مدیریت درمانی بیاختیاری مدفوع و یبوست در بزرگسالان مبتلا به بیماریهای عصبی مرکزی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised single‐blind trial | |
| Participants | Setting and country: Movement Disorders Clinic, USA Inclusion criteria: 7 Parkinson's disease patients Exclusion criteria: not mentioned Age: mean age 66 years, range 54‐80 Sex: 3 women, 4 men Other characteristics: reporting fewer than 3 stools during the final week of a 4‐week run‐in period. Duration of Parkinson's disease range 4‐14 years and mean duration of constipation was 9.4 years | |
| Interventions | Psyllium (5.1 g daily) versus placebo during an 8‐week period followed by a 4‐week washout period. Four patients received placebo and 3 psyllium | |
| Outcomes | Stool frequency and symptoms related to bowel function (stool consistency, straining effort, occurrence of anal pain, presence of a sensation of incomplete evacuation). Each symptom was scored on a visual analogue scale that ranged from 1 to 7. Total stool weight during the final week of each phase. Colon transit time and ano‐rectal manometry (basal anal sphincter pressure profile, the squeeze response, the recto‐anal inhibitory reflex, the threshold for rectal sensation) at entry, at the end of the 4th, 12th and 16th weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | no mention of method |
| Allocation concealment (selection bias) | Unclear risk | no mention of method |
| Blinding (performance bias and detection bias) | Unclear risk | no mention of blinding |
| Incomplete outcome data (attrition bias) | Low risk | all 7 completed and reported |
| Methods | Randomised controlled trial Intention‐to‐treat analysis: yes | |
| Participants | Setting and country: 5 spinal cord injury centres in European countries (Denmark, Italy, UK, Germany, Sweden) Inclusion criteria: 87 patients with spinal cord injury and neurogenic bowel dysfunction. SCI at any level; at least 3 months after injury and at least one of the following symptoms: 30 minutes + on bowel management; episodes of FI once or more per month; symptoms of autonomic dysreflexia before or during defecation; abdominal discomfort before or during defecation Exclusion criteria: coexiting major physical problems; using irrigation already; bowel obstruction or inflammatory bowel disease; cerebral palsy or stroke; multiple sclerosis; diabetic polyneuropathy; previous major abdominal or perineal surgery; pregnancy or lactation; spinal shock; mental instability; 5mg+ prednisolone; implant for sacral nerve stimulation Age: mean 47.5 years (transanal); 50.6 years (conservative) Sex: female 25; male 62 Other characteristics: details given of ASIA scores and functional level | |
| Interventions | 10 weeks of transanal irrigation (Peristeen, Coloplast, Denmark) using a specially designed system with a pump and self retaining balloon, used independently after training by a nurse, compared with conservative bowel management (best supportive bowel care using a guideline without using irrigation). Both each day or 2 days | |
| Outcomes | Primary endpoint: Cleveland Clinic constipation score and St Marks faecal incontinence Secondary outcomes: neurological bowel dysfunction score; modified American Society of Colorectal Surgeons FI score; bowel function; influence on daily activities; general satisfaction; impact on quality of life; urinary tract infection; time for bowel care | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer generated sequence: block randomisation by centre |
| Allocation concealment (selection bias) | Low risk | sealed numbered envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | not possible for participants but independent observer "who had not participated in the training" for outcomes |
| Incomplete outcome data (attrition bias) | Low risk | few missing data; "intention to treat analysis with baseline values carried forward for patients who did not complete" |
| Methods | Randomised controlled trial Intention‐to‐treat analysis: yes | |
| Participants | Setting and country: spinal cord injury centre in Stoke Mandeville, UK Inclusion criteria: 68 traumatic or non‐traumatic spinal cord injury. Any ASIA grade, discharged from rehabilitation one year or more Exclusion criteria: pregnancy, current or past bowel disease or major surgery, stoma Age: intervention 49.5 years (range 24‐73), control 47 years (range 27‐62) Sex: women 23, men 45 Other characteristics: flaccid bowel 9, reflex bowel 59 | |
| Interventions | Intervention: stepwise protocol of increasingly invasive evacuation methods (from massage to manual evacuation) Control: usual care in terms of type, number and order of interventions to achieve evacuation | |
| Outcomes | Primary: duration of bowel care and level of intervention required to complete evacuation Secondary: time to stool, level of intervention at which evacuation began, frequency of faecal incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer generated block randomisation for subjects to each block |
| Allocation concealment (selection bias) | Low risk | sealed opaque consecutively numbered envelopes, administered by someone not involved in study |
| Blinding (performance bias and detection bias) | Unclear risk | not possible to blind participants or care givers. No mention of outcome assessor blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | intention‐to‐treat analyses, 10 discontinued: 4 control, 6 intervention |
| Methods | Randomised trial | |
| Participants | Setting and country: Comprehensive Rehabilitation Institute, USA Inclusion criteria: 60 newly admitted SCI inpatients Exclusion criteria: patients re‐admitted or admitted 6 months after the SCI Age: mean 27.2, range 13 to 58 years Sex: 8 women, 52 men Other characteristics: mean duration of SCI 43.9 days | |
| Interventions | Patients randomly assigned to one of 3 bowel programmes: Longitudinal assessment of 6 periods were made: first week of admission, second week, week 3, week 6, week 9 and week of discharge | |
| Outcomes | Duration from stimulation until evacuation occurred Number of unsuccessful attempts at evacuation after stimulation (data from week 9 used) Number of unstimulated or accidental evacuations (faecal incontinence) (data from week 9 used) Staining test as oro‐anal transit indicator (carmine test) Global nursing evaluation of the bowel programme rated as "good to fair", "poor" and "questionable" | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | no description |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned, blinding of intervention not possible |
| Incomplete outcome data (attrition bias) | High risk | participants dropped from the study if they "did not have an optimal programme" (A: 7/20, B: 16/20 C: 11/20) |
| Methods | Randomised double‐blind crossover study Intention‐to‐treat analysis: not mentioned | |
| Participants | Setting and country: Canada, setting not specified Inclusion criteria: 15 wheelchair bound institutionalised adults, multiple sclerosis 7, cerebral palsy 4, spinal cord injury 2, brain injury 2 Exclusion criteria: Age: under 60 years of age Sex: not stated Other characteristics: 10 with dysphagia and 5 without dysphagia | |
| Interventions | 15g daily inulin‐fortified beverage versus standard modified starch‐thickened beverages for 3 weeks each | |
| Outcomes | Chart record of bowel frequency, enema administration, urine samples for calcium, sodium and potassium | |
| Notes | No washout period between crossover | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Low risk | double‐blind but no details given |
| Incomplete outcome data (attrition bias) | Unclear risk | blood results on 12/15; other results appear complete |
| Methods | Randomised crossover study Intention‐to‐treat analysis: no | |
| Participants | Setting and country: UK single long stay residential setting and 2 group homes Inclusion criteria: 32 profoundly disabled institutionalised adults with cerebral palsy or genetic conditions associated with abnormal muscle tone regular use of laxatives or enemas for at least 12 months Exclusion criteria: none stated Age: mean 42.25 years (massage); 43.53 years (laxatives) Sex: 14 men, 18 women Other characteristics: 71% non‐ambulant and totally physically dependent | |
| Interventions | Abdominal massage 5 times a week by physiotherapist or nurse for 20 minutes for 7 weeks versus usual laxative ± enema as a rescue for 7 weeks then crossover. All laxative medication was stopped for both groups for washout period | |
| Outcomes | 15 days baseline and 10 days after treatment used for assessment. Gastrointestional and segmental transit time; stool frequency; stool size and consistency; need for enemas; assessment of patient well‐being | |
| Notes | 7 day washout period between phases with no laxatives or massage | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Low risk | radiologists interpreting transit time were blinded |
| Incomplete outcome data (attrition bias) | Low risk | follow‐up for 30/32 |
| Methods | Randomised trial Intention‐to‐treat analysis: yes | |
| Participants | Setting and country: 3 stroke rehabilitation units and community in UK Inclusion criteria: 146 participants, 122 community and 24 stroke rehabilitation inpatients. Had a stroke between 1 month and 4 years previously. Patients screened by questionnaire to identify bowel dysfunction (constipation or faecal incontinence) according to pre‐set definitions Exclusion criteria: people reporting acute diarrhoea or colonic disease other than diverticular disease Age: intervention 72.2 ± 10.2 years; control 72.9 ± 9.6 years Sex: 59 women, 87 men Other characteristics: pre‐stroke self reported constipation and faecal incontinence were comparable to similarly aged populations | |
| Interventions | Intervention: one‐off assessment by a nurse leading to 1. targeted patient and carer education; 2. provision of a booklet; Control: routine care | |
| Outcomes | Primary outcome was bowel movements per week. Secondary outcomes were percentage of bowel movements graded as normal by patients and number of episodes of faecal incontinence all measured by postal prospective diary at 1, 3, 6 and 12 months. Other outcomes were bowel related symptoms, stool diary, visual analogue scores for severity rating, quality of life (bowel related and SF‐12) and self reported treatment and resource use | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | external process using computer generated numbers |
| Allocation concealment (selection bias) | Low risk | closed envelopes |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) | Unclear risk | 24% dropout at 6 months: 51/73 in usual care and 55/73 in intervention group |
| Methods | Randomised double‐blind controlled trial | |
| Participants | Setting and country: Physical Medicine and Rehabilitation Center, USA Inclusion criteria: 15 SCI inpatients; duration of SCI range from 3 months to 45 years. 3 months or longer since SCI, injury above T12, lack of anal sensation, lack of voluntary anal sphincter contraction, stable bowel program, absence of known gastrointestinal disease Exclusion criteria: not mentioned Age: age range 26 to 61 years Sex: not mentioned Other characteristics: subject history reviewed for consistency in bowel management | |
| Interventions | Comparison of two bowel programmes based on the use of different rectal stimulants: 1) hydrogenated vegetable oil‐based bisacodyl suppository (HVB) Randomised sequence for each of the six scheduled bowel care sessions | |
| Outcomes | Time to flatus, time to stool flow, defecation duration, total bowel care duration | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | reported as predetermined |
| Allocation concealment (selection bias) | Low risk | central pharmacy allocated |
| Blinding (performance bias and detection bias) | Low risk | reported as double‐blind |
| Incomplete outcome data (attrition bias) | Low risk | all 15 completed |
| Methods | Randomised controlled trial Intention‐to‐treat analysis: not stated | |
| Participants | Setting and country: outpatients and inpatients of a single hospital Inclusion criteria: 120 stroke patients, 90 patients in treatment group, 30 controls. Patients with a history of stroke evidenced by CT/MRI scan and constipation with bowel opening less frequently than every 72 hours and hard stool causing straining during defecation or difficulty in defecation Exclusion criteria: not stated Age: treatment group ‐ average 59 years ± 7 years, control group 60 years ± 9 years Sex: treatment group ‐ 41 male, 49 female, control group 13 male, 17 female Other characteristics: other Chinese medicine criteria also applied, other organic causes of constipation excluded | |
| Interventions | A (90): Quiong Runchang oral liquid ‐ a Chinese herbal medicine for intervention group B (30): Yichi Runchang ointment for controls. Treatment for 2 weeks | |
| Outcomes | Definitions: Cure ‐ normal stool consistency and frequency or a return to pre‐morbid level and all symptoms subsided. Good response ‐ significant improvement (near normal) in frequency of defecation and consistency of stool or slightly hard stool and frequency more than once in 72 hours and almost complete subsidence of symptoms of constipation. Partial response ‐ frequency of stool more than or equal to once a day or improvement in consistency of stool and improvement of symptoms of constipation. No response ‐ reaching none of the above | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomised 3:1 |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) | Unclear risk | intention‐to‐treat analysis, dropouts not mentioned |
| Methods | Randomised controlled trial Intention‐to‐treat analysis: not stated | |
| Participants | Setting and country: one centre, Korea Inclusion criteria: 31 stroke patients Rome II criteria for constipation. 21 more than one year after stroke Exclusion criteria: Age: median 63 years Sex: 13 men, 18 women Other characteristics: also used a constipation assessment for participant selection | |
| Interventions | Abdominal meridian massage versus no massage | |
| Outcomes | Frequency of defecation, constipation assessment scale | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) | Unclear risk | not mentioned |
| Methods | Randomised crossover design Intention‐to‐treat analysis: data on all 8 participants | |
| Participants | Setting and country: USA Inclusion criteria: 8 spinal cord injured patients, 6 tetraplegic, mean duration of injury 13 years (range 2 ‐33), fewer than 2 bowel motions per week all with stable bowel regimes Exclusion criteria: Age: average 48 ± 14 years Sex: all men Other characteristics: none stated | |
| Interventions | Abdominal belt with embedded electrodes applied at level of umbilicus used during bowel care, randomly activated or not activated, during 6 sessions of bowel care over 2 weeks | |
| Outcomes | Time to first stool, time for total bowel care | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | no mention |
| Allocation concealment (selection bias) | Unclear risk | no mention |
| Blinding (performance bias and detection bias) | Low risk | participants were blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | data on all 8 participants |
| Methods | Randomised crossover blinded study Intention‐to‐treat analysis: all subjects completed | |
| Participants | Setting and country: Veterans centre USA Inclusion criteria: 13 spinal cord injury patients, 5 quadriplegics Exclusion criteria: cardiac or renal disease Age: mean 46, range 25‐69 years Sex: not mentioned Other characteristics: mean duration of injury 14 years, range 1‐31; bowel care required 1‐2 hours at the time of the study | |
| Interventions | Intavenous infusion of neostigmine 2mg versus 2mg neostigmine plus 0.4mg glycopyrrolate versus normal saline | |
| Outcomes | Amount of a 200ml barium oatmeal paste evacuated from rectum seen radiographically 30 minutes after infusion (blinded assessor, graded 0‐4), blood pressure and pulse rate, total and central airway resistances | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Unclear risk | subjects blinded as to which infusion receiving |
| Incomplete outcome data (attrition bias) | Low risk | all subjects completed |
| Methods | Double‐blind placebo‐controlled, pilot, phase II, dose escalation study Intention‐to‐treat analysis: no | |
| Participants | Setting and country: two Danish centres. Inclusion criteria: 23 randomised ‐ 7 received placebo, 8 prucalopride 1 mg and 8 prucalopride 2 mg. SCI, more than 6 months since spinal cord injury; history of constipation subsequent to injury defined as 2 or fewer spontaneous bowel movements per week or needing manual assistance with evacuation in more than 50% of bowel movements per week Exclusion criteria: cauda equina lesions, drug induced constipation, organic causes of constipation, impaired renal function Age: 18‐60 years Sex: 5 women, 16 men Other characteristics: if participants reported constipation pre‐spinal cord injury, developed constipation aged >50 years or had macroscopic blood in their faeces underwent colonoscopy | |
| Interventions | Study consisted of 2 sessions each preceded by a 4 week run‐in period when patients' own bowel care recorded. For 1 group this was followed by random allocation to placebo or prucalopride 1 mg for 4 weeks. When safety of this dose established another group was randomised to placebo or prucalopride 2 mg for 4 weeks | |
| Outcomes | Bowel diary including time of evacuation, use of anal stimulation, stool evacuated or not, stool consistency, use of digital evacuation, time taken for evacuation, presence of faecal impaction. Patient‐based outcomes were changes in frequency and consistency of bowel evacuation, abdominal pain and distention, incontinence, laxative use, time to first bowel movement, time taken for defecation. Investigator outcomes were global assessment of treatment efficacy on a 5 point Likert scale and total colonic transit time | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Low risk | double‐blind |
| Incomplete outcome data (attrition bias) | Low risk | 7/8 completed 2mg intervention, all others completed |
| Methods | Randomised study Intention‐to‐treat analysis: no | |
| Participants | Setting and country: multicentre, UK Inclusion criteria: 30 people with confirmed multiple sclerosis, recruited via newsletter, websites, MS groups and day centres, Rome 11 criteria for constipation Exclusion criteria: history of bowel disease Age: mean 55 years (SD 13, range 34‐83) Sex: 18 women, 12 men Other characteristics: EDSS score 2.5‐6; 10% could walk unaided, 40% wheelchair bound | |
| Interventions | Abdominal massage daily by participant or carer (with supporting DVD) + lifestyle advice versus lifestyle advice alone. 4 weeks intervention period. Both groups received a weekly visit from a physiotherapist | |
| Outcomes | Measured before intervention and at 4 weeks and 8 weeks after end of intervention Primary: constipation score Secondary: Neurogenic Bowel Dysfunction score, MS impact score; Qualiveen questionnaire for bladder function, 7 day bowel diary | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | web‐based system |
| Allocation concealment (selection bias) | Low risk | web‐based system |
| Blinding (performance bias and detection bias) | Low risk | research assistant analysed data and was blinded |
| Incomplete outcome data (attrition bias) | Low risk | incomplete data on one control patient at 8 weeks |
| Methods | Double‐blind placebo‐controlled pilot phase 2 study Intention‐to‐treat analysis: no | |
| Participants | Setting and country: Belgium, site/s not specified Inclusion criteria: 11 patients with multiple sclerosis Exclusion criteria: not mentioned Age: not mentioned Sex: not mentioned Other characteristics: none stated | |
| Interventions | 4 week run‐in. Prucalopride 1 mg for 4 weeks then 2mg for 4 weeks before breakfast, versus placebo | |
| Outcomes | Stool frequency, number of spontaneous bowel motions per week, median time to first bowel movement after first treatment, unproductive toilet trips, patient evaluation of constipation severity visual analogue score, side effects | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | no mention |
| Allocation concealment (selection bias) | Unclear risk | no mention |
| Blinding (performance bias and detection bias) | Unclear risk | states double‐blind but no detail |
| Incomplete outcome data (attrition bias) | Unclear risk | not mentioned |
| Methods | Randomised controlled double‐blind study Intention‐to‐treat analysis: not clear, 6 dropouts | |
| Participants | Setting and country: one centre in Korea Inclusion criteria: 34 bedridden constipated older people following a stroke Exclusion criteria: none stated Age: treatment group 67.0 ± 6.0 years, controls 66.7 ± 5.4 years Sex: male 24, female 10 Other characteristics: none stated | |
| Interventions | Oral carbonated water versus oral tap water for two weeks | |
| Outcomes | Laxative use, frequency of defecation and constipation symptoms | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | random allocation |
| Blinding (performance bias and detection bias) | Unclear risk | double‐blind |
| Incomplete outcome data (attrition bias) | Unclear risk | 6 dropouts |
| Methods | Randomised crossover study Intention‐to‐treat analysis: all 7 participants reported | |
| Participants | Setting and country: USA, sites not specified Inclusion criteria: 7 spinal cord injured patients with documented defecation problems; mean duration of injury 15.9 years range 3‐27, 4 cervical, 3 thoracic Exclusion criteria: contraindications to neostigmine Age: mean age 47 years, range 30‐56 Sex: not mentioned Other characteristics: 5 Afro‐American, 2 Hispanic | |
| Interventions | 2mg neostigmine and 0.4 mg glycopyrrolate intramuscularly for 1 week, 1 week washout, 1 week placebo, in random order plus usual bowel care. Fleet enema administered after 60 minutes if no evacuation | |
| Outcomes | Time from injection to completion of bowel care, time to first flatus, time to beginning of bowel movement, time to end of bowel movement, total time for bowel movement including clean up, side effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Low risk | order determined by sealed random assignment |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | outcomes for all 7 participants reported |
| Methods | Randomised double‐blind controlled trial | |
| Participants | Setting and country: Hospital Rehabilitation Unit, USA Inclusion criteria: 58 stroke patients entered the trial. 46 patients were analysed Exclusion criteria: not mentioned Age:mean age 72 years, range 36 to 90 Sex: not mentioned Other characteristics: all participants were actively rehabilitating, were given a diet gradually increasing in fibre and encouraged to maintain a high fluid intake | |
| Interventions | Comparison of 4 suppository‐based bowel programmes during study period (1 month): (1) mandatory morning suppository (2) optional morning suppository (3) mandatory evening suppository (4) optional evening suppository | |
| Outcomes | Number of subjects with effective bowel programme defined as a bowel movement within the scheduled time for 5 consecutive days. Efficiency rating determined by the number of days needed to achieve effectiveness. Score starts at 16 and dropped by 1 for each 2 additional days required to establish effectiveness | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) | Unclear risk | 46/58 were analysed: not clear which group |
| Methods | Randomised controlled trial Intention‐to‐treat analysis: not mentioned | |
| Participants | Setting and country: China, site/s not specified Inclusion criteria: 80 patients with stroke Exclusion criteria: Age: not mentioned Sex: not mentioned Other characteristics: none stated | |
| Interventions | Abdominal electroacupuncture 30 minutes daily for 2 seven day courses (40 patients) versus 10mg oral cisapride three times a day for two 7 day courses (40 patients) | |
| Outcomes | Cumulative scores of symptoms, total effective rate (definition unclear) | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | random allocation |
| Allocation concealment (selection bias) | Unclear risk | method not described |
| Blinding (performance bias and detection bias) | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) | Unclear risk | not mentioned |
| Methods | Randomised placebo‐controlled trial Intention to treat analysis: no | |
| Participants | Setting and country: two Italian centres Inclusion criteria: 57 Parkinson's disease patients, with constipation on Rome ii criteria Exclusion criteria: pregnant or not using effective contraception, use of drugs affecting gastrointestinal motility, previous gastrointestinal surgery, other causes of constipation Age: mean age 71 years SD ± 6.5 years Sex: 34 male, 23 female Other characteristics: mean disease duration 6.4 years | |
| Interventions | Laxative free baseline followed by 8 weeks isosmotic macrogol electrolyte solution (7.3g in water) versus placebo (flavoured maltodextrine) both dissolved in 250ml water twice daily. Dose could be varied between 1 and 3 sachets daily depending on stool form, patients were asked to keep diet and fluid intake unchanged | |
| Outcomes | Predominant symptom, other symptoms, stool frequency (number of evacuations per week), straining (visual analogue scale), stool consistency (4 point scale), use of rectal laxative as a rescue, diary cards, unused sachets of medication | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) | Low risk | participants were blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | 9 out of 29 withdrew from intervention group compared with 5 out of 28 from placebo |
SCI: spinal cord injury
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Non‐randomised trial | |
| Non‐randomised trial | |
| Intervention drug withdrawn from market | |
| Randomised single blind therapy | |
| Non‐randomised trial | |
| Non‐randomised trial | |
| Non‐neurogenic population | |
| Only 4 out of 27 individuals randomised to the intervention had central neurological conditions and it was not possible to identify their contribution to the data | |
| Stroke patients without identified bowel dysfunction at recruitment and no bowel‐specific outcome measure, post hoc analysis | |
| Non‐randomised trial with non‐neurological patients | |
| Intervention drug withdrawn from market | |
| Non‐randomised trial | |
| Stroke patients without identified bowel dysfunction at baseline and no bowel specific outcome measures | |
| Non‐randomised trial | |
| Non‐randomised trial | |
| Intervention drug withdrawn from the market | |
| Non‐neurogenic population | |
| Continent and incontinent patients not reported separately. No primary bowel outcome measures reported | |
| Only 2 out of 8 patients with faecal incontinence were neurological (SCI and MS) | |
| Efficacy of biofeedback for faecal incontinence in 12 children with myelomeningocele. Three of eight patients in the biofeedback group and three of the four given conventional treatment alone reported greater than or equal to 75% improvement in frequency of soiling 1 year later. Biofeedback did not improve anal squeeze and rectal sensation | |
| Non‐neurogenic population | |
| Randomised controlled trial in children | |
| Non‐randomised trial | |
| Not a specific intervention for bowel function, with no result for bowel function alone (EDSS rates bladder and bowel together) | |
| Intervention drug withdrawn from the market | |
| Non‐neurogenic population | |
| Non‐neurogenic population | |
| Randomised comparison of a hydrogenated vegetable oil‐based bisacodyl (HVB) suppository with polyethylene glycol‐based bisacodyl suppositories (PGB) in a single SCI subject. The average total bowel care time was significantly shorter with PGB | |
| Non‐randomised trial | |
| Intervention drug withdrawn from the market | |
| Stroke patients without identified bowel problems at baseline and no bowel‐specific outcome measures | |
| Children | |
| Functional bowel disorders not neurogenic |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of bowel motions or successful bowel care routine per week Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Active treatment versus no treatment or placebo, Outcome 1 Number of bowel motions or successful bowel care routine per week. | ||||
| 1.1 diet / fibre vs usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 massage versus usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 laxative versus placebo | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Colonic transit time (hours) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2 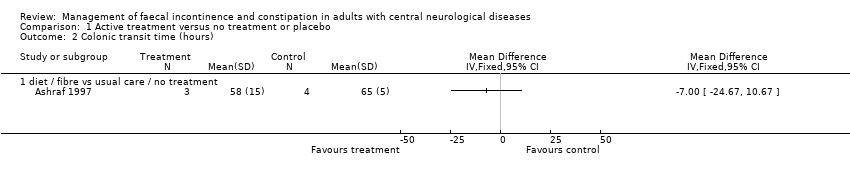 Comparison 1 Active treatment versus no treatment or placebo, Outcome 2 Colonic transit time (hours). | ||||
| 2.1 diet / fibre vs usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Stool weight (g) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3 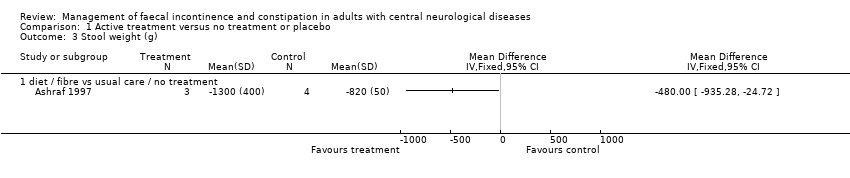 Comparison 1 Active treatment versus no treatment or placebo, Outcome 3 Stool weight (g). | ||||
| 3.1 diet / fibre vs usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Numbers NOT responding to treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 Active treatment versus no treatment or placebo, Outcome 4 Numbers NOT responding to treatment. | ||||
| 4.1 laxative versus placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 total bowel care time Show forest plot | 2 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5 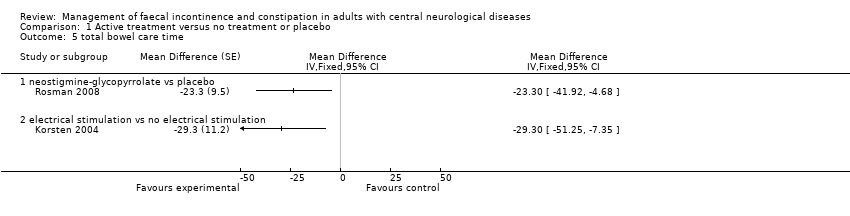 Comparison 1 Active treatment versus no treatment or placebo, Outcome 5 total bowel care time. | ||||
| 5.1 neostigmine‐glycopyrrolate vs placebo | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 electrical stimulation vs no electrical stimulation | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of bowel motions or successful bowel care routines per week Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 One treatment versus another treatment, Outcome 1 Number of bowel motions or successful bowel care routines per week. | ||||
| 1.1 assessment and education versus usual care | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 carbonated water versus tap water | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of people with no evacuation after stimulation (poor response) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2 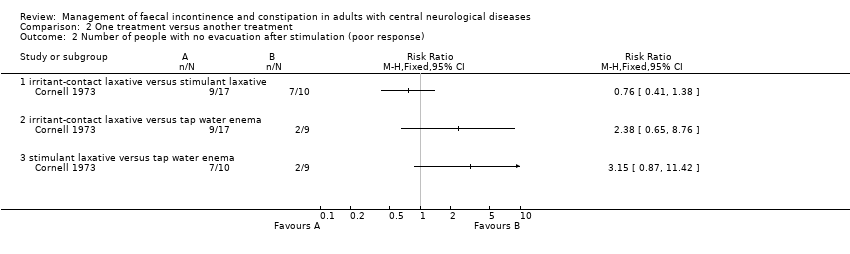 Comparison 2 One treatment versus another treatment, Outcome 2 Number of people with no evacuation after stimulation (poor response). | ||||
| 2.1 irritant‐contact laxative versus stimulant laxative | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 irritant‐contact laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 stimulant laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Constipation score (various) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3 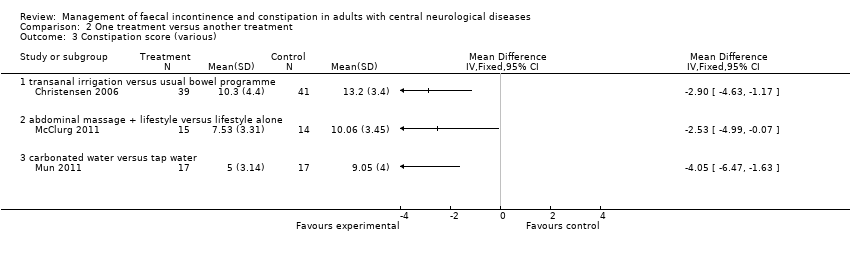 Comparison 2 One treatment versus another treatment, Outcome 3 Constipation score (various). | ||||
| 3.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 abdominal massage + lifestyle versus lifestyle alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 carbonated water versus tap water | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Neurogenic bowel dysfunction score Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 One treatment versus another treatment, Outcome 4 Neurogenic bowel dysfunction score. | ||||
| 4.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 abdominal massage + lifestyle versus lifestyle alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction with bowel care Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.5  Comparison 2 One treatment versus another treatment, Outcome 5 Satisfaction with bowel care. | ||||
| 5.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Number of people with faecal incontinence Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.6 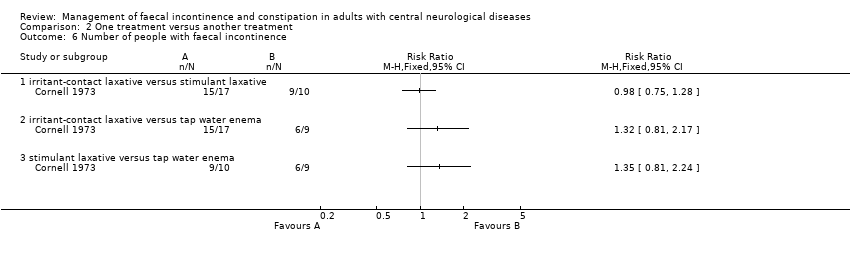 Comparison 2 One treatment versus another treatment, Outcome 6 Number of people with faecal incontinence. | ||||
| 6.1 irritant‐contact laxative versus stimulant laxative | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 irritant‐contact laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 stimulant laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Faecal incontinence score Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.7  Comparison 2 One treatment versus another treatment, Outcome 7 Faecal incontinence score. | ||||
| 7.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Total time for bowel care Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.8  Comparison 2 One treatment versus another treatment, Outcome 8 Total time for bowel care. | ||||
| 8.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Number of incontinence episodes between bowel cares, per day or per w Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.9 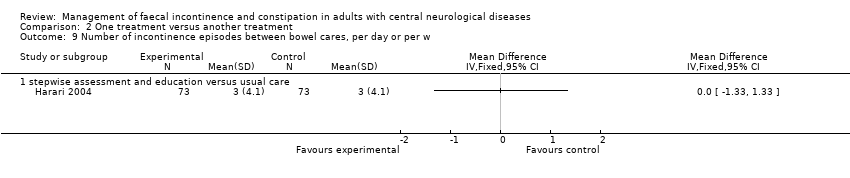 Comparison 2 One treatment versus another treatment, Outcome 9 Number of incontinence episodes between bowel cares, per day or per w. | ||||
| 9.1 stepwise assessment and education versus usual care | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

PRISMA study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
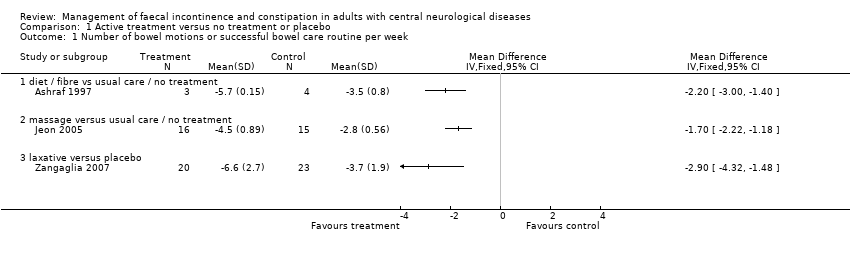
Comparison 1 Active treatment versus no treatment or placebo, Outcome 1 Number of bowel motions or successful bowel care routine per week.
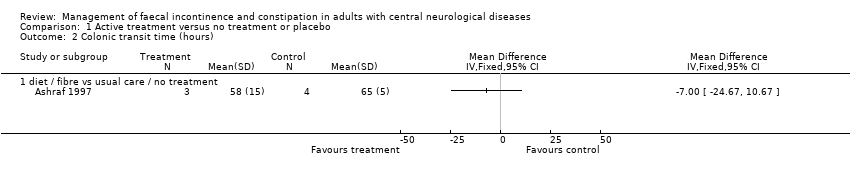
Comparison 1 Active treatment versus no treatment or placebo, Outcome 2 Colonic transit time (hours).
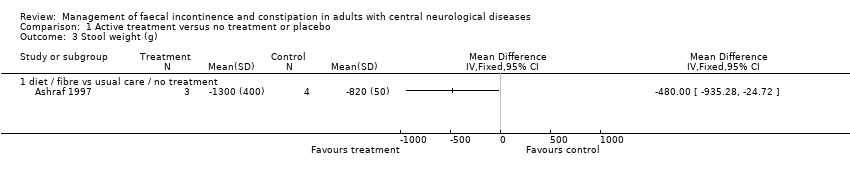
Comparison 1 Active treatment versus no treatment or placebo, Outcome 3 Stool weight (g).

Comparison 1 Active treatment versus no treatment or placebo, Outcome 4 Numbers NOT responding to treatment.
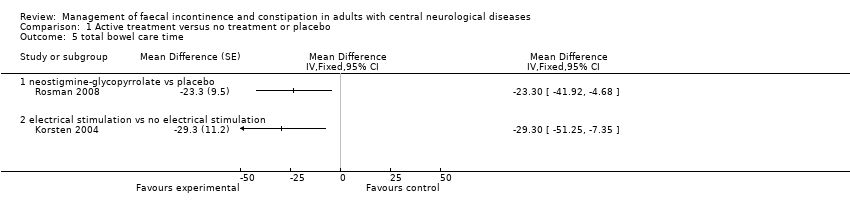
Comparison 1 Active treatment versus no treatment or placebo, Outcome 5 total bowel care time.
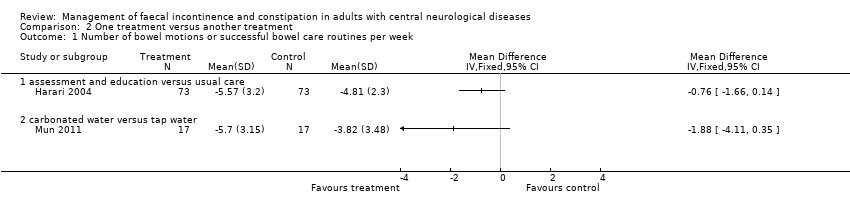
Comparison 2 One treatment versus another treatment, Outcome 1 Number of bowel motions or successful bowel care routines per week.

Comparison 2 One treatment versus another treatment, Outcome 2 Number of people with no evacuation after stimulation (poor response).
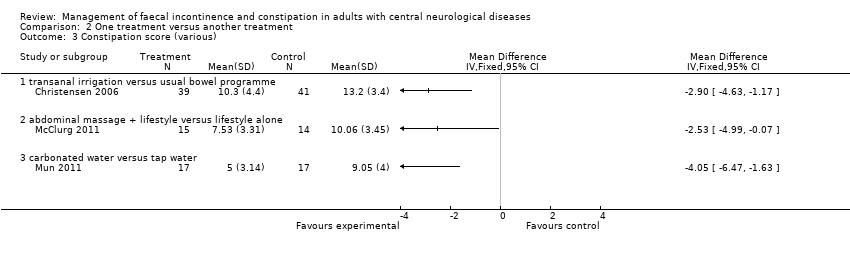
Comparison 2 One treatment versus another treatment, Outcome 3 Constipation score (various).

Comparison 2 One treatment versus another treatment, Outcome 4 Neurogenic bowel dysfunction score.

Comparison 2 One treatment versus another treatment, Outcome 5 Satisfaction with bowel care.
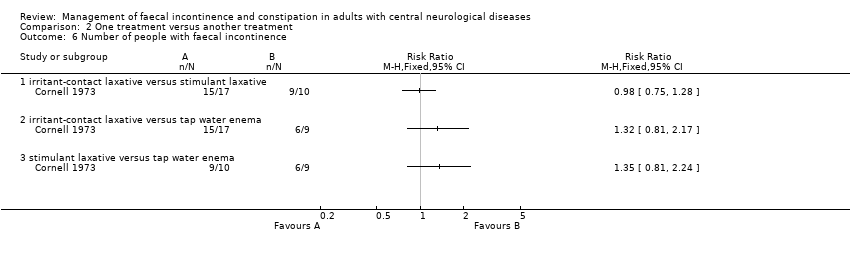
Comparison 2 One treatment versus another treatment, Outcome 6 Number of people with faecal incontinence.

Comparison 2 One treatment versus another treatment, Outcome 7 Faecal incontinence score.

Comparison 2 One treatment versus another treatment, Outcome 8 Total time for bowel care.
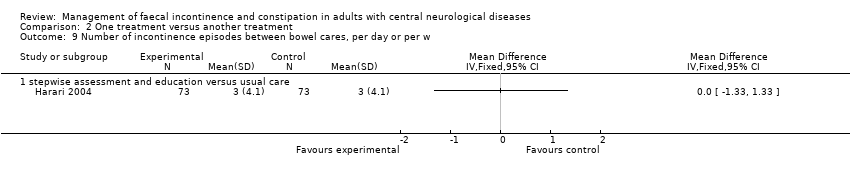
Comparison 2 One treatment versus another treatment, Outcome 9 Number of incontinence episodes between bowel cares, per day or per w.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of bowel motions or successful bowel care routine per week Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 diet / fibre vs usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 massage versus usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 laxative versus placebo | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Colonic transit time (hours) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 diet / fibre vs usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Stool weight (g) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 diet / fibre vs usual care / no treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Numbers NOT responding to treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 laxative versus placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 total bowel care time Show forest plot | 2 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5.1 neostigmine‐glycopyrrolate vs placebo | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 electrical stimulation vs no electrical stimulation | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of bowel motions or successful bowel care routines per week Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 assessment and education versus usual care | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 carbonated water versus tap water | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of people with no evacuation after stimulation (poor response) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 irritant‐contact laxative versus stimulant laxative | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 irritant‐contact laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 stimulant laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Constipation score (various) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 abdominal massage + lifestyle versus lifestyle alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 carbonated water versus tap water | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Neurogenic bowel dysfunction score Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 abdominal massage + lifestyle versus lifestyle alone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction with bowel care Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Number of people with faecal incontinence Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 irritant‐contact laxative versus stimulant laxative | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 irritant‐contact laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 stimulant laxative versus tap water enema | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Faecal incontinence score Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Total time for bowel care Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 transanal irrigation versus usual bowel programme | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Number of incontinence episodes between bowel cares, per day or per w Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 stepwise assessment and education versus usual care | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

