Coasting疗法(抑制促性腺激素)预防卵巢过度刺激综合征
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial, single centre. | |
| Participants | Eygpt. IVF centre. Of 1536 women undergoing IVF/ICSI, 190 were eligible and randomised. Inclusion: undergoing first IVF trial, at actual risk of developing severe OHSS with large number of follicles (≥ 20) on both ovaries, with 90% of the follicles being small (< 14 mm in mean diameter), and estradiol concentration ≥ 3000 pg/ml. Age in the coasting group was 30 ± 4.9 years, and in the antagonist group was 29.6 ± 4.6 years | |
| Interventions | Ovarian stimulation using long GnRH agonist down‐regulation protocol. Coasting group (N = 96) hMG injections stopped and GnRH agonist continued. HmCG given when E2 ≤ 3000 pg/ml. Oocyte retrieval performed 36 hours after HCG administration. GnRHa group (N = 94) treated with subcutaneous GnRH antagonist (ganirelix acetate 250 µg) daily until day of HCG administration. GnRH agonist was discontinued with the start of antagonist and hMG injections continued daily until E2 ≤ 3000 pg/ml, then 10,000 IU of hCG given. Oocyte retrieval performed 36 hours after HCG administration. Embryo transfer on day 2 or day 3 with two to three embryos transferred. | |
| Outcomes | The primary outcomes were number of high quality embryos. Secondary outcomes were days of intervention, number of oocytes, pregnancy rate, multiple pregnancy, number of cryopreserved embryos and incidence of severe OHSS | |
| Notes | Sample size calculation estimated N = 182 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomised' ‐ no other details |
| Allocation concealment (selection bias) | Low risk | 'dark, sealed envelopes .... created by a third party not involved in the allocation process.' 'sequentially numbered' |
| Blinding (performance bias and detection bias) | High risk | 'The patient was informed about the allocated arm' |
| Incomplete outcome data (attrition bias) | Low risk | All those randomised were analyzed, no loss to follow‐up reported |
| Selective reporting (reporting bias) | Unclear risk | Did not report live birth |
| Methods | Randomised controlled trial | |
| Participants | Iran and UK study 52 women undergoing IVF treatment cycles at high risk for developing OHSS (> 20 follicles in both ovaries, serum estradiol = E2 > 3000 pg/ml). | |
| Interventions | Induction of ovulation with long protocol beginning with pituitary desensitisation with subcutaneous buserelin and followed by hMG 3 amp from day 2. On day 9 randomised to: Coasting group (N = 27) IVF/ICSI defined as presence of > 10 follicles per ovary with a leading follicle > 17 mm and E2 > 3000 pg/ml (maximum 3 days). Then 10000 units hCG administered and oocyte retrieval 34 to 36 hours later. Aspiration follicle group (N = 26) had > 15 follicles 15 to 16mm in each ovary and E2 > 3000 pg/ml. Unilateral aspiration follicular aspiration performed before hCG administration. Oocyte retrieval performed 34 to 36 hours later in the other ovary. Embryo transfer was done 2 days later in both groups. | |
| Outcomes | Number of follicles, number of oocytes, pregnancy rate, OHSS. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'randomized controlled trial' |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | No details |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not mentioned in methods ‐ this was a conference abstract. Did not report live birth. |
| Methods | Randomised control trial | |
| Participants | India study 60 women undergoing IVF considered at risk of OHSS (> 20 follicles of more than 11 mm, serum E2 > 3000 pg/ml on day 9 of stimulation, or both). | |
| Interventions | Coasting group (30 patients), exogenous gonadotropins were withheld to allow E2 to decrease while GnRH‐a was maintained. Then 10,000 units hCG was administrated and oocyte retrieval was performed 36 hours later Cabergoline group (30 patients) were administered with 0.5 mg cabergoline tablet on day of hCG injection, continued for 8 days. | |
| Outcomes | Number of mature oocytes, number of embryos, clinical pregnancy rate, OHSS | |
| Notes | Source of funding not stated and no correspondence details for author. Obtained missing data from another review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomization |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Low risk | All participants analyzed |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not mentioned in methods. Did not report live birth |
| Methods | Randomised controlled trial; parallel prospective design; single centre; power calculation included; randomization based on serially numbered sealed envelopes. | |
| Participants | Kuwait study 37 women recruited: 30 infertile women (consented and randomised) < 39 years, considered at risk of OHSS (15 coasting/15 EUFA); | |
| Interventions | Treatment group: coasting (hMG injections were withheld until E2 < 3000 pg/ml and GnRh‐a continued until day of hCG; duration 3 to 7 days). | |
| Outcomes | Method of diagnosing different grades of OHSS: Schenker and Weinstein (1978) and Navot criteria (1992). | |
| Notes | Source of funding: not stated. Authors contacted on two occasions ‐ extra data obtained | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random numbers |
| Allocation concealment (selection bias) | Low risk | "serially numbered sealed envelopes" |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Low risk | All patients analyzed |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not mentioned in methods. Did not report live birth |
| Methods | Randomised controlled trial, single centre, randomization based on serially numbered sealed envelopes. | |
| Participants | Kuwait study, 102 women recruited undergoing IVF cycles at risk of OHS with serum E2 ≥ 3500 pg/ml, > 15 follicles in each ovary and two leading follicles of ≥18mm in size. | |
| Interventions | Coasting group (N = 51): long protocol starting dose 225 iu hMG, hMG was withheld until E2 levels fell < 1500 pg/ml, when trigger dose HCG was administered. FSH co‐trigger group (N = 51): Long protocol, pure FSH was administered with the trigger dose of hCG, regardless of the E2 levels ≥ 3500 pg/ml. Three cleaved D3 or two D5 blastocyst embryos transferred. | |
| Outcomes | Golan 2009 classification of OHSS used Moderate or severe OHSS Clinical pregnancy rate (48.6% versus 51.8%) Number of oocytes retrieved (8.6 ± 2.9 versus 26.4 ± 3.5) Multiple pregnancy rate, live birth rate, miscarriage rate (reported as no significant difference) | |
| Notes | Source of funding not stated, author contacted twice, responded once with partial data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random numbers |
| Allocation concealment (selection bias) | Low risk | "serially numbered sealed envelopes" |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Low risk | All participants analyzed |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not mentioned in methods. Did not report data suitable for analysis on live birth |
| Methods | Randomised study | |
| Participants | 68 patients at risk of developing OHSS, aged 25 to 38 years undergoing controlled ovarian hyperstimulation in IVF/ICSI. Inclusion: intermediate follicles (11 to 14mm) > 10, E2 > 700 pg/ml on day 7 or day 8 of controlled ovarian hyperstimulation, or both | |
| Interventions | Group A (N = 16) early coasting from day 8 onwards on basis of high E2 (> 700 pg/ml). Group B (N = 18) late coasting when one of the follicles reached 15 mm; E2 < 700 pg/ml on day 8 but number of intermediate follicles were more than 10. Group C (N = 34) no coasting, E2 level of 3000 pg/ml to < 4000 pg/ml hCG day. These women had neither E2 > 700 pg/ml, nor intermediate follicles > 10mm. | |
| Outcomes | OHSS severity, terminal E2 mean number of oocytes retrieved, endometrial thickness, clinical pregnancy, miscarriage, live birth. | |
| Notes | Women with E2 > 4000 pg/ml on hCG day had transvaginal ovum retrieval, and following fertilisation, the embryos were frozen and not transferred in that cycle. These women received prophylactic IV albumin and were excluded from the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomised' |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding (performance bias and detection bias) | Unclear risk | No details |
| Incomplete outcome data (attrition bias) | Unclear risk | Women who were excluded due to high E2 levels were not detailed |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported |
| Methods | Randomised controlled trial, single centre, randomization based on generated table of random numbers | |
| Participants | 139 women recruited, who had unsuccessfully undergone standard long protocol ICSI procedure complicated by moderate or severe OHSS. For the next cycle, women randomised to standard long protocol or 'internal' coasting. | |
| Interventions | Coasting group (N = 68): long protocol, received 2 days 225 iu hMG, then 2 days without hMG and 150 hMG for remainder of the stimulation period. Control group (N = 71): received standard dose hMG as in the first cycle. All patient underwent ICSI (routine practice in the centre) and maximum two embryos transferred on D3 for women < 36 and three embryos for older women. | |
| Outcomes | Rizk and Aboulgar OHSS classification used Moderate or severe OHSS Clinical pregnancy rate Number of oocytes retrieved Multiple pregnancy rate | |
| Notes | Source of funding not stated; author contacted twice ‐ no response. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'randomised'. |
| Allocation concealment (selection bias) | Low risk | only known to administrative staff |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Low risk | All participants analyzed |
| Selective reporting (reporting bias) | Low risk | Includes expected outcomes |
| Methods | Randomised controlled trial | |
| Participants | 60 participants undergoing IVF at risk of developing OHSS (20 follicles in both ovaries, majority < 15 mm in diameter and serum E2 level 3000 pg/ml) | |
| Interventions | All participants underwent long protocol with a starting dose of 75 to150 iu r‐FSH, and dose adjusted on individual response. In Cabergoline Group A (30 patients), when the number of follicles exceeded 20, with at least two leading follicles 18 mm, 10,000 hCG was administered and 0.5 mg oral cabergoline was started immediately for seven days after hCG administration In Coasting Group B (30 patients), when the number of follicles was 20 or more and mean leading follicle was 16 mm, gonadotrophin was ceased until E2 levels dropped below 3000 pg/ml. All participants underwent ICSI procedure and 2 to 3 embryos transferred, depending on patient's age and quality of embryos. | |
| Outcomes | Number of oocytes, clinical pregnancy rate, OHSS | |
| Notes | Source of funding not stated. Attempts made to contact authors but there was no response | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomization |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Low risk | All participants data analyzed |
| Selective reporting (reporting bias) | Low risk | Main outcome measure reported |
OHSS: ovarian hyperstimulation syndrome
EUFA: early unilateral follicular aspiration
E2: estradiol
BMI: body mass index
hMG: human menopausal gonadotrophin
GnRh‐a: gonadotrophin‐releasing hormone analogue
hCG: human chorionic gonadotrophin
FSH: Follicle stimulating hormone
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Prospective randomised trial with historical control | |
| Prospective observational study | |
| Retrospective observational study | |
| Retrospective case‐control study | |
| Retrospective cohort study | |
| Retrospective observational study | |
| Retrospective observational study | |
| Prospective observational study | |
| Prospective observational study | |
| Retrospective observational study | |
| Retrospective observational study | |
| Retrospective observational study | |
| Retrospective case‐control study | |
| Prospective observational study |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 2 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.05, 0.24] |
| Analysis 1.1  Comparison 1 Coasting versus no coasting, Outcome 1 OHSS. | ||||
| 2 Live birth Show forest plot | 1 | 68 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.14, 1.62] |
| Analysis 1.2 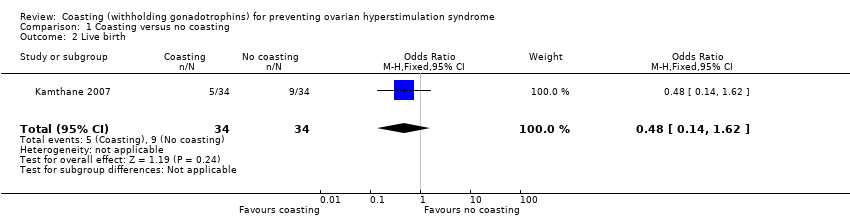 Comparison 1 Coasting versus no coasting, Outcome 2 Live birth. | ||||
| 3 Clinical pregnancy Show forest plot | 2 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.46, 1.44] |
| Analysis 1.3  Comparison 1 Coasting versus no coasting, Outcome 3 Clinical pregnancy. | ||||
| 4 Multiple pregnancy Show forest plot | 1 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.12, 0.81] |
| Analysis 1.4 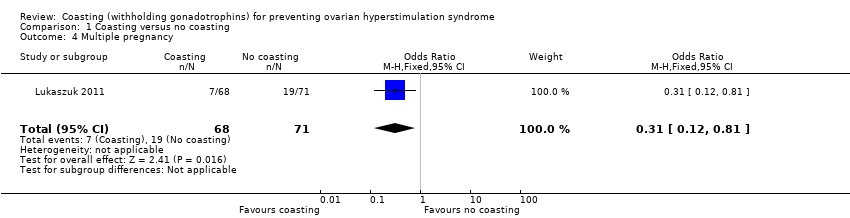 Comparison 1 Coasting versus no coasting, Outcome 4 Multiple pregnancy. | ||||
| 5 Miscarriage Show forest plot | 2 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.25, 2.86] |
| Analysis 1.5 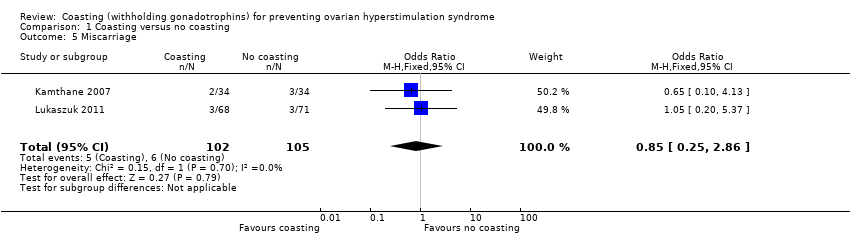 Comparison 1 Coasting versus no coasting, Outcome 5 Miscarriage. | ||||
| 6 Number of oocytes retrieved Show forest plot | 2 | 207 | Mean Difference (IV, Fixed, 95% CI) | ‐3.86 [‐4.38, ‐3.33] |
| Analysis 1.6  Comparison 1 Coasting versus no coasting, Outcome 6 Number of oocytes retrieved. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 2 | 83 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.34, 2.85] |
| Analysis 2.1 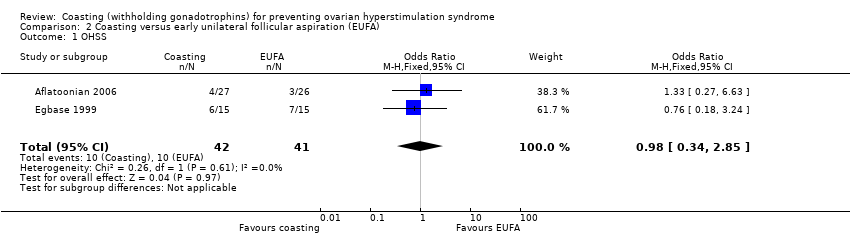 Comparison 2 Coasting versus early unilateral follicular aspiration (EUFA), Outcome 1 OHSS. | ||||
| 2 Clinical Pregnancy Show forest plot | 2 | 83 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.25, 1.79] |
| Analysis 2.2 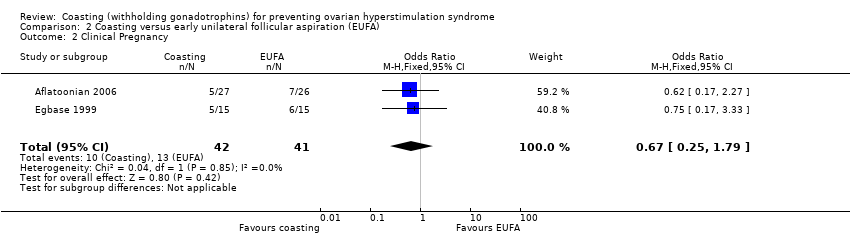 Comparison 2 Coasting versus early unilateral follicular aspiration (EUFA), Outcome 2 Clinical Pregnancy. | ||||
| 3 Number of oocytes retrieved Show forest plot | 2 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐4.42 [‐6.08, ‐2.75] |
| Analysis 2.3 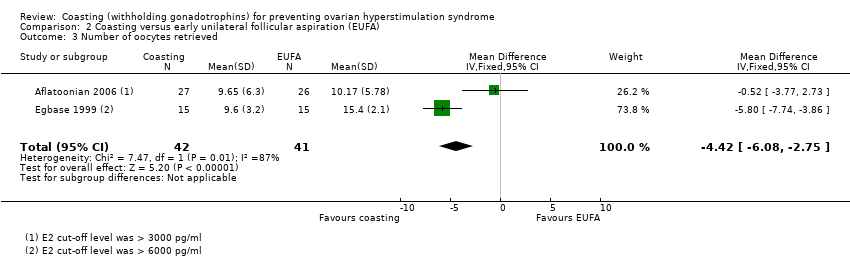 Comparison 2 Coasting versus early unilateral follicular aspiration (EUFA), Outcome 3 Number of oocytes retrieved. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 3.1  Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 1 OHSS. | ||||
| 2 Clinical Pregnancy Show forest plot | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.42, 1.31] |
| Analysis 3.2 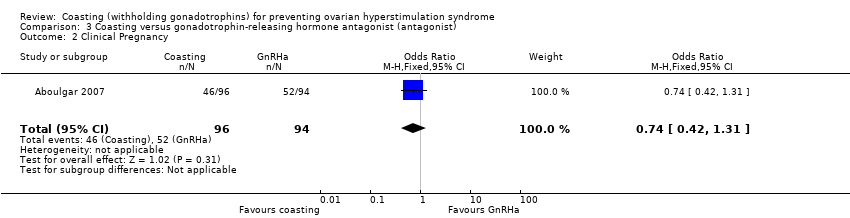 Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 2 Clinical Pregnancy. | ||||
| 3 Multiple pregnancy Show forest plot | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.39, 1.80] |
| Analysis 3.3  Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 3 Multiple pregnancy. | ||||
| 4 Number of oocytes retrieved Show forest plot | 1 | 190 | Mean Difference (IV, Fixed, 95% CI) | ‐2.44 [‐4.30, ‐0.58] |
| Analysis 3.4 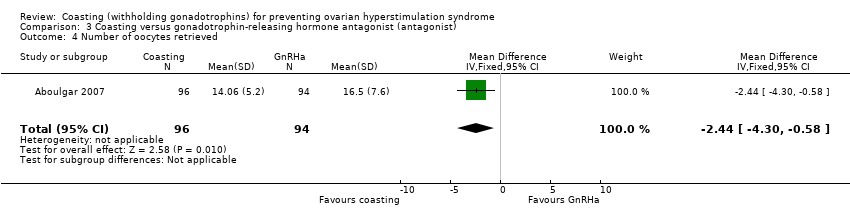 Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 4 Number of oocytes retrieved. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 1 | 102 | Odds Ratio (M‐H, Fixed, 95% CI) | 43.74 [2.54, 754.58] |
| Analysis 4.1 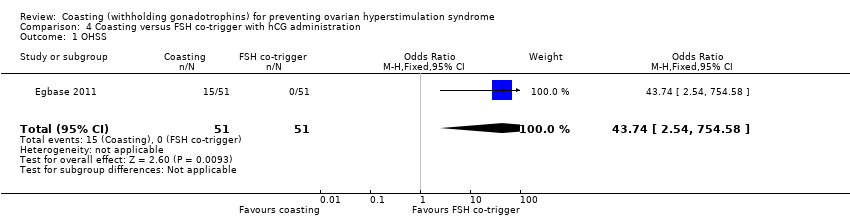 Comparison 4 Coasting versus FSH co‐trigger with hCG administration, Outcome 1 OHSS. | ||||
| 2 Clinical pregnancy Show forest plot | 1 | 102 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.43, 2.01] |
| Analysis 4.2  Comparison 4 Coasting versus FSH co‐trigger with hCG administration, Outcome 2 Clinical pregnancy. | ||||
| 3 Number of oocytes retrieved Show forest plot | 1 | 102 | Mean Difference (IV, Fixed, 95% CI) | ‐17.80 [‐19.05, ‐16.55] |
| Analysis 4.3 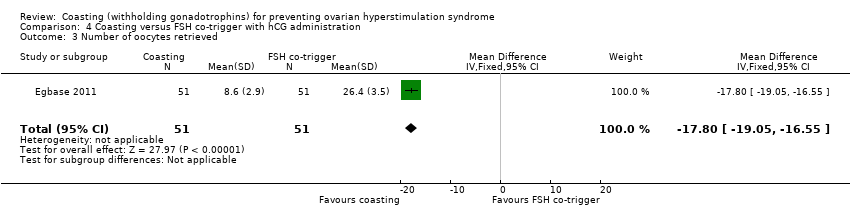 Comparison 4 Coasting versus FSH co‐trigger with hCG administration, Outcome 3 Number of oocytes retrieved. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 2 | 120 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.98 [0.69, 5.68] |
| Analysis 5.1  Comparison 5 Coasting versus cabergoline, Outcome 1 OHSS. | ||||
| 2 Clinical pregnancy rate Show forest plot | 2 | 120 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.16, 0.88] |
| Analysis 5.2 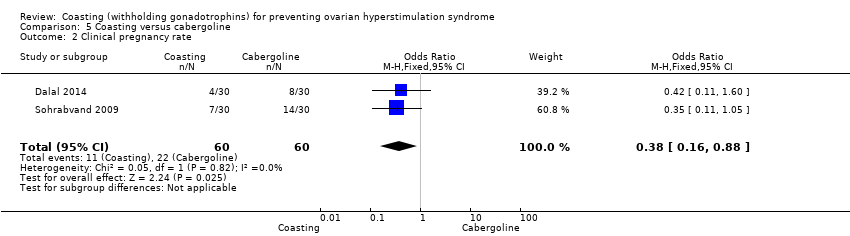 Comparison 5 Coasting versus cabergoline, Outcome 2 Clinical pregnancy rate. | ||||
| 3 Number of oocytes retrieved Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐7.88, ‐0.72] |
| Analysis 5.3  Comparison 5 Coasting versus cabergoline, Outcome 3 Number of oocytes retrieved. | ||||

Study flow diagram: July 2016 search for 2017 review update

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
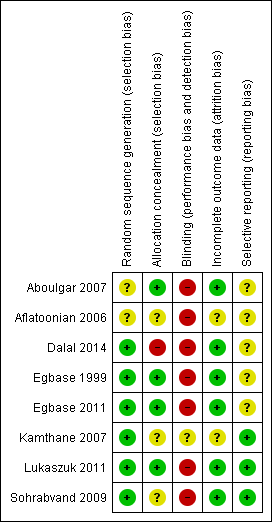
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 3 Coasting versus no coasting, outcome: 3.1 OHSS.

Forest plot of comparison: 1 Coasting versus EUFA, outcome: 1.1 OHSS.

Forest plot of comparison: 5 Coasting versus cabergoline, outcome: 5.1 OHSS.

Comparison 1 Coasting versus no coasting, Outcome 1 OHSS.

Comparison 1 Coasting versus no coasting, Outcome 2 Live birth.

Comparison 1 Coasting versus no coasting, Outcome 3 Clinical pregnancy.

Comparison 1 Coasting versus no coasting, Outcome 4 Multiple pregnancy.

Comparison 1 Coasting versus no coasting, Outcome 5 Miscarriage.

Comparison 1 Coasting versus no coasting, Outcome 6 Number of oocytes retrieved.

Comparison 2 Coasting versus early unilateral follicular aspiration (EUFA), Outcome 1 OHSS.

Comparison 2 Coasting versus early unilateral follicular aspiration (EUFA), Outcome 2 Clinical Pregnancy.
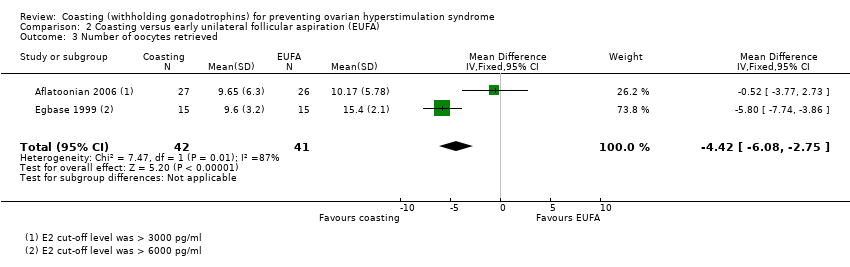
Comparison 2 Coasting versus early unilateral follicular aspiration (EUFA), Outcome 3 Number of oocytes retrieved.

Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 1 OHSS.

Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 2 Clinical Pregnancy.
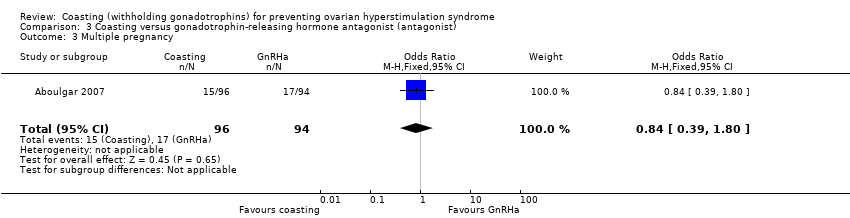
Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 3 Multiple pregnancy.

Comparison 3 Coasting versus gonadotrophin‐releasing hormone antagonist (antagonist), Outcome 4 Number of oocytes retrieved.

Comparison 4 Coasting versus FSH co‐trigger with hCG administration, Outcome 1 OHSS.
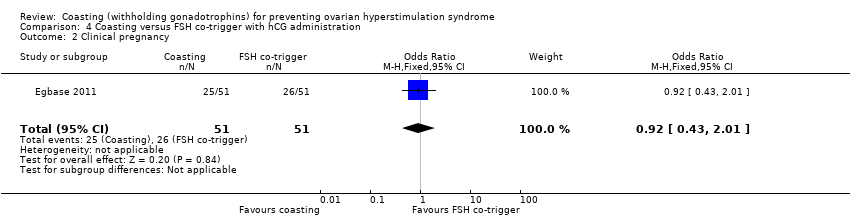
Comparison 4 Coasting versus FSH co‐trigger with hCG administration, Outcome 2 Clinical pregnancy.
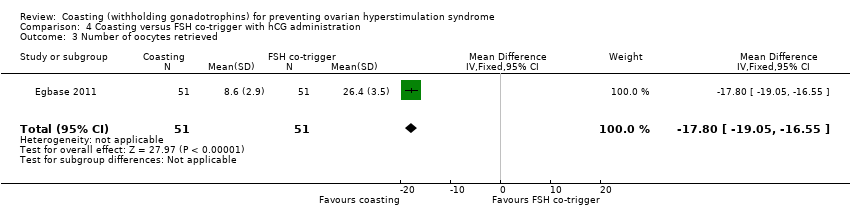
Comparison 4 Coasting versus FSH co‐trigger with hCG administration, Outcome 3 Number of oocytes retrieved.

Comparison 5 Coasting versus cabergoline, Outcome 1 OHSS.
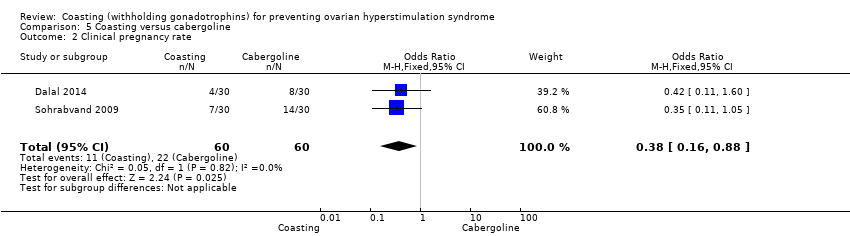
Comparison 5 Coasting versus cabergoline, Outcome 2 Clinical pregnancy rate.
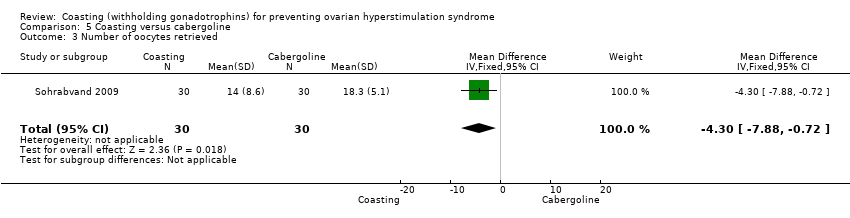
Comparison 5 Coasting versus cabergoline, Outcome 3 Number of oocytes retrieved.
| Coasting versus no coasting for prevention of ovarian hyperstimulation syndrome (OHSS) | ||||||
| Population: Women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no coasting | Risk with coasting | |||||
| OHSS | 457 per 1000 | 85 per 1000 | OR 0.11 | 207 | ⊕⊕⊝⊝ | |
| Live birth | 265 per 1000 | 147 per 1000 | OR 0.48 | 68 | ⊕⊝⊝⊝ | |
| Clinical pregnancy | 390 per 1000 | 344 per 1000 | OR 0.82 | 207 | ⊕⊕⊝⊝ | |
| Multiple pregnancy | 268 per 1000 | 102 per 1000 | OR 0.31 | 139 | ⊕⊝⊝⊝ | |
| Miscarriage | 57 per 1,000 | 49 per 1,000 (15 to 148) | OR 0.85 (0.25 to 2.86) | 207 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: one study did not clearly describe the methods used, studies not blinded 2 Downgraded one level for serious imprecision: few events, wide confidence intervals, or both 3 Downgraded two levels for very serious imprecision: very few events, very wide confidence intervals, or both | ||||||
| Coasting versus early unilateral follicular aspiration for preventing ovarian hyperstimulation syndrome (OHSS) | ||||||
| Population: Women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with early unilateral follicular aspiration (EUFA) | Risk with coasting | |||||
| OHSS | 244 per 1000 | 240 per 1000 | OR 0.98 | 83 | ⊕⊝⊝⊝ | |
| Live birth | No data available | |||||
| Clinical Pregnancy | 317 per 1000 | 237 per 1000 | OR 0.67 | 83 | ⊕⊝⊝⊝ | |
| Multiple pregnancy | No data available | |||||
| Miscarriage | No data available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: one study did not clearly describe methods, lack of blinding 2 Downgraded two levels for very serious imprecision: very few events and very wide confidence intervals | ||||||
| Coasting versus gonadotrophin‐releasing hormone antagonist for preventing ovarian hyperstimulation syndrome (OHSS) | ||||||
| Population: Women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with gonadotrophin‐releasing hormone antagonist | Risk with coasting | |||||
| OHSS | Not estimable | Not estimable | not estimable | 190 | ⊕⊕⊝⊝ | |
| Live birth | No data available | |||||
| Clinical Pregnancy | 553 per 1000 | 478 per 1000 | OR 0.74 | 190 | ⊕⊕⊝⊝ | |
| Multiple pregnancy | 181 per 1000 | 156 per 1000 | OR 0.84 | 98 | ⊕⊕⊝⊝ | |
| Miscarriage | No data available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: method of sequence generation not reported, lack of blinding 2 Downgraded two levels due to very serious imprecision: no OHSS occurred in either group. Few events for multiple pregnancy. 3 Downgraded one level due to serious imprecision. Wide confidence intervals, few events | ||||||
| Coasting versus follicle stimulating hormone (FSH) administration at time of hCG trigger in preventing ovarian hyperstimulation syndrome (OHSS) | ||||||
| Population: Women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with FSH co‐trigger with hCG administration | Risk with Coasting | |||||
| OHSS | Not estimable | Not estimable | OR 43.74 | 102 | ⊕⊝⊝⊝ | |
| Live birth | No data available | |||||
| Clinical Pregnancy | 510 per 1000 | 489 per 1000 | OR 0.92 | 102 | ⊕⊕⊝⊝1,3 | |
| Multiple pregnancy | No data available | |||||
| Miscarriage | No data available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: method of sequence generation not reported, lack of blinding 2 Downgraded two levels due to very serious imprecision: only 15 events, all in one arm. 3 Downgraded one level due to serious imprecision: very wide confidence intervals | ||||||
| Coasting compared to cabergoline for preventing ovarian hyperstimulation syndrome (OHSS) | ||||||
| Population: Women undergoing assisted reproduction | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with cabergoline | Risk with Coasting | |||||
| OHSS | 100 per 1000 | 180 per 1000 | OR 1.98 | 120 | ⊕⊝⊝⊝1,2 | |
| Live birth | Not reported | |||||
| Clinical pregnancy rate | 367 per 1000 | 180 per 1000 | OR 0.38 (0.16 to 0.88) | 120 | ⊕⊕⊝⊝1 | |
| Multiple pregnancy | Not reported | |||||
| Miscarriage | Not reported | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious risk of bias: one study did not clearly define method, method of sequence generation not reported, lack of blinding 2 Downgraded one level due to serious imprecision: very few events and/or wide confidence interval. | ||||||
| Classification | Size of ovaries | Grade | Symptoms |
| Mild | 5 to 10 cm | grade 1 | abdominal tension and discomfort |
| grade 2 | grade 1 signs plus nausea, vomiting, diarrhoea, or a combination | ||
| Moderate | > 10 cm | grade 3 | grade 2 signs plus ultrasound evidence of ascites |
| Severe | > 12 cm | grade 4 | grade 3 signs plus clinical evidence of ascites, pleural effusion and dyspnoea, or a combination |
| grade 5 | grade 4 signs plus haemoconcentration increased blood viscosity, hypovolaemia, decreased renal perfusion, oliguria | ||
| Severe | Critical |
| Variably enlarged ovary | Variably enlarged ovary |
| Massive ascites ± hydrothorax | Tense ascites ± hydrothorax |
| Hct > 45% (> 30% increment over baseline value) | Hct > 55% |
| WBC > 15,000 | WBC > 35,000 |
| Oliguria | |
| Creatinine 1.0 to 1.5 | Creatinine > 1.6 |
| Creatinine clearance > 50 ml/min | Creatinine clearance < 50ml/min |
| Liver dysfunction | Renal failure |
| Anasarca | Thromboembolic phenomena |
| Adult respiratory distress syndrome (ARDS) | |
| Moderate | Severe Grade A | Severe Grade B | Severe Grade C |
| Discomfort, pain, nausea, distension, ultrasonic evidence of ascites and enlarged ovaries, normal haematological and biological profile | Dyspnoea, oliguria, nausea, vomiting, diarrhoea, abdominal pain, clinical evidence of ascites, marked distension of abdomen or hydro‐thorax, US showing large ovaries and marked ascites, normal biochemical profile | Grade A plus massive tension ascites, markedly enlarged ovaries, severe dyspnoea and marked oliguria, increased haematocrit, elevated serum creatinine and liver dysfunction | Complications such as respiratory distress syndrome, renal shut‐down, or venous thrombosis |
| Authors | E2 at coasting | E2 at hCG | Number and follicle size | Coasting time |
| > 3000 pg/mL or > 11,000 pmol/L* | < 3000 pg/mL or < 11,000 pmol/L* | > 29 follicles at least 30% > 15 mm | 3 to 11 days (mean 6.1) | |
| ≥ 3000 pg/ml or ≥ 11,000 pmol/l* | < 3000 pg/ml or < 11,000 pmol/l* | at least 3 follicles of 15.6 ± 1.4 mm | 1.9 ± 0.9 days | |
| > 3000 pg/ml or > 11,000 pmol/l* | < 3000 pg/mL or < 11,000 pmol/L* | 5 follicles at least 16 mm, two of which are at least 19 mm | 1 to 5 days | |
| > 2500 pg/ml or > 9000 pmol/l* | < 2500 pg/ml or < 9000 pmol/l* | ≥ 20 follicles > 15 mm | 1 to 6 days (mean 1.94) | |
| > 2700 pg/ml or > 10,000 pmol/l* | no values given | many immature follicles < 3 at 18 mm | 3 days | |
| > 2500 pg/ml or > 9000 pmol/l* | < 2500 pg/ml or < 9000 pmol/l* | ≥ 20 follicles > 14 mm | 1 to 6 days (mean 1.94) | |
| > 6000 pg/ml or > 22,000 pmol/l* | < 3000 pg/ml or 11,000 pmol/l* | > 15 follicles, each of > 18 mm in each ovary | 4.9 ± 1.6 days | |
| > 2700 pg/ml or > 10,000 pmol/l* | < 2700 pg/ml or < 10,000 pmol/l* | > 25 follicles, at least 3 follicles > 17 mm | 3 to 6 days (mean 4.3) | |
| > 3000 pg/ml or > 11,000 pmol/l* | 25% decline < 2250 pg/ml or 8250 pmol/l* | > 3 follicles of > 18 mm | 3 to 5 days (mean 3.4 ± 0.1) | |
| > 3600 pg/ml or > 13,000 pmol/l* | < 2700 pg/ml or < 10,000 pmol/l* | at least 25% of the follicles > 15 mm | 2 to 9 days (mean 3.4 ± 1.6) | |
| > 3000 pg/ml or > 11,000 pmol/l* | < 5500 pg/ml or < 20,000 pmol/l* | > 20 follicles at least 15 mm | 2.8 days | |
| > 4000 pg/ml or > 14,684 pmol/l* | < 4000 pg/ml or < 14,684 pmol/l* | > 20 follicles, at least 30% of them >15 mm | 2.9 ± 0.33 days | |
| * conversion factor to SI unit, 3.671 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 2 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.05, 0.24] |
| 2 Live birth Show forest plot | 1 | 68 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.14, 1.62] |
| 3 Clinical pregnancy Show forest plot | 2 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.46, 1.44] |
| 4 Multiple pregnancy Show forest plot | 1 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.12, 0.81] |
| 5 Miscarriage Show forest plot | 2 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.25, 2.86] |
| 6 Number of oocytes retrieved Show forest plot | 2 | 207 | Mean Difference (IV, Fixed, 95% CI) | ‐3.86 [‐4.38, ‐3.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 2 | 83 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.34, 2.85] |
| 2 Clinical Pregnancy Show forest plot | 2 | 83 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.25, 1.79] |
| 3 Number of oocytes retrieved Show forest plot | 2 | 83 | Mean Difference (IV, Fixed, 95% CI) | ‐4.42 [‐6.08, ‐2.75] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Clinical Pregnancy Show forest plot | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.42, 1.31] |
| 3 Multiple pregnancy Show forest plot | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.39, 1.80] |
| 4 Number of oocytes retrieved Show forest plot | 1 | 190 | Mean Difference (IV, Fixed, 95% CI) | ‐2.44 [‐4.30, ‐0.58] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 1 | 102 | Odds Ratio (M‐H, Fixed, 95% CI) | 43.74 [2.54, 754.58] |
| 2 Clinical pregnancy Show forest plot | 1 | 102 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.43, 2.01] |
| 3 Number of oocytes retrieved Show forest plot | 1 | 102 | Mean Difference (IV, Fixed, 95% CI) | ‐17.80 [‐19.05, ‐16.55] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 OHSS Show forest plot | 2 | 120 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.98 [0.69, 5.68] |
| 2 Clinical pregnancy rate Show forest plot | 2 | 120 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.16, 0.88] |
| 3 Number of oocytes retrieved Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐7.88, ‐0.72] |

