Terapia electromagnética para el tratamiento de las úlceras por presión
Resumen
Antecedentes
Las úlceras por presión se definen como áreas "de daño localizado en la piel y el tejido subyacente causado por presión, cizallamiento, fricción o la combinación de estos". La terapia electromagnética (TEM), en la que los electrodos producen un campo electromagnético a través de la herida, puede mejorar la cicatrización de heridas crónicas como las úlceras por presión.
Objetivos
Evaluar los efectos de la TEM en la cicatrización de las úlceras por presión.
Métodos de búsqueda
Para esta actualización se hicieron búsquedas en el Registro Especializado del Grupo Cochrane de Heridas (Cochrane Wounds Group) (búsqueda 10 de junio de 2015); el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL) (The Cochrane Library 2015, número 6); Ovid MEDLINE (2014 hasta 10 de junio de 2015); Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations, 10 de junio de 2015); Ovid EMBASE (2014 hasta 10 de junio de 2015); y EBSCO CINAHL (2014 hasta 6 de julio de 2012).
Criterios de selección
Ensayos controlados aleatorizados que compararon el TEM con TEM simulada u otro tratamiento (estándar).
Obtención y análisis de los datos
Para esta actualización, dos autores de la revisión, de forma independiente, examinaron los resultados de la búsqueda para identificar los ECA pertinentes y obtuvieron los informes completos de los estudios potencialmente elegibles. En las versiones anteriores de la revisión se intentó obtener los datos que faltaban a través del contacto con los autores de los estudios. Un segundo autor de la revisión comprobó la extracción de datos y los desacuerdos se resolvieron tras la discusión entre los autores de la revisión.
Resultados principales
No se identificaron nuevos ensayos en esta actualización. En la revisión original se incluyeron dos ensayos controlados aleatorizados (ECA), con 60 participantes, con riesgo de sesgo incierto. Ambos ensayos compararon el uso de TEM con TEM simulada, aunque uno de los ensayos incluyó un tercer brazo en el que sólo se aplicó terapia estándar. Ninguno de los dos estudios encontró una diferencia estadísticamente significativa en la curación completa de los pacientes tratados con TEM en comparación con los del grupo control. En un ensayo que evaluó la reducción porcentual de la superficie de la herida, se informó de que la diferencia entre los dos grupos fue estadísticamente significativa a favor de la TEM. Sin embargo, este resultado se debe interpretar con cuidado, ya que se trata de un estudio pequeño y este hallazgo se puede deber al azar. Además, el resultado, la reducción porcentual del área de la herida, es menos significativo clínicamente que la cicatrización completa.
Conclusiones de los autores
Los resultados no proporcionan evidencia sólida de un efecto beneficioso del uso de la TEM para tratar las úlceras por presión. Sin embargo, no se puede descartar la posibilidad de un efecto beneficioso o perjudicial porque sólo se incluyeron dos ensayos, ambos con limitaciones metodológicas y un número reducido de participantes. Se recomienda la realización de estudios de investigación adicionales.
PICOs
Resumen en términos sencillos
Terapia electromagnética para el tratamiento de las úlceras por presión
Las úlceras por presión (también llamadas escaras, úlceras de decúbito o úlceras por compresión) son úlceras en la piel causadas por la presión o el roce. Suelen afectar a los pacientes con inmovilidad en las partes óseas de sus cuerpos como caderas, talones y codos, y tardan mucho tiempo en curarse. La terapia electromagnética no es una forma de radiación o calentamiento, sino que utiliza un campo electromagnético con el objetivo de estimular la cicatrización. Sin embargo, la revisión de los ensayos concluyó que no hay evidencia sólida de que la terapia electromagnética ayude u impida la cicatrización de las úlceras por presión.
Authors' conclusions
Background
Description of the condition
According to the European Pressure Ulcer Advisory Panel (EPUAP) and National Pressure Ulcer Advisory Panel (NPUAP), a pressure ulcer (also known as bed sore, bed ulcer, decubitus ulcer or pressure sore) is "an area of localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear" (EPUAP‐NPUAP 2009). Pressure ulcers usually develop on skin that covers bony areas such as the sacrum, heels, hips and elbows. Most often the ulcers develop in immobile elderly people (for example, elderly orthopaedic patients), patients with severe, acute illnesses (such as in people in intensive care units) and in people with neurological problems (for example, those with spinal cord injuries).
One cross‐sectional European study involving five countries found that the overall prevalence of pressure ulcers was approximately 18% of hospital patients (EPUAP 2002). In the UK, pressure ulcers have been recorded in 5% to 32% of patients admitted to a District General Hospital (the precise rate depends on case‐mix), and in 4% to 7% of patients in community settings (Kaltenthaler 2001). These ulcers represent a major burden of sickness and reduce quality of life for patients and their carers. There is also a considerable cost both to the patients (Clark 1994) and the health service (Touche Ross 1993). The annual treatment cost of pressure ulcers has been estimated to range from £1.4 to 2.1 billion, or 4% of total healthcare expenditure in the UK (Bennett 2004).
Pressure ulcers present as a continuum of tissue damage from unbroken skin with sustained redness after the release of pressure (non‐blanching erythema) to destruction of the muscle and bone.
The treatment of pressure ulcers has four main elements:
-
local treatment of wounds using wound dressings and other topical applications;
-
pressure relief using beds, mattresses or cushions, and repositioning of the patient;
-
treatment of concurrent conditions that may delay healing, e.g. poor nutrition and infection; and
-
use of physical therapies, such as electrical stimulation, ultrasound and laser therapy.
Description of the intervention
Recently there has been an increasing interest in the therapeutic use of electromagnetic fields for various medical conditions, including pressure ulcers (Markov 2007). Electromagnetic therapy (EMT), also known as electromagnetism, bioelectricity, magneto biology, magnetic healing and magnetic field therapy, uses electromagnetic energy applied to the body to treat various medical conditions, from bone and cartilage repair (Haddad 2007; Ryaby 1998) to pain relief (Shupak 2006; Thomas 2007), wound healing (Comorosan 1993; Kenkre 1996; Stiller 1992) and relatively new applications such as chronic musculoskeletal pain (Thomas 2007). EMT does not use direct electrical effects or radiation, unlike other forms of electrotherapy, but induces a field effect (Stiller 1992). A number of devices (e.g. Diapulse®, SoffPulse®, Pulsatron®) have been constructed to deliver a pulsed electromagnetic field (PEMF) in the radio frequency band. The frequency of short‐wavelength radio waves ranges from 10 to 100 MHz and the frequency commonly used in EMT is 27.12 MHz.
PEMFs are produced with an "on‐off" effect of pulsing current to produce effects which, it has been suggested, influence many biological processes, and thus may be useful for wound healing. The main advantage of PEMF compared with continuous fields is that the short duration of the pulses protects the tissues against potential damage from heat generated by continuous fields (Athanasiou 2007; Kitchen 2002).
How the intervention might work
There are several theories that explain how the PEMF may exert its effect on tissue generation and cell proliferation in wound healing. Lee 1993 suggested that PEMF might facilitate the migration of electrically charged cells involved in repairing the wound area, thereby restoring the metabolic conditions of the healing cells. It has also been proposed that PEMF induces a tiny electrical signal on the injured cell membrane, which initiates a series of physiological effects that include an increase in the number of macrophages and fibroblasts present in the wound, a reduction of the inflammation and an increased deposition of collagen and fibrin, all of which contribute to the healing process (Markoll 2003). Other theories suggest that PEMF is associated with the production of free radicals within cells, which mediate intracellular communication (Gordon 2007). PEMF may exert several biological processes involved in wound healing, but the exact mechanism is not clear.
Why it is important to do this review
There are several anecdotal reports of the beneficial effects of EMT for chronic skin wounds, despite the lack of standardisation of the PEMF devices in terms of type, duration, frequency, intensity and length of exposure. A systematic review to assess the available evidence for EMT on pressure ulcers was warranted.
Objectives
To assess the evidence for the effects of electromagnetic therapy (EMT) in the healing of pressure ulcers.
Methods
Criteria for considering studies for this review
Types of studies
We included trials if the allocation of participants to the therapies was described as randomised. There was no restriction on the basis of language, date of trial or publication status.
Types of participants
We included studies which involved people of any age and in any care setting, described as having a pressure ulcer. Studies which referred to the wounds using the synonyms decubitus, bed sore and pressure sore were also eligible for inclusion.
Types of interventions
The application of EMT to treat pressure ulcers compared with sham EMT, no EMT or other (standard) treatments.
Types of outcome measures
Primary outcomes
Healing of pressure ulcer using measures such as:
-
proportion of ulcers healed within trial period;
-
rate of change in ulcer area; and
-
time to complete healing.
Secondary outcomes
-
Costs.
-
Quality of life.
-
Pain.
-
Acceptability of treatment.
Search methods for identification of studies
Electronic searches
Details of the search strategy for fourth update of this review are shown in Appendix 1.
For this update, we searched the following databases to find reports of randomised controlled trials (RCTs) of EMT:
-
Cochrane Wounds Group Specialized Register (Searched 10/06/15)
-
The Cochrane Central Register of Controlled Trials (CENTRAL) ‐ The Cochrane Library 2015, Issue 6
-
Ovid MEDLINE & Ovid MEDLINE ‐ In‐Process & Other Non‐Indexed Citations 2014 to 10 June 2015
-
Ovid EMBASE ‐ 2014 to 10 June 2015
-
EBSCO CINAHL ‐ 2014 to 10 June 2015
The following search strategy was used in the Cochrane Central Register of Controlled Trials (CENTRAL):
#1 MeSH descriptor Electromagnetics explode all trees
#2 MeSH descriptor Electric Stimulation Therapy explode all trees
#3 (electromagnetic* or electrotherap*):ti,ab,kw
#4 (electric* NEXT current):ti,ab,kw
#5 ((direct or pulsed or alternating) NEXT current):ti,ab,kw
#6 (low NEXT intensity) or (low NEXT frequency):ti,ab,kw
#7 (high NEXT voltage):ti,ab,kw
#8 ("TENS" or "NMES"):ti,ab,kw
#9 (interferential NEXT therap*):ti,ab,kw
#10 (monophasic or galvanic):ti,ab,kw
#11 MeSH descriptor Diathermy explode all trees
#12 MeSH descriptor Microwaves explode all trees
#13 (diathermy or microwave*):ti,ab,kw
#14 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13)
#15 MeSH descriptor Pressure Ulcer explode all trees
#16 pressure NEXT (ulcer* or sore*):ti,ab,kw
#17 decubitus NEXT (ulcer* or sore*):ti,ab,kw
#18 (bed NEXT sore*) or bedsore:ti,ab,kw
#19 (#15 OR #16 OR #17 OR #18)
#20 (#14 AND #19)
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 2; Appendix 3 and Appendix 4 respectively. The Ovid MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format (Lefebvre 2011). The EMBASE and CINAHL searches were combined with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2010). There were no restrictions on the basis of language or date of publication.
Searching other resources
For the original review and the first update, experts in the field (e.g. SA Cooper‐Vastola) and manufacturers (Diapulse® and Elmedistraal®) were also contacted and asked to provide any information they might have about unpublished studies. In the second update we checked the reference list of the systematic review by McGaughey 2009 for additional studies.No other resources were searched for this update.
Data collection and analysis
Selection of studies
For this review update, two review authors independently checked titles and abstracts of studies identified by the update search for eligibility. We obtained full reports of articles if they appeared to satisfy, or to potentially satisfy, the inclusion criteria. Two review authors independently checked full papers to identify those trials that were eligible for inclusion. Any disagreement was resolved by discussion between the two review authors.
For the original review, titles and abstracts of studies identified by searching the Wounds Group Specialised Register were assessed by one review author (KF) for eligibility. Full reports of articles were obtained if they appeared to satisfy the inclusion criteria of the initial assessment. Those rejected were checked by another review author (NC). Full papers were checked to identify those that were eligible for inclusion (KF). This was repeated independently by another review author (NC) to provide verification. Any disagreement was resolved by discussion.
Data extraction and management
We extracted and summarised details of the eligible studies using a data extraction sheet. We made attempts to obtain any missing data by contacting the trial authors. We included data from studies published in duplicate only once. One review author undertook data extraction and the second author checked for accuracy. We extracted the following data:
-
design of study;
-
inclusion and exclusion criteria;
-
baseline characteristics (by treatment group);
-
intervention details;
-
outcome measures used;
-
results (by treatment group);
-
withdrawals (by treatment group); and
-
adverse effects.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias of the included studies. As recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), we assessed the following methodological domains:
-
Sequence generation ‐ was the method used to generate the allocation sequence appropriate to produce comparable groups?
-
Allocation sequence concealment ‐ was the method used to conceal the allocation sequence appropriate to prevent the allocation being known in advance of, or during, enrolment?
-
Blinding of participants, personnel and outcome assessors ‐ were measures used to blind study participants, personnel and outcome assessors from knowledge of which intervention a participant received?
-
Incomplete outcome data ‐ how complete were the outcome data for the primary outcomes? Were drop‐out rates and reasons for withdrawal reported? Were missing data imputed appropriately? We considered an overall completion rate of 80% or higher as having a low risk of bias.
-
Selective outcome reporting ‐ were appropriate outcomes reported and were any key outcomes missing?
-
Other potential threats to validity (considering external validity, e.g. relevant use of co‐interventions) ‐ what was the funding source of each of the studies?
We explicitly judged each of these criteria using the following system: Yes (i.e. low risk of bias); No (i.e. high risk of bias); and Unclear (i.e. either lack of information, or uncertainty over the potential for bias).
Data synthesis
We combined the studies included in the review by narrative overview with a quantitative summary of the result of similar trials where appropriate. For each trial with important dichotomous outcomes(e.g. ulcers healed ‐ yes or no) we calculated a risk ratio of healing with 95% confidence intervals (CI). Where outcomes for continuous variables were presented as medians without confidence intervals, standard deviations or some measure of the precision of the result, we entered the median into the table of Characteristics of included studies and did not use the data in data synthesis.
Results
Description of studies
No new reports were identified in this review update. Searches for the third review update identified four additional studies (Goldin 1981; Gupta 2009; Itoh 1991; Seaborne 1996) but none met the inclusion criteria and all were added to the Characteristics of excluded studies where reasons for exclusion are provided.
Two studies of EMT for the treatment of pressure ulcers, involving a total of 60 people, are included in the review (Comorosan 1993; Salzberg 1995). The first study (Comorosan 1993) was conducted in a social care unit in Bucharest, Romania. This study was a three‐arm study; EMT (plus standard therapy), sham EMT (plus standard therapy) and standard therapy alone. The treatment and follow up was over a two to eight‐week period. A total of 30 people were recruited: 17 female and 13 male, aged from 60 to 84 years, with Satge II (16 participants) and Stage III (14 participants) pressure ulcers (the grading system used was not described). Participants were described as randomly allocated to one of the three groups. Twenty people received EMT (Diapulse®) therapy plus standard therapy; five received sham EMT (Diapulse®) therapy plus standard therapy; and five received standard therapy alone. The EMT therapy involved local application of electromagnetic field at a frequency of 600 pulses per second, peak power 6 (117 V, 27.12 MHz). Treatment was given for 30 minutes, twice a day. The standard therapy involved cleansing with hydrogen peroxide and local application of talcum powder, methylene‐blue in solution and antibiotic ointment (tetracycline). The outcome assessed was the percentage of ulcers healed within two to eight weeks.
The second study (Salzberg 1995) compared EMT with sham EMT over a 12‐week period or until healing (if this was shorter than 12 weeks). The participants were volunteers admitted to a Veterans' Administration Hospital in New York and consisted of 30 male hospital inpatients with spinal cord injuries (20 with Stage II and 10 with Stage III pressure ulcers). The treatment with an electromagnetic field provided a radio frequency of 27.2 MHz and a pulse repetition rate of 80 to 600 pulses per second. This study also gave treatment for 30 minutes twice a day. A clear definition of the grading of the ulcers was provided by the authors: Stage II ulcers were defined as a partial‐thickness skin loss involving epidermis or dermis, superificial and clinically presenting as a deep crater, abrasion, blister or shallow crater; while Stage III were defined as full‐thickness skin loss involving damage or necrosis of subcutaneous tissue extending down to, but not through, underlying fascia, clinically presented as a deep crater with or without undermining of adjacent tissue. The outcomes assessed were time to complete healing, percent change in ulcer area and proportion of ulcers healed.
Risk of bias in included studies
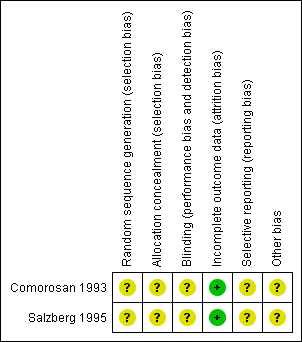
The risk of bias in the included studies is summarised in Figure 1.
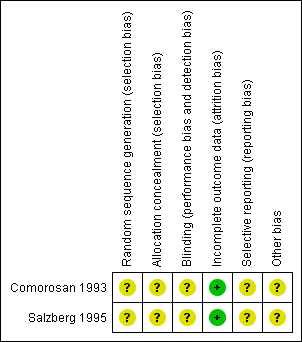
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Both trials have unclear risk of bias for sequence generation and allocation concealment. They described the allocation to treatment groups as randomised but there was no description on how randomisation was achieved. The lack of description of the allocation process also meant that the degree of allocation concealment was unclear.
Blinding
In judging the risk of bias for this item, we considered how subjective or objective an outcome is. There are particular risks of bias with more subjective outcomes (Higgins 2011). The two trials were judged to have unclear risk of bias for blinding. Both described how patients and investigators were blinded to EMT and sham EMT therapy but did not provide information on the blinding of the outcome assessors. In wound trials assessment of treatment outcome, namely reduction in surface area, involves an element of subjectivity (for example in judging where the wound edge lies), therefore it is important that outcome assessors are blinded.
Incomplete outcome data
In judging the risk of bias for this item, we considered whether missing data were imputed appropriately and whether an intention‐to‐treat analysis was reported for the primary outcome. The two trials were considered to have low risk of bias for incomplete outcome data. There was no loss to follow up in Comorosan 1993 while in Salzberg 1995 the loss to follow up occurred after the main outcome was assessed (after one week).
Selective reporting
In considering the risk of bias for selective reporting, we based our assessment on comparing outcomes listed in the methods section of the paper with those outcomes reported in the results section. Both trials had unclear risk of bias for selective reporting. Outcomes to be assessed were not listed in the methods section in Comorosan 1993, thus it was not clear whether the trial included all planned outcomes. In Salzberg 1995 a subset of patients with stage II pressure ulcers less than or equal to 60 cm2 and ulcer size more than 60 cm2 were analysed separately. Stage II and stage III patients were also analysed separately. These analyses were not prespecified in the methods section of the paper but may have been planned.
Other potential sources of bias
Baseline ulcer area was not reported in Comorosan 1993. Salzberg 1995 reported there was no statistically significant difference for the baseline parameters between the EMT group and the sham group for those with Stage II pressure ulcers (total n= 20). However, the randomisation process did not provide for an even distribution of large pressure ulcers between the two groups with the sham EMT group having larger ulcers than the EMT group. No baseline data were provided for patients with Stage III pressure ulcers, therefore we were unable to judge whether theses two groups (n=10) were comparable at the start of the study.
Effects of interventions
Proportions of ulcers healed
Two trials compared EMT with sham EMT, although the trial by Comorosan 1993 included a third arm in which only standard therapy was applied.
In the Comorosan 1993 trial, 17 out of 20 (85%) ulcers in the EMT group achieved complete healing within the duration of treatment compared with no ulcers healing in either of the other two groups (five ulcers in each); the risk ratio (RR) was 10.00 (95% CI 0.70 to 143.06) (Analysis 1.1; Analysis 2.1). The difference between the groups was statistically not significant.
In the Salzberg 1995 trial, at one week three out of 10 (30%) Stage II pressure ulcers and three out of five (60%) Stage III pressure ulcers in the EMT group had healed, compared with none in the sham EMT group (RR 7.00, 95% CI 0.41 to 120.16) and (RR 7.0, 95% CI 0.45 to 108.26) respectively (Analysis 3.1). The pooled RR for Stage II and III was 7.00 (95% CI 0.97 to 50.38) (Analysis 3.1).
The results from these two studies do not indicate a statistically significant treatment effect associated with EMT in healing pressure ulcers, however there is a great deal of uncertainty as there are only two small studies, both at unclear risk of bias.
We did not combine the results of the two studies (Comorosan 1993; Salzberg 1995) because of the different treatment durations.
Change in ulcer area
Change in ulcer area was not assessed in Comorosan 1993.
In Salzberg 1995, the overall change in ulcer area was presented in the discussion section of the paper. The ulcer area reduction at one week was 77% (SD = 21%) in the EMT group and 40% (SD = 28%) in the sham EMT group. The mean percent difference in area reduction between the two groups was statistically significantly greater in the EMT group (RR 37%, 95% CI 17.36 to 56.64) (Analysis 4.1). However, this result should be interpreted with caution for two reasons; firstly, this is a small study and there is a possibility that this finding may be due to chance differences in prognostic variables. The randomisation process did not provide for an even distribution of large pressure ulcers between the two groups with the sham EMT group having larger ulcers than the EMT group. In general, a change in area or volume would give a larger percentage reduction for a smaller ulcer than for a bigger ulcer. Subsequently, this would favour the EMT group as it has the smallest median wound size at baseline for stage II ulcers (baseline values for stage III ulcers were not provided). Secondly, the risk of bias due to generation of allocation sequence, allocation concealment and blinding of the outcome assessor was assessed as 'unclear' due to poor reporting.
Time to complete healing
Time to complete healing was reported only for the EMT group in one study (Comorosan 1993). Healing in Stage II ulcers was achieved between one and four weeks (mean 3.28 weeks), while for Stage III ulcers healing time was between two and eight weeks (mean = 4.87). In Salzberg 1995, the median time to complete healing was 13 days for the EMT group, compared with 31.5 days for the sham EMT group (P value < 0.001). However, the results of these two studies could not be combined as measures of variance were not reported. Furthermore baseline imbalances for wound area in Salzberg 1995 introduce bias for this outcome.
Secondary outcomes
Secondary outcomes, namely costs, quality of life, pain and acceptability of treatment were not assessed in either trial.
Adverse effects
No adverse effects were observed in Comorosan 1993, while Salzberg 1995 did not provide information on adverse effects.
Discussion
There is no strong evidence from two small trials that EMT speeds pressure ulcer healing. Both trials contained small numbers of patients and used different regimens of treatment over different time scales. There was evidence from one trial showing that the EMT group achieved more reduction in wound area than the sham EMT group. However, this result needs to be interpreted with caution. The result was based on data from a trial with a moderate risk of bias in which randomisation sequence, concealment allocation and blinding of outcome assessor were unclear.
The extent to which EMT contributes to healing in patients who are also receiving pressure relief and moist wound healing strategies should be explored. The included trials, particularly Comorosan 1993, did not report severity of pressure ulcers and baseline comparisons adequately. Consequently, the results should be viewed as unreliable until further research involving larger numbers of patients that can be considered alongside these trials becomes available.
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Comparison 1 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Pressure ulcers healed within 8 weeks of treatment.

Comparison 2 Electromagnetic therapy versus standard therapy alone, Outcome 1 Pressure ulcers healed within 8 weeks of treatment duration.

Comparison 3 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Healed ulcers at one week.

Comparison 4 Electromagnetic therapy versus sham electromagnetic therapy, Outcome 1 Percent reduction in wound surface area at one week.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcers healed within 8 weeks of treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcers healed within 8 weeks of treatment duration Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Healed ulcers at one week Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.97, 50.38] |
| 1.1 Stage II ulcers | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.41, 120.16] |
| 1.2 Stage III ulcers | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.45, 108.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Percent reduction in wound surface area at one week Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 37.0 [17.36, 56.64] |

