Раннее назначение ингаляционных кортикостероидов для профилактики хронического заболевания легких у недоношенных новорожденных с очень низкой массой тела при рождении
Abstract
Background
Chronic lung disease (CLD) remains a common complication among preterm infants. There is increasing evidence that inflammation plays an important role in the pathogenesis of CLD. Due to their strong anti‐inflammatory properties, corticosteroids are an attractive intervention strategy. However, there are growing concerns regarding short‐ and long‐term effects of systemic corticosteroids. Theoretically, administration of inhaled corticosteroids may allow for beneficial effects on the pulmonary system with a lower risk of undesirable systemic side effects.
Objectives
To determine the impact of inhaled corticosteroids administered to preterm infants with birth weight up to 1500 grams (VLBW) beginning in the first two weeks after birth for the prevention of CLD as reflected by the requirement for supplemental oxygen at 36 weeks' postmenstrual age (PMA).
Search methods
Randomised and quasi‐randomised trials were identified by searching the Cochrane Central Register of Controlled Trials (CENTRAL; 2015, Issue 12) in the Cochrane Library (searched 5 January 2016), MEDLINE (1966 to 5 January 2016), Embase (1980 to 5 January 2016), CINAHL (1982 to 5 January 2016), reference lists of published trials and abstracts published in Pediatric Research or electronically on the Pediatric Academic Societies web‐site (1990 to May 2016).
Selection criteria
We included in this review randomised controlled trials of inhaled corticosteroid therapy initiated within the first two weeks of life in VLBW preterm infants.
Data collection and analysis
We evaluated data regarding clinical outcomes, including: CLD at 28 days or 36 weeks' PMA; mortality; combined outcome of death or CLD at 28 days of age and at 36 weeks' PMA; the need for systemic corticosteroids; failure to extubate within 14 days; and adverse effects of corticosteroids. All data were analysed using Review Manager (RevMan) 5. Meta‐analyses were performed using relative risk (RR) and risk difference (RD), along with their 95% confidence intervals (CI). If RD was significant, the number needed to treat for an additional beneficial outcome (NNTB) was calculated. We used the GRADE approach to assess the quality of evidence.
Main results
According to GRADE the quality of the studies was moderate. Three additional trials are included in this update. The present review includes data analyses based on 10 qualifying trials that enrolled 1644 neonates. There was no significant difference in the incidence of CLD at 36 weeks' PMA in the inhaled steroid versus the placebo group (5 trials, 429 neonates) among all randomised (typical RR 0.97, 95% CI 0.62 to 1.52; typical RD −0.00, 95% CI −0.07 to 0.06). There was no heterogeneity for this outcome (typical RR I² = 11%; typical RD I² = 0%). There was a significant reduction in the incidence of CLD at 36 weeks' PMA among survivors (6 trials, 1088 neonates) (typical RR 0.76, 95% CI 0.63 to 0.93; typical RD −0.07, 95% CI −0.13 to −0.02; NNTB 14, 95% CI 8 to 50). There was a significant reduction in the combined outcome of death or CLD at 36 weeks' PMA among all randomised neonates (6 trials, 1285 neonates) (typical RR 0.86, 95% CI 0.75 to 0.99; typical RD −0.06, 95% CI −0.11 to −0.00) (P = 0.04); NNTB 17, 95% CI 9 to infinity). There was no significant heterogeneity for any of these analyses (I² = 0%). A lower rate of reintubation was noted in the inhaled steroid group compared with the control group in one study. There were no statistically significant differences in short‐term complications between groups and no differences in adverse events at long‐term follow‐up reported. Long‐term follow‐up of infants enrolled in the study by Bassler 2015 is ongoing.
Authors' conclusions
Based on this updated review, there is increasing evidence from the trials reviewed that early administration of inhaled steroids to VLBW neonates is effective in reducing the incidence of death or CLD at 36 weeks' PMA among either all randomised infants or among survivors. Even though there is statistical significance, the clinical relevance is of question as the upper CI limit for the outcome of death or CLD at 36 weeks' PMA is infinity. The long‐term follow‐up results of the Bassler 2015 study may affect the conclusions of this review. Further studies are needed to identify the risk/benefit ratio of different delivery techniques and dosing schedules for the administration of these medications. Studies need to address both the short‐ and long‐term benefits and adverse effects of inhaled steroids with particular attention to neurodevelopmental outcome.
PICO
Резюме на простом языке
Раннее назначение ингаляционных кортикостероидов для профилактики хронического заболевания легких у недоношенных новорожденных с очень низкой массой тела при рождении
Вопрос обзора
Предотвращают ингаляционные кортикостероиды, назначенные недоношенным новорожденным с массой тела при рождении до 1500 грамм в первые две недели после рождения, хроническое заболевание легких, которое отражается потребностью в дополнительном введении кислорода в 36 недель постменструального (постконцептуального) возраста?
Актуальность
У недоношенных детей, нуждающихся в респираторной поддержке, часто развивается хроническое заболевание легких. Считается, что воспаление в легких может быть одной из причин (частью причины). Препараты кортикостероидов при пероральном или внутривенном введении уменьшают это воспаление. Однако, применение кортикостероидов ассоциируется с развитием серьезных побочных эффектов, включая церебральный паралич (проблемы с движением) и задержку развития. Возможно, что вдыхание стероидов (ингаляции), когда лекарственное средство непосредственно попадает в легкие, может уменьшить неблагоприятные эффекты. В этом обзоре рассмотрели клинические испытания, в которых сравнивали недоношенных новорожденных, получавших стероиды или плацебо (неактивное лекарство) путем ингаляции (вдыхания) и в то же время получавших респираторную поддержку. До этого не было никаких доказательств, что раннее введение ингаляционных стероидов уменьшает риск развития хронического заболевания легких.
Характеристика исследований
В результате поиска литературы, обновленного к 5 января 2016 года, были включены 10 рандомизированных контролируемых испытаний, включавших 1644 младенцев.
Источники финансирования исследований
Мы не осведомлены о какой‐либо финансовой поддержке включенных исследований со стороны индустрии.
Основные результаты
В этом обновленном обзоре не выявлено значимого снижения частоты развития хронического заболевания легких в 36 недель постменструального (постконцептуального) возраста. Отмечалось значимое сокращение комбинированного исхода смерти или хронического заболевания легких в 36 недель постменструального возраста среди всех рандомизированных новорожденных и всех выживших. Несмотря на то, что результаты были значимыми, верхняя граница доверительного интервала была бесконечной (то есть мы должны были бы пролечить каждого ребенка ингаляционными стероидами, чтобы предотвратить 1 случай смерти ребенка или развития хронического заболевания легких в 36 недель постменструального возрасте). Это было бы не приемлемо в клинической практике. В одном крупном исследовании отмечалась более низкая частота повторной интубации (необходимость введения трубки в дыхательные пути) в группе, получавшей стероиды, по сравнению с контрольной группой. Не выявлено статистически значимых различий в в краткосрочных и долгосрочных осложнениях между группами. Ожидаются результаты одного крупного исследования с долгосрочным периодом наблюдения.
Качество доказательств
В целом качество исследований было хорошим.
Authors' conclusions
Summary of findings
| Early inhaled steroids (< 2 weeks) compared to placebo (among all randomised) for preventing chronic lung disease in very low birth weight preterm neonates | ||||||
| Patient or population: very low birth weight preterm neonates | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo (among all randomised) | Early inhaled steroids (< 2 weeks) | |||||
| CLD at 36 weeks' PMA | Study population | RR 0.97 | 429 | ⊕⊕⊕⊝ | ||
| 152 per 1000 | 148 per 1000 | |||||
| Moderate | ||||||
| 115 per 1000 | 112 per 1000 | |||||
| Death by, or CLD at, 36 weeks' PMA | Study population | RR 0.86 | 1285 | ⊕⊕⊕⊝ | ||
| 403 per 1000 | 346 per 1000 | |||||
| Moderate | ||||||
| 350 per 1000 | 301 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Method of sequence generation was unclear in all included studies except for the study by Bassler 2015. In the studies by Fok 1999, Jangaard 2002, Merz 1999 and Yong 1999 blinding of outcome assessment was unclear. Except for the study by Bassler 2015, none of the included studies were registered and we were unable to identify whether there was selective reporting or not. | ||||||
| Early inhaled steroid (< 2 weeks) compared to placebo (among survivors) for preventing chronic lung disease in very low birth weight preterm neonates | ||||||
| Patient or population: Very low birth weight preterm neonates | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo (among survivors) | Early inhaled steroid (< 2 weeks) | |||||
| CLD at 36 weeks' PMA | Study population | RR 0.76 | 1088 | ⊕⊕⊕⊝ | ||
| 314 per 1000 | 239 per 1000 | |||||
| Moderate | ||||||
| 188 per 1000 | 143 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
Background
Description of the condition
Chronic lung disease (CLD) remains a common complication among survivors of neonatal intensive care. Despite the use of antenatal corticosteroids and postnatal surfactant treatment, the incidence of CLD has increased. This is partly explained by increased survival of extremely low birth weight infants (Shaw 1993), in that the incidence of CLD has an inverse relationship with birth weight and gestational age (Sinkin 1990).
O'Brodovich and Mellins have used the term "unresolved neonatal acute lung injury" to describe CLD (O'Brodovich 1985). According to their model, CLD results from disordered repair processes in a susceptible baby following acute lung injury induced by various pulmonary disorders and positive pressure ventilation. Preventive strategies can focus on any point in the cascade, including prevention or amelioration of the primary pulmonary disorders affecting preterm babies, reduction in ventilator‐induced lung injury or modification of the response to tissue injury (Sinkin 1987).
Description of the intervention
There is increasing evidence that inflammation plays an important role in the pathogenesis of CLD (Pierce 1995). In many infants, an inflammatory reaction is evident shortly after birth suggesting that the process may have been triggered in utero (Watterberg 1996). Therefore, interventions aimed at reducing or modulating the inflammatory process may reduce the incidence or severity of CLD.
How the intervention might work
Treatment with corticosteroids is an attractive intervention strategy to achieve this goal due to their strong anti‐inflammatory properties. Systematic reviews on the early use of postnatal systemic corticosteroids (≤ 7 days) and the late use of postnatal systemic corticosteroids (> 7 days) have demonstrated a reduction in CLD at 28 days and 36 weeks' postmenstrual age (PMA) (Bhuta 1998; Doyle 2014a; Doyle 2014b). Doyle 2014a and Doyle 2014b concluded that the benefits of early and postnatal use of corticosteroids may not outweigh actual or potential adverse effects. There are concerns regarding the short‐ and long‐term adverse effects of systemic corticosteroid therapy in this population (Ng 1993; Yeh 1998; Doyle 2014b). These include hyperglycaemia, hypertension, hypertrophic obstructive cardiomyopathy, gastrointestinal haemorrhage and perforation, growth failure and hypothalamic‐pituitary‐adrenal axis suppression. The potential effects on brain growth and neurodevelopment are most alarming: studies in animals have shown that steroids can permanently affect brain cell division, differentiation and myelination, as well as the ontogeny of cerebral cortical development (Weichsel 1977; Johnson 1979). As both dexamethasone and hydrocortisone administration within the first seven days of life is associated with an increased risk of cerebral palsy, early postnatal corticosteroid therapy is not recommended to prevent CLD. After seven days of life, dexamethasone has been shown to decrease the rate of CLD at 36 weeks’ postmenstrual age with less impact on neurodevelopmental outcome. No trials have examined whether the benefits of corticosteroids outweigh the adverse effects for infants at high risk of, or with, severe CLD (Jefferies 2012). Follow‐up of double‐blind randomised controlled trials of dexamethasone, commenced within 12 hours of birth, showed a two‐fold increase in neuromotor impairments in surviving dexamethasone‐treated infants as compared with controls at two years' corrected age (Yeh 1998; Doyle 1999). Two meta‐regression meta‐analyses have concluded that the effect of postnatal corticosteroids on the combined outcome of death or cerebral palsy varies with the level of risk for CLD (Doyle 2005; Doyle 2014c). Theoretically, administration of corticosteroids topically may allow for beneficial effects on the pulmonary system with a lower risk of undesirable systemic side effects.
Why it is important to do this review
A variety of Cochrane reviews address the use of systemic or inhaled corticosteroids in the prevention or treatment of bronchopulmonary dysplasia (BPD) or CLD.
These include reviews of the early use (≤ 7 days) of systemic postnatal corticosteroids to prevent chronic lung disease (Doyle 2014a), as well as the late use (> 7 days) of systemic postnatal corticosteroids for CLD (Doyle 2014b).
In addition, a variety of reviews address the use of inhaled corticosteroids in the prevention or treatment of CLD. Onland and colleagues have reviewed the late use (≥ 7 days) of inhaled corticosteroids to reduce BPD in preterm infants (Onland 2012). Shah and colleagues have compared the use of inhaled versus systemic corticosteroids for preventing CLD in ventilated very low birth weight (VLBW) preterm neonates (Shah 2003); and the use of inhaled versus systemic corticosteroids for the treatment of CLD in ventilated VLBW preterm infants (Shah 2007b).
The use of corticosteroids for other indications in neonates including intravenous dexamethasone to facilitate extubation (Davis 2001), corticosteroids for the treatment of hypotension (Ibrahim 2011), and corticosteroids for the treatment of meconium aspiration syndrome (Ward 2003) are reviewed.
This review aims to examine the impact of inhaled corticosteroid therapy when administered to VLBW preterm infants within the first two weeks of life for the prevention of CLD. This is an update of our review in 2007 (Shah 2007a), and in 2012 (Shah 2012).
Objectives
Primary objective: to determine the impact of inhaled corticosteroids administered to preterm infants with birth weight up to 1500 grams (VLBW) beginning in the first two weeks after birth for the prevention of CLD as reflected by the requirement for supplemental oxygen at 36 weeks' PMA.
Secondary objectives: assessment of the effect of inhaled corticosteroids on:
1. Other indicators of CLD including:
-
requirement for supplemental oxygen at 28 days of age;
-
death by, or CLD at, 28 days of age;
-
death by, or CLD at, 36 weeks' PMA;
-
duration of requirement for supplemental oxygen;
-
duration of assisted ventilation;
-
requirement for systemic corticosteroids;
-
change in pulmonary function tests.
2. The incidence of adverse events including:
-
mortality;
-
hyperglycaemia;
-
culture‐proven infection (positive blood or cerebrospinal fluid (CSF); or positive blood culture only) during hospital stay;
-
hypertension;
-
hypertrophic obstructive cardiomyopathy;
-
gastrointestinal haemorrhage or perforation;
-
growth (weight, length/height and head circumference);
-
cataracts;
-
hypertrophy of tongue;
-
nephrocalcinosis;
-
suppression of the hypothalamic‐pituitary‐adrenal axis.
3. Long‐term neurodevelopmental outcome: neurodevelopmental impairment is defined as presence of cerebral palsy and/or mental retardation (Bayley Scales of Infant Development (BSID) Mental Development Index (MDI) < 70 and/or legal blindness (< 20/200 visual acuity) and/or deafness (aided or < 60 dB on audiometric testing) assessed at 18 to 24 months.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised clinical trials of inhaled corticosteroid therapy in very low birth weight (VLBW) preterm infants enrolled in the first two weeks after birth (early administration). Studies which evaluated a combination of systemic and inhaled corticosteroids were excluded.
Types of participants
Preterm neonates with birth weight up to 1500 grams (VLBW) and postnatal age of less than 2 weeks.
Types of interventions
Inhaled corticosteroids versus placebo or no intervention.
Types of outcome measures
Primary outcomes
1. Chronic Lung Disease (CLD) at 36 weeks' postmenstrual age (PMA):
-
among all randomised;
-
among survivors.
Secondary outcomes
1. Among all randomised:
-
CLD at 28 days of age;
-
death by 28 days of age;
-
death by 36 weeks' PMA;
-
death by, or CLD at, 28 days of age;
-
death by, or CLD at, 36 weeks' PMA;
-
death during hospital stay (this outcome was added in the 2016 update of the review);
-
survival to hospital discharge without CLD (this outcome was added in the 2016 update of the review);
-
requirement for systemic steroids;
-
failure to extubate within 14 days;
-
adverse events: culture‐proven infection (blood or CSF), hyperglycaemia, hypertension, gastrointestinal bleeding, cataracts, intraventricular haemorrhage (IVH), periventricular leukomalacia (PVL), brain injury*, necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP), pituitary‐adrenal suppression, and patent ductus arteriosus (PDA).
2. Among survivors:
-
CLD at 28 days of age.
3. Long‐term neurodevelopmental outcome: neurodevelopmental impairment is defined as presence of cerebral palsy and/or mental retardation (Bayley Scales of Infant Development (BSID), Mental Development Index (MDI) < 70) and/or legal blindness (< 20/200 visual acuity) and/or deafness (aided or < 60 dB on audiometric testing) assessed at 18 to 24 months.
* post hoc outcome
Search methods for identification of studies
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal search strategy for specialized register).
Electronic searches
For the 2016 update, we conducted a comprehensive search including: Cochrane Central Register of Controlled Trials (CENTRAL; 2015, Issue 12) in the Cochrane Library (searched 5 January 2016); MEDLINE via PubMed (1966 to 5 January 2016); Embase (1980 to 5 January 2016); and CINAHL (1982 to 5 January 2016) using the following search terms: (bronchopulmonary dysplasia OR lung diseases OR chronic lung disease) AND (anti‐inflammatory agents OR steroids OR dexamethasone OR inhalation OR aerosols OR budesonide OR beclomethasone dipropionate OR flunisolide OR fluticasone propionate)), plus database‐specific limiters for RCTs and neonates (see Appendix 1 for the full search strategies for each database). We did not apply language restrictions.
We searched clinical trials' registries for ongoing or recently completed trials (ClinicalTrials.gov; the World Health Organization’s International Trials Registry and Platform www.whoint/ictrp/search/en/; and the ISRCTN Registry).
For the 2011 update, randomised controlled trials of inhaled corticosteroid therapy in preterm neonates were identified from MEDLINE via PubMed using MeSH headings: infant‐newborn; bronchopulmonary dysplasia; lung diseases; anti‐inflammatory agents; steroids; administration; inhalation; aerosols; budesonide; beclomethasone dipropionate; flunisolide; and fluticasone propionate. We searched Embase and CINAHL. See Appendix 2 for the complete search strategies.
Searching other resources
We searched the reference lists of published trials. One trial was identified through an additional search of MEDLINE in May 2016 for reasons unrelated to this review (Nakamura 2016).
Data collection and analysis
We used the methods of the Cochrane Neonatal Review Group for data collection and analysis.
Selection of studies
We included all randomised and quasi‐randomised controlled trials that fulfilled the selection criteria described in the previous section. We would have included cluster randomised trials if they had been identified. The review authors independently reviewed the results of the updated search and selected studies for inclusion. We resolved any disagreement by discussion.
Data extraction and management
We sought information regarding the method of randomisation, blinding and reporting of all outcomes of all the infants enrolled in the trial for each trial. We obtained data from the primary investigator for unpublished trials or when published data were incomplete. We assessed retrieved articles and three review authors (VS, MD, AO) abstracted data independently. The updates of the review in 2012 and 2016 were performed by two review authors (VS, AO).
For each study, final data were entered into Review Manager 5 by one review author (AO) and then checked for accuracy by a second reviewer author (VS). We resolved discrepancies through discussion.
We attempted to contact authors of the original reports to provide further details when information regarding any of the above was unclear.
Assessment of risk of bias in included studies
The review authors independently assessed the risk of bias (low, high, or unclear) of all included trials using the Cochrane ‘Risk of bias’ tool (Higgins 2011) for the following domains:
-
selection bias;
-
performance bias;
-
detection bias;
-
attrition bias;
-
reporting bias;
-
or any other bias.
We resolved any disagreements by discussion or, in the event of deadlock, by a third assessor's adjudication. See Appendix 3 for a more detailed description of risk of bias for each domain.
Measures of treatment effect
We performed statistical analyses using Review Manager software (RevMan 2014). Dichotomous data were analysed using relative risk (RR), risk difference (RD) and the number needed to treat for an additional beneficial outcome (NNTB) or number needed to treat for an additional harmful outcome (NNTH). The 95% CI were reported on all estimates.
We analysed continuous data using mean difference (MD) or, if applicable, the standardized mean difference, to combine trials that measured the same outcome but used different methods.
Unit of analysis issues
We analysed the data as the proportion of neonates having one or more episodes for clinical outcomes such as episodes of sepsis.
Dealing with missing data
For included studies, levels of attrition were noted. The impact of including studies with high levels of missing data in the overall assessment of treatment effect was explored by using sensitivity analysis.
All outcomes analyses were on an intention‐to‐treat basis, i.e. we included all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We examined heterogeneity between trials by inspecting the forest plots and quantifying the impact of heterogeneity using the I² statistic. If noted, we planned to explore the possible causes of statistical heterogeneity using pre‐specified subgroup analysis (for example, differences in study quality, participants, intervention regimens, or outcome assessments).
Based on the results of the I² statistic we used the following cut‐offs and labels for heterogeneity: less than 25% – no heterogeneity; 25% to 49% – low heterogeneity; 50% to 74% – moderate heterogeneity; and 75% or above – high heterogeneity.
Assessment of reporting biases
We planned to assess possible publication bias and other biases using symmetry/asymmetry of funnel plots if there had been 10 or more trials included in an analysis.
For included trials that were recently performed (and therefore prospectively registered), we explored possible selective reporting of study outcomes by comparing the primary and secondary outcomes in the reports with the primary and secondary outcomes proposed at trial registration, using the web sites ClinicalTrials.gov and Controlled‐Trials.com. If such discrepancies were found, we planned to contact the primary investigators to obtain missing outcome data on outcomes pre‐specified at trial registration.
Data synthesis
Meta‐analysis was done using Review Manager software (RevMan 2014), supplied by Cochrane. We used the Mantel‐Haenszel method for estimates of typical relative risk and risk difference. We analysed continuous measures using the inverse variance method.
We used the fixed‐effect model for all meta‐analyses.
Quality of evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the quality of evidence for the following (clinically relevant) outcomes: chronic lung disease at 36 weeks' PMA and death and CLD at 36 weeks' PMA amongst all randomised and amongst survivors.
Two authors independently assessed the quality of the evidence for each of the outcomes above. We considered evidence from randomised controlled trials as high quality but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias), consistency across studies, directness of the evidence, precision of estimates and presence of publication bias. We used the GRADEpro 2014 Guideline Development Tool to create a ‘Summary of findings’ table to report the quality of the evidence.
The GRADE approach results in an assessment of the quality of a body of evidence in one of four grades:
-
High: We are very confident that the true effect lies close to that of the estimate of the effect.
-
Moderate: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
-
Low: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
-
Very low: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Subgroup analysis and investigation of heterogeneity
Groups were analysed based on 'all randomised' and 'survivors only'.
Sensitivity analysis
We planned sensitivity analyses for situations where this might affect the interpretation of significant results (for example, where there is risk of bias associated with the quality of some of the included trials or missing outcome data). None was thought necessary in this review.
Results
Description of studies
Results of the search
For the results of our literature searches see Study flow diagram (Figure 1).
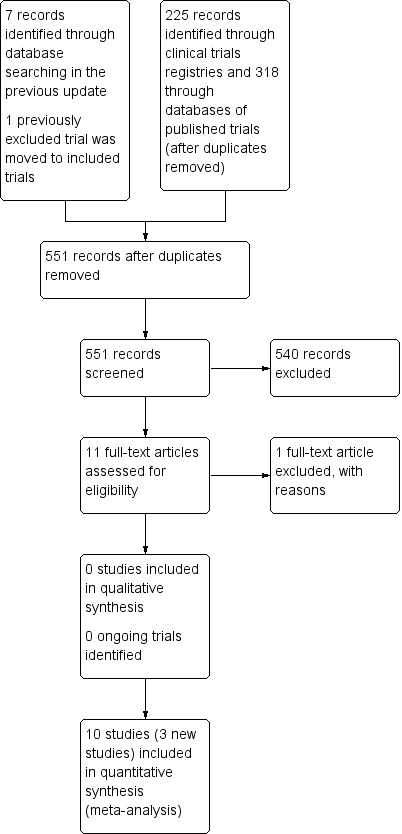
Study flow diagram.
For this update of the review two additional trials were identified (Bassler 2015; Nakamura 2016). The study by Denjean 1998 was moved from excluded to included studies.
Fourteen trials assessing the impact of inhaled corticosteroids were identified, of which four trials were excluded (Kovacs 1998; Beresford 2002; Dugas 2005; Yeh 2016).
Ten trials qualified for inclusion in this review: Denjean 1998; Townsend 1998; Yong 1999; Merz 1999; Fok 1999; Cole 1999; Jonsson 2000; Jangaard 2002; Bassler 2015; and Nakamura 2016. Eight included studies have been published as complete articles while two studies were presented at scientific meetings and published in abstract form (Townsend 1998; Yong 1999). Complete data from the investigators were available for Yong 1999, while information published in abstract form is presented for Townsend 1998.
Although all studies attempted to include infants thought to be at risk of developing CLD, the inclusion criteria, the intervention (type of inhaled corticosteroid) and duration of therapy varied between studies. All studies except Jonsson 2000 used a metered dose inhaler (MDI) and an Aerochamber interposed between the endotracheal tube and the ventilatory circuit or a manual puffer (anaesthesia bag). In Cole 1999, the drug was administered to infants who were extubated using the same procedure through a nasopharyngeal tube. In Jonsson 2000, a dosimetric jet nebulizer was used to deliver the aerosol.
Details of each study are given in the table 'Characteristics of included studies'.
Included studies
See 'Characteristics of included studies'.
Ten trials qualified for inclusion in this review: Denjean 1998; Townsend 1998; Yong 1999; Merz 1999; Fok 1999; Cole 1999; Jonsson 2000; Jangaard 2002; Bassler 2015; and Nakamura 2016.
Bassler 2015: the study by Bassler and co‐workers enrolled 863 infants with postmenstrual age (PMA) 230/7 weeks to 276/7 weeks and chronological age of 12 hours or less, who required any form of positive pressure support. Exclusion criteria were: palliative care; dysmorphic feature or congenital abnormalities likely to affect life expectancy or neurologic development; strongly suspected cyanotic heart disease; and, to prevent a correlated data problem, the infant was from a multiple‐birth pregnancy (other than the second infant in birth order, who was considered eligible). The budesonide group (n = 441; 437 followed to first discharge home) received two puffs of budesonide (200 µg/puff) administered every 12 hours for the first 14 days of life and one puff administered every 12 hours from day 15 until the last dose of study drug had been administered. Study drugs were administered until infants no longer needed supplemental oxygen and positive pressure support or reached a PMA of 320/7 weeks, regardless of ventilator status. The control group (n = 422; 419 followed to first discharge home) received two puffs of placebo containing only hydrofluoroalkane propellant.
Primary outcome: a composite of death or bronchopulmonary dysplasia (BPD) at 36 weeks' PMA. BPD was defined as the requirement for positive pressure support, the requirement for supplemental oxygen at FiO₂ exceeding 0.30, or in infants receiving low amounts of oxygen, an inability to maintain an oxygen saturation value above 90% during a structured, short period of saturation monitoring coupled with gradual weaning from oxygen to ambient air (oxygen reduction test).
Secondary outcomes included: death by any cause at 36 weeks' PMA, BPD at 36 weeks' PMA (defined as per above); duration of positive pressure respiratory support or supplemental oxygen; ventriculomegaly with or without intraventricular haemorrhage (IVH) on ultrasound at or before 36 weeks' PMA; patent ductus arteriosus (PDA) requiring medical or surgical treatment; intestinal perforation or necrotizing enterocolitis (NEC); retinopathy of prematurity (ROP) (stage 2 or higher); culture‐proven infections; increase in body weight and head circumference from birth to day 28; length of hospital stay; need for reintubation after the last dose of drug had been administered; occurrence of oral candidiasis requiring treatment; hyperglycaemia requiring insulin treatment; and hypertension requiring treatment.
Neurodevelopmental disability testing is to be conducted at 18 to 22 months (hence is not reported in this current publication).
Cole 1999: the study by Cole and co‐workers enrolled infants of less than 33 weeks gestational age (GA) and with birth weight equal up to 1250 grams who required assisted ventilation at three to 14 days of life. The infants were randomly assigned to receive inhaled beclomethasone dipropionate (n = 123) or placebo (n = 130). The desired dose was calculated to deliver to the lung 40 µg/kg/day for the first week, 30 and 15 µg/kg/day for the second and third weeks respectively, and then 10 and 5 µg/kg/day during the fourth week. The primary outcome was the incidence of BPD in survivors defined as an abnormal chest x‐ray and need for supplemental oxygen at 28 days of life. Secondary outcomes included the incidence of BPD in survivors at 36 weeks' PMA (defined as an abnormal chest x‐ray and need for supplemental oxygen at that age), duration of respiratory support (oxygen, mechanical ventilation and continuous positive airway pressure), the need for systemic glucocorticoids, diuretic or bronchodilator therapy, death, length of hospitalisation and the incidence of complications possibly attributable to the use of inhaled steroids. Systemic glucocorticoid therapy was permitted at the discretion of the infant's physician. The baseline characteristics of the two groups were similar except for maternal race or ethnic group (P = 0.03). Two additional reports from the same trial (Cole 1999) have been published as separate articles. One of these reports evaluated the effect of inhaled beclomethasone therapy on adrenal response and the other report evaluated its effect on tracheal aspirate inflammatory mediators (IL‐8 and IL‐1ra).
Denjean 1998: the study by Denjean and co‐workers enrolled infants with respiratory distress syndrome and PMA less than 31 weeks. Infants were eligible for the study if they required ventilator support (intermittent mandatory ventilation (IMV) or nasal IMV/continuous positive airway pressure (CPAP)) on the 10th postnatal day. 178 infants were randomised, five were withdrawn leaving 173 infants in the trial who were assigned to four groups (placebo + placebo; placebo + salbutamol; placebo + beclomethasone; beclomethasone + salbutamol) of which two (placebo + placebo and placebo + beclomethasone) are included in our review. Beclomethasone (250 µg) was given four times a day (1000 µg daily). Treatment was started on the 10th or 11th postnatal day and was given for 28 days, with dose tapering over a period of eight days. Total number reported on: n = 43. Placebo (250 µg) was given four times a day (1000 µg daily). Treatment was started on the 10th or 11th postnatal day and was given for 28 days, with dose tapering over a period of 8 days. Total number reported on: n = 43. Beclomethasone and placebo were administered by metered‐dose inhalers.
The main outcome criterion was CLD. The diagnosis of CLD was made at 28 days of age on the basis of clinical (oxygen dependence) and radiographic criteria. CLD was categorized in three grades of severity: severe: ventilation with endotracheal tube (ET) for more than three months or oxygen supplementation for more than four months; moderate: ventilation with ET for more than one month or oxygen supplementation for more than two months; and mild: ventilation with ET for less than one month and oxygen supplementation for less than two months. The definition of CLD was unclear. Secondary outcomes included: survival without CLD, death (during hospital stay), ventilatory support (nasal IMV, CPA or IMV) (days), need for supplementary oxygen (days), need for systemic dexamethasone (IV), and sepsis (positive blood culture).
Fok 1999: the study by Fok and co‐workers enrolled 53 infants born at less than 32 weeks' GA, birth weight less than 1.5 kg, requiring mechanical ventilation with an arterial PO₂/alveolar PO₂ ratio of less than 0.25 at 6 to 10 hours after the second dose of surfactant was administered. Infants were excluded if they needed high‐frequency ventilation at the time of enrolment. Infants were randomised to receive inhaled fluticasone propionate or placebo. Two puffs of fluticasone propionate (250 micrograms/puff) or placebo were administered 12 hourly for two weeks. The first dose was administered within 24 hours of birth. The primary outcome was successful extubation by day seven or day 14 of life. Secondary outcomes included mortality, oxygen dependency at 28 days of postnatal age and at 36 weeks' PMA. The incidence of complications possibly attributable to the use of inhaled steroids was monitored. Twenty‐seven infants were enrolled in the fluticasone propionate group and 26 in the placebo group. The two groups were similar in their demographic and perinatal characteristics.
Jangaard 2002: the study by Jangaard and co‐workers enrolled 60 preterm infants weighing less than 1250 grams with respiratory distress syndrome (RDS) and requiring ventilatory support at 72 hours of age. Infants were randomly assigned to receive inhaled beclomethasone dipropionate (250 µg/puff) or placebo for four weeks. Medication dosage assumed a 10% deposition of the administered dose with the aim to provide a total dose of 0.2 mg/kg/day. When the infants were extubated, the study drug was administered using an infant‐sized Aerochamber (Boehringer Ingelheim, Canada) with an appropriately fitted mask. The primary outcome for this study was BPD defined as oxygen dependency at 28 days of life. The demographic characteristics of the two groups were similar. Jangaard 2002 has been previously published in abstract form. The results of the published report are presented in this review.
Jonsson 2000: The study by Jonsson and co‐workers randomised 30 VLBW infants with median (range) GA of 26 weeks (23 to 29 weeks) and median birth weight of 805 g (525 to 1227 g). Inclusion criteria were 1) mechanical ventilation on day six of life, or 2) if extubated, nasal continuous positive airway pressure with FiO₂ of 0.3 or higher. Infants with the following conditions were excluded: congenital malformations, congenital heart disease and grades III‐IV IVH. Infants on high frequency oscillatory ventilation (HFOV) were excluded as the inhalations could not be given through the electronic dosimetric jet nebulizer. Infants were randomised to receive 500 µg twice a day or placebo delivered using a dosimetric jet nebulizer with variable inspiratory time and breath sensitivity. Inhalations were started on day seven of life. The primary objective was to attain a 30% reduction in FiO₂ levels in the budesonide treatment group after 14 days of therapy. Secondary outcomes included: duration of supplemental oxygen, duration of mechanical ventilation, duration of nasal CPAP, oxygen requirements at 28 days of age and at 36 weeks' postmenstrual age. Adrenal cortisol response to stimulation was measured at baseline (prior to commencement of inhalation) and at the end of the study period. Information on adverse events — hyperglycaemia, hypertension, sepsis, PDA, IVH and gastrointestinal problems — were collected. Of the 30 infants enrolled, one parent declined to participate and two eligible infants could not be included due to ongoing HFOV on day seven of life. Thirteen infants were enrolled in the budesonide group, of which eight were ventilated, while 14 infants were enrolled in the placebo group, of which nine were ventilated at the commencement of therapy. Only one outcome for ventilated infants was reported (successful extubation during the study period ‒ 14 days).
Merz 1999: the study by Merz and co‐workers enrolled 24 infants with a birth weight of 750 to 1500 grams, GA of 25 to 32 weeks, ventilator dependency on day three of life with a rate of 15 breaths/minute or more and FiO₂ of 0.25 or more to maintain oxygen saturation 90% or more. Infants were randomly assigned to inhaled budesonide (200 µg/puff) or placebo. Two puffs were administered four times a day for a total of 10 days. The primary outcome was duration of artificial ventilation. Secondary outcomes included the duration of supplemental oxygen and the release of albumin and different inflammatory mediators in the tracheobronchial aspirate fluid. Adverse events such as frequency of acute infections, hypertension, hyperglycaemia, and adrenal suppression were evaluated. The demographic and perinatal data were similar in both groups on the day of randomisation.
Nakamura 2016: The study by Nakamura and co‐workers enrolled 211 infants with birth weight of less than 1000 grams, who needed endotracheal intubation and respiratory support due to respiratory failure. Infants were randomised to prophylactic inhaled steroids starting within 24 hours of birth and continuing until six weeks of age or extubation. Two doses of 50 µg fluticasone propionate (FP) were administered every 24 hours. The placebo group received two doses of placebo every 24 hours. The placebo contained only hydrofluoroalkane propellant. The primary outcome was death or oxygen dependency at discharge from NICU. Secondary outcomes included death, severe BPD and neurodevelopmental outcomes at 18 months' PMA and three years of age. Complications of preterm birth (grade 3 or 4 IVH; periventricular leukomalacia (PVL); NEC; sepsis and ROP) were reported in combination with deaths.
Townsend 1998: The study by Townsend and co‐workers enrolled 32 infants with GA less than 28 weeks and birth weight up to 1100 grams who were ventilator dependent with RDS. Infants were randomised to receive flunisolide or placebo in the dose of 500 µg three times a day delivered via spacer chamber. Treatment was begun at 48 to 96 hours of age and continued for 28 days or until extubation. Outcomes included were: need for systemic dexamethasone, duration of ventilation, duration of hospitalisation, duration of supplemental oxygen and the incidence of adverse events (hyperglycaemia, hypertension, weight gain).
Yong 1999: The study by Yong and co‐workers enrolled 40 infants born at less than 32 weeks' GA and requiring mechanical ventilation at birth within 18 hours after birth. Infants were randomly assigned to receive fluticasone propionate or placebo. One puff (250 µg/puff) was administered twice a day for two weeks. There was no difference in the baseline characteristics between groups. Study outcomes included frequency of BPD at 28 days of life and at 36 weeks' PMA, duration of respiratory support, need for systemic corticosteroids, mortality, duration of hospitalisation, successful extubation by seven and 14 days of age, pulmonary function tests (compliance and resistance), inflammatory markers in the tracheal aspirates and incidence of adverse events.
Excluded studies
See 'Characteristics of excluded studies'.
Four trials were excluded (Kovacs 1998; Beresford 2002; Dugas 2005; Yeh 2016). Beresford 2002 was excluded as infants had to be receiving supplemental oxygen at 36 weeks' PMA at the time of randomisation. Denjean 1998 was excluded in previous versions of this review as both ventilated and non‐ventilated infants were included and we were unable to obtain data for ventilated infants from the authors. In a deviation from our protocol for this update we included all infants on any form of assisted ventilatory support (nasal CPAP/IMV or endotracheal IMV). Dugas 2005 was excluded as infants were randomised between 28 and 60 days of age (late). Kovacs 1998 was excluded as investigators evaluated the impact of a combination of systemic and inhaled corticosteroid for prevention of CLD. Yeh 2016 compared the effect of intratracheal administration of surfactant/budesonide with that of surfactant alone on the incidence of death or BPD.
Risk of bias in included studies
For details please see Figure 2; Figure 3.
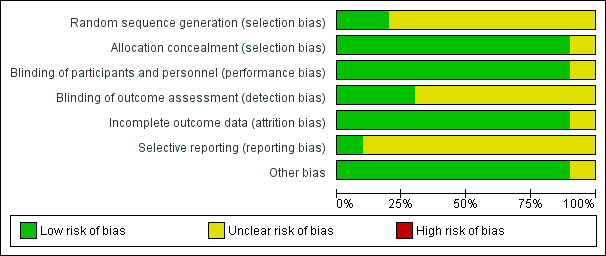
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
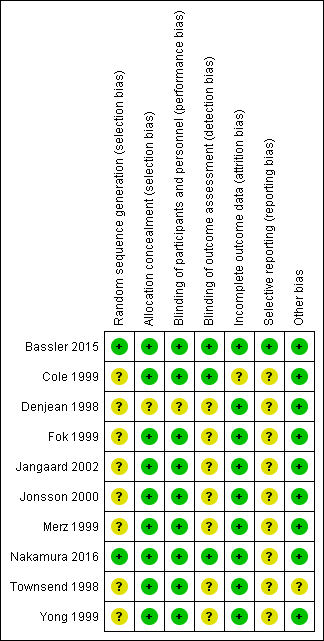
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The risk of bias regarding the random sequence generation was low in Bassler 2015 and Nakamura 2016 and the risk was unclear in the remaining eight studies.
The allocation concealment was of low risk of bias in all studies except for Denjean 1998 in which no information was provided.
Blinding
The risk of performance bias was low in nine studies (no information provided in Denjean 1998) and the risk of detection bias was low in three studies and unclear in seven studies.
Incomplete outcome data
Attrition bias was low in nine studies and unclear in one study (Cole 1999).
Exclusions after randomisation:
In Bassler 2015 four infants in the budesonide group and three infants in the placebo group had unknown outcomes because of withdrawal of consent or right to use the data.
In Cole 1999, three infants were withdrawn before the study drug was administered (two due to sepsis and one due to prior receipt of systemic glucocorticoid therapy). In the treatment group, one infant had been withdrawn prior to 28 days of life and eight more were withdrawn by 36 weeks' PMA. Similarly, in the placebo group, two infants had been withdrawn by 28 days of age and four more were withdrawn by 36 weeks' PMA. Reasons for these later withdrawals were not described. The outcome data for withdrawn infants were not provided. Thus, outcomes were reported at 28 days for 122 treated and 128 control infants, and at 36 weeks' PMA for 114 treated and 124 control infants.
In Denjean 1998 178 infants were initially randomised, but informed consent was either not obtained or withdrawn for five infants, leaving 173 infants in the trial. During the study the randomisation code was broken in three cases because of severe deterioration.
One infant in the placebo group was withdrawn from Merz 1999 due to severe sepsis.
Selective reporting
In only one study was the protocol available to us (Bassler 2015). In the other studies the study protocol was not available to us and we could not judge if there were any deviations from the protocol or not.
Other potential sources of bias
We could not ascertain if there was other bias in one study for which only the abstract was available to us (Townsend 1998). For the remaining studies we could not identify any other potential sources of bias.
Effects of interventions
See: Summary of findings for the main comparison Early inhaled steroids (< 2 weeks) compared to placebo (among all randomised) for preventing chronic lung disease in very low birth weight preterm neonates; Summary of findings 2 Early inhaled steroid (< 2 weeks) compared to placebo (among survivors) for preventing chronic lung disease in very low birth weight preterm neonates
Nakamura 2016 reported all outcomes as a combination of death and a short‐ or long‐term clinical outcome. We wrote to the authors for clarifications regarding the outcomes on 20th May 2016 but as of 20th July 2016 we have not received a response. We report their findings separately in Analysis 1.23 to Analysis 1.32 as their data could not be incorporated in any of the meta‐analyses. This is in a deviation from our protocol.
Early inhaled steroids (< 2 weeks) vs. placebo among all randomised (Comparison 1)
If only one study is included in an analysis tests for heterogeneity are not applicable.
Primary outcome
CLD at 36 weeks' PMA (Outcome 1.1):
Five trials enrolling 429 neonates reported on the incidence of CLD at 36 weeks' PMA among all randomised (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002). There was no significant difference in the incidence of CLD at 36 weeks' PMA in the inhaled steroid group versus the placebo group (typical RR 0.97, 95% CI 0.62 to 1.52; typical RD −0.00, 95% CI −0.07 to 0.06). There was no heterogeneity for this outcome for RR (I² = 11%) nor for RD (I² = 0%). Analysis 1.1Figure 4.

Forest plot of comparison: 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), outcome: 1.1 CLD at 36 weeks' PMA.
Secondary outcomes
CLD at 28 days of age (Outcome 1.2):
Five trials enrolling 429 neonates reported on the incidence of CLD at 28 days of age among all randomised (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002). There was no significant difference in the incidence of CLD at 28 days (typical RR 1.08, 95% CI 0.85 to 1.38; typical RD 0.03, 95% CI −0.08 to 0.14). There was no heterogeneity for this outcome for RR (I² = 4%) nor for RD (I² = 23%). Analysis 1.2.
Death by 28 days of age (Outcome 1.3):
Five trials enrolling 429 neonates reported on the incidence of death by 28 days of age among all randomised (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002). There was no significant effect on death by 28 days of age (typical RR 0.66, 95% CI 0.39 to 1.14; typical RD −0.04, 95% CI −0.09 to 0.01). There was no heterogeneity for this outcome for RR (I² = 0%); however, there was moderate heterogeneity for RD (I² = 59%). Analysis 1.3.
Death by 36 weeks' PMA (Outcome 1.4):
Six trials enrolling 1285 neonates reported on the incidence of death by 36 weeks' PMA among all randomised (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002; Bassler 2015). No significant effect on mortality by 36 weeks' PMA was noted (typical RR 1.07, 95% CI 0.82 to 1.40; typical RD 0.01, 95% CI −0.03 to 0.05). There was moderate heterogeneity for this outcome for RR (I² = 51%); and there was low heterogeneity for RD (I² = 48%). Analysis 1.4.
Death by, or CLD at, 28 days of age (Outcome 1.5):
Five trials enrolling 429 neonates reported on the incidence of death by or CLD at 28 days of age among all randomised (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002). There was no significant difference between the groups for the combined outcome of death by, or CLD at, 28 days of age (typical RR 0.96, 95% CI 0.80 to 1.14; typical RD −0.02, 95% CI −0.11 to 0.07). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.5.
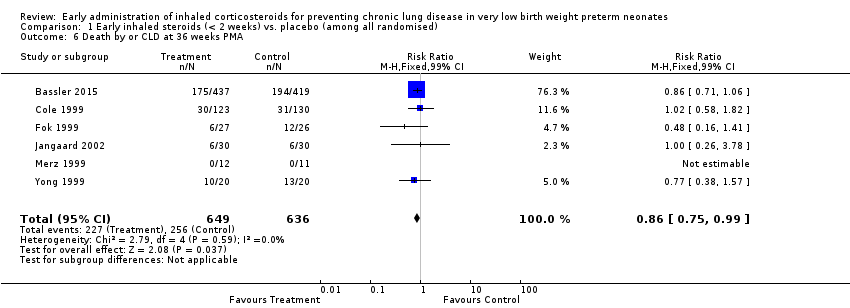
Death by, or CLD at, 36 weeks' PMA (Outcome 1.6):
Six trials enrolling 1285 neonates reported on this outcome (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002; Bassler 2015). There was a significant difference noted for the combined outcome of death by, or CLD at, 36 weeks' PMA (typical RR 0.86, 95% CI 0.75 to 0.99; typical RD −0.06, 95% CI −0.11 to −0.00) (P = 0.04); NNTB 17 (95% CI 9 to infinity). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.6; Figure 5.

Forest plot of comparison: 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), outcome: 1.6 Death by or CLD at 36 weeks' PMA.
Survival to hospital discharge without CLD (Outcome 1.7):
One trial enrolling 86 infants reported on this outcome (Denjean 1998). There was no significant difference between the groups for survival to discharge without CLD (RR 1.50, 95% CI 0.83 to 2.72; RD 0.14, 95% CI −0.06 to 0.34). Analysis 1.7.
Death during hospital stay (Outcome 1.8):
One trial enrolling 86 infants reported on this outcome (Denjean 1998). There was no significant difference between the groups for death during hospital stay (RR 1.75, 95% CI 0.55 to 5.55; RD 0.07, 95% CI −0.07 to 0.21). Analysis 1.8.
Culture‐proven infection (Outcome 1.9):
Two trials reported on 896 neonates for the incidence of culture‐proven infection (positive blood or CSF culture) (Yong 1999; Bassler 2015). There was no statistically significant difference in the incidence of culture‐proven infection based on this definition (typical RR 1.17, 95% CI 0.97 to 1.41; typical RD 0.05, 95% CI −0.01 to 0.11). There was low heterogeneity for this outcome for RR (I² = 34 %) and for RD (I² = 47 %).
Four trials reported on 225 neonates for the incidence of culture‐proven infection (positive blood culture) (Denjean 1998; Fok 1999; Jonsson 2000; Jangaard 2002). There was no statistically significant difference in the incidence of culture‐proven infection based on this definition (typical RR 1.17, 95% CI 0.83 to 1.65; typical RD 0.05, 95% CI −0.06 to 0.16). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%).
For the two outcomes (positive blood culture or CSF culture and positive blood culture) combined (N = 1121 neonates) there was no statistically significant difference for culture‐proven infection (typical RR 1.17, 95% CI 0.99 to 1.38; typical RD 0.05, 95% CI −0.00 to 0.11). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.9.
Hyperglycaemia (Outcome 1.10):
Three trials enrolling 116 neonates reported on the incidence of hyperglycaemia (Fok 1999; Merz 1999; Yong 1999). There was no significant difference in the incidence of hyperglycaemia (typical RR 0.84, 95% CI 0.49 to 1.44; typical RD −0.05, 95% CI −0.19 to 0.10). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.10.
Bassler 2015 found no significant difference in the occurrence of hyperglycaemia requiring insulin treatment between the two groups (n = 856) (RR 0.97, 95% CI 0.74 to 1.27; RD −0.01, 95% CI −0.06 to 0.05). Tests for heterogeneity were not applicable. Analysis 1.10.
Hypertension (Outcome 1.11):
Three trials enrolling 116 neonates reported on the incidence of hypertension (Fok 1999; Merz 1999; Yong 1999). There was no statistically significant difference in the incidence of hypertension between groups (typical RR 1.20, 95% CI 0.36 to 3.99; typical RD 0.01, 95% CI −0.09 to 0.12). Test for heterogeneity was not applicable for RR (two studies had no outcomes) and there was no heterogeneity for RD (I² = 0%). Analysis 1.11.
Bassler 2015 reported no significant difference in the occurrence of hypertension requiring treatment between the two groups (n = 856) (RR 0.58, 95% CI 0.21 to 1.57; RD −0.01, 95% CI −0.03 to 0.01). Tests for heterogeneity were not applicable. Analysis 1.11.
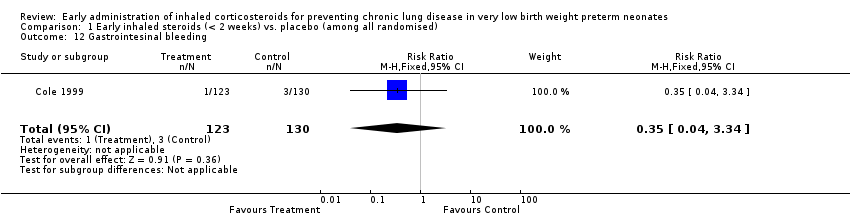
Gastrointestinal bleeding (Outcome 1.12):
One trial enrolling 253 neonates reported on the incidence of gastrointestinal bleeding (Cole 1999). There was no significant difference for this outcome between groups (RR 0.35, 95% CI 0.04 to 3.34; RD −0.01, 95% CI −0.05 to 0.02). Tests for heterogeneity were not applicable. Analysis 1.12.
Bassler 2015 did not report on gastrointestinal bleeding, but reported on gastrointestinal disorders which occurred in 30 cases (6.86%) in the inhaled budesonide group and in 32 cases (7.64%) in the placebo group. The contribution of gastrointestinal bleeding to the total number is not reported.
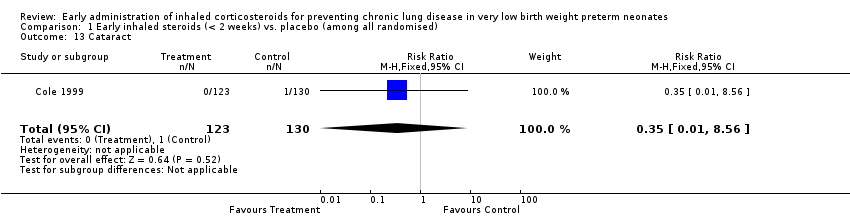
Cataract (Outcome 1.13):
One trial enrolling 253 neonates reported on the incidence of cataracts (Cole 1999). There was no significant difference in the incidence of cataracts between groups (RR 0.35, 95% CI 0.01 to 8.56; RD −0.01, 95% CI −0.03 to 0.01). Tests for heterogeneity were not applicable. Analysis 1.13.
Intraventricular haemorrhage (IVH) (Outcome 1.14):
Two trials enrolling 306 neonates reported on the incidence of IVH (Fok 1999; Cole 1999). There was no significant difference in the incidence of IVH between groups (typical RR 1.04, 95% CI 0.77 to 1.41; typical RD 0.02, 95% CI −0.09 to 0.12). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.14.
Periventricular leukomalacia (PVL) (Outcome 1.15):
Two trials enrolling 306 neonates reported on the incidence of PVL (Fok 1999; Cole 1999). There was no significant difference in the incidence of PVL between groups (typical RR 1.43, 95% CI 0.59 to 3.46; typical RD 0.02, 95%CI −0.03 to 0.08). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.15.
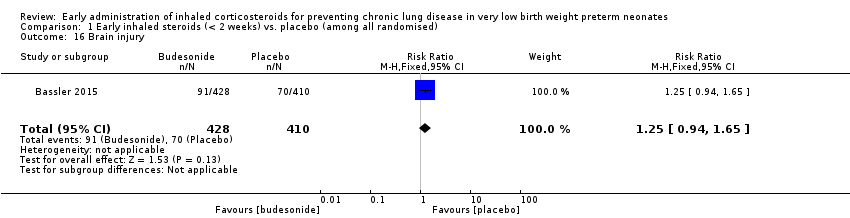
Brain injury (Outcome 1.16):
One trial reporting on 838 infants reported on the incidence of brain injury diagnosed based on the worst cranial ultrasound finding performed at or before 36 weeks' PMA (Bassler 2015). There was no significant difference in the incidence of brain injury between the two groups (RR 1.25, 95% CI 0.94 to 1.65; RD 0.04, 95% CI −0.01 to 0.10). Tests for heterogeneity were not applicable. Analysis 1.16
Necrotizing enterocolitis (NEC) (Outcome 1.17):
Three trials enrolling 1162 neonates reported on the incidence of NEC (Cole 1999; Fok 1999; Bassler 2015). There was no significant difference in the incidence of NEC between groups (typical RR 0.92, 95% CI 0.68 to 1.24; typical RD −0.01, 95% CI −0.05 to 0.03). There was low heterogeneity for this outcome for RR (I² = 31%) and for RD (I² = 40%). Analysis 1.17.
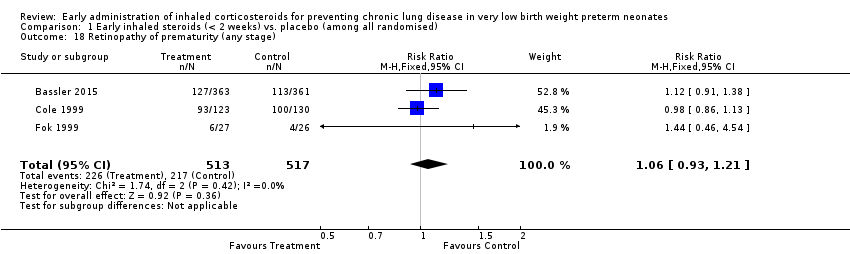
Retinopathy of prematurity (ROP) any stage (Outcome 1.18):
Two trials enrolling 306 neonates reported on the incidence of ROP (Fok 1999; Cole 1999). There was no significant difference in the incidence of ROP (typical RR 1.00, 95% CI 0.87 to 1.15; typical RD 0.00, 95% CI −0.09 to 0.09). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.18
Three trials enrolling 1030 neonates reported on the incidence of ROP (Cole 1999; Fok 1999; Bassler 2015). There was no significant difference in the incidence of ROP (typical RR 1.06, 95% CI 0.93 to 1.21; typical RD 0.03, 95% CI −0.03 to 0.08). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 1.18.
Patent ductus arteriosus (Outcome 1.19):
One trial enrolling 53 neonates reported on the incidence of PDA (Fok 1999). There was no significant difference in the incidence of PDA between the two groups (RR 0.82, 95% CI 0.57 to 1.17; RD −0.14, 95% CI −0.38 to 0.10). Tests for heterogeneity were not applicable. Bassler 2015 reported on PDA treated with drugs (reported un stratified RR 0.88, 95% CI 0.76 to 1.01) and with surgical ligation (reported un stratified RR 0.55, 95% CI 0.36 to 0.84). There was overlap between these groups and we are awaiting clarification by the first author prior to inclusion in the analysis. Analysis 1.19.
Reintubation (Outcome 1.20):
One trial reporting on 856 infants reported a significantly lower risk of reintubation in the steroid group compared with the control group (RR 0.58, 95% CI 0.35 to 0.96; RD −0.04, 95% CI −0.07 to −0.00; NNTB 25, 95% CI 14 to ∞) (Bassler 2015). Tests for heterogeneity were not applicable. Analysis 1.20.
Requirement for systemic steroids (Outcome 1.21):
Eight trials enrolling 1403 infants reported on the requirements for systemic steroids (Denjean 1998; Townsend 1998; Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002; Bassler 2015). The need for systemic steroids was not statistically significantly different between groups (typical RR 0.89, 95% CI 0.77 to 1.02; typical RD −0.04, 95% CI −0.09 to 0.01). There was low heterogeneity for this outcome for RR (I² = 33%) and moderate heterogeneity for RD (I² = 63%). Analysis 1.21.
Failure to extubate within 14 days (Outcome 1.22):
Five trials enrolling 193 neonates reported on this outcome (Fok 1999; Merz 1999; Yong 1999; Jonsson 2000; Jangaard 2002). There was no significant difference noted for this outcome (typical RR 0.97, 95% CI 0.76 to 1.24; typical RD −0.02, 95% CI −0.15 to 0.12). There was moderate heterogeneity for this outcome for RR (I² = 61%) and high heterogeneity for RD (I² = 80%). Analysis 1.22.
The following outcomes (Analysis 1.23 to Analysis 1.32) all pertain to the trial by Nakamura and co‐workers (Nakamura 2016), who for all outcomes reported a combination of deaths and complications of preterm birth. As there is only one trial included in these analyses tests for heterogeneity are not applicable. Some denominators exclude infants for which the outcome could not be ascertained.
Death or oxygen dependency at discharge (Outcome 1.23):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 0.63, 95% CI 0.35 to 1.15; RD −0.08, 95% CI −0.18 to 0.02). Analysis 1.23.
Death or severe BPD (Outcome 1.24):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 0.93, 95% CI 0.70 to 1.25; RD −0.03, 95% CI −0.17 to 0.10). Analysis 1.24.
Death or grade 3 or 4 IVH (Outcome 1.25):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 1.05, 95% CI 0.65 to 1.68; RD 0.01, 95% CI −0.10 to 0.13). Analysis 1.25.
Death or PVL (Outcome 1.26):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 0.89, 95% CI 0.41 to 1.93; RD −0.01, 95% CI −0.10 to 0.07). Analysis 1.26.
Death or NEC (Outcome 1.27):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 0.97, 95% CI 0.46 to 2.06; RD −0.00, 95% CI −0.09 to 0.08). Analysis 1.27.
Death or sepsis (Outcome 1.28):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 0.79, 95% CI 0.44 to 1.40; RD −0.04, 95% CI −0.15 to 0.06). Analysis 1.28.
Death or ROP (stage not stated) (Outcome 1.29):
This outcome was reported for all 211 randomised infants (Nakamura 2016). There was no significant difference between the two groups (RR 1.05, 95% CI 0.79 to 1.40; RD 0.02, 95% CI −0.11 to 0.16). Analysis 1.29.
Death or neurodevelopmental impairment at 18 months PMA (Outcome 1.30):
This outcome was reported in 187 infants available at follow‐up (Nakamura 2016). There was no significant difference between the two groups (RR 1.09, 95% CI 0.70 to 1.70; RD 0.03, 95% CI −0.10 to 0.16). Analysis 1.30
Death or neurodevelopmental impairment at 3 years of age (Outcome 1.31):
This outcome was reported in 179 infants available at follow‐up (Nakamura 2016). There was no significant difference between the two groups (RR 1.03, 95% CI 0.68 to 1.56; RD 0.01, 95% CI −0.13 to 0.15). Analysis 1.31.
Death or cerebral palsy at 3 years of age (Outcome 1.32):
This outcome was reported in 190 infants available at follow‐up (Nakamura 2016). There was no significant difference between the two groups (RR 1.12, 95% CI 0.64 to 1.96; RD 0.02, 95% CI −0.09 to 0.14). Analysis 1.32.
Early inhaled steroids (< 2 weeks) vs. placebo among survivors (Comparison 2)
Primary outcome
CLD at 36 weeks' PMA (Outcome 2.1):
Six trials enrolling 1088 neonates reported on this outcome among survivors (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002; Bassler 2015). There was a significant difference in the incidence of CLD at 36 weeks' PMA among survivors (typical RR 0.76, 95% CI 0.63 to 0.93; typical RD −0.07, 95% CI −0.13 to −0.02; NNTB 14, 95% CI 8 to 50). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 2.1; Figure 6.
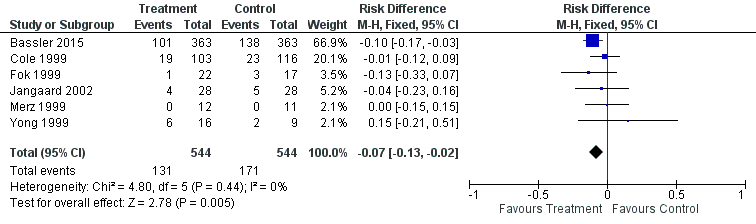
Forest plot of comparison: 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), outcome: 2.1 CLD at 36 weeks' PMA.
Secondary outcomes
CLD at 28 days of age (Outcome 2.2):
Five trials enrolling 380 neonates reported on this outcome (Cole 1999; Fok 1999; Merz 1999; Yong 1999; Jangaard 2002). There was no significant difference in the incidence of CLD at 28 days of age among survivors (typical RR 0.97, 95% CI 0.78 to 1.21; typical RD −0.01, 95% CI −0.11 to 0.08). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). Analysis 2.2.
Cerebral palsy (Outcome 2.3):
One trial enrolling 56 neonates reported on this outcome (Jangaard 2002). There was no significant difference in the incidence of cerebral palsy among survivors (RR 1.33, 95% CI 0.33 to 5.42; RD 0.04, 95% CI −0.14 to 0.21). Tests for heterogeneity were not applicable. Analysis 2.3.
Mean developmental index on BSID‐II < 2 SD of the mean (Outcome 2.4):
One trial enrolling 56 neonates reported on this outcome (Jangaard 2002). There was no significant difference in the incidence of mean developmental index on BSID‐II less than 2 SD of the mean among survivors (RR 1.25, 95% CI 0.37 to 4.17; RD 0.04, 95% CI −0.16 to 0.23). Tests for heterogeneity were not applicable. Analysis 2.4.
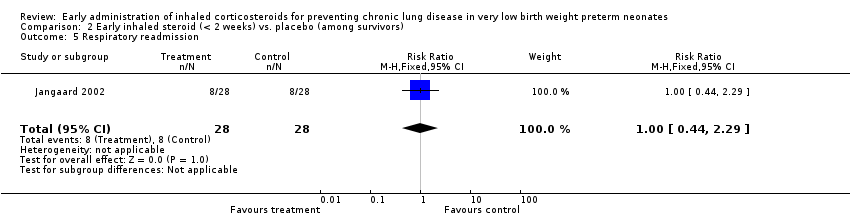
Respiratory readmission (Outcome 2.5):
One trial enrolling 56 neonates reported on this outcome (Jangaard 2002). There was no statistically significant difference in the incidence of respiratory readmission (RR 1.00, 95% CI 0.44 to 2.29; RD 0.00, 95% CI −0.24 to 0.24). Tests for heterogeneity were not applicable. Analysis 2.5.
Additional outcomes
The functioning of the hypothalamic‐pituitary‐adrenal axis in a subset of infants enrolled in the randomised controlled trial by Cole and co‐workers is reported in a separate publication (Cole 1999). Inhaled beclomethasone therapy was associated with a small decrease in the basal cortisol levels. There was no evidence of adrenal suppression as reflected by the response to cosyntropin stimulation. Ng 1993 reported on pituitary‐adrenal suppression in preterm, VLBW infants after inhaled fluticasone propionate treatment. This study evaluated a subset of infants enrolled in the trial of Fok 1999 using the human CRH stimulation test. Basal and post‐stimulation plasma ACTH and serum cortisol concentrations were significantly suppressed in the group receiving inhaled fluticasone when compared to the control group.
No relevant data for the following outcomes were available for analysis: duration of requirement for supplemental oxygen, duration of assisted ventilation, measurements of pulmonary function, growth, hypertrophy of the tongue, hypertrophic obstructive cardiomyopathy and nephrocalcinosis.
Discussion
Summary of main results
This review update identified one additional published trial that previously was listed as an ongoing trial in Europe (Bassler 2015); and one new trial from Japan (Nakamura 2016). Both trials were of high GRADE quality, but Nakamura 2016 reported all outcomes as a combination of death and a complication of preterm birth. We therefore could not include the results in meta‐analyses. Denjean 1998 was moved from excluded to included trials. The study lacks information on most items in the 'Risk of bias' assessment. The review now includes information from 10 trials which have enrolled 1644 infants.
There is now evidence that inhaled steroids are effective in reducing the incidence of death or CLD at 36 weeks' PMA among all randomised infants. There was a significant difference noted for the combined outcome of death by, or CLD at, 36 weeks' PMA (typical RR 0.86, 95% CI 0.75 to 0.99; typical RD −0.06, 95% CI −0.11 to −0.00 (P = 0.04); NNTB 17, 95% CI 9 to infinity). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). In addition there is evidence that inhaled steroids reduce the risk of need for reintubation. Even though there is evidence, the concern is whether this benefit is of any clinical relevance. The NNTB to prevent one infant from developing death or CLD at 36 weeks' PMA is 17 with the upper 95% CI of infinity and therefore not clinically important. Based on this result the use of inhaled steroids in this population cannot be recommended. The long‐term follow‐up results of Bassler 2015 may affect the conclusion of this review.
Among survivors, inhaled steroids are effective in reducing the incidence of CLD at 36 weeks' PMA (typical RR 0.76, 95% CI 0.63 to 0.93; typical RD −0.07, 95% CI −0.13 to −0.02 (P = 0.005); NNTB 14, 95% CI 8 to 15). There was no statistically significant heterogeneity for this outcome (RR I² = 0%; RD I² = 0%). In one trial enrolling 56 neonates, no significant difference in the incidence of cerebral palsy was noted.
A major concern with studies of inhalation therapy in neonates is the uncertainty regarding drug delivery and deposition in the peripheral airways. Numerous factors affect drug delivery and deposition including the number of particles in the respirable range, the delivery technique (use of MDI in combination with a spacer or face mask and nebuliser (ultrasonic or jet)) and the presence or absence of an endotracheal tube. Previous workers have shown that the amount of aerosol delivery varies from 0.4% to 14% based on the technique used (Arnon 1992; Grigg 1992; O'Callaghan 1992). Delivery technique, type of inhaled steroid and dosage used varied among the studies included in this review, making the interpretation of aggregate data difficult.
In conclusion, there is now some evidence from this systematic review that inhaled steroids reduce the incidence of death or CLD at 36 weeks' PMA amongst all randomised but the evidence is not of clinical relevance.
Studies are needed to examine the effect of different delivery techniques and dosing schedules for the administration of these medications. It is possible that, with improved and/or more consistent delivery of inhaled steroids to the target organ, an important therapeutic effect will be demonstrated. Long‐term outcomes are awaited from the trial by Bassler 2015.
Overall completeness and applicability of evidence
By 2016 a total of 1644 infants have been enrolled in trials testing the effectiveness of early administration of inhaled steroids. There is now moderate GRADE evidence that early administration of inhaled steroids reduces the incidence of death or CLD at 36 weeks' PMA among all randomised infants and among survivors only, but the significance is not clinically relevant. In addition there is evidence that inhaled steroids reduces the risk of need for reintubation.
Quality of the evidence
According to GRADE the quality of evidence was moderate for the outcomes of chronic lung disease at 36 weeks' PMA and death and CLD at 36 weeks' PMA amongst all randomised and amongst survivors. There was serious risk of bias, with method of sequence generation being unclear in all included studies except for Bassler 2015. In Denjean 1998, Fok 1999, Jangaard 2002, Merz 1999 and Yong 1999 blinding of outcome assessment was unclear. Except for the study by Bassler 2015, none of the included studies were registered and we were unable to identify whether there was selective reporting or not. There was no evidence to support inconsistency, imprecision or indirectness among the included studies.
Potential biases in the review process
We are not aware of any potential bias in our review process.
Agreements and disagreements with other studies or reviews
Of the included studies in this review, only the study by Bassler 2015 showed a reduction in CLD at 36 weeks' PMA amongst survivors. No difference was noted for the outcome of CLD at 36 weeks' PMA amongst all randomised infants. The inclusion of the trial by Bassler 2015 for the combined outcome of death and CLD at 36 weeks' PMA amongst all randomised was significant; however the CI is close to 1 and of questionable clinical relevance. In a systematic review published by Beam and colleagues the authors concluded that inhaled steroids were ineffective in preventing bronchopulmonary dysplasia (Beam 2014). This review was completed before the publication by Bassler 2015. In an editorial regarding the Bassler 2015 study Schmidt concluded that "Uncertainty prevails with respect to the use of early inhaled glucocorticosteroids to prevent bronchopulmonary dysplasia in extremely preterm infants" (Schmidt 2015). In contrast in an editorial to the excluded study by Yeh 2016, Bancalari and Jobe concluded: "If the striking pulmonary benefits with absent detrimental effects described by Yeh and colleagues are replicated in large randomised controlled trials done in different clinical setting, this could very well become a 'magic bullet' in the prevention of BPD" (Bancalari 2016). We excluded the study by Yeh 2016, as the intervention was a combination of intratracheal steroids and surfactant.
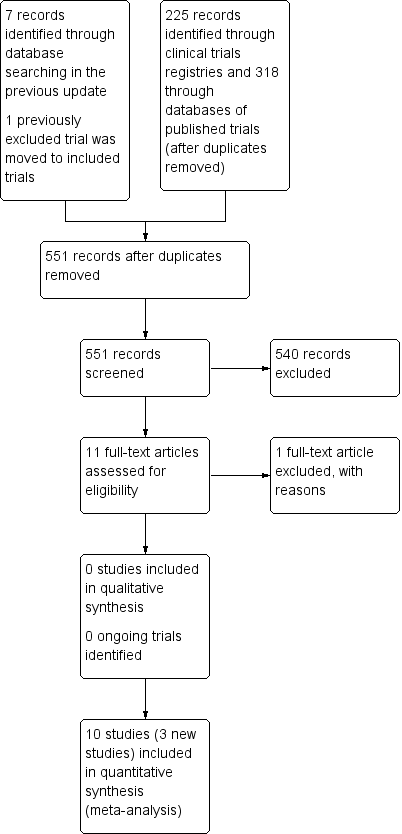
Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
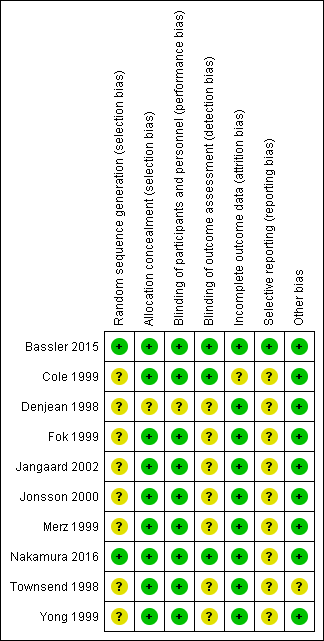
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), outcome: 1.1 CLD at 36 weeks' PMA.

Forest plot of comparison: 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), outcome: 1.6 Death by or CLD at 36 weeks' PMA.

Forest plot of comparison: 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), outcome: 2.1 CLD at 36 weeks' PMA.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 1 CLD at 36 weeks PMA.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 2 CLD at 28 days of age.
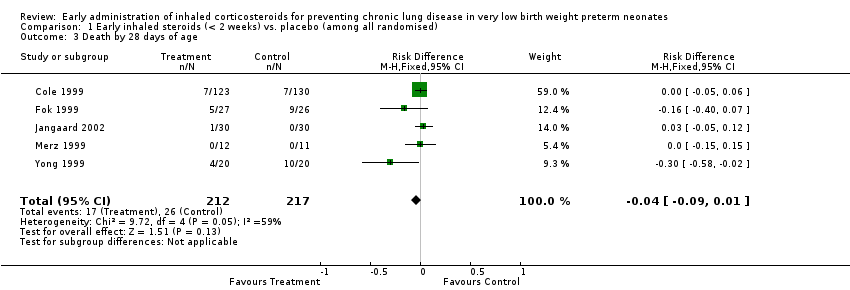
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 3 Death by 28 days of age.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 4 Death by 36 weeks PMA.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 5 Death by or CLD at 28 days of age.
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 6 Death by or CLD at 36 weeks PMA.
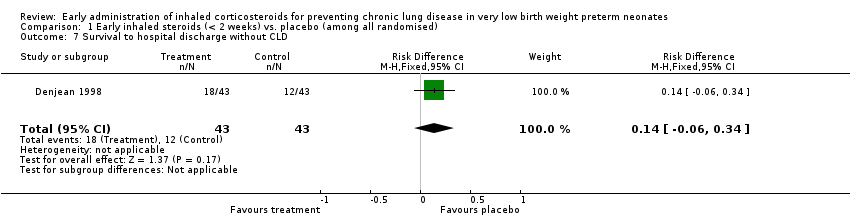
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 7 Survival to hospital discharge without CLD.
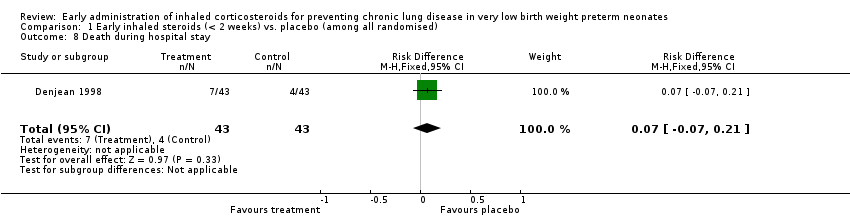
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 8 Death during hospital stay.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 9 Culture proven infection during hospital stay.
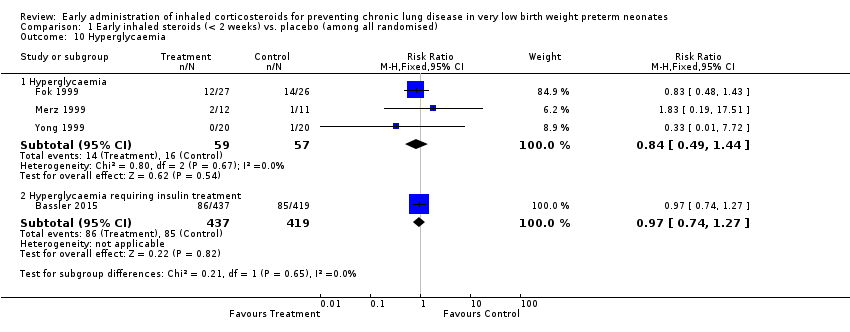
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 10 Hyperglycaemia.
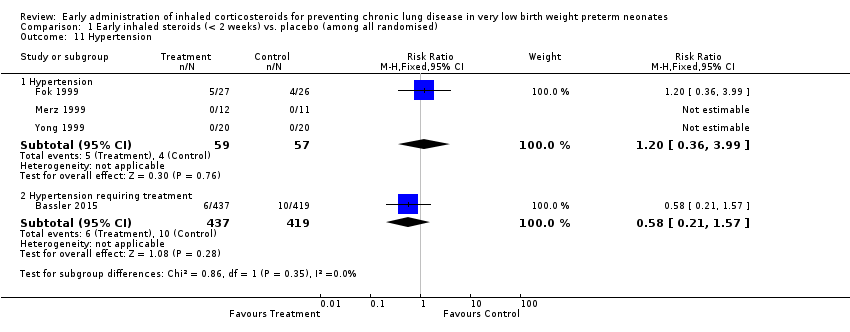
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 11 Hypertension.
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 12 Gastrointesinal bleeding.
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 13 Cataract.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 14 Intraventricular haemorrhage.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 15 Periventricular leukomalacia.
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 16 Brain injury.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 17 Necrotizing enterocolitis.
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 18 Retinopathy of prematurity (any stage).

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 19 Patent ductus arteriosus.
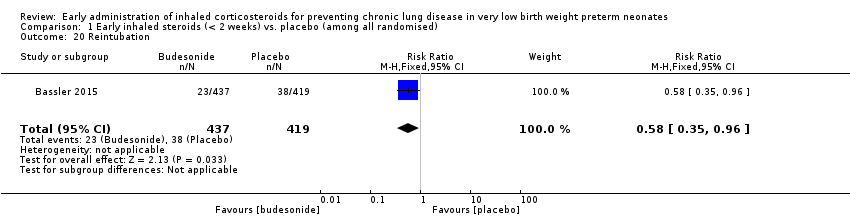
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 20 Reintubation.
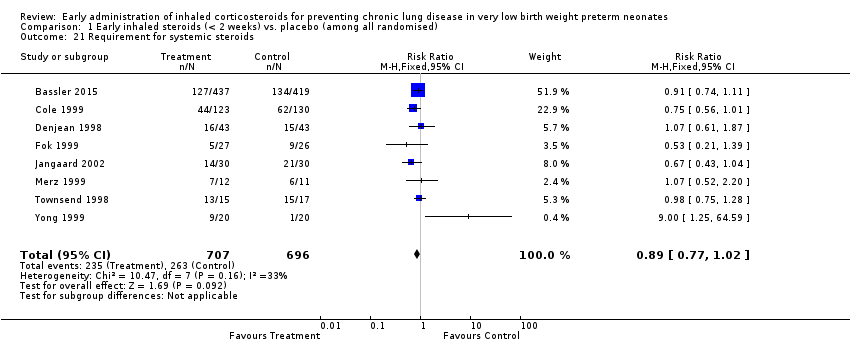
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 21 Requirement for systemic steroids.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 22 Failure to extubate within 14 days.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 23 Death or oxygen dependency at discharge.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 24 Death or severe BPD.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 25 Death or grade 3 or 4 IVH.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 26 Death or PVL.
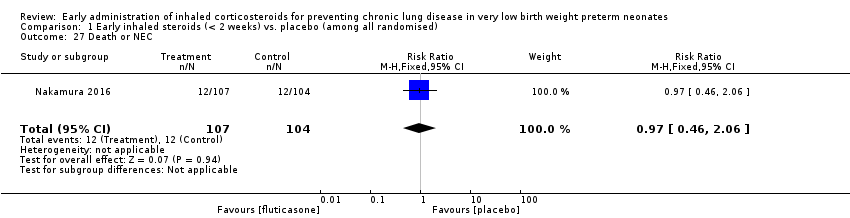
Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 27 Death or NEC.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 28 Death or sepsis.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 29 Death or ROP (stage not stated).

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 30 Death or neurodevelopmental impairment at 18 months PMA.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 31 Death or neurodevelopmental impairment at 3 years of age.

Comparison 1 Early inhaled steroids (< 2 weeks) vs. placebo (among all randomised), Outcome 32 Death or cerebral palsy at 3 years of age.

Comparison 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), Outcome 1 CLD at 36 weeks PMA.

Comparison 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), Outcome 2 CLD at 28 days of age.

Comparison 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), Outcome 3 Cerebral palsy.
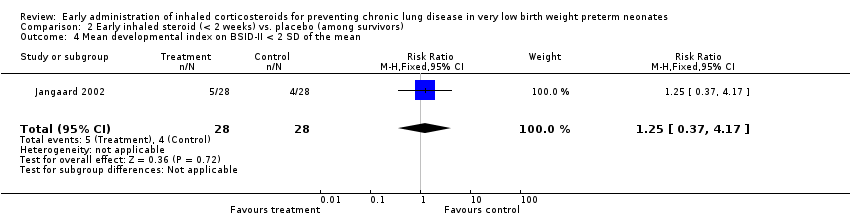
Comparison 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), Outcome 4 Mean developmental index on BSID‐II < 2 SD of the mean.
Comparison 2 Early inhaled steroid (< 2 weeks) vs. placebo (among survivors), Outcome 5 Respiratory readmission.
| Early inhaled steroids (< 2 weeks) compared to placebo (among all randomised) for preventing chronic lung disease in very low birth weight preterm neonates | ||||||
| Patient or population: very low birth weight preterm neonates | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo (among all randomised) | Early inhaled steroids (< 2 weeks) | |||||
| CLD at 36 weeks' PMA | Study population | RR 0.97 | 429 | ⊕⊕⊕⊝ | ||
| 152 per 1000 | 148 per 1000 | |||||
| Moderate | ||||||
| 115 per 1000 | 112 per 1000 | |||||
| Death by, or CLD at, 36 weeks' PMA | Study population | RR 0.86 | 1285 | ⊕⊕⊕⊝ | ||
| 403 per 1000 | 346 per 1000 | |||||
| Moderate | ||||||
| 350 per 1000 | 301 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Method of sequence generation was unclear in all included studies except for the study by Bassler 2015. In the studies by Fok 1999, Jangaard 2002, Merz 1999 and Yong 1999 blinding of outcome assessment was unclear. Except for the study by Bassler 2015, none of the included studies were registered and we were unable to identify whether there was selective reporting or not. | ||||||
| Early inhaled steroid (< 2 weeks) compared to placebo (among survivors) for preventing chronic lung disease in very low birth weight preterm neonates | ||||||
| Patient or population: Very low birth weight preterm neonates | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo (among survivors) | Early inhaled steroid (< 2 weeks) | |||||
| CLD at 36 weeks' PMA | Study population | RR 0.76 | 1088 | ⊕⊕⊕⊝ | ||
| 314 per 1000 | 239 per 1000 | |||||
| Moderate | ||||||
| 188 per 1000 | 143 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 CLD at 36 weeks PMA Show forest plot | 5 | 429 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.62, 1.52] |
| 2 CLD at 28 days of age Show forest plot | 5 | 429 | Risk Difference (M‐H, Random, 95% CI) | 0.03 [‐0.08, 0.14] |
| 3 Death by 28 days of age Show forest plot | 5 | 429 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.09, 0.01] |
| 4 Death by 36 weeks PMA Show forest plot | 6 | 1285 | Risk Difference (M‐H, Fixed, 95% CI) | 0.01 [‐0.03, 0.05] |
| 5 Death by or CLD at 28 days of age Show forest plot | 5 | 429 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.11, 0.07] |
| 6 Death by or CLD at 36 weeks PMA Show forest plot | 6 | 1285 | Risk Ratio (M‐H, Fixed, 99% CI) | 0.86 [0.75, 0.99] |
| 7 Survival to hospital discharge without CLD Show forest plot | 1 | 86 | Risk Difference (M‐H, Fixed, 95% CI) | 0.14 [‐0.06, 0.34] |
| 8 Death during hospital stay Show forest plot | 1 | 86 | Risk Difference (M‐H, Fixed, 95% CI) | 0.07 [‐0.07, 0.21] |
| 9 Culture proven infection during hospital stay Show forest plot | 6 | 1121 | Risk Difference (M‐H, Fixed, 95% CI) | 0.05 [‐0.00, 0.11] |
| 9.1 Positive blood or CSF culture | 2 | 896 | Risk Difference (M‐H, Fixed, 95% CI) | 0.05 [‐0.01, 0.11] |
| 9.2 Positive blood culture | 4 | 225 | Risk Difference (M‐H, Fixed, 95% CI) | 0.05 [‐0.06, 0.16] |
| 10 Hyperglycaemia Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Hyperglycaemia | 3 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.49, 1.44] |
| 10.2 Hyperglycaemia requiring insulin treatment | 1 | 856 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.74, 1.27] |
| 11 Hypertension Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Hypertension | 3 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.36, 3.99] |
| 11.2 Hypertension requiring treatment | 1 | 856 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.21, 1.57] |
| 12 Gastrointesinal bleeding Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.34] |
| 13 Cataract Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.56] |
| 14 Intraventricular haemorrhage Show forest plot | 2 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.77, 1.41] |
| 15 Periventricular leukomalacia Show forest plot | 2 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.59, 3.46] |
| 16 Brain injury Show forest plot | 1 | 838 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.94, 1.65] |
| 17 Necrotizing enterocolitis Show forest plot | 3 | 1162 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.68, 1.24] |
| 18 Retinopathy of prematurity (any stage) Show forest plot | 3 | 1030 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.93, 1.21] |
| 19 Patent ductus arteriosus Show forest plot | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.57, 1.17] |
| 20 Reintubation Show forest plot | 1 | 856 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.35, 0.96] |
| 21 Requirement for systemic steroids Show forest plot | 8 | 1403 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.77, 1.02] |
| 22 Failure to extubate within 14 days Show forest plot | 5 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.76, 1.24] |
| 23 Death or oxygen dependency at discharge Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.35, 1.15] |
| 24 Death or severe BPD Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.25] |
| 25 Death or grade 3 or 4 IVH Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.65, 1.68] |
| 26 Death or PVL Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.41, 1.93] |
| 27 Death or NEC Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.46, 2.06] |
| 28 Death or sepsis Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.44, 1.40] |
| 29 Death or ROP (stage not stated) Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.79, 1.40] |
| 30 Death or neurodevelopmental impairment at 18 months PMA Show forest plot | 1 | 187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.70, 1.70] |
| 31 Death or neurodevelopmental impairment at 3 years of age Show forest plot | 1 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.68, 1.56] |
| 32 Death or cerebral palsy at 3 years of age Show forest plot | 1 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.64, 1.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 CLD at 36 weeks PMA Show forest plot | 6 | 1088 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.07 [‐0.13, ‐0.02] |
| 2 CLD at 28 days of age Show forest plot | 5 | 380 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.78, 1.21] |
| 3 Cerebral palsy Show forest plot | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.33, 5.42] |
| 4 Mean developmental index on BSID‐II < 2 SD of the mean Show forest plot | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.37, 4.17] |
| 5 Respiratory readmission Show forest plot | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.44, 2.29] |

