نقش کورتیکواستروئید استنشاقی با تاخیر (بیشتر یا مساوی با 7 روز) برای کاهش دیسپلازی برونکوپولمونری در نوزادان پرهترم
چکیده
پیشینه
دیسپلازی برونکوپولمونری (bronchopulmonary dysplasia; BPD) که یک عارضه مهم پرهمچوریتی (prematurity) نوزادان است که به صورت وابستگی به اکسیژن تا سن جنینی (postmenstrual age; PMA) 36 هفته تعریف میشود. التهاب ریوی نقش مهمی در پاتوژنز BPD بازی میکند. کم کردن التهاب ریه با کورتیکواستروئیدهای سیستمیک پس از زایمان (postnatal) بروز BPD را در نوزادان پرهترم کاهش میدهد اما ممکن است با افزیش خطر پیامدهای جانبی تکامل سیستم عصبی همراه باشد. تجویز موضعی کورتیکواستروئیدها از طریق استنشاق ممکن است جایگزین موثر و ایمنی باشد.
اهداف
هدف این مرور سیستماتیک تعیین این نکته بود که تجویز کورتیکواستروئیدهای استنشاقی پس از اولین هفته حیات تا 36 هفتگی PMA در نوزادان پرهترم در معرض خطر بالای BPD در کاهش بروز مرگومیر و BPD به صورت مجزا یا پیامدهای ترکیبی موثر و ایمن است یا خیر.
روشهای جستوجو
ما از استراتژی جستوجوی استاندارد گروه نوزادان در کاکرین استفاده کردیم که شامل جستوجو در این موارد بود: پایگاه ثبت مرکزی کارآزماییهای کنترل شده کاکرین ( CENTRAL؛ شماره 4؛ 2017 )؛ MEDLINE via PubMed (از 1966 تا 19 می 2017)، Embase (از 1980 تا 19 می 2017)؛ و CINAHL (از 1982 تا 19 می 2017). بانکهای اطلاعاتی کارآزماییهای بالینی، خلاصه مقالات کنفرانسها و فهرست منابع مقالات بازیابی شده را برای یافتن کارآزماییهای تصادفیسازی و کنترل شده و کارآزماییهای شبه‐تصادفیسازی شده جستوجو کردیم..
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شدهای را وارد کردیم که دارای این ویژگی بودند: تجویز کورتیکواستروئیدهای استنشاقی با تاخیر یعنی بیشتر یا مساوی با 7 روز پس از زایمان (postnatal age; PNA) اما پیش از 36 هفته PMA در مقایسه با دارونما (placebo) در نوزادان در معرض خطر BPD ونتیله شده یا ونتیله نشده. کارآزماییهایی را که کورتیکواستروئیدهای سیستمیک را در برابر نوع استنشاقی آن مقایسه کرده بودند از این مرور کنار گذاشتیم.
گردآوری و تجزیهوتحلیل دادهها
دادهها را بر اساس خصوصیات شرکتکنندگان، متدولوژی کارآزمایی و نوع رژیمهای استنشاقی جمعآوری کردیم. پیامد اولیه شامل مرگومیر یا BPD در 36 هفته PMA بود. پیامدهای ثانویه، ترکیب پیامد مرگومیر یا BPD در PNA حدود 28 روزگی، پیامدهای جداگانه مرگومیر و BPD هم در PNA حدود 28 روزگی و 36 هفتگی و پیامدهای تنفسی کوتاه‐مدت مانند ناتوانی در اکستوبه کردن (برداشتن لوله جایگذاری شده در نای)، کل روزهایی که نوزاد تحت ونتیلاسیون مکانیکی بوده و از اکسیژن استفاده میکرد و نیاز به کورتیکواستروئیدهای سیستمیک داشته است. با محققان اصلی کارآزماییها تماس گرفتیم تا اعتبار دادههای استخراج شده را تایید کنیم و دادههای ازدسترفته را نیز به دست آوریم. تمام دادهها را با استفاده از نرمافزار Review Manager 5 تجزیهوتحلیل کردیم. متاآنالیز را، در جایی که امکانپذیر بود، با استفاده از خطر نسبی (RR) معمول برای پیامدهای دو‐حالتی و تفاوت میانگین وزندهی شده (WMD) برای پیامدهای پیوسته همراه با 95% فواصل اطمینان (CI) آنها انجام دادیم. نوزادان ونتیله شده و ونتیله نشده را به طور جداگانه تجزیهوتحلیل کردیم.
از رویکرد درجهبندی توصیه، ارزیابی، توسعه و ارزشیابی (GRADE) برای ارزیابی کیفیت شواهد استفاده کردیم.
نتایج اصلی
هشت کارآزمایی را با تصادفیسازی 232 نوزاد پرهترم در این مرور وارد کردیم. کورتیکواستروئیدهای استنشاقی پیامدهای جداگانه یا ترکیبی از مرگومیر یا BPD را کاهش ندادند. متاآنالیز مطالعات، کاهش خطر ناتوانی در اکستوبه کردن را در روز هفتم با استروئیدهای استنشاقی (RR معمول (TRR): 0.80؛ 95% CI؛ 0.66 تا 0.98؛ 5 مطالعه؛ 79 شیرخوار) و در آخرین زمان گزارش شده پس از شروع درمان (TRR: 0.60؛ 95% CI؛ 0.45 تا 0.80؛ 6 مطالعه؛ 90 شیرخوار) نشان داد. با این حال هر دو تجزیهوتحلیل نشان دهنده افزایش ناهمگونی آماری بود (آماره I2 به ترتیب 73% و 86%). همچنین استروئیدهای استننشاقی تاثیری بر طول مدت استفاده از ونتیلاسیون مکانیکی یا وابستگی به اکسیژن نداشتند. معمولا این تمایل وجود دارد که از کورتیکواستروئیدهای سیستمیک در کودکانی که نوع استنشاقی آن را دریافت میکنند کمتر استفاده شود (RRT: 0.51؛ 95% CI؛ 0.26 تا 1.00؛ 4 مطالعه؛ 74 شیرخوار؛ شواهد با کیفیت بسیار پائین). دادههای اندکی درباره عوارض جانبی کوتاه‐مدت و طولانیمدت وجود دارد. نتایج ما باید بنا به این دلایل با احتیاط تفسیر شوند: تعداد کلی شرکتکنندگان تصادفیسازی شده نسبتا پائین بود و اکثر کارآزماییها در خصوصیات شرکتکنندگان، درمان استنشاقی و تعاریف پیامد با یکدیگر متفاوت بودند.
نتیجهگیریهای نویسندگان
بر اساس نتایج شواهد فعلی در دسترس، تجویز کورتیکواستروئیدهای استنشاقی در ≥ 7 روز از زندگی برای نوزادان پرهترم در معرض خطر BPD نمیتواند در این مقطع زمانی توصیه شود. کارآزماییهای تصادفیسازی و کنترل شده با دارونما (placebo) بیشتر و بزرگتری نیاز است تا اثربخشی و ایمنی کورتیکواستروئیدهای استنشاقی را تثبیت کند.
PICO
خلاصه به زبان ساده
کورتیکواستروئیدهای استنشاقی برای درمان برونکوپولمونری دیسپلازی
سوال مطالعه مروری
آیا استنشاق کورتیکواستروئیدها پس از اولین هفته زندگی خطر ابتلا به برونکوپولمونری دیسپلازی (bronchopulmonary dysplasia; BPD) را در نوزادان پرهترم کاهش میدهد؟ این مرور به بررسی مطالعاتی پرداخت که در آنها نوزادان پرهترم در معرض خطر BPD پس از اولین هفته زندگی تحت درمان با کورتیکواستروئیدهای استنشاقی با نوزادان تحت درمان با دارونمای (placebo) استنشاقی مقایسه شده بودند.
پیشینه
نوزادان پرهترم در معرض خطر بالای ابتلا به بیماری مزمن ریوی یا برونکودیسپلازی ریوی قرار دارند. التهاب در ریه یک نقش محوری در ابتلا به BPD بازی میکند. تجویز داروهای ضد‐التهابی مانند کورتیکواستروئیدها در جریان خون (به صورت سیستمیک) خطر BPD را کاهش میدهد اما در عین حال میتواند باعث ایجاد عوارض جانبی جدی نیز شود. تجویز کورتیکواستروئیدها به روش استنشاق که مستقیما به داخل ریهها برود، ممکن است این عوارض جانبی را کاهش دهد.
ویژگیهای مطالعه
ما هشت مطالعه را که به بررسی این نوع درمان در 232 نوزاد پرداخته بودند، شناسایی کردیم. اگرچه ما خطر سوگیری (bias) را پائین میدانیم، اما تعداد بسیار کمی از مطالعات پیامدهای مورد علاقه ما را گزارش کردهاند.
نتایج کلیدی
کارآزماییهای وارد شده در این مرور، هیچ تاثیر سودمندی را از کورتیکواستروئیدهای استنشاقی بر مرگومیر یا BPD نشان ندادند. علاوه بر این، ایمنی کورتیکواستروئیدهای استنشاقی در تعداد کمی از کارآزماییها ارزیابی شده بود. بر اساس این نتایج، شروع کورتیکواستروئیدهای استنشاقی پس از اولین هفته زندگی نمیتواند برای نوزادان پرهترم در معرض خطر BPD توصیه شود. انجام مطالعات بیشتری در این زمینه لازم است.
کیفیت شواهد
کیفیت شواهد برای پیامدهای اصلی پائین تا بسیار پائین بود.
Authors' conclusions
Summary of findings
| Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants | ||||||
| Patient or population: preterm infants | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with inhaled corticosteroids | |||||
| Combined outcome mortality or bronchopulmonary dysplasia at 36 weeks postmenstrual age | Study population | RR 1.10 | 30 | ⊕⊝⊝⊝ | ||
| 533 per 1000 | 587 per 1000 | |||||
| Mortality at 36 weeks postmenstrual age | Study population | RR 3.00 | 61 | ⊕⊕⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Bronchopulmonary dysplasia at 36 weeks postmenstrual age | Study population | RR 1.00 | 30 | ⊕⊝⊝⊝ | ||
| 600 per 1000 | 600 per 1000 | |||||
| Open‐label intravenous corticosteroids | Study population | RR 0.51 | 74 | ⊕⊝⊝⊝ | ||
| 432 per 1000 | 320 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Risk of bias: No serious limitations. No downgrade. | ||||||
Background
Description of the condition
Bronchopulmonary dysplasia (BPD), defined as oxygen dependency at 36 weeks postmenstrual age (PMA), is the most important complication of prematurity, with a reported incidence of 23% in infants born at 28 weeks and increasing to 73% in infants born at 23 weeks (Stoll 2010). Bronchopulmonary dysplasia is characterised by prolonged respiratory support, compromised lung function, and recurrent respiratory infections during the first years of life (Bolton 2015; Doyle 2006). Furthermore, BPD is considered an independent risk factor for neurodevelopmental impairment (Short 2007; Walsh 2005). Bronchopulmonary dysplasia is a multifactorial disease with mechanical ventilation, oxygen toxicity, and pre‐ and postnatal infection as the most important risk factors, and pulmonary inflammation playing a central mediating role.
Description of the intervention
The intervention of interest was inhaled corticosteroids administered to either ventilated or non‐ventilated newborn infants at risk of developing BPD. Budesonide, beclomethasone, and fluticasone are the most frequently used inhaled corticosteroids in newborn infants, and these drugs are almost exclusively delivered using a pressurised metered dose inhaler or a nebuliser. Studies in preterm infants have revealed that metered‐dose inhalation results in a far better deposition than nebulisation. In addition, inhalation via an endotracheal tube provides better deposition than inhalation via a face mask (Fok 1996).
How the intervention might work
Pulmonary inflammation plays a central modulating role in the pathogenesis of BPD (Jobe 2001; McEvoy 2014; Pierce 1995). Corticosteroids have a strong anti‐inflammatory effect, making them an ideal candidate to attenuate the inflammatory response associated with BPD. Randomised controlled trials (RCTs) have shown that systemic administration of corticosteroids reduces the incidence of BPD and the combined outcome of death or BPD in ventilated preterm infants (Doyle 2014; Doyle 2014a). However, systemic corticosteroids are also associated with short‐term (e.g. hyperglycaemia, hypertension, infection) and long‐term (neurodevelopmental impairment) adverse effects. This balance between beneficial and adverse effects of corticosteroids may be more favourable when using the inhalation route because, ideally, inhaled corticosteroids should demonstrate high pulmonary deposition in addition to a low systemic bioavailability and rapid systemic clearance.
Why it is important to do this review
The association between early (< 7 days of life) systemic corticosteroids use and adverse neurodevelopmental outcomes has resulted in a reduction in the overall use of corticosteroids in ventilated preterm infants (Cheong 2013; Walsh 2006; Yoder 2009). Administering corticosteroids by inhalation might be a safe and effective alternative, and this method of administering corticosteroids to infants at risk for BPD is already frequently being used in every part of the world (Job 2015; Maas 2010; Ogawa 2015; Slaughter 2014). A systematic review of the randomised evidence on inhaled corticosteroids in preterm infants was first published in the Cochrane Library in 1999, followed by an update in 2002 (Lister 2000). The second update of this systematic review included those RCTs published after 2002 and extended the inclusion criteria by including all RCTs initiating inhalation corticosteroids after the first week of life, in line with the Cochrane Reviews on systemic corticosteroids (Doyle 2014; Doyle 2014a). The conclusions of that review were that in ventilated infants, administration of inhalation corticosteroids resulted in an improved rate of extubation without any apparent adverse effects. No firm conclusions could be drawn for non‐ventilated infants (Onland 2012).
Other Cochrane Neonatal reviews of corticosteroids in the Cochrane Library
Additional neonatal reviews in the Cochrane Library that address the use of corticosteroids in the prevention or treatment of bronchopulmonary dysplasia include the following.
-
Use of systemic steroids:
-
early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants (Doyle 2014a);
-
late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants (Doyle 2014);
-
systemic corticosteroid regimens for the prevention of bronchopulmonary dysplasia in preterm infants (Onland 2017).
-
-
Inhaled steroids:
-
early administration of inhaled corticosteroids for preventing chronic lung disease in ventilated very low birthweight preterm neonates (Shah 2017).
-
-
Comparison trials (inhaled versus systemic corticosteroids):
-
inhaled versus systemic corticosteroids for preventing chronic lung disease in ventilated very low birthweight preterm neonates (Shah 2012);
-
inhaled versus systemic corticosteroids for the treatment of chronic lung disease in ventilated very low birthweight preterm infants (Shah 2012a).
-
-
Other studies of corticosteroids in neonates:
-
intravenous dexamethasone for extubation of newborn infants (Davis 2001);
-
corticosteroids for treating hypotension in preterm infants (Ibrahim 2011);
-
steroid therapy for meconium aspiration syndrome in newborn infants (Ward 2003).
-
Objectives
To determine if administration of inhalation corticosteroids after the first week of life until 36 weeks PMA to preterm infants at high risk of developing BPD is effective and safe in reducing the incidence of death and BPD as separate or combined outcomes.
The secondary objective was to compare the effectiveness of inhaled corticosteroids versus placebo on respiratory support, the need for systemic corticosteroids, and adverse effects during hospitalisation and long‐term follow‐up. Furthermore, we performed subgroup analyses on the timing of therapy onset and the difference in effect estimates for ventilated and non‐ventilated infants.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised placebo‐controlled trials.
Types of participants
Preterm infants ≥ 7 days postnatal age (PNA) but before 36 weeks PMA needing mechanical ventilation or supplemental oxygen, or both.
Types of interventions
We included trials if infants were randomised to treatment with inhalation corticosteroid or placebo. The intervention had to be a standardised (non‐individualised) dosage regimen of inhalation corticosteroids, initiated between seven days of life and 36 weeks PMA. We excluded studies investigating inhalation corticosteroids compared to, or in addition to, systemic corticosteroids (dexamethasone, hydrocortisone, or methylprednisolone).
Types of outcome measures
To be included in the review, the trials had to report on one or more of the following outcome parameters.
-
The combined outcome death or BPD at 28 days PNA and 36 weeks PMA
-
Death at 28 days PNA, 36 weeks PMA, and hospital discharge
-
BPD (defined as the need for supplemental oxygen) at 28 days PNA and 36 weeks PMA
-
Failure to extubate at day 7 and 14 after initiating therapy and at the latest reported time point
-
Days of mechanical ventilation
-
Days of supplemental oxygen
-
Days of hospitalisation
-
The use of systemic corticosteroids
-
Sepsis, defined as clinical suspected or culture proven
-
Hypertension
-
Hyperglycaemia
-
Gastrointestinal bleeding or perforation (spontaneous intestinal perforation)
-
Necrotising enterocolitis
-
Patent ductus arteriosus (PDA)
-
Intraventricular haemorrhage, any grade
-
Periventricular leukomalacia
-
Retinopathy of prematurity, any grade
-
Long‐term neurodevelopmental sequelae, assessed after at least one year corrected gestational age (CGA) and before a CGA of four years, including cerebral palsy and Bayley Scales of Infant Development (Mental Development Index)
-
Blindness
-
Deafness
Primary outcomes
-
Combined outcome of death or BPD at 36 weeks PMA (BPD defined as oxygen dependency at 36 weeks PMA).
Secondary outcomes
Secondary outcomes in the ventilated infants were total duration of mechanical ventilation, failure to extubate at day 7 and day 14 after initiating therapy and, in the non‐ventilated infants, the supplemental fractional concentration of inspired oxygen (FiO2).
In both groups further secondary outcomes were mortality at hospital discharge, at 28 days PNA, and 36 weeks PMA, BPD at 28 days PNA and at 36 weeks PMA, the airway resistance, dynamic lung compliance, the use of systemic corticosteroids; incidence of PDA, necrotising enterocolitis, hypertension, sepsis, or hyperglycaemia during hospitalisation; long‐term neurodevelopmental sequelae, assessed after at least one‐year corrected gestational age (CGA) and before a CGA of four years including cerebral palsy and Bayley Scales of Infant Development (Mental Development Index).
Search methods for identification of studies
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal search strategy for specialized register).
Electronic searches
We conducted a comprehensive search including: Cochrane Central Register of Controlled Trials (CENTRAL 2017, Issue 4) in the Cochrane Library; MEDLINE via PubMed (1966 to 19 May 2017); Embase (1980 to 19 May 2017); and CINAHL (Cumulative Index to Nursing and Allied Health Literature) (1982 to 19 May 2017) using the following search terms: (Adrenal cortex hormones[MeSH] OR steroids[MeSH] OR glucocorticoid OR dexamethasone OR flixotide OR fluticasone OR becotide OR beclomethasone OR pulmicort OR budesonide OR (anti‐inflammatory Agents[MeSH] NOT anti‐inflammatory Agents, non‐steroidal[MeSH])) AND (inhal* OR nebulis* OR nebuliz* OR aerolis* OR aeroliz*), plus database‐specific limiters for RCTs and neonates (see Appendix 1 for the full search strategies for each database). We applied no language restrictions.
See Appendix 2 for the search methodology used in previous versions of this review.
We searched clinical trials registries (19 May 2017) for ongoing or recently completed trials (ClinicalTrials.gov (www.clinicaltrials.gov/), the World Health Organization International Clinical Trials Registry Platform (www.whoint/ictrp/search/en/), and the ISRCTN registry (www.isrctn.com/)).
Searching other resources
We also searched the reference lists of any articles selected for inclusion in this review in order to identify additional relevant articles.
Data collection and analysis
Selection of studies
Two review authors (WO and AvK) further classified the relevant citations found following the database searches into three groups, namely 'clearly an RCT', 'clearly not an RCT', and 'possibly an RCT'. We performed full‐text review on all studies except those 'clearly not an RCT'. We resolved any disagreements by consensus.
Data extraction and management
In addition to the predefined outcome parameters, two review authors (WO and AvK) independently extracted the following clinical data using a preset data extraction form: participant characteristics (birthweight, gestational age, gender), number of participants randomised, treatment with antenatal glucocorticoids, postnatal surfactant. We resolved any disagreement by consensus.
We asked the original investigators of the included RCTs to confirm whether the data extraction was accurate and, where necessary, to provide additional (unpublished) data.
Assessment of risk of bias in included studies
Two review authors (WO and AvK) independently assessed the risk of bias (low, high, or unclear) of all included trials using the Cochrane ‘Risk of bias’ tool for the following domains (Higgins 2011).
-
Sequence generation (selection bias)
-
Allocation concealment (selection bias)
-
Blinding of participants and personnel (performance bias)
-
Blinding of outcome assessment (detection bias)
-
Incomplete outcome data (attrition bias)
-
Selective reporting (reporting bias)
-
Any other bias
Any disagreements were resolved by discussion or by a third assessor. See Appendix 3 for a more detailed description of risk of bias for each domain.
Measures of treatment effect
We performed meta‐analysis of the extracted data using the standard methods of the Cochrane Neonatal Review Group. We processed the extracted data using the Cochrane statistical package, RevMan 5. Treatment effect estimates for all trials were calculated, expressed as typical risk ratio (typical RR) for dichotomous outcomes and weighted mean difference (WMD) for continuous outcomes, all with a 95% confidence interval (CI).
Unit of analysis issues
This review did not include trials with non‐standard designs, and no effect measures for counts and rates were necessary.
Dealing with missing data
All trials were performed with an intention‐to‐treat analysis. We asked the original investigators of the included RCTs to provide additional (unpublished) data.
Assessment of heterogeneity
We assessed heterogeneity between trials by inspecting the forest plots and quantifying the impact of heterogeneity employing the I2 statistic, using the following categories as defined by the Cochrane Neonatal Review Group.
-
Less than 25%: no heterogeneity
-
25% to 49%: low heterogeneity
-
50% to 74%: moderate heterogeneity
-
75% or greater: high heterogeneity
We explored possible causes of statistical heterogeneity using prespecified subgroup analysis (e.g. differences in inclusions of ventilated and non‐ventilated infants). We used fixed‐effect models for the meta‐analyses.
Assessment of reporting biases
We planned funnel plots to assess possible reporting biases. We used no language restriction in the search strategy.
Data synthesis
We performed meta‐analysis of the extracted data using standard Cochrane methods and Review Manager 5. Treatment effects for dichotomous outcomes were expressed as typical RR with a 95% CI, typical risk difference (TRD), and number needed to treat for an additional beneficial outcome (NNTB) or number needed to treat for an additional harmful outcome (NNTH) in case of significance. We used mean differences (MD) for continuous outcomes. In case of variance of outcome measures (with different standard deviation) measuring the same outcome, we calculated standardised mean differences (SMD) in the meta‐analysis. We used fixed‐effect models.
Quality of evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the quality of evidence for the following (clinically relevant) outcomes: the combined outcome of BPD or death at 36 weeks PMA, as well as the combined outcomes of death or cerebral palsy, and death or abnormal neurodevelopmental outcome, and open‐label rescue therapy of systemic corticosteroids during study medication or after study medication was stopped.
Two review authors (WO and AvK) independently assessed the quality of the evidence for each of the outcomes above. We considered evidence from RCTs as high quality but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias), consistency across studies, directness of the evidence, precision of estimates, and presence of publication bias. We used GRADEpro to create a ‘Summary of findings’ table to report the quality of the evidence (GRADEpro GDT).
The GRADE approach results in an assessment of the quality of a body of evidence in one of the following four grades.
-
High: We are very confident that the true effect lies close to that of the estimate of the effect.
-
Moderate: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
-
Low: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
-
Very low: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Subgroup analysis and investigation of heterogeneity
We handled data on outcomes of ventilated and non‐ventilated participants at trial entry as two separate subgroups.
Sensitivity analysis
We planned sensitivity analyses to examine the potential influence of treatment variation (type and dose of inhalation corticosteroid, duration of treatment, and delivery system).
Results
Description of studies
See Characteristics of included studies.
Results of the search
The original search strategy in 2011 identified 46 relevant manuscripts (27 published in MEDLINE and 19 by handsearching) (Figure 1). Electronic searches of Embase, CINAHL, and CENTRAL in 2011 revealed no new relevant manuscripts. Two review authors (WO and AvK) independently reviewed the abstracts of these studies for inclusion in this review. There was consensus between the review authors. The electronic search of the different registries from 2011 to 2017 revealed one potentially eligible abstract (Figure 2). However, after reading the full‐text manuscript, we excluded this RCT because it included only infants > 36 weeks PMA (Kugelman 2017).
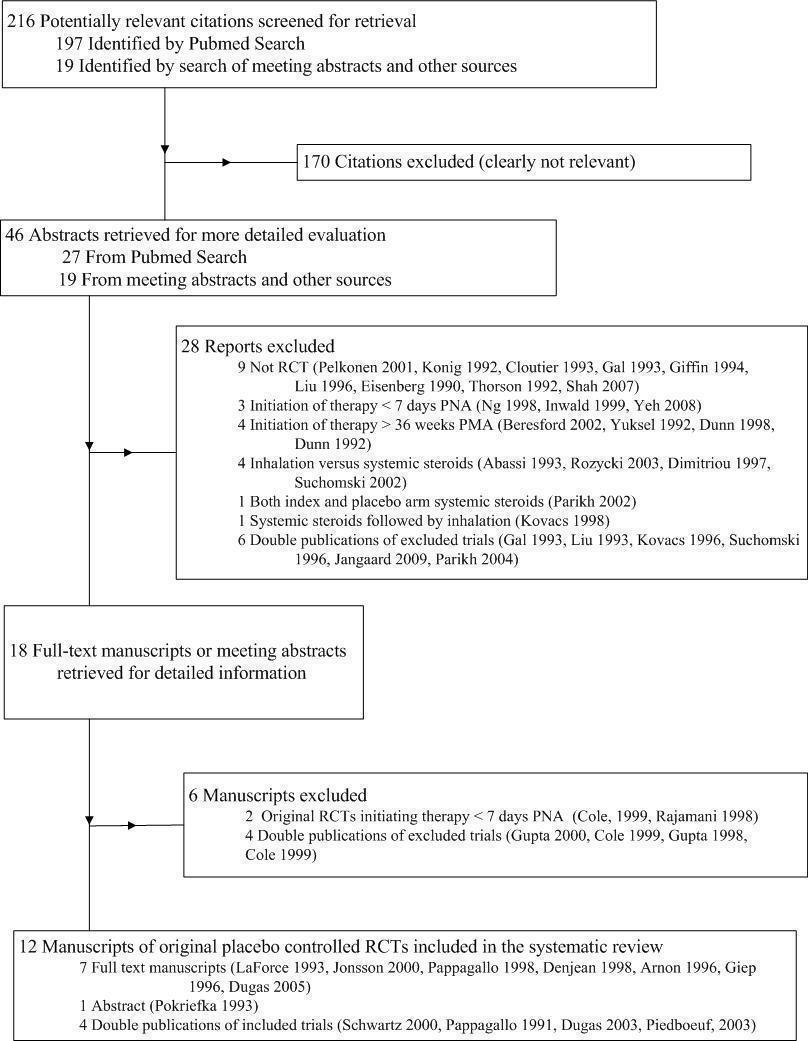
Flow of inclusion of randomised controlled trials in different phases of search.

Study flow diagram: review update.
Included studies
Eight RCTs, reported in a total of 12 manuscripts, met the inclusion criteria for this review. Seven trials were available as full‐text publications (Arnon 1996; Denjean 1998; Dugas 2005; Giep 1996; Jonsson 2000; LaForce 1993; Pappagallo 1998), and one as an abstract (Pokriefka 1993).
Description of separate trials
Arnon 1996: This double‐blind trial included 20 preterm infants with a birthweight < 2000 grams and a gestational age < 33 weeks that were still in need of mechanical ventilation at 14 days PNA with a FiO2 ≥ 0.30. Participants with PDA, sepsis, air leak, or congenital malformation were not included. Eligible participants were randomly assigned to budesonide 600 μg twice daily or placebo given by metered‐dose inhalation (MDI), inserted into small volume spacer, for seven days or until extubation, whichever came first. From the reported outcome parameters, only the rate of PDA and sepsis rate during the study period could be used for this review. The authors provided additional data on extubation rate.
Denjean 1998: This was a double‐blind, placebo‐controlled, multicentre trial conducted in six centres in France over a two‐year period. A total of 86 preterm infants with gestational age < 31 weeks, respiratory distress syndrome (RDS), and in need of mechanical ventilation, nasal ventilation, or continuous positive airway pressure at 10 days PNA were included in this study. Infants with PDA, sepsis, pulmonary infections, major malformation, or prior treatment with corticosteroids or bronchodilators were excluded. Although this study consisted of four treatment arms, only those infants treated with beclomethasone 250 μg/puff delivered by a MDI (inserted into a small volume spacer) four times a day or placebo were included in this review. Therapy was started on the 10th or 11th day and given for 28 days with a tapering dose for the last eight days. The primary outcome was BPD, defined as oxygen dependency at 28 days PNA in combination with radiographic abnormalities consistent with BPD. However, except for the total duration of supplemental oxygen, all outcomes of interest for this review were presented for the combined group of ventilated and non‐ventilated infants and were therefore excluded from the final analysis. The author provided additional data on the randomisation process.
Dugas 2005: This was a double‐blind, randomised trial of 32 infants with a gestational age ≤ 32 weeks, postnatal age between 28 and 60 days, and a diagnosis of BPD, which was defined as FiO2 ≥ 0.25 to maintain oxygen saturation between 88% and 92%, partial pressure of carbon dioxide (pCO2) ≥ 45 mmHg, and chest radiography consistent with BPD. Reasons for exclusion were hypertension, hyperglycaemia, sepsis, pneumonia, renal failure, treatment with corticosteroids five days prior to inclusion, a FiO2 ≥ 0.30 in ventilated or FiO2 ≥ 0.40 in non‐ventilated infants, and congenital heart disease. The infants were treated with placebo or fluticasone propionate 125 μg/puff given by MDI inserted into a small volume spacer and interposed between an anaesthesia bag and the tube or a face mask. Infants with a birthweight between 500 and 1200 grams received one puff twice daily for three weeks and once daily in the fourth week. The number of puffs was double if the infant's weight was ≥ 1200 grams. The primary outcome was the total duration of supplemental oxygen. Other outcomes, such as total duration of hospitalisation or duration of mechanical ventilation, were only reported for the combined group of ventilated and non‐ventilated infants and therefore could not be used for this review. From the reported outcome parameters, only mortality at 36 weeks PMA, mortality at hospital discharge, open‐label intravenous glucocorticoids, and hyperglycaemia during the study period in the ventilated subgroup could be used for this review. The original authors did not provide additional data.
Giep 1996: A total of 19 infants were included in this feasibility and safety study with a randomised design. Infants were eligible if their birthweight was between 500 and 1500 grams, the X‐ray showed signs of RDS or BPD, the postnatal age was at least 14 days, and the infant was still mechanically ventilated with a FiO2 > 0.40 and a peak inspiratory pressure > 14 cm H2O after failing an extubation attempt. Infants with PDA, sepsis, congenital heart disease, congenital malformations, or previous postnatal or concurrent administration of corticosteroids were not included. The participating infants were randomised to be treated with beclomethasone (1 mg/kg/day) or placebo delivered by MDI and an AeroChamber. Infants weighing 500 to 799 grams, 800 to 1000 grams, 1001 to 1300 grams, and above 1300 grams were treated with three, four, five, and six puffs every eight hours, respectively, for a total duration of seven days. We included the reported outcomes failure to extubate, use of systemic corticosteroids, sepsis rate, and intraventricular haemorrhage in this review. Although data on blood pressure and blood glucose were reported on a daily basis, the number of infants with hypertension and hyperglycaemia was not reported. Attempts to contact the original authors failed.
Jonsson 2000: In this double‐blind, placebo‐controlled study, 30 very low birthweight infants, either mechanically ventilated or supported by continuous positive airway pressure with FiO2 ≥ 0.3, were randomised to budesonide or placebo, delivered by an electronic dosimetric jet nebuliser. Infants with malformations, congenital heart disease, intraventricular haemorrhage grades III‐IV, deteriorating ventilator settings, or on high frequency ventilation were excluded. Starting on day seven of life, infants were treated with a dose of 500 μg twice a day for a total duration of 14 days. Reported outcomes of interest for this review were use of open‐label corticosteroids, failure to extubate on day 14 in the ventilated subgroup, and mortality at hospital discharge and at 36 weeks PMA. The authors provided separate data for the ventilated and non‐ventilated subgroups for the outcomes oxygen requirements at 28 days of age and at 36 weeks PMA, duration of supplemental oxygen, duration of mechanical ventilation, failure to extubate, and the adverse outcomes hyperglycaemia, hypertension, and sepsis.
LaForce 1993: This prospective, randomised, paired analysis study included infants with a birthweight < 1500 grams and RDS who were ventilator dependent at 14 days with X‐ray abnormalities indicative of BPD. Infants with PDA, pneumonia, sepsis, congenital heart disease, or an air leak were not included. Those allocated to the intervention group were treated with nebulised beclomethasone dipropionate 50 μg three times a day for 28 days. Medication was delivered via a Whisper Jet nebuliser system in the ventilator circuit or a blow‐by with 8 litre of humidified gas per minute in ventilated and non‐ventilated infants, respectively. The reported outcome of interest for this review was mortality at hospital discharge.The original authors provided data on randomisation and sepsis rates.
Pappagallo 1998: This single‐centre study included preterm infants with a birthweight < 1500 grams of more than seven days PNA with a high probability of developing BPD based on a prediction model or ventilator dependency. This study had two phases, with only the second phase having a randomised, placebo‐controlled design. We used data on the 18 infants included in this second phase for this review. Infants with sepsis, pulmonary hypoplasia, congenital anomalies, or heart disease were excluded. Infants were randomly assigned to dexamethasone inhalation 1 mg/kg 8‐hourly for seven days followed by 0.5 mg/kg for three days or placebo using a jet nebuliser. The reported outcomes of interest for this review were the use of intravenous corticosteroids, duration of mechanical ventilation, days on supplemental oxygen, and total duration of hospitalisation. We found the rate of failure to extubate in an abstract identified by handsearching, which reported on the preliminary outcomes of 10 infants. The original authors could not provide additional data.
Pokriefka 1993: In this RCT, 14 ventilator‐dependent preterm infants with moderate to severe BPD were enrolled and treated with flunisolide or placebo for 28 days, followed by a weaning schedule. No inclusion or exclusion criteria were described. This study was available only as an abstract, reporting clinical and respiratory outcomes without dichotomous or continuous data. Continuous data on the mean number of intubation days were reported with neither standard deviations nor standard errors, therefore these data could not be used. The rates of extubation were stated, although not on which day after initiating therapy. We used these data in the outcome failure to extubate at the latest reported time point. All attempts to contact the original authors failed.
Description of aggregated participant characteristics and intervention
Five trials included only ventilated infants at trial entry (Arnon 1996; Giep 1996; LaForce 1993; Pappagallo 1998; Pokriefka 1993), whereas three trials included both ventilated and non‐ventilated preterm infants (Denjean 1998; Dugas 2005; Jonsson 2000). Criteria for including participants were comparable between trials, that is ventilator or oxygen dependency, or both, at ≥ 7 days PNA. The exclusion criteria were the presence of a PDA, signs of sepsis, congenital malformations, and treatment with postnatal corticosteroids prior to inclusion. Most trials started therapy moderately early (seven to 21 days PNA), whereas one study started therapy > 21 days PNA (delayed onset) (Dugas 2005). The gestational age and birthweight of the included infants were comparable between trials.
Three trials did not report on the use of antenatal corticosteroids or postnatal surfactant (LaForce 1993; Pappagallo 1998; Pokriefka 1993). In the remaining trials the use of antenatal corticosteroids and postnatal surfactant varied from 25% to 80% and 69% to 100%, respectively. Within the trials, participants in the treatment and placebo groups were similar with regard to clinical characteristics such as birthweight, gestational age, gender, use of antenatal corticosteroids and surfactant, Apgar scores, FiO2 and ventilator settings or respiratory support at trial entry.
Interventions differed in every trial with regard to the type of corticosteroid, dosage, delivery system, and duration of treatment. The corticosteroids used included beclomethasone, flunisolide, budesonide, and dexamethasone. Delivery systems included MDI with a spacer device and nebulisation. Total duration of study medication ranged from seven to 28 days.
Description of aggregated outcome parameters
Three trials reported or provided data on mortality in the ventilated infants at the different points in hospitalisation (mortality at 28 days PNA, 36 weeks PMA, and at hospital discharge) (Dugas 2005; Jonsson 2000; LaForce 1993), whereas Jonsson 2000 provided us with additional data on non‐ventilated infants.
None of the manuscripts reported the incidence of BPD at 28 days PNA or 36 weeks PMA for the ventilated and non‐ventilated infants separately; however, we obtained these data for the study of Jonsson 2000 by personal communication.
Five trials reported failure to extubate seven days after initiating therapy (Arnon 1996; Dugas 2005; Giep 1996; Jonsson 2000; Pappagallo 1998), whereas Pokriefka 1993 reported failure to extubate at an unknown date. Three trials reported on the duration of mechanical ventilation for the subgroup of ventilated infants at trial entry (Dugas 2005; Jonsson 2000; Pappagallo 1998). Four trials reported data on the total days of supplemental oxygen in the subgroup of ventilated infants (Denjean 1998; Dugas 2005; Jonsson 2000; Pappagallo 1998), and two in the subgroup of non‐ventilated infants (Denjean 1998; Jonsson 2000). Pappagallo 1998 reported total days of hospitalisation in the intervention and placebo arms.
Five trials reported the incidence of open‐label corticosteroid use outside the study protocol in both arms (Denjean 1998; Dugas 2005; Giep 1996; Jonsson 2000; Pappagallo 1998). Four studies reported or provided additional data on the outcome of sepsis (Arnon 1996; Giep 1996; Jonsson 2000; LaForce 1993). The studies of Arnon 1996, Giep 1996, Jonsson 2000, and LaForce 1993 also reported or provided additional data on one of the following outcomes in both arms: PDA, hypertension, necrotising enterocolitis, and intraventricular haemorrhage.
Three studies reported no increase in adverse side effects, such as impaired glucose homeostasis and hypertension, but did not provide the actual data in the manuscripts (Arnon 1996; Giep 1996; Pokriefka 1993).
None of the included trials reported on gastrointestinal bleeding or perforation, periventricular leukomalacia, retinopathy of prematurity, and long‐term neurodevelopmental sequelae. None of the original authors were able to provide data on these outcomes.
Excluded studies
See Characteristics of excluded studies table.
We excluded 29 trials (17 full‐text publications and 12 abstracts) for the following reasons (Figure 1; Figure 2): non‐randomised design or without placebo (N = 9) (Cloutier 1993; Eisenberg 1990; Giffin 1994; Konig 1992; Liu 1996; Pappagallo 1990; Pelkonen 2001; Shah 2007; Thorson 1992), initiation of therapy before seven days PNA or after 36 weeks PMA (N = 8) (Beresford 2002; Dunn 1989; Dunn 1992; Inwald 1999; Kugelman 2017; Ng 1998; Yeh 2008; Yuksel 1992), administration of systemic steroids as co‐intervention or as control intervention (N = 6) (Abbasi 1993; Kovacs 1998; Parikh 2002; Rozycki 2003; Suchomski 1996), and double publications of excluded trials (N = 6) (Kovacs 1998; Liu 1996; Parikh 2002; Shah 2007; Suchomski 1996; Thorson 1992).
Two trials might have included participants within the inclusion criteria of this review (Cole 1999a; Rajamani 1998), however all attempts at contacting the original trialist to request subgroup data failed, therefore these trials were excluded.
Risk of bias in included studies
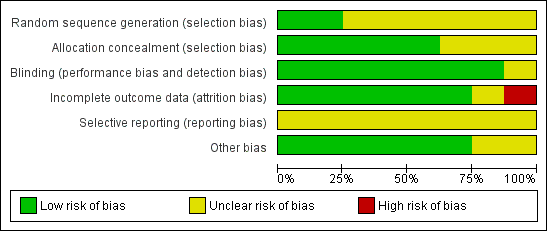
All of the included trials were randomised and double‐blinded with placebo controls. LaForce 1993, Arnon 1996, Giep 1996, and Jonsson 2000 provided us with additional information. The quality of the trials ranged from moderate to high, with some trials failing to provide sufficient details on the randomisation process, method of blinding, the management of withdrawals, and reporting bias (Figure 3; Figure 4).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
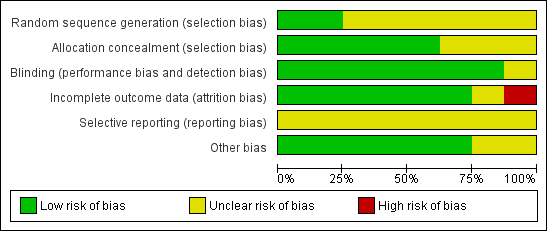
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Risk of bias in individual studies
Arnon 1996: The method of randomisation was not mentioned in the manuscript. Personal communication revealed that randomisation was performed by the pharmacy. The code and drugs were kept until the end of the trial and released from the hospital pharmacy in sealed envelopes. Blinding was established by using identical MDIs for corticosteroids and placebo administration. Ten infants were withdrawn and did not complete the study: five because of sepsis (three placebo, two treatment group), four because of PDA (two in each group), and one because of an air leak (treatment group). These infants were excluded from the analysis in the original manuscript but were included in this review. It was unclear whether the study was free of selective reporting.
Denjean 1998: The methods of allocation concealment or randomisation process were not mentioned in the manuscript, however accuracy was confirmed by personal communication. Randomisation by pre‐established tables was stratified by centre, gestational age, and type of ventilator support. The method of blinding was not clearly stated in the manuscript, but again we ensured it to be genuine by personal communication. Due to severe clinical deterioration, the code for three infants was broken. Furthermore, it was stated that of the 178 infants randomised, informed consent was either not obtained or withdrawn for five infants for unclear reasons. It was unclear whether the study was free of selective reporting.
Dugas 2005: The method of concealment was not mentioned in the manuscripts. Infants were assigned to the treatment or placebo arm by block randomisation with stratification of intubated and extubated infants. Blinding was ensured by identical MDIs supplied by the drug manufacturer. The pharmacist in charge of the medication, the treating physician, and the investigators were unaware of treatment allocation. Three infants in the placebo group did not complete the study protocol (two because of clinical pulmonary deterioration and one because of central line sepsis). All infants were analysed on an intention‐to‐treat basis. Mean supplemental oxygen at study enrolment differed between the treatment and placebo arms, being significantly lower in the treatment group. The predefined outcomes were reported accurately.
Giep 1996: The methods of allocation concealment or randomisation of the infants were not described in the manuscript. Observers were blinded to treatment allocation, however the method ensuring this was not reported. Three infants in the placebo group and two in the treatment group received systemic corticosteroids after study entry, and continuous data that were not of interest for this review were excluded from the analysis thereafter.
Jonsson 2000: Randomisation was computer generated, and sealed envelopes were consecutively numbered. Clinical staff were blinded to group assignment, and the code was broken after the last infant finished the treatment. Blinding of the intervention was ensured by supplying the study drug in identical opaque, unmarked plastic vials. Outcome assessments were also blinded. Two infants were withdrawn by attending clinician due to deterioration and received systemic corticosteroids, and one died on ninth day of life. Outcomes for all enrolled infants were provided. The predefined outcomes were reported accurately.
LaForce 1993: The attending neonatologist was unaware of the treatment regimen. However, the method of allocation concealment or blinding was unclear. Nine infants were withdrawn from the analysis due to technical problems with equipment (two in each group), lost to referring hospital (two in each group), and one because of sudden death before start of the study (in treatment group). These infants were not included in the analyses of the original manuscript but were used for the dichotomous outcomes during the study period in this review. It was unclear whether the study was free of selective reporting.
Pappagallo 1998: The manuscript revealed no information regarding the method of sequence generation, allocation concealment, or randomisation. Clinical staff were unaware of the intervention since the vials were prepared by the pharmacist, labelled with a code, and both the study and placebo medications were clear solutions and the dosage was calculated on the basis of volume. Outcomes were given for all infants enrolled.
Pokriefka 1993: The authors stated in the abstract that this was a double‐blind, randomised trial, but no information was available regarding the method of randomisation, blinding of intervention, or outcome assessments. Outcomes for all enrolled infants were provided.
Summarised risk of bias
Allocation
Allocation concealment was blinded in five trials (Arnon 1996; Denjean 1998; Dugas 2005; Jonsson 2000; LaForce 1993), and unclear in the remaining trials. However, adequate sequence generation was only clear in two trials (Denjean 1998; Jonsson 2000).
Blinding
Based on the reported data and personal communications, we judged all studies as having a double‐blind design. The double‐blind design was not clearly stated in the abstract of Pokriefka 1993.
Incomplete outcome data
Five trials reported the outcomes of all included infants (Dugas 2005; Giep 1996; Jonsson 2000; Pappagallo 1998; Pokriefka 1993), whereas in two trials infants were not included due to not obtaining informed consent or excluded for the outcomes (Arnon 1996; Denjean 1998), and in one trial this was unclear (LaForce 1993).
Selective reporting
Five trials reported the predefined outcome data completely. In three trials it was unclear whether all predefined outcome data had been reported (Arnon 1996; Denjean 1998; LaForce 1993). None of the studies published a study protocol.
Other potential sources of bias
With the exception of three trials (Arnon 1996; Giep 1996; Jonsson 2000), we could not exclude other potential sources of bias based on the available information.
Effects of interventions
Inhaled corticosteroids versus placebo, administered after the first week of life until 36 weeks PMA in preterm infants at high risk of developing BPD (Comparison 1)
Primary outcome
Combined outcome death or BPD at 36 weeks PMA:
Meta‐analysis of combined outcomes mortality and BPD at 36 weeks PMA did not show a significant difference between the treatment and placebo arms in either the ventilated or non‐ventilated subgroup (RR 1.10, 95% CI 0.74 to 1.63) (Analysis 1.1).
Secondary outcomes
Other respiratory outcomes
Meta‐analysis of separate outcomes death at 28 days PNA and at 36 weeks PMA, the seperate outcomes BPD at 28 days PNA and at 36 weeks PMA, as well as the combined outcome death or BPD at 28 days PNA did not show a significant difference between the treatment and placebo arms in either the ventilated or non‐ventilated subgroup.
Compared to the infants allocated to the placebo group, the infants treated with inhalation corticosteroids had a lower risk of failure to extubate at seven days (typical RR 0.80, 95% CI 0.66 to 0.98; NNTB 5, 95% CI 3 to 19; 5 studies, 79 infants) (Analysis 1.8) and at the latest reported time point after treatment onset (typical RR 0.60, 95% CI 0.45 to 0.80; NNTB 3, 95% CI 2 to 5; 6 studies, 90 infants) (Analysis 1.10), respectively. However, both analyses showed increased statistical heterogeneity (I2 statistic 73% and 86%, respectively).
Failure to extubate at 14 days showed no difference between the two groups (typical RR 0.36, 95% CI 0.10 to 1.33; 2 studies, 27 infants) (Analysis 1.9).
The meta‐analysis of the outcome duration of mechanical ventilation in the ventilated infants showed no significant statistical difference between the treatment arms. Meta‐analysis showed no significant difference between the treatment and placebo arms regarding duration of supplemental oxygen for the ventilated (MD 5.53, 95% CI ‐3.99 to 15.05) and non‐ventilated infants (MD ‐3.74, 95% CI ‐12.63 to 5.14) (Analysis 1.12).
Adverse effects during hospitalisation
Meta‐analysis showed that open‐label intravenous corticosteroids were used less often in ventilated infants treated with inhaled corticosteroids, but this difference only approached statistical significance (typical RR 0.51, 95% CI 0.26 to 1.00; 4 studies, 74 infants) (Analysis 1.13). Only one trial reported on the use of open‐label intravenous corticosteroids in non‐ventilated infants (Jonsson 2000), stating that this intervention was not used in any of the included infants.
Five trials reported either suspected, in Giep 1996, or documented sepsis rates (Arnon 1996; Dugas 2005; Jonsson 2000; LaForce 1993), and the meta‐analysis of these results failed to show a significant difference between the inhaled corticosteroids and placebo groups (typical RR 0.90, 95% CI 0.50 to 1.64; 5 studies, 107 infants) (Analysis 1.14). Subgroup analysis did not change this finding.
We were unable to perform meta‐analysis on the outcomes of PDA, hypertension, necrotising enterocolitis, intraventricular haemorrhage, and total days of hospitalisation because these outcomes were only reported in single trials. None of these trials reported a significant difference in these outcomes, except for total days of hospitalisation; Pappagallo 1998 showed a significant decrease in the total days of hospitalisation in favour of the inhaled corticosteroids group (MD ‐24.70, 95% CI ‐41.75 to ‐7.65) (Analysis 1.19). Two trials assessed the airway resistance and dynamic lung compliance, but we were unable to perform a meta‐analyses including both studies, because LaForce 1993 did not report the standard deviations or absolute numbers of the measurement. Compared to the placebo group, Pappagallo 1998 did show a significant decreased lung compliance in the patient group allocated to inhalation steroids (Analysis 1.21), but not in airway resistance. None of the studies reported the outcomes hyperglycaemia and long‐term neurodevelopmental sequelae, assessed between one‐year and four years of CGA, including cerebral palsy and Bayley Scales of infant Development.
Discussion
Summary of main results
Based on the predefined inclusion criteria, this systematic review identified eight relatively small RCTs comparing inhalation corticosteroids to placebo in a total of 232 ventilated and non‐ventilated preterm infants. These trials differed considerably in participant characteristics, intervention (medication, dose, duration, and delivery), reported outcomes, and the definitions of these outcomes. This heterogeneity and the small number of randomised infants should be taken into account when interpreting the results of this review.
As the aim of this review was to examine the use of inhalation corticosteroids to prevent BPD, we chose the endpoint of inclusion to exclude those trials investigating inhaled corticosteroids in preterms with established BPD after 36 weeks PMA. It is, to our knowledge, unknown how much time before the primary endpoint BPD the inhaled corticosteroids might be effective. It could be argued that therapy would need to be initiated two weeks before that endpoint, or even four weeks before, as there needs to be an exposure for some time to reduce inflammation. The only trial that could have theoretically included infants around the corrected gestation of 36 weeks PMA could not provide us with data on the primary outcome BPD at 36 weeks PMA (Dugas 2005). All of the other included trials treated infants for an average of eight weeks. Consequently, we feel that the inclusion criteria fulfilled the purpose of this review.
Meta‐analysis of reported and provided data showed that inhalation corticosteroids do not improve the separate or combined outcomes mortality or BPD at any time point during hospitalisation. In addition, there were no significant differences in the short‐term respiratory outcomes such as failure to extubate at 14 days, total days of mechanical ventilation, or days of supplemental oxygen. This is despite the fact that several studies reported that inhalation corticosteroids improved resistance and compliance of the respiratory system, sometimes resulting in a reduction in FiO2 or respiratory rate. However, the heterogeneity in how lung function was measured and the data were reported prevented a valid meta‐analysis of these outcomes (Arnon 1996; Giep 1996; LaForce 1993; Pappagallo 1998; Pokriefka 1993). This review showed a significant reduction in failure to extubate at day seven, and at the latest reported time point, but these analyses were seriously hampered by moderate to high statistical heterogeneity (I2 statistic 73% and 86%, respectively). No firm conclusions can therefore be drawn from these analyses. One possible explanation for this heterogeneity might be that the trials reporting these outcomes used different drugs and methods of delivery.
Our meta‐analysis did show a trend to a reduced use of systemic corticosteroids for the reduction of BPD in the inhaled corticosteroids group. In light of the growing concerns about the adverse effects of systemic corticosteroids, this might prove to be an important and clinically relevant finding. However, the lack of data on short‐ and long‐term adverse effects in most trials precludes any firm conclusions at this time.
Overall completeness and applicability of evidence
The overall completeness and applicability of this review are low for several reasons. First, most of the manuscripts identified by the search strategy had either an observational study design or were not placebo controlled, instead comparing systemic versus inhalation corticosteroids, and were therefore not eligible for inclusion. The numbers of participants within each of these included trials were small, which limits their power to detect small but clinically important effects of treatment. Second, most placebo‐controlled trials investigating inhalation corticosteroids differed considerably in terms of participant characteristics and study design, including differences in type of inhalation medication, dose, duration of therapy, and delivery systems. It is unknown if and how these factors modify the treatment effect of inhalation corticosteroids on the outcome parameters reported in this review since we were unable to perform sensitivity analysis to assess the potential impact of different drugs, dosages, delivery systems, and treatment duration on the magnitude of the expected benefit. Third, not all trials reported the primary and secondary outcome parameters. Various definitions were used, and outcomes were assessed at different time points. Our extended attempts to retrieve unpublished data did not change this shortcoming.
Quality of the evidence
Three out of the eight included studies did not report allocation concealment, and the majority of included studies did not report adequacy of allocation sequence (Figure 3). However, all but one included trial reported adequate blinding of the intervention, therefore we judged the quality of these RCTs as moderate to high. Nevertheless, the overall quality of the evidence provided by the meta‐analyses using the GRADE approach for each outcome was assessed as low to very low due to inconsistency, imprecision of the effect estimates, and risk of publication bias (summary of findings Table for the main comparison). The sample size of the reported outcomes was small, resulting in inadequate power to detect clinically relevant differences in all of the important outcomes. Even if all the trials were to have reported on the same outcomes, the meta‐analyses are at high risk of inconsistency due to the considerable diversity between the different trials in design, choice of drugs, dosage, and delivery systems.
Potential biases in the review process
Due to the lack of possible aggregation data reported in the eligible trials, we were unable to create funnel plots, therefore we cannot exclude the potential risk of publication bias.

Flow of inclusion of randomised controlled trials in different phases of search.

Study flow diagram: review update.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
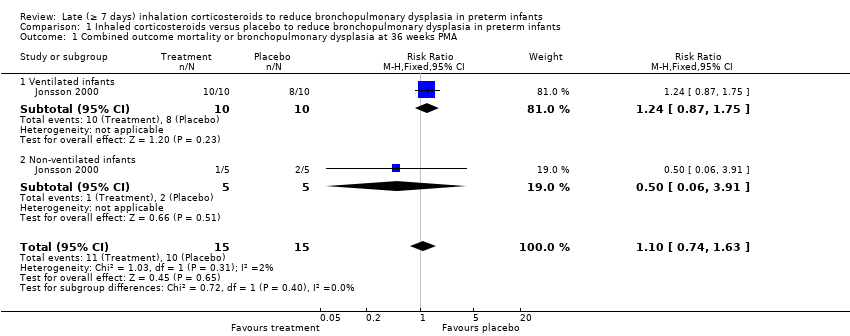
Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 1 Combined outcome mortality or bronchopulmonary dysplasia at 36 weeks PMA.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 2 Mortality at 28 days PNA.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 3 Mortality at 36 weeks PMA.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 4 Mortality at hospital discharge.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 5 Bronchopulmonary dysplasia at 28 days PNA.
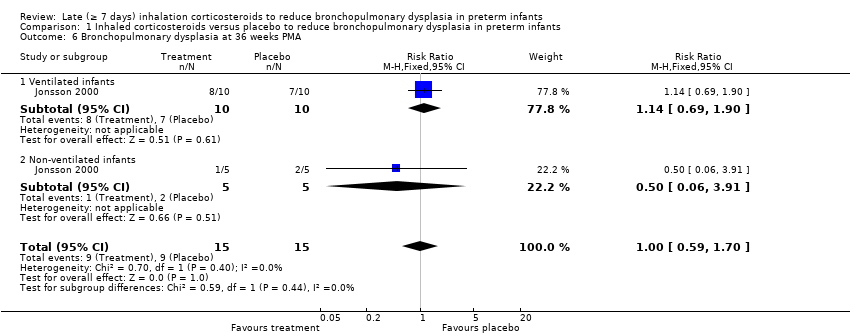
Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 6 Bronchopulmonary dysplasia at 36 weeks PMA.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 7 Combined outcome mortality and bronchopulmonary dysplasia at 28 days PNA.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 8 Failure to extubate day 7.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 9 Failure to extubate day 14.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 10 Failure to extubate at the latest reported moment.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 11 Days of mechanical ventilation.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 12 Days of supplemental oxygen.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 13 Open‐label intravenous corticosteroids.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 14 Sepsis (clinical suspected or culture proven).

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 15 Patent ductus arteriosus.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 16 Hypertension (> 2 SD).

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 17 Necrotising enterocolitis.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 18 Intraventricular haemorrhage (any grade).

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 19 Days of hospitalisation.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 20 Airway resistance.

Comparison 1 Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants, Outcome 21 Dynamic lung compliance.
| Inhaled corticosteroids versus placebo to reduce bronchopulmonary dysplasia in preterm infants | ||||||
| Patient or population: preterm infants | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with inhaled corticosteroids | |||||
| Combined outcome mortality or bronchopulmonary dysplasia at 36 weeks postmenstrual age | Study population | RR 1.10 | 30 | ⊕⊝⊝⊝ | ||
| 533 per 1000 | 587 per 1000 | |||||
| Mortality at 36 weeks postmenstrual age | Study population | RR 3.00 | 61 | ⊕⊕⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Bronchopulmonary dysplasia at 36 weeks postmenstrual age | Study population | RR 1.00 | 30 | ⊕⊝⊝⊝ | ||
| 600 per 1000 | 600 per 1000 | |||||
| Open‐label intravenous corticosteroids | Study population | RR 0.51 | 74 | ⊕⊝⊝⊝ | ||
| 432 per 1000 | 320 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Risk of bias: No serious limitations. No downgrade. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Combined outcome mortality or bronchopulmonary dysplasia at 36 weeks PMA Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.74, 1.63] |
| 1.1 Ventilated infants | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.87, 1.75] |
| 1.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.06, 3.91] |
| 2 Mortality at 28 days PNA Show forest plot | 2 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.14, 65.90] |
| 2.1 Ventilated infants | 2 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.14, 65.90] |
| 2.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Mortality at 36 weeks PMA Show forest plot | 3 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.78] |
| 3.1 Ventilated infants | 3 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.78] |
| 3.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Mortality at hospital discharge Show forest plot | 3 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.78] |
| 4.1 Ventilated infants | 3 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.78] |
| 4.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Bronchopulmonary dysplasia at 28 days PNA Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.72, 1.21] |
| 5.1 Ventilated infants | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.61, 1.29] |
| 5.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.71, 1.41] |
| 6 Bronchopulmonary dysplasia at 36 weeks PMA Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.59, 1.70] |
| 6.1 Ventilated infants | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.69, 1.90] |
| 6.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.06, 3.91] |
| 7 Combined outcome mortality and bronchopulmonary dysplasia at 28 days PNA Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.85, 1.18] |
| 7.1 Ventilated infants | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.83, 1.20] |
| 7.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.71, 1.41] |
| 8 Failure to extubate day 7 Show forest plot | 5 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.66, 0.98] |
| 9 Failure to extubate day 14 Show forest plot | 2 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.10, 1.33] |
| 10 Failure to extubate at the latest reported moment Show forest plot | 6 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.45, 0.80] |
| 11 Days of mechanical ventilation Show forest plot | 3 | 45 | Mean Difference (IV, Fixed, 95% CI) | 3.42 [‐1.30, 8.13] |
| 12 Days of supplemental oxygen Show forest plot | 4 | 141 | Mean Difference (IV, Fixed, 95% CI) | 0.57 [‐5.92, 7.07] |
| 12.1 Ventilated infants | 4 | 100 | Mean Difference (IV, Fixed, 95% CI) | 5.53 [‐3.99, 15.05] |
| 12.2 Non‐ventilated infants | 2 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐3.74 [‐12.63, 5.14] |
| 13 Open‐label intravenous corticosteroids Show forest plot | 4 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.26, 1.00] |
| 13.1 Ventilated infants | 4 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.26, 1.00] |
| 13.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Sepsis (clinical suspected or culture proven) Show forest plot | 5 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.50, 1.64] |
| 14.1 Ventilated infants | 5 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.44, 1.77] |
| 14.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.36, 2.75] |
| 15 Patent ductus arteriosus Show forest plot | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.16, 6.20] |
| 15.1 Ventilated infants | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.16, 6.20] |
| 16 Hypertension (> 2 SD) Show forest plot | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.1 Ventilated infants | 1 | 17 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Necrotising enterocolitis Show forest plot | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Ventilated infants | 1 | 17 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Non‐ventilated infants | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Intraventricular haemorrhage (any grade) Show forest plot | 1 | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.13, 2.82] |
| 18.1 Ventilated infants | 1 | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.13, 2.82] |
| 19 Days of hospitalisation Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐24.70 [‐41.75, ‐7.65] |
| 19.1 Ventilated infants | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐24.70 [‐41.75, ‐7.65] |
| 20 Airway resistance Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 21.40 [‐71.11, 113.91] |
| 21 Dynamic lung compliance Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.22 [‐0.33, ‐0.11] |

