Terapia electromagnética para el tratamiento de las úlceras por presión
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | RCT | |
| Participants | 30 (13 M;17 F) patients in an elderly care unit with either Stage II (16 participants) or Stage III (14 participants) pressure ulcer. Ulcers were located on the buttocks (9), sacrum (8), knee (6), coxal (2), back (3), heel(1) and leg (1). | |
| Interventions | Group 1: (n = 20) Diapulse® plus conventional therapy* *Conventional therapy consisted of H2O2 cleansing and local applications of talcum powder, methylene blue in solution and tetracycline ointments | |
| Outcomes | The outcomes assessed were proportion of ulcers healed and time to complete healing PRIMARY OUTCOMES: b) Rate of change in ulcer area: Not assessed in this study c)Time to complete healing (weeks): SECONDARY OUTCOMES: The trial had no loss to follow up | |
| Notes | No report of concurrent pressure relief used, such as support surfaces (bed, mattresses and cushions). Locations of wounds were provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: allocation to the 3 treatment groups was described as "randomly organized" but there was no description of how randomisation was achieved. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the process of allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Comment: whilst "technician in charge , nor the clinician" were reportedly blinded to Diapulse® and sham therapy, it would not have been possible to blind the third group. There was also no information on whether the outcome assessor was blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Comment: reported no loss to follow up. |
| Selective reporting (reporting bias) | Unclear risk | Comment: outcomes to be assessed were not stated in the methods section of the article, therefore it was not clear whether the trial included all planned outcomes. No access to trial protocol. |
| Other bias | Unclear risk | The median baseline ulcer area varied between the 3 groups. This difference may bias the evaluation in favour of the Diapulse® group as this group has the lowest value (ulcer size). |
| Methods | RCT | |
| Participants | 30 (30 M) inpatients with spinal cord compression and a Stage II (n = 20) or Stage III (n = 10) pressure ulcer. Grading defined by authors. Patients in both stage II and III were allocated in equal numbers to the control and intervention groups. Baseline features: Reported ‐ duration of ulcers prior to admission, degree of edema, erythema, epithelialization, and ulcer size. Satge II patients there was no statistically significant difference for the baseline parameters between the 10 in the EMT group and the 10 in the sham group. But the randomisation process did not provide for an even distribution of large pressure ulcers. No data were reported on baseline parameters from the 10 patients with Satge II pressure ulcers. | |
| Interventions | Group 1: (n = 15) electromagnetic energy at a frequency of 27.12 MHz, pulse repetition 80 to 600 pps, pulse width 65 microseconds, per pulse power range of 293 and 975 peak watts ‐ delivered through wound dressing, 30 minutes treatment 2 x daily for 12 weeks. Group 2: (n = 15) sham treatment as above. All ulcers were dressed with moist saline gauze. | |
| Outcomes | The outcomes assessed were proportion of ulcers healed, percent of ulcers healed (defined as reduction in wound surface area from the initial measurements) and time to complete healing. PRIMARY OUTCOMES: b) Percent reduction in ulcers surface area at 1 week: Percent overall reduction (SD): (this result was presented in the discussion section of the paper) c) Time to complete healing in days (median): SECONDARY OUTCOMES: The trial has 1 loss to follow up in the EMT group after week 1 | |
| Notes | No report of concurrent pressure relief used, such as support surfaces (bed, mattresses and cushions) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: allocation to the treatment groups was described as "randomly assigned to receive therapy from either an active or control sham" but there was no description of how randomisation was achieved |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the process of allocation |
| Blinding (performance bias and detection bias) | Unclear risk | Comment: "Patients, staff and authors were blinded to the identity of the functioning unit" and the sham unit was identical in operation, appearance, and sound to the active unit, the study described that the outcomes were assessed by a single observer. It was unclear if this assessor was blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Comment: the trial had one loss to follow up after the outcome was assessed, week 1 (the outcomes were reported at week 1) |
| Selective reporting (reporting bias) | Unclear risk | Comment: subset of patients with Stage II pressure ulcers less than or equal to 60 cm2 and ulcer size more than 60 cm2 were analysed separately. Stage II and Stage III patients were also analysed separately. These analyses were not prespecified in the methods section but may have been planned. |
| Other bias | Unclear risk | Comment: baseline data were provided only for patients with Stage II but not for patients with Stage III pressure ulcers |
Abbreviations:
H2O2 = hydrogen peroxide
n = number in sample group
pps = pulses per second
x = times
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| In the initial assessment, the title of article seemed relevant to the objective of the review. The abstract of the study was unavailable. We requested the article via an interlibrary loan and direct contact with the author and the journal publisher (Journal of American Paraplegia Society), all of which were unsuccessful. Therefore, this study was excluded for pragmatic reasons because its content could not be verified firsthand. | |
| This study assessed wound healing of the donor site | |
| Bates‐Jensen wound assessment tool (also known as Pressure Sore Status Tool ) was used to assess the main outcome measure. Data to validate the use of this tool to assess wound healing are still limited. | |
| Not a controlled trial | |
| Not a controlled trial. This study did not meet the inclusion criteria as it evaluated the effectiveness of pulsed electromagnetic energy in the treatment of pressure ulcers using 4 different protocols (treatment plans). | |
| This study did not meet the inclusion criteria as it examined micro current stimulation therapy and not electromagnetic therapy |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcers healed within 8 weeks of treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Pressure ulcers healed within 8 weeks of treatment. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcers healed within 8 weeks of treatment duration Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Electromagnetic therapy versus standard therapy alone, Outcome 1 Pressure ulcers healed within 8 weeks of treatment duration. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Healed ulcers at one week Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.97, 50.38] |
| Analysis 3.1  Comparison 3 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Healed ulcers at one week. | ||||
| 1.1 Stage II ulcers | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.41, 120.16] |
| 1.2 Stage III ulcers | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.45, 108.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Percent reduction in wound surface area at one week Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 37.0 [17.36, 56.64] |
| Analysis 4.1  Comparison 4 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Percent reduction in wound surface area at one week. | ||||
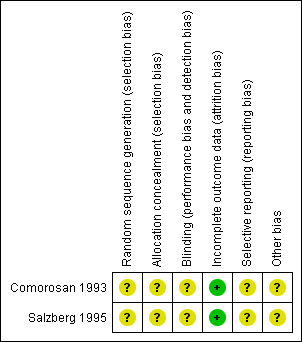
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Comparison 1 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Pressure ulcers healed within 8 weeks of treatment.

Comparison 2 Electromagnetic therapy versus standard therapy alone, Outcome 1 Pressure ulcers healed within 8 weeks of treatment duration.

Comparison 3 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Healed ulcers at one week.

Comparison 4 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Percent reduction in wound surface area at one week.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcers healed within 8 weeks of treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcers healed within 8 weeks of treatment duration Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Healed ulcers at one week Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.97, 50.38] |
| 1.1 Stage II ulcers | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.41, 120.16] |
| 1.2 Stage III ulcers | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.45, 108.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Percent reduction in wound surface area at one week Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 37.0 [17.36, 56.64] |

