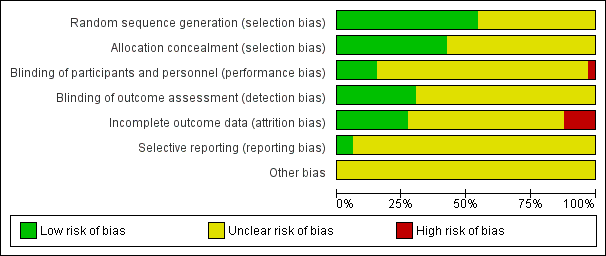
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Acupuncture versus control, Outcome 1 Death or dependency at end of follow‐up.

Comparison 1 Acupuncture versus control, Outcome 2 Death or dependency at end of follow‐up (> 3 months).
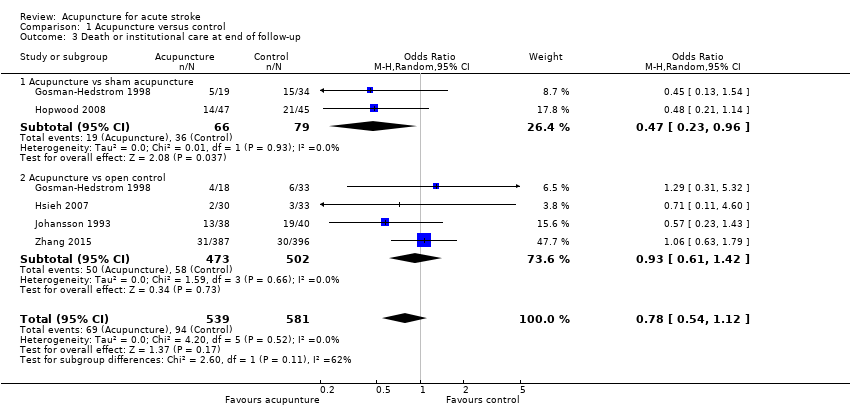
Comparison 1 Acupuncture versus control, Outcome 3 Death or institutional care at end of follow‐up.

Comparison 1 Acupuncture versus control, Outcome 4 Change in global neurological deficit score at end of treatment period.
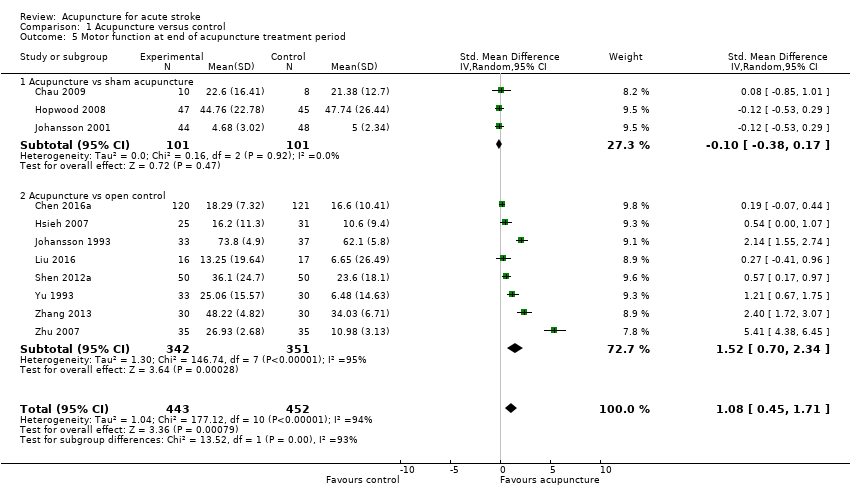
Comparison 1 Acupuncture versus control, Outcome 5 Motor function at end of acupuncture treatment period.

Comparison 1 Acupuncture versus control, Outcome 6 Motor function at end of follow‐up (> 3 months).

Comparison 1 Acupuncture versus control, Outcome 7 Death within first 2 weeks.
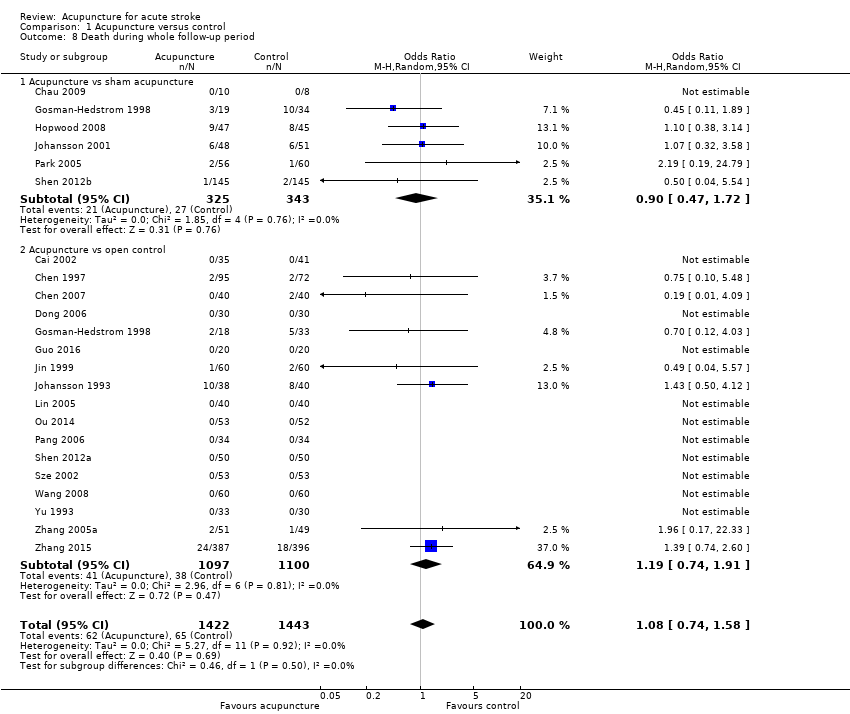
Comparison 1 Acupuncture versus control, Outcome 8 Death during whole follow‐up period.
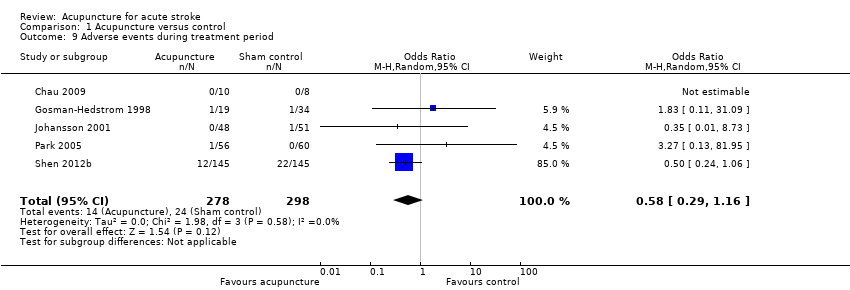
Comparison 1 Acupuncture versus control, Outcome 9 Adverse events during treatment period.
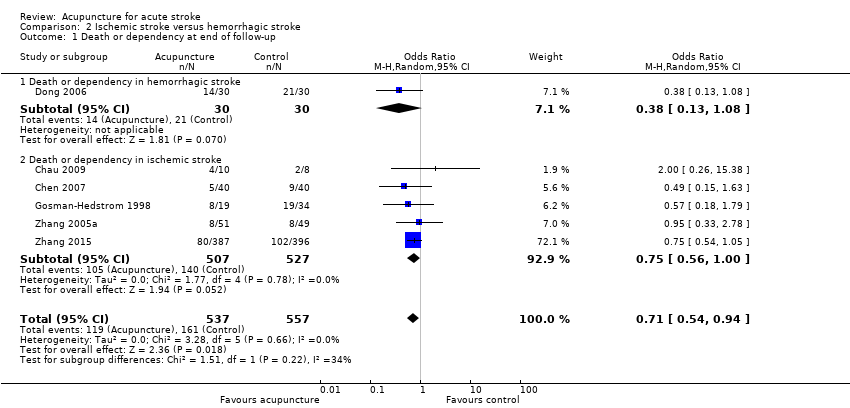
Comparison 2 Ischemic stroke versus hemorrhagic stroke, Outcome 1 Death or dependency at end of follow‐up.
| Acupuncture compared with all control for patients with acute stroke | ||||||
| Patient or population: patients with acute stroke | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Acupuncture | |||||
| Death or dependency at end of follow‐up | Study population | OR 0.61 | 1582 | ⊕⊝⊝⊝ | Dependency was defined as BI ≤ 60 (of a potential total of 100), BI ≤ 70 (of a potential total of 100), or BI ≤ 12 (of a potential total of 20). One trial used the trialists' own definition. | |
| 347 per 1000 | 245 per 1000 | |||||
| Death or dependency at end of follow‐up (> 3 months) | Study population | OR 0.67 | 1436 | ⊕⊝⊝⊝ | Dependency was defined as BI ≤ 60 (of a potential total of 100), BI ≤ 70 (of a potential total of 100), or BI ≤ 12 (of a potential total of 20). One trial used the trialists' own definition. | |
| 325 per 1000 | 244 per 1000 | |||||
| Moderate | ||||||
| 444 per 1000 | 349 per 1000 | |||||
| Death or institutional care at end of follow‐up | Study population | OR 0.78 | 1120 | ⊕⊕⊝⊝ | ||
| 162 per 1000 | 131 per 1000 | |||||
| Changes in global neurological deficit score at end of treatment period | Mean change in global neurological deficit score at end of treatment period in intervention groups was | 1086 | ⊕⊝⊝⊝ | Global neurological function was measured via modified Edinburgh‐Scandinavian Stroke Scale in 9 trials, NIHSS in 2, and SSS in 1. | ||
| Motor function at end of acupuncture treatment period | Mean motor function at end of acupuncture treatment period in intervention groups was | 895 | ⊕⊝⊝⊝ | Motor function was measured via Fugl‐Meyer Assessment in 7 trials, Motricity Index in 1, motor function score in 1, Rivermead Mobility Index in 1, and mobility index in 1. | ||
| Death within first 2 weeks | Study population | OR 0.91 | 1612 | ⊕⊕⊝⊝ | ||
| 10 per 1000 | 9 per 1000 | |||||
| Death during whole follow‐up period | Study population | OR 1.08 | 2865 | ⊕⊕⊝⊝ | ||
| 45 per 1000 | 48 per 1000 | |||||
| Adverse events related to acupuncture | See comments. | See comments. | See comments. | (13 studies) | ⊕⊕⊝⊝ | The incidence of adverse events directly related to acupuncture (such as pain, dizziness, faint) was approximately 6.17% (64/1037 participants) in the acupuncture group, and 1.35% (14/1037 participants) discontinued acupuncture. AEs related to sham acupuncture occurred in 8.0% (24/298) of participants. |
| *The basis for the assumed risk (eg, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOf the 33 included RCTs, the acupuncture treatment type and period were heterogeneous. The acupuncture treatment period ranged from one to three months. The acupoints varied across trials. The needling sensation could be provoked by manual stimulation or electrical stimulation. bDowngraded one level for serious inconsistency: variation in the definition of dependency and acupuncture treatment type and duration. cDowngraded two levels for very serious risk of bias: Among the 11 included trials, eight had risk of performance bias and seven had risk of detection bias; the result was not consistent with the sensitivity analysis using only sham controls. dDowngraded two levels for very serious risk of bias: Among the eight included trials, six had risk of performance bias and four had risk of detection bias; the result was not consistent with the sensitivity analysis using only sham controls. eDowngraded two levels for very serious risk of bias: Among the five included trials, four had risk of performance bias; the result was not consistent with the sensitivity analysis using only sham controls. fDowngraded two levels for very serious inconsistency: considerable statistical heterogeneity (I2 > 50%) and variation in acupuncture treatment type and duration. gDowngraded two levels for very serious risk of bias: Among the 13 included trials, at least eight trials had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. hDowngraded two levels for very serious risk of bias: Among the 11 included trials, at least six had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. iDowngraded two levels for very serious risk of bias: Among the 18 included trials, at least 10 trials had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. jDowngraded two levels for very serious risk of bias: Among the 22 included trials, at least 11 trials had risk of allocation bias, performance bias, or detection bias; the result was not consistent with the sensitivity analysis using only sham controls. kDowngraded two levels for very serious inconsistency: variation between trials in reporting of adverse events and in acupuncture treatment type and duration. | ||||||
| Acupuncture compared with sham control for patients with acute stroke | ||||||
| Patient or population: patients with acute stroke | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Acupuncture | |||||
| Death or dependency at end of follow‐up | Study population | OR 0.71 | 262 | ⊕⊕⊝⊝ | ||
| 464 per 1000 | 384 per 1000 | |||||
| Death or dependency at end of follow‐up (> 3 months) | Study population | OR 0.67 | 244 | ⊕⊕⊝⊝ | ||
| 476 per 1000 | 376 per 1000 | |||||
| Death or institutional care at end of follow‐up | Study population | OR 0.47 | 145 | ⊕⊕⊝⊝ | ||
| 456 per 1000 | 286 per 1000 | |||||
| Changes in global neurological deficit score at end of treatment period | Mean change in global neurological deficit score at end of treatment period in intervention groups was | 53 | ⊕⊕⊝⊝ | |||
| Motor function at end of acupuncture treatment period | Mean motor function at end of acupuncture treatment period in intervention groups was | 202 | ⊕⊕⊝⊝ | |||
| Death within first 2 weeks | Study population | OR 1.20 | 378 | ⊕⊕⊝⊝ | ||
| 15 per 1000 | 4 per 1000 | |||||
| Death during whole follow‐up period | Study population | OR 0.90 | 668 | ⊕⊕⊝⊝ | ||
| 79 per 1000 | 79 per 1000 | |||||
| Adverse events related to acupuncture | See comments. | See comments. | OR 0.58 (0.29 to 1.16) | 576 (5 studies) | ⊕⊕⊝⊝ | The incidence of adverse events directly related to acupuncture (such as pain, dizziness, faint) was approximately 8.0% (24/298) in sham acupuncture patients. |
| *The basis for the assumed risk (eg, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOf the 33 included RCTs, the acupuncture treatment type and period were heterogeneous. The treatment period for acupuncture ranged from one to three months. Acupoints varied across trials. The needling sensation could be provoked by manual stimulation or electrical stimulation. bDowngraded one level for serious imprecision: small number of studies and wide confidence intervals. cDowngraded one level for serious risk of bias: Among the four included trials, two trials had risk of performance bias or attrition bias. dDowngraded one level for serious risk of bias: Among the three included trials, one trial had risk of performance bias. eDowngraded one level for serious risk of bias: Among the two included trials, one trial had risk of performance bias. fDowngraded two levels for very serious imprecision: single study and very wide confidence intervals. gDowngraded one level for serious risk of bias: Among the three included trials, at least two trials had risk of performance bias or attrition bias. hDowngraded one level for serious risk of bias: Among the five included trials, at least two trials had risk of performance bias or attrition bias. iDowngraded one level for serious risk of bias: Among the six included trials, at least two trials had risk of performance bias or attrition bias. jDowngraded one level for serious inconsistency: Reporting of adverse events varied between trials. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependency at end of follow‐up Show forest plot | 11 | 1582 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.46, 0.79] |
| 1.1 Acupuncture vs sham acupuncture | 4 | 262 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.43, 1.18] |
| 1.2 Acupuncture vs open control | 8 | 1320 | Odds Ratio (M‐H, Random, 95% CI) | 0.55 [0.37, 0.80] |
| 2 Death or dependency at end of follow‐up (> 3 months) Show forest plot | 8 | 1436 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.53, 0.85] |
| 2.1 Acupuncture vs sham acupuncture | 3 | 244 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.40, 1.12] |
| 2.2 Acupuncture vs open control | 6 | 1192 | Odds Ratio (M‐H, Random, 95% CI) | 0.62 [0.42, 0.93] |
| 3 Death or institutional care at end of follow‐up Show forest plot | 5 | 1120 | Odds Ratio (M‐H, Random, 95% CI) | 0.78 [0.54, 1.12] |
| 3.1 Acupuncture vs sham acupuncture | 2 | 145 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.23, 0.96] |
| 3.2 Acupuncture vs open control | 4 | 975 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.61, 1.42] |
| 4 Change in global neurological deficit score at end of treatment period Show forest plot | 12 | 1086 | Std. Mean Difference (IV, Random, 95% CI) | 0.84 [0.36, 1.32] |
| 4.1 Acupuncture vs sham acupuncture | 1 | 53 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.55, 0.57] |
| 4.2 Acupuncture vs open control | 12 | 1033 | Std. Mean Difference (IV, Random, 95% CI) | 0.91 [0.41, 1.41] |
| 5 Motor function at end of acupuncture treatment period Show forest plot | 11 | 895 | Std. Mean Difference (IV, Random, 95% CI) | 1.08 [0.45, 1.71] |
| 5.1 Acupuncture vs sham acupuncture | 3 | 202 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.38, 0.17] |
| 5.2 Acupuncture vs open control | 8 | 693 | Std. Mean Difference (IV, Random, 95% CI) | 1.52 [0.70, 2.34] |
| 6 Motor function at end of follow‐up (> 3 months) Show forest plot | 3 | 186 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.21, 0.37] |
| 6.1 Acupuncture vs sham acupuncture | 2 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.35, 0.31] |
| 6.2 Acupuncture vs open control | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [‐0.18, 1.05] |
| 7 Death within first 2 weeks Show forest plot | 18 | 1612 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.33, 2.55] |
| 7.1 Acupuncture vs sham acupuncture | 5 | 378 | Odds Ratio (M‐H, Random, 95% CI) | 1.20 [0.27, 5.26] |
| 7.2 Acupuncture vs open control | 14 | 1234 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.17, 2.96] |
| 8 Death during whole follow‐up period Show forest plot | 22 | 2865 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.74, 1.58] |
| 8.1 Acupuncture vs sham acupuncture | 6 | 668 | Odds Ratio (M‐H, Random, 95% CI) | 0.90 [0.47, 1.72] |
| 8.2 Acupuncture vs open control | 17 | 2197 | Odds Ratio (M‐H, Random, 95% CI) | 1.19 [0.74, 1.91] |
| 9 Adverse events during treatment period Show forest plot | 5 | 576 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.29, 1.16] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependency at end of follow‐up Show forest plot | 6 | 1094 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.54, 0.94] |
| 1.1 Death or dependency in hemorrhagic stroke | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.13, 1.08] |
| 1.2 Death or dependency in ischemic stroke | 5 | 1034 | Odds Ratio (M‐H, Random, 95% CI) | 0.75 [0.56, 1.00] |


