Liječenje pulpe kod opsežnog karijesa primarnih zubi
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT, parallel‐arm Children randomly assigned Conducted in the dental clinic of Azad University, Tehran, Iran. Operators were a dentist under the supervision of an endodontist | |
| Participants | 126 children, 126 teeth, mean age 6.5 years, standard deviation age 1.16 years, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 75 (1 visit) Rubber dam Caries removal prior to pulpal access: not mentioned Pulp access with high‐speed burr Pulpotomy amputation with excavator For haemostasis, moistened cotton pellet with saline Irrigation with saline Group 2: Pulpotomy (MTA); n = 51 (1 visit) Rubber dam Caries removal prior to pulpal access: not mentioned Pulp access with high‐speed burr Pulpotomy amputation with excavator For haemostasis, moistened cotton pellet with saline Irrigation with saline MTA applied after pulpotomy, followed by amalgam | |
| Outcomes | Clinical failure (spontaneous pain, swelling, pain on palpation or percussion and sinus tract formation, periodontal ligament widening, furcal radiolucency or apical radiolucency), pathological root resorption: evaluation at 3 and 6 months (at tooth level) Radiological failure (pathological root resorption, periodontal ligament widening and apical, lateral or furcal radiolucency): evaluation at 3 months (at tooth level) | |
| Notes | Reasons for dropouts: quote: "18 in the FC group and 8 in the MTA group did not attend the 3‐month follow‐up" Comment: 55 participants excluded: not meeting inclusion (39 children), refused to participate (12 children), other reasons (4 children) Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number producing system |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Paediatric Dentistry Department, Alexandria University, Alexandria, Egypt. Operators not mentioned | |
| Participants | 24 children, 72 teeth, mean age 6.1 years, age range 4‐8 years | |
| Interventions | Group 1: Pulpotomy (grey MTA); n = 24 (1 visit) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access with high‐speed bur Pulpotomy amputation with excavator For haemostasis, moistened cotton pellet with water No irrigation Grey MTA (3:1 powder:saline ratio) applied after pulpotomy, followed by IRM dressings before being restored with stainless‐steel crowns Group 2: Pulpotomy (white MTA); n = 24 (1 visit) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access with high‐speed bur Pulpotomy amputation with excavator For haemostasis, moistened cotton pellet with water No irrigation White MTA (3:1 powder:saline ratio) applied after pulpotomy, followed by IRM dressings before being restored with stainless‐steel crowns Group 3: Pulpotomy (formocresol); n = 24 (1 visit) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access with high‐speed bur Pulpotomy amputation with excavator For haemostasis, moistened cotton pellet with water No irrigation Cotton wool pellet soaked with FC placed on pulp stumps for 5 minutes after pulpotomy, followed by ZOE and IRM dressings before being restored with stainless‐steel crowns | |
| Outcomes | Clinical success (no pain symptoms, or no tenderness to percussion, or no swelling, or no fistulation, or no pathological mobility), radiographic success (no radicular radiolucency, or internal or external resorption, or periodontal ligament space widening), radicular radiolucency, pulp canal obliteration: evaluation at 1, 3, 6 and 12 months (at tooth level) | |
| Notes | Reasons of dropouts: quote: "Four children with 12 pulpotimized molars, failed to return for evaluations and were excluded from the study" Comment: 17% of participants (8% of teeth) dropped out of the study. The reasons for failure to return were not reported Source of funding: quote "This study was supported by the Zawawi Pediatric Dentistry Fund of the Indiana University Foundation. [...] The authors also wish to thank Dentsply Tulsa Dental for donating the MTA materials used in this study" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Two examiners, who were blinded to the treatment type, evaluated the teeth clinically" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Two examiners, who were blinded to the treatment type, evaluated the teeth [...] and radiographically" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Pediatric Dentistry Department, Faculty of Dentistry, Ankara University. Operators not mentioned | |
| Participants | 64 children, 128 teeth, mean age 8.2 years, age range 6‐10 years | |
| Interventions | Group 1: Pulpotomy (CH NaCOl); n = 31 (1 visit) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access not mentioned Pulpotomy amputation with excavator For haemostasis, dry cotton pellet Irrigation with 5% NaOCl for 30 seconds, then water CH, followed by IRM then stainless steel crown Group 2: Pulpotomy (CH); n = 31 (1 visit) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access not mentioned Pulpotomy amputation with excavator For haemostasis, dry cotton pellet Irrigation with saline for 30 seconds then water CH, followed by IRM then stainless steel crown Group 3: Pulpotomy (MTA NaOCl); n = 31 (2 visits) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access not mentioned Pulpotomy amputation with excavator For haemostasis, dry cotton pellet Irrigation with 5% NaOCl for 30 seconds then water MTA, followed by a moistened cotton pellet, followed by IRM. Second visit: IRM and the cotton pellets were removed after 24 hours, then stainless steel crown Group 4: Pulpotomy (MTA); n = 31 (2 visits) Rubber dam Caries removal prior to pulpal access not mentioned Pulp access not mentioned Pulpotomy amputation with excavator For haemostasis, dry cotton pellet Irrigation with saline for 30 seconds then water MTA, followed by a moistened cotton pellet, followed by IRM. Second visit: IRM and the cotton pellets were removed after 24 hours, then stainless steel crown | |
| Outcomes | clinical success (absence of spontaneous pain, pathologic mobility, tenderness to percussion, swelling, fistula, or gingival inflammation), radiographic success (absence of internal/external root resorption and periapical/furcal radiolucency), calcific metamorphosis of the pulp: evaluation at 3, 6, 9 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | a toss of a coin |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | quote: "One examiner, who was blinded to treatment type, evaluated the teeth clinically " |
| Blinding of radiological outcomes assessment | Low risk | quote: "One examiner, who was blinded to treatment type, evaluated the teeth [...] radiographically" |
| Incomplete outcome data (attrition bias) | Unclear risk | missing data balanced in numbers across intervention groups, with similar reasons for missing data across groups (2 in each group because of uncontrolled bleeding) |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive Dentistry at School of Dentistry, Damascus, Syria. Operators not mentioned | |
| Participants | 39 children, 64 teeth, mean age 8.2 years, age range 3 to 9 years | |
| Interventions | Group 1: Pulpectomy (zinc oxide and propolis); n = 16 (1 visit)
Group 2: Pulpectomy (endoflas‐chlorophenol‐free); n = 16 (1 visit)
Group 3: Pulpectomy (Metapex); n = 16 (2 visits)
Group 4: Pulpectomy (ZOE); n = 16 (2 visits)
| |
| Outcomes | Clinical success (no abnormal mobility, pain, or sensitivity to percussion), radiographic success (decrease in the size of radiolucency and the presence of bone regeneration), at 6 and 12 months. Treatment failure was classified into two degrees as (a) the radiolucency slightly increased in size, but it was separated from succeeding bud with adequate bone and (b) the radiolucency threatening the succeeding buds, so the tooth was extracted. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The treated molars were evaluated double‐blindly by three observers" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "The treated molars were evaluated double‐blindly by three observers" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in Turkey. Setting and operators not mentioned | |
| Participants | 42 children, 69 teeth, age range 7 to 11 years | |
| Interventions | Group 1: Pulpotomy (glutaraldehyde + ZOE); n = 25 (1 visit)
Group 2: Pulpotomy (glutaraldehyde + calcium hydroxide); n = 21 (1 visit)
Group 3: Pulpotomy (formocresol + ZOE); n = 23 (1 visit)
| |
| Outcomes | Clinical success (pain symptoms, thermal sensitivity, tenderness to percussion, changes in the mucous membrane in the surrounding area, sensitivity to sour, sensitivity to sweet), radiological success (internal root resorption, changes in the integrity of lamina dura, abnormalities in the structure of trabecular bone): evaluation at 3 months (at tooth level) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Conducted in the University of Gazi Department of Pediatric Dentistry, Turkey. Operators were undergraduate dental students supervised by members of senior staff clinics | |
| Participants | 105 children, 105 teeth, mean age 6.4 years, age range 4 to 8 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 35 (1 visit)
Group 2: Pulpotomy (calcium hydroxide); n = 35 (1 visit)
Group 3: Pulpotomy (calcium hydroxide/iodoform)n = 35 (1 visit)
| |
| Outcomes | Clinical success (teeth remained asymptomatic, no tenderness to percussion, no sinus tract or no premature tooth loss), radiological success (no furcal or periapical radiolucencies or internal or external root resorption), tenderness to percussion, swelling, spontaneous pain, fistula, internal root resorption, external root resorption, periapical radiolucency, furcal radiolucency, widened periodontal ligament: evaluation at 1, 3, 6, 9 and 12 months (at tooth level) | |
| Notes | Quote: "9 children, with 9 pulpotomized molars, failed to return for evaluations and were excluded from the study" "5 bleeding cases were excluded from analysis" Group 1 ‐ received intervention, n = 35; no exclusions Group 2 ‐ received intervention, n = 33; excluded due to uncontrolled bleeding from paste placement n = 2 Group 3 ‐ received intervention, n = 32; excluded due to uncontrolled bleeding from paste placement n = 3 Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Radiographic outcome assessments were made by the primary investigator and 1 independent experienced clinician who was blind to the treatment" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pediatric Dentistry, Tabriz University of Medical Science, Iran. Operator was an expert paediatric dentist. | |
| Participants | 83 children, 160 teeth, mean age 5.14 years, age range 3 to 6 years | |
| Interventions | Group 1: direct pulp capping (3 Mix); n = 40 (1 visit)
Group 2: direct pulp capping (3 Mixtatin); n = 40 (1 visit)
Group 3: direct pulp capping (simvastatin); n = 40 (1 visit)
Group 4: direct pulp capping (White MTA); n = 40 (1 visit)
| |
| Outcomes | Failure of treatment: pain, tenderness to palpation and percussion, sinus tract, and swelling; presence of internal or external root resorption, inter‐radicular radiolucency, and periapical lesion: evaluation at 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a computer random number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "The operator was not blinded to the treatment because of different manipulation techniques implemented for the study groups" |
| Blinding of clinical outcomes assessment | Low risk | Quote: "clinical and radiographic examinations were conducted at each appointment by two experienced paediatric dentists that were blinded to the techniques applied to each group" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "clinical and radiographic examinations were conducted at each appointment by two experienced paediatric dentists that were blinded to the techniques applied to each group" |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pediatric Dentistry at Tabriz University of Medical Sciences School of Dentistry, Iran. Operators not mentioned | |
| Participants | 84 children, 120 teeth, mean age 4.4 years, age range 4 to 5 years | |
| Interventions | Group 1: Direct pulp capping (formocresol + ZOE); n = 60 (1 visit)
Group 2: Direct pulp capping (calcium hydroxide + ZOE); n = 60 (1 visit)
| |
| Outcomes | Clinical success (spontaneous pain, or pain initiated by stimuli; signs of a defective restoration or recurrent caries; signs of mobility, sinus formation, tenderness to percussion, or soft tissue swelling; and signs of exfoliation, mobility or signs/symptoms of the successor tooth erupting), radiological success (defective restoration or recurrent caries; periradicular pathology such as periapical or furcal radiolucency; and pathological internal resorption, replacement resorption, intracanal calcifications, or physiological root resorption): evaluation at 24 months (at tooth level) Spontaneous pain, tenderness to percussion, fistula or parulis, periapical radiolucency or furcal radiolucency, internal resorption or external resorption: evaluation at 6, 12, 18 and 24 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "objectivity was maximized by not having direct access during [...] clinical evaluation to records detailing which pulp therapy agent was used" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "objectivity was maximized by not having direct access during [...] radiological evaluation to records detailing which pulp therapy agent was used" |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Paedodontic Department at Shahid Beheshti University, Dental School, Iran. Operator was an investigator | |
| Participants | 17 children, 40 teeth, age range 4 to 9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 20 (1 visit)
Group 2: Pulpotomy (MTA); n = 20 (2 visits)
| |
| Outcomes | Signs of failure (internal resorption, radiographic signs of pathosis (periapical radiolucency), report of pain, presence of gingival swelling and sinus tract): evaluation at 24 months (at tooth level) Fistula, furcal radiolucency, periapical radiolucency, internal resorption, external resorption, periodontal ligament widening, pulp canal obliteration: evaluation at 6, 12 and 24 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in Turkey. Operator was a paediatric dentist | |
| Participants | 50 children, 50 teeth, age range 4 to 9 years | |
| Interventions | Group 1: Pulpectomy (IRM); n = 25 (3 visits)
Group 2: Pulpectomy (MTA); n = 25 (3 visits)
| |
| Outcomes | Clinical failure (pain, pathological mobility, tenderness to percussion and palpation, and any soft tissue pathology and sinus tract) and radiographical failure (pathological root resorption, reduced size or healing of existing lesion, and absence of new lesions at the interradicular or periapical area): evaluation at 3, 6, 12 and 18 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Examiners were blinded to the groups" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Examiners were blinded to the groups" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Pedodontics Department of Yazd Faculty of Dentistry, Iran. Operators were the principal investigator or co investigators | |
| Participants | 46 children, 70 teeth, mean age 6.1 years, standard deviation age 1.4 years, age range 4 to 10 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 35 (1 visit)
Group 2: Pulpotomy (electrosurgery); n = 35 (2 visits)
In the experimental electrosurgical group, a series of large, sterile cotton pellets were placed in the chamber with pressure to obtain temporary haemostasis. The cotton pellets were then removed and the electrosurgery dental U‐shaped electrode (Whaledent perfect TCS, Colten Whaledent Inc., USA) was immediately placed 1 to 2 mm above the tissue. The electrosurgery unit power was set at 40%. The electrical arc was allowed to bridge the gap to the first pulpal stump for 1 second followed by a cool‐down period of 10 to 15 seconds. Heat was minimised by keeping the electrode as far away from the pulpal stumps and the tooth structure as possible while still allowing electrical arcing to occur. This procedure was repeated up to 3 times at each pulpal orifice. To avoid heat build‐up in any 1 area of the tooth, single applications of 1 second were performed to each orifice in a rotational sequence. After each current application, a new large sterile cotton pellet was placed with pressure on the next pulpal orifice to be electrosurgically treated to absorb any blood or tissue fluid before the next current application (i.e. pellet‐electrode‐pellet‐electrode). Pulpal stumps were dry and blackened, followed by ZOE dressings before being restored with amalgam | |
| Outcomes | Clinical success (absence of pain, abscess, fistula or excessive mobility), radiological success (presence of a normal periodontal ligament space, absence of pathological root resorption or canal calcification, and no periradicular or furcal radiolucency): evaluation at 9 months (at tooth level) Pain symptoms, fistula, pathological mobility, abscess, furcal radiolucency, internal resorption, external resorption: evaluation at 3, 6 and 9 months | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...examiner who was ...blind to the treatment" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...examiner who was ...blind to the treatment" |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in Turkey. Operator was a paediatric dentist | |
| Participants | 16 children, 20 teeth, age range 6 to 13 years, mean age 10.5 years | |
| Interventions | Group 1: Pulpectomy (gutta‐percha/AH‐Plus); n = 10 (1 visit)
Group 2: Pulpectomy (MTA); n = 10 (2 visits)
| |
| Outcomes | Clinical success (no symptoms of pain, tenderness to percussion, swelling, and presence of a fistula or pathological mobility), radiographic success (no evidence of periradicular or interradicular radiolucency or internal or external root resorption): evaluation at 6, 12, 18, 24 and 36 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | High risk | Quote: "examiners could not be blinded to the type of the root canal filling" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the clinic of the Department of Pediatric Dentistry, Erciyes University, Kayseri, Turkey. Operators were not mentioned | |
| Participants | 35 children, 70 teeth, age range 4 to 6 years | |
| Interventions | Group 1: Pulpotomy (Ankaferd Blood Stopper); n = 35 (1 or 2 visits)
Group 2: Pulpotomy (FS); n = 35 (1 or 2 visits)
| |
| Outcomes | Clinical failure (pain, tenderness to percussion, gingival abscess, sinus/fistula, and pathological mobility), radiographic success (absence of abnormal root resorption, internal root resorption, furcation involvement, and periapical bone destruction), Calcification in pulpal tissue and pulp canal obliteration: evaluation at 3, 6, 9 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "All pre‐ and postoperative clinical and digital radiographic examinations were performed at followup by one experienced investigator who was blind to the group being studied" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "All pre‐ and postoperative clinical and digital radiographic examinations were performed at followup by one experienced investigator who was blind to the group being studied" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Hospital for Sick Children, Toronto, Canada. Operators were 3 paediatric dentists | |
| Participants | 130 children, 291 teeth, mean age 4.4 years, standard deviation age 1.3 years | |
| Interventions | Group 1: Pulpotomy (ferric sulphate); n = 182 (1 visit)
Group 2: Pulpectomy (ZOE); n = 109 (1 visit)
| |
| Outcomes | Radiological success (N ‐ normal molar without evidence of radiographic change or H ‐ radiographic changes associated with normal physiological molar resorption): evaluation at 36 months (at tooth level) Furcal radiolucency, periapical radiolucency, internal root resorption, external resorption, periodontal ligament widening, pulp canal obliteration, N (score 4‐rx), H (score 4‐rx), Po (score 4‐rx), Px (score 4‐rx), pain symptoms, tenderness to percussion, (swelling or parulis), (fistula or swelling): evaluation at 24 and 36 months | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the paediatric dental clinic at the School of Dentistry, Hacettepe University, Ankara, Turkey. Operator was a paediatric dentist. | |
| Participants | 75 children, 139 teeth, 3 to 9 years | |
| Interventions | Group 1: Pulpotomy (ProRoot MTA); n = 46 (1 visit)
Group 2: Pulpotomy (MTA Angelus); n = 45 (1 visit)
Group 3: Pulpotomy (CH); n = 48 (1 visit)
| |
| Outcomes | Clinical success (absence of spontaneous pain and/ or sensitivity to palpation/percussion; absence of fistula, swelling, and/or abnormal mobility), radiological success (absence of radiolucencies at the inter‐radicular and/or periapical regions, absence of pulp canal obliteration (fully obliterated canals); and absence of internal or external (pathologic) resorption), defective restoration (clinically): evaluation at 1, 3, 6, 12, 18, 24 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Low risk | Quote: "...sequentially numbered opaque‐sealed envelopes" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "Operator blinding was not possible" |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Two calibrated operators, blinded to group assignment and treatment, performed ...clinical ...recall examinations" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Two calibrated operators, blinded to group assignment and treatment, performed ...radiographic recall examinations" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in India. Operator not mentioned. | |
| Participants | 52 children, 60 teeth, 3.8 to 7.6 years | |
| Interventions | Group 1: Pulpectomy (ozonated oil‐ZO); n = 30 (1 visit)
Group 2: Pulpectomy (ZOE); n = 30 (1 visit)
| |
| Outcomes | Clinical success (absence of pain, tenderness to percussion, absence or decrease in mobility and sinus opening), radiographic success (signs of resolution in the radiolucency, no new signs of post‐operative radiolucency and no signs of internal or external pathological root resorption), radiographic failure (increase in postoperative inter‐radicular radiolucency or development of new postoperative radiolucency): evaluation at 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The teeth were evaluated for success or failure based on clinical and radiographic criteria by a blinded investigator" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "The teeth were evaluated for success or failure based on clinical and radiographic criteria by a blinded investigator" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pediatric Dentistry, First Dental Center, Peking University School and Hospital of Stomatology, Beijing, China. Operator was one investigator | |
| Participants | 155 children, 160 teeth, average age: 5.88 ± 1.27 years | |
| Interventions | Group 1: Pulpectomy (ZOE); n = 51 (2 visits)
Group 2: Pulpectomy (Vitapex); n = 56 (2 visits)
Group 3: Pulpectomy (MPRCF); n = 53 (2 visits)
| |
| Outcomes | Clinical and radiologic success: evaluation at 6 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...the clinical ...diagnoses were blindly assessed by other two investigators" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...the ...radiogaphic diagnoses were blindly assessed by other two investigators" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the University Center Heminio Ometto, School of Dentistry, Araras, Sao Paulo, Brazil. Operators not mentioned | |
| Participants | 29 children, 51 teeth, age range 4.5 to 6.5 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 28 (4 visits)
Group 2: Pulpectomy (calcium hydroxide); n = 23 (4 visits)
| |
| Outcomes | No data provided | |
| Notes | Dropouts: no information provided Follow‐up for 48 months; reporting at baseline, 12, 24, 26, 48 months Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to make a clear judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Paediatric Dentistry at the Universitat Internacional de Catalunya, Spain. Operator was a postgraduate student | |
| Participants | 68 children, 90 teeth, age range 4 to 9 years, mean 6.6 ± 1.3 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 45 (1 visit)
Group 2: Pulpotomy (Biodentine); n = 45 (1 visit)
| |
| Outcomes | Clinical success (no symptoms of pain, and there was no swelling or gingival inflammation, fistulation, or pathologic mobility), radiologic success (no evidence of internal or external resorption or periradicular radiolucency): evaluation at 6 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | Protocol prospectively registered (NCT01591278). no discrepancies in outcomes between registered record and published RCT. |
| Methods | RCT, parallel‐arm Children randomly assigned Conducted in the dental clinics of the Indiana University Institutional Review Board, USA. Operators were investigators: "...standardization of the investigators in the experimental technique was attempted by using a clinician with over 20 years of experience in performing the electrosurgical…" | |
| Participants | 50 children, 50 teeth mean age 5.3 years, age range 2.2 to 8.1 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 25 (1 visit)
Group 2: Pulpotomy (electrosurgery); n = 25 (1 visit)
| |
| Outcomes | Clinical success (no pain, no abscess, no fistula or no excessive mobility), radiological success (normal periodontal ligament space, no pathological root resorption, no canal calcification and no periradicular radiolucency): mean evaluation at 11.5 (range 5‐25) months for Group 1 and 10.9 (6‐31) for Group 2 (at tooth level) | |
| Notes | Source of funding: quote: "This study was supported by Birtcher Medical Services, Inc" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...the patients were assigned randomly by the flip of a coin" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Setting not mentioned. Conducted in Turkey. Operators were investigators | |
| Participants | 67 children, 100 teeth, age range 5 to 9 years | |
| Interventions | Group 1: Direct pulp capping (calcium hydroxide); n = 20 (1 visit)
Group 2: Direct pulp capping (acetone‐based total‐etch adhesive); n = 20 (1 visit)
Group 3: Direct pulp capping (acetone‐based total‐etch adhesive ‐ non rinse conditioner); n = 20 (1 visit)
Group 4: Direct pulp capping (acetone‐based total‐etch adhesive ‐ total etching); n = 20 (1 visit)
Group 5: Direct pulp capping (acetone‐based total‐etch adhesive ‐ self‐etch); n = 20 (1 visit)
| |
| Outcomes | Clinical success (no spontaneous pain or sensitivity (or both) to pressure/percussion, no fistula, oedema, abnormal mobility, or a combination), radiological success (no radiolucency at the inter‐radicular or periapical regions (or both), no internal or external (pathological) resorption that was not compatible with the expected resorption due to the exfoliation process), inter‐radicular radiolucency or periapical radiolucency, internal root resorption or external root resorption, pain symptoms or spontaneous pain: evaluation at 1, 3, 6, 9, 12, 18 and 24 months (at tooth level) | |
| Notes | Reasons for dropouts: 9 exfoliations (7 at 18 months, 2 at 24 months); 2 extractions (12 and 18 months), 1 extraction (6 months), 1 extraction (12 months) Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...two calibrated operators, blinded to the treatments, performed the clinical ...recall examinations" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...two calibrated operators, blinded to the treatments, performed the ...radiological recall examinations" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Hospital for Sick Children, Toronto, Canada. Operators were 3 paediatric dentists | |
| Participants | 112 children, 266 teeth, mean age 4.0 years, standard deviation age 1.1 years | |
| Interventions | Group 1: Pulpotomy (FS + eugenol); n = 58 (1 visit)
Group 2: Pulpotomy (FS); n = 78 (1 visit)
Group 3: Pulpotomy (MTA); n = 53 (1 visit)
Group 4: Pulpotomy (MTA + FS + eugenol); n = 77 (1 visit)
| |
| Outcomes | Tenderness to percussion, pathological mobility, erythema, parulis, pathological radiolucency, internal root resorption, external root resorption, periodontal ligament widening, pulp canal obliteration, N (score 5‐rx), Po (score 5‐rx), Px (score 5‐rx): mean evaluation at 22 (range 6 to 38) months (at tooth level) Quote: "Subjects were invited to return for clinical and radiographic assessments at 12, 24, and 36 months after treatment" | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Low risk | Quote: "2 blinded, disinterested raters classified each molar into 1 of 3 radiographic outcomes" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the University of Marmara, Department of Paediatric Dentistry, in Istanbul. Operator was one paediatric dentist. | |
| Participants | 58 children, 120 teeth, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (diode laser); n = 40 (1 visit)
Group 2: Pulpotomy (formocresol); n = 40 (1 visit)
Group 3: Pulpotomy (ferric sulphate); n = 40 (1 visit)
| |
| Outcomes | Clinical failure (spontaneous pain, percussion/palpation, abscess, swelling, fistula, or pathologic mobility), radiological failure (periapical radiolucency, widened periodontal ligament space (PDL), pathologic internal/external root resorption, or pathological changes of the alveolar bone in the furcation): evaluation at 1, 3, 6, 9, and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The outcome assessment and data analysis were blinded " |
| Blinding of radiological outcomes assessment | Unclear risk | Quote: "The outcome assessment and data analysis were blinded " BUT "Two blinded observers evaluated a set of radiographs separately" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the undergraduate and graduate Pediatric Dentistry Clinics of the Hebrew University‐Hadassah School of Dental Medicine, Israel. Operators were authors | |
| Participants | 26 children, 45 teeth; 32 teeth from 18 children analysed, mean age 6.4 years, age range 5 to 12 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 17 teeth (1 visit)
Group 2: Pulpotomy (MTA); n = 15 teeth (1 visit)
| |
| Outcomes | Signs of failure (internal root resorption, furcation radiolucency, periapical bone destruction, pain, swelling, or sinus tract), internal root resorption, furcation radiolucency, periapical bone destruction, pain, swelling, or sinus tract: evaluation at 13 (6 to 30) months (at tooth level) | |
| Notes | Reasons of dropouts: quotes: "a total of 45 primary molars were pulpotomized in 26 children. Of these 32 teeth in 18 children were available for follow‐up evaluation"; "4 children with 8 teeth had less than 6 months postoperative period at the time of data analysis. 3 children with 5 teeth were not available for follow‐up examination since they moved to another city" Source of funding: not reported, although the MTA material was provided by a colleague at another university in the USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement of Yes or No |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement of Yes or No |
| Blinding of clinical outcomes assessment | High risk | Quote: "the children were examined clinically at follow‐up by one of the 3 authors who were not blind to which treatment group the subject belong" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "all 3 authors blindly evaluated the radiographs" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted at the Pediatric Dental Clinics, Faculty of Dentistry, King Abdulaziz University (KAU), Jeddah. Operators not mentioned | |
| Participants | 37 children, 56 pairs, 112 teeth; mean age 6 ± 0.75 years, age range 4 to 8 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 56 teeth (1 visit)
Group 2: Pulpotomy (Biodentine); n = 56 teeth (1 visit)
| |
| Outcomes | Clinical success (absence of sensitivity, pain, or swelling, no tenderness to percussion, no abscess or fistulation, no tooth mobility), radiographic success (absence of furcation and periapical radiolucency, absence of internal or external root resorption), presence of a normal periodontal ligament space, presence of pulp canal obliteration: evaluation at 3 and 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement of Yes or No |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement of Yes or No |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement of Yes or No |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Independently, two examiners who were blinded to treatment type evaluated the teeth clinically and radiographically." |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Independently, two examiners who were blinded to treatment type evaluated the teeth clinically and radiographically." |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned Setting not mentioned. Conducted in Turkey. Operators were 3 paediatric dentists | |
| Participants | 32 children, 100 teeth, mean age 6.2 years, standard deviation age 0.7 years. age range 5 to 7 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 25 (1 visit)
Group 2: Pulpotomy (ferric sulphate); n = 25 (1 visit)
Group 3: Pulpotomy (formocresol); n = 25 (1 visit)
Group 4: n = 25 (1 visit)
| |
| Outcomes | Clinical failure (pain, swelling, mobility, percussion pain), radiological failure (internal root resorption, and furcation or periapical bone destruction (or both)), signs of failure (pain, swelling, mobility, percussion pain, internal root resorption, and furcation or periapical bone destruction (or both)), internal root resorption, pulp canal obliteration, tenderness to percussion, inter‐radicular bone destruction, physiological root resorption: evaluation at 6, 12 and 24 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "the children were examined clinically by 3 experienced pediatric dentists (not the operators) blinded to the technique" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "the children were examined radiographically by 3 experienced pediatric dentists (not the operators) blinded to the technique" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Setting not mentioned. Conducted in Iran. One operator (no detail) | |
| Participants | 21 children, 42 teeth, mean age 6.9 ± 0.7, age range 5 to 8 years | |
| Interventions | Group 1: Direct pulp capping (MTA); n = 21 (1 visit)
Group 2: Direct pulp capping (CEM); n = 21 (1 visit)
| |
| Outcomes | Clinical failure (pain, swelling, tenderness to pressure, sinus tract, swelling and tenderness to percussion), radiological failure (internal and/or external root resorption, interradicular radiolucencies, and periapical lesions): evaluation at 6 and 20 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Low risk | The single operator and children were blind to biomaterial/treatment |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Treatment outcomes ...were evaluated at 20 months by a calibrated dentist, radiologist and a statistician who were also blind to the type of used biomaterial" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Treatment outcomes ...were evaluated at 20 months by a calibrated dentist, radiologist and a statistician who were also blind to the type of used biomaterial" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Setting not mentioned. Operators were paediatric dentists. Conducted in Saudi Arabia | |
| Participants | 100 children, 120 teeth, mean age 6 years, standard deviation age 1.6 years, age range 3 to 8 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 60 (1 visit)
Group 2: Pulpotomy (MTA); n = 60 (1 visit)
| |
| Outcomes | Clinical success (no pain, sinus tract or swelling), radiographic success (no evidence of furcation radiolucency, internal root resorption, or periapical bone destruction), physiological root resorption, furcation radiolucency, periapical radiolucency, internal root resorption, pulp canal obliteration, pain symptoms, sinus tract, swelling: evaluation at 6, 12, 18 and 24 months (at tooth level) | |
| Notes | Dropouts: "Out of 120 teeth, only 74 were assessed clinically and radiographically throughout the follow up period" Comment: only the results for these 74 teeth were reported Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Pediatric Dental Clinic at the University of Southern California School of Dentistry. Operators not mentioned | |
| Participants | 62 children, 83 teeth, mean age 6.7 years, age range 3.2 to 10.1 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = not stated (27 teeth analysed) (1 visit)
Group 2: Pulpotomy (ferric sulphate); n = not stated (29 teeth analysed) (1 visit)
| |
| Outcomes | Clinical success (no symptoms of pain, tenderness to percussion, swelling, fistulation or pathological tooth mobility), radiographic success (normal periodontal ligament, absence of pathological internal root resorption, external root resorption, no intraradicular or no periapical radiolucency), signs of failure (symptoms of pain, tenderness to percussion, swelling, fistulation, pathological tooth mobility, abnormal periodontal ligament, pathological internal root resorption, external root resorption, intraradicular or periapical radiolucency), internal root resorption, pulp canal obliteration: evaluation at 3, 6 and 12 months (at tooth level) | |
| Notes | 56 teeth from 48 children were available for evaluation after 12 months (Group 1: 27; Group 2: 29) Source of funding: not reported, although FS material was provided by a manufacturer | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Clinical evaluations of the teeth were conducted by two independent examiners who had no knowledge of the group to which the particular tooth was assigned" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Radiological evaluations of the teeth were conducted by two independent examiners who had no knowledge of the group to which the particular tooth was assigned" |
| Incomplete outcome data (attrition bias) | High risk | Number of randomised teeth unknown |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Setting not mentioned. Operators not mentioned. Conducted in Brazil | |
| Participants | number of children not mentioned, 60 teeth, mean age 6.5 years, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 15 (1 visit)
Group 2: Pulpotomy (CH); n = 15 (1 visit)
Group 3: Pulpotomy (LLLT); n = 15 (1 visit)
Group 4: Pulpotomy (CH+ LLLT); n = 15 (1 visit)
| |
| Outcomes | Clinical success (absence of spontaneous pain, mobility, swelling, or fistula), Radiographic success (presence of hard tissue barrier formation and pulp calcifications, and absence of internal or external root resorption and furcation radiolucency) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "At each checkup, two blinded and calibrated investigators performed clinical and periapical radiographic examination of the pulpotomized teeth" |
| Blinding of radiological outcomes assessment | Low risk | quote: "At each checkup, two blinded and calibrated investigators performed clinical and periapical radiographic examination of the pulpotomized teeth" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Paediatric Dentistry at the Universitat Internacional de Catalunya. Operators were student and dentists. | |
| Participants | 81 children, 100 teeth, mean age 6.7 ± 1.6 years, age range 3.2 to 10.1 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 25 (1 visit)
Group 2: Pulpotomy (MTA); n = 25 (1 visit)
Group 3: Pulpotomy (ferric sulphate); n = 25 (1 visit)
Group 4: Pulpotomy (sodium hypochlorite); n = 25 (1 visit)
| |
| Outcomes | Clinical success (no pain, swelling, fistulation, or pathologic mobility), radiographic success (no evidence of internal or external resorption, or periradicular radiolucency), overall success: evaluation at 6, 12, 18, and 24 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Low risk | Quote: "the radiographs were ...re‐evaluated independently by two blinded observers" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in a hospital‐based (Long Beach Memorial Medical Center) dental clinic in California, USA (noted as predominantly children from low‐income families). Operators not mentioned | |
| Participants | 38 children, 47 teeth, mean age 5 years, age range 3.1 to 8.1 years | |
| Interventions | Group 1: Pulpotomy (ZOE); n = 24 (1 visit)
Group 2: Pulpotomy (calcium hydroxide); n = 23 (1 visit)
| |
| Outcomes | Clinical success (no excessive tooth mobility, no subjective symptoms of pain, no tenderness to percussion, and no fistula), radiographic success (normal periodontal ligament and absence of furcation or periapical radiolucency, internal or external resorption and calcific degeneration in the remaining pulp tissue), signs of failure (excessive tooth mobility, subjective symptoms of pain, tenderness to percussion, fistula, abnormal periodontal ligament, furcation or periapical radiolucency, internal or external resorption, and calcific degeneration in the remaining pulp tissue), periapical radiolucency, internal root resorption, external root resorption, periodontal ligament widening, pulp canal obliteration (parulis, fistula or swelling): evaluation at 1, 3 and 6 months (at tooth level) | |
| Notes | 47 teeth for treatment; 43 teeth from 35 children were available for evaluation after 6 months 1 month: 11 teeth in CH group and 10 teeth in ZOE group unavailable for recall; 3 months: 9 teeth in CH group and 8 teeth in ZOE group unavailable for recall; 6 months: 3 teeth in CH group and 1 tooth in ZOE group unavailable for recall Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Low risk | Numerical code which was available only to the operator |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Clinical evaluation was determined by 2 examiners who had no knowledge if the experimental group of the tooth" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "radiologic evaluation was determined by 2 examiners who had no knowledge if the experimental group of the tooth" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the paediatric dentistry undergraduate student's clinic of the Hebrew University‐Hadassah School of Dental Medicine, Israel Operators were the Israeli authors of this study | |
| Participants | 72 children, 96 teeth, mean age 7.5 years, age range 4.5 to 10 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 38 (1 visit)
Group 2: Pulpotomy (ferric sulphate); n = 58 (1 visit)
| |
| Outcomes | Radiographic success (internal root resorption, furcation radiolucency or periapical bone destruction), furcal radiolucency, periapical radiolucency, internal root resorption, pulp canal obliteration, faster root resorption compared with contralateral, slower root resorption compared with contralateral, similar root resorption compared with contralateral: evaluation at 20.5: (6 to 11), (12 to 23) and (24 to 35) months (at tooth level) Signs of failure (internal root resorption, furcation radiolucency, periapical bone destruction, pain, swelling, or sinus tract): evaluation at 20.5 (24 to 35) months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Pediatric Dentistry Postgraduate Program, Faculty of Dentistry of San Luis Potosi University, Mexico. A single operator performed all procedures | |
| Participants | 45 children, 90 teeth, median age (± standard deviation) boys: 6.4 ± 1.16 years, girls: 5.7 ± 1.01 years | |
| Interventions | Group 1: Direct pulp capping (EMD); n = 45 (1 visit)
Group 2: Direct pulp capping (calcium hydroxide); n = 45 (1 visit)
| |
| Outcomes | Signs of failure (internal dentin resorption, spontaneous pain, gingival abscess (sinus tract), external root resorption or pathological mobility), internal dentin resorption, spontaneous pain, abscess, pathological root resorption, swelling or pathological mobility; evaluation at 1, 6 and 12 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random using number sequences generated by R 2.4.0 software |
| Allocation concealment (selection bias) | Low risk | Quote: "The operator was blind to the random number schemes until just before placing the materials" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The participants…were blind regarding capping material group assignation" |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Assessing observer and analyst were blind regarding capping material group assignation" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Assessing observer and analyst were blind regarding capping material group assignation" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned Setting not mentioned. Conducted in India. Operator not mentioned | |
| Participants | 41 children, 45 teeth, age range 4 to 8 years | |
| Interventions | Group 1: Pulpotomy (full strength formocresol); n = 15 (2 visits)
Group 2: Pulpotomy (1:5 diluted formocresol); n = 15 (2 visits)
Group 3: Pulpotomy (1:25 diluted formocresol); n = 15 (2 visits) No details 1:25 diluted FC: 18 mL glycerine and 6 mL distilled water are thoroughly mixed and to which 1 part of FC is added. A number 1 foam pellet saturated with 1:25 diluted FC then twice squeezed to remove excess 1:25 diluted FC and placed for 5 minutes. Then teeth restored with stainless‐steel crown (second visit) | |
| Outcomes | Clinical failure (pain, intra‐oral/extra‐oral swelling, tenderness on percussion, sinus/fistula), radiological failure (furcation radiolucency, periapical changes, internal/external resorption): evaluation at 1, 3, 6 and 9 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "the subjects were unaware of their group" Insufficient information to make a clear judgement for blinding of personnel |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned at 9 months |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned DAV Dental College Yamuna Nagar, Haryana. A single operator (investigator) performed all procedures | |
| Participants | 42 children, 90 teeth, 4 to 8 years | |
| Interventions | Group 1: Pulpotomy (15.5% ferric sulphate); n = 30 (2 visits)
Group 2: Pulpotomy (2% buffered glutaraldehyde); n = 30 (2 visits)
Group 3: Pulpotomy (MTA); n = 30 (2 visits)
| |
| Outcomes | Clinical parameters (pain, sinus formation, swelling (intra oral), and mobility), radiological parameters (PDL widening, internal resorption, external resorption, periapical radiolucency, canal obliteration, and furcation radiolucency): evaluation at 24 h, 1 month, 3 months and 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Children randomly assigned Conducted at the Outpatient Department of Paediatric Dentistry, Punjab Government Dental College and Hospital, Amritsar, Punjab, India. Operators not mentioned. | |
| Participants | 20 children, 40 teeth, mean age 7.35 years, age range 5 to 10 years | |
| Interventions | Group 1: Pulpotomy (Biodentine); n = 20 (2 visits)
Group 2: Pulpotomy (CH); n = 20 (2 visits)
| |
| Outcomes | Pain, swelling: evaluation at 3, 6 and 12 months; mean dentin thickness, internal root resorption: evaluation at 6 and 12 months; colour matching, marginal discolouration, secondary caries, anatomic form, surface texture, marginal integrity, pulp sensitivity: evaluation at 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random‐number |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Blinded clinical and radiographic outcomes were observed" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Blinded clinical and radiographic outcomes were observed" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned Outpatient Department of Pediatric Dentistry of Subharti Dental College, Meerut. A single operator (investigator) performed all procedures | |
| Participants | 30 children, 30 teeth, 4 to 10 years | |
| Interventions | Group 1: Pulpotomy (ferric sulphate); n = 10 (1 visit)
Group 2: Pulpotomy (electrosurgery); n = 10 (1 visit)
Group 3: Pulpotomy (diode laser); n = 10 (1 visit)
| |
| Outcomes | Clinical success, radiological success, pain, furcal and periapical radiolucency, internal root resorption: evaluation at 3, 6, 9 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned | |
| Participants | 70 teeth, age range 4 to 7 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 35 (1 visit) Group 2: Pulpotomy (Iranian Root MTA); n = 35 (1 visit) | |
| Outcomes | Clinical failure, radiological failure, pain, soft tissue pathology, pathological radiolucency, pathological root resorption: evaluation at 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | The clinical ...follow up evaluations were performed at 6, 12 months by a blinded dentist |
| Blinding of radiological outcomes assessment | Low risk | The ...radiographic follow up evaluations were performed at 6, 12 months by a blinded dentist |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Pediatric Dentistry Clinic of the Hebrew University‐Hadassah School of Dental Medicine in Jerusalem, Israel. Operators were the authors of this study | |
| Participants | 35 children, 64 teeth, mean age 6.5 years, age range 4.4 to 11 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 31 (1 visit)
Group 2: Pulpotomy (MTA); n = 33 (1 visit)
| |
| Outcomes | Signs of failure (furcation radiolucency, periapical bone destruction, internal root resorption, swelling or sinus tract), abscess, pulp canal obliteration, dentine bridge formation, furcal radiolucency, periapical radiolucency, internal root resorption, external root resorption, calcific metamorphosis (periapical radiolucency or inter‐radicular radiolucency): evaluation at 36 (range 4 to 74) months (at tooth level) | |
| Notes | Reasons of dropouts: "Of the 64 pulpotomized teeth, 62 teeth in 33 children were available for analysis of success/failure rate. 2 molars in 2 patients, both of the FC group, were excluded from the study because the patients never returned for follow‐up examination" Comment: quotes: "when a patient did not respond or broke an appointment, further attempts were made to call the parents and a follow‐up examination was rescheduled"; "the follow‐up period was defined as the time elapsed between treatment and one of the following: 1/detection of pulpotomy failure; 2/naturally exfoliated tooth; 3/patient's last visit for recall examination. Teeth with less than 12 months follow‐up time were excluded from the study, unless a failure was detected during the first postoperative year" Source of funding: not reported, although the MTA material was provided by a colleague at another university in the USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | High risk | Quote: "the children were then examined clinically by 1 of the 3 authors who were not blind to which treatment group the assessed tooth belonged" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "All 3 authors blindly evaluated the radiographs" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Pedodontic Section, Department of Restorative Dentistry and Periodontology, Ludwig‐Maximilians‐University, Munich, Germany. Operators were 2 paedodontists | |
| Participants | 107 children, 191 teeth, mean age 4.8 years, standard deviation age 1.6 years, age range 2 to 8 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 50 (1 visit)
Group 2: Pulpotomy (Er:YAG); n = 47 (1 visit)
Group 3: Pulpotomy (calcium hydroxide); n = 44 (1 visit)
Group 4: Pulpotomy (ferric sulphate); n = 50 (1 visit)
| |
| Outcomes | Clinical failure (spontaneous pain, tenderness to percussion, fistula, soft tissue swelling, and pathological tooth mobility), spontaneous pain, tenderness to percussion, swelling, fistula, pathological mobility: evaluation at 6, 12, 18 and 24 months Radiological failure (periapical or furcal radiolucency, pathological external or distinct internal root resorption, or widened periodontal ligament space), signs of failure (spontaneous pain, tenderness to percussion, fistula, soft tissue swelling, pathological tooth mobility, periapical or furcal radiolucency, pathological external or distinct internal root resorption, or widened periodontal ligament space), furcal radiolucency, periapical radiolucency, internal root resorption, external root resorption, periodontal ligament widening: evaluation at 12 and 24 months (at tooth level) | |
| Notes | Reasons of dropouts: "103 patients (191 teeth followed up): 3 teeth from the laser group and 6 from the calcium hydroxide group were excluded from follow‐up and statistical analysis, due to uncontrollable bleeding during radiation or placement of calcium hydroxide, since a hyperemic, inflamed radicular pulp is considered a contraindication for vital pulpotomy"; "12 teeth had exfoliated physiologically" Comment: quotes: "4 patients moved away" Source of funding: quote: "The study was completely financed by Departmental funding". (Department of Restorative Dentistry & Periodontology, Dental School, Ludwig‐Maximilians‐University, Munich) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...by an assistant casting a concealed lot from a box containing 4 x 50 lots (block randomization)" |
| Allocation concealment (selection bias) | Low risk | Quote: "...all other contributors for the study were blinded to generation and implementation of the treatment assignment" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "clinical re‐evaluations …were performed independently by two experienced dentists (not the operators) blinded to the technique"; "the outcome assessment and data analysis were blinded, since the techniques were indistinguishable and coded" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "radiographic examinations were performed independently by two experienced dentists (not the operators) blinded to the technique"; "the outcome assessment and data analysis were blinded, since the techniques were indistinguishable and coded" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Setting not mentioned. Conducted in Kuwait. Operator was 1 senior paedodontist | |
| Participants | 70 children, 164 teeth, mean age 4.3 years, age range 3 to 6 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 80 (1 visit)
Group 2: Pulpotomy (ferric sulphate); n = 84 (1 or 2 visits)
| |
| Outcomes | Clinical success (absence of any fistula, abscess, swelling, spontaneous pain or pathological mobility), radiological failure (normal periodontal ligament space, no pathological internal or external root resorption and no intraradicular or periapical radiolucency), internal root resorption, periapical bone destruction, inter‐radicular bone destruction, succedaneous tooth structural anomaly: evaluation at 3 to 20 and 46 to 48 months (at tooth level) Signs of failure (internal root resorption, furcation radiolucency, periapical bone destruction, or a combination): evaluation at 46 to 48 months (at tooth level) | |
| Notes | The first 70 teeth were all treated within 1 month. The pulpotomy therapy of a further 124 primary molars was performed on the same children, during the following 6 months. On the final recall after 42 to 48 months, only 60 children appeared within the 4 months' recall period Clinical follow‐up: every 3 months Radiographic follow‐up: 6, 20 and 42 to 48 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate allocation |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | High risk | Quote: "The clinical follow‐up by the same examiner who had performed all pulpotomies and was aware to which treatment groups the subjects belonged" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Both authors, blindly, evaluated radiographs" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Conducted at the outpatient department, Dr R Ahmed Dental College and Hospital, India. Operators not mentioned. | |
| Participants | 66 children, 100 teeth, age range 3 to 7 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 50 (2 visits)
Group 2: Pulpotomy (FC); n = 50 (2 visits)
| |
| Outcomes | Clinical failure (history of pain, tenderness to palpation/percussion, pathological mobility, intra‐ or extra‐oral swelling, intra‐ or extra‐oral sinus, radiograph evaluation (integrity of lamina dura, presence or absence of radiolucencies in the apical or bifurcation areas of tooth, pathological internal or external root resorption, pulp canal obliteration), dentin bridge formation, overall success: evaluation at 1, 3, 6, 12 and 24 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Conducted in India. Setting and operators not mentioned. | |
| Participants | 48 children, 60 teeth, age range 4 to 10 years, mean 6.5 ± 1.2 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 30 (1 visit)
Group 2: Pulpotomy (Aloe vera); n = 30 (1 visit)
| |
| Outcomes | Clinical failure (ain, tenderness, mobility, swelling, sinus), radiographic failure (widening of periodontal ligament space, radiolucency, root resorption, pulp obliteration): evaluation at 1, 3, 6, 9, and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Low risk | Quote: "...the parent selecting a color‑coded stick out from an opaque bag mentioning the medicament" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pediatric Dentistry at the Yonsei University Dental Hospital. Operators were seven paediatric dentists | |
| Participants | 102 children, 151 teeth, age range 3 to 10 years | |
| Interventions | Group 1: Pulpotomy (RetroMTA); n = 49 (1 visit)
Group 2: Pulpotomy (OrthoMTA); n = 47 (2 visits)
Group 3: Pulpotomy (ProRoot MTA); n = 47 (2 visits)
| |
| Outcomes | Clinical failure (spontaneous pain and/or sensitivity to palpation/percussion; fistula, gingival redness, and swelling and/or mobility), radiological failure (bone resorption at the periapical and/or interradicular regions; PDL space widening; and external/internal root resorption): evaluation at 3, 6 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...one dental radiologist (KT Kim) who were not involved in this study were blinded to the group assignment and treatment and performed all radiographic follow‐up examinations after the completion of the 12‐month study period." |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the paediatric department of Mashhad Dental School, Iran. Operator was a postgraduate student of paediatric dentistry, who was supervised by two academic staff | |
| Participants | 51 children, 102 teeth, age range 4 to 6 years | |
| Interventions | Group 1: Pulpotomy (CEM); n = 51 (1 visit)
Group 2: Pulpotomy (ES/ZOE); n = 51 (1 visit)
| |
| Outcomes | Clinical success (lack of pain, mobility, swelling, sinus tract, tenderness to percussion and bone swelling), radiographic success (PDL and periapical regions with normal width and trabeculation minimal internal resorption), pulp canal obliteration: evaluation at 6, 12 and 24 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random‐number |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "...both the patients and outcome assessors were blinded to the type of treatment" |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...both the patients and outcome assessors were blinded to the type of treatment" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...both the patients and outcome assessors were blinded to the type of treatment" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pediatric and Preventive Dentistry, Faculty of Dental Sciences, King George’s Medical University, UP, Lucknow. Operator not mentioned. | |
| Participants | 90 children, 90 teeth, mean age 6.8 years, age range 3 to 10 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 25 (2 visits)
Group 2: Pulpotomy (Biodentine); n = 25 (2 visits)
Group 3: Pulpotomy (propolis); n = 25 (2 visits)
| |
| Outcomes | Clinical and radiographic criteria for assessing teeth were explained along with a calibration process to the two observers on three initial cases. The criteria, based on Zurn and Seale has been used for scoring the clinical and radiographic findings. The scoring system was devised to represent severity of changes but not to define an individual tooth as a ‘success’ or ‘failure’, i.e. as the score gets larger, the pathologies get progressively more invasive and require more frequent follow‐up. Teeth scored as 1 or 2 were considered successful. Evaluation at 3, 6 and 9 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The teeth were evaluated clinically and radiographically by two observers independently who were blinded to the treatment type" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "The teeth were evaluated clinically and radiographically by two observers independently who were blinded to the treatment type" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted at the Department of Pediatric dentistry, Pekin. Operator not mentioned. | |
| Participants | 18 children, 40 teeth, age range 4 to 9 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 25 (1 visit)
Group 2: Pulpotomy (CH); n = 25 (1 visit)
| |
| Outcomes | Clinical success (no pain, swelling, fistula, tenderness to percussion, pathologic mobility), radiologic success (no periapical or interradicular radiolucency, pathological root resorption): evaluation at 10 to 56 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned Setting and operators not mentioned | |
| Participants | 22 children, 30 teeth, mean age 6.6 years, standard deviation age 1.4 years. | |
| Interventions | Group 1: Pulpotomy (Portland cement, PC); n = 10 (1 visit)
Group 2: Pulpotomy (PC + iodoform, PC + CHI₃); n = 10 (1 visit)
Group 3: Pulpotomy (PC + zirconium oxide, PC + ZrO₂); n = 10 (1 visit)
| |
| Outcomes | Clinical success (no swelling, fistula, spontaneous pain, mobility), radiological success (no furcation radiolucency, internal root resorption, external root resorption): evaluation at 6, 12 and 24 months (at tooth level) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...at each follow‐up examination two investigators who were blinded to the identification of the medicaments ... performed clinical... examination of the pulpotomized teeth" |
| Blinding of radiological outcomes assessment | Low risk | quote: "...at each follow‐up examination two investigators who were blinded to the identification of the medicaments ... performed... periapical examination of the pulpotomized teeth" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Paediatric Dental Clinic of Shahid Beheshti dental School, Tehran, Iran. Operators not mentioned | |
| Participants | 40 children, 80 teeth, mean age 6 years, standard deviation age 0.8 years, age range 4 to 8 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 40 (1 visit)
Group 2: Pulpotomy (calcium enriched mixture); n = 40 (1 visit)
| |
| Outcomes | Clinical failure (swelling/abscess, sinus tract, spontaneous pain, pathological mobility, or a combination), radiological failure (furcation radiolucency, periapical bone destruction, internal root resorption and pathological external root resorption), external root resorption: evaluation at 6, 12 and 24 months (at tooth level) | |
| Notes | Source of funding: "This trial was supported by Iran National Science Foundation and Iranian Center for Endodontic Research, Shahid Beheshti Medical University, Tehran, Iran" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The children were examined clinically by a blinded paediatric dentist" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Radiographic evaluations were performed by a blinded oral radiologist and paedodontist" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Children randomly assigned Conducted in the Clinic of Preventive and Pediatric Dentistry, School of Dentistry, University of Belgrade, Serbia and Montenegro. Operators were 3 paedodontists with a minimum of 5 years' clinical experience | |
| Participants | 104 children, 104 teeth, mean age 6.4 years, standard deviation age 1.1 years, age range 4 to 9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 33 (1 visit)
Group 2: Pulpotomy (calcium hydroxide); n = 34 (1 visit)
Group 3: Pulpotomy (ferric sulphate)n = 37 (1 visit)
| |
| Outcomes | Radiographic success (pathological changes of the alveolar bone in the apical or furcation (or both) area, visible periapical or inter‐radicular radiolucency, integrity of lamina dura, pathological internal resorption, external root resorption), spontaneous pain, abnormal mobility, tenderness to percussion, changes in the integrity of lamina dura, pathological internal resorption, external root resorption, dentine bridge formation, abscess or fistula, apical and furcal destruction: reporting at 3, 6, 12 and 18 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Setting not mentioned. Conducted in Brazil. Operators were 3 authors of the article | |
| Participants | 23 children, 45 teeth, mean age 6 years, standard deviation age 0.4 years, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 15 (1 visit)
Group 2: Pulpotomy (MTA); n = 15 (1 visit)
Group 3: Pulpotomy (calcium hydroxide); n = 15 (1 visit)
| |
| Outcomes | Clinical success (no spontaneous pain, no mobility, no swelling, no fistula and no smell), radiographic success (no internal root resorption, no inter‐radicular bone destruction, no furcation radiolucency or dentine bridge formation), fistula, pathological mobility, inter‐radicular bone destruction, internal root resorption, dentine bridge formation: evaluation at 3, 6, 12, 18 and 24 months (at tooth level) | |
| Notes | Dropouts: "Two children… were lost to follow‐up because they moved to another city" Group 1: 6, 12, 18, 24 months: 1 exfoliation per month Group 2: 18 months: 1 exfoliation Group 3: 12 and 18 months: 1 exfoliation per month; 24 months: 3 exfoliations Exfoliations and extractions were excluded from analysis? No information Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number‐producing system |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...each checkup involved a clinical examination of the pulpotomized teeth, which was performed by two blinded and previously calibrated investigators" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...each checkup involved a periapical radiographic examination of the pulpotomized teeth, which was performed by two blinded and previously calibrated investigators" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% of children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Setting and operators not mentioned. Conducted in Iran | |
| Participants | 58 children, 58 teeth, mean age 5.7 years, standard deviation age 1.5 years, age range 3 to 13 years | |
| Interventions | Group 1: Pulpectomy (ZOE); n = 32 (2 visits)
Group 2: Pulpectomy (calcium hydroxide + iodoform); n = 26 (2 visits)
| |
| Outcomes | Signs of success (absence of pain, fistula, intraoral swelling, extraoral swelling, abnormal mobility, bone radiolucency or position and eruption pathway of the permanent successor tooth), pain symptoms, fistula, pathological mobility, extraoral swelling, intraoral swelling, bone radiolucency, position and eruption pathway of the permanent successor tooth: evaluation at 12 (range 10 to 16) months (at tooth level) | |
| Notes | Of the 58 original children selected and treated at the beginning of the study, 52 returned for follow‐up. Six children had either moved from the area, or changed addresses or phone numbers (or both), and contact was lost Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Outpatient Department, Department of Pediatric Dentistry, Nair Hospital Dental College, Mumbai, India. Operators not mentioned | |
| Participants | 60 children, 70 teeth, age range 4 to 8 years | |
| Interventions | Group 1: Pulpectomy (calcium hydroxide); n = 35 (2 visits)
Group 2: Pulpectomy (ZOE); n = 35 (2 visits)
| |
| Outcomes | Pain symptoms, tenderness to percussion, pathological mobility, pathological radiolucency: evaluation at 1, 3, 6 and 9 months (at tooth level) Radiographic success (the radiolucency did not increase and when it was the same as the preoperative status): evaluation at 3, 6 and 9 months (at tooth level) Clinical success (absence of pain, absence of tenderness to percussion and absence of, or decrease in mobility), signs of success (pain symptoms, tenderness to percussion, pathological mobility, pathological radiolucency): evaluation at 9 months (at tooth level) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive Dentistry, Mangalore, India. Operators not mentioned | |
| Participants | 38 children, 50 teeth | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 25 (2 visits)
Group 2: Pulpotomy (MTA); n = 25 (2 visits)
| |
| Outcomes | Pain, mobility, swelling, sinus tract, internal root resorption, external root resorption (periapical or furcal radiolucency), root resorption in relation to contralateral tooth, pulp canal obliteration: evaluation at 1, 3 and 6 months (at tooth level) | |
| Notes | 3 teeth were not available for further follow‐up after 1 month Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Setting not mentioned. Conducted in Thailand. 1 operator not mentioned | |
| Participants | 37 children, 50 teeth, age range 3 to 8 years | |
| Interventions | Group 1: Pulpectomy (ciprofloxacin + metronidazole + minocycline); n = 25 (1 visit)
Group 2: Pulpectomy (calcium hydroxide + iodoform); n = 25 (1 or 2 visits)
| |
| Outcomes | Clinical success (pain, gingival abscesses, fistula openings or abnormal mobility), radiological success (static or reduced size of bifurcation/periapical radiolucency, no progression of pathological external root resorption, no progression of internal root resorption and no newly formed radiographic lesions), spontaneous pain, tenderness to percussion, swelling, fistula, pathological mobility, abscess, furcal radiolucency, periapical radiolucency, internal root resorption, external root resorption, calcific metamorphosis: evaluation at 9 and 12 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Blinded clinical evaluations were performed by the operator |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Hospital for Sick Children, Toronto, Canada. Operators were 5 paediatric dentists | |
| Participants | 70 children, 172 teeth, mean age 2.5 years, standard deviation age 0.5 years, min‐max 1.5 to 4 years | |
| Interventions | Group 1: Pulpotomy (ferric sulphate); n = 100 (1 visit)
Group 2: Pulpectomy (ZOE); n = 72 (1 visit)
| |
| Outcomes | (1) N equals incisor without pathologic change; (2) P equals pathologic change present, follow‐up recommended; and (3) Px equals pathologic change present, extract. N or Pq were considered an acceptable outcome, while incisors rated as P were considered unacceptable. + presence or absence of periapical radiolucency, pathological external root resorption, widened PDL space, physiological root resorption, internal root resorption, PCO, and dentin bridge formation, and whether the restoration was intact or not + spontaneous pain, tenderness to percussion, fistula/sinus tract, soft tissue swelling, and/or pathological tooth mobility at 12 and 18 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement of Yes or No |
| Blinding of participants and personnel (performance bias) | Unclear risk | No blinding of personnel providing treatment |
| Blinding of clinical outcomes assessment | Low risk | Quote: "A single investigator, who did not perform any pulp therapy or participate in radiographic evaluation, performed all clinical assessments." |
| Blinding of radiological outcomes assessment | High risk | No blinding of raters assessing radiographic outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive dentistry, St. Joseph Dental College and Hospital, Eluru, Andhra Pradesh, India. Operator not mentioned | |
| Participants | 60 children, 60 teeth, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (Biodentine); n = 20 (1 visit)
Group 2: Pulpotomy (diode laser); n = 20 (1 visit)
Group 3: Pulpotomy (MTA); n = 20 (1 visit)
| |
| Outcomes | Clinical criteria (pain, sinus tract, swelling and mobility), radiographic criteria (premature exfoliation, PDL widening, internal/external resorption and periapical/furcal radiolucency): evaluation at 3 and 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Paediatric Dentistry Department, Faculty of Dentistry, Zahedan University of Medical Sciences, Iran. Operators not mentioned | |
| Participants | 46 children, 60 teeth, mean age 6.1 years, age range 5 to 7 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 30 (1 visit)
Group 2: Pulpotomy (MTA); n = 30 (2 visits)
| |
| Outcomes | Clinical success (no pain symptoms, no tenderness of percussion, no swelling, no fistulation or no pathological mobility), radiological success (no evidence of radicular radiolucency, no internal or external root resorption or no periodontal ligament space widening), signs of failure (internal root resorption, furcation radiolucency, periapical bone destruction, pain, swelling or sinus tract), furcation involvement, pulp canal obliteration: evaluation at 6, 12 and 24 months (at tooth level) | |
| Notes | Dropouts: at 24 months "12 out of 30 teeth in the two groups", no reasons stated Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...the children were examined clinically by the author who was blind to which treatment group the subject belonged" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...the children were examined radiographically by the author who was blind to which treatment group the subject belonged" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Pediatric Dentistry unit of the Department of Child Dental Health Lagos University Teaching Hospital. Operator was a paediatric dentist | |
| Participants | 37 children, 50 teeth, mean age 6.1 years, age range 4 to 7 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 25 (1 visit)
Group 2: Pulpotomy (MTA); n = 25 (1 visit)
| |
| Outcomes | Clinical success (no pain, no tenderness to percussion, no swelling or sinus tract, no pathologic tooth mobility), radiological success (normal periodontal ligament space, no furcation or periapical radiolucency, no active/progressing internal root resorption, no pathologic external root resorption): evaluation at 1, 3, 6, 9, and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...clinical assessment of the treated teeth which were only identified by code was carried out by two experienced dentists who were blinded to the treatment groups." |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Paediatric Dentistry Department, University of São Paulo, Brazil. Operators not mentioned | |
| Participants | 45 children, 45 teeth, mean age not mentioned, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (CH); n = 15 (1 visit)
Group 2: Pulpotomy (MTA); n = 15 (1 visit)
Group 3: Pulpotomy (PC); n = 15 (1 visit)
| |
| Outcomes | Clinical success (no spontaneous pain, no swelling, no fistula or no mobility), radiological success (no evidence of furcation radiolucency, no internal root resorption, dentine bridge formation), intra‐canal obliteration, inter‐radicular bone destruction, intra‐canal obliteration: evaluation at 6, 12 and 24 months (at tooth level) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...each check‐up involved a clinical... examination of the pulpotomized teeth, which was performed by two blinded and previously calibrated investigators" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...each check‐up involved a... periapical radiographic examination of the pulpotomized teeth, which was performed by two blinded and previously calibrated investigators" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pediatric Dentistry, University of Ankara, Turkey. Operators were 2 experienced paediatric dentists | |
| Participants | 76 children, 80 teeth, age range 4 to 9 years | |
| Interventions | Group 1: Pulpectomy (ZOE); n = 20 (1 or 2 visits)
Group 2: Pulpectomy (calcium hydroxide eugenol free); n = 20 (1 or 2 visits)
Group 3: Pulpectomy (calcium hydroxide); n = 20 (1 or 2 visits)
Group 4: Pulpectomy (calcium hydroxide + iodoform); n = 20 (1 or 2 visits)
| |
| Outcomes | Clinical success (no pain, no gingival swelling, no tenderness to percussion, no abnormal mobility, no fistula or no abscess), radiological success (no (increase in size of) furcation radiolucency, no (increase in size of) periapical radiolucency, no (increase in size of) discontinuity of lamina dura and no (increase in size of) pathological root resorption), tenderness to percussion, pathological mobility, periapical radiolucency, pathological root resorption, excess filling material and its resorption: evaluation at 2, 4, 6, 8, 10, 12 and 18 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The clinical success were assessed by the clinicians blindly" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "The radiographic success were assessed by the clinicians blindly" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned Conducted at the Department of Pediatric Dentistry, Turkey. Operator was an investigator | |
| Participants | 26 children, 45 teeth, age range 6 to 9 years, mean age: 7.36 ± 0.96 years | |
| Interventions | Group 1: Pulpotomy (FC); n = 15 (1 visit)
Group 2: Pulpotomy (FS); n = 15 (1 visit)
Group 3: Pulpotomy (Ankaferd Blood Stopper); n = 15 (1 visit)
| |
| Outcomes | Clinical failure (spontaneous or severe pain, pathological mobility, swelling or sinus tract, tenderness to percussion or palpation), radiological failure (furcal or periapical radiolucency, didened periodontal ligament spaces, internal or external root resorption, loss of lamina dura), pulp canal obliteration: evaluation every 3 or 6 months (up to 24 months). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin tossing |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Outpatient Department of Pedodontics and Preventive Dentistry, College of Dental Sciences, Davangere, India. Operators not mentioned | |
| Participants | 28 children, 40 teeth, age range 4 to 10 years | |
| Interventions | Group 1: Pulpectomy (ciprofloxacin + metronidazole + minocycline); n = 20 (3 visits)
3Mix (ciprofloxacin + metronidazole + minocycline) after pulpectomy. Commercially available chemotherapeutic agents such as ciprofloxacin, metronidazole and minocycline, were used. After removal of enteric coating, these drugs were pulverised using sterile porcelain mortar and pestle. These powdered drugs were mixed into 2 different combinations in the ratio of 1:3:3, i.e. 1 group being 1 part of ciprofloxacin, 3 parts of metronidazole and 3 parts of minocycline, kept separately to prevent exposure to light and moisture. 1 increment of each powdered drug was mixed with propylene glycol to form an ointment just before use. Canal orifices were enlarged to receive medicament termed as "medication cavity". This was accomplished using a round bur, following which cavities were cleaned and irrigated with the help of saline and dried. The medication cavities were filled with 1 of the pastes and given a temporary dressing with ZOE. Children were recalled after 15 days for resolution of clinical signs and symptoms, following which permanent restoration was done with glass‐ionomer cement. At 30 days, following successful treatment, stainless‐steel crowns were placed and x‐rays taken Group 2: Pulpectomy (ciprofloxacin + ornidazole + minocycline); n = 20 (3 visits)
Ciprofloxacin + ornidazole + minocycline after pulpectomy. Commercially available chemotherapeutic agents such as ciprofloxacin, minocycline and ornidazole were used. After removal of enteric coating, these drugs were pulverised using sterile porcelain mortar and pestle. These powdered drugs were mixed into 2 different combinations in the ratio of 1:3:3, i.e. 1 group being 1 part of ciprofloxacin with 3 parts of ornidazole and 3 parts of minocycline, kept separately to prevent exposure to light and moisture. 1 increment of each powdered drug was mixed with propylene glycol to form an ointment just before use. Canal orifices were enlarged to receive medicament termed as "medication cavity". This was accomplished using a round bur, following which cavities were cleaned and irrigated with the help of saline and dried. The medication cavities were filled with 1 of the pastes and given a temporary dressing with ZOE. Children were recalled after 15 days for resolution of clinical signs and symptoms, following which permanent restoration was done with glass‐ionomer cement. At 30 days, following successful treatment, stainless‐steel crowns were placed and x‐rays taken | |
| Outcomes | Clinical success (absence of spontaneous pain, tenderness to percussion, abnormal mobility and signs of pathology such as intraoral or extraoral abscess), pain symptoms, tenderness to percussion, abscess: evaluation at 3, 6 and 12 months (at tooth level) Radiological success (radiolucency decreased compared with preoperative status or remained same), furcal radiolucency: evaluation at 6 and 12 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the clinic of the department of Pedodontics and Preventive Dentistry, Bapuji Dental College and Hospital, Davangere, India. Operators not mentioned | |
| Participants | 41 children, 60 teeth, age range 4 to 10 years | |
| Interventions | Group 1: Pulpotomy (3Mix); n = 30 (1 visit)
Only the necrotic coronal pulp was removed for pulpotomy. The orifice of the canal was enlarged and was termed as "medication cavity" which was half‐filled with antibacterial mix, before being restored with glass‐ionomer cement and composite Group 2: Pulpectomy (3MIx); n = 30 (1 visit)
Both necrotic coronal as well as all accessible radicular pulp tissue was extirpated for pulpotomy. The orifice of the canal was enlarged and was termed as "medication cavity" which was half‐filled with antibacterial mix, before being restored with glass‐ionomer cement and composite | |
| Outcomes | Pain symptoms, tenderness to percussion, pathological mobility, abscess: evaluation at 1, 6 and 12 months (at tooth level) Furcal radiolucency: evaluation at 6 and 12 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in Saveetha Dental College and Hospital, India. Operator was an investigator | |
| Participants | 88 children, 129 teeth, age range 4 to 9 years | |
| Interventions | Group 1: Pulpectomy (RC Fill); n = 43 (1 visit)
RC Fill available in powder and liquid form, mixed to the desired consistency according to the manufacturer’s instructions. A Lentulo spiral was used to place the RC Fill, followed by glass ionomer cement, before being restored with stainless steel crown. Group 2: Pulpectomy (Vitapex); n = 43 (1 visit)
Vitapex available in preformed syringes. The syringe was inserted into the canal near the apex. The paste was extruded into the canal, and the syringe was then slowly withdrawn as it filled the entire canal, followed by glass ionomer cement, before being restored with stainless steel crown. Group 3: Pulpectomy (ZOE); n = 43 (1 visit)
ZOE available in powder and liquid form, mixed to the desired consistency according to the manufacturer’s instructions. An Endodontic Pressure Syringe was used to place ZOE, followed by glass ionomer cement, before being restored with stainless steel crown. | |
| Outcomes | Clinical failure (pain, tenderness to percussion, swelling/abscess, mobility and draining fistula), radiographic failure (furcation, radiolucency, periapical radiolucency, internal root resorption, external root resorption, lamina dura, deviation in the path of eruption, intraradicular resorption, resorption of extruded material), overall success: evaluation at 6, 12 and 30 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque and sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The participants and outcome assessors were blinded about the filling materials used" |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The participants and outcome assessors were blinded about the filling materials used" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "The participants and outcome assessors were blinded about the filling materials used" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% of children randomly assigned |
| Selective reporting (reporting bias) | Low risk | Protocol prospectively registered (CTRI/2011/06/001776). no discrepancies in outcomes between registered record and published RCT. |
| Methods | RCT, parallel arm Teeth randomly assigned Conducted in the Department of Paediatric Dentistry and Special Care, University Hospital, Ghent University, Belgium. Operators were five (professor, doctoral graduate, doctoral student, master graduate and master student) | |
| Participants | 58 children, 81 teeth, age range 3 to 8 years, mean age: 4.79 ± 1.23 | |
| Interventions | Group 1: Pulpotomy (Biodentine); n = 25 (1 visit)
Group 2: Pulpotomy (MTA); n = 29 (1 visit)
Group 3: Pulpotomy (Tempophore); n = 27 (1 visit)
| |
| Outcomes | Clinical and radiographic scoring criteria adapted from Zurn & Seale (2008): evaluation at 1, 6, 12 and 18 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "All teeth were followed up clinically and radiographically by two blinded calibrated investigators" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "All teeth were followed up clinically and radiographically by two blinded calibrated investigators" |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups in two trials |
| Selective reporting (reporting bias) | High risk | Protocol retrospectively registered (NCT01733420). Registered primary outcomes were reported as secondary outcomes in the published article and new primary outcomes were introduced in the published article. |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive Dentistry, Ragas Dental College and Hospital, Chennai, India. Operators not mentioned | |
| Participants | 77 children, 96 teeth, age range 4 to 7 years | |
| Interventions | Group 1: Pulpectomy (ZOE); n = 34 (1 visit)
Group 2: Pulpectomy (calcium hydroxide + iodoform); n = 30 (1 visit)
Group 3: Pulpectomy (ZOE + calcium hydroxide); n = 32 (1 visit)
| |
| Outcomes | Pain symptoms, furcal radiolucency, periapical radiolucency, excess filling material and its resorption, faster root resorption compared with contralateral, slower root resorption compared with contralateral, similar root resorption compared with contralateral: evaluation at 3, 6 and 9 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive Dentistry, India. Operator was an investigator. | |
| Participants | 50 children, 50 teeth, age range 4 to 9 years | |
| Interventions | Group 1: Pulpectomy (ZOE); n = 24 (1 visit)
Group 2: Pulpectomy (Endoflas); n = 26 (1 visit)
| |
| Outcomes | Clinical success (absence of pain, redness, swelling, tenderness on percussion, and sinus or fistula), radiographic success (reduction in the size of interradicular radiolucency or the size remaining the same): evaluation at 3, 6 and 9 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the paediatric dental clinics, Department of Pediatric Dentistry, Alexandria University, Egypt. Operators not mentioned | |
| Participants | 15 children, 30 teeth, mean age 5 years, standard deviation age 0.7 years, age range 4 to 7 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 15 (1 visit)
Group 2: Pulpotomy (EMD); n = 15 (1 visit)
A cotton pellet was placed to cover the amputated pulpal stumps, and the tooth was then conditioned with polyacrylic acid gel. The cotton pellet was then removed, and the amputated pulpal stumps were covered with protein EMD gel from a 0.3 mL syringe, before being restored with glass‐ionomer cement and stainless‐steel crown | |
| Outcomes | Clinical success (absence of pain, pain on percussion, mobility, and abscess or fistula formation), radiological success (normal periodontal ligament space and had an absence of furcation and periapical radiolucency, pulp calcification, and internal resorption), pain symptoms, tenderness to percussion, pathological mobility, sinus tract, abscess: evaluation at 2, 4 and 6 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "2 examiners who were blinded to treatment type evaluated the teeth clinically" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "2 examiners who were blinded to treatment type evaluated the teeth radiographically" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned. Conducted in Brazil. Operators and setting not mentioned | |
| Participants | 30 children, 30 teeth, mean age 6.8 years, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (Portland cement); n = 15 (1 visit)
Group 2: Pulpotomy (MTA); n = 15 (1 visit)
| |
| Outcomes | Clinical success (no spontaneous pain, no mobility, no swelling, no fistula or no smell), radiographic success (no internal root resorption and no furcation radiolucency, dentine bridge formation), swelling, pathological mobility, sinus tract, inflammation in the adjacent tissues, furcal radiolucency, internal resorption, pulp canal obliteration, dentine bridge formation: evaluation at 6, 12, 18 and 24 months (at tooth level) | |
| Notes | Reasons of dropouts: Group 1: 3 (of 24‐month follow‐up) + 3 (after 24 months) exfoliations Group 2: 1 (of 18‐month follow‐up) + 1 (of 24‐month follow‐up) + 3 (after 24 months) exfoliations Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The primary mandibular molars were randomly assigned to MTA or PC groups by the toss of a coin" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Clinical examination… which was performed by two blinded and previously calibrated investigators" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Periapical radiographic examination… which was performed by two blinded and previously calibrated investigators" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the University of Toronto Faculty of Dentistry Paediatric Clinic, Canada. Operators were 1 of 7 paediatric dental residents, including the primary investigator | |
| Participants | 16 children, 52 teeth, mean age 5.1 years, age range 3 to 8 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 26 (1 visit)
Group 2: Pulpotomy (MTA); n = 26 (1 visit)
| |
| Outcomes | Clinical success (teeth remained asymptomatic, absence of a sinus tract, premature tooth loss), radiographic success (absence of furcal radiolucencies, pathological root resorption, damage to succedaneous follicle, or a combination), signs of success (teeth remained asymptomatic, absence of a sinus tract, absence of furcal radiolucencies, pathological root resorption, damage to succedaneous follicle and premature tooth loss, or a combination), furcal radiolucency, periapical radiolucency, pathological root resorption, root resorption in relation to contralateral: evaluation at (mean ± standard deviation) 2.3 ± 2.1, 5.2 ± 1.9, 9.5 ± 2.3 and 15.7 ±3 months (at tooth level) | |
| Notes | 4 follow‐up visits (mean ± standard deviation): first: 2.3 ± 2.1, second: 5.2 ± 1.9, third: 9.5 ± 2.3, fourth: 15.7 ± 3.0 months Source of funding: quote: "The investigators wish to thank BioLitec and Lasers in Dentistry for the donation of the diode laser, and Dentsply for the donation of the MTA. Funding for this study was provided by the University of Toronto and Alpha Omega. The authors of this study do not have any financial interest in the commercial products used" Comment: Alpha Omega International Dental Fraternity is a Jewish philanthropic charity and presents no apparent conflict of interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | High risk | Quote: "clinical outcome assessments were made by the primary investigator at each follow‐up visit" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "radiographic outcome assessments were made by the primary investigator and one independent experienced clinician who was blind to the treatment" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel arm Teeth randomly assigned Conducted in the clinic of the Pediatric Dentistry Department of the university's School of Dentistry. Operators not mentioned | |
| Participants | 100 children, 100 teeth, mean age 4.3 years, age range 3 to 6 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 50 (1 visit)
Group 2: Pulpotomy (3% NaOCl); n = 50 (1 visit)
| |
| Outcomes | Clinical success (no pain symptoms, tenderness to percussion, swelling, fistula, and pathologic mobility), radiographic success (no evidence of inter‐radicular radiolucency, internal or external root resorption, and periapical radiolucency): evaluation at 6 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The dentists assessing the outcomes were blinded to group assignment" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "The dentists assessing the outcomes were blinded to group assignment" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the paediatric dentistry postgraduate clinics of King Saud University College of Dentistry, Saudi Arabia. Operators not mentioned | |
| Participants | 19 children, 61 teeth, age range 5 to 10 years | |
| Interventions | Group 1: Pulpotomy (glutaraldehyde + ZOE); n = 30 (2 visits)
Group 2: Pulpotomy (glutaraldehyde + calcium hydroxide); n = 31 (2 visits)
| |
| Outcomes | Clinical success (no history of pain, no swelling or sinus tract, no history of thermal sensitivity and no tenderness to percussion), radiographic success (no loss of lamina dura, no loss of trabecular bone, no furcal or periapical radiolucency and no internal resorption), pain symptoms, thermal sensitivity, tenderness to percussion, internal root resorption, changes in the integrity of lamina dura, loss of trabecular bone, furcal or periapical radiolucency: evaluation at 12 months (at tooth level) | |
| Notes | Reasons of dropouts: 2 children with 4 treated teeth did not attend the follow‐up appointments Source of funding: quote: "This project was supported by a grant from the College of Dentistry Research Center (CDRC) at King Saud University" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "...the teeth treated by pulpotomy were only identified by code under the supervision of the assistant" |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...clinical evaluations of the treated teeth were carried out by the investigator without knowing which tooth had been treated with" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...radiographic evaluations of the treated teeth were carried out by the investigator without knowing which tooth had been treated with…" "the… radiographs… were also evaluated by the principal investigator and another pediatric dentist" |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Clinic of the Pediatric Dentistry Department at the Ankara University, Turkey. Operator was the same paedodontist | |
| Participants | Treated: 16 children, 80 teeth; analysed: 11 children, 56 teeth, mean age 6.6 years, age range 4 to9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 13 (analysed) (1 visit)
Group 2: Pulpotomy (ferric sulphate); n = 15 (analysed, not treated) (1 visit)
Group 3: Pulpotomy (calcium hydroxide); n = 13 (analysed, not treated) (1 visit)
Group 4: Pulpotomy (MTA); n = 15 (analysed, not treated) (2 visits)
| |
| Outcomes | Clinical success (no symptoms of pain, no tenderness on percussion, no swelling, no fistulae or no pathological mobility), radiographic success (no periradicular or inter‐radicular radiolucency, no external or internal resorption or no periodontal ligament space widening), signs of success (no symptoms of pain, no tenderness of percussion, no swelling, no fistulae or no pathological mobility, no periradicular or inter‐radicular radiolucency, no external or internal resorption or no periodontal ligament space widening), internal resorption, external resorption, pulp canal obliteration: evaluation at 6, 12, 18 and 24 months (at tooth level) | |
| Notes | 5 excluded participants. Quote: "Four children did not come to follow‐up appointments 6 months after the first treatment and were excluded from the study. Follow‐up of one child with four pulpotomised primary molars had to be discontinued after 1 year because the family moved to another city." Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive Dentistry, The Oxford Dental College, Hospital and Research Center, Bangalore, India. Operators not mentioned | |
| Participants | 19 children, 40 teeth, age range 6 to 8 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 20 (2 visits)
Group 2: Pulpotomy (MTA); n = 20 (2 visits)
| |
| Outcomes | Clinical success (no history of pain, no tenderness to percussion, no gingival abscess, no sinus/fistula and no pathological mobility), radiographic success (no internal/external root resorption or no periapical/furcal radiolucency), signs of success (no history of pain, no tenderness to percussion, no gingival abscess, no sinus/fistula and no pathological mobility, no internal/external root resorption or no periapical/furcal radiolucency), furcal radiolucency, pulp canal obliteration, dentine bridge formation: evaluation at 1, 6, 12 and 24 months (at tooth level) | |
| Notes | Source of funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics and Preventive Dentistry, The Oxford Dental College, Hospital and Research Centre, Bangalore, India. Operators not mentioned | |
| Participants | Number of enrolled children not mentioned, 45 teeth, age range 5 to 9 years | |
| Interventions | Group 1: Pulpectomy (calcium hydroxide + iodoform); n = 15 (2 visits)
Group 2: Pulpectomy (calcium hydroxide + ZOE + iodoform); n = 15 (2 visits)
Group 3: Pulpectomy (ZOE); n = 15 (2 visits)
| |
| Outcomes | Clinical success (no gingival swelling/inflammation/redness, no sinus opening in the oral mucosa or purulent exudate expressed from the gingival margin, no abnormal mobility other than mobility due to normal exfoliation, absence of pain on percussion/tenderness), radiographic success (no evidence of extensive pathological root resorption, reduction or no change in preoperative pathological inter‐radicular or periapical radiolucency (or both), no evidence of development of new postoperative pathological radiolucency involving the succedaneous tooth germ), pain symptoms, tenderness to percussion, swelling, pathological mobility, pathological root resorption, damage in succedaneous follicle: evaluation at 3, 6, 12 and 18 months (at tooth level) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned. Conducted in Thailand Setting not mentioned. Operator was 1 investigator (paediatric dentist) | |
| Participants | 42 children, 54 teeth, mean age 5.6 years, standard deviation age 1.2 years, age range 3.3 to 7.8 years | |
| Interventions | Group 1: Pulpectomy (ZOE); n = 27 (1 visit)
Group 2: Pulpectomy (calcium hydroxide + iodoform); n = 27 (1 visit)
| |
| Outcomes | Clinical success (no pain, healthy soft tissue (defined as the absence of swelling, redness or sinus tract) and no abnormal mobility), radiographic success (radiographic continuity of the lamina dura, reduction in the size of any pathological inter‐radicular or periapical radiolucencies (or both) or evidence of bone regeneration), signs of success (absence of change or more discontinuity of lamina dura and absence of change in size of radiolucency area), pain symptoms, swelling, fistula, pathological mobility: evaluation at 6 and 12 months (at tooth level) | |
| Notes | Source of funding: "The authors wish to thank the Chulalongkorn University Postgraduate Research Fund for financial support" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "the clinical diagnoses were blindly assessed by another investigator" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "the radiographic diagnoses were blindly assessed by another investigator" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned. Conducted in Turkey Setting and operators not mentioned | |
| Participants | 25 children, 50 teeth, age range 5 to 8 years | |
| Interventions | Group 1: Direct pulp capping (MTA + ZOE); n = 25 (1 visit)
Group 2 : Direct pulp capping (CH + ZOE); n = 25 (1 visit)
| |
| Outcomes | Clinical success (no spontaneous pain, no tenderness of percussion, no swelling, no fistulation or no pathological mobility), radiographic success (no furcation radiolucency, no periodontal ligament space widening or no internal or external root resorption), thermal sensitivity: evaluation at 3, 6, 12, 18 and 24 months (at tooth level) | |
| Notes | Reasons of dropouts: 1 child did not return for evaluation after 1 month, 1 after 9 months and 1 after 12 months because of the loss of restoration that had been placed on the pulp capping material, 1 tooth was excluded from the clinical study after 9 months and 1 tooth after 18 months, both from the CH group Lost to follow‐up: Group 1: failure to attend, n = 3; Group 2: failure to attend, n = 3; loss of restoration, n = 2 Analysed: Group 1: n = 22; Group 2: n = 20. No exclusions Source of funding: quote: "This study was supported financially by the Scientific Research Foundation of Gazi University, Ankara, Turkey (grant no. 03/2003‐15)" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...two investigators, who attended a calibration session before the follow‐up examinations, blindly evaluated the teeth clinically" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...two investigators, who attended a calibration session before the follow‐up examinations, blindly evaluated the teeth radiographically" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Paediatric Dentistry, Vishnu Dental College, Bhimavaram. Operator not mentioned | |
| Participants | 29 children, 40 teeth, mean 5.6, age range 4 to 7 years | |
| Interventions | Group 1: Pulpotomy (MTA); n = 20 (1 visit)
Group 2: Pulpotomy (low‐level laser therapy);n = 20 (1 visit)
| |
| Outcomes | Clinical success (no pain, tenderness to percussion, swelling, fistulation or pathologic mobility), radiologic success (no radicular radiolucency, internal or external root resorption or periodontal ligament space widening), overall success: evaluation at 3, 6 and 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Department of Pedodontics, Faculty of Dentistry, Turkey. Operator was the principal investigator | |
| Participants | 40 children, 40 teeth, mean age 7.3 years, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (CH cement/Dycal); n = 20 (1 visit)
Group 2: Pulpotomy (calcium sulphate hemihydrate/Dentogen); n = 20 (1 visit)
| |
| Outcomes | Clinical success (no pathologic mobility, fistula, spontaneous pain, sensitivity to percussion/palpation, oedema), radiographic success (no external root resorption, internal root resorption, inter‐radicular radiolucency, periapical radiolucency), inter‐radicular radiolucency, external root resorption, internal root resorption, fistula, pathologic mobility, spontaneous pain: evaluation at 1, 3, 6, 9 and 12 months (at tooth level). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "...all clinical... recall examinations were performed by the same clinician who was blinded to the treatment groups" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...all... radiographic recall examinations were performed by the same clinician who was blinded to the treatment groups" |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Department of Pediatric Dentistry, The University of Iowa, Iowa City, Iowa, USA. Operator was the principal investigator | |
| Participants | 23 children, 60 teeth, mean age 5 years, age range 4 to 9 years | |
| Interventions | Group 1: Pulpotomy (ferric sulphate); n = 28 (1 visit)
Group 2: Pulpotomy (sodium hypochlorite); n = 32 (1 visit)
| |
| Outcomes | Clinical failure (mobility, swelling, fistula, history of spontaneous pain), radiographic success (no external root resorption, no internal root resorption, no inter‐radicular bone destruction), overall success ((% clinical success + % radiographic success)/2), pain palpation, swelling, fistula, pathological mobility, redness, bleeding, furcation involvement, internal resorption: evaluation at 6 and 12 months (at tooth level) | |
| Notes | No reason of dropouts, except "2 teeth exfoliated and were eliminated from further follow‐up" Source of funding: quote: "This research was supported by the Obermann Center for Advanced Studies Spelman Rockefeller Grant from The University of Iowa, Iowa City, Iowa" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random table |
| Allocation concealment (selection bias) | Low risk | Quote: "subject assignment was made at the consent appointment, but allocation of the tooth according to the allocation sequence was made the day of the treatment visit"; "this allocation followed the current guidelines for randomised clinical trials put forth by CONSORT [Consolidated Standards of Reporting Trials]" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Quote: "...the clinical examination was performed by the principal investigator without immediate knowledge of which treatment has been rendered on which tooth" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...all radiographs were read… by 2 co‐investigators who were blinded to the technique used" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the paediatric dental clinic within the Dental Hospital, Newcastle‐upon‐Tyne, UK. Operator not mentioned | |
| Participants | 52 children, 84 teeth, mean age 5 years, age range 3.3 to 12.5 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 46 (1 visit)
Group 2: Pulpotomy (calcium hydroxide); n = 38 (1 visit)
| |
| Outcomes | Clinical failure (symptoms from the treated tooth reported by the child or parent, spontaneous pain, pain initiated by stimuli, signs of defective restoration or recurrent caries, signs of mobility, sinus formation, tenderness to percussion, soft tissues swelling, signs of exfoliation, mobility or signs/symptoms of the successor tooth erupting), tenderness to percussion, swelling, pathological mobility, sinus tract, secondary caries, defective restoration: evaluation at 6 and 12 months (at tooth level) Radiographic success (defective restoration or recurrent caries, periradicular pathology such as periapical or furcal radiolucency, pathological internal resorption, replacement resorption, intracanal calcifications, physiological root resorption, position and eruption pathway of the permanent successor tooth), periradicular radiolucency, furcal radiolucency, periapical radiolucency, internal resorption, pulp canal obliteration, physiological root resorption, recurrent caries: evaluation at 12 months (at tooth level) | |
| Notes | 5 teeth lost to follow‐up Clinical follow‐up: 22.5 months (range 6.1 to 38.5) Radiographic follow‐up: 18.9 months (range 1.3 to 36.9) Source of funding: "This study was supported by The Shirley Glasstone‐Hughes Memorial prize awarded to the authors by the British Dental Association, in September 1993" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "Objectivity was maximized during clinical assessment, by not having direct access to records detailing which pulp therapy agent was used" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "Objectivity was maximized during radiographic assessment, by not having direct access to records detailing which pulp therapy agent was used" |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to make a clear judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in Sudha Rustagi Dental College, Faridabad. Operator not mentioned | |
| Participants | 37 children, 45 teeth, age range 4 to 7 years | |
| Interventions | Group 1: Pulpotomy (15.5% ferric sulphate); n = 15 (1 visit)
Cotton pellet was first saturated with 15.5% ferric sulphate and later compressed between gauze to remove excess so it was just moistened with the solution. It was then placed for 15 seconds on amputated pulp stumps. After this the pulp stumps were observed for brownish to black discolouration of the fixed radicular pulp tissue. Excess ferric sulphate was flushed from the pulp chamber with copious amount of saline and clot remnants were removed from the chamber followed by placement of a thick mix of zinc oxide eugenol into the pulp chamber. Then teeth restored by glass ionomer cement Group 2: Pulpotomy (electrosurgery); n = 15 (1 visit)
The ART‐E1 electrosurgery unit was set at COAG 1 mode to perform both electrofulguration and electrocoagulation. The handpiece with appropriate electrode tips, kept 1 to 2 mm away from the pulpal tissue, was used to deliver the electric current. The duration of application was not more than 2 to 3 seconds followed by a cool down period of 5 seconds. If necessary, this procedure was repeated up to a maximum of three times. After each current application, a new large moist sterile cotton pellet was placed with pressure on the pulpal tissue near to orifice to absorb any blood or tissue fluids before the next current application (e.g. pellet‐electrode‐pellet‐electrode). When properly completed, the pulpal stumps appeared dry and completely blackened. This was followed by placement of a thick mix of zinc oxide eugenol into the pulp chamber. Then teeth restored by glass ionomer cement Group 3: Pulpotomy (diode laser); n = 15 (1 visit)
The remaining coronal pulp tissue was exposed to laser energy through an optical fibre using the diode laser (810 nm, output power: 7 W) set at 3 W of power in Continuous Wave. The laser energy was delivered through a 400 μm diameter optical fibre in a non contact mode with pulp tissue for not more than 2‐3 sec (PD = 2388.53, Fluence = 7165.60). Application of laser was administered until the pulp was ablated and complete haemostasis was achieved. All children and clinical staff wore appropriate eye protection during application of the laser. Applications were administered as per the requirement of each tooth followed by placement of a thick mix of zinc oxide eugenol into the pulp chamber. Then teeth restored by glass ionomer cement | |
| Outcomes | Clinical success (absence of pain and tenderness, absence of abscess, absence of sinus or fistula, absence of mobility), radiographic success (absence of widened periodontal space, absence of inter‐radicular or periapical radiolucency, absence of sinus or fistula, absence of internal resorption, absence of abnormal canal calcification): evaluation at 1, 3, 6 and 9 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Gülhane Military Medical Academy (GMMA) Pediatric Dentistry Clinic. One operator (investigator). | |
| Participants | 65 children, 140 teeth, age range 5 to 9 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 35 (1 visit)
Group 2: Pulpotomy (MTA); n = 35 (1 visit)
Group 3: Pulpotomy (Portland cement); n = 35 (1 visit)
Group 4: Pulpotomy (EMD); n = 35 (1 visit)
| |
| Outcomes | Clinical failure (spontaneous pain, swelling, fistula), radiological failure (radiolucency of the periapical or furcation, and pathological external root resorption), overall success, pulp canal obliteration, internal root resorption, marginal adaptation of the crown, crushing or deformities of the crown, changes in occlusion: evaluation at 3, 6, 12, 18, and 24 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Incomplete outcome data (attrition bias) | Low risk | Proportion of missing outcomes < 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, parallel‐arm Teeth randomly assigned Conducted in the Children's Clinic of the University of Michigan School of Dentistry, USA. Operator not mentioned | |
| Participants | 152 children, 252 teeth, mean age 5.5 years, standard deviation age 1.5 years, age range 2.5 to 10 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 133 (1 visit)
Group 2: Pulpotomy (MTA); n = 119 (1 visit)
| |
| Outcomes | Clinical success (not clearly defined), radiographic failure (internal root resorption, external root resorption, internal root resorption with perforated form, periradicular lesion), score 2‐1 (clinically), score 2‐2 (clinically), score 2‐3 (clinically), score 2‐4 (clinically), internal resorption, internal resorption with perforated form, external resorption, periodontal ligament widening, pulp canal obliteration, dentine bridge formation, score 7‐1 (rx), score 7‐2 (rx), score 7‐3 (rx), score 7‐4 (rx): evaluation at 6 months (at tooth level) | |
| Notes | 203/252 teeth were available for the 6‐month evaluation resulting in 19% lost at follow‐up Source of funding: "This study was supported by Michigan Institute for Clinical & Health Research and Delta Dental Foundation of Michigan. The authors declare no conflict of interest" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization of the medicament used was done by an envelope draw" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Low risk | Quote: "The blinded clinical examination was performed by 1 to 19 operators who were calibrated to the clinical scoring criteria" |
| Blinding of radiological outcomes assessment | Low risk | Quote: "All radiographs were viewed by 4 blinded, calibrated evaluators" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
| Methods | RCT, split‐mouth Teeth randomly assigned Conducted in the Department of Pediatric Dentistry, Baylor College of Dentistry Texas, Health Science Center, Dallas, Texas, USA. Operator were 2 standardised operators | |
| Participants | 23 children, 76 teeth, mean age 5.3 years, standard deviation age 1.7 years, age range 2.3 to 8.5 years | |
| Interventions | Group 1: Pulpotomy (formocresol); n = 38 (1 visit)
Group 2: Pulpotomy (calcium hydroxide); n = 38 (1 visit)
| |
| Outcomes | Clinical success (not clearly defined), radiographic failure (not clearly defined), overall success (the cumulative rate of failure due to clinical abscesses or osseous radiolucencies was calculated for each treatment, as was an overall cumulative rate of success. These calculations were based on the following equation: failure percentage = 100% x (previous failures + new failures)/(previous failures + currently examined teeth)), abscess, internal resorption, internal resorption with perforated form, external resorption, periodontal ligament widening, calcific metamorphosis, bone radiolucency: evaluation at 0 to 6, 7 to 12 and 13 to 24 months (at tooth level) | |
| Notes | 3 children were lost due to failure to return for follow‐up Analysed: 20 children, 68 teeth Source of funding: quote: "This research project won the Ralph E. MacDonald (sic) Award at the 2006 AAPD annual session for the most outstanding research presented by a graduate student" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of clinical outcomes assessment | Unclear risk | Insufficient information to make a clear judgement |
| Blinding of radiological outcomes assessment | Low risk | Quote: "...all postoperative radiographs were digitally scanned and evaluated by 2 standardized and calibrated examiners. To blind the examiners to the treatment regimens, the coronal portions were blackened‐out" |
| Incomplete outcome data (attrition bias) | High risk | Proportion of missing outcomes > 10% children randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make a clear judgement |
CEM: calcium‐enriched mixture; CH: calcium hydroxide; clin: clinically; EMD: enamel matrix derivative; Er‐YAG: erbium:yttrium‐aluminium garnet; FC: formocresol; FS: ferric sulphate; IRM: intermediate restorative material (reinforced zinc oxide and eugenol); MTA: mineral trioxide aggregate; n: number of teeth; PC: Portland cement; RCT: randomised controlled trial; rx: radiographically; ZOE: zinc oxide and eugenol
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Not an RCT | |
| Biomaterials not compared | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Human and dog permanent teeth. In vitro study | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Review | |
| Not an RCT | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to obtain further information from the authors were unsuccessful | |
| Not an RCT | |
| Not an RCT | |
| Not an RCT | |
| Review | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Not an RCT | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Duplicate | |
| Biomaterials not compared | |
| Not an RCT | |
| Not an RCT | |
| Restorative dentistry | |
| Ongoing trial comparing pulpotomy formocresol with electrical pulpotomy, which was terminated because use of one of the materials was discontinued | |
| Not an RCT | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Case report | |
| Review | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Case report | |
| Review | |
| Not an RCT. Intact human teeth | |
| Not an RCT | |
| Abstract only. Insufficient information presented. Attempts to contact the authors were unsuccessful | |
| Not an RCT | |
| Not an RCT | |
| Not an RCT | |
| Not an RCT |
Abbreviation ‐ RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Root Canal Treatment in Milk Teeth using Three Root Canal Filling Materials: a Double‐Blinded Randomized Controlled Trial |
| Methods | RCT with participant and outcome assessor blinding |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | RC fill |
| Outcomes | Clinical evaluation: pain, redness, swelling/abscess, draining fistula and mobility Clinical and radiographic evaluation of three root filling materials for a period of 3,6 and 12 months |
| Starting date | 10 June 2011 first recruitment |
| Contact information | Dr R Pramila (Postgraduate (Pedodontics)) |
| Notes |
| Trial name or title | Comparative Evaluation of Pulpotomized Primary Molars With Mineral Trioxide Aggregate and New Endodonthic Cement |
| Methods | "Forty patients are selected randomly. Each patient has at least 2 teeth which require pulpotomy treatment. After removing of carious teeth by a low speed round bur and pulp exposure, roof of pulp chamber is removed completely by a high speed 008 fissure bur. Life tissues of pulp are removed by sharp excavator and rinsing with normal saline. Hemostat is achieved and cavity will be cleaned by 0.5% hypo chlorate solution. MTA or NEC material is mixed according to manufacturer instruction and will be placed in pulp chamber and over pulpal canal orifices for at least 1 mm. The light cure glass ionomer is also mixed according to manufacturer instruction and is placed over the A or B material and cured for 40 minutes. The treated tooth will be restored with a stainless steel crown or amalgam filling material." |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental A: teeth that are treated with Mineral Trioxide Aggregate (MTA) material Experimental B: teeth that are treated with new Endodontic Cement (NEC) material |
| Outcomes | Primary outcome measures: clinical features and radiographic examination |
| Starting date | October 2008 |
| Contact information | Contact: Fatemeh Shekarchi, student |
| Notes |
| Trial name or title | Comparison of Mineral Trioxide Aggregate (MTA) and 20% formocresol in Pulpotomized Human Primary Molars |
| Methods |
|
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Primary: clinically and radiographically outcomes (time frame: six, 12, 18, and 24 months); Secondary: histological outcome (time frame: when the subjective tooth physically exfoliates from oral cavity) |
| Starting date | September 2009 |
| Contact information | Contact: Yuan‐Ling Lee, PhD, Contact: Hsiao‐Hua Chang, MS |
| Notes |
| Trial name or title | Antimicrobial Pulpotomy of Primary Molars |
| Methods | None |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | None |
| Starting date | August 2000 |
| Contact information | None |
| Notes |
| Trial name or title | MTA and Biodentine in Pulpotomized Primary Molars |
| Methods | Parallel RCT |
| Participants | Age 4 to 9 years Inclusion criteria
Exclusion criteria
|
| Interventions | Biodentine and MTA |
| Outcomes | Primary
Secondary
Time frame for all secondary outcomes: 6 and 12 months |
| Starting date | March 2012 |
| Contact information | Cristina Cuadros, International University of Catalonia |
| Notes |
| Trial name or title | Biodentine Versus White MTA Pulpotomy |
| Methods | Parallel RCT |
| Participants |
|
| Interventions | Experimental: Biodentine Active comparator: white mineral trioxide aggregate (MTA) Active comparator: Tempophore |
| Outcomes | Not provided |
| Starting date | October 2011 |
| Contact information | Luc Martens, Ghent University |
| Notes |
| Trial name or title | Sodium Hypochlorite Pulpotomies in Primary Molars: Comparison With Conventional 20% Formocresol Pulpotomies |
| Methods | Formocresol is the most universally taught and most widely used pulpotomy medicament in the primary teeth. However, concerns have been raised over the use of formocresol because of its toxicity and potential carcinogenicity. A substitute for formocresol has been investigated but evidence is lacking to conclude which is the most appropriate technique for pulpotomies in primary teeth. Sodium hypochlorite (NaOCl) has been used in root canal irrigant for more than 80 years, and it is at present the most popular irrigant in root canal treatment. Studies have showed that NaOCl is biological compatible and is a very good antimicrobial solution without being a pulpal irritant. Recent studies using sodium hypochlorite as pulpotomy medicament in primary molars showed promising results. In this project, the investigators propose a randomised clinical trial, which will be performed in Paediatric Dentistry Department of the National Taiwan University Hospital, to compare the treatment outcomes between NaOCl and formocresol in human primary molars needing pulpotomy treatment. The aim of this study is to determining whether NaOCl is a suitable replacement for formocresol in the pulpotomy of human primary molar teeth. To assess this aim, 200 healthy children aged from 2.5 to 9 years, who have at least one primary first or second molars diagnosed to receive pulpotomy treatment will be recruited. The involved teeth will be randomly assigned to the control group (dilute 20% formocresol (DFC)) or experimental group (2.5% NaOCl). At three, six, nine, 12, 15, 18, 21 and 24 months post‐treatment, the randomly assigned teeth will be clinically and radiographically evaluated by blinded independent evaluators to the treatment group. The differences will be statistically analysed using Chi² test, Fisher's exact test, and t‐test, using a statistical significance at P < 0.05. |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Primary: change of clinical findings (time frame: at three, six, nine, 12, 15, 18, 21 and 24 months post‐treatment). The outcome will be assessed first by clinical findings. We can discriminate the result are successful or not by scoring the clinical finding from 1 to 4. Criteria for clinical scoring asymptomatic, clinical score = 1 Slight discomfort: percussion sensitivity; mobility > 1 mm but < 2 mm, clinical score = 2 Minor discomfort: long‐lasting chewing sensitivity; gingival swelling; periodontal pocket formation without exudate; mobility> 2 mm but < 3 mm, clinical score = 3 major discomfort: Late pathological changes; spontaneous pain; periodontal pocket formation with exudate; sinus tract; mobility ≧ 3 mm; premature tooth loss due to pathology, clinical score = 4 Secondary: change of radiographic findings (time frame: at three, six, nine, 12, 15, 18, 21 and 24 months post‐treatment). The outcome will be assessed then by radiographic findings. We can discriminate the result are successful or not by scoring the radiographic findings from1 to 5. Criteria for radiographic scoring Dentinal bridge, clinical score = 1, regeneration tissue response No change, clinical score = 2, no pathological changes Pulp canal obliteration, clinical score = 3, slight pathological changes, no clinical significance Periodontal ligament widening, clinical score = 3, slight pathological changes, no clinical significance Internal root resorption (non‐perforated), clinical score = 4, minor pathological changes External root resorption, clinical score = 4, minor pathological changes Internal root resorption (perforated), clinical score = 4, minor pathological changes Peri‐radicular lesion, clinical score = 5, major pathological changes, treatment needed |
| Starting date | August 2011 |
| Contact information | Hsiao‐Hua Chang, PhD |
| Notes |
| Trial name or title | Randomized Clinical Trial for Primary Molar Pulpotomy, Biodentine versus Formocresol‐ZOE |
| Methods | None |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes |
|
| Starting date | September 2014 |
| Contact information | None |
| Notes |
| Trial name or title | Success Rate Evaluation of Miniature Pulpotomy With MTA in Primary Molars |
| Methods | None |
| Participants | 4 years to 7 years (child) Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Primary: successful outcome of treatment as indicated by clinical signs defined with observation and checklist (time frame: up to 12 months) success or failure of treatment defined with observation and checklist Secondary: successful outcome of treatment as indicated by radiographic signs defined with observation and checklist (time frame: up to 12 months) success or failure of treatment defined with observation and checklist |
| Starting date | February 2014 |
| Contact information | None |
| Notes |
| Trial name or title | Vital Pulp Treatment in Primary Teeth |
| Methods | Paediatric patients having deep decay in primary molars seen at UMMC, UMSOD, and University of Maryland Rehabilitation and Orthopaedic Institute, will be included in the sample. Teeth with deep caries, > 50% into dentin, will be randomly assigned using a table of random numbers to the three treatment groups: Group 1 pulpotomy with MTA, Group 2 pulpotomy with Biodentine, Group 3 indirect pulp treatment. Treatment will be performed by board certified paediatric dentists or they will directly supervise paediatric dental residents at each site as part of their regular protocol for treating deep caries. Radiographs will be taken as prescribed in the Guideline for taking Radiographs in Children by the American Academy of Pediatric Dentistry. Twice‐yearly clinical examinations will be performed by the treating dentists or paediatric dental residents to check for any soft tissue pathology such as abscess or mobility of treated tooth/teeth. If treatment success/failure consensus between the blinded dentists is not reached, a third dentist will be consulted. The success/failure data will be entered onto spreadsheets and examined statistically using statistical software. |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes |
|
| Starting date | November 2015 |
| Contact information | None |
| Notes |
| Trial name or title | Biodentine Partial Pulpotomy of Pulpally Exposed Primary Molars |
| Methods |
|
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Primary
Secondary
|
| Starting date | May 2015 |
| Contact information | Contact: Avia Fux‐Noy, DMD, Contact: Hadas Lemberg, PhD |
| Notes |
| Trial name or title | Success and Color Stability of MTA Pulpotomized Primary Molars: an RCT (MTA) |
| Methods | This randomised control, split‐mouth trial will use 50 paediatric participants selected from the patient population in the paediatric dental clinics at Baylor College of Dentistry and in select faculty private practices. The study will use a within‐subject control design whereby one tooth will be treated with a pulpotomy using the new formulation of MTA (NeoMTA Plus, Avalon Biomed Inc., Bradenton, FL, USA) and restored with a multi‐surface composite, and the other tooth with an MTA pulpotomy and restored with a SSC; thus, approximately 50 teeth will be treated for each treatment group. The restoration type will be randomised as to which side will receive the SSC or composite using sealed, opaque envelopes. Approximately 50 participants will be needed for the study in order to elicit any significant findings as demonstrated by a power analysis from a similar study. |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes |
|
| Starting date | November 2014 |
| Contact information | Carolyn A Kerins, DDS, PhD |
| Notes |
| Trial name or title | Comparison of mineral trioxide aggregate (MTA) and ferric sulfate pulpotomies |
| Methods | Comparison of clinical and radiographic success between MTA and ferric sulphate pulpotomies for primary molars. Recall appointments are completed six months, nine months and 12 months. Regular recall and follow‐up will be performed for patients who has MTA or ferric sulphate pulpotomies. Clinical and radiographic findings will be recorded. |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Comparison of the clinical and radiographic success between MTA and ferric sulphate pulpotomies in primary molars (time frame: 1 year). At recall visits six, nine and 12 months, blinded clinical examination will be completed by participating faculty members who are calibrated to clinical scaring criteria. Periapical radiographs will be taken and evaluated by 2 paediatric dentists and 1 endodontist, for presence of various pathologies. Scored based on the criteria established by Zurn and Seale 2008. Scores will be transferred to Microsoft Excel. The difference between the two materials will be analysed using the Mann‐Whitney U test, Chi² test and Fisher's exact test. Intra‐ and inter‐rater agreement will be measured for radiographic assessment using Cohen's kappa test |
| Starting date | April 2016 |
| Contact information | Jung‐Wei Chen, DDS, MS, PhD |
| Notes |
| Trial name or title | Clinical and radiographical evaluation of the effect of Dycal and Biodentine in DPC in primary teeth |
| Methods | "The aim of the present study is to compare Calcium Hydroxide cement (Dycal) and Calcium Silicate cement (Biodentine)TM as pulp capping agents in primary molars. The objective of this study include the evaluation of clinical and radiographic efficacy of Calcium Hydroxide cement (Dycal) and Calcium Silicate cement (Biodentine), and their response in direct pulp capping treatment on primary molars during a 6‐month follow‐up. After following the proper standardized procedure for direct pulp cap. In the current study direct pulp capping was performed using calcium hydroxide cement (Dycal) and Calcium Silicate cement (Biodentine) on 60 primary teeth of children equally divided between 2 study groups randomly of both sexes aged 4 to 9 years old. Complete case history was recorded in detail and intraoral periapical radiograph was also taken for teeth indicated for direct pulp capping. Written consent was obtained from the parents of participants before starting the procedure. Strict standardised procedure had been followed and the pulp capping agent (Dycal/Biodentine) were applied according to the manufacturer's instructions. Each participant was evaluated clinically and radiographically for any abnormal clinical signs and symptoms at one, three and six months postoperatively. Better results for the success of the study could be relatively enhanced by close attention to rigid criteria for case selection, standardisation of direct pulp capping procedure and meticulous performance of the procedure appear to be prerequisites for successful treatment." |
| Participants | Inclusion criteria
In addition, the teeth treated by direct pulp capping had only a pinpoint mechanical exposure (0.5 mm to 1 mm), for which haemorrhage control could be achieved within two minutes before proceeding with direct pulp capping. Radiographically, there was absence of internal resorption, external resorption, periapical or furcation radiolucencies and pathology of succedaneous permanent tooth follicle. Exclusion criteria
|
| Interventions |
|
| Outcomes | Evidence of effectiveness of Dycal and Biodentine as Direct Pulp Capping agent in primary molars confirmed by clinical and radiographic evaluation (time frame: 6 months) |
| Starting date | June 2014 |
| Contact information | Dr Komal IM Gandhi, BDS, Dr Mishthu Solanki, MDS |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 13 | 1048 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.07, 1.89] |
| 1.2 12 months | 12 | 740 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.10, 0.93] |
| 1.3 24 months | 9 | 548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.18, 1.19] |
| 2 Radiological failure Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 12 | 922 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.17, 0.86] |
| 2.2 12 months | 12 | 740 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.19, 0.89] |
| 2.3 24 months | 9 | 548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.22, 0.80] |
| 3 Overall failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 3 Overall failure. | ||||
| 3.1 6 months | 6 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.04, 1.32] |
| 3.2 12 months | 6 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.17, 1.36] |
| 3.3 24 months | 7 | 368 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.25, 1.01] |
| 4 Pain Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4 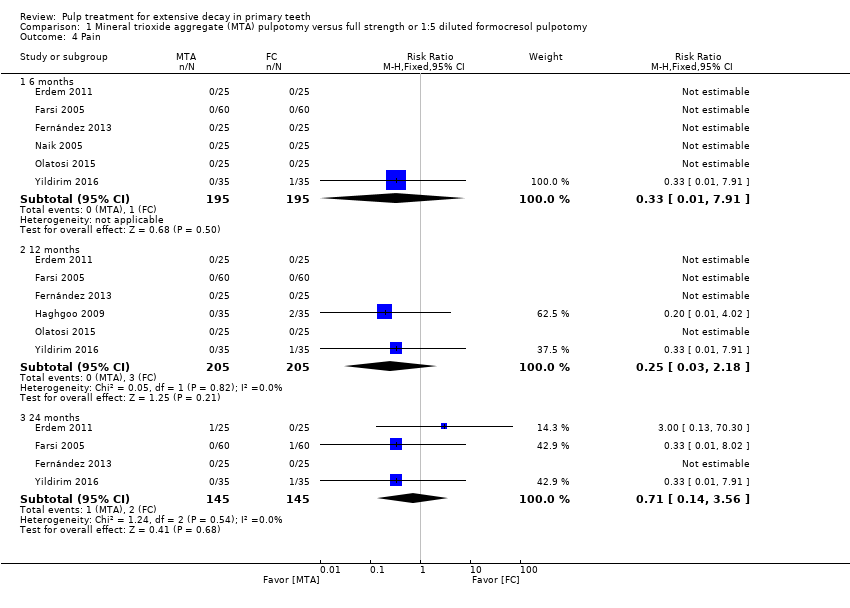 Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 4 Pain. | ||||
| 4.1 6 months | 6 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 4.2 12 months | 6 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.18] |
| 4.3 24 months | 4 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.14, 3.56] |
| 5 Soft tissue pathology Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.5 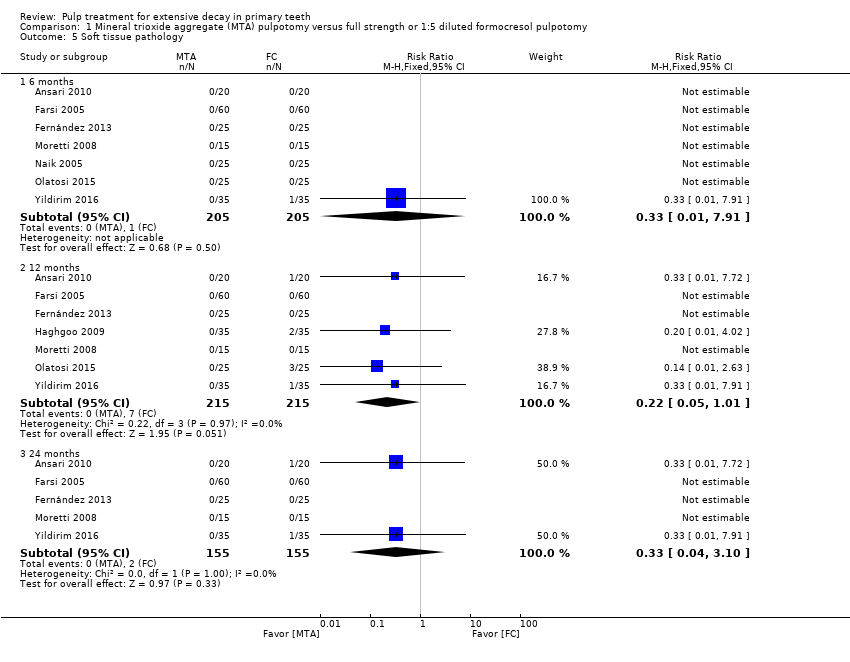 Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 5 Soft tissue pathology. | ||||
| 5.1 6 months | 7 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5.2 12 months | 7 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 1.01] |
| 5.3 24 months | 5 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.10] |
| 6 Pathological mobility Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 6 Pathological mobility. | ||||
| 6.1 6 months | 5 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 6.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pathological radiolucency Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.7 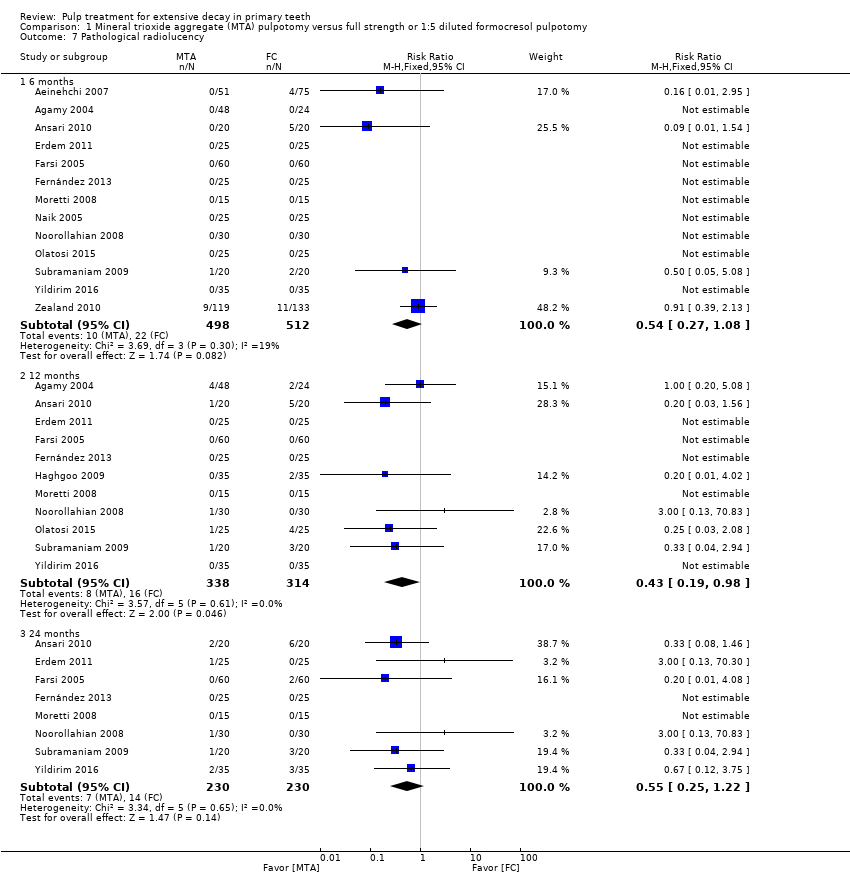 Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 7 Pathological radiolucency. | ||||
| 7.1 6 months | 13 | 1010 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.27, 1.08] |
| 7.2 12 months | 11 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.19, 0.98] |
| 7.3 24 months | 8 | 460 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.25, 1.22] |
| 8 Pathological root resorption Show forest plot | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.8 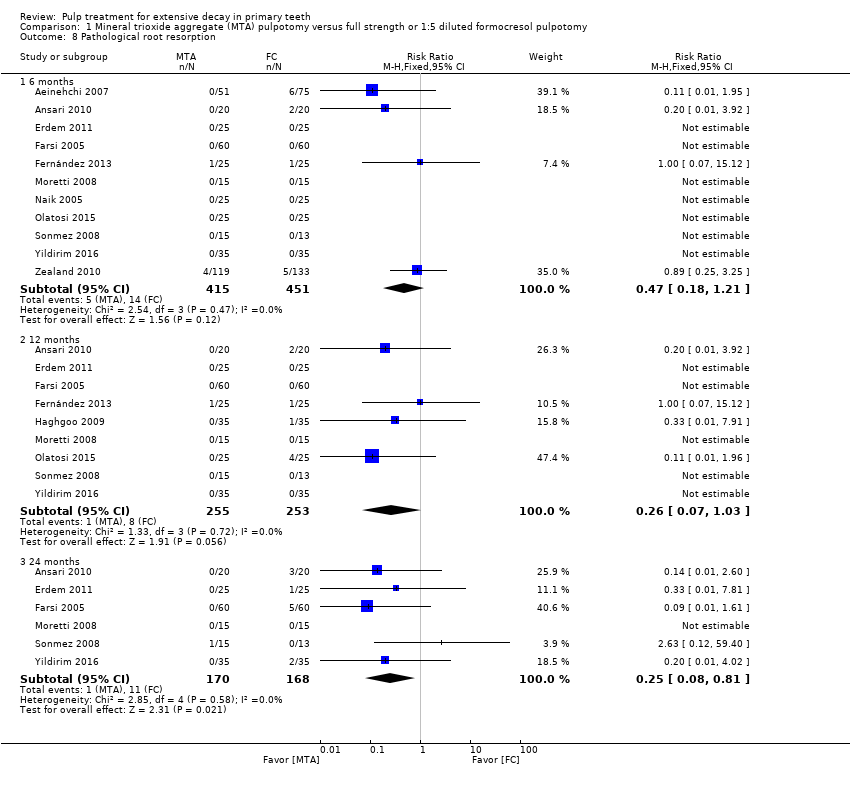 Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 8 Pathological root resorption. | ||||
| 8.1 6 months | 11 | 866 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.18, 1.21] |
| 8.2 12 months | 9 | 508 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.07, 1.03] |
| 8.3 24 months | 6 | 338 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.08, 0.81] |
| 9 Pulp canal obliteration Show forest plot | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 9 Pulp canal obliteration. | ||||
| 9.1 6 months | 9 | 712 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.00, 2.30] |
| 9.2 12 months | 7 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.81, 3.57] |
| 9.3 24 months | 6 | 338 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [1.07, 3.94] |
| 10 Dentin bridge formation Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.10  Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 10 Dentin bridge formation. | ||||
| 10.1 6 months | 3 | 322 | Risk Ratio (M‐H, Fixed, 95% CI) | 18.16 [3.63, 90.91] |
| 10.2 12 months | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.76, 47.22] |
| 10.3 24 months | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.76, 47.22] |
| 11 Physiological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.11 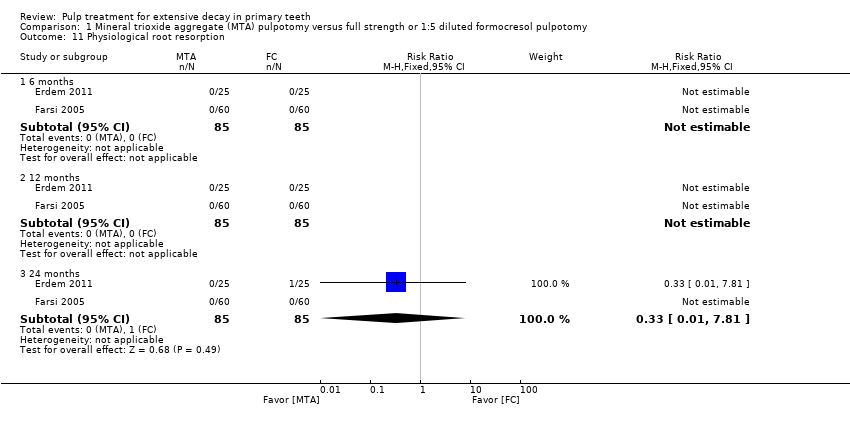 Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 11 Physiological root resorption. | ||||
| 11.1 6 months | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 12 months | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 24 months | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.81] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1 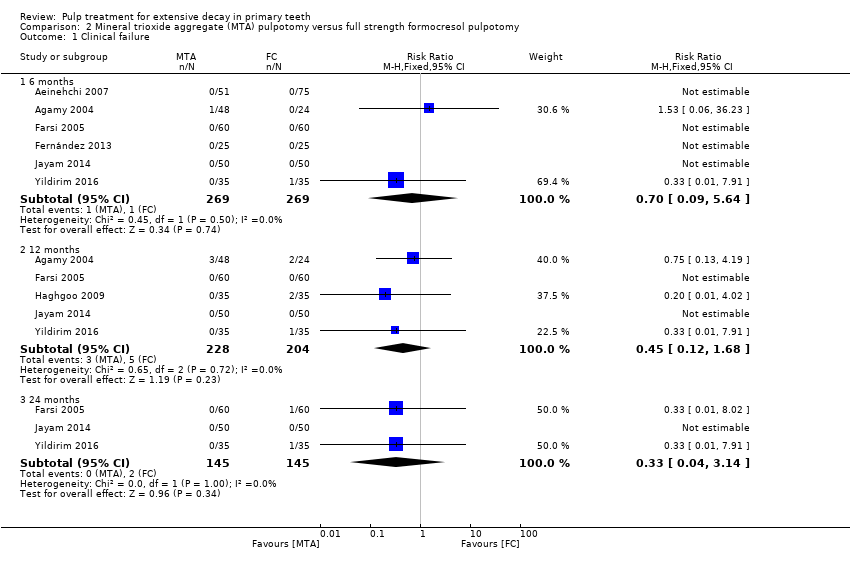 Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 6 | 538 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.09, 5.64] |
| 1.2 12 months | 5 | 432 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.12, 1.68] |
| 1.3 24 months | 3 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.14] |
| 2 Radiological failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 4 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.05, 1.79] |
| 2.2 12 months | 5 | 432 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.08, 0.98] |
| 2.3 24 months | 3 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.06, 0.67] |
| 3 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 3.2 12 months | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.18] |
| 3.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.14] |
| 4 Soft tissue pathology Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.4 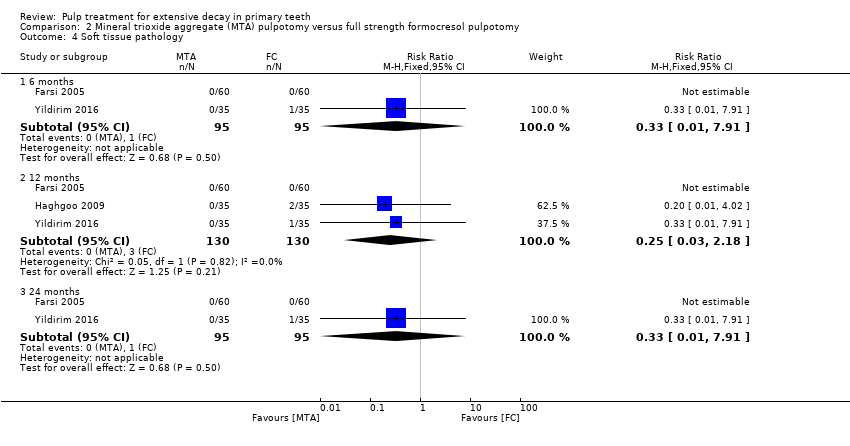 Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 4.2 12 months | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.18] |
| 4.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5 Pathological radiolucency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 5 Pathological radiolucency. | ||||
| 5.1 6 months | 4 | 388 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 2.95] |
| 5.2 12 months | 4 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.16, 2.38] |
| 5.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.11, 1.95] |
| 6 Pathological root resorption Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.6 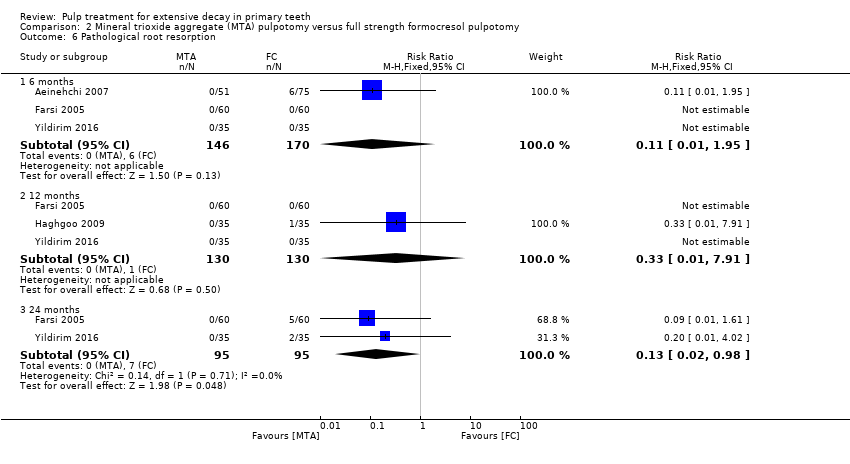 Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 6 Pathological root resorption. | ||||
| 6.1 6 months | 3 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 1.95] |
| 6.2 12 months | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 6.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.02, 0.98] |
| 7 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 7 Pulp canal obliteration. | ||||
| 7.1 6 months | 2 | 192 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 12 months | 2 | 192 | Risk Ratio (M‐H, Fixed, 95% CI) | 12.76 [0.79, 206.70] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1 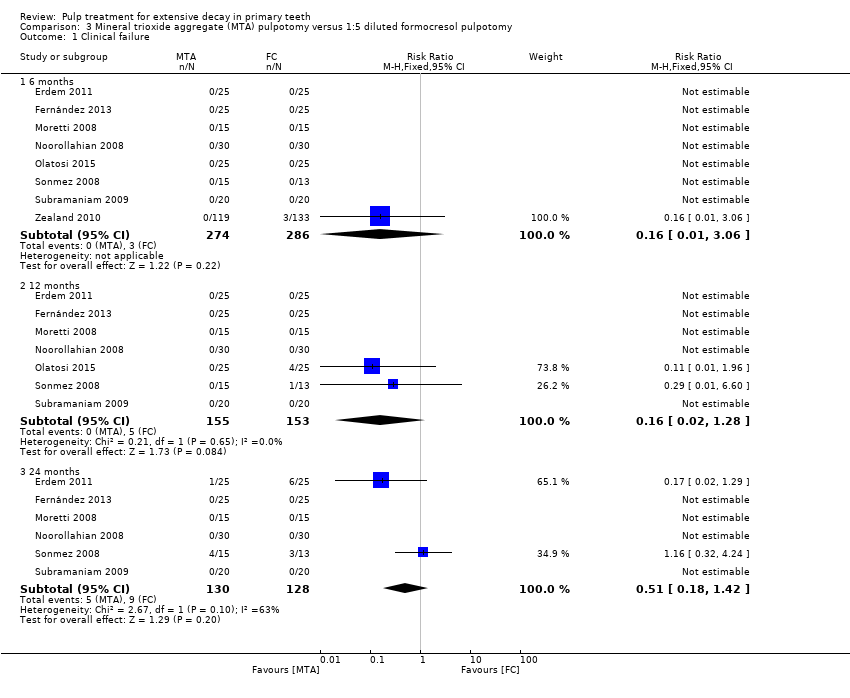 Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 8 | 560 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 3.06] |
| 1.2 12 months | 7 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.28] |
| 1.3 24 months | 6 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.18, 1.42] |
| 2 Radiological failure Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 8 | 560 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.17, 1.03] |
| 2.2 12 months | 7 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.20, 1.53] |
| 2.3 24 months | 6 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.31, 1.46] |
| 3 Pain Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.3  Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 24 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.30] |
| 4 Soft tissue pathology Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.4 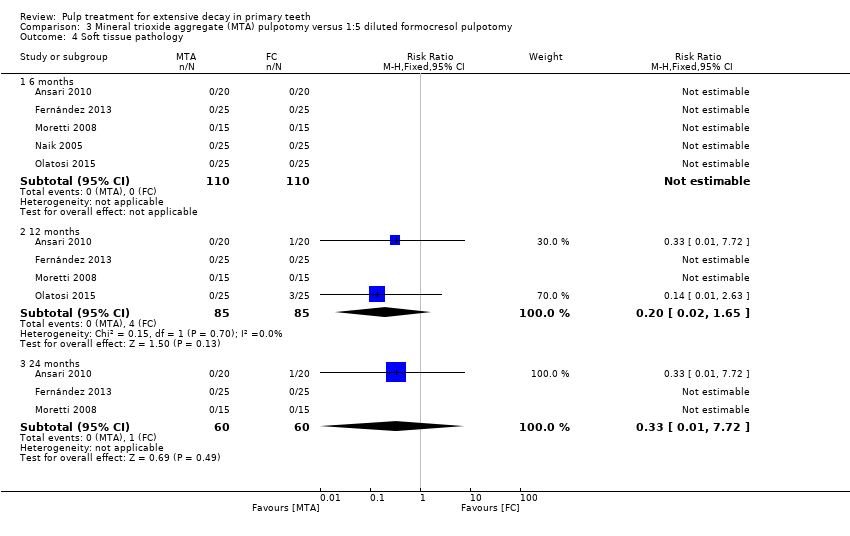 Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 5 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 4 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.65] |
| 4.3 24 months | 3 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.72] |
| 5 Pathological mobility Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.5 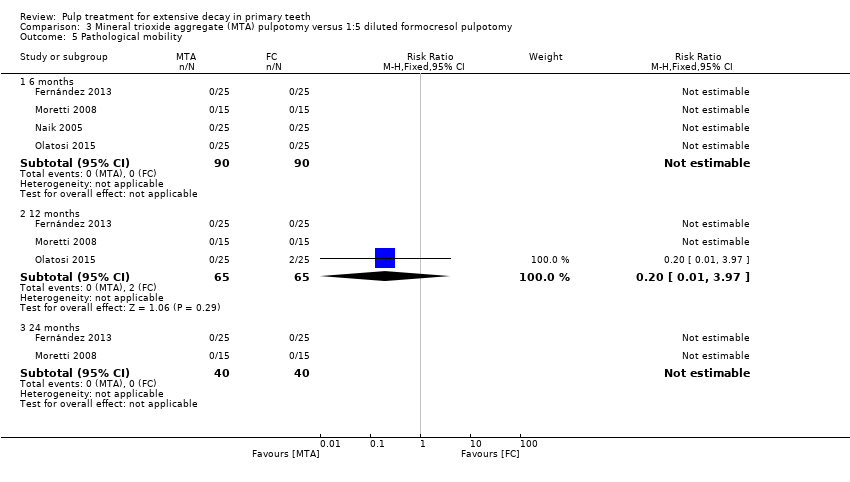 Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 5 Pathological mobility. | ||||
| 5.1 6 months | 4 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 5.3 24 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathological radiolucency Show forest plot | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.6  Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 6 Pathological radiolucency. | ||||
| 6.1 6 months | 9 | 622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.30, 1.27] |
| 6.2 12 months | 7 | 320 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.13, 1.02] |
| 6.3 24 months | 6 | 270 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.23, 1.57] |
| 7 Pathological root resorption Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.7  Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 7 Pathological root resorption. | ||||
| 7.1 6 months | 8 | 550 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.24, 1.99] |
| 7.2 12 months | 6 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.05, 1.14] |
| 7.3 24 months | 4 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.10, 1.92] |
| 8 Pulp canal obliteration Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.8  Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 8 Pulp canal obliteration. | ||||
| 8.1 6 months | 7 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.00, 2.30] |
| 8.2 12 months | 5 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.44, 2.26] |
| 8.3 24 months | 5 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [0.99, 3.89] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1 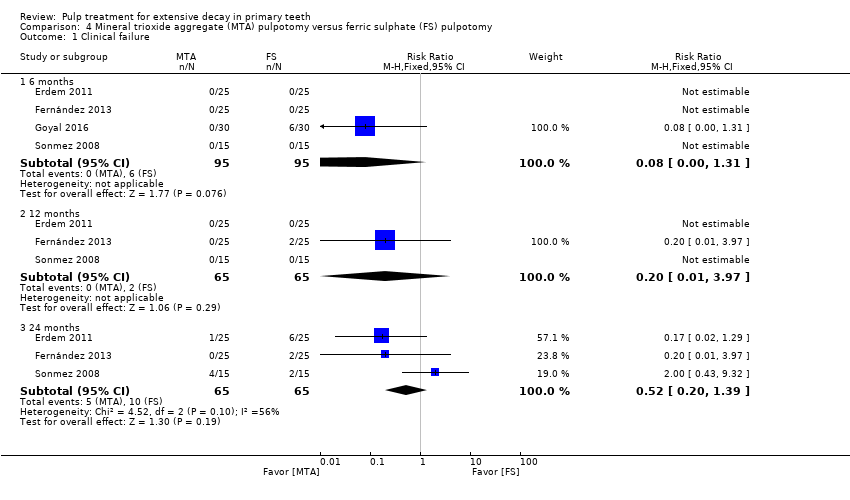 Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.31] |
| 1.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 1.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.20, 1.39] |
| 2 Radiological failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2 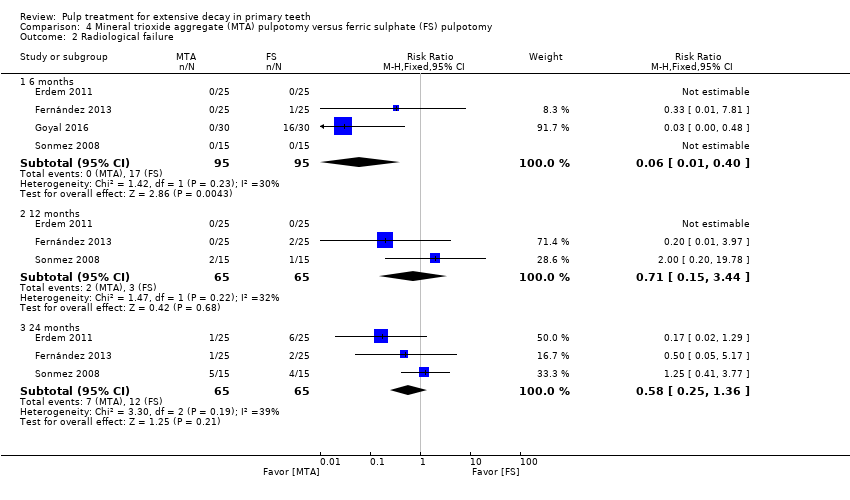 Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.40] |
| 2.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.15, 3.44] |
| 2.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.25, 1.36] |
| 3 Overall failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3 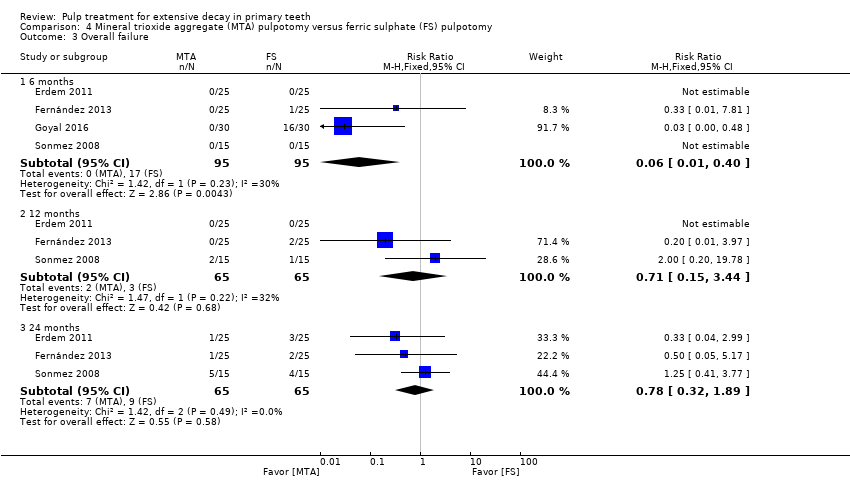 Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 3 Overall failure. | ||||
| 3.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.40] |
| 3.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.15, 3.44] |
| 3.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.32, 1.89] |
| 4 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.4  Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 4 Pain. | ||||
| 4.1 6 months | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.00] |
| 4.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 5 Soft tissue pathology. | ||||
| 5.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.00] |
| 6 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.6  Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 6 Pathologic mobility. | ||||
| 6.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.31] |
| 7 Pathologic radiolucency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.7  Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 7 Pathologic radiolucency. | ||||
| 7.1 6 months | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.48] |
| 7.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.81] |
| 7.3 24 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 8 Pathological root resorption Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.8  Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 8 Pathological root resorption. | ||||
| 8.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.01, 0.53] |
| 8.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 8.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.12, 2.51] |
| 9 Pulp canal obliteration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.9  Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 9 Pulp canal obliteration. | ||||
| 9.1 6 months | 3 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 12 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.30] |
| 9.3 24 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.47, 5.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.85] |
| 1.2 12 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.04, 0.70] |
| 1.3 24 months | 5 | 284 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.12, 0.52] |
| 2 Radiological failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.2  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.02, 0.41] |
| 2.2 12 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.04, 0.36] |
| 2.3 24 months | 5 | 284 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.08, 0.26] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.3  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 3 Overall failure. | ||||
| 3.1 6 months | 2 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.92] |
| 3.2 12 months | 2 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.10, 1.19] |
| 3.3 24 months | 2 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 0.95] |
| 4 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.4  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 4 Pain. | ||||
| 4.1 24 months | 2 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.09, 1.73] |
| 5 Soft tissue pathology Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.5  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 5 Soft tissue pathology. | ||||
| 5.1 6 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.62] |
| 5.2 12 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.62] |
| 5.3 24 months | 4 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.06, 0.47] |
| 6 Pathological mobility Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.6 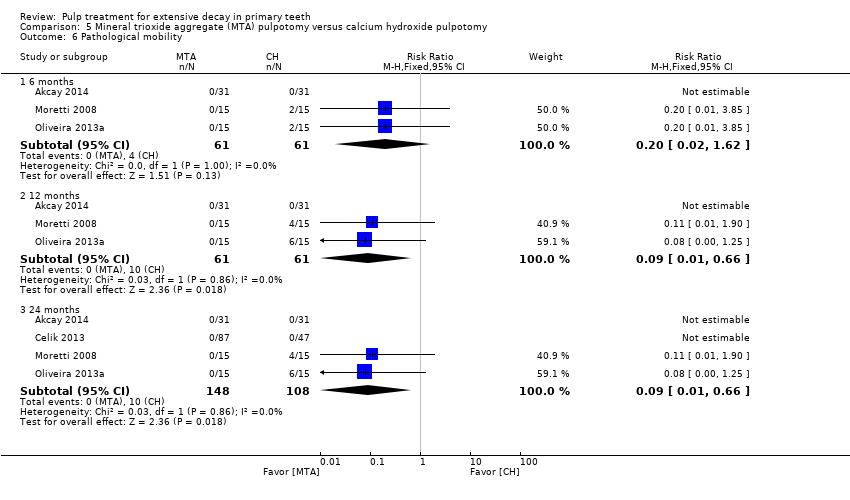 Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 6 Pathological mobility. | ||||
| 6.1 6 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.62] |
| 6.2 12 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 0.66] |
| 6.3 24 months | 4 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 0.66] |
| 7 Pathological radiolucency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.7  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 7 Pathological radiolucency. | ||||
| 7.1 6 months | 4 | 162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.02, 0.50] |
| 7.2 12 months | 4 | 162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.04, 0.47] |
| 7.3 24 months | 5 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.03, 0.22] |
| 8 Pathological root resorption Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.8  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 8 Pathological root resorption. | ||||
| 8.1 6 months | 5 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.02, 0.39] |
| 8.2 12 months | 5 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.02, 0.29] |
| 8.3 24 months | 6 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.03, 0.18] |
| 9 Pulp canal obliteration Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.9  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 9 Pulp canal obliteration. | ||||
| 9.1 6 months | 3 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.77 [1.56, 38.69] |
| 9.2 12 months | 3 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.01 [0.97, 4.17] |
| 9.3 24 months | 4 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [1.01, 4.19] |
| 10 Dentin bridge formation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.10  Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 10 Dentin bridge formation. | ||||
| 10.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.05, 0.84] |
| 10.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.37, 1.74] |
| 10.3 24 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.37, 1.74] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.1  Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 1.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 1.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 2 Radiological failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.2  Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.10, 2.56] |
| 3 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.3  Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 3.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 3.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 4 Soft tissue pathology Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.4  Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 4.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 4.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 5 Pathologic mobility Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.5  Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 5 Pathologic mobility. | ||||
| 5.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 6 Pathological radiolucency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.6  Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 6 Pathological radiolucency. | ||||
| 6.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.75] |
| 7 Pathological root resorption Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.7 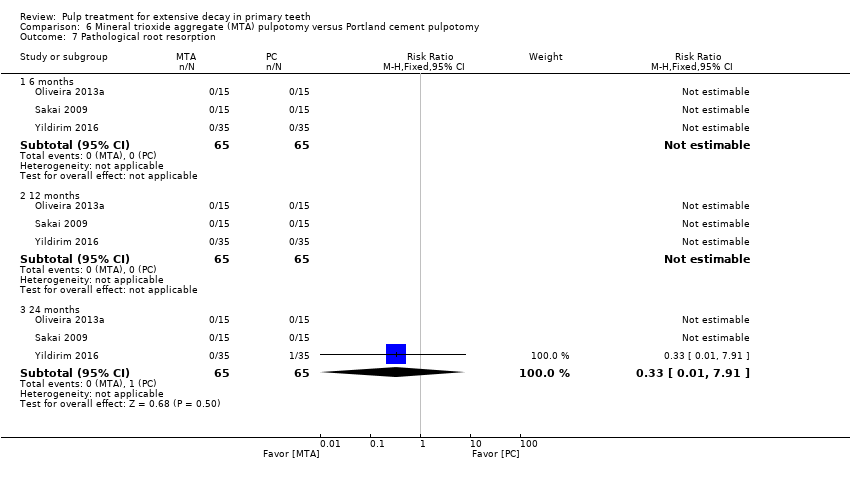 Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 7 Pathological root resorption. | ||||
| 7.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 8 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.8 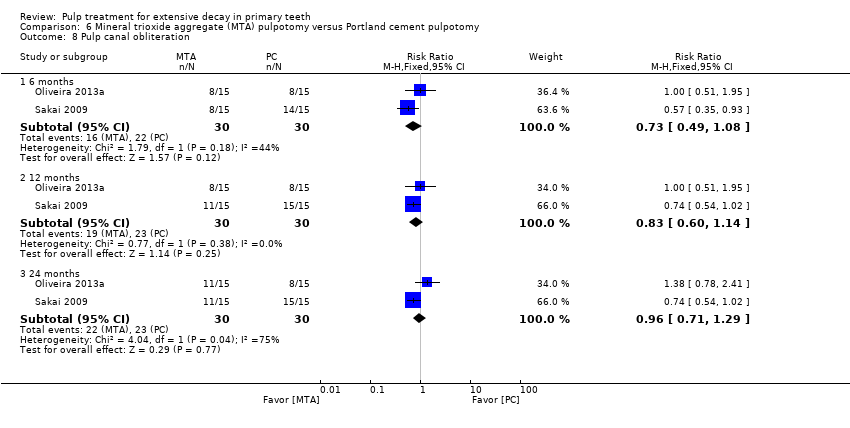 Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 8 Pulp canal obliteration. | ||||
| 8.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.49, 1.08] |
| 8.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.60, 1.14] |
| 8.3 24 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.71, 1.29] |
| 9 Dentin bridge formation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.9 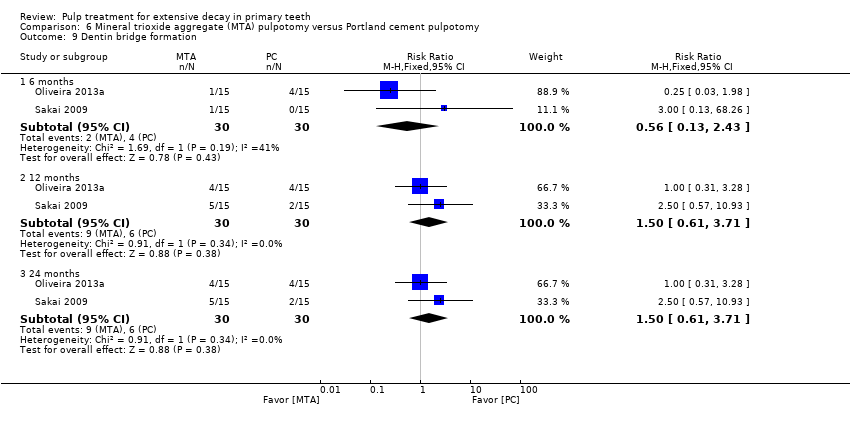 Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 9 Dentin bridge formation. | ||||
| 9.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.43] |
| 9.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.61, 3.71] |
| 9.3 24 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.61, 3.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.1  Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 4 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.42, 6.99] |
| 1.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.16, 3.62] |
| 2 Radiological failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.2  Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 4 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.40 [0.65, 8.84] |
| 2.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.22, 5.27] |
| 3 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.3  Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 98.00] |
| 4 Soft tissue pathology Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.4  Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 98.00] |
| 5 Pathologic mobility Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.5  Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 5 Pathologic mobility. | ||||
| 5.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 98.00] |
| 6 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.6 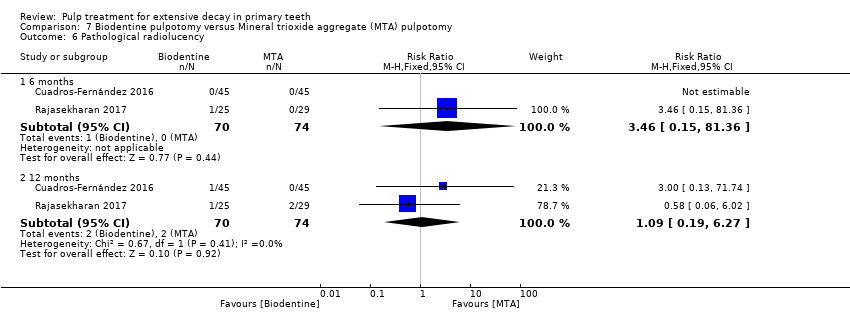 Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 6 Pathological radiolucency. | ||||
| 6.1 6 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.46 [0.15, 81.36] |
| 6.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.19, 6.27] |
| 7 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.7  Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 7 Pathological root resorption. | ||||
| 7.1 6 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.32 [0.22, 24.09] |
| 7.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.30, 4.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.1  Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.98 [1.17, 3.37] |
| 1.2 12 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.87 [1.22, 2.89] |
| 1.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [0.78, 6.11] |
| 2 Radiological failure Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.2  Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 4 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.48 [3.86, 62.06] |
| 2.2 12 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [1.42, 2.44] |
| 2.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.63 [1.73, 7.61] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.3 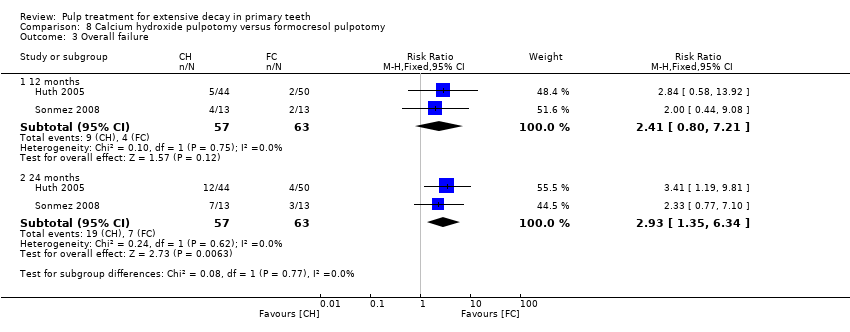 Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 3 Overall failure. | ||||
| 3.1 12 months | 2 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.41 [0.80, 7.21] |
| 3.2 24 months | 2 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.93 [1.35, 6.34] |
| 4 Pain Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.4 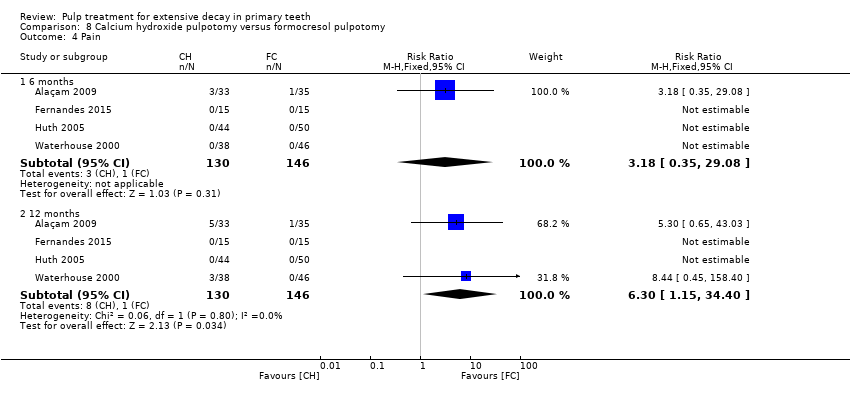 Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 4 Pain. | ||||
| 4.1 6 months | 4 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.18 [0.35, 29.08] |
| 4.2 12 months | 4 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.30 [1.15, 34.40] |
| 5 Soft tissue pathology Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.5  Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 5 Soft tissue pathology. | ||||
| 5.1 6 months | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.14 [0.63, 42.25] |
| 5.2 12 months | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.77 [1.23, 37.10] |
| 5.3 24 months | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.64 [0.51, 13.55] |
| 6 Pathological mobility Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.6 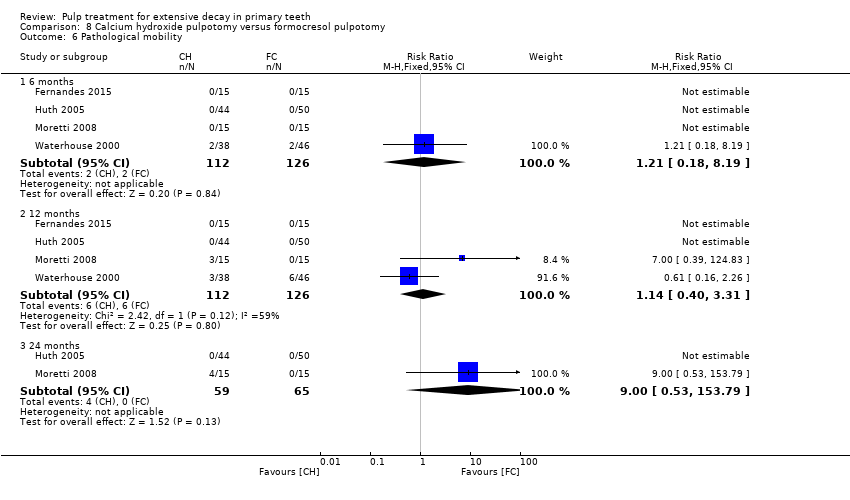 Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 6 Pathological mobility. | ||||
| 6.1 6 months | 4 | 238 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.18, 8.19] |
| 6.2 12 months | 4 | 238 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.40, 3.31] |
| 6.3 24 months | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.0 [0.53, 153.79] |
| 7 Pathological radiolucency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.7  Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 7 Pathological radiolucency. | ||||
| 7.1 6 months | 3 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.78 [0.64, 22.17] |
| 7.2 12 months | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [0.67, 5.40] |
| 7.3 24 months | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.79, 13.28] |
| 8 Pathological root resorption Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.8  Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 8 Pathological root resorption. | ||||
| 8.1 6 months | 4 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.87 [2.33, 60.40] |
| 8.2 12 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.25 [2.04, 19.14] |
| 8.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.59 [1.33, 15.81] |
| 9 Pulp canal obliteration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.9 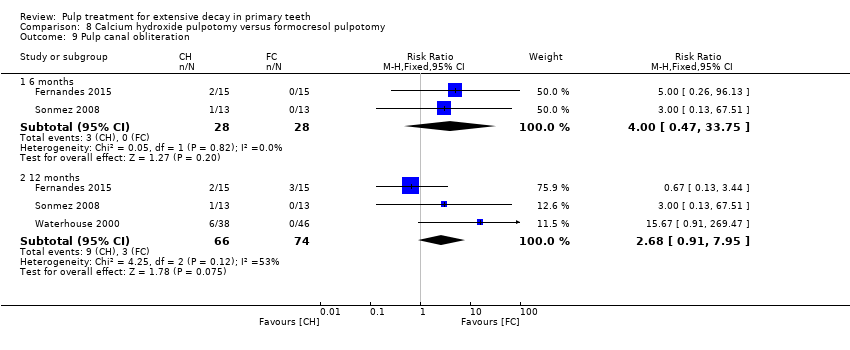 Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 9 Pulp canal obliteration. | ||||
| 9.1 6 months | 2 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.0 [0.47, 33.75] |
| 9.2 12 months | 3 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.68 [0.91, 7.95] |
| 10 Dentin bridge formation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 8.10  Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 10 Dentin bridge formation. | ||||
| 10.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 13.0 [1.81, 93.60] |
| 10.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 14.0 [1.95, 100.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 9.1  Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.4 [0.14, 81.38] |
| 1.2 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.41 [0.37, 31.61] |
| 1.3 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.44 [0.90, 13.18] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 9.2  Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.53, 3.13] |
| 2.2 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [1.04, 3.75] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 9.3 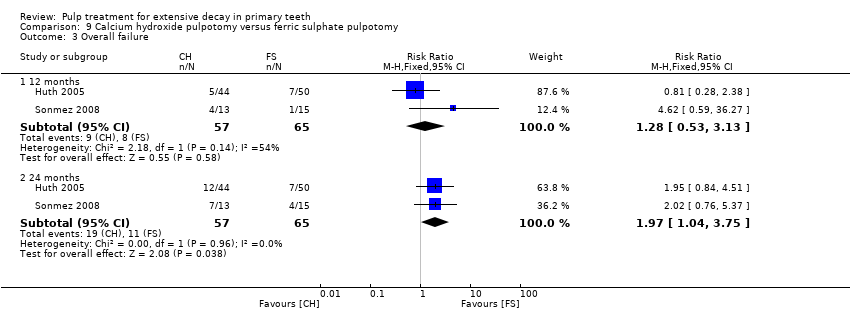 Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 3 Overall failure. | ||||
| 3.1 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.53, 3.13] |
| 3.2 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [1.04, 3.75] |
| 4 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 9.4  Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 4 Pathological root resorption. | ||||
| 4.1 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.05, 6.05] |
| 4.2 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [0.60, 8.66] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.1  Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 7 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.87] |
| 1.2 12 months | 7 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.45, 4.27] |
| 1.3 24 months | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.40, 1.70] |
| 2 Radiological failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.2 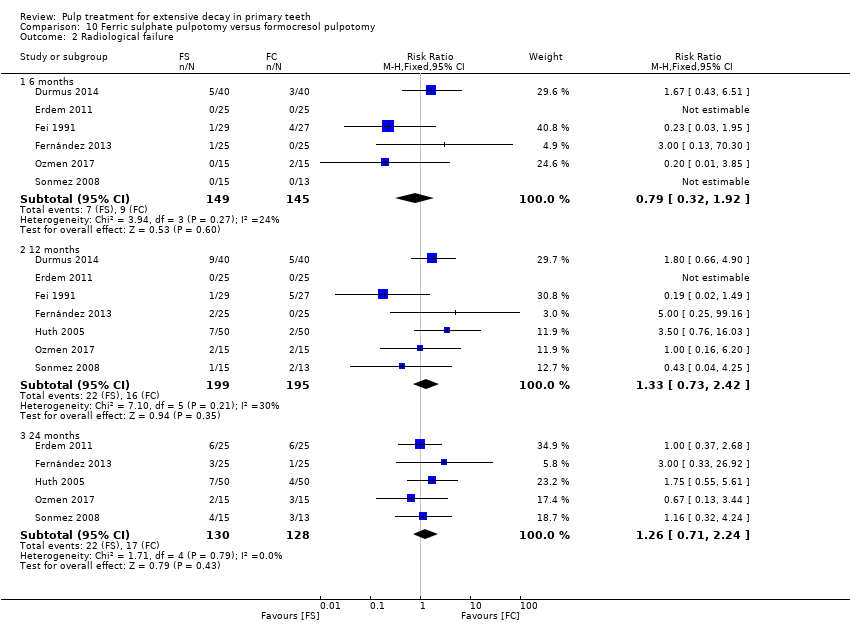 Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 6 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.32, 1.92] |
| 2.2 12 months | 7 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.73, 2.42] |
| 2.3 24 months | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.71, 2.24] |
| 3 Overall failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.3 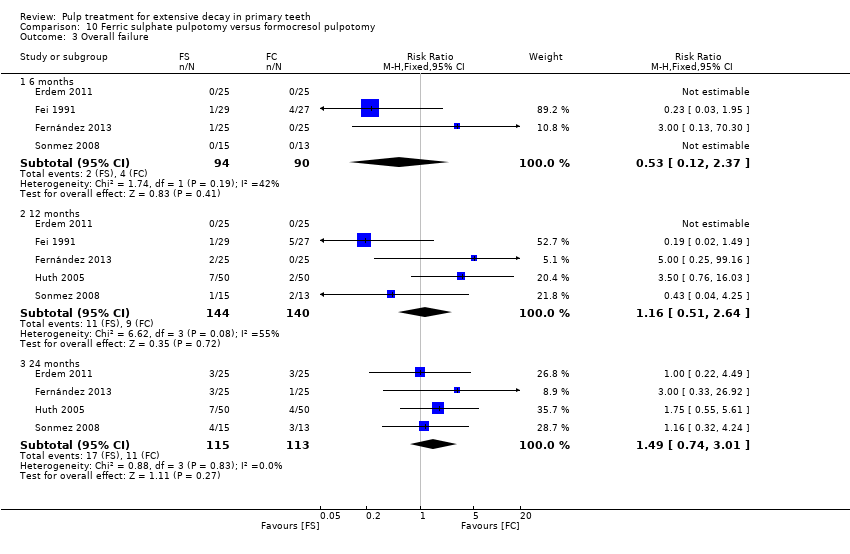 Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 3 Overall failure. | ||||
| 3.1 6 months | 4 | 184 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.12, 2.37] |
| 3.2 12 months | 5 | 284 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.51, 2.64] |
| 3.3 24 months | 4 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.74, 3.01] |
| 4 Pain Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.4 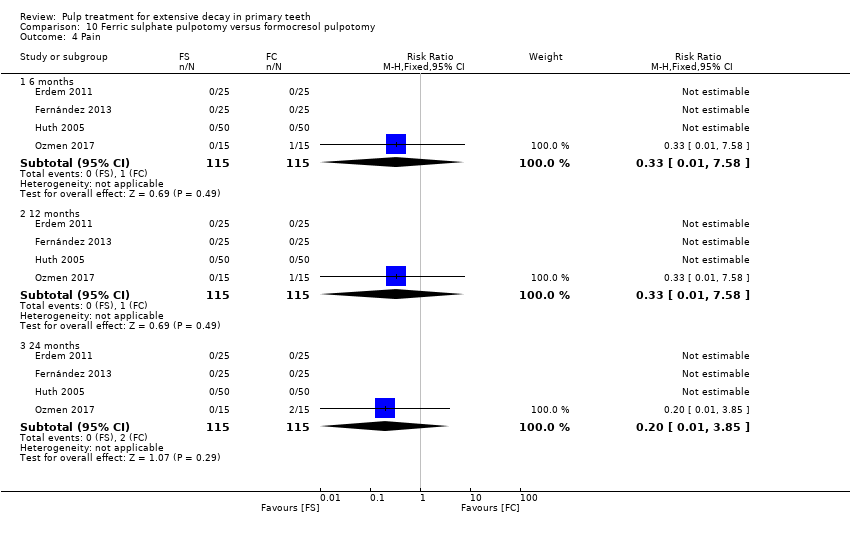 Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 4 Pain. | ||||
| 4.1 6 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 4.2 12 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 4.3 24 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.85] |
| 5 Pathological radiolucency Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.5  Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 5 Pathological radiolucency. | ||||
| 5.1 12 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.8 [0.40, 8.17] |
| 5.2 24 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.2 [0.51, 9.50] |
| 6 Pathological root resorption Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.6 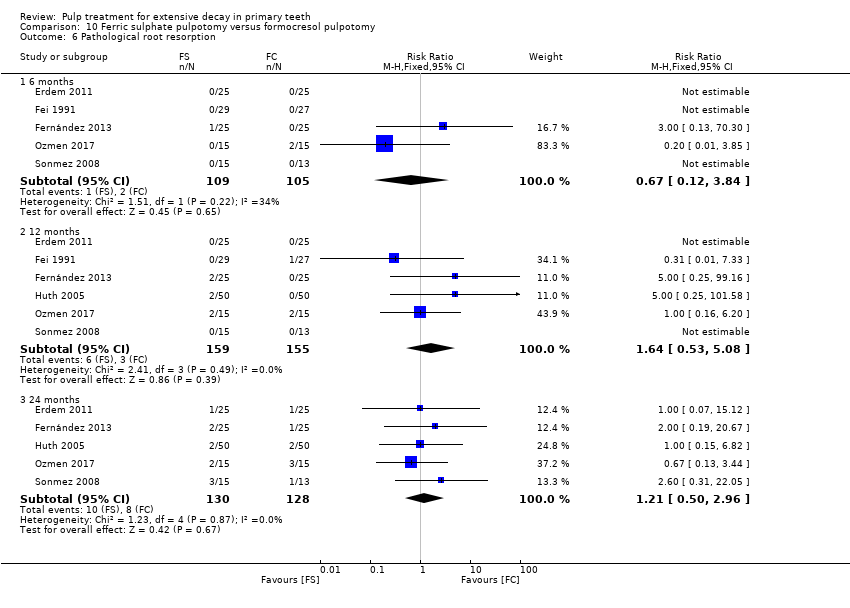 Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 6 Pathological root resorption. | ||||
| 6.1 6 months | 5 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.84] |
| 6.2 12 months | 6 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.53, 5.08] |
| 6.3 24 months | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.50, 2.96] |
| 7 Pulp canal obliteration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 10.7  Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 7 Pulp canal obliteration. | ||||
| 7.1 6 months | 3 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 12 months | 3 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.54, 1.64] |
| 7.3 24 months | 2 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.28, 5.54] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.1 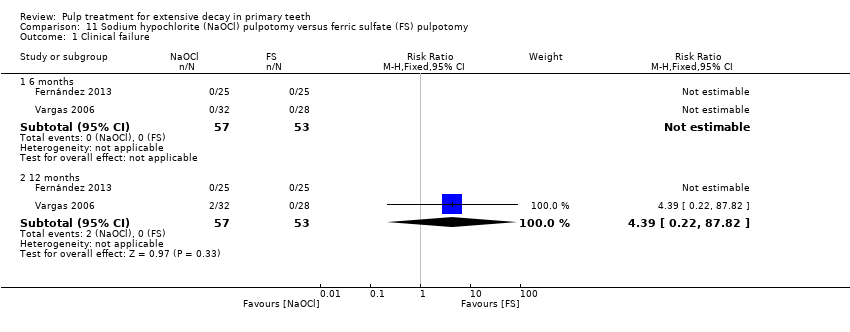 Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.39 [0.22, 87.82] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.2 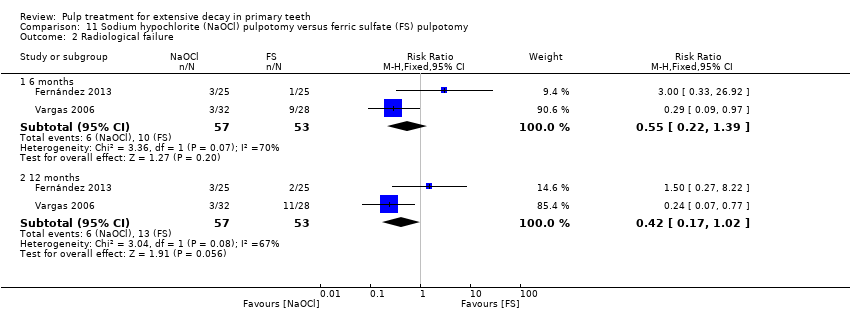 Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.22, 1.39] |
| 2.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.17, 1.02] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.3  Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.4  Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.01, 6.91] |
| 5 Adjacent tissue inflammation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.5 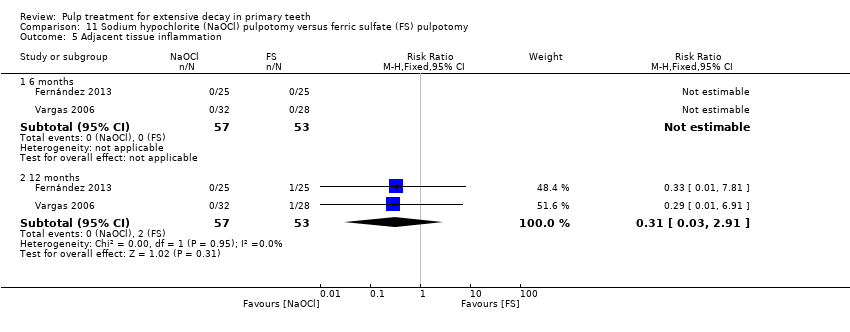 Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 5 Adjacent tissue inflammation. | ||||
| 5.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.03, 2.91] |
| 6 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.6  Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 6 Pathologic mobility. | ||||
| 6.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.7  Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 7 Pathologic radiolucency. | ||||
| 7.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.06, 13.35] |
| 7.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.07, 4.17] |
| 8 Pathologic root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 11.8  Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 8 Pathologic root resorption. | ||||
| 8.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.18, 1.42] |
| 8.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.15, 1.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 12.1  Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.04, 1.30] |
| 1.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.62] |
| 2 Radiological failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 12.2  Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.38, 2.12] |
| 2.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.44, 1.92] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 12.3 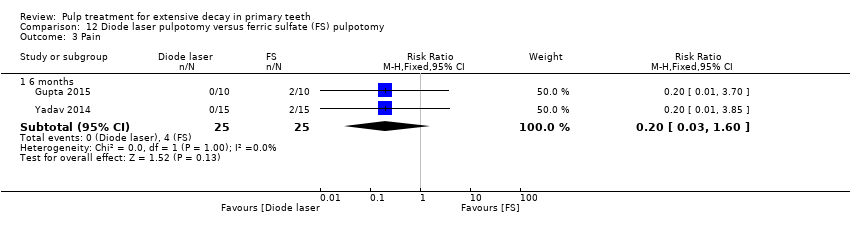 Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.60] |
| 4 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 12.4 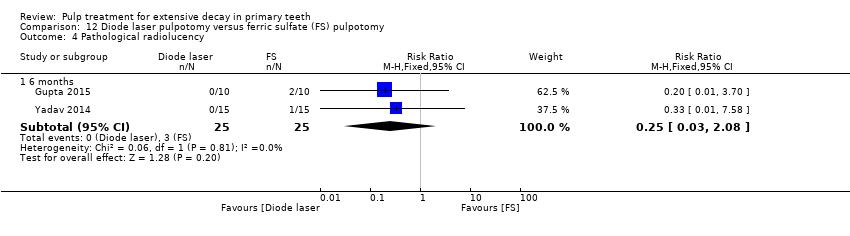 Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 4 Pathological radiolucency. | ||||
| 4.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.08] |
| 5 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 12.5  Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 5 Pathological root resorption. | ||||
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.29, 7.73] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 13.1  Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.34] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 13.2  Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.38, 4.12] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 13.3  Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.34] |
| 4 Pathological mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 13.4 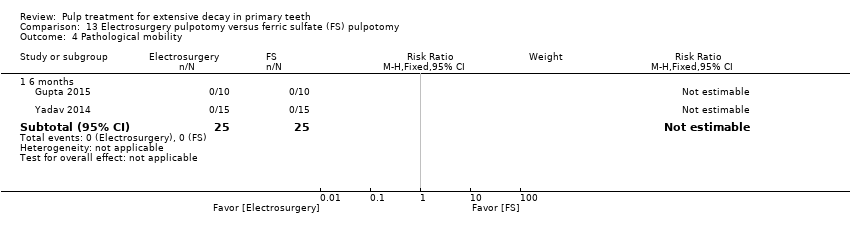 Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 4 Pathological mobility. | ||||
| 4.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 13.5  Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 5 Pathological root resorption. | ||||
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.2 [0.54, 8.88] |
| 6 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 13.6  Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 6 Pulp canal obliteration. | ||||
| 6.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.1 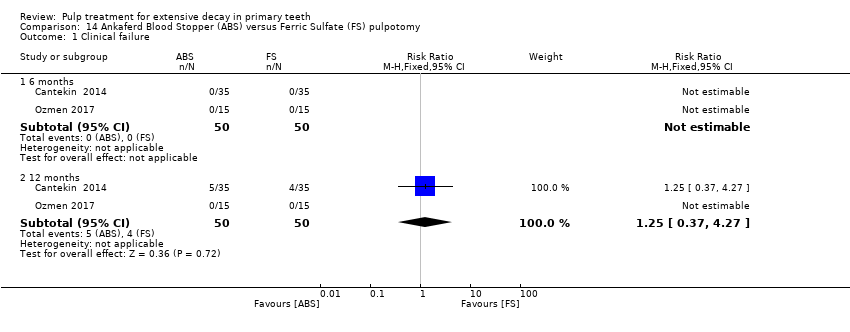 Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.37, 4.27] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.2  Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.16, 6.20] |
| 2.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.34, 2.23] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.3 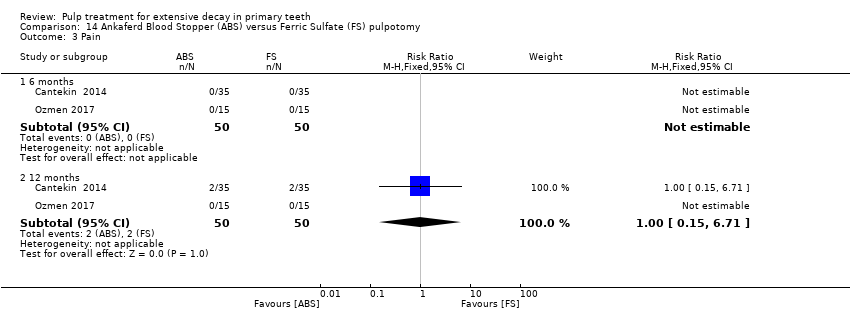 Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.71] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.4 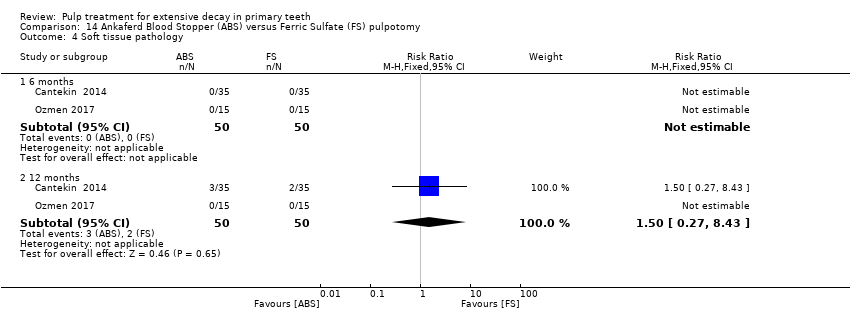 Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.27, 8.43] |
| 5 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.5 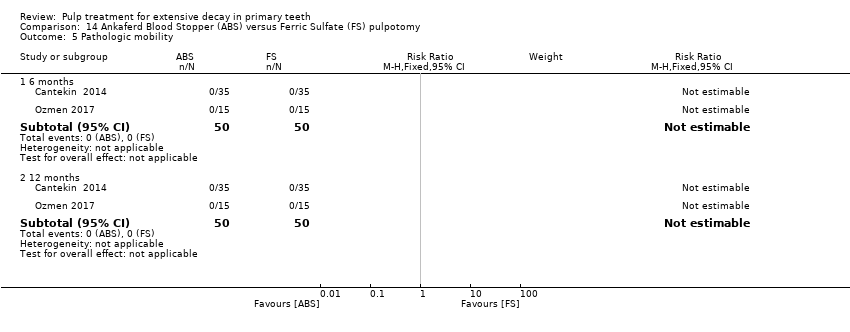 Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 5 Pathologic mobility. | ||||
| 5.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.6 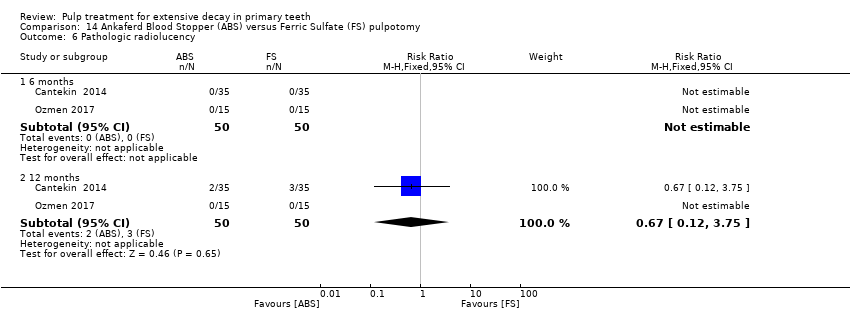 Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 6 Pathologic radiolucency. | ||||
| 6.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.75] |
| 7 Pathologic root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 14.7  Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 7 Pathologic root resorption. | ||||
| 7.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 96.13] |
| 7.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.1  Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.70] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.2 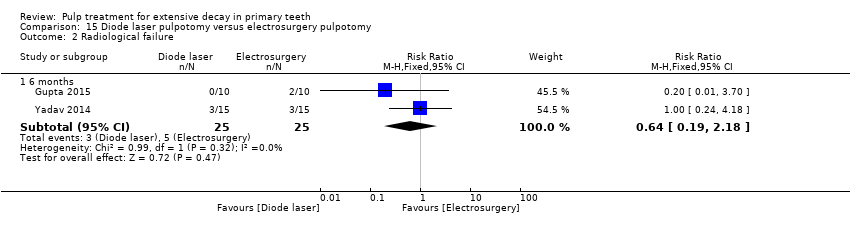 Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.19, 2.18] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.3  Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.70] |
| 4 Pathological mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.4  Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 4 Pathological mobility. | ||||
| 4.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.5  Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 5 Pathological radiolucency. | ||||
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.6  Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 6 Pathological root resorption. | ||||
| 6.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.19, 2.18] |
| 7 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 15.7  Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 7 Pulp canal obliteration. | ||||
| 7.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.1  Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.2 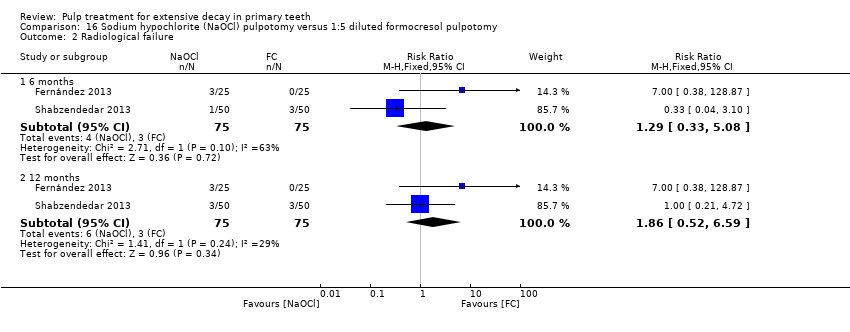 Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.33, 5.08] |
| 2.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [0.52, 6.59] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.3  Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.4  Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.5 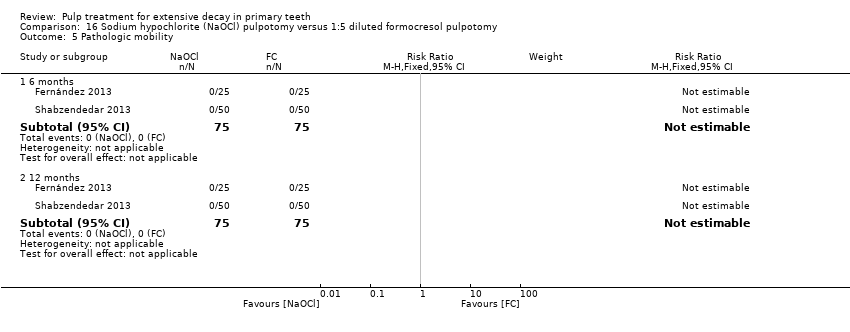 Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 5 Pathologic mobility. | ||||
| 5.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.6 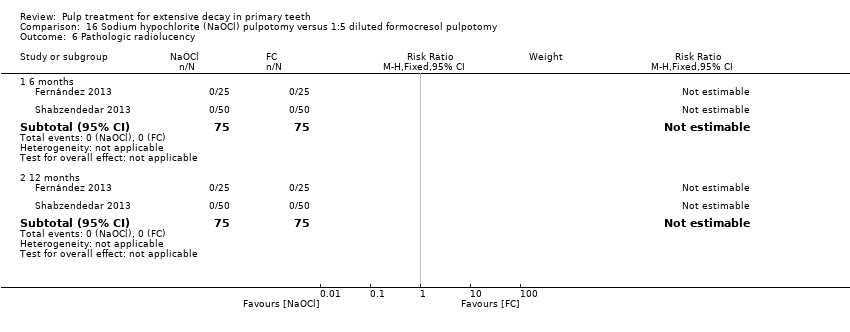 Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 6 Pathologic radiolucency. | ||||
| 6.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pathologic root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 16.7  Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 7 Pathologic root resorption. | ||||
| 7.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.33, 5.08] |
| 7.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [0.52, 6.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 17.1 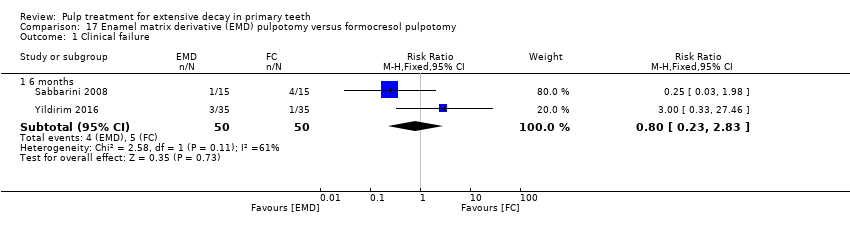 Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.23, 2.83] |
| 2 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 17.2 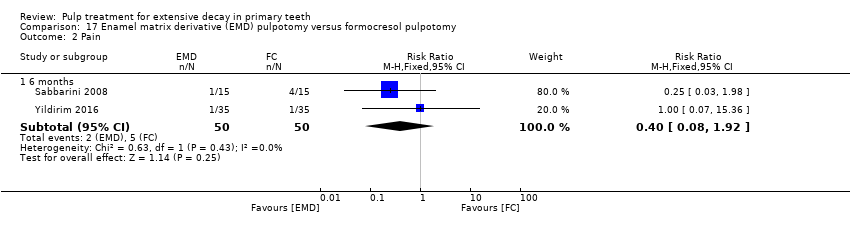 Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 2 Pain. | ||||
| 2.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.92] |
| 3 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 17.3  Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 3 Soft tissue pathology. | ||||
| 3.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.06] |
| 4 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 17.4  Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 4 Pathologic mobility. | ||||
| 4.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 96.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 18.1  Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 1 Radiological failure. | ||||
| 1.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.5 [0.50, 12.50] |
| 2 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 18.2 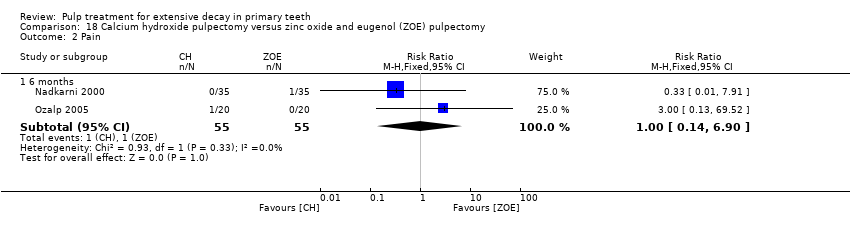 Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 2 Pain. | ||||
| 2.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 6.90] |
| 3 Pathological mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 18.3 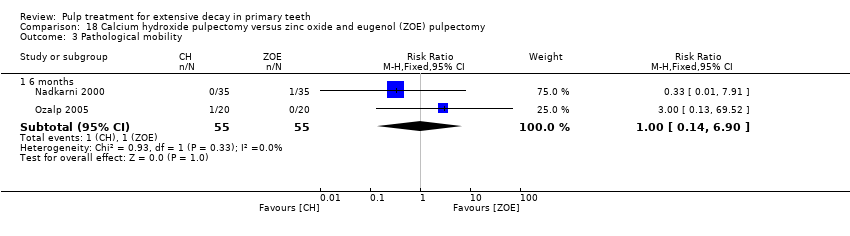 Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 3 Pathological mobility. | ||||
| 3.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 6.90] |
| 4 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 18.4  Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 4 Pathological radiolucency. | ||||
| 4.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.72] |
| 5 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 18.5  Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 5 Pathological radiolucency. | ||||
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 19.1 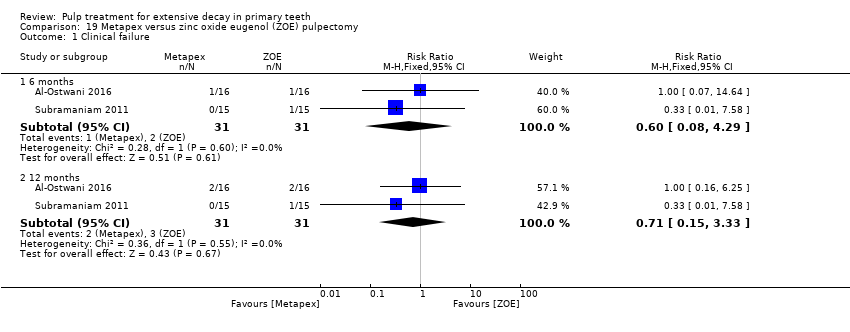 Comparison 19 Metapex versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.08, 4.29] |
| 1.2 12 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.15, 3.33] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 19.2 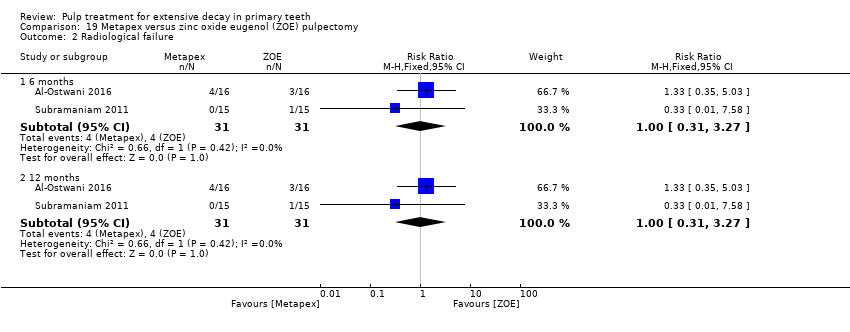 Comparison 19 Metapex versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.27] |
| 2.2 12 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clincal failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.1  Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 1 Clincal failure. | ||||
| 1.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.2  Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.79, 5.15] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.3  Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.4 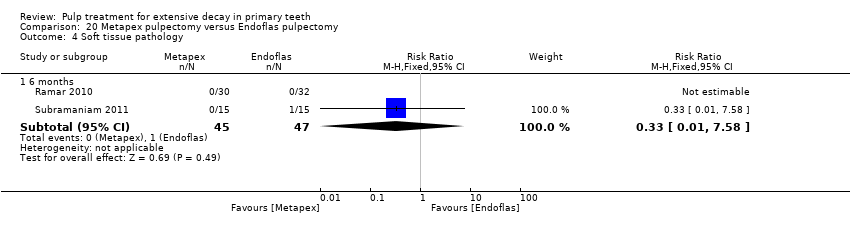 Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 4 Soft tissue pathology. | ||||
| 4.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 5 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.5  Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 5 Pathologic mobility. | ||||
| 5.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.6  Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 6 Pathological radiolucency. | ||||
| 6.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.79, 5.15] |
| 7 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 20.7  Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 7 Pathological root resorption. | ||||
| 7.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 21.1  Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.84] |
| 1.2 12 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.75 [1.21, 18.55] |
| 2 Radiological failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 21.2  Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.36 [0.86, 6.50] |
| 2.2 12 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.56 [2.58, 16.67] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 21.3 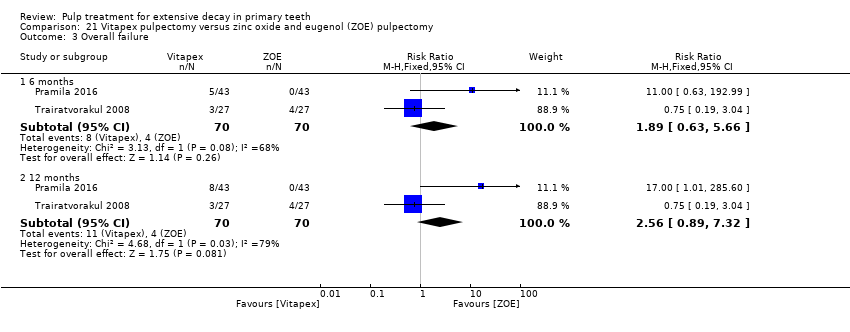 Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 3 Overall failure. | ||||
| 3.1 6 months | 2 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.63, 5.66] |
| 3.2 12 months | 2 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.56 [0.89, 7.32] |
| 4 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 21.4 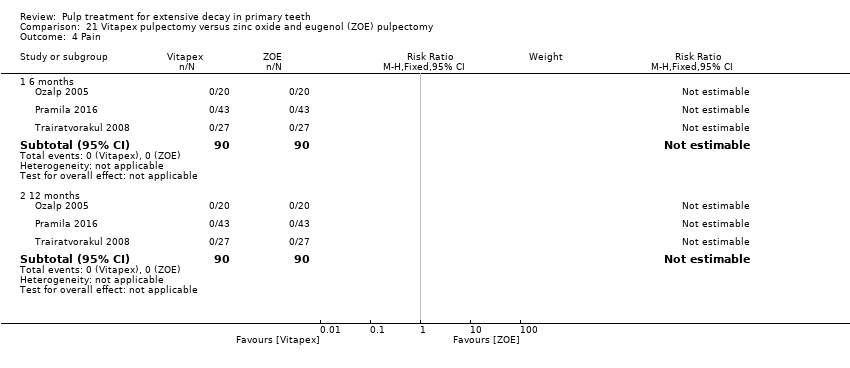 Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 4 Pain. | ||||
| 4.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathological mobility Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 21.5 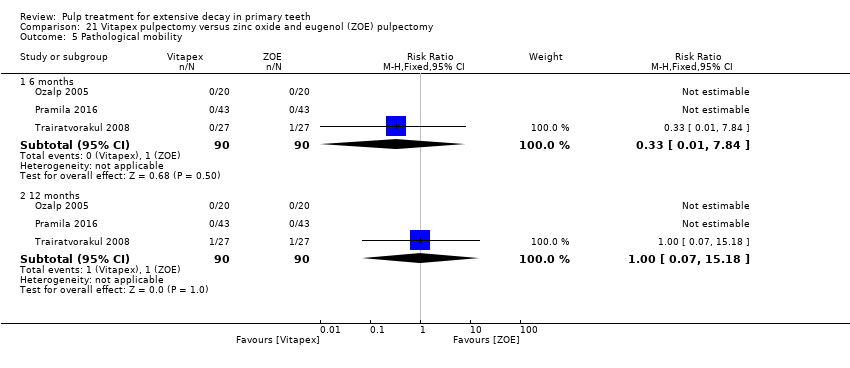 Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 5 Pathological mobility. | ||||
| 5.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.84] |
| 5.2 12 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 22.1  Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 1 Clinical failure. | ||||
| 1.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.05, 1.50] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 22.2 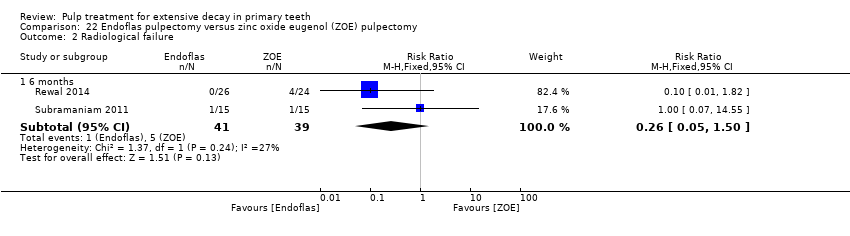 Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 2 Radiological failure. | ||||
| 2.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.05, 1.50] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 22.3 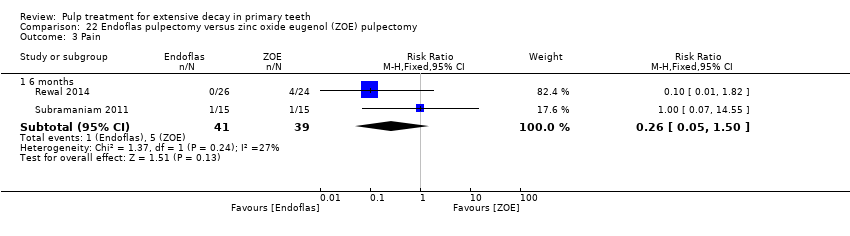 Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 3 Pain. | ||||
| 3.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.05, 1.50] |
| 4 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 22.4  Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 4 Pathologic mobility. | ||||
| 4.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.25] |
| 5 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 22.5  Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 5 Pathologic radiolucency. | ||||
| 5.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.11, 3.63] |

Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 1 Clinical failure.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 2 Radiological failure.
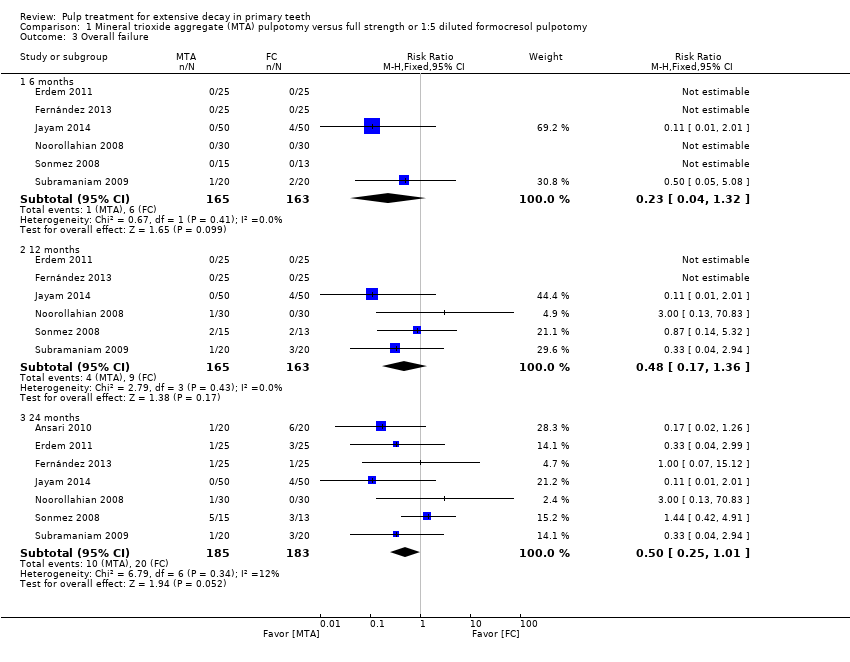
Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 3 Overall failure.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 4 Pain.
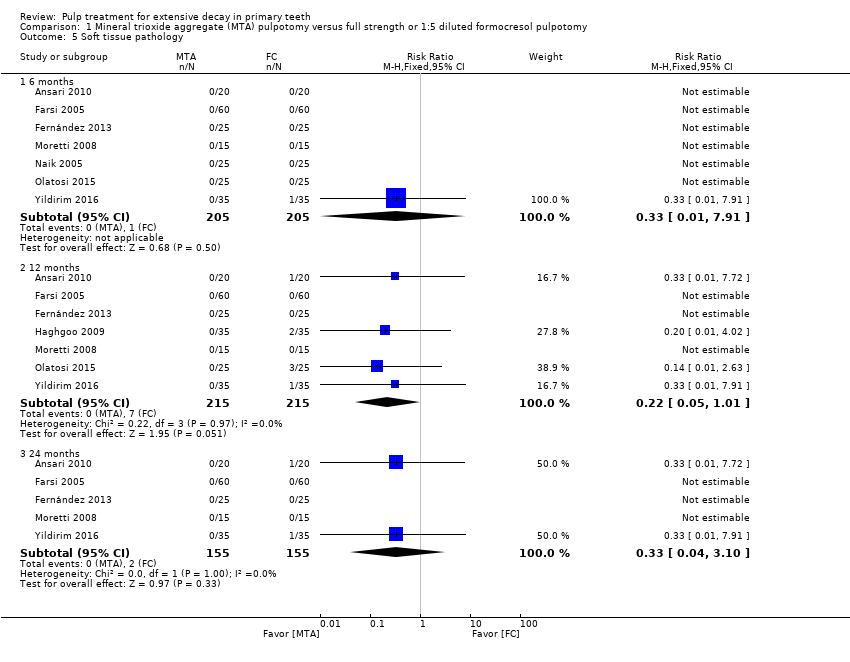
Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 5 Soft tissue pathology.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 6 Pathological mobility.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 7 Pathological radiolucency.
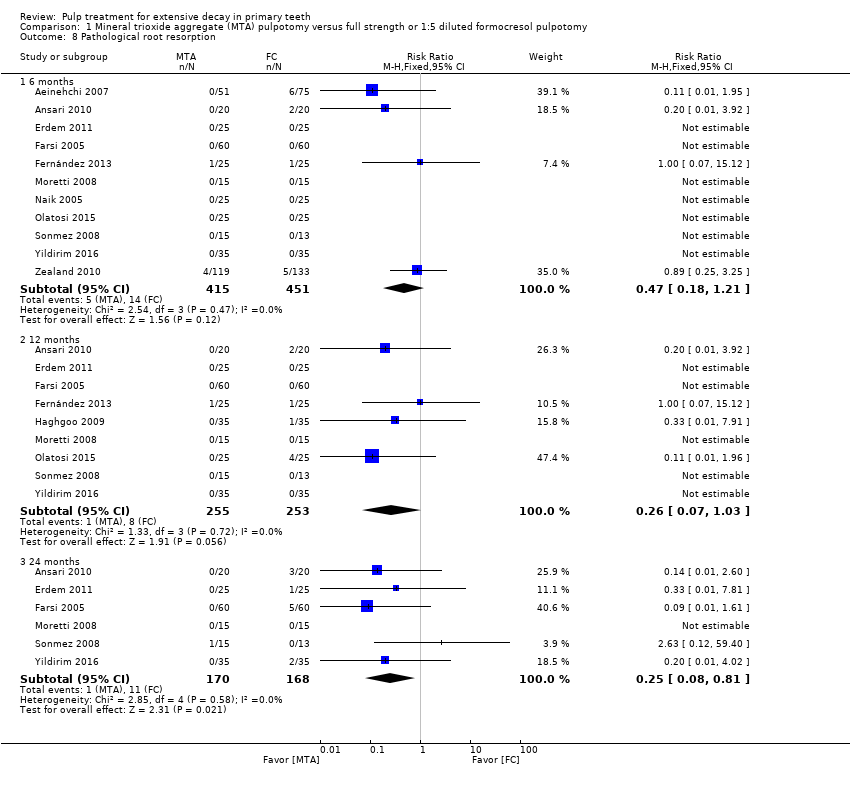
Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 8 Pathological root resorption.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 9 Pulp canal obliteration.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 10 Dentin bridge formation.

Comparison 1 Mineral trioxide aggregate (MTA) pulpotomy versus full strength or 1:5 diluted formocresol pulpotomy, Outcome 11 Physiological root resorption.

Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 1 Clinical failure.

Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 2 Radiological failure.
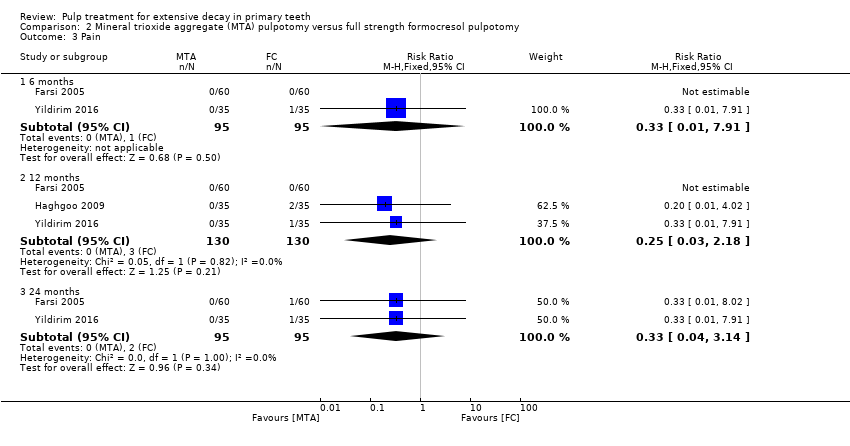
Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 3 Pain.

Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 4 Soft tissue pathology.
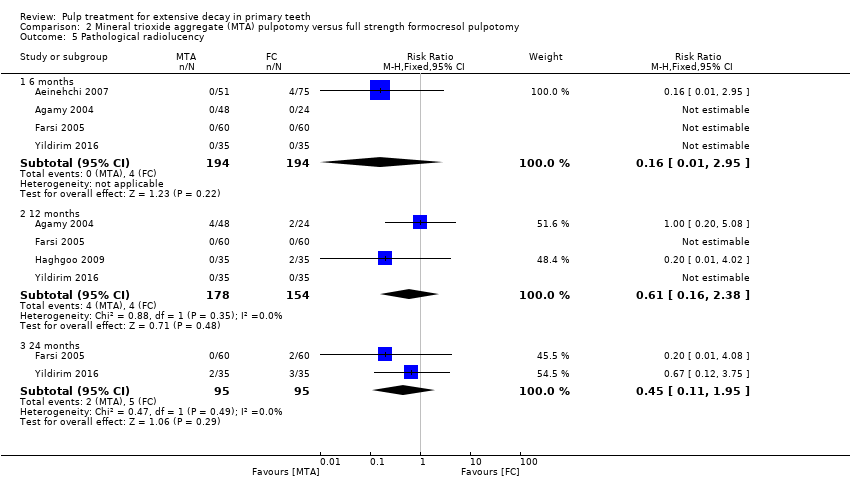
Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 5 Pathological radiolucency.

Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 6 Pathological root resorption.

Comparison 2 Mineral trioxide aggregate (MTA) pulpotomy versus full strength formocresol pulpotomy, Outcome 7 Pulp canal obliteration.

Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 1 Clinical failure.

Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 2 Radiological failure.

Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 3 Pain.
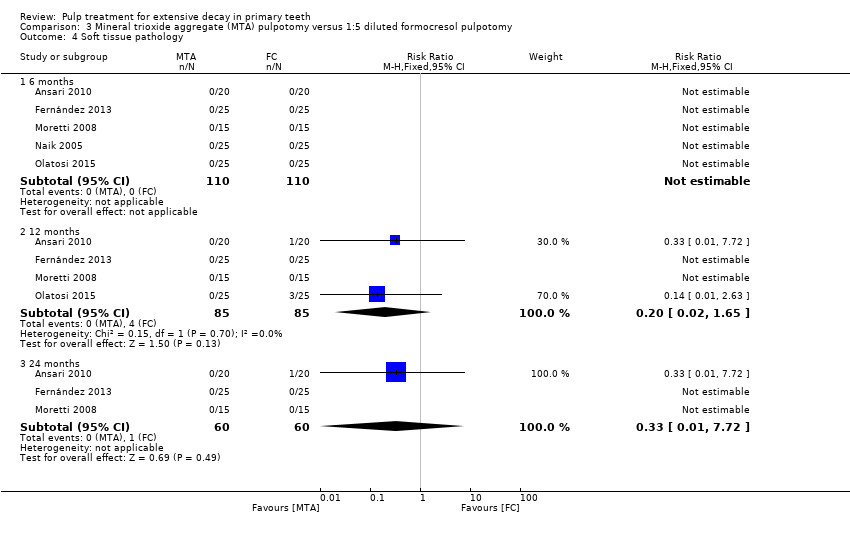
Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 4 Soft tissue pathology.

Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 5 Pathological mobility.

Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 6 Pathological radiolucency.
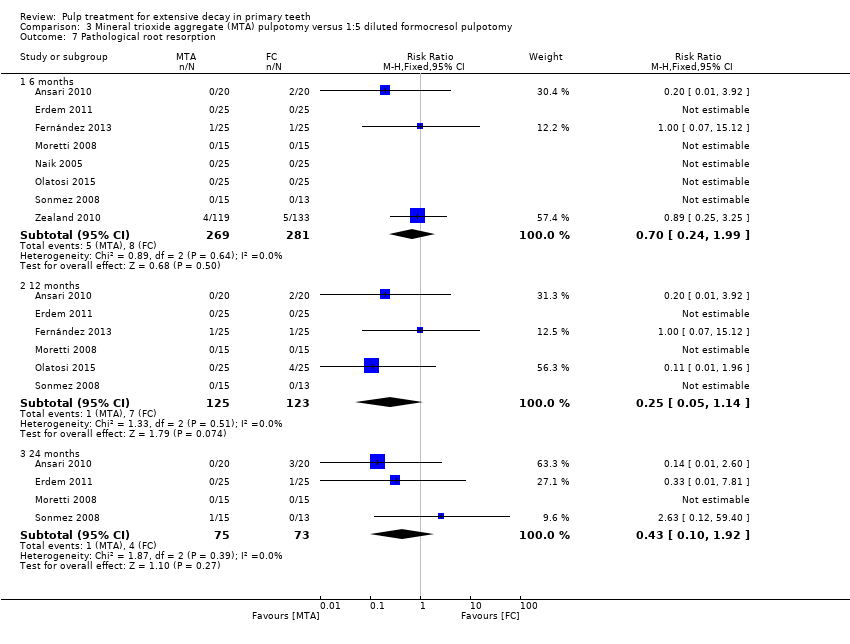
Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 7 Pathological root resorption.
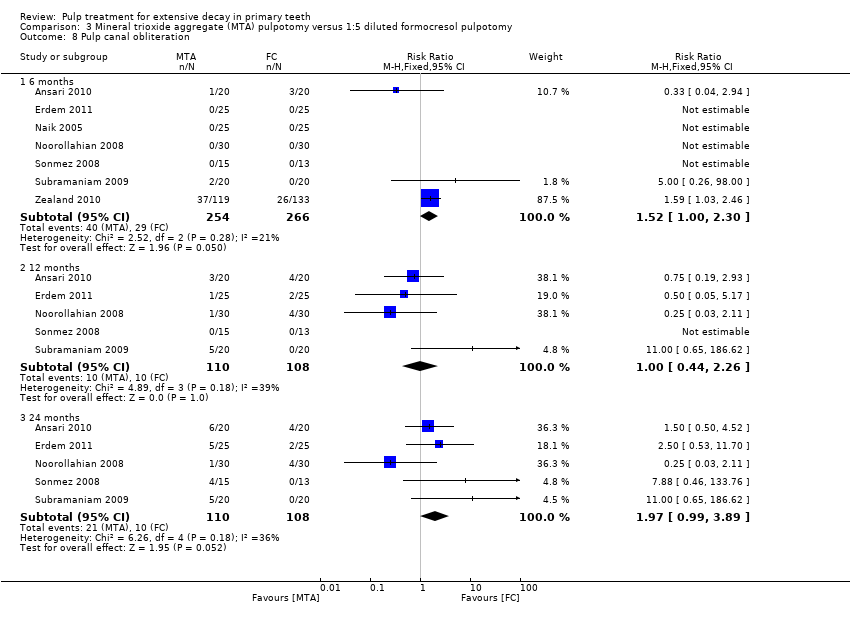
Comparison 3 Mineral trioxide aggregate (MTA) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 8 Pulp canal obliteration.

Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 1 Clinical failure.

Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 2 Radiological failure.

Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 3 Overall failure.
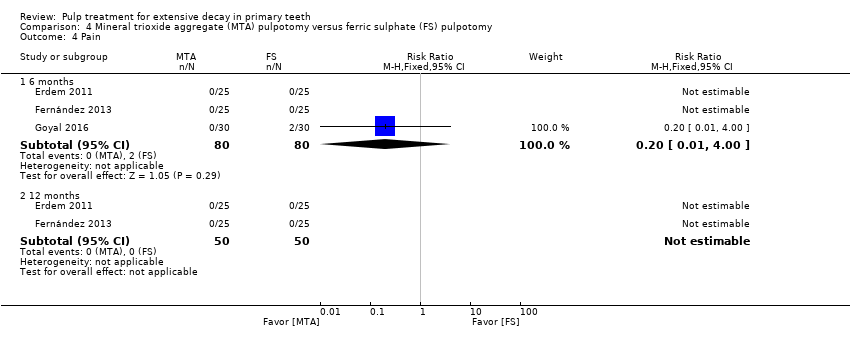
Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 4 Pain.
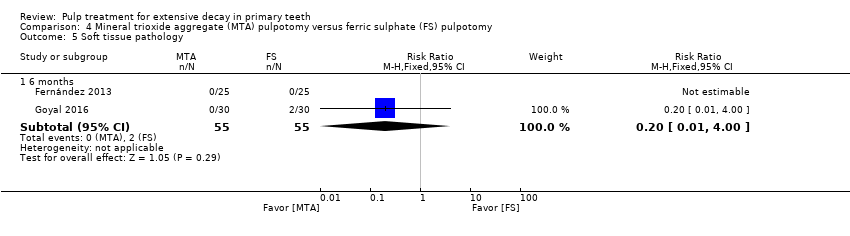
Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 5 Soft tissue pathology.
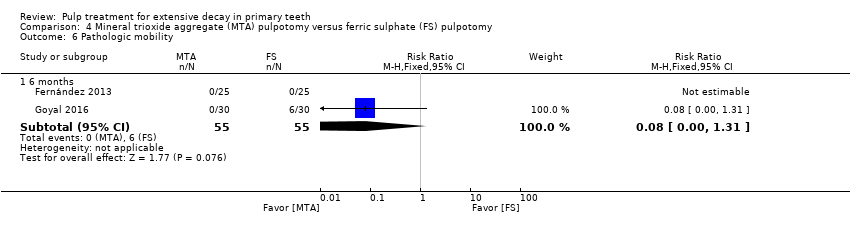
Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 6 Pathologic mobility.

Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 7 Pathologic radiolucency.
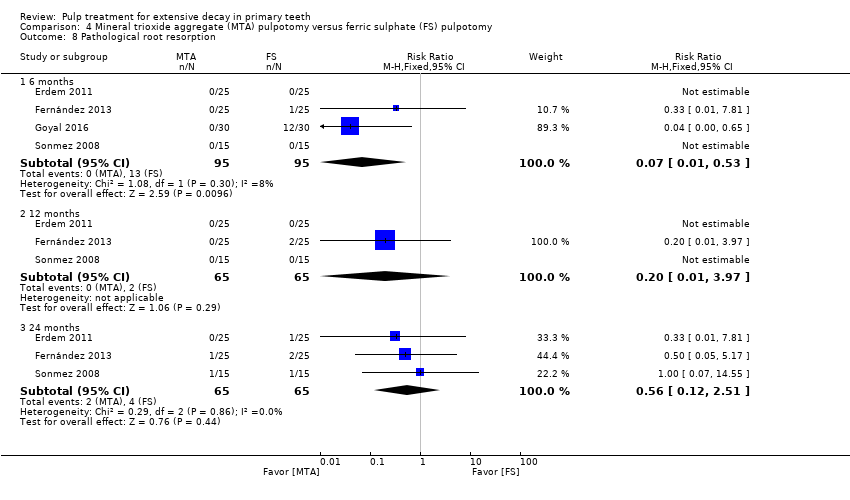
Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 8 Pathological root resorption.
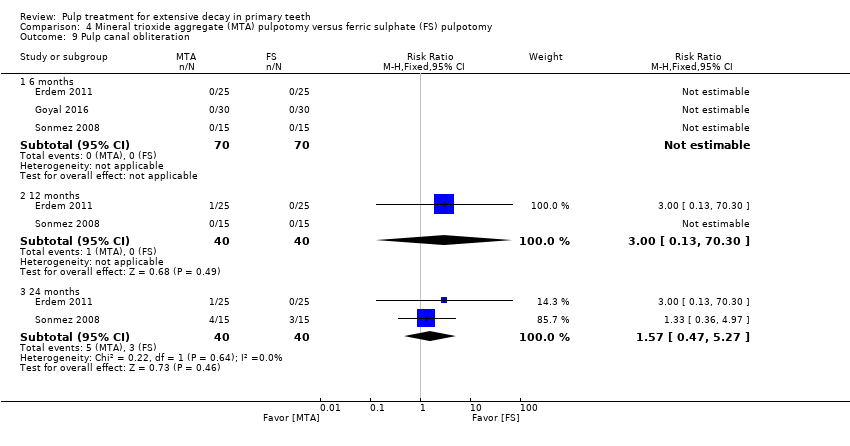
Comparison 4 Mineral trioxide aggregate (MTA) pulpotomy versus ferric sulphate (FS) pulpotomy, Outcome 9 Pulp canal obliteration.
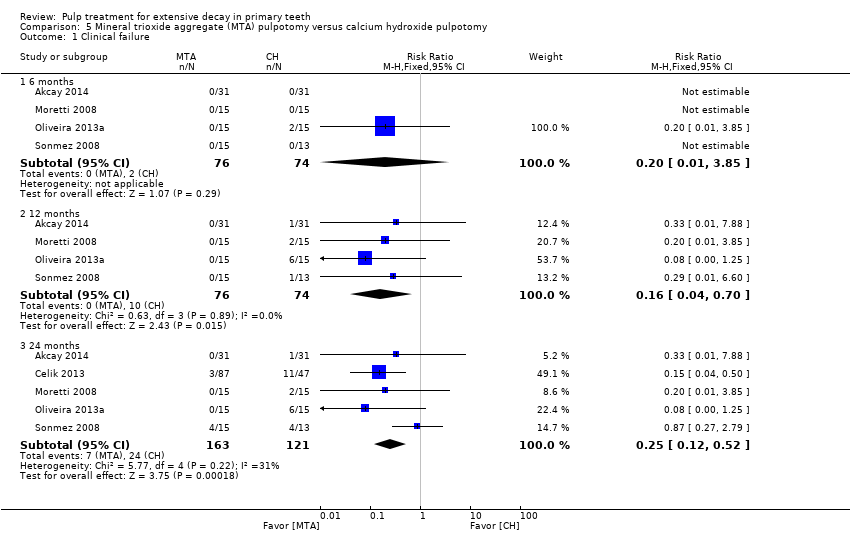
Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 1 Clinical failure.
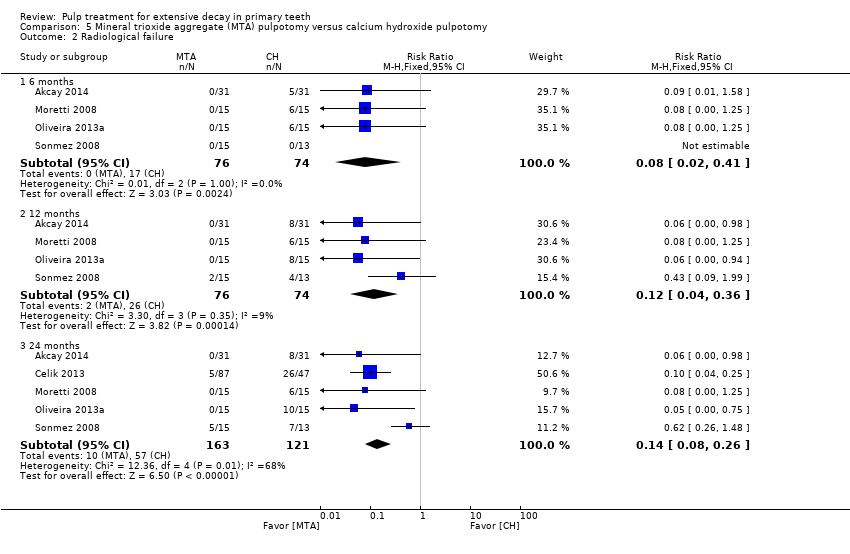
Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 2 Radiological failure.

Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 3 Overall failure.

Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 4 Pain.
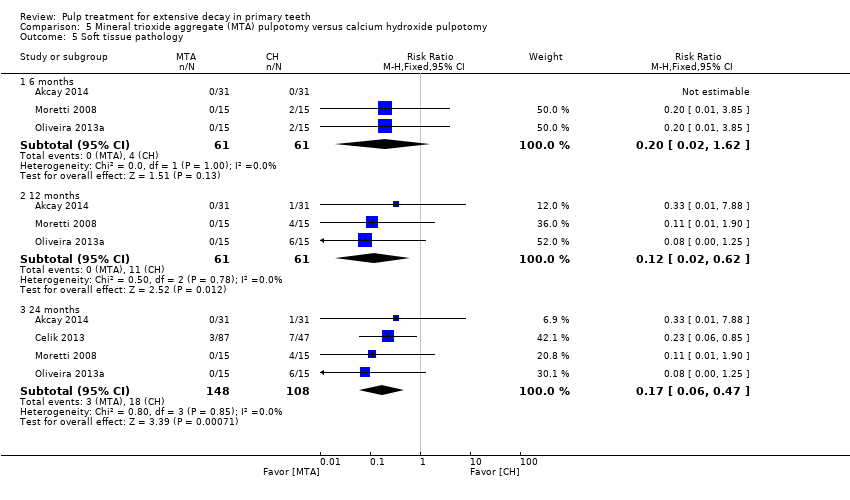
Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 5 Soft tissue pathology.
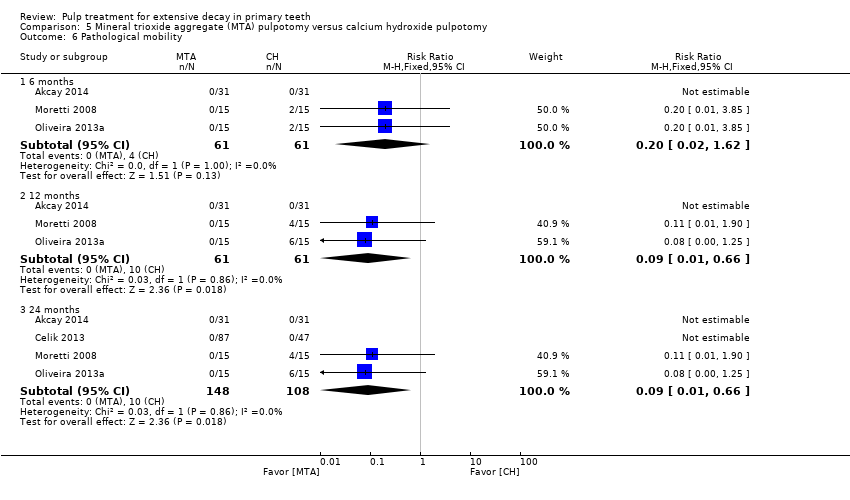
Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 6 Pathological mobility.

Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 7 Pathological radiolucency.

Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 8 Pathological root resorption.
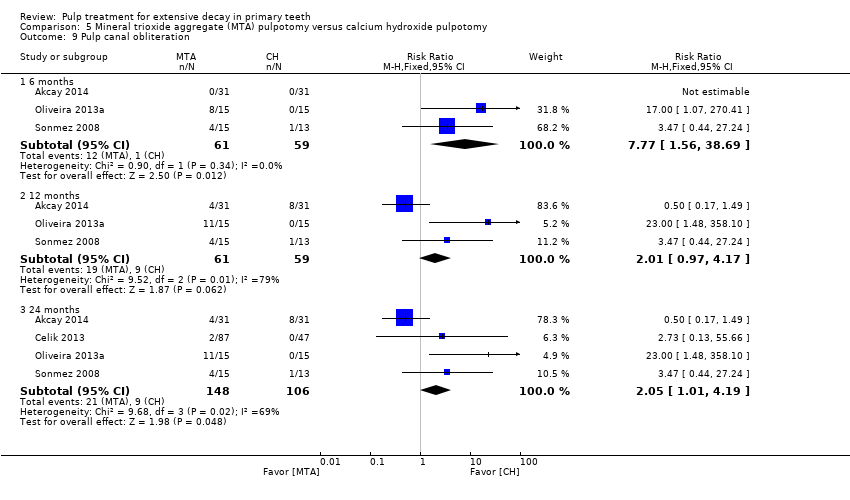
Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 9 Pulp canal obliteration.

Comparison 5 Mineral trioxide aggregate (MTA) pulpotomy versus calcium hydroxide pulpotomy, Outcome 10 Dentin bridge formation.

Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 1 Clinical failure.

Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 2 Radiological failure.

Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 3 Pain.

Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 4 Soft tissue pathology.
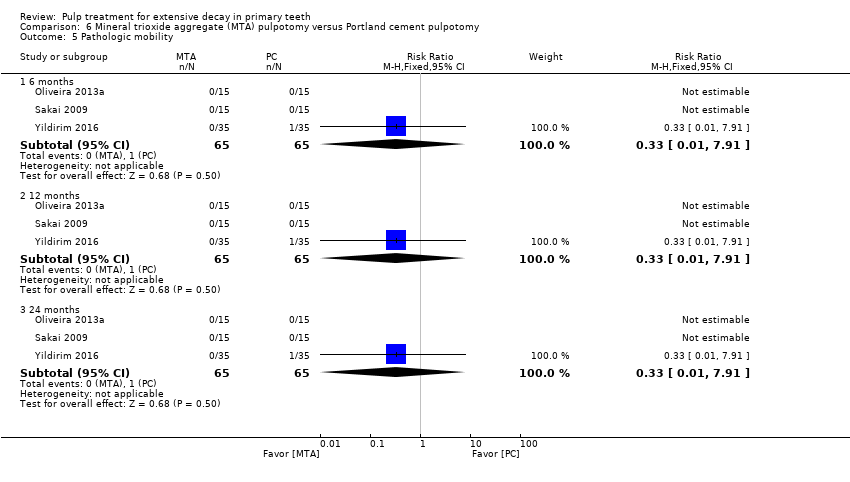
Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 5 Pathologic mobility.
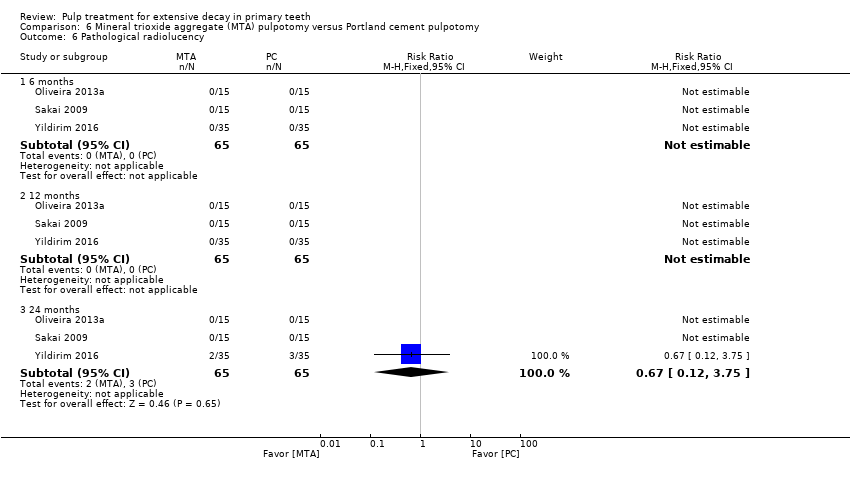
Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 6 Pathological radiolucency.

Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 7 Pathological root resorption.

Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 8 Pulp canal obliteration.
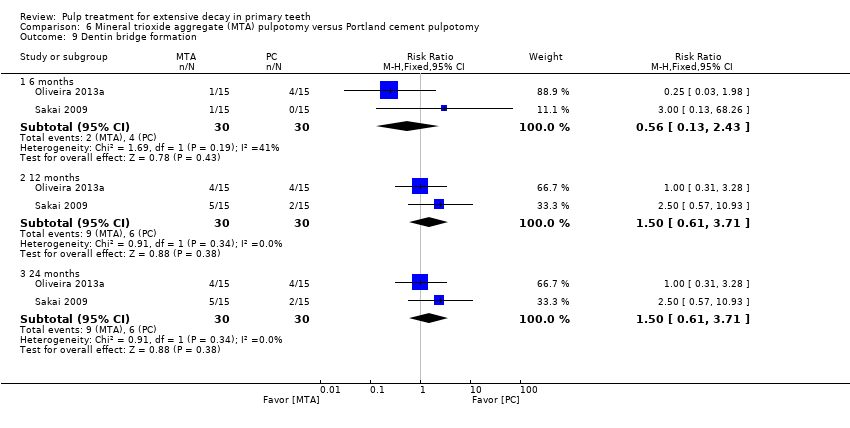
Comparison 6 Mineral trioxide aggregate (MTA) pulpotomy versus Portland cement pulpotomy, Outcome 9 Dentin bridge formation.

Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 1 Clinical failure.
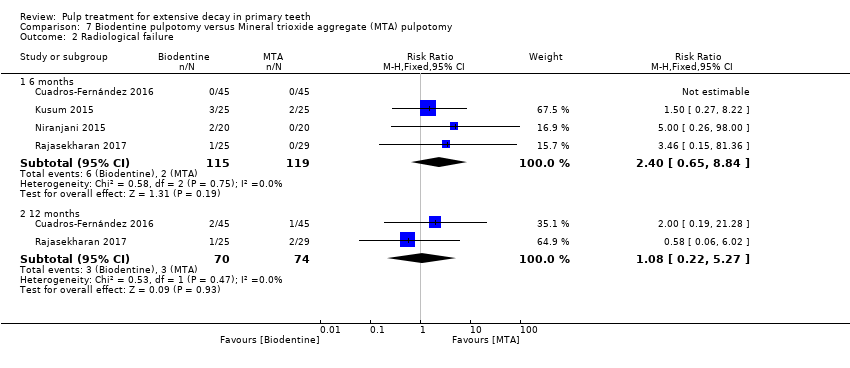
Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 2 Radiological failure.

Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 3 Pain.
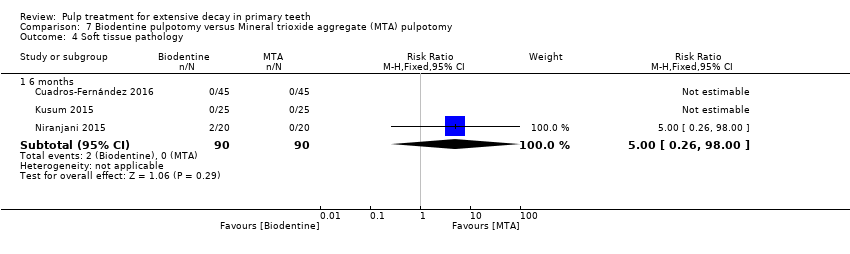
Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 4 Soft tissue pathology.
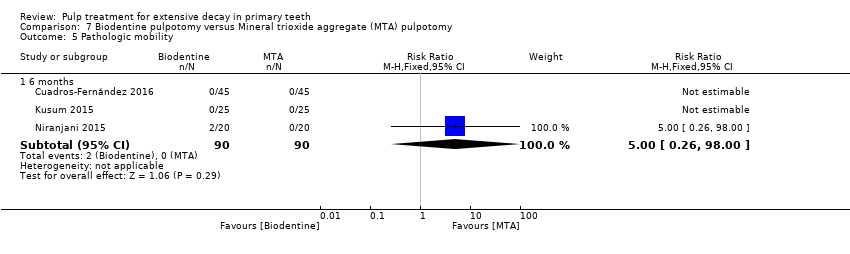
Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 5 Pathologic mobility.

Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 6 Pathological radiolucency.
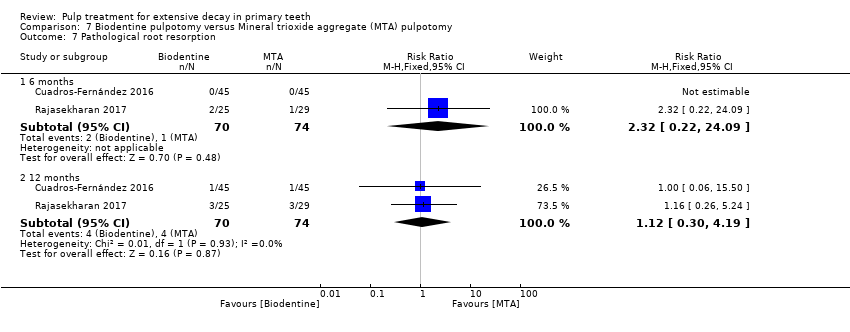
Comparison 7 Biodentine pulpotomy versus Mineral trioxide aggregate (MTA) pulpotomy, Outcome 7 Pathological root resorption.
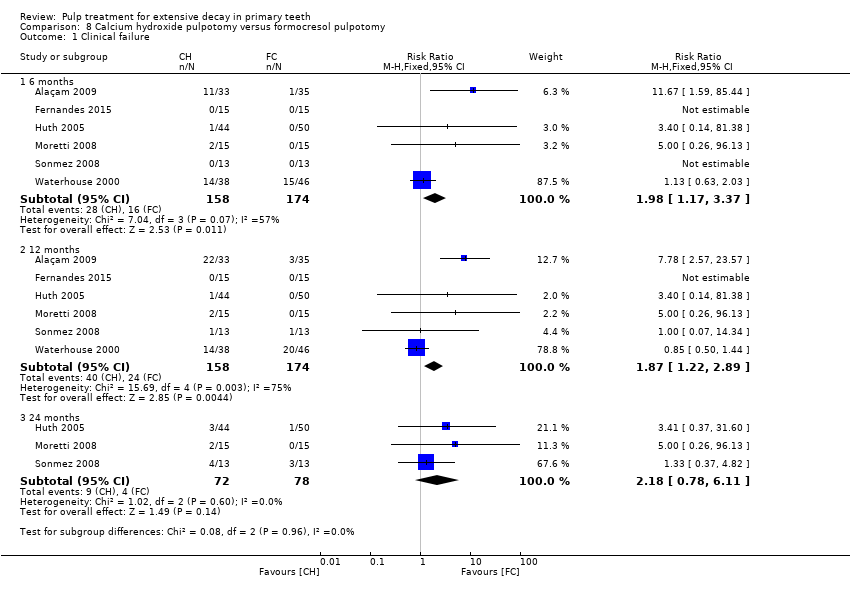
Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 1 Clinical failure.

Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 2 Radiological failure.

Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 3 Overall failure.
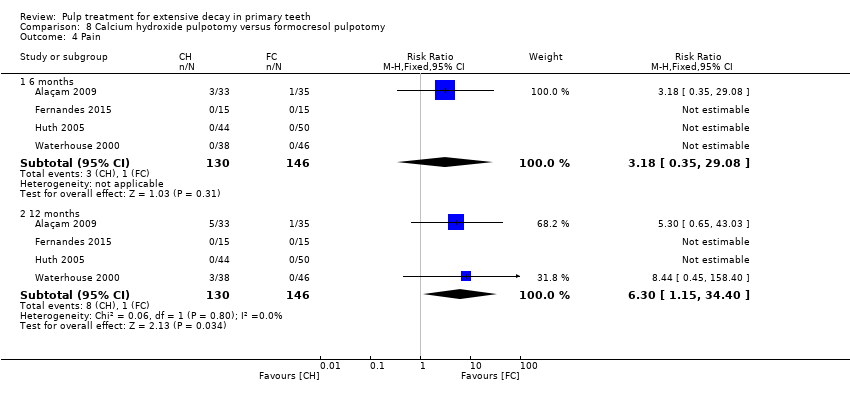
Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 4 Pain.

Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 5 Soft tissue pathology.

Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 6 Pathological mobility.
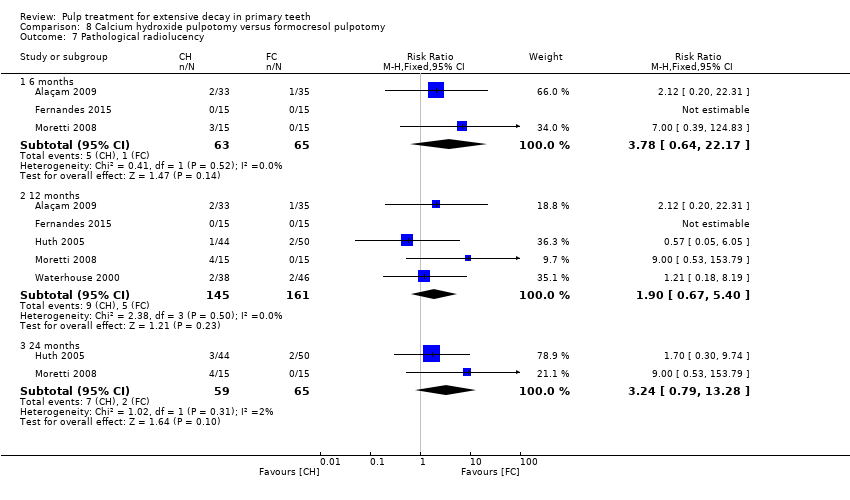
Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 7 Pathological radiolucency.
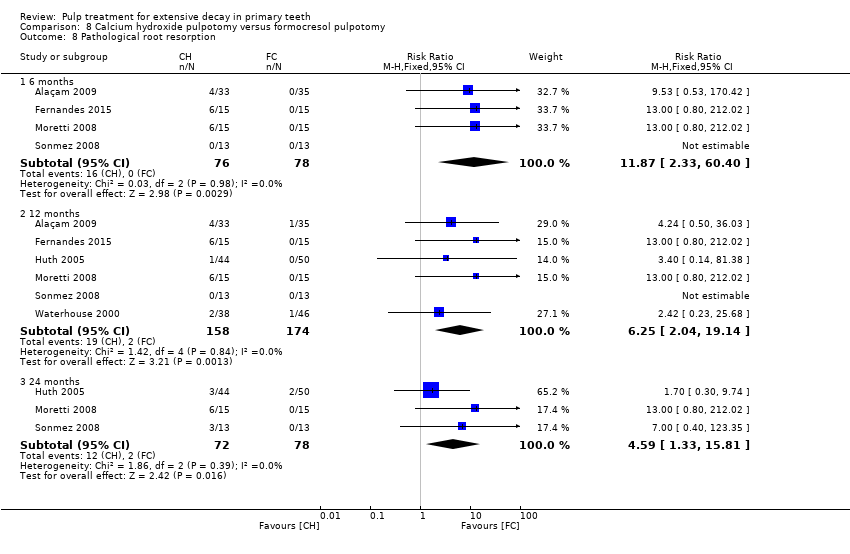
Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 8 Pathological root resorption.
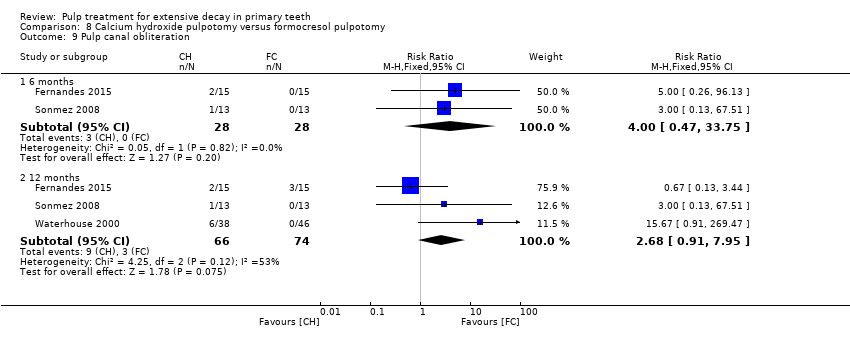
Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 9 Pulp canal obliteration.

Comparison 8 Calcium hydroxide pulpotomy versus formocresol pulpotomy, Outcome 10 Dentin bridge formation.

Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 1 Clinical failure.

Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 2 Radiological failure.
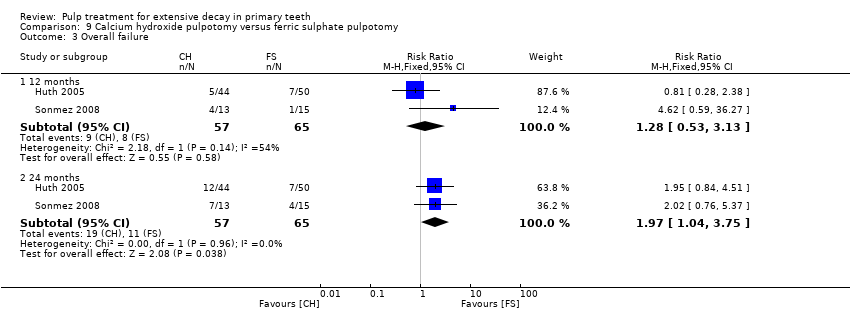
Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 3 Overall failure.
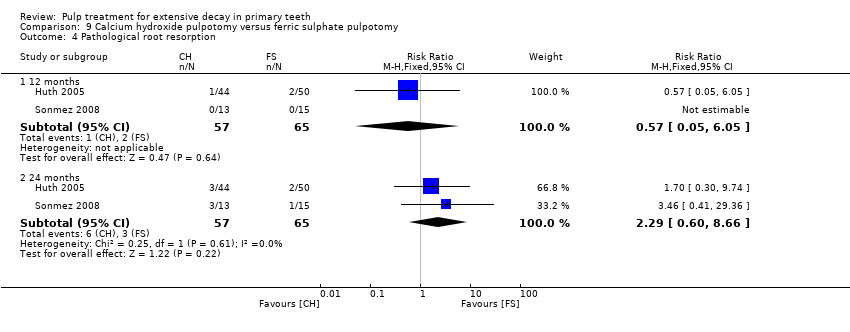
Comparison 9 Calcium hydroxide pulpotomy versus ferric sulphate pulpotomy, Outcome 4 Pathological root resorption.

Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 1 Clinical failure.
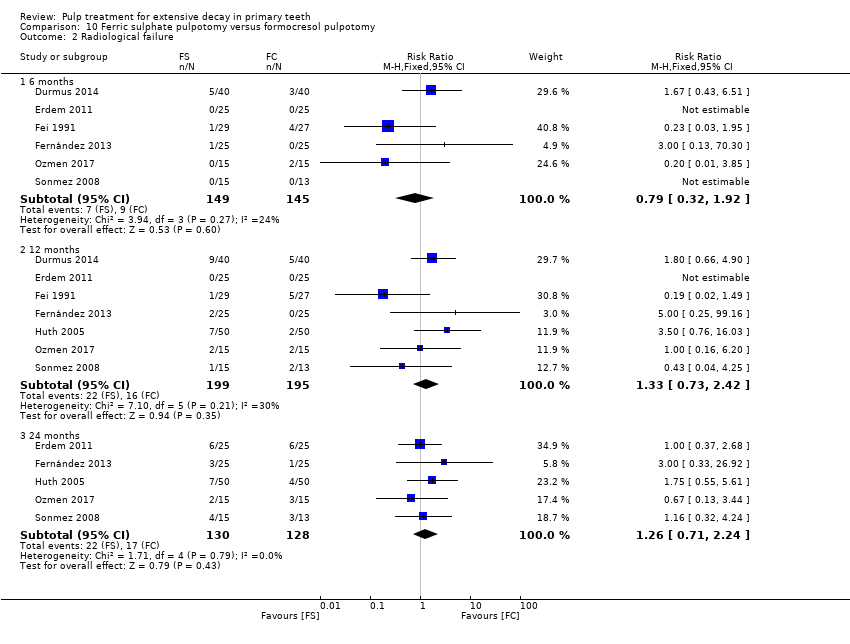
Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 2 Radiological failure.

Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 3 Overall failure.

Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 4 Pain.

Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 5 Pathological radiolucency.

Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 6 Pathological root resorption.

Comparison 10 Ferric sulphate pulpotomy versus formocresol pulpotomy, Outcome 7 Pulp canal obliteration.
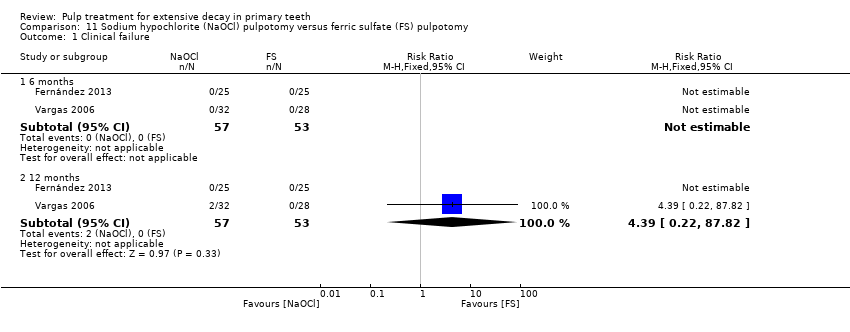
Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 1 Clinical failure.

Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 2 Radiological failure.
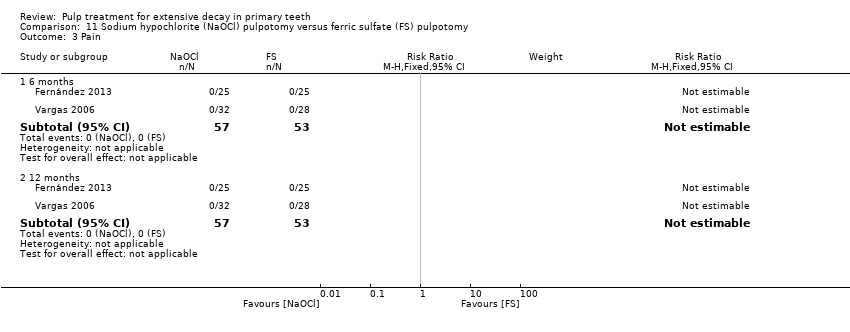
Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 3 Pain.
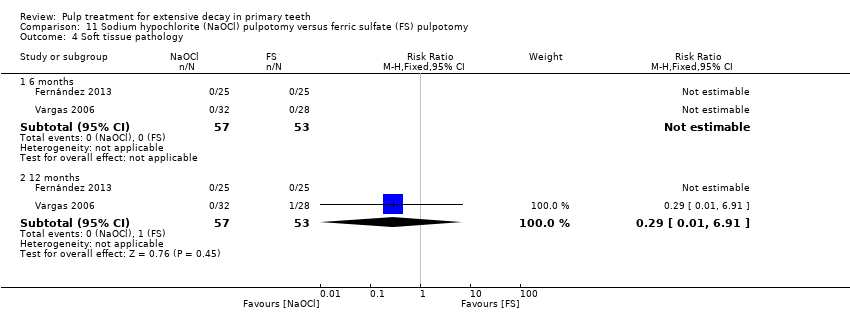
Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 4 Soft tissue pathology.
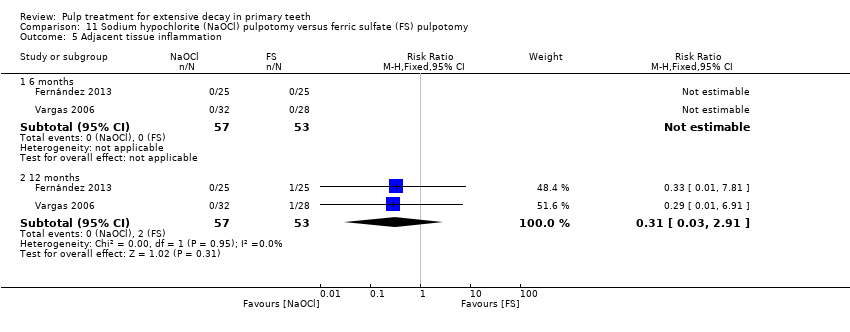
Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 5 Adjacent tissue inflammation.

Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 6 Pathologic mobility.

Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 7 Pathologic radiolucency.
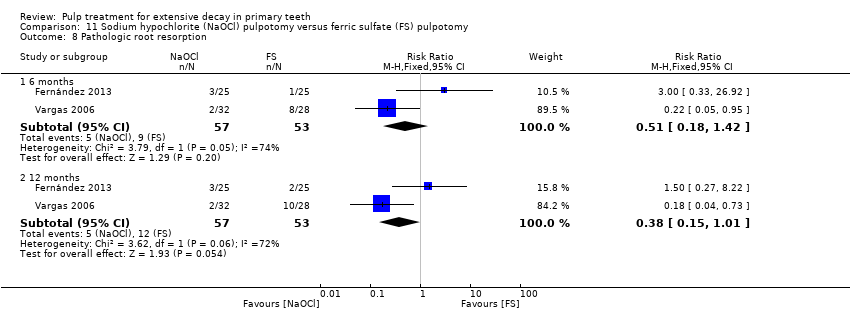
Comparison 11 Sodium hypochlorite (NaOCl) pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 8 Pathologic root resorption.

Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 1 Clinical failure.

Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 2 Radiological failure.

Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 3 Pain.

Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 4 Pathological radiolucency.
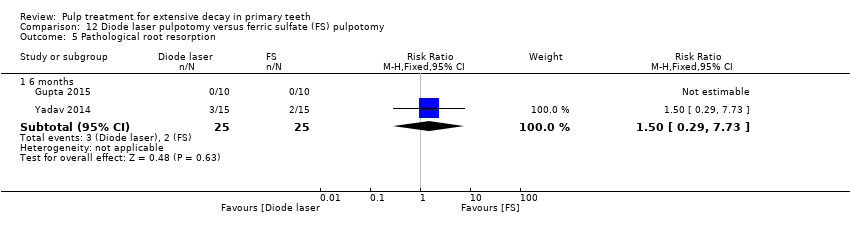
Comparison 12 Diode laser pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 5 Pathological root resorption.
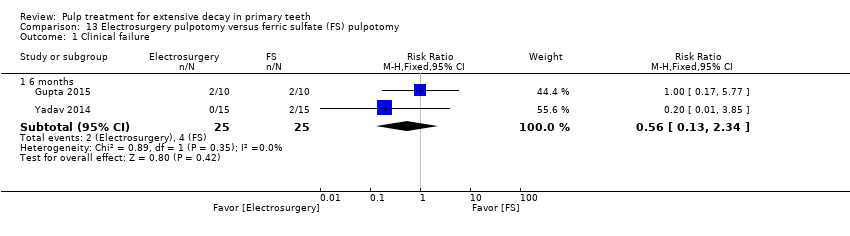
Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 1 Clinical failure.
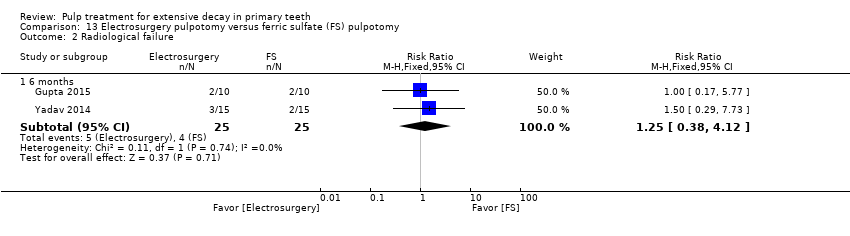
Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 2 Radiological failure.
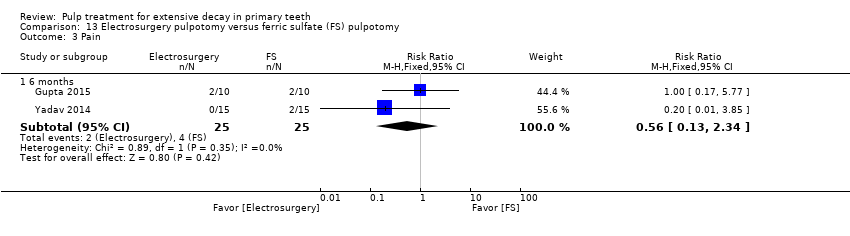
Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 3 Pain.

Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 4 Pathological mobility.

Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 5 Pathological root resorption.

Comparison 13 Electrosurgery pulpotomy versus ferric sulfate (FS) pulpotomy, Outcome 6 Pulp canal obliteration.

Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 1 Clinical failure.

Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 2 Radiological failure.

Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 3 Pain.
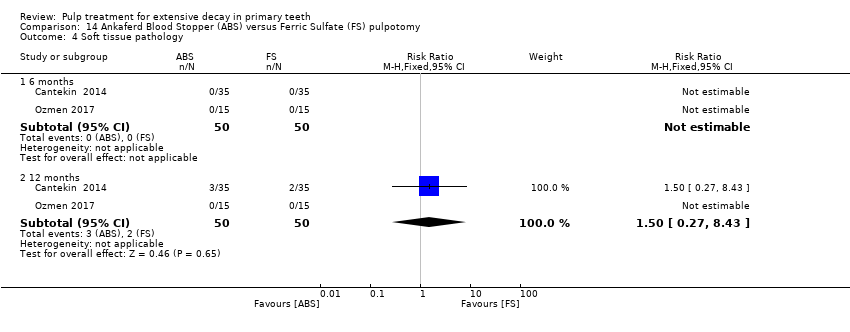
Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 4 Soft tissue pathology.
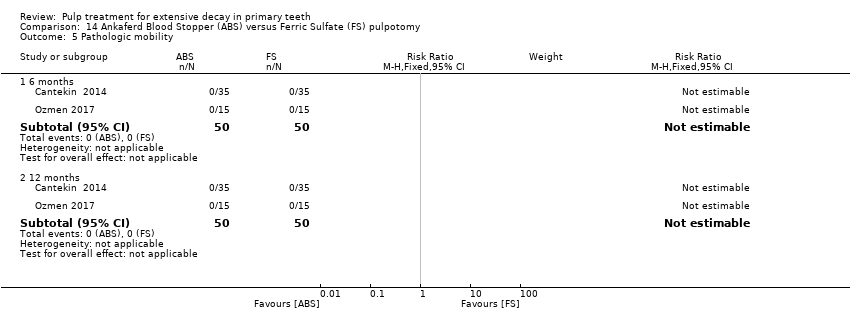
Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 5 Pathologic mobility.

Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 6 Pathologic radiolucency.

Comparison 14 Ankaferd Blood Stopper (ABS) versus Ferric Sulfate (FS) pulpotomy, Outcome 7 Pathologic root resorption.
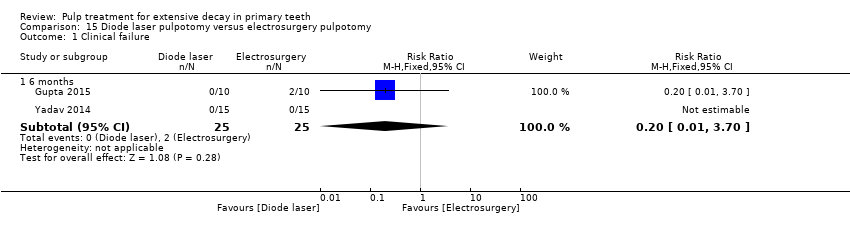
Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 1 Clinical failure.

Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 2 Radiological failure.

Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 3 Pain.
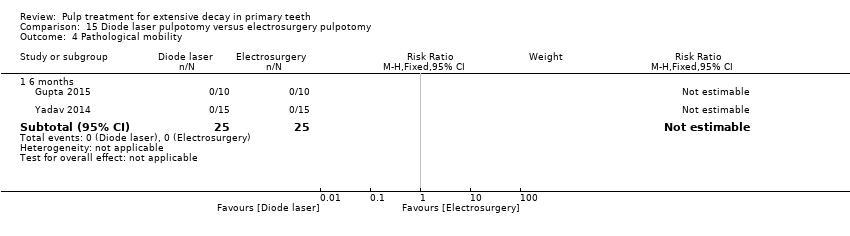
Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 4 Pathological mobility.

Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 5 Pathological radiolucency.
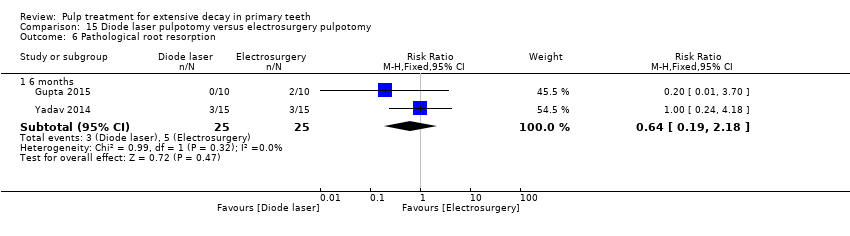
Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 6 Pathological root resorption.

Comparison 15 Diode laser pulpotomy versus electrosurgery pulpotomy, Outcome 7 Pulp canal obliteration.

Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 1 Clinical failure.

Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 2 Radiological failure.
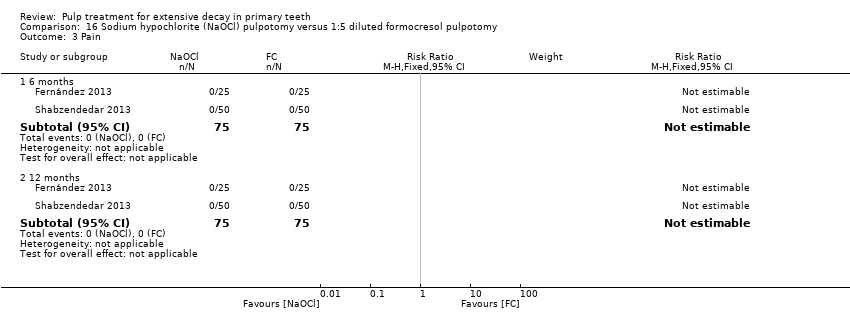
Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 3 Pain.

Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 4 Soft tissue pathology.

Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 5 Pathologic mobility.

Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 6 Pathologic radiolucency.

Comparison 16 Sodium hypochlorite (NaOCl) pulpotomy versus 1:5 diluted formocresol pulpotomy, Outcome 7 Pathologic root resorption.

Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 1 Clinical failure.

Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 2 Pain.

Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 3 Soft tissue pathology.

Comparison 17 Enamel matrix derivative (EMD) pulpotomy versus formocresol pulpotomy, Outcome 4 Pathologic mobility.
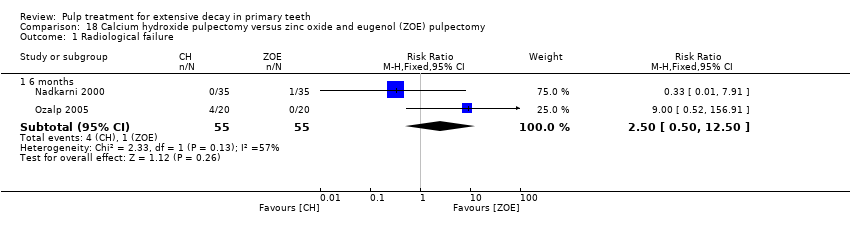
Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 1 Radiological failure.

Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 2 Pain.

Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 3 Pathological mobility.
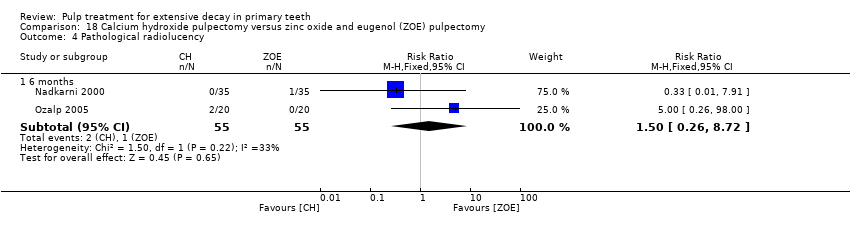
Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 4 Pathological radiolucency.
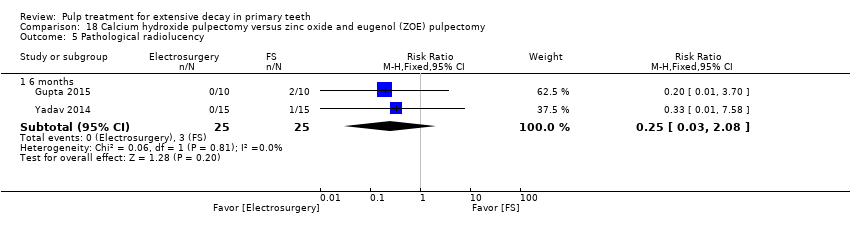
Comparison 18 Calcium hydroxide pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 5 Pathological radiolucency.

Comparison 19 Metapex versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 1 Clinical failure.
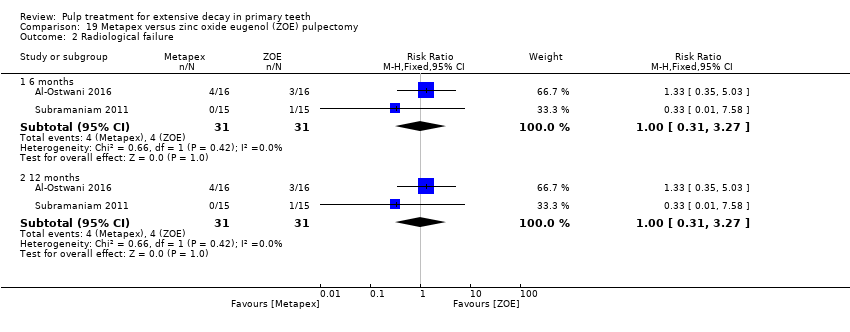
Comparison 19 Metapex versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 2 Radiological failure.

Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 1 Clincal failure.

Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 2 Radiological failure.
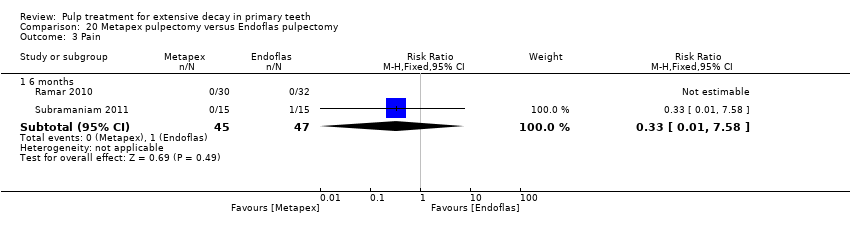
Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 3 Pain.

Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 4 Soft tissue pathology.

Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 5 Pathologic mobility.

Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 6 Pathological radiolucency.

Comparison 20 Metapex pulpectomy versus Endoflas pulpectomy, Outcome 7 Pathological root resorption.

Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 1 Clinical failure.
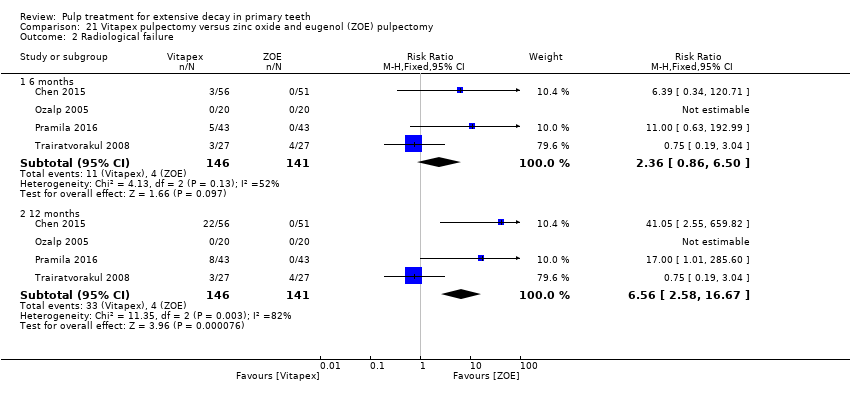
Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 2 Radiological failure.
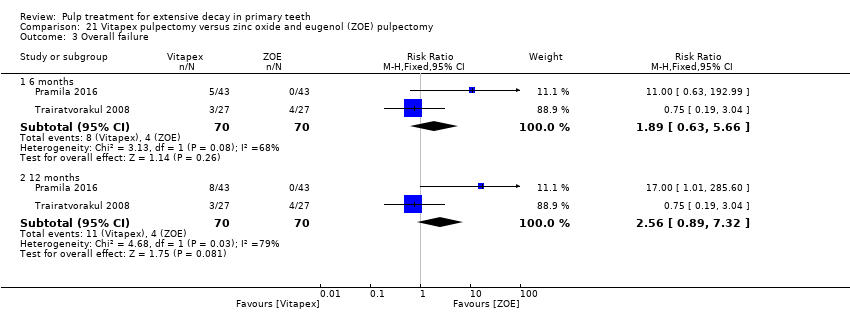
Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 3 Overall failure.

Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 4 Pain.
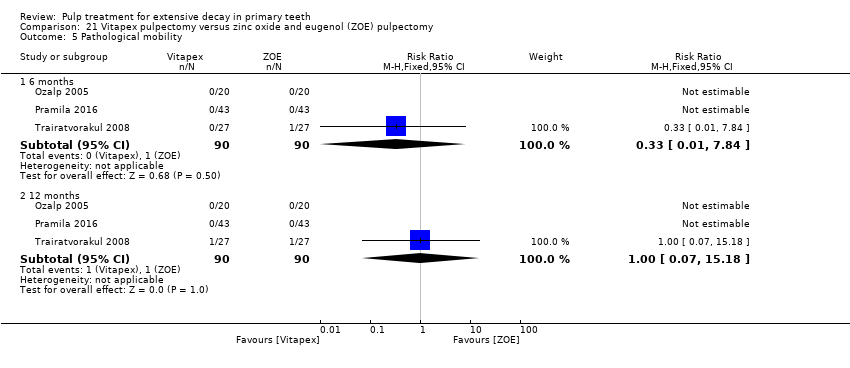
Comparison 21 Vitapex pulpectomy versus zinc oxide and eugenol (ZOE) pulpectomy, Outcome 5 Pathological mobility.

Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 1 Clinical failure.
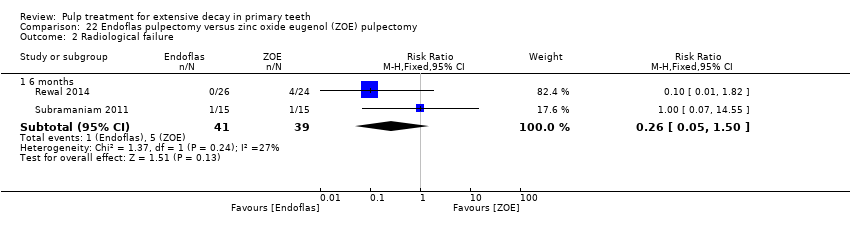
Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 2 Radiological failure.

Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 3 Pain.
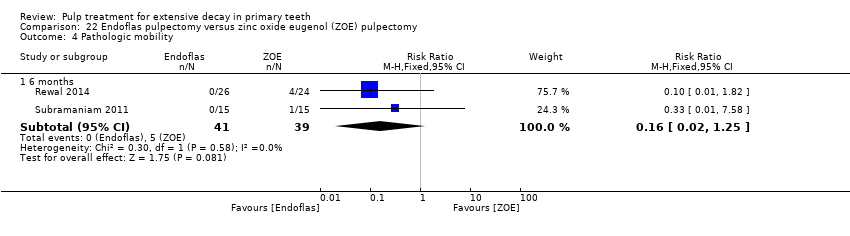
Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 4 Pathologic mobility.

Comparison 22 Endoflas pulpectomy versus zinc oxide eugenol (ZOE) pulpectomy, Outcome 5 Pathologic radiolucency.
| Pulpotomy compared with pulpotomy using alternative medicament/technique for extensive decay in primary teeth | ||||||
| Population: children with extensive decay in primary teeth Settings: primary care Intervention: pulpotomy with one type of medicament Comparison: pulpotomy using alternative medicament or different technique | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Experimental | |||||
| MTA versus formocresol | ||||||
| Clinical failure (12 months) | 28 per 1000 | 8.6 per 1000 (2.8 per 1000 to 26.0 per 1000) | RR 0.31 (0.10 to 0.93) | 740 (12 studies) | ⊕⊕⊕⊝ | Failure rate less than 3% across both the MTA and formocresol treatment groups. Seven of the 12 studies had no failures at 12 months. No evidence of a difference in clinical failure at 6 months or 24 months |
| Radiological failure (12 months) | 50 per 1000 | 20.5 per 1000 (9.5 per 1000 to 44.5 per 1000) | RR 0.41 (0.19 to 0.89) | 740 (12 studies) | ⊕⊕⊕⊝ | Failure rate 5% across formocresol treatment groups and 2.1% across MTA treatment groups. Five of the 12 studies had no failures at 12 months. Results similar at 6 and 24 months |
| MTA versus calcium hydroxide | ||||||
| Clinical failure (12 months) | 14 per 1000 | 2.2 per 1000 (0.02 per 1000 to 9.8 per 1000) | RR 0.16 (0.04 to 0.70) | 150 (4 studies) | ⊕⊕⊕⊝ | Results similar at 24 months. No evidence of a difference in clinical failure at 6 months |
| Radiological failure (12 months) | 351 per 1000 | 42.1 per 1000 (14 per 1000 to 126.4 per 1000) | RR 0.12 (0.04 to 0.36) | 150 (4 studies) | ⊕⊕⊝⊝ | Results similar at 6 and 24 months |
| Calcium hydroxide versus formocresol | ||||||
| Clinical failure (12 months) | 115 per 1000 | 215 per 1000 (140.3 per 1000 to 332.4 per 1000) | RR 1.87 (1.22 to 2.89) | 332 (6 studies) | ⊕⊕⊕⊝ | Results similar at 6 months No evidence of a difference in clinical failure at 24 months |
| Radiological failure (12 months) | 253 per 1000 | 470.6 per 1000 (359.3 per 1000 to 617.3 per 1000) | RR 1.86 (1.42 to 2.44) | 332 (6 studies) | ⊕⊕⊕⊝ | Results similar at 6 and 24 months |
| Other comparisons assessed in more than one trial that had treatment failures | ||||||
| Clinical failure (at six, 12 and 24 months) | The quality of the evidence waslow for 4 comparisons3: laser versus ferric sulphate; Biodentine versus MTA; ferric sulphate versus formocresol; electrosurgery versus ferric sulphate; calcium hydroxide versus ferric sulphate. The quality of the evidence was very low for 5 comparisons: NaOCl versus ferric sulphate4; laser versus electrosurgery4; MTA versus ferric sulphate5; ABS versus ferric sulphate6; EMD versus formocresol7. | |||||
| Radiological failure (at six, 12 and 24 months) | The quality of the evidence waslow for 8 comparisons: NaOCl versus ferric sulphate2; MTA versus ferric sulphate3; Biodentine versus MTA3; ferric sulphate versus formocresol3; laser versus ferric sulphate3; electrosurgery versus ferric sulphate3; ABS versus ferric sulphate3; laser versus electrosurgery3; calcium hydroxide versus ferric sulphate (favouring ferric sulphate)3. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. Downgraded 1 level due to high risk of bias | ||||||
| Pulpectomy compared with pulpectomy using alternative medicament for extensive decay in primary teeth | ||||||
| Population: children with extensive decay in primary teeth Settings: primary care Intervention: pulpectomy with 1 type of medicament Comparison: pulpectomy using alternative medicament | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Experimental | |||||
| Endoflas versus ZOE | ||||||
| Clinical failure (6 months) | 128 per 1000 | 33.3 per 1000 (6.4 per 1000 to 192 per 1000) | RR 0.26 (0.05 to 1.50) | 80 (2 studies) | ⊕⊕⊕⊝ | One trial assessed failure at 12 months: RR 1.00, 95% 0.07 to 14.55 |
| Radiological failure (6 months) | 128 per 1000 | 33.3 per 1000 (6.4 per 1000 to 192 per 1000) | RR 0.26 (0.05 to 1.50) | 80 (2 studies) | ⊕⊕⊕⊝ | |
| Metapex versus ZOE | ||||||
| Clinical failure (12 months) | 97 per 1000 | 68.9 per 1000 (14.6 per 1000 to 323 per 1000) | RR 0.71 (0.15 to 3.33) | 62 (2 studies) | ⊕⊕⊕⊝ | Results similar at 6 months |
| Radiological failure (12 months) | 129 per 1000 | 129 per 1000 (40 per 1000 to 421.8 per 1000) | RR 1.00 (0.31 to 3.27) | 62 (2 studies) | ⊕⊕⊕⊝ | Results similar at 6 months |
| Other comparisons assessed in more than one trial that had treatment failures | ||||||
| Clinical failure | The quality of the evidence was rated as low for 1 comparison: Vitapex versus ZOE (favouring ZOE)2 | |||||
| Radiological failure | The quality of the evidence was rated as low for 2 comparisons: Vitapex versus ZOE2 (favouring ZOE); calcium hydroxide versus ZOE3 | |||||
| 1. Downgraded 1 level due to imprecision | ||||||
| Direct pulp capping compared with direct pulp capping using alternative medicament for extensive decay in primary teeth | ||||||
| Population: children with extensive decay in primary teeth Settings: primary care Intervention: direct pulp capping with 1 type of medicament Comparison: direct pulp capping using alternative medicament | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Experimental | |||||
| Seven trials evaluated 22 comparisons of different medicaments for direct pulp capping. Each comparison was assessed by a single trial. There were no clinical or radiological failures in two comparisons: acetone‐based total‐etch adhesive versus calcium hydroxide; MTA versus calcium hydroxide. | ||||||
| Clinical failure (at six, 12 and 24 months) | The quality of the evidence was assessed as low for 5 comparisons1: calcium hydroxide versus formocresol (favouring formocrescol), MTA versus 3Mix and MTA versus simvastatin (favouring MTA), 3Mix versus 3Mixtatin and 3Mixtatin versus simvastatin (favouring 3Mixtatin). The quality of the evidence was rated as very low for all other comparisons.2 | |||||
| Radiological failure (at six, 12 and 24 months) | The quality of the evidence was rated as low for 1 comparison: calcium hydroxide versus formocresol1 (favouring formocresol). The quality of the evidence was rated as very low for all other comparisons.2 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. Downgraded 1 level due to risk of bias and 1 level due to imprecision | ||||||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Pain | mean 22 | 1 | Not estimable* |
| Soft tissue pathology | mean 22 | 1 | Not estimable* |
| Pathological mobility | mean 22 | 1 | Not estimable* |
| Pathological radiolucency | mean 22 | 1 | 3.46 (0.17 to 70.69) |
| Pathological root resorption | mean 22 | 1 | 2.75 (0.82 to 9.29) |
| Pulp canal obliteration | mean 22 | 1 | 0.83 (0.51 to 1.33) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FS: ferric sulphate; MTA: mineral trioxide aggregate | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 18 | 1 | Not estimable* |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.04 to 2.94) | |
| 18 | 1 | 0.33 (0.04 to 2.94) | |
| Pathological root resorption | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.04 to 2.94) | |
| 18 | 1 | 0.33 (0.04 to 2.94) | |
| *due to lack of events Abbreviations ‐ CEM: calcium‐enriched mixture; CI: confidence interval; MTA: mineral trioxide aggregate | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | Not estimable* |
| 24 | 1 | 0.33 (0.01, 7.81) | |
| Radiological failure | 6 and 12 | 1 | 0.14 (0.01, 2.63) |
| 24 | 1 | 0.33 (0.04, 2.99) | |
| Overall failure | 24 | 1 | 0.33 (0.04, 2.99) |
| Pain | 6, 12 and 24 months | 1 | Not estimable* |
| Soft tissue pathology | 6 and 12 | 1 | Not estimable* |
| 24 | 1 | 0.33 (0.01, 7.81) | |
| Pathologic mobility | 6, 12 and 24 months | 1 | Not estimable* |
| Pathologic radiolucency | 6, 12 and 24 months | 1 | Not estimable* |
| Pathologicroot resorption | 6 and 12 | 1 | 0.14 (0.01, 2.63) |
| 24 | 1 | 0.33 (0.04, 2.99) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate; NaOCl: sodium hypochlorite | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | Not estimable* |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 | 1 | 0.09 (0.01, 1.58) | |
| Soft tissue pathology | 6 and 12 | 1 | Not estimable* |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Adjacent tissue inflammation | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 0.14 (0.01, 2.66) | |
| Pathologicroot resorption | 6 | 1 | Not estimable* |
| 12 | 1 | 0.14 (0.01, 2.66) | |
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 0.44 (0.15, 1.29) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate; CH: calcium hydroxyde; NaOCl; sodium hypochlorite | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | Not estimable* |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 | 1 | 0.20 (0.02, 1.61) | |
| Soft tissue pathology | 6 and 12 | 1 | Not estimable* |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Adjacent tissue inflammation | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 0.14 (0.01, 2.66) | |
| Pathologic root resorption | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.04, 3.03) | |
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 0.67 (0.27, 1.65) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate; NaOCl; sodium hypochlorite; CH: calcium hydroxyde. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Pain | 6 | 1 | 0.06 (0.00, 0.98) |
| Soft tissue pathology | 6 | 1 | 0.08 (0.00, 1.31) |
| Pathologic mobility | 6 | 1 | 0.06 (0.00, 0.98) |
| Pathologic radiolucency | 6 | 1 | 0.03 (0.00, 0.55) |
| Pathologic root resorption | 6 | 1 | 0.05 (0.00, 0.78) |
| Pulp canal obliteration | 6 | 1 | 0.11 (0.01, 1.98) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 0.20 (0.03 to 1.59) | |
| Radiological failure | 6 | 1 | 0.33 (0.01 to 7.81) |
| 12 | 1 | 0.20 (0.01 to 3.97) | |
| 24 | 1 | 0.10 (0.01 to 0.72) | |
| Overall failure | 6 | 1 | 0.33 (0.01 to 7.81) |
| 12 | 1 | 0.20 (0.01 to 3.97) | |
| 24 | 1 | 0.13 (0.02 to 0.93) | |
| Pain | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 3.00 (0.13 to 70.30) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 3.00 (0.13 to 70.30) | |
| Pathological root resorption | 6 | 1 | 0.33 (0.01 to 7.81) |
| 12 | 1 | 0.33 (0.01 to 7.81) | |
| 24 | 1 | 0.08 (0.00 to 1.30) | |
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 70.30) | |
| 24 | 1 | 11.0 (0.64 to 188.96) | |
| Physiological root resorption | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 0.20 (0.01 to 3.97) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate; ZOE: zinc oxide and eugenol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 15.7 | 1 | Not estimable* |
| Radiological failure | 15.7 | 1 | 4.00 (0.48 to 33.42) |
| Overall failure | 15.7 | 1 | 2.00 (0.40 to 9.99) |
| Pathological radiolucency | 15.7 | 1 | 3.00 (0.33 to 26.99) |
| Pathological root resorption | 15.7 | 1 | 1.50 (0.27 to 8.25) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FC: formocresol; MTA: mineral trioxide aggregate; ZOE: zinc oxide and eugenol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 24 | 1 | 0.14 (0.01, 2.67) |
| Radiological failure | 24 | 1 | 0.29 (0.06, 1.28) |
| Overall failure | 6, 12 and 24 | 1 | 0.14 (0.01, 2.67) |
| Pain | 6, 12 and 24 | 1 | 0.33 (0.01, 7.91) |
| Soft tissue pathology | 6, 12 and 24 | 1 | 0.20 (0.01, 4.02) |
| Pathologic mobility | 6, 12 and 24 | 1 | 0.20 (0.01, 4.02) |
| Pathologic radiolucency | 24 | 1 | 0.40 (0.08, 1.93) |
| Pathologic root resorption | 24 | 1 | 0.20 (0.01, 4.02) |
| Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate; EMD: enamel matrix derivative | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | 3.21 (0.14, 75.68) |
| Radiological failure | 6 | 1 | 9.64 (0.54, 171.09) |
| 12 | 1 | 2.69 (0.57, 12.70) | |
| Pathological radiolucency | 6 | 1 | 3.21 (0.14, 75.68) |
| 12 | 1 | 2.15 (0.43, 10.79) | |
| Pathological root resorption | 6 | 1 | 6.44 (0.83, 50.11) |
| 12 | 1 | 4.30 (1.00, 18.47) | |
| Pulp canal obliteration | 6 | 1 | 3.76 (0.85, 16.54) |
| 12 | 1 | 1.61 (0.78, 3.33) | |
| Dentine bridge formation | 6 | 1 | 0.15 (0.01, 2.83) |
| 12 | 1 | 0.07 (0.00, 1.19) | |
| Abbreviation: CI: confidence interval | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | Not estimable* |
| Radiological failure | 6 and 12 | 1 | 0.33 (0.01, 7.88) |
| Soft tissue pathology | 6 and 12 | 1 | Not estimable* |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Adjacent tissue inflammation | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 and 12 | 1 | Not estimable* |
| Pathologic root resorption | 6 and 12 | 1 | 0.33 (0.01, 7.88) |
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 0.67 (0.21, 2.13) | |
| * due to lack of events Abbreviations ‐ CI: confidence interval; MTA: mineral trioxide aggregate; NaOCl; sodium hypochlorite. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.01, 7.98) | |
| Radiological failure | 6 | 1 | 1.00 (0.06, 15.52) |
| 12 | 1 | 0.50 (0.05, 5.33) | |
| Pain | 6 and 12 | 1 | Not estimable* |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.01, 7.98) | |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | 0.33 (0.01, 7.98) |
| 12 | 1 | 0.20 (0.01, 4.06) | |
| Pathologic root resorption | 6 | 1 | 3.00 (0.13, 71.82) |
| 12 | 1 | 1.00 (0.06, 15.52) | |
| *due to lack of events Abbreviation: CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | Not estimable* |
| Radiological failure | 6 and 12 | 1 | 0.35 (0.04, 3.22) |
| Pain | 6 and 12 | 1 | Not estimable* |
| Soft tissue pathology | 6 and 12 | 1 | Not estimable* |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 and 12 | 1 | 0.35 (0.01, 8.32) |
| Pathologic root resorption | 6 and 12 | 1 | 0.35 (0.04, 3.22) |
| *due to lack of events Abbreviation: CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 3.13 (0.13, 74.85) | |
| Radiological failure | 6 | 1 | 0.35 (0.04, 3.22) |
| 12 | 1 | 0.70 (0.12, 3.98) | |
| Pain | 6 and 12 | 1 | Not estimable* |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | 3.13 (0.13, 74.85) | |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | 1.04 (0.07, 16.19) |
| 12 | 1 | 2.09 (0.20, 22.24) | |
| Pathologic root resorption | 6 | 1 | 0.15 (0.01, 2.81) |
| 12 | 1 | 0.35 (0.04, 3.22) | |
| *due to lack of events Abbreviation: CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 5.00 (0.26, 96.13) |
| 12 and 24 | 1 | 13.00 (0.80, 212.02) | |
| Radiological failure | 6 | 1 | 13.00 (0.80, 212.02) |
| 12 | 1 | 17.00 (1.07 to 270.41) | |
| 24 | 1 | 21.00 (1.34 to 328.86) | |
| Soft tissue pathology | 6 | 1 | 5.00 (0.26, 96.13) |
| 12 and 24 | 1 | 13.00 (0.80, 212.02) | |
| Pathologic mobility | 6 | 1 | 5.00 (0.26, 96.13) |
| 12 and 24 | 1 | 13.00 (0.80, 212.02) | |
| Adjacent tissue inflammation | 6, 12 and 24 | 1 | Not estimable * |
| Pathologic radiolucency | 6 | 1 | 13.00 (0.80, 212.02) |
| 12 | 1 | 17.00 (1.07 to 270.41) | |
| 24 | 1 | 21.00 (1.34 to 328.86) | |
| Pathologic root resorption | 6 | 1 | 13.00 (0.80, 212.02) |
| 12 | 1 | 17.00 (1.07 to 270.41) | |
| 24 | 1 | 21.00 (1.34 to 328.86) | |
| Dentine bridge formation | 6, 12 and 24 | 1 | 0.50 (0.11 to 2.33) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; CH: calcium hydroxide; PC: Portland cement. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13, 70.92) | |
| Radiological failure | 6 | 1 | 5.00 (0.62, 40.36) |
| 12 | 1 | 8.00 (1.06, 60.21) | |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13, 70.92) | |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Adjacent tissue inflammation | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 15.00 (0.89, 251.77) | |
| Pathologic root resorption | 6 | 1 | Not estimable* |
| 12 | 17.00 (1.02, 282.30) | ||
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 1.33 (0.52, 3.39) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; CH: calcium hydroxyde; MTA: mineral trioxide aggregate; NaOCl; sodium hypochlorite. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 0.31 (0.01 to 7.48) |
| 12 | 1 | 0.94 (0.60 to 14.52) | |
| 24 | 1 | 0.62 (0.11 to 3.56) | |
| Radiological failure | 12 | 1 | 0.56 (0.14 to 2.21) |
| 24 | 1 | 0.31 (0.11 to 0.90) | |
| Overall failure | 12 | 1 | 0.56 (0.14 to 2.21) |
| 24 | 1 | 0.31 (0.11 to 0.90) | |
| Pain | 6, 12 and 24 | 1 | Not estimable* |
| Soft tissue pathology | 6, 12 and 24 | 1 | Not estimable* |
| Pathological mobility | 6, 12 and 24 | 1 | Not estimable* |
| Pathological radiolucency | 12 | 1 | 0.31 (0.01 to 7.48) |
| 24 | 1 | 0.62 (0.11 to 3.56) | |
| Pathological root resorption | 12 | 1 | 0.94 (0.60 to 14.52) |
| 24 | 1 | 0.62 (0.11 to 3.56) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Er:YAG: erbium:yttrium‐aluminium garnet; CH: calcium hydroxide. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 1.41 (0.77 to 2.58) |
| 12 | 1 | 1.13 (0.82 to 1.54) | |
| Radiological failure | 6 | 1 | 1.33 (0.89 to 2.00) |
| 12 | 1 | 1.17 (0.87 to 1.59) | |
| Pain | 6 | 1 | 1.72 (0.45 to 6.61) |
| 12 | 1 | 1.03 (0.33 to 3.23) | |
| Soft tissue pathology | 6 | 1 | 1.55 (0.28 to 8.65) |
| 12 | 1 | 1.03 (0.22 to 4.74) | |
| Pathological radiolucency | 6 and 12 | 1 | 5.15 (0.26 to 103.31) |
| Pathological root resorption | 6 | 1 | 1.72 (0.45 to 6.61) |
| 12 | 1 | 1.29 (0.38 to 4.37) | |
| CI: confidence interval; CH: calcium hydroxide. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.01, 7.88) | |
| Radiological failure | 6 | 1 | 0.09 (0.01, 1.58) |
| 12 | 1 | 0.63 (0.23, 1.70) | |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.01, 7.88) | |
| Pathologic mobility | 6 and 12 | 1 | Not estimable* |
| Adjacent tissue inflammation | 6 and 12 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 0.43 (0.12, 1.51) | |
| Pathologic root resorption | 6 | 1 | Not estimable* |
| 12 | 0.38 (0.11, 1.28) | ||
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 1.13 (0.50, 2.53) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; CH: calcium hydroxide; NaOCl: sodium hypochlorite. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Pain | 6 | 1 | 0.25 (0.06, 1.08) |
| Soft tissue pathology | 6 | 1 | 0.33 (0.07, 1.52) |
| Pathologic mobility | 6 | 1 | 0.75 (0.30, 1.90) |
| Pathologic radiolucency | 6 | 1 | 1.14 (0.69, 1.90) |
| Pathologic root resorption | 6 | 1 | 1.20 (0.61, 2.34) |
| Pulp canal obliteration | 6 | 1 | 0.11 (0.01, 1.98) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FS: ferric sulfate. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | Not estimable* |
| 24 | 1 | 1.20 (0.42 to 3.43) | |
| Radiological failure | 6 | 1 | 0.33 (0.01 to 7.81) |
| 12 | 1 | 0.20 (0.01 to 3.97) | |
| 24 | 1 | 0.60 (0.26 to 1.40) | |
| Overall failure | 6 | 1 | 0.33 (0.01 to 7.81) |
| 12 | 1 | 0.20 (0.01 to 3.97) | |
| 24 | 1 | 0.38 (0.11 to 1.25) | |
| Pain | 6, 12 and 24 | 1 | Not estimable* |
| Pathological radiolucency | 6, 12 and 24 | 1 | Not estimable* |
| Pathological root resorption | 6 | 1 | 0.33 (0.01 to 7.81) |
| 12 | 1 | 0.33 (0.01 to 7.81) | |
| 24 | 1 | 0.17 (0.02 to 1.29) | |
| Physiological root resorption | 6 and 12 | 1 | Not estimable* |
| 24 | 1 | 1.50 (0.27 to 8.22) | |
| Pulp canal obliteration | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FS: ferric sulphate; ZOE: zinc oxide and eugenol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 3.19 (0.13 to 76.37) | |
| 24 | 1 | 5.31 (0.26 to 107.86) | |
| Radiological failure | 12 | 1 | 0.46 (0.13 to 1.66) |
| 24 | 1 | 0.61 (0.19 to 1.94) | |
| Overall failure | 12 | 1 | 0.46 (0.13 to 1.66) |
| 24 | 1 | 0.61 (0.19 to 1.94) | |
| Pain | 6, 12 and 24 | 1 | Not estimable* |
| Soft tissue pathology | 6, 12 and 24 | 1 | Not estimable* |
| Pathological mobility | 6, 12 and 24 | 1 | Not estimable* |
| Pathological radiolucency | 12 | 1 | 0.15 (0.01 to 2.86) |
| 24 | 1 | 0.71 (0.12 to 4.06) | |
| Pathological root resorption | 12 | 1 | 0.53 (0.05 to 5.67) |
| 24 | 1 | 1.06 (0.16 to 7.25) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Er:YAG: erbium:yttrium‐aluminium garnet; FS: ferric sulphate | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Pain | mean 22 | 1 | 0.25 (0.01 to 6.08) |
| Soft tissue pathology | mean 22 | 1 | 0.25 (0.01 to 6.08) |
| Pathological mobility | mean 22 | 1 | 0.15 (0.01 to 3.09) |
| Adjacent tissue inflammation | mean 22 | 1 | 0.25 (0.01 to 6.08) |
| Pathological radiolucency | mean 22 | 1 | 0.29 (0.01 to 6.92) |
| Pathological root resorption | mean 22 | 1 | 0.60 (0.31 to 1.19) |
| Pulp canal obliteration | mean 22 | 1 | 1.39 (0.78 to 2.49) |
| CI: confidence interval; FS: ferric sulphate; MTA: mineral trioxide aggregate | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 24 | 1 | 2.00 (0.19, 21.06) |
| Radiological failure | 24 | 1 | 0.80 (0.23, 2.73) |
| Overall failure | 6, 12 and 24 | 1 | 2.00 (0.19, 21.06) |
| Pain | 6, 12 and 24 | 1 | 1.00 (0.07, 15.36) |
| Soft tissue pathology | 6, 12 and 24 | 1 | 2.00 (0.19, 21.06) |
| Pathologic mobility | 6, 12 and 24 | 1 | 3.00 (0.13, 71.22) |
| Pathologic radiolucency | 24 | 1 | 1.00 (0.22, 4.62) |
| Pathologic root resorption | 24 | 1 | 0.50 (0.05, 5.27) |
| Abbreviations ‐ CI: confidence interval; PC: Portland cement; FC: formocresol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 24 | 1 | 0.67 (0.12, 3.75) |
| Radiological failure | 24 | 1 | 0.57 (0.18, 1.78) |
| Overall failure | 6, 12 and 24 | 1 | 0.67 (0.12, 3.75) |
| Pain | 6, 12 and 24 | 1 | 1.00 (0.07, 15.36) |
| Soft tissue pathology | 6, 12 and 24 | 1 | 1.00 (0.15, 6.71) |
| Pathologic mobility | 6, 12 and 24 | 1 | 0.50 (0.05, 5.27) |
| Pathologic radiolucency | 24 | 1 | 0.60 (0.16, 2.32) |
| Pathologic root resorption | 24 | 1 | 0.50 (0.05, 5.27) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; PC: Portland cement; EMD: enamel matrix derivative | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 12 | 1 | 2.90 (0.32 to 26.38) |
| Radiological failure | 12 | 1 | 1.11 (0.46 to 2.67) |
| Pain | 12 | 1 | Not estimable* |
| Pathological radiolucency | 12 | 1 | 0.97 (0.39 to 2.43) |
| Pathological root resorption | 12 | 1 | 0.97 (0.15 to 6.44) |
| *due to lack of events Abbreviations ‐ CH: calcium hydroxide; CI: confidence interval; ZOE: zinc oxide and eugenol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 0.83 (0.26, 2.73) |
| Radiological failure | 6 | 1 | 0.94 (0.47, 1.88) |
| Overall failure | 6 | 1 | 0.94 (0.47, 1.88) |
| Pain | 6 | 1 | Not estimable* |
| Soft tissue pathology | 6 | 1 | 0.83 (0.26, 2.73) |
| Pathologic mobility | 6 | 1 | Not estimable* |
| Pathologic radiolucency | 6 | 1 | 1.04 (0.43, 2.51) |
| Pathologic root resorption | 6 | 1 | 0.75 (0.28, 2.02) |
| Pulp canal obliteration | 6 | 1 | 1.04 (0.16, 6.80) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; CH: calcium hydroxide; ZOE: zinc oxide eugenol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 9 | 1 | 3.00 (0.13 to 71.22) |
| Radiological failure | 9 | 1 | 5.00 (0.62 to 40.64) |
| Pain | 6 | 1 | Not estimable* |
| Soft tissue pathology | 6 | 1 | 3.00 (0.13 to 71.22) |
| Pathological mobility | 6 | 1 | Not estimable* |
| Pathological radiolucency | 6 | 1 | 5.00 (0.25 to 100.54) |
| Pathological root resorption | 6 | 1 | 5.00 (0.25 to 100.54) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FC: formocresol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | 1.08 (0.07, 16.36) |
| Radiological failure | 6 and 12 | 1 | 0.54 (0.11, 2.70) |
| Pathological radiolucency | 6 | 1 | 2.16 (0.21, 22.38) |
| 12 | 1 | 0.54 (0.11, 2.70) | |
| Pathological root resorption | 6 | 1 | 0.36 (0.08, 1.62) |
| 12 | 1 | 0.31 (0.07, 1.35) | |
| Pulp canal obliteration | 6 | 1 | 1.39 (0.61, 3.17) |
| 12 | 1 | 1.08 (0.60, 1.94) | |
| Dentine bridge formation | 6 | 1 | Not estimable* |
| 12 | 1 | 11.85 (0.69, 203.86) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 16.41 (2.30 to 117.26) |
| 12 | 1 | 9.11 (3.04 to 27.31) | |
| Radiological failure | 6 | 1 | 24.06 (3.44 to 168.43) |
| 12 | 1 | 9.11 (3.04 to 27.31) | |
| Pain | 6 | 1 | 5.47 (0.67 to 44.34) |
| 12 | 1 | 5.47 (0.67 to 44.34) | |
| Soft tissue pathology | 6 | 1 | 7.64 (0.41 to 142.35) |
| 12 | 1 | 7.64 (0.41 to 142.35) | |
| Pathological radiolucency | 6 | 1 | 2.19 (0.21 to 22.99) |
| 12 | 1 | 2.19 (0.21 to 22.99) | |
| Pathological root resorption | 6 | 1 | 12.00 (0.69 to 208.77) |
| 12 | 1 | 5.47 (0.67 to 44.34) | |
| Abbreviations ‐ CH: calcium hydroxide; CI: confidence interval; FC: formocresol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 0.83 (0.29 to 2.38) | |
| Radiological failure | 6 | 1 | 3.00 (0.13 to 70.30) |
| 12 | 1 | 5.00 (0.25 to 99.17) | |
| 24 | 1 | 1.67 (0.71 to 3.89) | |
| Overall failure | 6 | 1 | 3.00 (0.13 to 70.30) |
| 12 | 1 | 5.00 (0.25 to 99.17) | |
| 24 | 1 | 2.67 (0.80 to 8.90) | |
| Pain | 6, 12 and 24 | 1 | Not estimable* |
| Pathological radiolucency | 6, 12 and 24 | 1 | Not estimable* |
| Pathological root resorption | 6 | 1 | 3.00 (0.13 to 70.30) |
| 12 | 1 | 3.00 (0.13 to 70.30) | |
| 24 | 1 | 6.00 (0.78 to 46.29) | |
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 0.20 (0.01 to 3.97) | |
| 24 | 1 | 0.20 (0.01 to 3.97) | |
| Physiological root resorption | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 2.00 (0.19 to 20.67) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FC: formocresol; ZOE: zinc oxide and eugenol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 3.19 (0.13 to 76.37) | |
| 24 | 1 | 2.13 (0.20 to 22.70) | |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 | 1 | 1.60 (0.28 to 9.13) | |
| 24 | 1 | 1.06 (0.28 to 4.01) | |
| Overall failure | 6 | 1 | Not estimable* |
| 12 | 1 | 1.60 (0.28 to 9.13) | |
| 24 | 1 | 1.06 (0.28 to 4.01) | |
| Pain | 6, 12 and 24 | 1 | Not estimable* |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | Not estimable* | |
| 24 | 1 | 0.35 (0.01 to 8.49) | |
| Pathological mobility | 6, 12 and 24 | 1 | Not estimable* |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 0.21 (0.01 to 4.31) | |
| 24 | 1 | 1.06 (0.16 to 7.25) | |
| Pathological root resorption | 6 | 1 | Not estimable* |
| 12 | 1 | 3.19 (0.13 to 76.37) | |
| 24 | 1 | 1.06 (0.16 to 7.25) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Er:YAG: erbium:yttrium‐aluminium garnet; FC: formocresol | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 0.33 (0.01, 7.95) | |
| Radiological failure | 6 | 1 | 1.67 (0.43, 6.51) |
| 12 | 1 | 2.00 (0.75, 5.33) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; FC: formocresol. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 and 12 | 1 | 0.33 (0.01, 7.58) |
| 24 | 1 | 1.00 (0.16, 6.20) | |
| Radiological failure | 6 and 12 | 1 | 1.00 (0.16, 6.20) |
| 24 | 1 | 0.67 (0.13, 3.44) | |
| Pain | 6 and 12 | 1 | 0.33 (0.01, 7.58) |
| 24 | 1 | 1.00 (0.16, 6.20) | |
| Soft tissue pathology | 6, 12 and 24 months | 1 | 0.33 (0.01, 7.58) |
| Pathologic mobility | 6, 12 and 24 months | 1 | 0.33 (0.01, 7.58) |
| Pathological radiolucency | 6 and 12 | 1 | Not estimable* |
| Pathological root resorption | 6 and 12 | 1 | 1.00 (0.16, 6.20) |
| 24 | 1 | 0.67 (0.13, 3.44) | |
| *due to lack of events Abbreviation ‐ CI: confidence interval | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 1.00 (0.07 to 14.90) |
| 12 | 1 | 0.50 (0.10 to 2.43) | |
| Radiological failure | 6 and 12 | 1 | 0.50 (0.10 to 2.43) |
| Pain | 6 and 12 | 1 | 1.00 (0.07 to 14.90) |
| Pathological mobility | 6 and 12 | 1 | 1.00 (0.07 to 14.90) |
| Pathological radiolucency | 6 and 12 | 1 | 0.20 (0.01 to 3.92) |
| Pathological root resorption | 6 and 12 | 1 | 5.00 (0.26 to 98.00) |
| Filling material anomaly | 6 and 12 | 1 | Not estimable* |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Sealapex: eugenol‐free CH; CH: calcium hydroxide. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 0.33 (0.01 to 7.72) |
| 12 | 1 | 0.11 (0.01 to 1.94) | |
| Radiological failure | 6 and 12 | 1 | 0.11 (0.01 to 1.94) |
| Pain | 6 and 12 | 1 | 0.33 (0.01 to 7.72) |
| Pathological mobility | 6 and 12 | 1 | 0.33 (0.01 to 7.72) |
| Pathological radiolucency | 6 and 12 | 1 | 0.20 (0.01 to 3.92) |
| Pathological root resorption | 6 and 12 | 1 | Not estimable* |
| Filling material anomaly | 6 and 12 | 1 | 3.00 (0.13 to 69.52) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Vitapex: CH/iodoform; CH: calcium hydroxide. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 0.33 (0.01 to 7.72) |
| 12 | 1 | 0.20 (0.01 to 3.92) | |
| Radiological failure | 6 and 12 | 1 | 0.20 (0.01 to 3.92) |
| Pain | 6 and 12 | 1 | 0.33 (0.01 to 7.72) |
| Pathological mobility | 6 and 12 | 1 | 0.33 (0.01 to 7.72) |
| Pathological radiolucency | 6 and 12 | 1 | Not estimable* |
| Pathological root resorption | 6 and 12 | 1 | 0.20 (0.01 to 3.92) |
| Filling material anomaly | 6 and 12 | 1 | 3.00 (0.13 to 69.52) |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Vitapex: CH/iodoform; CH: calcium hydroxide; Sealapex: eugenol‐free CH. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 1.0 (0.07 to 15.12) | |
| Radiological failure | 6 | 1 | 1.25 (0.38 to 4.12) |
| 12 | 1 | 1.83 (0.80 to 4.19) | |
| Pain | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 70.30) | |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | 1.0 (0.07 to 15.12) | |
| Pathological mobility | 6 and 12 | 1 | Not estimable* |
| Pathological radiolucency | 6 | 1 | 1.50 (0.27 to 8.22) |
| 12 | 1 | 2.75 (1.01 to 7.48) | |
| Pathological root resorption | 6 and 12 | 1 | 0.20 (0.01 to 3.97) |
| Pulp canal obliteration | 6 | 1 | Not estimable* |
| 12 | 1 | 0.20 (0.01 to 3.97) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Vitapex: CH/iodoform; CH: calcium hydroxide; 3Mix: ciprofloxacin + metronidazole + minocycline. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 | 1 | 21.79 (1.32, 360.78) | |
| Radiological failure | 6 | 1 | 6.63 (0.35, 125.41) |
| 12 | 1 | 42.63 (2.65, 685.54) | |
| *due to lack of events Abbreviations ‐ CI: confidence interval; Vitapex: CH/iodoform; MPRCF: ZOE (zinc oxide eugenol), calcium hydroxide, iodoform. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Pain | 24 | 1 | 1.80 (0.07 to 43.88) |
| Soft tissue pathology | 24 | 1 | 4.21 (0.22 to 80.70) |
| Pathological radiolucency | 24 | 1 | 0.60 (0.25 to 1.46) |
| Pathological root resorption | 24 | 1 | 21.04 (1.28 to 346.39) |
| Pulp canal obliteration | 24 | 1 | 27.05 (1.66 to 441.49) |
| Abbreviations ‐ CI: confidence interval; FS: ferric sulphate; Sedanol=ZOE: zinc oxide and eugenol. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 3.00 (0.13, 70.83) |
| 12 | 1 | 5.00 (0.25, 99.95) | |
| Pain | 6 | 1 | 3.00 (0.13, 70.83) |
| 12 | 1 | 5.00 (0.25, 99.95) | |
| Soft tissue pathology | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13, 70.83) | |
| Pathologic mobility | 6 and 12 | 1 | 3.00 (0.13, 70.83) |
| Pathologic radiolucency | 6 | 1 | 23.00 (1.42, 373.46) |
| 12 | 1 | 11.00 (0.64, 190.53) | |
| *due to lack events Abbreviations ‐ CI: confidence interval; 3Mix: ciprofloxacin + metronidazole + minocycline. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 24 | 1 | 3.83 (1.68 to 8.74) |
| Radiological failure | 24 | 1 | 3.11 (1.61 to 6.02) |
| Pain | 6 | 1 | 7.00 (0.37 to 132.66) |
| 12 | 1 | 9.00 (0.50 to 163.59) | |
| 24 | 1 | 4.00 (0.89 to 18.06) | |
| Soft tissue pathology | 6 | 1 | 7.00 (0.37 to 132.66) |
| 12 | 1 | 2.5 (0.50 to 12.39) | |
| 24 | 1 | 1.8 (0.64 to 5.06) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 4.00 (0.46 to 34.75) | |
| 24 | 1 | 5.00 (1.14 to 21.86) | |
| Pathological root resorption | 6 | 1 | Not estimable* |
| 12 | 1 | 3.33 (0.96 to 11.51) | |
| 24 | 1 | 2.00 (0.87 to 4.60) | |
| *due to lack of events Abbreviations ‐ CH: calcium hydroxide; CI: confidence interval; FC: formocresol. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 69.52) | |
| 24 | 1 | 7.00 (0.38 to 127.33) | |
| Pain | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 69.52) | |
| 24 | 1 | 7.00 (0.38 to 127.33) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviations ‐ CH: calcium hydroxide; CI: confidence interval | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 24 | 1 | 3.00 (0.13 to 69.52) |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pain | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviations ‐ CH: calcium hydroxide; CI: confidence interval | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Radiological failure | 6 and 12 | 1 | 3.00 (0.13 to 69.52) |
| 24 | 1 | 7.00 (0.38 to 127.33) | |
| Pain | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviation ‐ CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 24 | 1 | 3.00 (0.13 to 69.52) |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pain | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviation ‐ CI: confidence interval | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 69.52) | |
| 24 | 1 | 7.00 (0.38 to 127.33) | |
| Pain | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 69.52) | |
| 24 | 1 | 7.00 (0.38 to 127.33) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviations ‐ CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6, 12 and 24 | 1 | 3.00 (0.13 to 69.52) |
| Radiological failure | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 1.00 (0.07 to 14.90) | |
| Pain | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 3.00 (0.13 to 69.52) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 and 24 | 1 | 1.00 (0.07 to 14.90) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviation ‐ CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 6 | 1 | 3.00 (0.13 to 69.52) |
| 12 and 24 | 1 | 1.00 (0.07 to 14.90) | |
| Radiological failure | 6 | 1 | 0.33 (0.01 to 7.72) |
| 12 | 1 | 1.00 (0.07 to 14.90) | |
| 24 | 1 | 0.33 (0.04 to 2.94) | |
| Pain | 6 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13 to 69.52) | |
| 24 | 1 | 1.00 (0.07 to 14.90) | |
| Pathological radiolucency | 6 | 1 | Not estimable* |
| 12 | 1 | 1.00 (0.07 to 14.90) | |
| 24 | 1 | 0.33 (0.04 to 2.94) | |
| Pathological root resorption | 6, 12 and 24 | 1 | Not estimable* |
| *due to lack of events Abbreviation ‐ CI: confidence interval. | |||
| Outcome | Time point (months) | No. of studies | Risk ratio (95% CI) |
| Clinical failure | 1, 3, 6 | 1 | 5.00 (0.26, 98.00) |
| 9 | 1 | 7.00 (0.38, 127.32) | |
| 12 | 1 | 4.00 (0.49, 32.72) | |
| Radiological failure | 1, 3, 6 | 1 | 5.00 (0.26, 98.00) |
| 9 | 1 | 3.00 (0.34, 26.45) | |
| 12 | 1 | 1.67 (0.46, 6.06) | |
| Pain | 1, 3, 6, 9 | 1 | Not estimable* |
| 12 | 1 | 3.00 (0.13, 69.52) | |
| Soft tissue pathology | 1, 3, 6, 9 | 1 | 5.00 (0.26, 98.00) |
| 12 | 1 | 2.00 (0.20, 20.33) | |
| Pathologic mobility | 1, 3, 6, 9 | 1 | 5.00 (0.26, 98.00) |
| 12 | 1 | 2.00 (0.20, 20.33) | |
| Pathologic radiolucency | 1, 3, 6 | 1 | 5.00 (0.26, 98.00) |
| 9 | 1 | 3.00 (0.34, 26.45) | |
| 12 | 1 | 1.33 (0.34, 5.21) | |
| Pathologic root resorption | 1, 3, 6 | 1 | 5.00 (0.26, 98.00) |
| 9 | 1 | 2.00 (0.20, 20.33) | |
| 12 | 1.33 (0.34, 5.21) | ||
| *due to lack of events Abbreviation ‐ CI: confidence interval. | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 13 | 1048 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.07, 1.89] |
| 1.2 12 months | 12 | 740 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.10, 0.93] |
| 1.3 24 months | 9 | 548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.18, 1.19] |
| 2 Radiological failure Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 12 | 922 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.17, 0.86] |
| 2.2 12 months | 12 | 740 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.19, 0.89] |
| 2.3 24 months | 9 | 548 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.22, 0.80] |
| 3 Overall failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 6 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.04, 1.32] |
| 3.2 12 months | 6 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.17, 1.36] |
| 3.3 24 months | 7 | 368 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.25, 1.01] |
| 4 Pain Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 6 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 4.2 12 months | 6 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.18] |
| 4.3 24 months | 4 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.14, 3.56] |
| 5 Soft tissue pathology Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 7 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5.2 12 months | 7 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 1.01] |
| 5.3 24 months | 5 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.10] |
| 6 Pathological mobility Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 5 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 6.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pathological radiolucency Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 13 | 1010 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.27, 1.08] |
| 7.2 12 months | 11 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.19, 0.98] |
| 7.3 24 months | 8 | 460 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.25, 1.22] |
| 8 Pathological root resorption Show forest plot | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 11 | 866 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.18, 1.21] |
| 8.2 12 months | 9 | 508 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.07, 1.03] |
| 8.3 24 months | 6 | 338 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.08, 0.81] |
| 9 Pulp canal obliteration Show forest plot | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 6 months | 9 | 712 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.00, 2.30] |
| 9.2 12 months | 7 | 410 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.70 [0.81, 3.57] |
| 9.3 24 months | 6 | 338 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [1.07, 3.94] |
| 10 Dentin bridge formation Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 6 months | 3 | 322 | Risk Ratio (M‐H, Fixed, 95% CI) | 18.16 [3.63, 90.91] |
| 10.2 12 months | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.76, 47.22] |
| 10.3 24 months | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.76, 47.22] |
| 11 Physiological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 6 months | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 12 months | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 24 months | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.81] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 6 | 538 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.09, 5.64] |
| 1.2 12 months | 5 | 432 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.12, 1.68] |
| 1.3 24 months | 3 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.14] |
| 2 Radiological failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 4 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.05, 1.79] |
| 2.2 12 months | 5 | 432 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.08, 0.98] |
| 2.3 24 months | 3 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.06, 0.67] |
| 3 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 3.2 12 months | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.18] |
| 3.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.14] |
| 4 Soft tissue pathology Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 4.2 12 months | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.18] |
| 4.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5 Pathological radiolucency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 4 | 388 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 2.95] |
| 5.2 12 months | 4 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.16, 2.38] |
| 5.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.11, 1.95] |
| 6 Pathological root resorption Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 3 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 1.95] |
| 6.2 12 months | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 6.3 24 months | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.02, 0.98] |
| 7 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 192 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 12 months | 2 | 192 | Risk Ratio (M‐H, Fixed, 95% CI) | 12.76 [0.79, 206.70] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 8 | 560 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 3.06] |
| 1.2 12 months | 7 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.28] |
| 1.3 24 months | 6 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.18, 1.42] |
| 2 Radiological failure Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 8 | 560 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.17, 1.03] |
| 2.2 12 months | 7 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.20, 1.53] |
| 2.3 24 months | 6 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.31, 1.46] |
| 3 Pain Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 24 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.30] |
| 4 Soft tissue pathology Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 5 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 4 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.65] |
| 4.3 24 months | 3 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.72] |
| 5 Pathological mobility Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 4 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 5.3 24 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathological radiolucency Show forest plot | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 9 | 622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.30, 1.27] |
| 6.2 12 months | 7 | 320 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.13, 1.02] |
| 6.3 24 months | 6 | 270 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.23, 1.57] |
| 7 Pathological root resorption Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 8 | 550 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.24, 1.99] |
| 7.2 12 months | 6 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.05, 1.14] |
| 7.3 24 months | 4 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.10, 1.92] |
| 8 Pulp canal obliteration Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 7 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.00, 2.30] |
| 8.2 12 months | 5 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.44, 2.26] |
| 8.3 24 months | 5 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [0.99, 3.89] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.31] |
| 1.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 1.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.20, 1.39] |
| 2 Radiological failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.40] |
| 2.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.15, 3.44] |
| 2.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.25, 1.36] |
| 3 Overall failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.40] |
| 3.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.15, 3.44] |
| 3.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.32, 1.89] |
| 4 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.00] |
| 4.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.00] |
| 6 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.31] |
| 7 Pathologic radiolucency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.48] |
| 7.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.81] |
| 7.3 24 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 8 Pathological root resorption Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 4 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.01, 0.53] |
| 8.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 8.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.12, 2.51] |
| 9 Pulp canal obliteration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 6 months | 3 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 12 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.30] |
| 9.3 24 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.47, 5.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.85] |
| 1.2 12 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.04, 0.70] |
| 1.3 24 months | 5 | 284 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.12, 0.52] |
| 2 Radiological failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.02, 0.41] |
| 2.2 12 months | 4 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.04, 0.36] |
| 2.3 24 months | 5 | 284 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.08, 0.26] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.92] |
| 3.2 12 months | 2 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.10, 1.19] |
| 3.3 24 months | 2 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 0.95] |
| 4 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 24 months | 2 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.09, 1.73] |
| 5 Soft tissue pathology Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.62] |
| 5.2 12 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.62] |
| 5.3 24 months | 4 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.06, 0.47] |
| 6 Pathological mobility Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.62] |
| 6.2 12 months | 3 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 0.66] |
| 6.3 24 months | 4 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 0.66] |
| 7 Pathological radiolucency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 4 | 162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.02, 0.50] |
| 7.2 12 months | 4 | 162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.04, 0.47] |
| 7.3 24 months | 5 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.03, 0.22] |
| 8 Pathological root resorption Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 5 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.02, 0.39] |
| 8.2 12 months | 5 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.02, 0.29] |
| 8.3 24 months | 6 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.03, 0.18] |
| 9 Pulp canal obliteration Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 6 months | 3 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.77 [1.56, 38.69] |
| 9.2 12 months | 3 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.01 [0.97, 4.17] |
| 9.3 24 months | 4 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [1.01, 4.19] |
| 10 Dentin bridge formation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.05, 0.84] |
| 10.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.37, 1.74] |
| 10.3 24 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.37, 1.74] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 1.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 1.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 2 Radiological failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.10, 2.56] |
| 3 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 3.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 3.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 4 Soft tissue pathology Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 4.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 4.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 5 Pathologic mobility Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 5.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 6 Pathological radiolucency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.75] |
| 7 Pathological root resorption Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 12 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 24 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 8 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.49, 1.08] |
| 8.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.60, 1.14] |
| 8.3 24 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.71, 1.29] |
| 9 Dentin bridge formation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.43] |
| 9.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.61, 3.71] |
| 9.3 24 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.61, 3.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 4 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.42, 6.99] |
| 1.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.16, 3.62] |
| 2 Radiological failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 4 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.40 [0.65, 8.84] |
| 2.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.22, 5.27] |
| 3 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 98.00] |
| 4 Soft tissue pathology Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 98.00] |
| 5 Pathologic mobility Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 98.00] |
| 6 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.46 [0.15, 81.36] |
| 6.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.19, 6.27] |
| 7 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.32 [0.22, 24.09] |
| 7.2 12 months | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.30, 4.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.98 [1.17, 3.37] |
| 1.2 12 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.87 [1.22, 2.89] |
| 1.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [0.78, 6.11] |
| 2 Radiological failure Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 4 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.48 [3.86, 62.06] |
| 2.2 12 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [1.42, 2.44] |
| 2.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.63 [1.73, 7.61] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 12 months | 2 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.41 [0.80, 7.21] |
| 3.2 24 months | 2 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.93 [1.35, 6.34] |
| 4 Pain Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 4 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.18 [0.35, 29.08] |
| 4.2 12 months | 4 | 276 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.30 [1.15, 34.40] |
| 5 Soft tissue pathology Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.14 [0.63, 42.25] |
| 5.2 12 months | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.77 [1.23, 37.10] |
| 5.3 24 months | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.64 [0.51, 13.55] |
| 6 Pathological mobility Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 4 | 238 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.18, 8.19] |
| 6.2 12 months | 4 | 238 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.40, 3.31] |
| 6.3 24 months | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.0 [0.53, 153.79] |
| 7 Pathological radiolucency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 3 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.78 [0.64, 22.17] |
| 7.2 12 months | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [0.67, 5.40] |
| 7.3 24 months | 2 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.79, 13.28] |
| 8 Pathological root resorption Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 4 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.87 [2.33, 60.40] |
| 8.2 12 months | 6 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.25 [2.04, 19.14] |
| 8.3 24 months | 3 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.59 [1.33, 15.81] |
| 9 Pulp canal obliteration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 6 months | 2 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.0 [0.47, 33.75] |
| 9.2 12 months | 3 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.68 [0.91, 7.95] |
| 10 Dentin bridge formation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 6 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 13.0 [1.81, 93.60] |
| 10.2 12 months | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 14.0 [1.95, 100.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.4 [0.14, 81.38] |
| 1.2 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.41 [0.37, 31.61] |
| 1.3 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.44 [0.90, 13.18] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.53, 3.13] |
| 2.2 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [1.04, 3.75] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.53, 3.13] |
| 3.2 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [1.04, 3.75] |
| 4 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 12 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.05, 6.05] |
| 4.2 24 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [0.60, 8.66] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 7 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.87] |
| 1.2 12 months | 7 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.45, 4.27] |
| 1.3 24 months | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.40, 1.70] |
| 2 Radiological failure Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 6 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.32, 1.92] |
| 2.2 12 months | 7 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.73, 2.42] |
| 2.3 24 months | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.71, 2.24] |
| 3 Overall failure Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 4 | 184 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.12, 2.37] |
| 3.2 12 months | 5 | 284 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.51, 2.64] |
| 3.3 24 months | 4 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.74, 3.01] |
| 4 Pain Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 4.2 12 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 4.3 24 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.85] |
| 5 Pathological radiolucency Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 12 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.8 [0.40, 8.17] |
| 5.2 24 months | 4 | 230 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.2 [0.51, 9.50] |
| 6 Pathological root resorption Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 5 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.84] |
| 6.2 12 months | 6 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.53, 5.08] |
| 6.3 24 months | 5 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.50, 2.96] |
| 7 Pulp canal obliteration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 3 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 12 months | 3 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.54, 1.64] |
| 7.3 24 months | 2 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.28, 5.54] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.39 [0.22, 87.82] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.22, 1.39] |
| 2.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.17, 1.02] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.01, 6.91] |
| 5 Adjacent tissue inflammation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.03, 2.91] |
| 6 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.06, 13.35] |
| 7.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.07, 4.17] |
| 8 Pathologic root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.18, 1.42] |
| 8.2 12 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.15, 1.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.04, 1.30] |
| 1.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.02, 1.62] |
| 2 Radiological failure Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 3 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.38, 2.12] |
| 2.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.44, 1.92] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.60] |
| 4 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.08] |
| 5 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.29, 7.73] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.34] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.38, 4.12] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.34] |
| 4 Pathological mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.2 [0.54, 8.88] |
| 6 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.37, 4.27] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.16, 6.20] |
| 2.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.34, 2.23] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.71] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.27, 8.43] |
| 5 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.75] |
| 7 Pathologic root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 96.13] |
| 7.2 12 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.70] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.19, 2.18] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.70] |
| 4 Pathological mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.19, 2.18] |
| 7 Pulp canal obliteration Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.33, 5.08] |
| 2.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [0.52, 6.59] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pathologic root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.33, 5.08] |
| 7.2 12 months | 2 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [0.52, 6.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.23, 2.83] |
| 2 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.92] |
| 3 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.06] |
| 4 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 96.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.5 [0.50, 12.50] |
| 2 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 6.90] |
| 3 Pathological mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 6.90] |
| 4 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.72] |
| 5 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.08, 4.29] |
| 1.2 12 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.15, 3.33] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.27] |
| 2.2 12 months | 2 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clincal failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.79, 5.15] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 4 Soft tissue pathology Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.58] |
| 5 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Pathological radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.79, 5.15] |
| 7 Pathological root resorption Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 6 months | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.84] |
| 1.2 12 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.75 [1.21, 18.55] |
| 2 Radiological failure Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.36 [0.86, 6.50] |
| 2.2 12 months | 4 | 287 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.56 [2.58, 16.67] |
| 3 Overall failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.63, 5.66] |
| 3.2 12 months | 2 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.56 [0.89, 7.32] |
| 4 Pain Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 12 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pathological mobility Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.84] |
| 5.2 12 months | 3 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.05, 1.50] |
| 2 Radiological failure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.05, 1.50] |
| 3 Pain Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.05, 1.50] |
| 4 Pathologic mobility Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.25] |
| 5 Pathologic radiolucency Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 6 months | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.11, 3.63] |

