Kangaroo mother care เพื่อลดการเจ็บป่วยและการตายของทารกแรกเกิดที่มีน้ำหนักตัวน้อย
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomized controlled trial conducted in Dharan, Nepal | |
| Participants | Number of infants: 126 Inclusion criteria: stable infants with birthweight < 2000 g admitted to the newborn nursery Exclusion criteria: neonates critically ill requiring ventilatory or ionotropic support or radiant warmer, neonates with chromosomal and life‐threatening congenital anomalies, neonates whose mothers were critically ill, and neonates whose mothers did not provide consent for enrollment into the study Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean weight at recruitment was 1362 ± 240 g and 1452 ± 175 g for KMC and control infants, respectively. No data on infant age at recruitment | |
| Interventions | KMC group: SSC between the mother's breasts in an upright position. Infants were dressed with diaper and a cap, and the mother's blouse covered the infant’s trunk and extremities but not the head. The duration of KMC was ≥ 6 hours per day in not more than 4 sittings, with each sitting lasting ≥ 1 hour. No data on total number of days that KMC was given after enrollment in the study (n = 63) Control group: Infants were adequately clothed, covered, and kept with their mother. If infants did not maintain temperature, they were kept under a radiant warmer (n = 63) Level of care: nursery of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported. However, it was mentioned that LBW infants were discharged when weight was > 1.600 g Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Gain in weight, length, and head circumference; hypothermia; apnea; hospital stay | |
| Notes | 87% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | No infants apparently lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Aligarh, India | |
| Participants | Number of infants: 114 Inclusion criteria: hemodynamically stable infants delivered by vaginal route with birthweight between 1200 and 1800 g Exclusion criteria: neonates delivered by cesarean section, major life‐threatening congenital malformations, severe perinatal complications, parental refusal of KMC intervention Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 4.7 ± 2.9 and 4.8 ± 2.4 days, and mean weight was 1607 ± 211 and 1615 ± 179 g, for KMC and control infants, respectively | |
| Interventions | KMC group: SSC between the mother's breasts in an upright position. Infants were dressed with a cap, socks, and a diaper and were supported at the bottom with a sling/binder. The duration of KMC during hospital stay was 6.3 ± 1.5 hours (range, 4 to 12) per day, and KMC was given for a period of 25.7 ± 6.9 (range, 15 to 43) days after enrollment in the study (n = 58) Control group: Infants were kept in radiant warmers or open cots in warm rooms (n = 56) In both groups, mothers were allowed to handle their babies at any hour of the day and to breastfeed them by nasogastric tube, by paladai, or directly. Babies in both groups were provided with vitamins and mineral supplementation Level of care: NICU of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: weight gain for ≥ 3 consecutive days, no overt illness, no intravenous medications, exclusive breastfeeding Scheme for follow‐up of infants after discharge: weekly until 40 weeks' postmenstrual age, fortnightly until 3 months' corrected age, and monthly thereafter until 6 months' corrected age | |
| Outcomes | Duration of hospital stay, weight gain, head circumference, length, exclusive breastfeeding, nosocomial sepsis, hypothermia, mild/moderate infection, severe infection, mortality | |
| Notes | 81% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization technique |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | 10 infants (8.8%) lost at 40 weeks' corrected gestational age follow‐up (KMC 4, control 6), 21 (18.4%) lost at 3 months' corrected age (KMC 10, control 11), and 39 (34.2%) lost at 6 months' corrected age (KMC 19, control 20) |
| Selective reporting (reporting bias) | High risk | Non‐significant results such as infant mortality and weight, length, and head circumference at discharge and follow‐up (secondary outcomes listed in Methods) mentioned but not reported adequately |
| Other bias | High risk | Use of blocked randomization, which could make possible prediction of future assignments in an unblinded trial when assignments are revealed, subsequently to the person recruiting into the trial |
| Methods | Randomized controlled trial conducted in Providence, Rhode Island, United States | |
| Participants | Number of infants: 50 Inclusion criteria: medically stable infants from singleton or multiple pregnancy with birth weight < 1500 g, whose mothers planned to breastfeed. Infants were no longer ventilator dependent and were without chest tubes, and they no longer required continuous positive airway pressure, when the study was begun Exclusion criteria: mother's positive history of illicit drug use, mental illness, human immunodeficiency virus (HIV) infection, receiving any medications contraindicative to breastfeeding. In addition, any infants who had a positive toxicologic screen for cocaine or other illicit drugs or were showing drug withdrawal symptoms at birth were excluded Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 29 and 30 days, and mean weight was 993 ± 275 and 942 ± 322 g, for KMC and control infants, respectively | |
| Interventions | KMC group: SSC involved included the infant clothed in only a diaper and hat, held upright between the mother's breasts, with the mother and infant covered with a blanket (n = 25) Control group: Standard contact involved a fully clothed infant wrapped in a blanket and held cradled in his or her mother's arms (n = 25) During the study, the mother‐infant dyad was observed participating in SSC or standard contact once each weekday until bottle feedings and breastfeedings were initiated, or for a maximum of 10 days. The duration of the SSC and of standard contact sessions was 10 minutes per day Level of care: special care nursery of a hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: at 1, 3, and 6 months after hospital discharge | |
| Outcomes | Breastfeeding and physiological data | |
| Notes | No data on percentage of LBW infants who met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Shuffling of envelopes |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | 21 mothers of 25 infants allocated to KMC group, and 20 mothers of 25 infants to standard contact group. One mother in the KMC group lost to follow‐up after discharge. Two mothers in the control group excluded because they wanted to participate in the KMC group |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Kebangsaan, Malaysia | |
| Participants | Number of infants: 128 Inclusion criteria: very low‐birthweight infants (< 1501 g) in stable condition, nursed in a closed incubator, not requiring ventilatory support other than nasal continuous positive airway pressure, able to tolerate enteral feeds of ≥ 50% of required fluid volume, having ≥ 1 parent or guardian who was willing to participate in the study Exclusion criteria: lethal or major malformations, severe perinatal asphyxia, with evidence of hypoxic ischemic encephalopathy, transfer to another hospital, abandoned by parents, parental refusal to participate Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Median age at recruitment was 24.5 and 20.5 days, and median weight was 1514 and 1492 g, for KMC and control infants, respectively | |
| Interventions | KMC group: Parent held the infant prone on naked chest, in a semi‐upright position, and between his/her breasts. Infants wore only a nappy and a bonnet. Both parent and infant were covered with a thermal blanket. Median duration of SSC was 1 hour per day with a mean total duration of 12.7 ± 5.0 days (n = 65) Control group: Infants were not exposed to SSC while in the NICU All mothers were encouraged to breastfeed their infants (n = 63) Level of care: NICU of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: clinically well, able to tolerate oral feeds totally, weight gain ≥ 10 g/d, no apnea, bradycardia, and/or desaturation for ≥ 5 consecutive days Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Duration of hospital stay, weight gain, weekly increase in head circumference, breastfeeding rate at discharge, sepsis, mortality at discharge | |
| Notes | 43% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Shuffling of envelopes |
| Allocation concealment (selection bias) | Low risk | Numbered sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | High risk | 8 infants in the KMC group (12.3%) excluded because SSC sessions were carried out on < 50% of hospital stay days after recruitment |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Multicenter randomized controlled trial conducted in Addis Ababa (Ethiopia), Yogyakarta (Indonesia), and Merida (Mexico) | |
| Participants | Number of infants: 285 Inclusion criteria: infants with birthweight between 1000 and 1999 g without gestational age limits, no dependency on oxygen and/or i.v. fluids, ability (at least partial) to feed, no visible major malformation, mother present and willing to collaborate Exclusion criteria: unreported Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Median age (range) at recruitment was 10 (1 to 74) and 8 (1 to 40) days, and and mean weight (SD) was 1584 (223) and 1574 (251) g, for KMC and control infants, respectively | |
| Interventions | KMC group: Infants were kept in close and continuous SSC, between the mother's breasts, naked except for a diaper and a hat covered across their backs with their mother's clothes, day and night, for an average of about 20 hours/d, including when the mother was asleep. The mother was replaced occasionally, for a few hours, by another person, usually the father or a member of the family. For short absences of the mother (< 1 hour), the baby was left on the mother's bed, covered by a blanket (n = 149) Control group: Infants were kept in a warm room in Addis Ababa, with open cribs and the possibility of rewarming in a bulb‐heated cot, and in incubators in the other 2 hospitals. SSC with their mothers was not allowed (n = 136) Level of care: neonatal units of teaching hospitals Human resources: doctors and nurses Criteria for infant discharge from the hospital: weight ≥ 1500 g, clear upward growth trend (≥ 15 g/kg/d) and stable temperature for ≥ 3 days, satisfactory ability to suck, good general conditions, mother considered capable of good home care Scheme for follow‐up of infants after discharge: ≥ 4 times, at 3, 10, 20, and 30 days, and as usually scheduled at each hospital afterward | |
| Outcomes | Severe illness, hypothermia, hyperthermia, breastfeeding, weight gain, neonatal death, acceptability to health workers, acceptability to mothers, costs | |
| Notes | 44% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Unclear risk | Number of infants lost to follow‐up or excluded after randomization not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Unclear risk | In Indonesia, randomization was carried out in blocks of 6 with stratification by weight, which could make prediction of future assignments possible in an unblinded trial when assignments are revealed subsequent to recruitment into the trial |
| Methods | Randomized controlled trial carried out in Bogotá, Colombia | |
| Participants | Number of infants: 777 Inclusion criteria: infants from singleton or multiple pregnancies with birthweights ≤ 2000 g, with a mother or a relative able to understand and willing to follow general program instructions. Infants were eligible when they had overcome major problems of adaptation to extrauterine life, had received proper treatment for infection or a concomitant condition, sucked and swallowed properly, and had achieved a positive weight gain Exclusion criteria: referred to another institution, plans to leave Bogotá in the near future, life‐threatening or major malformations, early detected major conditions arising from perinatal problems, parental or family refusal to comply with the follow‐up program; for those assigned to the KMC group, refusal to comply with specifics of the intervention Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: At recruitment, median age (range) was 4 (1 to 60) and 3 (1 to 55) days, and mean weight (SD) was 1678 (226) and 1715 (228) g, for KMC and control infants, respectively | |
| Interventions | KMC group: Infants were kept 24 hours a day in a strict upright position, in SSC, while firmly attached to the mother's chest. Infants were breastfed regularly, although premature formula supplements were administered if necessary (n = 396) Control group: Infants were kept in an incubator until they were able to regulate temperature and were thriving. Parents' access to their babies was severely restricted (n = 381) Level of care: pediatric hospital (KMC infants) and NICU of a tertiary care hospital (controls) Human resources: doctors and nurses Criteria for infant discharge from the hospital: (1) For infants in the KMC group: temperature regulated in the kangaroo position, adequate weight gain, completion of treatment, if any; ability to be fed by direct suction from the breast or expressed milk, adequate sucking‐swallowing‐breathing coordination, and ability of mother to care for her baby using the kangaroo method at home. Infants were discharged from the hospital regardless of their weight or gestational age. (2) For infants in the control group: weight ≥ 1700 g Scheme for follow‐up of infants after discharge: at least once a week until 40 weeks' postmenstrual age; then, monthly up to 3 months' corrected age, every 6 weeks until at least 6 months' corrected age, and every third month until 12 months' corrected age | |
| Outcomes | At 40 to 41 weeks' postmenstrual: mortality, infant growth, length of hospital stay, infection, breastfeeding, and mother‐infant attachment At 12 months' corrected age: neurodevelopmental disability, and social and home environment | |
| Notes | 72% of LBW infants met eligibility criteria. Informed consent was not asked of parents of infants allocated to the control group. Additional data provided by Dr Nathalie Charpak | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Person managing allocation aware of weight at birth and whether the infant was a twin or a triplet |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | High risk | Infants allocated to KMC group were managed in a pediatric hospital, whereas infants allocated to control group remained in an NICU of a tertiary care hospital |
| Incomplete outcome data (attrition bias) | Low risk | 31 infants (4%) (KMC 14, control 17) excluded after randomization owing to pre‐existing neurological impairment, or fetal intrauterine infection not detected at time of randomization. Follow‐up at 40 to 41 weeks' corrected gestational age incomplete for 67 (8.6%) survivor infants (KMC 33, control 34), but mortality data available for 30 of these, yielding mortality data for 364 vs 345 |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | High risk | Use of blocked randomization (block size of 4), which could make possible prediction of future assignments in an unblinded trial when assignments are revealed subsequent to recruitment of the person into the trial |
| Methods | Randomized controlled trial conducted in Bali, Indonesia | |
| Participants | Number of infants: 93 Inclusion criteria: infants with birthweight between 1500 and 2250 g, with Apgar score > 6 at 5 minutes, and mother willing to follow study instructions Exclusion criteria: infants with major congenital malformations, cardiopulmonary problems, critical illness (sepsis, necrotizing enterocolitis, intracranial bleeding); twin gestation or complicated pregnancy and/or labor; mothers with history of drug abuse, psychiatric disorders, or cesarean section, or unable to take care of themselves or their babies Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean birthweight at recruitment was 2034 ± 159 and 1988 ± 176 g for KMC and control infants, respectively. No data on infant age at recruitment. However, researchers mentioned that KMC was started "in the first day or in several hours after birth" | |
| Interventions | KMC group: Infants were kept in close SSC with the mother whilst in vertical position. Specially tailored kangaroo suits were used by mother‐infant pairs to enable SSC. Mean duration of KMC was 10.0 ± 1.8 hours per day (range, 5.3 to 13.5 hours) (n = 48) Control group: Infants were kept in incubators or open cribs in warm rooms (n = 45) Level of care: NICU of a public hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Hypothermia, birthweight regain, sepsis, mortality | |
| Notes | 37% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | High risk | Unblinded assessors |
| Incomplete outcome data (attrition bias) | Low risk | One infant (1%) lost to follow‐up; 4 (4.1%) excluded after randomization owing to sepsis |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | High risk | Use of block randomization (block size of 6), which could make possible prediction of future assignments in an unblinded trial when assignments are revealed subsequent to recruitment of the person into the trial |
| Methods | Randomized controlled trial carried out in Rohtak, India | |
| Participants | Number of infants: 110 Inclusion criteria: infants with birthweight ≤ 1800 g, stable cardiopulmonary status, Apgar score ≥ 7 at 1 and 5 minutes, tolerating enteral feeds, and maintaining temperature Exclusion criteria: infants sick, unstable, or with major congenital malformations, or whose mothers were unwell and unable to come or refused consent Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 1.7 ± 0.5 days, and mean birthweight was 1690 ± 110 and 1690 ± 120 g, for KMC and control infants, respectively. No data on infant weight at recruitment | |
| Interventions | KMC group: Infants were kept in SSC, between the mother's breasts, naked except for a cap and nappy, for ≥ 6 hours per day. Duration of KMC in the first month was 10.2 ± 1.5 hours per day, in the second month 10.0 ± 1.6, and in the third month 9.0 ± 1.4. The gown covered the baby's trunk and extremities, but not the head. KMC was given for a minimum of 1 hour at a stretch and was continued for as long as it was comfortable for baby and mother. When not receiving KMC, infants received standard care under a warmer or incubator. Infants continued to receive KMC after they were shifted to the mother in the ward (n = 50) Control group: Infants were kept in a warmer or incubator. Mothers were allowed to visit their babies and touch and handle them. Infants were shifted to the mother in her bed but did not receive KMC (n = 50) Level of care: neonatal unit of a public hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: weekly until 3 months of age | |
| Outcomes | Attachment between mother and infant at 3 months' follow‐up; duration of hospital stay; breastfeeding; weight, length and circumference head gain | |
| Notes | No data on percentage of LBW infants who met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Unclear risk | 10 infants (9.1%) lost to follow‐up. Number of infants lost to follow‐up in each intervention group not reported. Of the remaining 100, 50 received KMC and 50 standard care |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial conducted in Hyderabad, India | |
| Participants | Number of infants: 140 Inclusion criteria: infants with birthweight < 1500 g, tolerating spoon feeds of 150 mL/kg/d, and hemodynamically stable (not receiving oxygen or respiratory support, no apnea for 72 hours, not receiving intravenous fluids) Exclusion criteria: major malformations, refused consent Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 14.1 ± 10.3 and 13.7 ± 10.2 days, and mean weight was 1191 ± 131 and 1223 ± 125 g, for KMC and control infants, respectively | |
| Interventions | KMC group: Infants were kept in SSC, between the mother's breasts, in an upright position, dressed with a cap, socks, and diaper, and supported at the bottom with a cloth sling/binder, for ≥ 8 hours per day. When not receiving KMC, infants were placed in open cribs (n = 71) Control group: Infants were kept in a warmer or incubator. Mothers were allowed to visit their babies and were encouraged to perform infant care activities such as diaper change, oil massage, and paladai feeding (n = 69) Level of care: "kangaroo ward" (KMC infants) and neonatal intermediate care unit (controls) at a level III tertiary care hospital Human resources: Infants in KMC group were cared for solely by their mothers, assisted by a trained nurse. Infants in control group were cared for by doctors and nurses Criteria for infant discharge from the hospital: (1) For infants in KMC group: weight ≥ 1300 g or weight gain ≥ 10 g/d on 3 consecutive days if weight at randomization was > 1300 g. (2) For infants in control group: weight ≥ 1300 g, weight gain ≥ 10 g/d on 3 consecutive days, and skin temperature of 36°C to 37°C in the servo mode of the incubator with heater output < 25% Scheme for follow‐up of infants after discharge: weekly until 40 weeks' postmenstrual age | |
| Outcomes | At 40 weeks' postmenstrual age: infant growth At discharge: breastfeeding, sepsis, hypothermia, apnea, hypoglycemia, length of hospital stay, mortality | |
| Notes | No data on percentage of LBW infants who met eligibility criteria. Additional data provided by Dr Srinivas Murki | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Web‐based random number generator |
| Allocation concealment (selection bias) | Low risk | Numbered sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Low risk | Physician who assessed growth outcomes was blinded to infants' intervention group |
| Incomplete outcome data (attrition bias) | Low risk | 4 infants (2.9%) lost to follow‐up (KMC 3, control 1); no exclusions |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Mumbai, India | |
| Participants | Number of infants: 89 Inclusion criteria: infants with birthweight ≤ 1800 g, stable cardiopulmonary status, Apgar score ≥ 7 at 5 minutes, and on feeds (breastfeeds or spoon wati feeds with expressed breast milk) Exclusion criteria: infants sick and unstable, or with major congenital malformations, or whose parents refused consent Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age (range) at enrollment was 3.2 (1 to 8) days for both groups. Mean birthweight was 1467 ± 228 and 1461 ± 217 g for KMC and control infants, respectively. No data on infant weight at recruitment | |
| Interventions | KMC group: Infants were placed on mother's chest in between the breasts in a vertical position, supported by a cloth dupatta, with mothers seated in a semi reclining position, for a mean of 9.8 ± 3.7 hours per day. In case of any problem, the baby was transferred to conventional care, and after stabilization was transferred back to KMC, which was continued till discharge (n = 44) Control group: Infants were kept in radiant warmers (n = 45) More than 95% of infants in both groups received exclusive breastfeeding; the remaining were supplemented by banked human milk. Mothers in both groups were allowed to enter and handle the babies at any hour of the day, change diapers, and breastfeed the babies Level of care: NICU of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: weight gain for ≥ 3 consecutive days, maintenance of temperature without the need for a warmer, feeding well on breastfeeds or wati spoon‐feeds, and mother confident of taking care of the infant at home Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Mortality, morbidity (hypothermia, hyperthermia, sepsis, apnea), onset of breastfeeding, duration of hospital stay, weight at discharge | |
| Notes | No data on percentage of LBW infants who met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed envelope method |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial conducted in Kolhapur, India | |
| Participants | Number of infants: 120 Inclusion criteria: stable infants with birthweight < 2000 g Exclusion criteria: infants critically ill requiring ventilator support or inotropic support, or with chromosomal and life‐threatening congenital anomalies, or whose mother was critically ill or unable to comply with the follow‐up schedule Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 3 and 4 days, and mean weight was 1610 ± 200 and 1627 ± 204 g, for KMC and control infants, respectively | |
| Interventions | KMC group: Infants were kept in SSC using a specially tailored "kangaroo bag" made of soft flannel cloth on the reclining cot in the semi upright position with the help of pillows. Mothers were encouraged to keep the baby in KMC as long as possible during the day and night for a minimum period of 1 to 2 hours at a time. When the baby was receiving intravenous fluids, the mother provided kangaroo care while seated in a comfortable chair placed close to the baby's cradle. Mean duration of KMC was 11.5 hours per day. No data on total number of days that KMC was given after enrollment (n = 60) Control group: Infants were managed under a servo‐controlled radiant warmer or in a cradle under hot lamp in NICU, adequately clothed and covered (n = 60) All babies were exclusively breastfed and also received calcium, phosphorus, and multivitamin supplements. Infants who developed a life‐threatening event or required phototherapy were temporarily withdrawn from the KMC group Level of care: NICU of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: weight gain of 10 to 15 g/kg/d for ≥ 3 consecutive days, maintenance of temperature without assistance, feeding well, and mother confident of taking care of the infant at home Scheme for follow‐up of infants after discharge: weekly until 40 weeks' postmenstrual age in preterm infants, or until a weight of 2500 g was reached in term SGA infants. Home visits were not possible | |
| Outcomes | Gain in weight, length, and head circumference; hospital stay; hypothermia; sepsis; apnea; acceptability of KMC; breastfeeding | |
| Notes | No data on percentage of LBW infants who met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomization |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | High risk | No information on infants lost to follow‐up nor on exclusions. However, it was stated in the Discussion section that poor follow‐up in the control group was a limitation of this study |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial conducted in Mahajanga, Madagascar | |
| Participants | Number of infants: 73 Inclusion criteria: infants with birthweight < 2500 g, < 24 hours post birth, no serious malformation, relatively stable clinical condition (oxygen saturation ≥ 95%; heart rate > 100 beats/min; respiratory rate < 60 times/min; capillary refilling time < 3 seconds), and healthy mother and/or other family members willing to practice KMC Exclusion criteria: prolonged apnea (> 20 seconds) and intravenous infusion Infant stabilization status at trial entry: relatively stabilized Infant age and weight at trial entry: Mean age at recruitment was 19.8 ± 14.3 and 33.0 ± 13.2 hours, and mean weight was 2075 ± 272 and 2078 ± 292 g, for early‐onset KMC and late‐onset KMC infants, respectively | |
| Interventions | Early KMC group: Infants were kept in direct and continuous SSC (without underwear, except for a diaper, a warm hat, and socks for the baby) for as long as possible. SSC was begun as soon as possible, within 24 hours post birth (n = 37) Late KMC group: Initially, infants were kept in an incubator or radiant warmer. Later, infants were covered with cotton cloth and were laid beside their mothers. KMC was begun after complete stabilization (generally after 24 hours post birth) of infant (n = 36) After KMC was initiated, all participants were encouraged to continue KMC for as long as possible during hospitalization and after discharge. Other family members assisted the mother occasionally in performing continuous KMC Level of care: neonatal unit of a referral university hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: at 14 and 28 days of age | |
| Outcomes | Primary outcome: mortality at 4 weeks of age Secondary outcomes: morbidity; severe infection; re‐admission to hospital; adverse events (hypothermia, hyperthermia, bradycardia and/or tachycardia, and prolonged apnea) at 4 weeks of age; body weight changes from birth to 24 hours, 48 hours, 14 days, and 28 days post birth; length of hospital stay; discharge within 7 days post birth; exclusive breastfeeding at 24 and 48 hours, 2 and 4 weeks, and 6 months post birth; mortality; re‐admission to hospital; nutritional indicators at 6 to 12 months of age | |
| Notes | 52% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Minimization method by software "minim" |
| Allocation concealment (selection bias) | Low risk | Software automatically provided random allocation for each participant |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Low risk | A neonatologist who was masked to allocation of participants and had no contact with participants determined the classification of morbidities using interview records and medical charts |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Aurora, Colorado, United States | |
| Participants | Number of infants: 60 Inclusion criteria: healthy infants with gestational age between 32 and 34 weeks, oxygen requirement < ½ liter O2 per nasal cannula, infant without umbilical lines, intraventricular hemorrhage, physical anomalies or anticipated major surgery, mother fluent in English or Spanish without recorded or stated illicit drug use, or diagnosis of serious chronic illness Exclusion criteria: unreported Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 15.0 ± 6.7 and 15.0 ± 4.9 days, and mean birthweight was 1990 ± 450 and 1880 ± 340 g, for KMC and control infants, respectively | |
| Interventions | KMC group: infant in SSC on mother's chest for 60 consecutive minutes at least once daily over 8 weeks (n = 31) Control group: infant wrapped in blanket and held in mother's arms for 60 consecutive minutes at least once daily over 8 weeks (n = 29) In both conditions, weekly home visits by an experienced registered nurse included encouragement to hold the infant, emotional support, and information about infant behavior and development. Other control group received brief social visits with no holding constraints and participated in all assessments. In the meta‐analysis, we excluded results from this last control group Level of care: initially at the hospital, then at home Human resources: nurses Criteria for infant discharge from the hospital: not applicable Scheme for follow‐up of infants after discharge: twice a week for 2 weeks, followed by weekly visits for 6 months | |
| Outcomes | Mother‐infant interaction at 6 months' follow‐up and infant vitality during the neutral‐face period of the Still‐Face Procedure | |
| Notes | No data on percentage of LBW infants who met eligibility criteria. Approximately 60% of mothers who were approached declined to be included in the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Four researchers assessed outcome measures. Two outcome assessors were blinded to the hypotheses of the study but not to group assignment of mother‐infant dyads. The other 2 researchers were blinded to group assignment and hypotheses |
| Incomplete outcome data (attrition bias) | High risk | 87 infants were randomized: 31 to KMC, 29 to traditional holding, and 36 to control. At 6 months of age, 8 infants (9.2%) were lost to follow‐up and 14 (16.1%) were excluded (8 withdrawn for maternal reasons and 6 because of technical problems during videotaping) |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial conducted in Karamsad, India | |
| Participants | Number of infants: 100, of whom 45 were LBW Inclusion criteria: stable infants delivered vaginally with birthweight ≥ 1800 g Exclusion criteria: infants delivered by cesarean section or needing any resuscitation measures or with any congenital malformation at birth Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age was 43 ± 13 minutes in the KMC group and 30 to 60 minutes in the control group. Mean birthweight (and weight at recruitment) was 2622 ± 399 g and 2589 ± 443 g for KMC and control infants, respectively | |
| Interventions | KMC group: Mothers started SSC 30 minutes to 1 hour after delivery and continued for as long as possible in the first 24 hours, with each session lasting a minimum of 60 minutes. SSC was discontinued after 24 hours and conventional care was provided for next 24 hours of life. Mean duration of KMC was 17.0 ± 0.3 hours during first 24 hours (n = 22) Control group: Infants were kept clothed (including head cap) and covered with a blanket with their mother (bedding in) for first 48 hours (n = 23) In both groups, infants were taken under radiant warmers immediately after delivery and were exclusively breastfed Level of care: maternity ward of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Hypothermia within first 48 hours of life | |
| Notes | 43% of infants met eligibility criteria. Results for the 45 LBW infants reported separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Web‐based software (WINPEPI) |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial conducted in New Delhi, India | |
| Participants | Number of infants: 28 Inclusion criteria: infants with birthweight < 1500 g, stable cardiopulmonary status, tolerating enteral feeds, and maintaining temperature in the thermoneutral environment Exclusion criteria: infants whose mothers were unable to come to the nursery because of illness or disability Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Median age at initiation of KMC was 11.8 days. Mean birthweight was 1219 ± 186 and 1271 ± 170 g for KMC and control infants, respectively. No data on infant weight at recruitment | |
| Interventions | KMC group: Infants were kept between the mother's breasts for ≥ 4 hours per day in not more than 3 sittings. The gown covered the baby's trunk and extremities but not the head. When not receiving KMC, infants received standard care under a warmer or incubator (n = 14) Control group: Infants were kept in a warmer or incubator. Mothers were allowed to visit their babies and touch and handle them (n = 14) Breastfeeding guidelines were followed for both groups and lactational counseling was emphasized to ensure breast milk feeding Level of care: NICU of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: weight > 1400 g, “adequate” weight gain, gestation over 34 weeks, only on enteral feeds, no intravenous medications, no overt illness, exclusive breastfeeding, and mother confident of taking care of the infant at home Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Weight gain, breastfeeding, duration of hospitalization | |
| Notes | No data on percentage of LBW infants who met eligibility criteria. Infants in KMC group required positive‐pressure ventilation, continuous positive airway pressure, and oxygen therapy over greater duration than infants in control group, indicating that these infants were sicker before enrollment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Neonatal complications prospectively recorded but not reported |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Darwin, Australia | |
| Participants | Number of infants: 30 Inclusion criteria: premature or small for gestational age infants born at 30 or more weeks' gestation or corrected age, with 5‐minute Apgar of ≥ 5, medically stable, without congenital abnormalities or central nervous system impairment. Infants could have received nasal continuous positive airway pressure in place or a nasal cannula Exclusion criteria: phototherapy within previous 24 hours, resuscitated infants, mothers with a history of drug use Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 31.5 ± 2.7 days and mean weight was 1690 ± 333 g, respectively | |
| Interventions | KMC group: Infants were dressed in only a diaper, with a bonnet added for smaller infants. They were placed on the mother's skin and covered with a light blanket. Mean duration of KMC was 1.6 ± 0.9 hours per day, 5 days a week (n = 16) Control group: Infants were swaddled in infant clothing and a light blanket. They had contact with the mother only through normal clothing (n = 14) Breastfeeding was permitted as desired in both groups Level of care: neonatal intensive care nurseries of 2 hospitals Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: at 6 weeks after discharge or at 3 months of age, whichever was later, and at 6 months of age | |
| Outcomes | Weight gain, length of stay in hospital, temperature, breastfeeding | |
| Notes | No data on percentage of LBW infants who met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Shuffling envelopes |
| Allocation concealment (selection bias) | Low risk | Numbered envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial conducted in Connecticut, United States | |
| Participants | Number of infants: 60 Inclusion criteria: very low birthweight infants (< 1501 g) with gestational age ≤ 32 weeks, with minimal ventilatory support or extubated on nasal continuous positive airway pressure or nasal canula, with hemodynamic stability Exclusion criteria: mother's age < 18 years, history of illicit drug use during pregnancy, clinical evidence of perinatal asphyxia, potential transfer within the first month after birth, presence of a major congenital anomaly, planned adoption, grade III or IV intraventricular hemorrhage, fetal growth restriction, suspected sepsis Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at trial entry was 19 days, and mean weight was 1021 ± 268 g and 1002 ± 219 g for KMC and control infants, respectively | |
| Interventions | KMC group: Infants were held in a prone semi upright position at approximately a 45° angle, in direct SSC with the parent's chest. Infants wore only a diaper, and their backs were covered with a blanket. Mean duration of KMC was 1.3 ± 0.7 hours per day for an average of 15 ± 16 days (n = 33) Control group: Parents removed their infants from the incubator and held them in their arms in supine position with eye‐to‐eye contact. Infants wore diapers and T‐shirts and were wrapped in a blanket (n = 27) Level of care: NICU of a hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: not performed | |
| Outcomes | Mortality at discharge; sepsis; necrotizing enterocolitis; intraventricular hemorrhage; weight, head circumference, and length at discharge; rate of weight gain and head circumference growth; total weight gain and head circumference growth; breastfeeding at discharge; hospital stay | |
| Notes | 19% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Numbered sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Quito, Ecuador | |
| Participants | Number of infants: 300 Inclusion criteria: singleton infants weighing < 2000 g, with no serious congenital abnormalities or respiratory, metabolic, or infectious disease. Infants had to be stabilized for 24 hours before enrollment (temperature between 36.5°C and 37.0°C); acceptable tolerance of food; stable weight Exclusion criteria: unreported Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 13.0 ± 10.5 days, and mean weight was 1618 ± 317 g, respectively | |
| Interventions | KMC group: Infants were kept in an upright position, in SSC contact (diapers allowed) against the mother's breasts, and had frequent breastfeeding. SSC was reported by 68% of mothers at follow‐up of 1 month, 47% at 1.5 months, 20% at 2 months, and 7% at 3 months (n = 140) Control group: Infants stayed in an incubator or thermal crib and were breastfed at scheduled times (n = 160) Level of care: NICU of a maternity hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow‐up of infants after discharge: at 1, 1.5, 2, 3, 4, 5, and 6 months of age | |
| Outcomes | Severe illness (lower respiratory tract disorder, apnea, aspiration, pneumonia, septicemia, general infection), moderate illness (urinary infection), mild illness (upper respiratory tract disorder, dermatitis, jaundice, hip displacement), diarrhea, infant growth (weight, length, upper arm and head circumference), duration of hospital stay, re‐admission, costs of care | |
| Notes | 53% of LBW infants met eligibility criteria. Additional data provided by Dr Nancy L. Sloan | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | Low risk | Outcome data reported for 131 KMC infants and 152 controls. 17 infants (5.7%) lost to follow‐up (KMC 9, control 8); no exclusions |
| Selective reporting (reporting bias) | Unclear risk | Secondary outcomes such as infant growth indices at follow‐up and costs of care were mentioned but were not reported adequately |
| Other bias | Unclear risk | Trial was stopped early because a highly significant difference (P value < 0.02 at 2 months, P value < 0.005 at 6 months) in severe morbidity arose. No information about whether this was a planned interim analysis |
| Methods | Randomized controlled trial conducted in Mumbai, India | |
| Participants | Number of infants: 220 Inclusion criteria: singleton infants with birthweight < 2000 g Exclusion criteria: infants critically ill requiring ventilatory or inotropic support, or with chromosomal and life‐threatening congenital anomalies, or requiring transfer, or whose mothers were critically ill or unable to comply with the follow‐up schedule Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean age at recruitment was 3.7 ± 2.8 and 2.3 ± 1.9 days, and mean weight was 1608 ± 278 and 1691 ± 273 g, for KMC and control infants, respectively | |
| Interventions | KMC group: Infants were kept in SSC using a specially tailored "kangaroo bag" made of soft flannel cloth on the reclining cot in the semi upright position with the help of pillows. Mothers were encouraged to keep the baby in KMC as long as possible during the day and night, for a minimum period of 1 to 2 hours at a time. When not in KMC, the baby was placed under a servo‐controlled radiant warmer or in a cradle under a hot lamp adequately clothed and covered. Mean duration of KMC was 13.5 hours per day, with a mean total duration of 33.8 ± 15.1 days (n = 108) Control group: Infants were managed under a servo‐controlled radiant warmer or in a cradle under a hot lamp in the NICU adequately clothed and covered (n = 112) All babies were exclusively breastfed. Infants who developed a life‐threatening event or required phototherapy were temporarily withdrawn from the KMC group Level of care: NICU of a tertiary care hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: weight gain of 10 to 15 g/kg/d for ≥ 3 consecutive days, maintenance of temperature without assistance, feeding well, and mother confident of taking care of the infant at home Scheme for follow‐up of infants after discharge: weekly until 40 weeks' postmenstrual age in preterm infants, or until a weight of 2500 g was reached in term SGA infants | |
| Outcomes | Infant growth (weight, length, head, chest, mid‐arm circumference, and foot length), mortality, morbidity (hypothermia, hyperthermia, hypoglycemia, sepsis, apnea in < 1500 g, other minor illness), duration of hospital stay | |
| Notes | 63% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomization |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unreported |
| Incomplete outcome data (attrition bias) | High risk | 49 infants (22.3%) lost to follow‐up (KMC 11 [10.2%], control 38 [33.9%]); 14 babies (6.4%) were excluded (KMC 5, control 9) because they did not receive assigned care |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods section adequately reported or explained in Results |
| Other bias | Unclear risk | Groups were different at baseline in 2 important variables: (1) weight at enrollment (1608 ± 278 g and 1691 ± 273 g for KMC and control infants, respectively; P value = 0.03), and (2) age at enrollment (3.7 ± 2.8 days and 2.3 ± 1.9 days for KMC and control infants, respectively; P value < 0.01) |
| Methods | Randomized controlled trial carried out in London, United Kingdom | |
| Participants | Number of infants: 71 Inclusion criteria: infants from singleton or twin pregnancy with weight < 1500 g, stable breathing with no oxygen requirement, and ≥ 1 parent speaking fluent English. Stable infants were not excluded if they had congenital malformations such as hydronephrosis or scoliosis, nor if they had intracranial lesions such as periventricular leukomalacia or ventricular dilatation Exclusion criteria: unreported Infant stabilization status at trial entry: stabilized Infant age and weight at trial entry: Mean (range) age at enrollment was 16 (1 to 66) days. Mean birthweight was 1152 ± 220 g and 1135 ± 263 g for KMC and control infants, respectively. No data on infant weight at recruitment | |
| Interventions | KMC group: Infants were kept in an upright position, in SSC between the mother's breasts, with a cardiac or respiration monitor attached. Mean (range) duration of KMC was 0.6 (0 to 1.5) hours per day (n = 35) Control group: Mother was encouraged to visit as much as she liked and helped to take her baby out of the incubator for a cuddle. However, baby and mother remained clothed Care was taken that the normal contact group would receive no less attention from the nursing staff (n = 36) Level of care: NICU of a hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: unreported Scheme for follow up of infants after discharge: at 6, 9, and 12 months of age | |
| Outcomes | Breastfeeding and infant's behavior at 6 months of age, mother's feelings about the infant at discharge and at 6 months of age | |
| Notes | 50% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Shuffling of envelopes |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | High risk | No |
| Incomplete outcome data (attrition bias) | Low risk | No infants lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Non‐significant results for some outcome measures (eg, mother's feelings about the infant at discharge and at 6 months' follow‐up) were mentioned but were not reported adequately |
| Other bias | Low risk | Other biases not identified |
| Methods | Randomized controlled trial carried out in Addis Ababa, Ethiopia | |
| Participants | Number of infants: 123 Inclusion criteria: infants with birthweight < 2000 g, singletons unless 1 of the twins died, no major congenital malformations, and mother healthy and willing to participate Exclusion criteria: unreported Infant stabilization status at trial entry: non‐stabilized Infant age and weight at trial entry: Mean age at enrollment was 10.0 and 9.8 hours, and mean birthweight was 1515 g and 1472 g for KMC and control infants, respectively | |
| Interventions | Early KMC group: Infants were kept in continuous SSC with their mother beginning immediately after birth or within the first 24 hours of life (before stabilization). The mother kept her newborn infant between the breasts, in close contact with her body and covered with her clothes day and night. Breastfeeding was the standard feeding method. However, the mother could also feed her baby with formula milk using tube or cup when needed. KMC could be combined with a heated room during low environmental temperatures (n = 62) Control group: Infants were kept in a heated room with overhead lamp warmers and received oxygen therapy and breast, tube, cup, or mixed feeding (n = 61) The 2 methods of care were applied and continued until the baby was considered stabilized (stable temperature, stabilized cardiovascular status, satisfactory ability to suck, and good general condition); then both group of babies were transferred to the ward for routine kangaroo care service. KMC was continued at home after discharge in both groups Level of care: neonatal unit of a teaching hospital Human resources: doctors and nurses Criteria for infant discharge from the hospital: (1) for discharge from the study to the ward routine kangaroo care service: stable temperature, stabilized cardiovascular status, satisfactory ability to suck, and good general condition; (2) for discharge from the hospital: "according to the hospital's protocol" Scheme for follow‐up of infants after discharge: unreported | |
| Outcomes | Death, serious illness (sepsis, diarrhea, pneumonia, aspiration, pneumonia), mothers' feeling about the method of care | |
| Notes | 48% of LBW infants met eligibility criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants: no/unfeasible; blinding of clinical staff: no/unfeasible |
| Blinding of outcome assessment (detection bias) | High risk | No |
| Incomplete outcome data (attrition bias) | Unclear risk | No information on infants lost to follow‐up; no exclusions |
| Selective reporting (reporting bias) | High risk | Great majority of outcomes listed in Methods section of the article, such as weight gain, mild/moderate and severe illness, sepsis, diarrhea, pneumonia, aspiration, and mother's feelings, collected but not reported |
| Other bias | Low risk | Other biases not identified |
KMC = kangaroo mother care
LBW = low birthweight
SSC = skin‐to‐skin contact
SGA = small for gestational age
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a randomized controlled trial | |
| Study compared SSC (N = 48) and standard care (N = 43) in preterm infants born at 32 to 36 weeks' gestation with birthweight between 1300 and 3000 g. No data on daily duration of KMC. Study did not report results for clinical outcomes | |
| Not a randomized controlled trial | |
| Study assessed effect of KMC (N = 25) vs standard care (N = 25) on mental health of mothers of LBW infants in the postpartum period. No data on neonatal morbidity and mortality | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Study compared SSC (N = 21) from birth and standard care (N = 14) in LBW infants. Study period was 6 hours. Study reported results only for physiological parameters. Newborns receiving SSC from birth were significantly advantaged in some measures of cardiorespiratory stability | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Study compared early KMC (N = 52) and standard care (N = 48) in late preterm infants (32 to < 37 weeks' gestation). Study included infants with birthweight ≥ 2500 g. No data for subgroup of infants < 2500 g at birth. KMC infants had lower infant teaching scores at 6 months than controls ‐ a difference that disappeared thereafter. Feeding scores at 6 and 12 months' follow‐up were similar for KMC infants and controls | |
| Study compared SSC and incubator care for rewarming in 80 low‐risk hypothermic infants (clinically stable with admission weight ≥ 1500 g) | |
| Study compared SSC (N = 17) and standard contact (N = 17) in infants born at 34 to 36 weeks' gestation. 20 of 34 included infants (59%) had birthweight > 2500 g. No data for the remaining 14 LBW infants | |
| Not a randomized controlled trial | |
| Study evaluated acceptance of KMC within a trial of impact of a package of essential newborn care | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Study compared SSC (N = 27) and standard care (N = 26) in infants hospitalized in the NICU, and reported results only for physiological parameters. Newborns receiving SSC had a significant increase in average temperature and arterial oxygen saturation rate | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Study compared KMC (N = 36) and standard care (N = 30) in preterm infants. Study included infants with birthweight of 1300 to 3000 g. 39% of included infants had a gestational age of 36 weeks. No data for subgroup of infants < 2500 g at birth. KMC was associated with a significantly longer breastfeeding duration and a higher frequency of exclusive breastfeeding at discharge and at 1.5, 3, and 6 months | |
| Study compared early KMC (N = 39) and use of radiant warmers (N = 39) in term infants with hypothermia problems. Mean (SD) birthweight was 3072 (393) and 2808 (428) g for KMC and control infants, respectively. After 4 hours, more infants in the KMC group had reached normal body temperature | |
| Not a randomized controlled trial | |
| Quasi‐random allocation to treatment (alternation). 74 (37 per group) infants were subjected to KMC or incubator care. Infants in the KMC group had higher mean daily weight gain, shorter stay in hospital, and better survival rates | |
| 72 infants born between 32 and 42 weeks' gestation were randomly assigned to KMC or routine care. Study included infants with birthweight > 2500 g and reported results only for breastfeeding self efficacy score at 3 months post partum. No data for subgroup of infants ≤ 2500 g at birth | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Cluster‐randomized controlled trial in which SSC was part of a preventive package of interventions for essential newborn care | |
| Study compared music during KMC (N = 15) and standard care (N = 15) in preterm infants. Study included infants with birthweight of 1505 to 3285 g. No data for subgroup of infants < 2500 g at birth. In addition, the study did not report results for clinical outcomes | |
| Not a randomized controlled trial | |
| Study compared SSC (N = 53) and no intervention (N = 49) in LBW infants hospitalized in NICU whose nostrils were colonized with methicillin‐oxacillin‐resistant Staphylococcus aureus or methicillin‐oxacillin‐resistant coagulase‐negative Staphylococcus aureus. Study reported results only for colonization status of newborns’ nostrils after 7 days of intervention | |
| Participant allocation was by a cross‐over recruitment design. Study did not report results for clinical outcomes | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Not a randomized controlled trial | |
| Randomized controlled trial that compared KMC and standard care in cardiorespiratory, thermal, and state effects in preterm infants. No data on neonatal morbidity and mortality | |
| Randomized controlled trial that compared KMC (N = 16) and standard care (N = 13) in maintenance of body warmth in preterm infants. No data on neonatal morbidity and mortality | |
| Randomized controlled trial that compared KMC (N = 11) and standard care (N = 13) for assessment of cardiorespiratory and thermal responses in preterm infants. No data on neonatal morbidity and mortality | |
| Randomized controlled trial that compared KMC (N = 14) and standard care (N = 14) for assessment of neonatal sleep organization in preterm infants. No data on neonatal morbidity and mortality | |
| Randomized controlled trial with a cross‐over design (N = 19), which assessed SSC for reducing stress of preterm infants during diaper change | |
| Study was a pragmatic, controlled trial in which participant allocation was by a cross‐over, cluster recruitment design between 2 tertiary referral NICUs. Each hospital remained in KMC or control group for 4 months, then crossed over following a washout phase, during which no recruitment was undertaken. No significant difference was found in any infant or maternal measure at any time point | |
| Quasi‐random allocation to treatment (even or odd number). Length of hospital stay was 8 ± 1 days for the KMC group and 10 ± 1.9 days for the control group (P value = 0.004) | |
| 38 infants (27 to 30 weeks' gestational age) were randomly assigned to 2 hours of KMC daily between days of life 5 and 10, or to standard incubator care. Study reported results only for physiological parameters. Infants allocated to KMC had significantly fewer events of bradycardia and oxygen desaturation than infants allocated to standard care | |
| Study compared SSC (N = 18) and standard care (N = 19) in preterm infants (32 to 36 weeks' gestation). Study included infants with birthweight ≥ 2500 g. No data for subgroup of infants < 2500 g at birth. Overall, SSC decreased infants' cortisol reactivity in response to handling, improved concordance between mothers' and infants' salivary cortisol levels, and decreased fathers' experiences of spouse relationship problems | |
| Not a randomized controlled trial | |
| Randomized controlled trial that assessed effects of skin‐to‐skin holding (N = 20) versus blanket holding (N = 20) on stress of mothers of late preterm infants (34 to 36 weeks' gestation). Study included infants with birthweight ≥ 2500 g. No data for subgroup of infants < 2500 g at birth. Overall, no significant differences in stress scores between study groups | |
| Not a randomized controlled trial | |
| Randomized controlled cluster trial in which 4165 infants were assigned to community‐based KMC or control. 40% overall and 65% of newborns who died were not weighed at birth, and missing birthweight was differential for study group. 68.6% of weighed infants had a birthweight ≥ 2500 g. No difference in overall neonatal mortality rate nor infant mortality rate | |
| Quasi‐random allocation (alternation) to KMC (N = 30) or conventional care (N = 30). Infants in KMC group had greater weight, length, and head circumference gain, and decreased risk of hypothermia compared with infants in the control group | |
| Not a randomized controlled trial | |
| Published as abstract only. Insufficient information to include this study in the systematic review, and unsuccessful attempts to locate full publication or to contact study author |
KMC = kangaroo mother care
LBW = low birthweight
SSC = skin‐to‐skin contact
SGA = small for gestational age
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomized controlled trial carried out in North Carolina and Illinois, United States |
| Participants | Number of infants: 162 Inclusion criteria: non‐critically ill preterm infants with birthweight < 1750 g Exclusion criteria: infants with congenital neurological problems (eg, congenital hydrocephalus, Down syndrome), mothers who had symptoms of substance exposure or who did not have custody of the infant or who had a risk factor that could affect their ability to administer the intervention (eg, age < 15 years; history of psychosis or bipolar disease; current diagnosis of major depression; non‐English speaking); follow‐up for 12 months unlikely Infant stabilization status at trial entry: stabilized |
| Interventions | KMC group: Infants were kept in SSC in an upright position between the mother's breasts, dressed with a diaper and a hat. Mothers were instructed to perform the intervention at least once a day, 3 times a week, and for ≥ 15 minutes during infant hospitalization, and to continue at home until the infant was 2 months' corrected age (n = 81) Control group: Mothers spent a similar amount of time each week as KMC mothers with the study nurse, discussing how to select and locate safe equipment needed to care for preterm infants at home, for example, clothes, diapers, formula, and toys. Holding was not part of the control group intervention (n = 81) Level of care: initially at the NICU, then at home Human resources: nurses |
| Outcomes | Mother‐infant relationship, maternal psychological distress, social and home environment, mother's satisfaction |
| Notes | This study examined effects of KMC vs massage with auditory, tactile, visual, and vestibular (ATVV) stimulation vs an attention control group. If included in the review, we would exclude results of the ATVV intervention group |
KMC = kangaroo mother care
LBW = low birthweight
SSC = skin‐to‐skin contact
SGA = small for gestational age
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality at discharge or at 40 to 41 weeks' postmenstrual age Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 1 Mortality at discharge or at 40 to 41 weeks' postmenstrual age. | ||||
| 1.1 All studies | 8 | 1736 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.39, 0.92] |
| 1.2 Intermittent KMC | 5 | 619 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.19, 1.81] |
| 1.3 Continuous KMC | 3 | 1117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.38, 0.96] |
| 1.4 Duration of KMC < 2 hours/d | 2 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.22, 7.73] |
| 1.5 Duration of KMC between 6 and 15 hours/d | 3 | 431 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.07, 1.64] |
| 1.6 Duration of KMC ≥ 20 hours/d | 3 | 1117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.38, 0.96] |
| 1.7 Infant age ≤ 10 days at initiation of KMC | 5 | 1412 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.36, 0.88] |
| 1.8 Infant age > 10 days at initiation of KMC | 3 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.22, 7.73] |
| 1.9 Low/middle‐income countries | 7 | 1676 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.89] |
| 1.10 High‐income countries | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.16, 17.09] |
| 1.11 infant entered into trial before stabilization | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.33, 1.00] |
| 1.12 infant entered into trial after stabilization | 7 | 1613 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.32, 1.23] |
| 2 Mortality at 6 months of age or 6 months' follow‐up Show forest plot | 2 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.48, 2.02] |
| Analysis 1.2 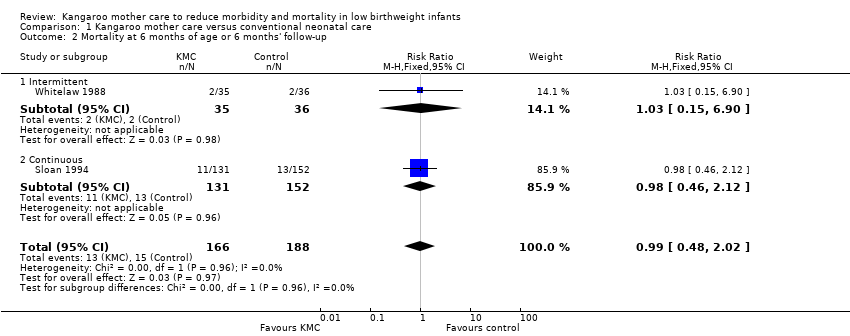 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 2 Mortality at 6 months of age or 6 months' follow‐up. | ||||
| 2.1 Intermittent | 1 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.15, 6.90] |
| 2.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.46, 2.12] |
| 3 Mortality at 12 months' corrected age Show forest plot | 1 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.27, 1.17] |
| Analysis 1.3  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 3 Mortality at 12 months' corrected age. | ||||
| 3.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Continuous | 1 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.27, 1.17] |
| 4 Mortality at latest follow‐up Show forest plot | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 4 Mortality at latest follow‐up. | ||||
| 4.1 All studies | 12 | 2293 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.48, 0.95] |
| 4.2 Intermittent KMC | 8 | 909 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.26, 1.77] |
| 4.3 Continuous KMC | 4 | 1384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.46, 0.98] |
| 4.4 Duration of KMC < 2 hours/d | 3 | 259 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.32, 4.30] |
| 4.5 Duration of KMC between 6 and 15 hours/d | 5 | 650 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.07, 1.64] |
| 4.6 Duration of KMC ≥ 20 hours/d | 4 | 1384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.46, 0.98] |
| 4.7 Infant age ≤ 10 days at initiation of KMC | 6 | 1489 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.37, 0.85] |
| 4.8 Infant age > 10 days at initiation of KMC | 5 | 678 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.53, 2.00] |
| 4.9 Low/middle‐income countries | 10 | 2162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.45, 0.93] |
| 4.10 High‐income countries | 2 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.29, 5.42] |
| 4.11 Infant entered into trial before stabilization | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.33, 1.00] |
| 4.12 Infant entered into trial after stabilization | 11 | 2170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.47, 1.13] |
| 5 Severe infection/sepsis at latest follow‐up ‐ stabilized infants Show forest plot | 8 | 1463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.36, 0.69] |
| Analysis 1.5 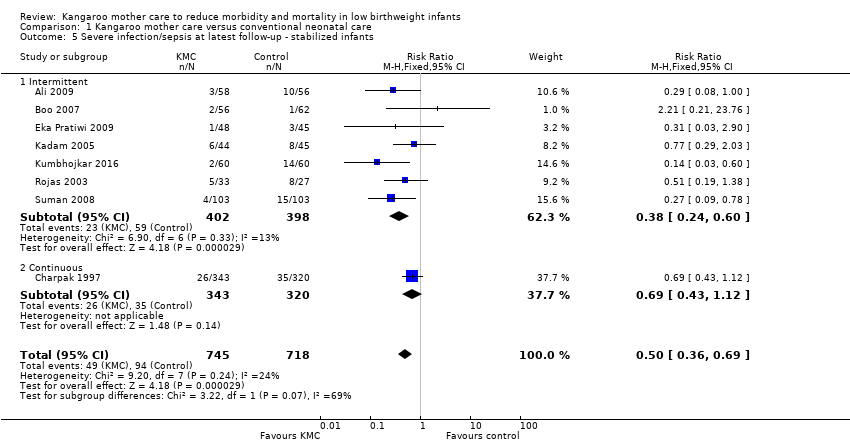 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 5 Severe infection/sepsis at latest follow‐up ‐ stabilized infants. | ||||
| 5.1 Intermittent | 7 | 800 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.24, 0.60] |
| 5.2 Continuous | 1 | 663 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.43, 1.12] |
| 6 Severe illness at 6 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.14, 0.67] |
| Analysis 1.6 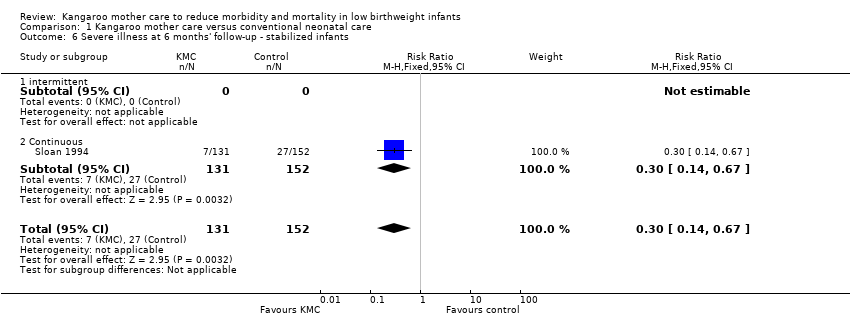 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 6 Severe illness at 6 months' follow‐up ‐ stabilized infants. | ||||
| 6.1 intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.14, 0.67] |
| 7 Nosocomial infection/sepsis at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 5 | 1239 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.22, 0.54] |
| Analysis 1.7  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 7 Nosocomial infection/sepsis at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants. | ||||
| 7.1 Intermittent | 4 | 576 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.15, 0.50] |
| 7.2 Continuous | 1 | 663 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.25, 0.93] |
| 8 Mild/moderate infection or illness at latest follow‐up ‐ stabilized infants Show forest plot | 4 | 1266 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.87, 1.88] |
| Analysis 1.8  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 8 Mild/moderate infection or illness at latest follow‐up ‐ stabilized infants. | ||||
| 8.1 Intermittent | 2 | 320 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.43, 5.38] |
| 8.2 Continuous | 2 | 946 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.53, 3.79] |
| 9 Lower respiratory tract disease at 6 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.15, 0.89] |
| Analysis 1.9 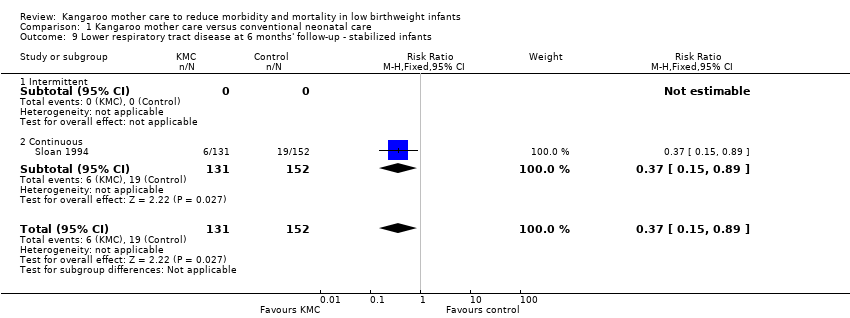 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 9 Lower respiratory tract disease at 6 months' follow‐up ‐ stabilized infants. | ||||
| 9.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.15, 0.89] |
| 10 Diarrhea at 6 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.35, 1.20] |
| Analysis 1.10  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 10 Diarrhea at 6 months' follow‐up ‐ stabilized infants. | ||||
| 10.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.35, 1.20] |
| 11 Hypothermia at discharge or at 40 to 41 weeks’ postmenstrual age ‐ stabilized infants Show forest plot | 9 | 989 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.16, 0.49] |
| Analysis 1.11  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 11 Hypothermia at discharge or at 40 to 41 weeks’ postmenstrual age ‐ stabilized infants. | ||||
| 11.1 Intermittent | 9 | 989 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.16, 0.49] |
| 11.2 Continuous | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Hyperthermia at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 4 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.59, 1.05] |
| Analysis 1.12 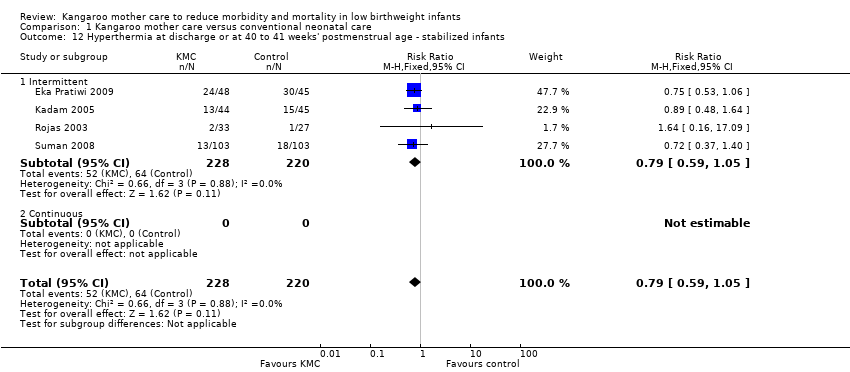 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 12 Hyperthermia at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants. | ||||
| 12.1 Intermittent | 4 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.59, 1.05] |
| 12.2 Continuous | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Length of hospital stay (days) ‐ stabilized infants Show forest plot | 11 | 1057 | Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐3.41, 0.18] |
| Analysis 1.13 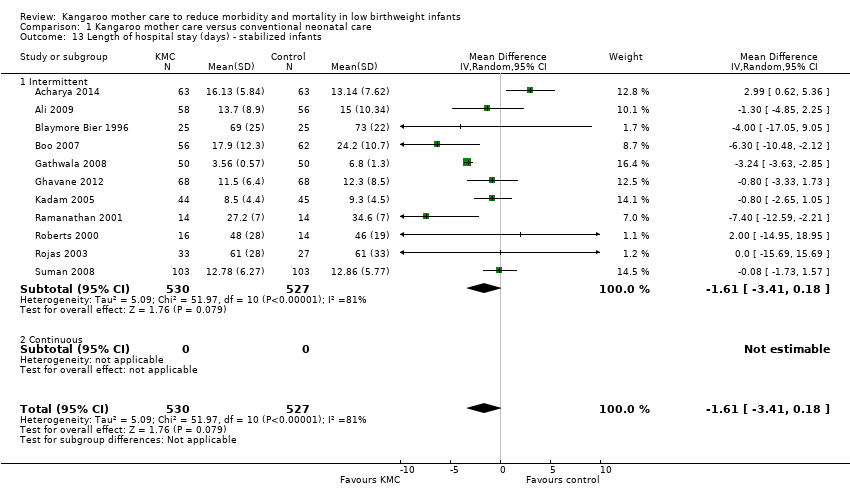 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 13 Length of hospital stay (days) ‐ stabilized infants. | ||||
| 13.1 Intermittent | 11 | 1057 | Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐3.41, 0.18] |
| 13.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Re‐admission to hospital at latest follow‐up ‐ stabilized infants Show forest plot | 2 | 946 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.34, 1.06] |
| Analysis 1.14 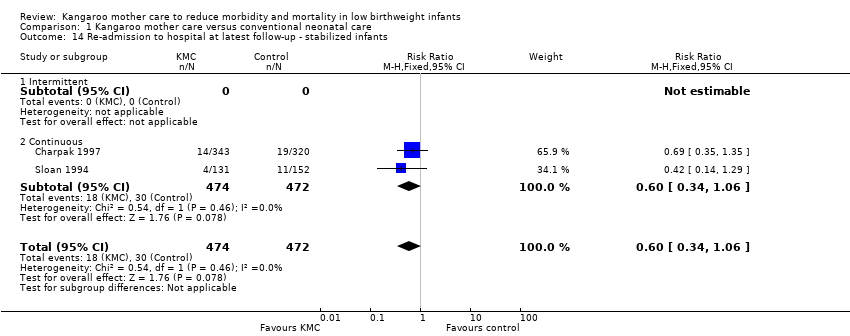 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 14 Re‐admission to hospital at latest follow‐up ‐ stabilized infants. | ||||
| 14.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Continuous | 2 | 946 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.34, 1.06] |
| 15 Weight at discharge or at 40 to 41 weeks' postmenstrual age (g) ‐ stabilized infants Show forest plot | 5 | 1233 | Mean Difference (IV, Fixed, 95% CI) | 16.07 [‐20.54, 52.68] |
| Analysis 1.15  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 15 Weight at discharge or at 40 to 41 weeks' postmenstrual age (g) ‐ stabilized infants. | ||||
| 15.1 Intermittent | 3 | 285 | Mean Difference (IV, Fixed, 95% CI) | 41.84 [‐19.19, 102.87] |
| 15.2 Continuous | 2 | 948 | Mean Difference (IV, Fixed, 95% CI) | 1.59 [‐44.16, 47.34] |
| 16 Weight at 6 months' corrected age (g) ‐ stabilized infants Show forest plot | 1 | 591 | Mean Difference (IV, Fixed, 95% CI) | 78.19 [‐52.26, 208.64] |
| Analysis 1.16  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 16 Weight at 6 months' corrected age (g) ‐ stabilized infants. | ||||
| 16.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Continuous | 1 | 591 | Mean Difference (IV, Fixed, 95% CI) | 78.19 [‐52.26, 208.64] |
| 17 Weight at 12 months' corrected age (g) ‐ stabilized infants Show forest plot | 1 | 596 | Mean Difference (IV, Fixed, 95% CI) | 31.46 [‐135.08, 198.00] |
| Analysis 1.17  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 17 Weight at 12 months' corrected age (g) ‐ stabilized infants. | ||||
| 17.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Continuous | 1 | 596 | Mean Difference (IV, Fixed, 95% CI) | 31.46 [‐135.08, 198.00] |
| 18 Weight gain at latest follow‐up (g/d) ‐ stabilized infants Show forest plot | 11 | 1198 | Mean Difference (IV, Random, 95% CI) | 4.08 [2.30, 5.86] |
| Analysis 1.18  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 18 Weight gain at latest follow‐up (g/d) ‐ stabilized infants. | ||||
| 18.1 Intermittent | 10 | 913 | Mean Difference (IV, Random, 95% CI) | 4.13 [2.19, 6.07] |
| 18.2 Continuous | 1 | 285 | Mean Difference (IV, Random, 95% CI) | 3.60 [0.78, 6.42] |
| 19 Length at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants Show forest plot | 3 | 856 | Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.69, 0.48] |
| Analysis 1.19 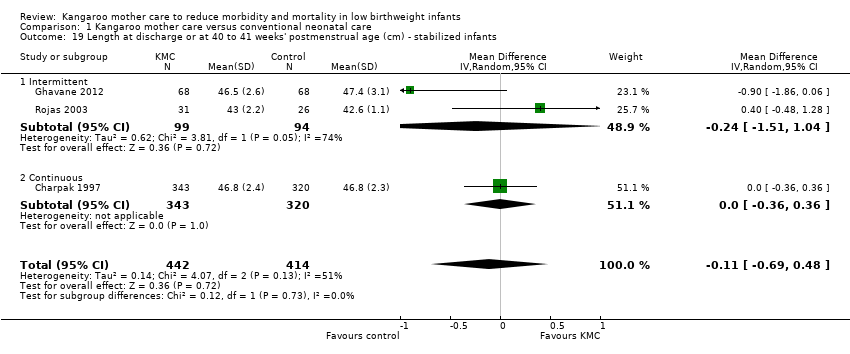 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 19 Length at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants. | ||||
| 19.1 Intermittent | 2 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.51, 1.04] |
| 19.2 Continuous | 1 | 663 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.36, 0.36] |
| 20 Length at 6 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 590 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [‐0.18, 0.64] |
| Analysis 1.20  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 20 Length at 6 months' corrected age (cm) ‐ stabilized infants. | ||||
| 20.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Continuous | 1 | 590 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [‐0.18, 0.64] |
| 21 Length at 12 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 586 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.17, 0.79] |
| Analysis 1.21  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 21 Length at 12 months' corrected age (cm) ‐ stabilized infants. | ||||
| 21.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Continuous | 1 | 586 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.17, 0.79] |
| 22 Length gain at latest follow‐up (cm/wk) ‐ stabilized infants Show forest plot | 3 | 377 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.03, 0.38] |
| Analysis 1.22 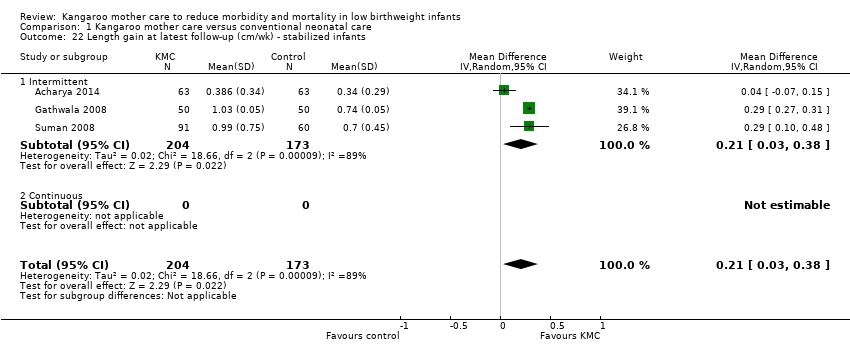 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 22 Length gain at latest follow‐up (cm/wk) ‐ stabilized infants. | ||||
| 22.1 Intermittent | 3 | 377 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.03, 0.38] |
| 22.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Head circumference at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants Show forest plot | 3 | 856 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.33, 0.66] |
| Analysis 1.23  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 23 Head circumference at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants. | ||||
| 23.1 Intermittent | 2 | 193 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.84, 1.31] |
| 23.2 Continuous | 1 | 663 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.14, 0.34] |
| 24 Head circumference at 6 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 592 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.11, 0.57] |
| Analysis 1.24  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 24 Head circumference at 6 months' corrected age (cm) ‐ stabilized infants. | ||||
| 24.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Continuous | 1 | 592 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.11, 0.57] |
| 25 Head circumference at 12 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 597 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.00, 0.78] |
| Analysis 1.25 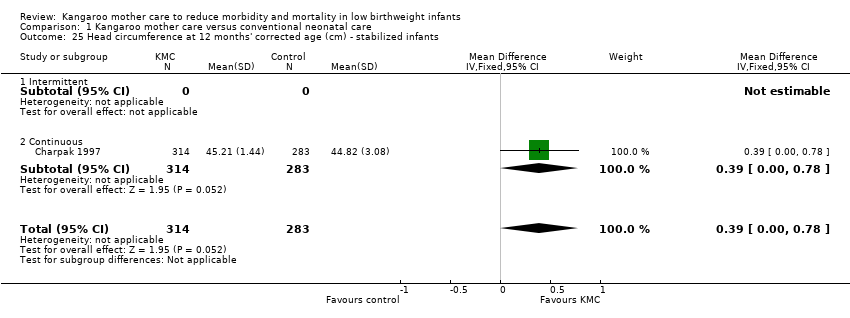 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 25 Head circumference at 12 months' corrected age (cm) ‐ stabilized infants. | ||||
| 25.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Continuous | 1 | 597 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.00, 0.78] |
| 26 Head circumference gain at latest follow‐up (cm/wk) ‐ stabilized infants Show forest plot | 4 | 495 | Mean Difference (IV, Random, 95% CI) | 0.14 [0.06, 0.22] |
| Analysis 1.26  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 26 Head circumference gain at latest follow‐up (cm/wk) ‐ stabilized infants. | ||||
| 26.1 Intermittent | 4 | 495 | Mean Difference (IV, Random, 95% CI) | 0.14 [0.06, 0.22] |
| 26.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Psychomotor development (Griffith quotients) at 12 months' corrected age Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.27  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 27 Psychomotor development (Griffith quotients) at 12 months' corrected age. | ||||
| 27.1 Locomotion | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 2.25 [‐0.45, 4.95] |
| 27.2 Personal, social | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 0.97 [‐1.27, 3.21] |
| 27.3 Hand‐eye coordination | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 0.57 [‐1.25, 2.39] |
| 27.4 Audition, language | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 1.29 [‐0.98, 3.56] |
| 27.5 Execution | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐1.50, 2.10] |
| 27.6 All criteria | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [‐0.75, 2.85] |
| 28 Cerebral palsy at 12 months' corrected age Show forest plot | 1 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.21, 2.02] |
| Analysis 1.28  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 28 Cerebral palsy at 12 months' corrected age. | ||||
| 29 Deafness at 12 months' corrected age Show forest plot | 1 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.03, 2.90] |
| Analysis 1.29 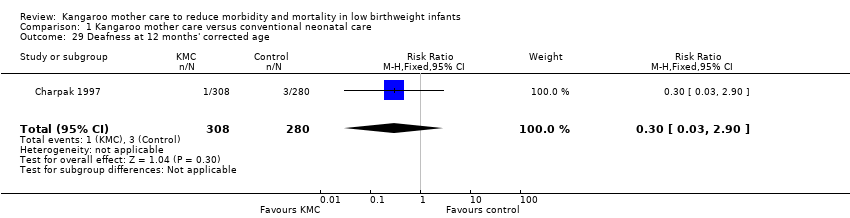 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 29 Deafness at 12 months' corrected age. | ||||
| 30 Visual impairment at 12 months' corrected age Show forest plot | 1 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.53, 1.56] |
| Analysis 1.30  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 30 Visual impairment at 12 months' corrected age. | ||||
| 31 Exclusive breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 6 | 1453 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.07, 1.25] |
| Analysis 1.31  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 31 Exclusive breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants. | ||||
| 31.1 Intermittent | 4 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [1.11, 1.35] |
| 31.2 Continuous | 2 | 942 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [1.00, 1.24] |
| 32 Exclusive breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants Show forest plot | 5 | 600 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.01, 1.43] |
| Analysis 1.32  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 32 Exclusive breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants. | ||||
| 32.1 Intermittent | 3 | 221 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [1.12, 1.65] |
| 32.2 Continuous | 2 | 379 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.96, 1.10] |
| 33 Exclusive breastfeeding at 6 to 12 months' follow‐up ‐ stabilized infants Show forest plot | 3 | 810 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.95, 1.76] |
| Analysis 1.33 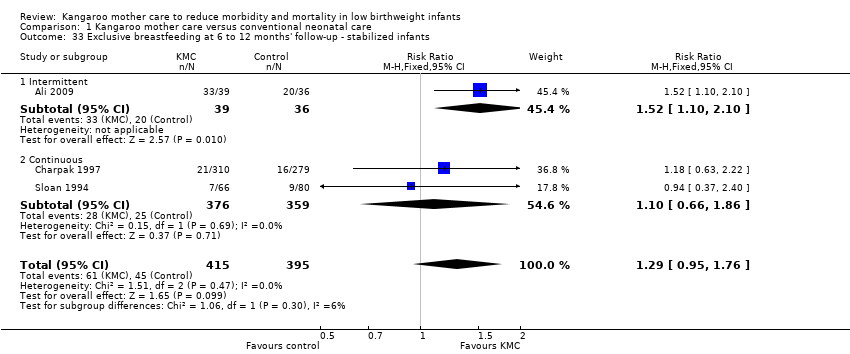 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 33 Exclusive breastfeeding at 6 to 12 months' follow‐up ‐ stabilized infants. | ||||
| 33.1 Intermittent | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.10, 2.10] |
| 33.2 Continuous | 2 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.66, 1.86] |
| 34 Any breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 10 | 1696 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| Analysis 1.34  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 34 Any breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants. | ||||
| 34.1 Intermittent | 8 | 754 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.07, 1.41] |
| 34.2 Continuous | 2 | 942 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.93, 1.40] |
| 35 Any breastfeeding at 1 to 2 months' follow‐up ‐ stabilized infants Show forest plot | 6 | 538 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [1.00, 1.78] |
| Analysis 1.35  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 35 Any breastfeeding at 1 to 2 months' follow‐up ‐ stabilized infants. | ||||
| 35.1 Intermittent | 4 | 159 | Risk Ratio (M‐H, Random, 95% CI) | 1.89 [1.30, 2.75] |
| 35.2 Continuous | 2 | 379 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.96, 1.10] |
| 36 Any breastfeeding at 3 months' follow‐up ‐ stabilized infants Show forest plot | 5 | 924 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [1.06, 1.23] |
| Analysis 1.36  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 36 Any breastfeeding at 3 months' follow‐up ‐ stabilized infants. | ||||
| 36.1 Intermittent | 4 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.15, 1.59] |
| 36.2 Continuous | 1 | 663 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [1.00, 1.17] |
| 37 Any breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants Show forest plot | 9 | 1394 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.05, 1.31] |
| Analysis 1.37 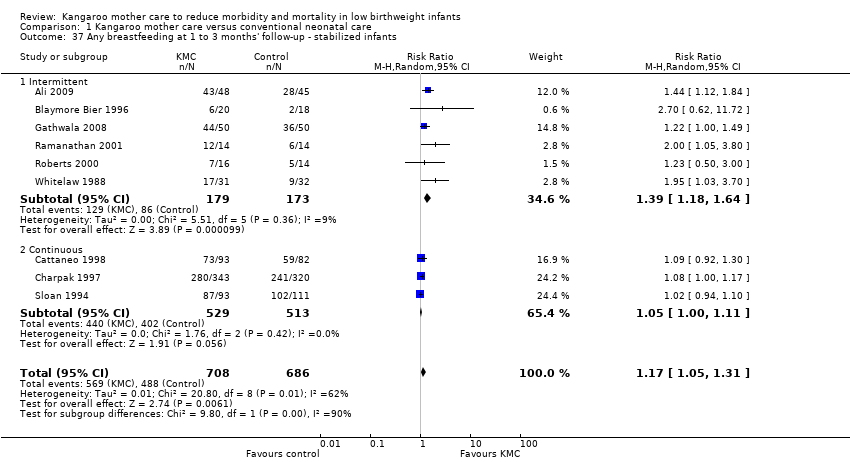 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 37 Any breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants. | ||||
| 37.1 Intermittent | 6 | 352 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [1.18, 1.64] |
| 37.2 Continuous | 3 | 1042 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.00, 1.11] |
| 38 Any breastfeeding at 6 months' follow‐up ‐ stabilized infants Show forest plot | 5 | 952 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.98, 1.29] |
| Analysis 1.38 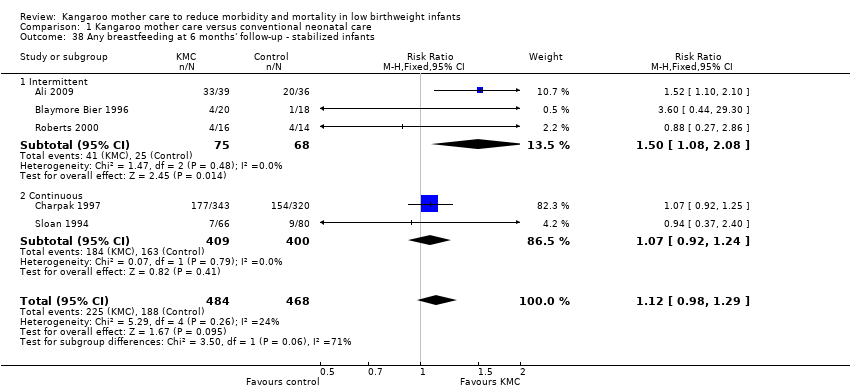 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 38 Any breastfeeding at 6 months' follow‐up ‐ stabilized infants. | ||||
| 38.1 Intermittent | 3 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [1.08, 2.08] |
| 38.2 Continuous | 2 | 809 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.92, 1.24] |
| 39 Any breastfeeding at 12 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 589 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.21] |
| Analysis 1.39  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 39 Any breastfeeding at 12 months' follow‐up ‐ stabilized infants. | ||||
| 39.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Continuous | 1 | 589 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.21] |
| 40 Onset of breastfeeding (days) ‐ stabilized infants Show forest plot | 2 | 295 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.64, 1.70] |
| Analysis 1.40 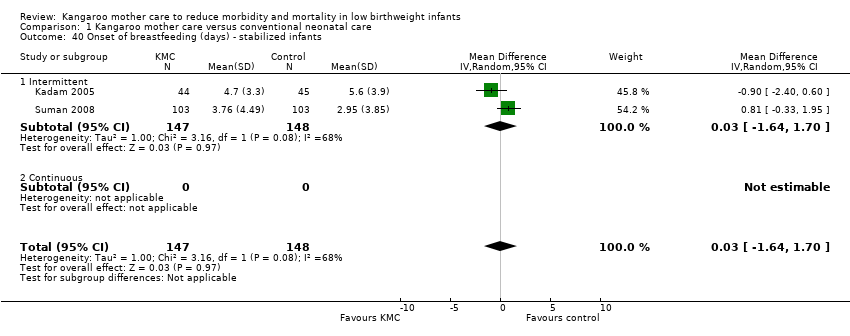 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 40 Onset of breastfeeding (days) ‐ stabilized infants. | ||||
| 40.1 Intermittent | 2 | 295 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.64, 1.70] |
| 40.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Parental and familial satisfaction (continuous KMC) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.41 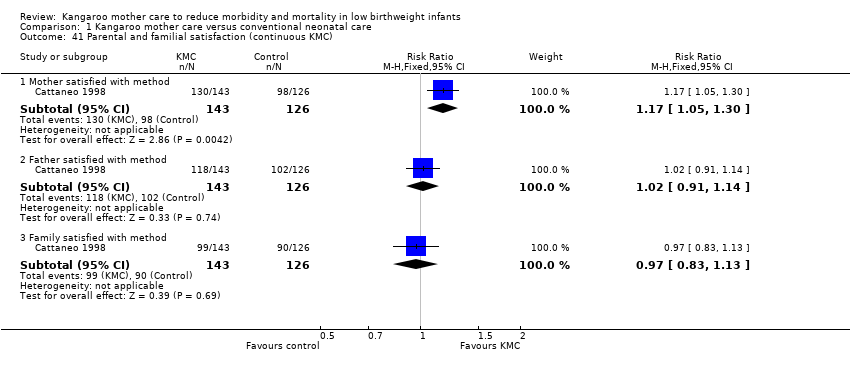 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 41 Parental and familial satisfaction (continuous KMC). | ||||
| 41.1 Mother satisfied with method | 1 | 269 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [1.05, 1.30] |
| 41.2 Father satisfied with method | 1 | 269 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.14] |
| 41.3 Family satisfied with method | 1 | 269 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.83, 1.13] |
| 42 Mother‐infant attachment: mother's feelings and perceptions according to interval between birth and start of intervention, and infant admission to NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.42  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 42 Mother‐infant attachment: mother's feelings and perceptions according to interval between birth and start of intervention, and infant admission to NICU. | ||||
| 42.1 Sense of competence ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [0.14, 0.68] |
| 42.2 Sense of competence ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.08, 0.58] |
| 42.3 Sense of competence ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.17, 0.59] |
| 42.4 Sense of competence ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.07, 1.01] |
| 42.5 Sense of competence ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.05, 0.43] |
| 42.6 Worry and stress ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [0.04, 0.58] |
| 42.7 Worry and stress ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.20, 0.38] |
| 42.8 Worry and stress ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.70, 0.12] |
| 42.9 Worry and stress ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.1 [‐0.60, 0.40] |
| 42.10 Worry and stress ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.06, 0.30] |
| 42.11 Social support ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.35, 0.23] |
| 42.12 Social support ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.34, 0.22] |
| 42.13 Social support ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐0.84, ‐0.10] |
| 42.14 Social support ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.52, 0.42] |
| 42.15 Social support ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | ‐0.2 [‐0.39, ‐0.01] |
| 43 Mother‐infant attachment: mother's responses to the infant according to interval between birth and start of intervention, and infant admission to NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.43 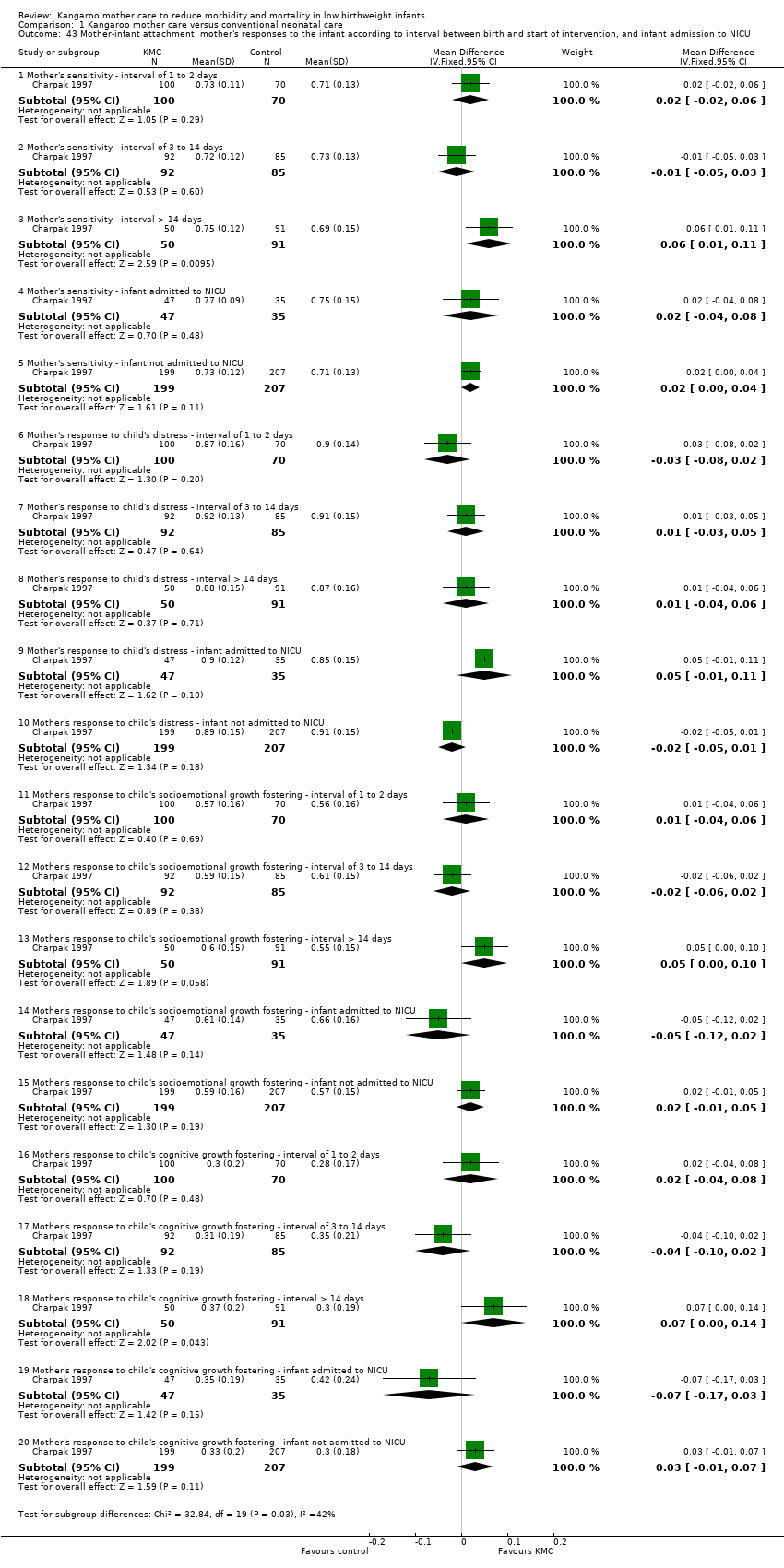 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 43 Mother‐infant attachment: mother's responses to the infant according to interval between birth and start of intervention, and infant admission to NICU. | ||||
| 43.1 Mother's sensitivity ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.02, 0.06] |
| 43.2 Mother's sensitivity ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.05, 0.03] |
| 43.3 Mother's sensitivity ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [0.01, 0.11] |
| 43.4 Mother's sensitivity ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.04, 0.08] |
| 43.5 Mother's sensitivity ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.00, 0.04] |
| 43.6 Mother's response to child's distress ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.08, 0.02] |
| 43.7 Mother's response to child's distress ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.03, 0.05] |
| 43.8 Mother's response to child's distress ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.04, 0.06] |
| 43.9 Mother's response to child's distress ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.01, 0.11] |
| 43.10 Mother's response to child's distress ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.01] |
| 43.11 Mother's response to child's socioemotional growth fostering ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.04, 0.06] |
| 43.12 Mother's response to child's socioemotional growth fostering ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.02] |
| 43.13 Mother's response to child's socioemotional growth fostering ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.00, 0.10] |
| 43.14 Mother's response to child's socioemotional growth fostering ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.12, 0.02] |
| 43.15 Mother's response to child's socioemotional growth fostering ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 43.16 Mother's response to child's cognitive growth fostering ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.04, 0.08] |
| 43.17 Mother's response to child's cognitive growth fostering ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.10, 0.02] |
| 43.18 Mother's response to child's cognitive growth fostering ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [0.00, 0.14] |
| 43.19 Mother's response to child's cognitive growth fostering ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.17, 0.03] |
| 43.20 Mother's response to child's cognitive growth fostering ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.01, 0.07] |
| 44 Mother‐infant attachment: infant's responses to the mother according to interval between birth and start of intervention, and infant admission to NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.44 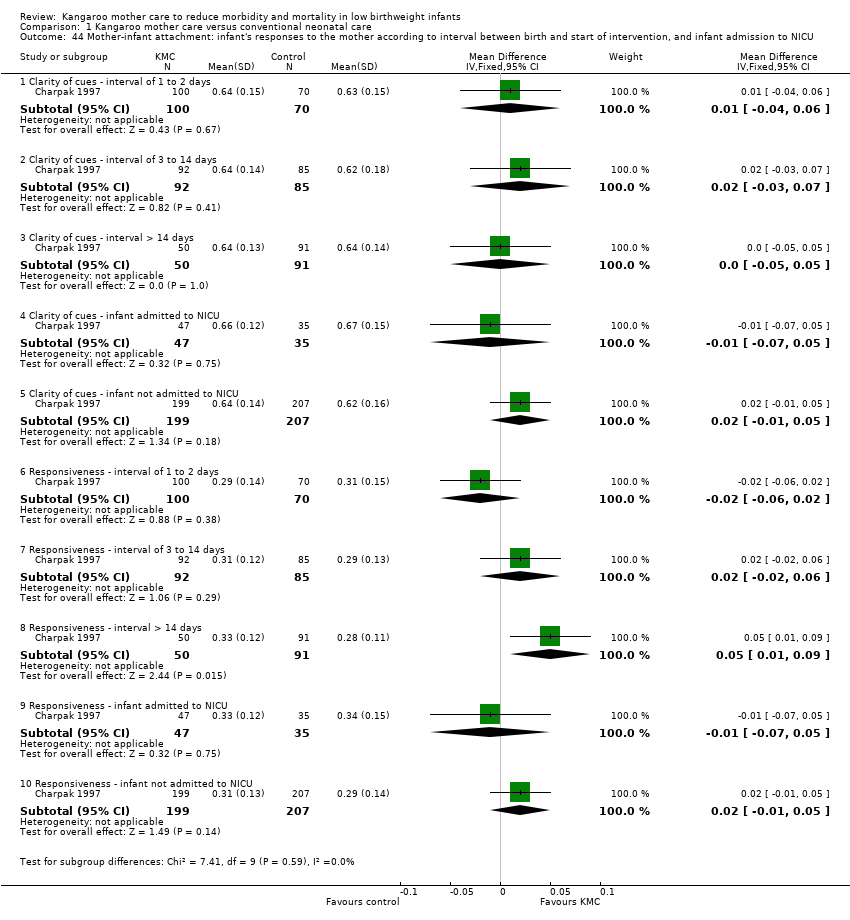 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 44 Mother‐infant attachment: infant's responses to the mother according to interval between birth and start of intervention, and infant admission to NICU. | ||||
| 44.1 Clarity of cues ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.04, 0.06] |
| 44.2 Clarity of cues ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.03, 0.07] |
| 44.3 Clarity of cues ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 44.4 Clarity of cues ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.07, 0.05] |
| 44.5 Clarity of cues ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 44.6 Responsiveness ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.02] |
| 44.7 Responsiveness ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.02, 0.06] |
| 44.8 Responsiveness ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [0.01, 0.09] |
| 44.9 Responsiveness ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.07, 0.05] |
| 44.10 Responsiveness ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 45 Mother‐infant attachment at 3 months' follow‐up Show forest plot | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 6.24 [5.57, 6.91] |
| Analysis 1.45 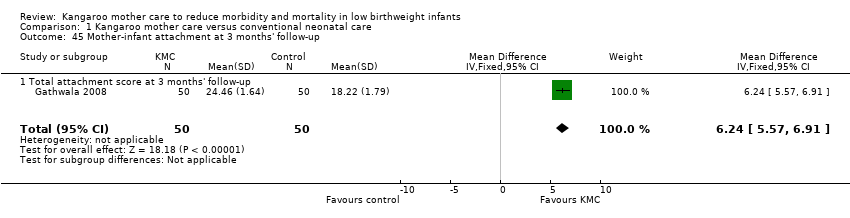 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 45 Mother‐infant attachment at 3 months' follow‐up. | ||||
| 45.1 Total attachment score at 3 months' follow‐up | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 6.24 [5.57, 6.91] |
| 46 Mother‐infant attachment: stress in NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.46 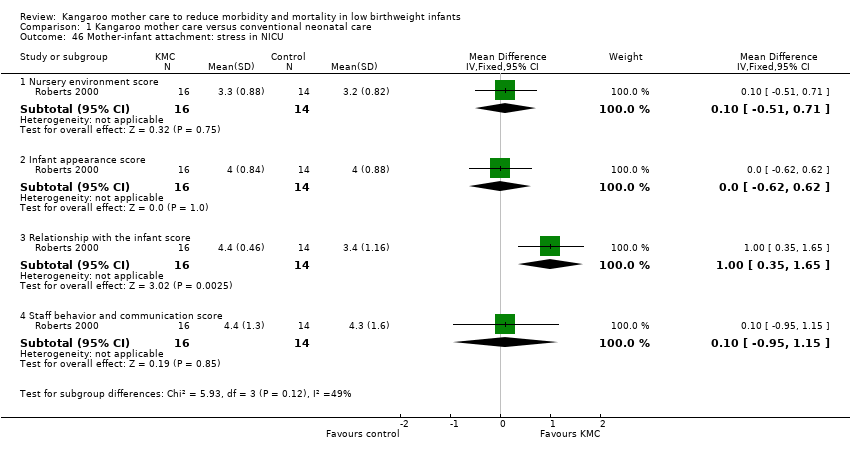 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 46 Mother‐infant attachment: stress in NICU. | ||||
| 46.1 Nursery environment score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.51, 0.71] |
| 46.2 Infant appearance score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.62, 0.62] |
| 46.3 Relationship with the infant score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [0.35, 1.65] |
| 46.4 Staff behavior and communication score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.95, 1.15] |
| 47 Mother‐infant attachment: parenting skills Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.89, 0.09] |
| Analysis 1.47 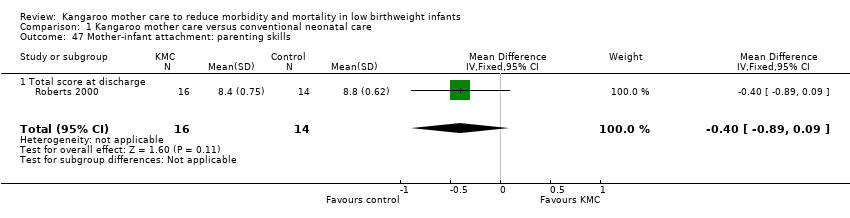 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 47 Mother‐infant attachment: parenting skills. | ||||
| 47.1 Total score at discharge | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.89, 0.09] |
| 48 Mother‐infant interaction at 6 months' follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.48  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 48 Mother‐infant interaction at 6 months' follow‐up. | ||||
| 48.1 Symmetrical co‐regulation | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 16.38 [13.61, 19.15] |
| 48.2 Asymmetrical co‐regulation | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐18.31 [‐21.42, ‐15.20] |
| 48.3 Unilateral regulation | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 2.12 [‐1.24, 5.48] |
| 49 Infant behavior at 40 to 44 weeks’ postmenstrual age Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.49 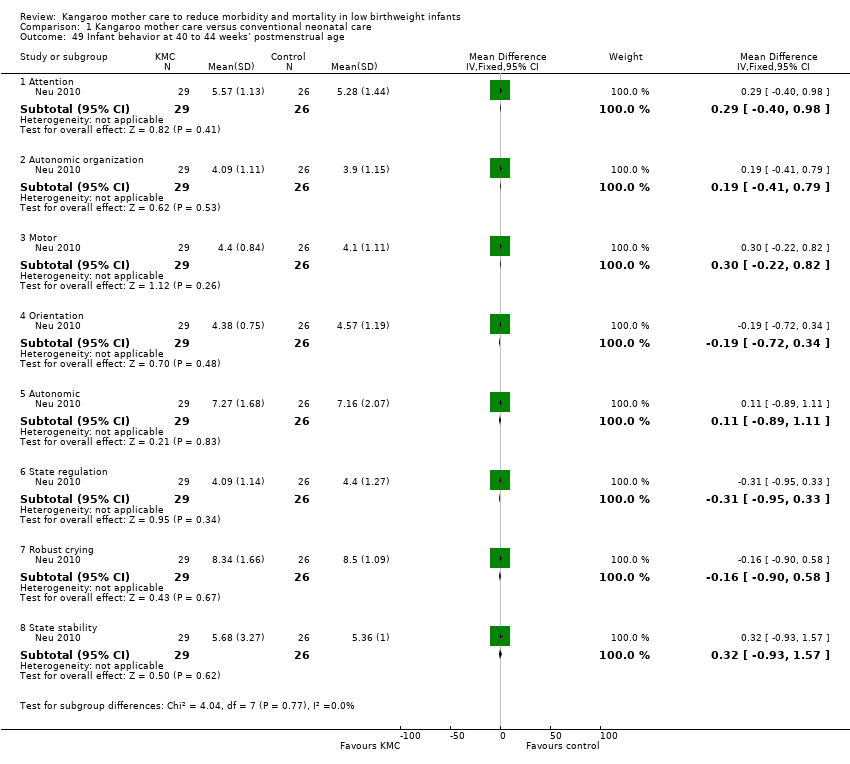 Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 49 Infant behavior at 40 to 44 weeks’ postmenstrual age. | ||||
| 49.1 Attention | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.29 [‐0.40, 0.98] |
| 49.2 Autonomic organization | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.41, 0.79] |
| 49.3 Motor | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.22, 0.82] |
| 49.4 Orientation | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.72, 0.34] |
| 49.5 Autonomic | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.89, 1.11] |
| 49.6 State regulation | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.95, 0.33] |
| 49.7 Robust crying | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.90, 0.58] |
| 49.8 State stability | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.93, 1.57] |
| 50 Social and home environment Show forest plot | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [0.74, 0.84] |
| Analysis 1.50  Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 50 Social and home environment. | ||||
| 50.1 HOME environment total score at 12 months' corrected age | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [0.74, 0.84] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.18, 20.53] |
| Analysis 2.1 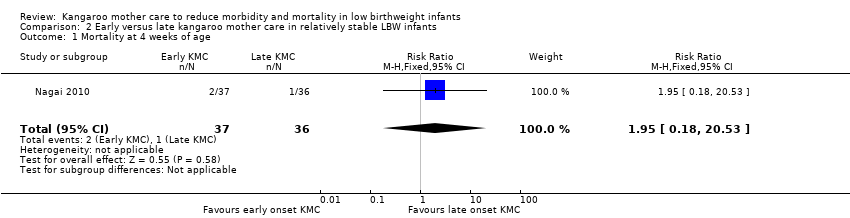 Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 1 Mortality at 4 weeks of age. | ||||
| 2 Morbidity at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.28] |
| Analysis 2.2  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 2 Morbidity at 4 weeks of age. | ||||
| 3 Severe infection at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.12, 1.49] |
| Analysis 2.3 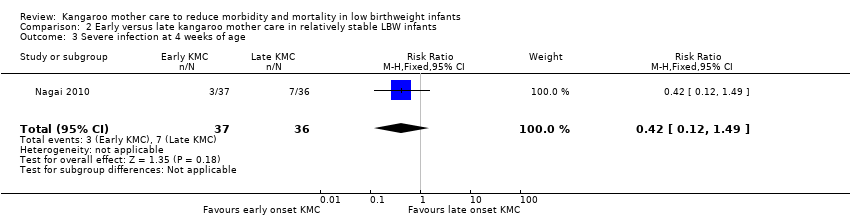 Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 3 Severe infection at 4 weeks of age. | ||||
| 4 Re‐admission to hospital at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.18, 20.53] |
| Analysis 2.4  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 4 Re‐admission to hospital at 4 weeks of age. | ||||
| 5 Hypothermia Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.15, 2.27] |
| Analysis 2.5  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 5 Hypothermia. | ||||
| 6 Hyperthermia Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.56, 1.99] |
| Analysis 2.6  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 6 Hyperthermia. | ||||
| 7 Weight gain (grams) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 7 Weight gain (grams). | ||||
| 7.1 At 24 hours post birth | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 39.16 [11.11, 67.21] |
| 7.2 At 48 hours post birth | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 43.3 [5.49, 81.11] |
| 7.3 At 2 weeks of age | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 12.14 [‐83.18, 107.46] |
| 7.4 At 4 weeks of age | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 58.85 [‐116.93, 234.63] |
| 8 Exclusive breastfeeding Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.8  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 8 Exclusive breastfeeding. | ||||
| 8.1 At 24 hours of age | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.67, 1.57] |
| 8.2 At 2 weeks of age | 1 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.89, 1.12] |
| 8.3 At 4 weeks of age | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.85, 1.04] |
| 8.4 At 6 months of age | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.69 [0.99, 7.31] |
| 9 Length of hospital stay (days) Show forest plot | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.24, ‐0.56] |
| Analysis 2.9  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 9 Length of hospital stay (days). | ||||
| 10 Mortality at 6 months of age Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.72] |
| Analysis 2.10  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 10 Mortality at 6 months of age. | ||||
| 11 Re‐admission to hospital at 6 to 12 months of age Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.32, 3.16] |
| Analysis 2.11 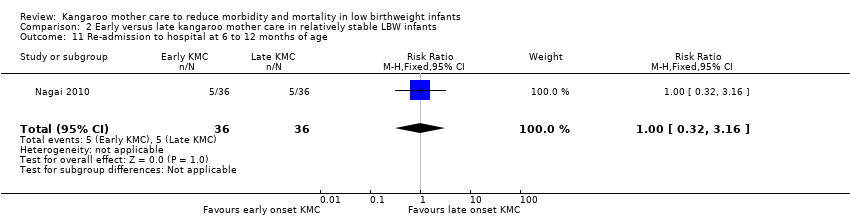 Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 11 Re‐admission to hospital at 6 to 12 months of age. | ||||
| 12 Stunting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.46, 1.48] |
| Analysis 2.12  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 12 Stunting at 6 to 12 months of age. | ||||
| 13 Severe stunting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.17, 2.73] |
| Analysis 2.13  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 13 Severe stunting at 6 to 12 months of age. | ||||
| 14 Wasting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.1 [0.01, 1.77] |
| Analysis 2.14 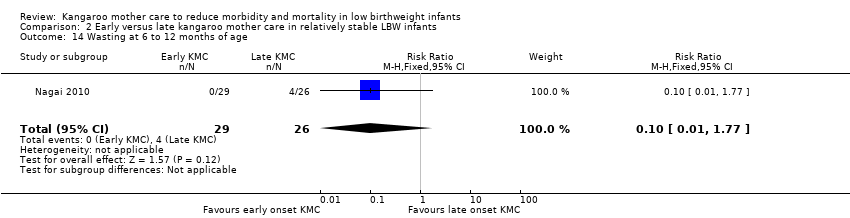 Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 14 Wasting at 6 to 12 months of age. | ||||
| 15 Severe wasting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 2.15 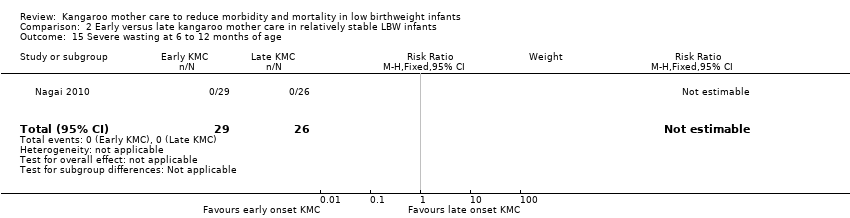 Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 15 Severe wasting at 6 to 12 months of age. | ||||
| 16 Underweight at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.21, 1.14] |
| Analysis 2.16  Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 16 Underweight at 6 to 12 months of age. | ||||
| 17 Severe underweight at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.03, 1.88] |
| Analysis 2.17 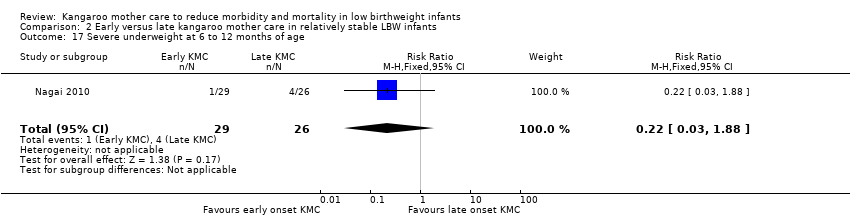 Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 17 Severe underweight at 6 to 12 months of age. | ||||

Study flow diagram: review update

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Kangaroo mother care versus conventional neonatal care, outcome: 1.1 Mortality at latest follow‐up.
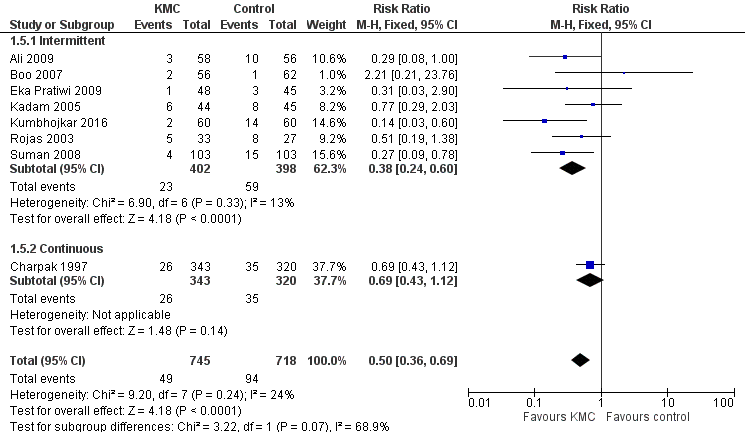
Forest plot of comparison: 1 Kangaroo mother care versus conventional neonatal care, outcome: 1.2 Severe infection/sepsis at latest follow‐up ‐ stabilized infants.

Forest plot of comparison: 1 Kangaroo mother care versus conventional neonatal care, outcome: 1.10 Weight gain at latest follow‐up (g/d) ‐ stabilized infants.

Forest plot of comparison: 1 Kangaroo mother care versus conventional neonatal care, outcome: 1.34 Any breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 1 Mortality at discharge or at 40 to 41 weeks' postmenstrual age.
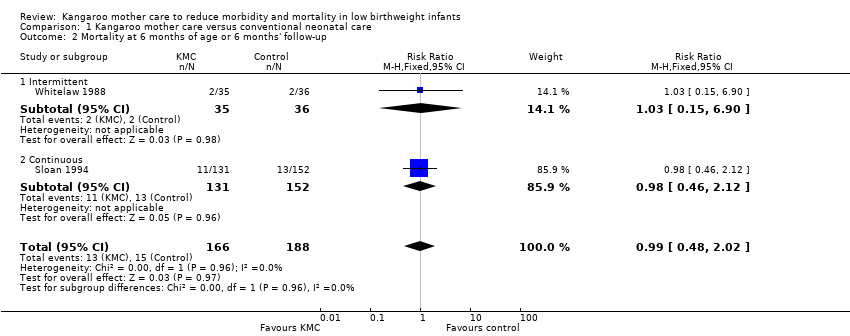
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 2 Mortality at 6 months of age or 6 months' follow‐up.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 3 Mortality at 12 months' corrected age.
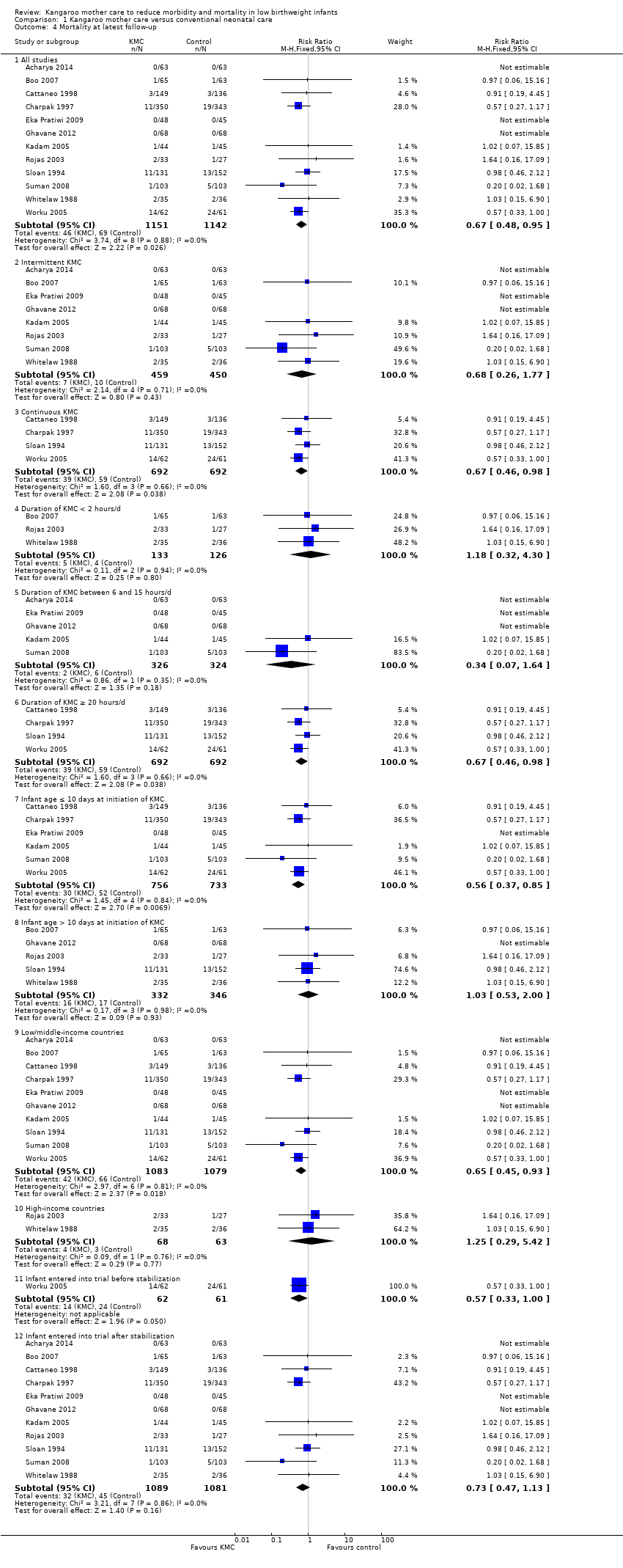
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 4 Mortality at latest follow‐up.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 5 Severe infection/sepsis at latest follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 6 Severe illness at 6 months' follow‐up ‐ stabilized infants.
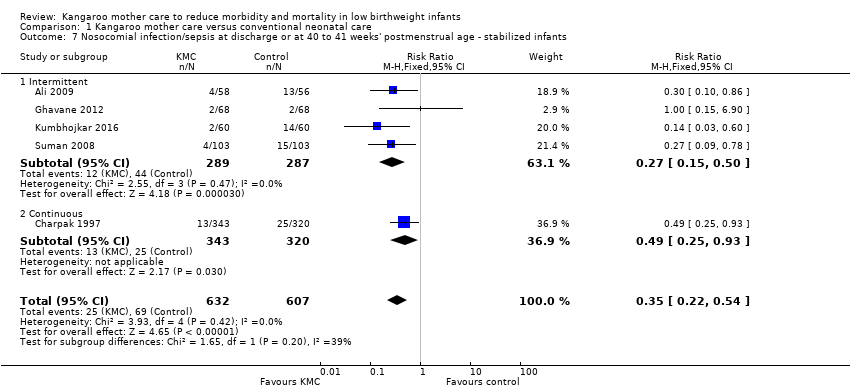
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 7 Nosocomial infection/sepsis at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants.
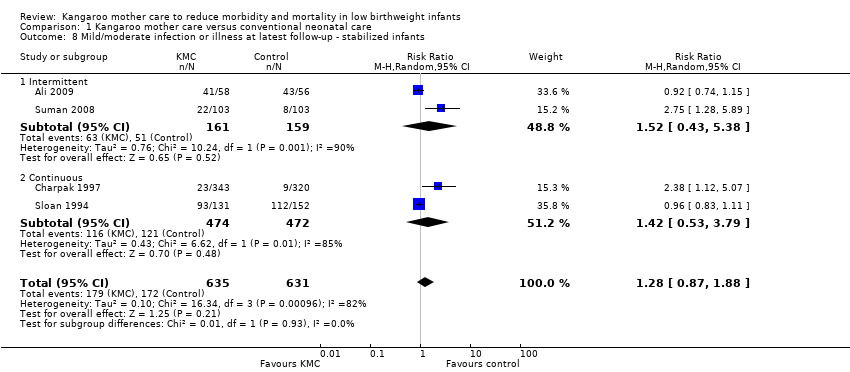
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 8 Mild/moderate infection or illness at latest follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 9 Lower respiratory tract disease at 6 months' follow‐up ‐ stabilized infants.
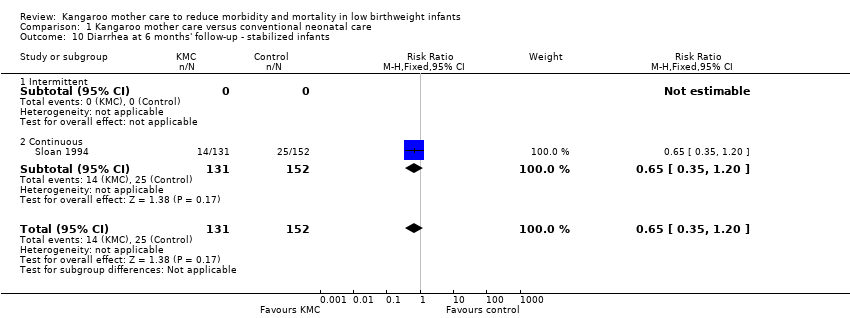
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 10 Diarrhea at 6 months' follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 11 Hypothermia at discharge or at 40 to 41 weeks’ postmenstrual age ‐ stabilized infants.
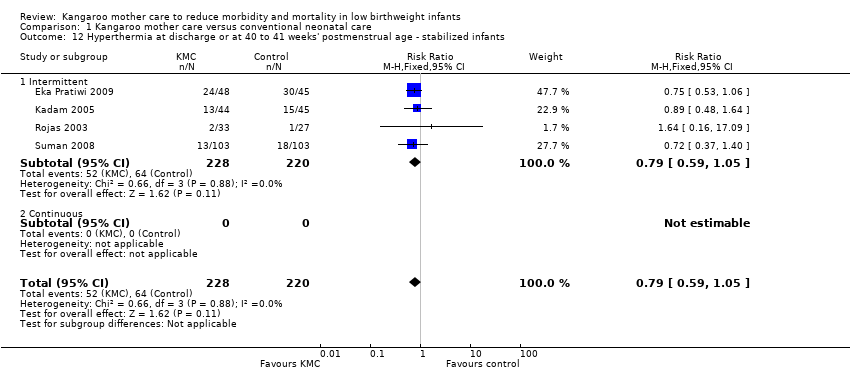
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 12 Hyperthermia at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 13 Length of hospital stay (days) ‐ stabilized infants.
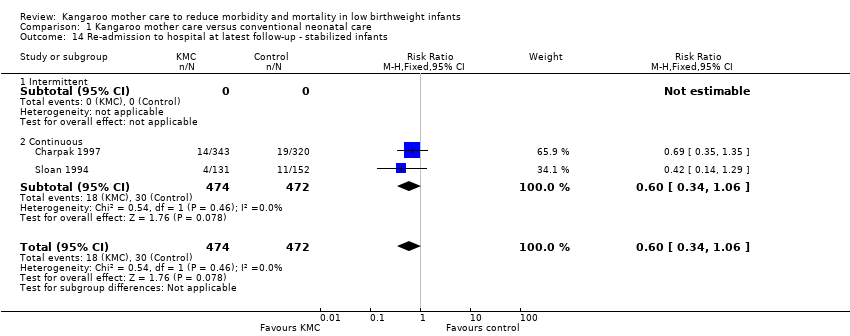
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 14 Re‐admission to hospital at latest follow‐up ‐ stabilized infants.
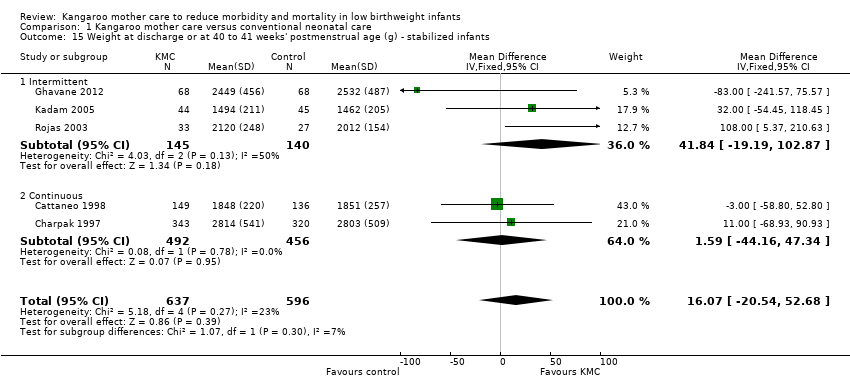
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 15 Weight at discharge or at 40 to 41 weeks' postmenstrual age (g) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 16 Weight at 6 months' corrected age (g) ‐ stabilized infants.
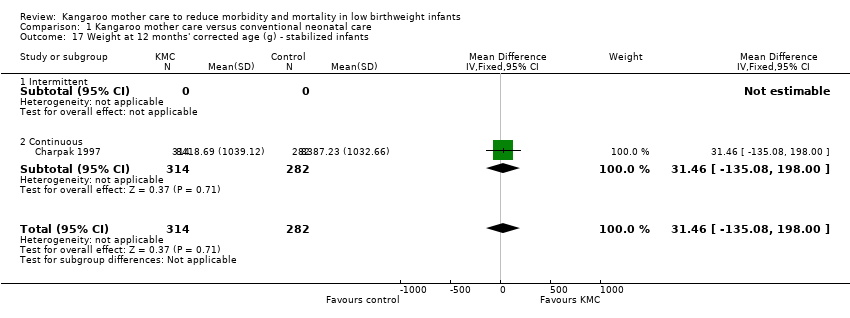
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 17 Weight at 12 months' corrected age (g) ‐ stabilized infants.
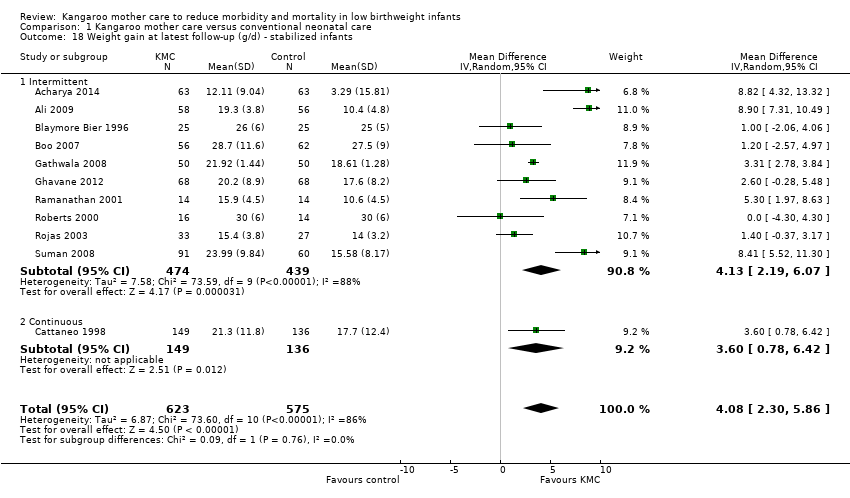
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 18 Weight gain at latest follow‐up (g/d) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 19 Length at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 20 Length at 6 months' corrected age (cm) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 21 Length at 12 months' corrected age (cm) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 22 Length gain at latest follow‐up (cm/wk) ‐ stabilized infants.
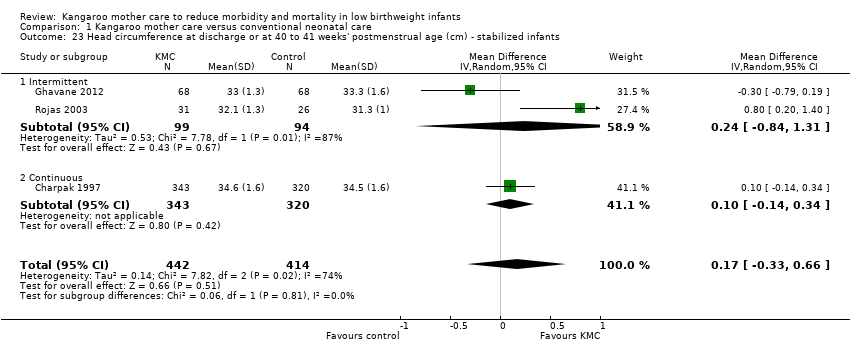
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 23 Head circumference at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 24 Head circumference at 6 months' corrected age (cm) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 25 Head circumference at 12 months' corrected age (cm) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 26 Head circumference gain at latest follow‐up (cm/wk) ‐ stabilized infants.
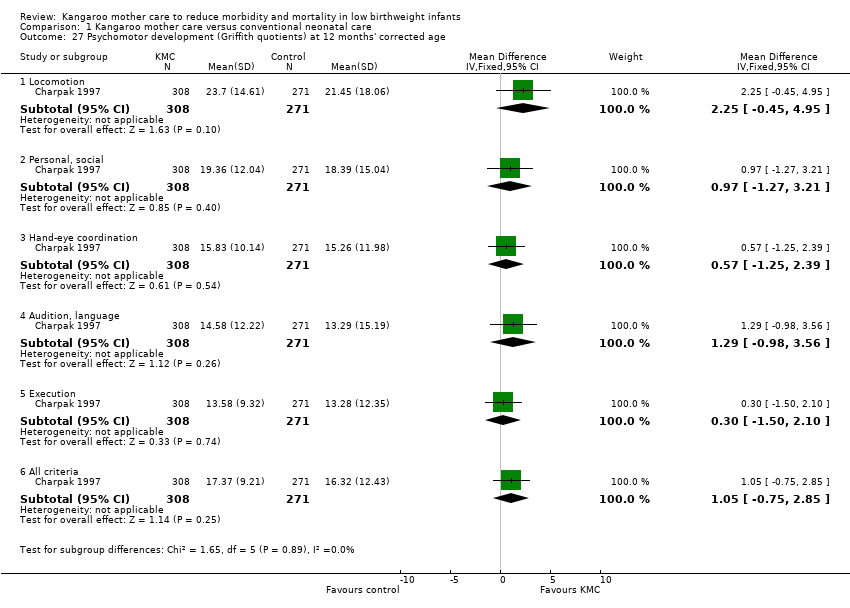
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 27 Psychomotor development (Griffith quotients) at 12 months' corrected age.
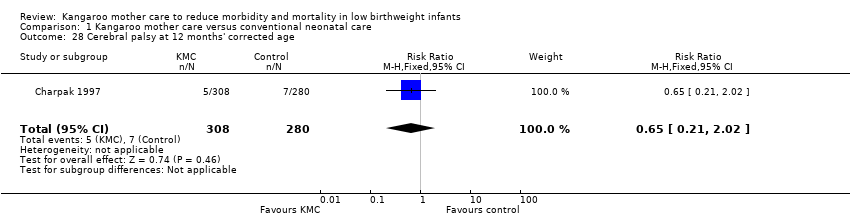
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 28 Cerebral palsy at 12 months' corrected age.
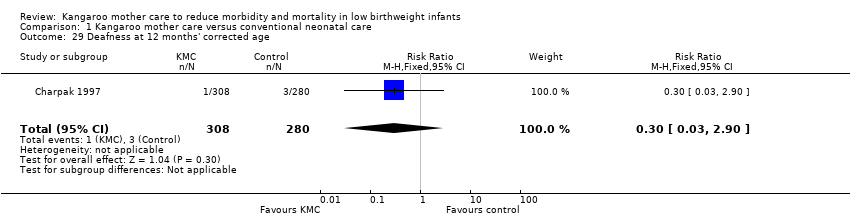
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 29 Deafness at 12 months' corrected age.
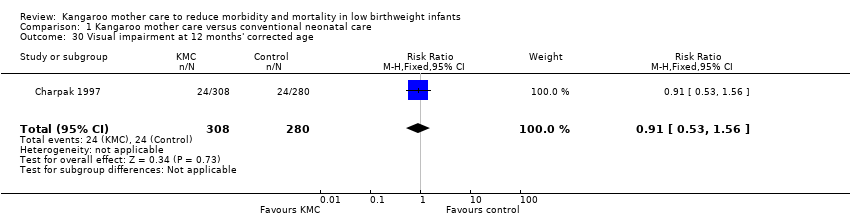
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 30 Visual impairment at 12 months' corrected age.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 31 Exclusive breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 32 Exclusive breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 33 Exclusive breastfeeding at 6 to 12 months' follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 34 Any breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 35 Any breastfeeding at 1 to 2 months' follow‐up ‐ stabilized infants.
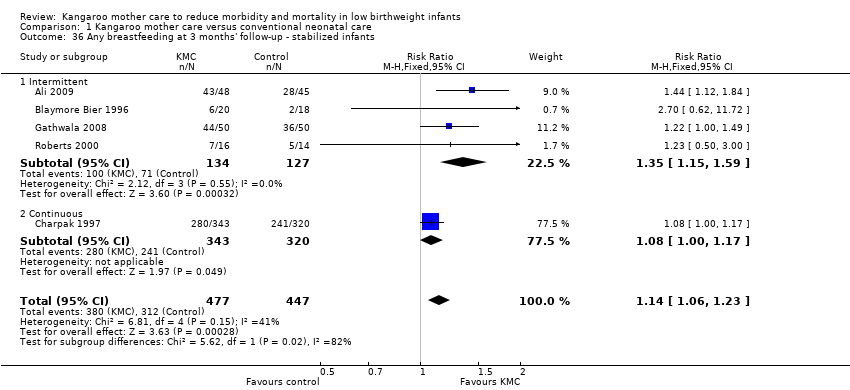
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 36 Any breastfeeding at 3 months' follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 37 Any breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 38 Any breastfeeding at 6 months' follow‐up ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 39 Any breastfeeding at 12 months' follow‐up ‐ stabilized infants.
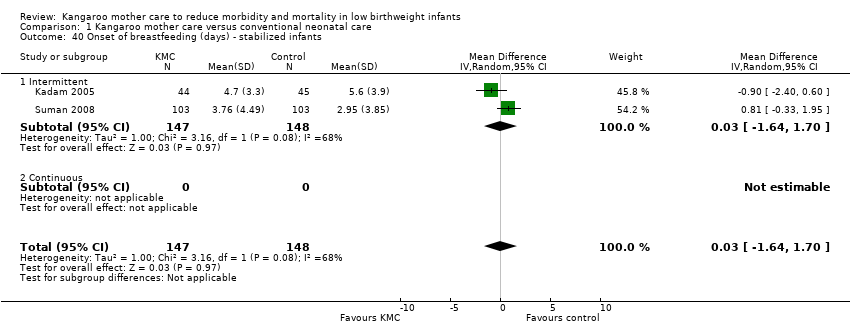
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 40 Onset of breastfeeding (days) ‐ stabilized infants.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 41 Parental and familial satisfaction (continuous KMC).

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 42 Mother‐infant attachment: mother's feelings and perceptions according to interval between birth and start of intervention, and infant admission to NICU.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 43 Mother‐infant attachment: mother's responses to the infant according to interval between birth and start of intervention, and infant admission to NICU.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 44 Mother‐infant attachment: infant's responses to the mother according to interval between birth and start of intervention, and infant admission to NICU.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 45 Mother‐infant attachment at 3 months' follow‐up.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 46 Mother‐infant attachment: stress in NICU.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 47 Mother‐infant attachment: parenting skills.
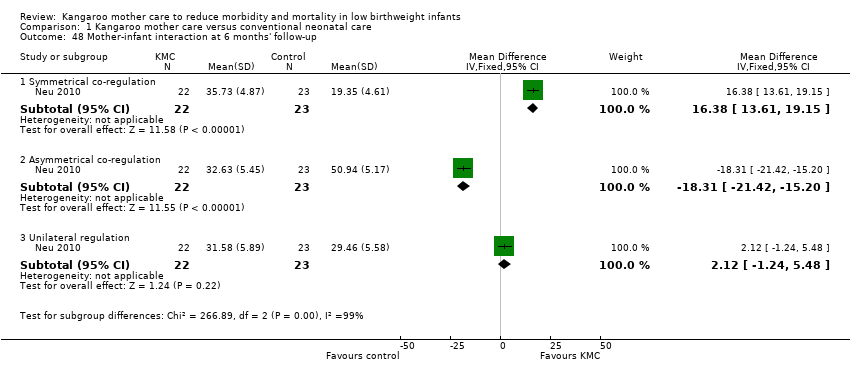
Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 48 Mother‐infant interaction at 6 months' follow‐up.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 49 Infant behavior at 40 to 44 weeks’ postmenstrual age.

Comparison 1 Kangaroo mother care versus conventional neonatal care, Outcome 50 Social and home environment.
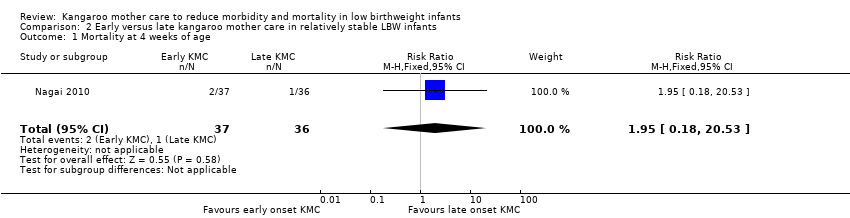
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 1 Mortality at 4 weeks of age.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 2 Morbidity at 4 weeks of age.
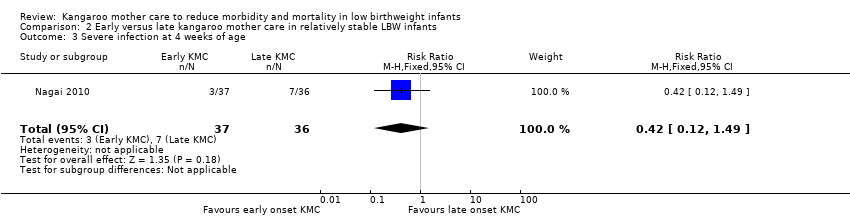
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 3 Severe infection at 4 weeks of age.
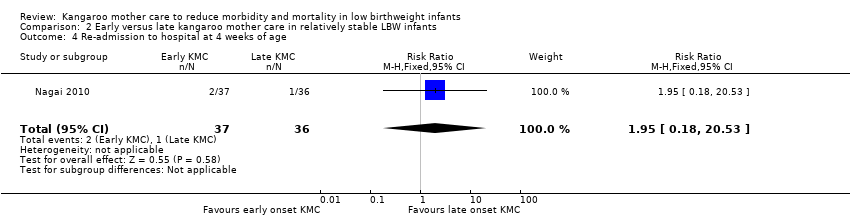
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 4 Re‐admission to hospital at 4 weeks of age.
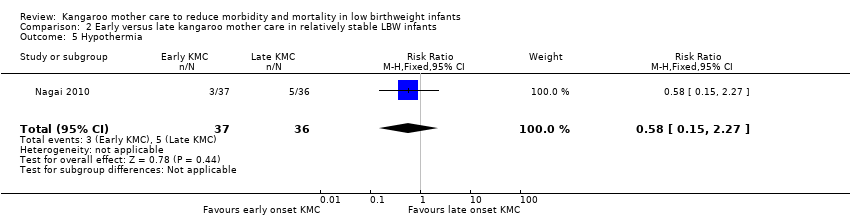
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 5 Hypothermia.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 6 Hyperthermia.
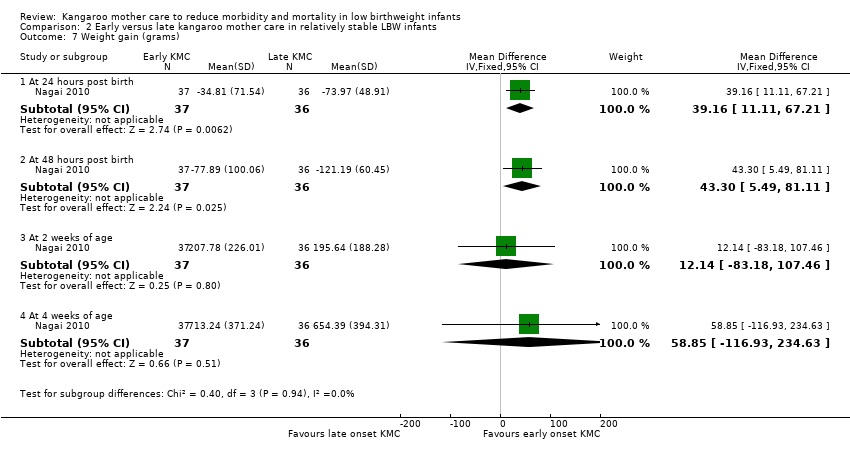
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 7 Weight gain (grams).

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 8 Exclusive breastfeeding.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 9 Length of hospital stay (days).
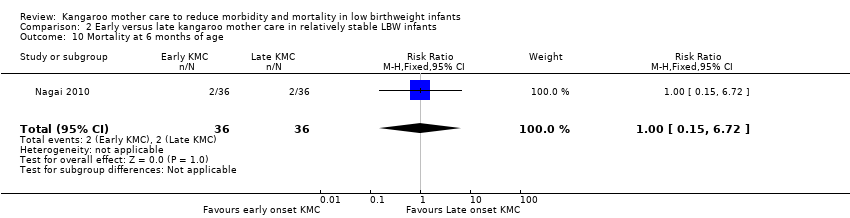
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 10 Mortality at 6 months of age.
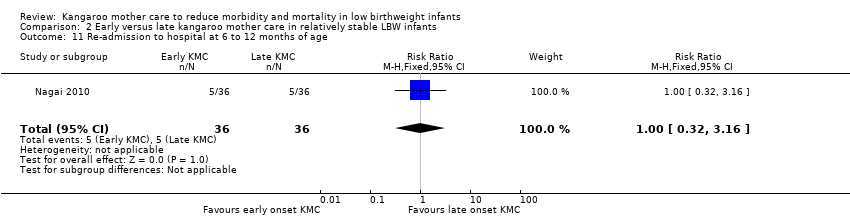
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 11 Re‐admission to hospital at 6 to 12 months of age.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 12 Stunting at 6 to 12 months of age.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 13 Severe stunting at 6 to 12 months of age.
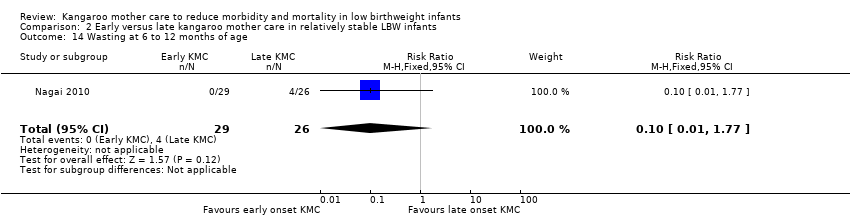
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 14 Wasting at 6 to 12 months of age.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 15 Severe wasting at 6 to 12 months of age.

Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 16 Underweight at 6 to 12 months of age.
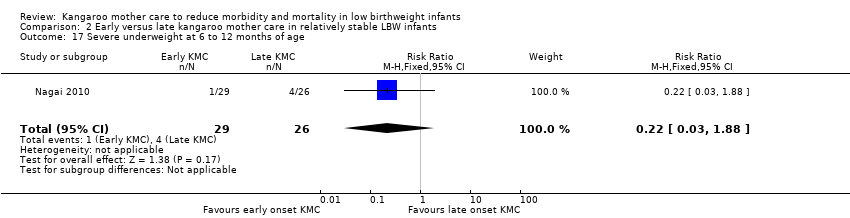
Comparison 2 Early versus late kangaroo mother care in relatively stable LBW infants, Outcome 17 Severe underweight at 6 to 12 months of age.
| Kangaroo mother care versus conventional neonatal care for reducing morbidity and mortality in low birthweight infants | ||||||
| Patient or population: infants with low birthweight | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional neonatal care | Kangaroo mother care | |||||
| Mortality at latest follow‐up | Study population | RR 0.67 | 2293 | ⊕⊕⊕⊝ | ||
| 60 per 1000 | 40 per 1000 | |||||
| Moderate | ||||||
| 30 per 1000 | 20 per 1000 | |||||
| Severe infection/sepsis at latest follow‐up ‐ stabilized infants | Study population | RR 0.5 | 1463 | ⊕⊕⊕⊝ | ||
| 131 per 1000 | 65 per 1000 | |||||
| Moderate | ||||||
| 162 per 1000 | 81 per 1000 | |||||
| Hypothermia at discharge or at 40 to 41 weeks’ postmenstrual age ‐ stabilized infants | Study population | RR 0.28 | 989 | ⊕⊕⊕⊝ | ||
| 271 per 1000 | 76 per 1000 | |||||
| Moderate | ||||||
| 333 per 1000 | 93 per 1000 | |||||
| Weight gain at latest follow‐up (g/d) ‐ stabilized infants | Mean weight gain at latest follow‐up (g/d) ‐ stabilized infants in the intervention groups ‐ was | 1198 | ⊕⊕⊕⊝ | |||
| Any breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants | Study population | RR 1.2 | 1696 | ⊕⊕⊕⊝ | ||
| 762 per 1000 | 914 per 1000 | |||||
| Moderate | ||||||
| 743 per 1000 | 892 per 1000 | |||||
| Any breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants | Study population | RR 1.17 | 1394 | ⊕⊕⊝⊝ | ||
| 711 per 1000 | 832 per 1000 | |||||
| Moderate | ||||||
| 622 per 1000 | 728 per 1000 | |||||
| Griffith quotient for psychomotor development (all subscales) at 12 months' corrected age (copy) | Mean Griffith quotient for psychomotor development (all subscales) at 12 months' corrected age (copy) in the intervention groups was | 579 | ⊕⊕⊝⊝ | |||
| *The basis for the assumed risk (eg, median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aMost of the pooled effect provided by studies with moderate or high risk of bias | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality at discharge or at 40 to 41 weeks' postmenstrual age Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 All studies | 8 | 1736 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.39, 0.92] |
| 1.2 Intermittent KMC | 5 | 619 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.19, 1.81] |
| 1.3 Continuous KMC | 3 | 1117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.38, 0.96] |
| 1.4 Duration of KMC < 2 hours/d | 2 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.22, 7.73] |
| 1.5 Duration of KMC between 6 and 15 hours/d | 3 | 431 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.07, 1.64] |
| 1.6 Duration of KMC ≥ 20 hours/d | 3 | 1117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.38, 0.96] |
| 1.7 Infant age ≤ 10 days at initiation of KMC | 5 | 1412 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.36, 0.88] |
| 1.8 Infant age > 10 days at initiation of KMC | 3 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.22, 7.73] |
| 1.9 Low/middle‐income countries | 7 | 1676 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.89] |
| 1.10 High‐income countries | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.16, 17.09] |
| 1.11 infant entered into trial before stabilization | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.33, 1.00] |
| 1.12 infant entered into trial after stabilization | 7 | 1613 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.32, 1.23] |
| 2 Mortality at 6 months of age or 6 months' follow‐up Show forest plot | 2 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.48, 2.02] |
| 2.1 Intermittent | 1 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.15, 6.90] |
| 2.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.46, 2.12] |
| 3 Mortality at 12 months' corrected age Show forest plot | 1 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.27, 1.17] |
| 3.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Continuous | 1 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.27, 1.17] |
| 4 Mortality at latest follow‐up Show forest plot | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 All studies | 12 | 2293 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.48, 0.95] |
| 4.2 Intermittent KMC | 8 | 909 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.26, 1.77] |
| 4.3 Continuous KMC | 4 | 1384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.46, 0.98] |
| 4.4 Duration of KMC < 2 hours/d | 3 | 259 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.32, 4.30] |
| 4.5 Duration of KMC between 6 and 15 hours/d | 5 | 650 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.07, 1.64] |
| 4.6 Duration of KMC ≥ 20 hours/d | 4 | 1384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.46, 0.98] |
| 4.7 Infant age ≤ 10 days at initiation of KMC | 6 | 1489 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.37, 0.85] |
| 4.8 Infant age > 10 days at initiation of KMC | 5 | 678 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.53, 2.00] |
| 4.9 Low/middle‐income countries | 10 | 2162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.45, 0.93] |
| 4.10 High‐income countries | 2 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.29, 5.42] |
| 4.11 Infant entered into trial before stabilization | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.33, 1.00] |
| 4.12 Infant entered into trial after stabilization | 11 | 2170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.47, 1.13] |
| 5 Severe infection/sepsis at latest follow‐up ‐ stabilized infants Show forest plot | 8 | 1463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.36, 0.69] |
| 5.1 Intermittent | 7 | 800 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.24, 0.60] |
| 5.2 Continuous | 1 | 663 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.43, 1.12] |
| 6 Severe illness at 6 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.14, 0.67] |
| 6.1 intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.14, 0.67] |
| 7 Nosocomial infection/sepsis at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 5 | 1239 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.22, 0.54] |
| 7.1 Intermittent | 4 | 576 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.15, 0.50] |
| 7.2 Continuous | 1 | 663 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.25, 0.93] |
| 8 Mild/moderate infection or illness at latest follow‐up ‐ stabilized infants Show forest plot | 4 | 1266 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.87, 1.88] |
| 8.1 Intermittent | 2 | 320 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.43, 5.38] |
| 8.2 Continuous | 2 | 946 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.53, 3.79] |
| 9 Lower respiratory tract disease at 6 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.15, 0.89] |
| 9.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.15, 0.89] |
| 10 Diarrhea at 6 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.35, 1.20] |
| 10.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Continuous | 1 | 283 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.35, 1.20] |
| 11 Hypothermia at discharge or at 40 to 41 weeks’ postmenstrual age ‐ stabilized infants Show forest plot | 9 | 989 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.16, 0.49] |
| 11.1 Intermittent | 9 | 989 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.16, 0.49] |
| 11.2 Continuous | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Hyperthermia at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 4 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.59, 1.05] |
| 12.1 Intermittent | 4 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.59, 1.05] |
| 12.2 Continuous | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Length of hospital stay (days) ‐ stabilized infants Show forest plot | 11 | 1057 | Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐3.41, 0.18] |
| 13.1 Intermittent | 11 | 1057 | Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐3.41, 0.18] |
| 13.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Re‐admission to hospital at latest follow‐up ‐ stabilized infants Show forest plot | 2 | 946 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.34, 1.06] |
| 14.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Continuous | 2 | 946 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.34, 1.06] |
| 15 Weight at discharge or at 40 to 41 weeks' postmenstrual age (g) ‐ stabilized infants Show forest plot | 5 | 1233 | Mean Difference (IV, Fixed, 95% CI) | 16.07 [‐20.54, 52.68] |
| 15.1 Intermittent | 3 | 285 | Mean Difference (IV, Fixed, 95% CI) | 41.84 [‐19.19, 102.87] |
| 15.2 Continuous | 2 | 948 | Mean Difference (IV, Fixed, 95% CI) | 1.59 [‐44.16, 47.34] |
| 16 Weight at 6 months' corrected age (g) ‐ stabilized infants Show forest plot | 1 | 591 | Mean Difference (IV, Fixed, 95% CI) | 78.19 [‐52.26, 208.64] |
| 16.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Continuous | 1 | 591 | Mean Difference (IV, Fixed, 95% CI) | 78.19 [‐52.26, 208.64] |
| 17 Weight at 12 months' corrected age (g) ‐ stabilized infants Show forest plot | 1 | 596 | Mean Difference (IV, Fixed, 95% CI) | 31.46 [‐135.08, 198.00] |
| 17.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Continuous | 1 | 596 | Mean Difference (IV, Fixed, 95% CI) | 31.46 [‐135.08, 198.00] |
| 18 Weight gain at latest follow‐up (g/d) ‐ stabilized infants Show forest plot | 11 | 1198 | Mean Difference (IV, Random, 95% CI) | 4.08 [2.30, 5.86] |
| 18.1 Intermittent | 10 | 913 | Mean Difference (IV, Random, 95% CI) | 4.13 [2.19, 6.07] |
| 18.2 Continuous | 1 | 285 | Mean Difference (IV, Random, 95% CI) | 3.60 [0.78, 6.42] |
| 19 Length at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants Show forest plot | 3 | 856 | Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.69, 0.48] |
| 19.1 Intermittent | 2 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.51, 1.04] |
| 19.2 Continuous | 1 | 663 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.36, 0.36] |
| 20 Length at 6 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 590 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [‐0.18, 0.64] |
| 20.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Continuous | 1 | 590 | Mean Difference (IV, Fixed, 95% CI) | 0.23 [‐0.18, 0.64] |
| 21 Length at 12 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 586 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.17, 0.79] |
| 21.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 Continuous | 1 | 586 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.17, 0.79] |
| 22 Length gain at latest follow‐up (cm/wk) ‐ stabilized infants Show forest plot | 3 | 377 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.03, 0.38] |
| 22.1 Intermittent | 3 | 377 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.03, 0.38] |
| 22.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Head circumference at discharge or at 40 to 41 weeks' postmenstrual age (cm) ‐ stabilized infants Show forest plot | 3 | 856 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.33, 0.66] |
| 23.1 Intermittent | 2 | 193 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.84, 1.31] |
| 23.2 Continuous | 1 | 663 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.14, 0.34] |
| 24 Head circumference at 6 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 592 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.11, 0.57] |
| 24.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Continuous | 1 | 592 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [0.11, 0.57] |
| 25 Head circumference at 12 months' corrected age (cm) ‐ stabilized infants Show forest plot | 1 | 597 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.00, 0.78] |
| 25.1 Intermittent | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Continuous | 1 | 597 | Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.00, 0.78] |
| 26 Head circumference gain at latest follow‐up (cm/wk) ‐ stabilized infants Show forest plot | 4 | 495 | Mean Difference (IV, Random, 95% CI) | 0.14 [0.06, 0.22] |
| 26.1 Intermittent | 4 | 495 | Mean Difference (IV, Random, 95% CI) | 0.14 [0.06, 0.22] |
| 26.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Psychomotor development (Griffith quotients) at 12 months' corrected age Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 27.1 Locomotion | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 2.25 [‐0.45, 4.95] |
| 27.2 Personal, social | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 0.97 [‐1.27, 3.21] |
| 27.3 Hand‐eye coordination | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 0.57 [‐1.25, 2.39] |
| 27.4 Audition, language | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 1.29 [‐0.98, 3.56] |
| 27.5 Execution | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐1.50, 2.10] |
| 27.6 All criteria | 1 | 579 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [‐0.75, 2.85] |
| 28 Cerebral palsy at 12 months' corrected age Show forest plot | 1 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.21, 2.02] |
| 29 Deafness at 12 months' corrected age Show forest plot | 1 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.03, 2.90] |
| 30 Visual impairment at 12 months' corrected age Show forest plot | 1 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.53, 1.56] |
| 31 Exclusive breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 6 | 1453 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.07, 1.25] |
| 31.1 Intermittent | 4 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [1.11, 1.35] |
| 31.2 Continuous | 2 | 942 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [1.00, 1.24] |
| 32 Exclusive breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants Show forest plot | 5 | 600 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.01, 1.43] |
| 32.1 Intermittent | 3 | 221 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [1.12, 1.65] |
| 32.2 Continuous | 2 | 379 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.96, 1.10] |
| 33 Exclusive breastfeeding at 6 to 12 months' follow‐up ‐ stabilized infants Show forest plot | 3 | 810 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.95, 1.76] |
| 33.1 Intermittent | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.10, 2.10] |
| 33.2 Continuous | 2 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.66, 1.86] |
| 34 Any breastfeeding at discharge or at 40 to 41 weeks' postmenstrual age ‐ stabilized infants Show forest plot | 10 | 1696 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.07, 1.34] |
| 34.1 Intermittent | 8 | 754 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.07, 1.41] |
| 34.2 Continuous | 2 | 942 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.93, 1.40] |
| 35 Any breastfeeding at 1 to 2 months' follow‐up ‐ stabilized infants Show forest plot | 6 | 538 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [1.00, 1.78] |
| 35.1 Intermittent | 4 | 159 | Risk Ratio (M‐H, Random, 95% CI) | 1.89 [1.30, 2.75] |
| 35.2 Continuous | 2 | 379 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.96, 1.10] |
| 36 Any breastfeeding at 3 months' follow‐up ‐ stabilized infants Show forest plot | 5 | 924 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [1.06, 1.23] |
| 36.1 Intermittent | 4 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.15, 1.59] |
| 36.2 Continuous | 1 | 663 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [1.00, 1.17] |
| 37 Any breastfeeding at 1 to 3 months' follow‐up ‐ stabilized infants Show forest plot | 9 | 1394 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.05, 1.31] |
| 37.1 Intermittent | 6 | 352 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [1.18, 1.64] |
| 37.2 Continuous | 3 | 1042 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.00, 1.11] |
| 38 Any breastfeeding at 6 months' follow‐up ‐ stabilized infants Show forest plot | 5 | 952 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.98, 1.29] |
| 38.1 Intermittent | 3 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [1.08, 2.08] |
| 38.2 Continuous | 2 | 809 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.92, 1.24] |
| 39 Any breastfeeding at 12 months' follow‐up ‐ stabilized infants Show forest plot | 1 | 589 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.21] |
| 39.1 Intermittent | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 39.2 Continuous | 1 | 589 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.21] |
| 40 Onset of breastfeeding (days) ‐ stabilized infants Show forest plot | 2 | 295 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.64, 1.70] |
| 40.1 Intermittent | 2 | 295 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.64, 1.70] |
| 40.2 Continuous | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Parental and familial satisfaction (continuous KMC) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 41.1 Mother satisfied with method | 1 | 269 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [1.05, 1.30] |
| 41.2 Father satisfied with method | 1 | 269 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.14] |
| 41.3 Family satisfied with method | 1 | 269 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.83, 1.13] |
| 42 Mother‐infant attachment: mother's feelings and perceptions according to interval between birth and start of intervention, and infant admission to NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 42.1 Sense of competence ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [0.14, 0.68] |
| 42.2 Sense of competence ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.08, 0.58] |
| 42.3 Sense of competence ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.17, 0.59] |
| 42.4 Sense of competence ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.07, 1.01] |
| 42.5 Sense of competence ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.05, 0.43] |
| 42.6 Worry and stress ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.31 [0.04, 0.58] |
| 42.7 Worry and stress ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.20, 0.38] |
| 42.8 Worry and stress ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.70, 0.12] |
| 42.9 Worry and stress ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.1 [‐0.60, 0.40] |
| 42.10 Worry and stress ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.06, 0.30] |
| 42.11 Social support ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.35, 0.23] |
| 42.12 Social support ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.34, 0.22] |
| 42.13 Social support ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐0.84, ‐0.10] |
| 42.14 Social support ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.52, 0.42] |
| 42.15 Social support ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | ‐0.2 [‐0.39, ‐0.01] |
| 43 Mother‐infant attachment: mother's responses to the infant according to interval between birth and start of intervention, and infant admission to NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 43.1 Mother's sensitivity ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.02, 0.06] |
| 43.2 Mother's sensitivity ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.05, 0.03] |
| 43.3 Mother's sensitivity ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [0.01, 0.11] |
| 43.4 Mother's sensitivity ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.04, 0.08] |
| 43.5 Mother's sensitivity ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.00, 0.04] |
| 43.6 Mother's response to child's distress ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.08, 0.02] |
| 43.7 Mother's response to child's distress ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.03, 0.05] |
| 43.8 Mother's response to child's distress ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.04, 0.06] |
| 43.9 Mother's response to child's distress ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.01, 0.11] |
| 43.10 Mother's response to child's distress ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.01] |
| 43.11 Mother's response to child's socioemotional growth fostering ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.04, 0.06] |
| 43.12 Mother's response to child's socioemotional growth fostering ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.02] |
| 43.13 Mother's response to child's socioemotional growth fostering ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.00, 0.10] |
| 43.14 Mother's response to child's socioemotional growth fostering ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.12, 0.02] |
| 43.15 Mother's response to child's socioemotional growth fostering ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 43.16 Mother's response to child's cognitive growth fostering ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.04, 0.08] |
| 43.17 Mother's response to child's cognitive growth fostering ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.10, 0.02] |
| 43.18 Mother's response to child's cognitive growth fostering ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [0.00, 0.14] |
| 43.19 Mother's response to child's cognitive growth fostering ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.17, 0.03] |
| 43.20 Mother's response to child's cognitive growth fostering ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.01, 0.07] |
| 44 Mother‐infant attachment: infant's responses to the mother according to interval between birth and start of intervention, and infant admission to NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 44.1 Clarity of cues ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.04, 0.06] |
| 44.2 Clarity of cues ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.03, 0.07] |
| 44.3 Clarity of cues ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 44.4 Clarity of cues ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.07, 0.05] |
| 44.5 Clarity of cues ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 44.6 Responsiveness ‐ interval of 1 to 2 days | 1 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.02] |
| 44.7 Responsiveness ‐ interval of 3 to 14 days | 1 | 177 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.02, 0.06] |
| 44.8 Responsiveness ‐ interval > 14 days | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [0.01, 0.09] |
| 44.9 Responsiveness ‐ infant admitted to NICU | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.07, 0.05] |
| 44.10 Responsiveness ‐ infant not admitted to NICU | 1 | 406 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 45 Mother‐infant attachment at 3 months' follow‐up Show forest plot | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 6.24 [5.57, 6.91] |
| 45.1 Total attachment score at 3 months' follow‐up | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 6.24 [5.57, 6.91] |
| 46 Mother‐infant attachment: stress in NICU Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 46.1 Nursery environment score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.51, 0.71] |
| 46.2 Infant appearance score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.62, 0.62] |
| 46.3 Relationship with the infant score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [0.35, 1.65] |
| 46.4 Staff behavior and communication score | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.95, 1.15] |
| 47 Mother‐infant attachment: parenting skills Show forest plot | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.89, 0.09] |
| 47.1 Total score at discharge | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.89, 0.09] |
| 48 Mother‐infant interaction at 6 months' follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 48.1 Symmetrical co‐regulation | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 16.38 [13.61, 19.15] |
| 48.2 Asymmetrical co‐regulation | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐18.31 [‐21.42, ‐15.20] |
| 48.3 Unilateral regulation | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 2.12 [‐1.24, 5.48] |
| 49 Infant behavior at 40 to 44 weeks’ postmenstrual age Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 49.1 Attention | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.29 [‐0.40, 0.98] |
| 49.2 Autonomic organization | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.41, 0.79] |
| 49.3 Motor | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.22, 0.82] |
| 49.4 Orientation | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.72, 0.34] |
| 49.5 Autonomic | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.89, 1.11] |
| 49.6 State regulation | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.95, 0.33] |
| 49.7 Robust crying | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.90, 0.58] |
| 49.8 State stability | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.93, 1.57] |
| 50 Social and home environment Show forest plot | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [0.74, 0.84] |
| 50.1 HOME environment total score at 12 months' corrected age | 1 | 338 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [0.74, 0.84] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.18, 20.53] |
| 2 Morbidity at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.28] |
| 3 Severe infection at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.12, 1.49] |
| 4 Re‐admission to hospital at 4 weeks of age Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.18, 20.53] |
| 5 Hypothermia Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.15, 2.27] |
| 6 Hyperthermia Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.56, 1.99] |
| 7 Weight gain (grams) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 At 24 hours post birth | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 39.16 [11.11, 67.21] |
| 7.2 At 48 hours post birth | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 43.3 [5.49, 81.11] |
| 7.3 At 2 weeks of age | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 12.14 [‐83.18, 107.46] |
| 7.4 At 4 weeks of age | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 58.85 [‐116.93, 234.63] |
| 8 Exclusive breastfeeding Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 At 24 hours of age | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.67, 1.57] |
| 8.2 At 2 weeks of age | 1 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.89, 1.12] |
| 8.3 At 4 weeks of age | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.85, 1.04] |
| 8.4 At 6 months of age | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.69 [0.99, 7.31] |
| 9 Length of hospital stay (days) Show forest plot | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.24, ‐0.56] |
| 10 Mortality at 6 months of age Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.72] |
| 11 Re‐admission to hospital at 6 to 12 months of age Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.32, 3.16] |
| 12 Stunting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.46, 1.48] |
| 13 Severe stunting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.17, 2.73] |
| 14 Wasting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.1 [0.01, 1.77] |
| 15 Severe wasting at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Underweight at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.21, 1.14] |
| 17 Severe underweight at 6 to 12 months of age Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.03, 1.88] |

