Monoterapia con carbamazepina versus fenobarbitona para la epilepsia: una revisión de datos de participantes individuales
Resumen
Antecedentes
Esta es una versión actualizada de la revisión Cochrane publicada anteriormente en 2016. Esta revisión es una de una serie de revisiones Cochrane que estudia las comparaciones por pares de monoterapias.
La epilepsia es una afección neurológica frecuente en la que descargas eléctricas anormales del cerebro provocan convulsiones espontáneas recurrentes. Se considera que con un tratamiento farmacológico eficaz, hasta el 70% de los pacientes con epilepsia activa tienen la posibilidad de estar libres de convulsiones y entrar en remisión durante un largo plazo poco después de iniciar el tratamiento farmacológico con un solo fármaco antiepiléptico como monoterapia.
En todo el mundo, la carbamazepina y la fenobarbitona son fármacos antiepilépticos de amplio espectro de uso común, adecuados para la mayoría de los tipos de crisis epilépticas. La carbamazepina es un tratamiento actual de primera línea para las convulsiones de inicio focal, y se utiliza en los Estados Unidos y Europa. La fenobarbitona ya no se considera un tratamiento de primera línea debido a la preocupación por los efectos adversos asociados, en particular, los efectos adversos de comportamiento documentados en los niños tratados con el fármaco. Sin embargo, la fenobarbitona se sigue utilizando comúnmente en los países de ingresos bajos y medios debido a su bajo coste. No se han encontrado diferencias consistentes en la eficacia entre la carbamazepina y la fenobarbitona en ensayos individuales; sin embargo, los intervalos de confianza generados por estos ensayos son amplios y, por lo tanto, la síntesis de los datos de los ensayos individuales puede mostrar diferencias en la eficacia.
Objetivos
Revisar el tiempo transcurrido hasta el fracaso del tratamiento, la remisión y la primera convulsión con carbamazepina comparada con fenobarbitona cuando se utilizan como monoterapia en pacientes con convulsiones de inicio focal (focal simple o compleja y secundariamente generalizada), o convulsiones tónico‐clónicas de inicio generalizado (con o sin otros tipos de convulsiones generalizadas).
Métodos de búsqueda
Para la última actualización, se realizaron búsquedas en las siguientes bases de datos el 24 de mato de 2018: el Registro Cochrane de Estudios (Cochrane Register of Studies, CRS Web), que incluye el Registro Especializado del Grupo Cochrane de Epilepsia (Cochrane Epilepsy's Specialized Register) y el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL); MEDLINE; el National Institutes of Health Ongoing Trials Register de los EE.UU. (ClinicalTrials.gov) y la World Health Organization International Clinical Trials Registry Platform (ICTRP). Se hicieron búsquedas manuales en revistas relevantes y se estableció contacto con compañías farmacéuticas, investigadores de ensayos originales y expertos en el tema.
Criterios de selección
Ensayos controlados aleatorizados que compararon la monoterapia con carbamazepina o fenobarbitona en niños o adultos con convulsiones de inicio focal o convulsiones tónico‐clónicas de inicio generalizado.
Obtención y análisis de los datos
Ésta fue una revisión de datos de pacientes individuales (DPI). El resultado primario fue el tiempo al fracaso del tratamiento. Los resultados secundarios fueron el tiempo hasta la primera convulsión después de la asignación al azar, el tiempo hasta la remisión de seis meses, el tiempo hasta la remisión de 12 meses y la incidencia de eventos adversos. Se utilizaron los modelos de regresión de riesgos proporcionales de Cox para obtener las estimaciones específicas de los ensayos de los cocientes de riesgos instantáneos (CRI) con intervalos de confianza (IC) del 95% mediante el método de la varianza inversa genérica para obtener los CRI y los IC del 95% agrupados generales.
Resultados principales
Se incluyeron 13 ensayos en esta revisión y se dispuso de DPI para 836 individuos de los 1455 individuos elegibles de seis ensayos, el 57% de los datos potenciales. Para los resultados de remisión, un CRI inferior a 1 indica una ventaja para la fenobarbitona y para los resultados de la primera convulsión y el fracaso del tratamiento un CRI inferior a 1 indica una ventaja para la carbamazepina.
Los resultados primarios de la revisión fueron: tiempo transcurrido hasta el fracaso del tratamiento por cualquier motivo relacionado con el tratamiento (CRI agrupado ajustado según el tipo de convulsión para 676 participantes): 0,66, IC del 95% 0,50 a 0,86, evidencia de calidad moderada), el tiempo transcurrido hasta el fracaso del tratamiento debido a los eventos adversos (CRI agrupado ajustado por el tipo de convulsiones para 619 participantes: 0,69, IC del 95% 0,49 a 0,97, evidencia de baja calidad), el tiempo transcurrido hasta el fracaso del tratamiento debido a la falta de eficacia (CRI combinado ajustado por el tipo de convulsiones para 487 participantes: 0,54, IC 95% 0,38 a 0,78, evidencia de calidad moderada), mostrando una ventaja estadísticamente significativa para la carbamazepina en comparación con la fenobarbitona.
Para los resultados secundarios, no se encontraron diferencias estadísticamente significativas entre la carbamazepina y la fenobarbitona: tiempo hasta la primera convulsión después de la asignación al azar (CRI agrupado ajustado por el tipo de convulsión para 822 participantes: 1,13, IC del 95% 0,93 a 1,38, evidencia de calidad moderada), tiempo de remisión de 12 meses (CRI combinado ajustado por tipo de convulsiones para 683 participantes: 1,09, IC del 95% 0,84 a 1,40, evidencia de baja calidad), y el tiempo hasta la remisión a seis meses de los CRI combinados ajustados por el tipo de convulsiones para 683 participantes: 1,01, 95% CI 0,81 a 1,24, evidencia de baja calidad).
Los resultados de estos resultados secundarios sugieren que puede haber una asociación entre el efecto del tratamiento en términos de eficacia y el tipo de convulsiones; es decir, que los participantes con convulsiones de inicio focal experimentan una recurrencia de las convulsiones más tarde y, por lo tanto, la remisión de las convulsiones antes con la fenobarbitona que con la carbamazepina, y viceversa para los individuos con convulsiones generalizadas. Es probable que los análisis de estos resultados se hayan visto confundidos por varias cuestiones metodológicas y la clasificación errónea del tipo de convulsiones, que podrían haber introducido la heterogeneidad y el sesgo en los resultados de esta revisión.
Se disponía de información limitada con respecto a los eventos adversos en los ensayos y no se pudieron comparar las tasas de eventos adversos entre la carbamazepina y la fenobarbitona. Algunos eventos adversos informados sobre ambos fármacos fueron dolor abdominal, náuseas y vómitos, somnolencia, trastornos motores y cognitivos, efectos secundarios dismórficos (como erupción cutánea) y efectos secundarios conductuales en tres ensayos pediátricos.
Conclusiones de los autores
La evidencia de calidad moderada de esta revisión indica que es probable que la carbamazepina sea un fármaco más efectivo que la fenobarbitona en lo que respecta a la retención del tratamiento (fracasos del tratamiento debido a la falta de eficacia o a eventos adversos o a ambos). La evidencia de calidad moderada a baja de esta revisión también sugiere una asociación entre la eficacia del tratamiento y el tipo de convulsiones en cuanto a la recurrencia y la remisión de las convulsiones, con una ventaja para la fenobarbitona en el caso de las convulsiones de comienzo focal y una ventaja para la carbamazepina en el caso de las convulsiones de comienzo generalizado.
Sin embargo, algunos de los ensayos que contribuyeron a los análisis tenían insuficiencias e inconsistencias metodológicas que pueden haber repercutido en los resultados de esta revisión. Por lo tanto, no se indica que los resultados de esta revisión por sí solos constituyan la base de la elección del tratamiento de un paciente con convulsiones de aparición reciente. Se recomienda que los ensayos futuros se diseñen con la mayor calidad posible, teniendo en cuenta el enmascaramiento, la elección de la población, la clasificación del tipo de convulsión, la duración del seguimiento, la elección de los resultados y el análisis, y la presentación de los resultados.
PICO
Resumen en términos sencillos
Monoterapia con carbamazepina versus fenobarbitona (tratamiento con un solo fármaco) para la epilepsia
Esta es una actualización de una revisión Cochrane publicada previamente en el número 12, 2016, de la Base de Datos Cochrane de Revisiones Sistemáticas (Cochrane Database of Systematic Reviews).
Antecedentes
La epilepsia es un trastorno neurológico frecuente en el que las descargas eléctricas anormales en el cerebro provocan convulsiones recurrentes. En esta revisión, se estudiaron dos tipos de crisis epilépticas: las convulsiones de inicio generalizado, en las que las descargas eléctricas comienzan en una parte del cerebro y se desplazan por todo el cerebro; y las convulsiones de inicio focal, en las que las convulsiones se generan en una parte del cerebro y afectan a una parte de éste (todo el hemisferio cerebral o parte de un lóbulo del cerebro). Las convulsiones focales se pueden generalizar (generalización secundaria) y desplazarse desde una parte del cerebro a través de todo el cerebro. En aproximadamente el 70% de los pacientes con epilepsia, un solo fármaco antiepiléptico puede controlar las convulsiones generalizadas o focales.
Esta revisión se aplica a los pacientes con convulsiones focales (con o sin generalización secundaria) y a los pacientes con convulsiones tónico‐clónicas generalizadas, un tipo específico de convulsiones generalizadas. Esta revisión no se aplica a los pacientes con otros tipos de convulsiones generalizadas, como las convulsiones de ausencia o las convulsiones mioclónicas, ya que los tratamientos recomendados para estos tipos de convulsiones son diferentes.
En todo el mundo, la fenobarbitona y la carbamazepina se utilizan comúnmente como fármacos antiepilépticos; sin embargo, la carbamazepina se utiliza más comúnmente en los Estados Unidos y Europa debido a la preocupación por los efectos secundarios asociados a la fenobarbitona, en particular, la preocupación por los cambios de comportamiento en los niños tratados con fenobarbitona. La fenobarbitona se sigue utilizando comúnmente en los países de ingresos bajos y medios de África, Asia y América del Sur debido al bajo costo del fármaco.
Objetivo
El objetivo de esta revisión fue comparar la efectividad de estos fármacos para controlar las convulsiones, determinar si se asocian con efectos secundarios que puedan provocar la interrupción de la medicación e informar sobre la elección entre estos fármacos.
Métodos
La última búsqueda de ensayos fue en mayo de 2018. Se evaluó la evidencia de 13 ensayos clínicos en los que los pacientes recibieron carbamazepina o fenobarbitona y su tratamiento se decidió de forma aleatoria. Se pudieron combinar los datos de 836 pacientes de seis de los 13 ensayos; para los 619 pacientes restantes de siete ensayos, no se disponía de datos para utilizar en esta revisión.
Resultados clave
Los resultados de la revisión indican que es probable que los pacientes dejen de tomar el tratamiento con fenobarbitona antes que el tratamiento con carbamazepina, debido a la recurrencia de las convulsiones, a los efectos secundarios del fármaco o a ambos. Los resultados también sugieren que la recurrencia de las convulsiones después de iniciar el tratamiento con fenobarbitona puede ocurrir más tarde que el tratamiento con carbamazepina (y, por lo tanto, un período libre de convulsiones de seis o 12 meses puede ocurrir antes con la fenobarbitona que con la carbamazepina) en el caso de los pacientes con convulsiones de comienzo focal, y viceversa en el caso de los pacientes con convulsiones de comienzo generalizado.
Algunos efectos secundarios informados por los pacientes que recibieron carbamazepina y los pacientes que recibieron fenobarbitona fueron dolor abdominal, náuseas, vómitos, cansancio, problemas motores (como coordinación deficiente), problemas cognitivos (mala memoria), erupciones cutáneas y otros problemas cutáneos. En tres ensayos realizados con niños, se informó de efectos secundarios de comportamiento como la agresión, con ambos fármacos.
Calidad de la evidencia
Algunos de los ensayos que contribuyeron con datos a la revisión tuvieron problemas metodológicos, que pueden haber introducido sesgos y resultados inconsistentes en esta revisión, y algunos pacientes mayores de 30 años con convulsiones de inicio generalizado recién diagnosticados pueden haber tenido un diagnóstico erróneo de su tipo de convulsión. Estos problemas pueden haber afectado los resultados de esta revisión y se consideró que la calidad de la evidencia proporcionada por esta revisión es de calidad moderada a baja . No se recomienda utilizar solo los resultados de esta revisión para elegir entre la carbamazepina o la fenobarbitona para el tratamiento de la epilepsia. Se recomienda que todos los ensayos futuros que comparen estos fármacos o cualquier otro antiepiléptico se diseñen utilizando métodos de alta calidad para asegurar que los resultados sean también de alta calidad.
Authors' conclusions
Summary of findings
| Carbamazepine compared with phenobarbitone for epilepsy (time to treatment failure) | ||||||
| Patient or population: adults and children with newly onset focal or generalised epilepsy Settings: outpatients Intervention: carbamazepine Comparison: phenobarbitone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Phenobarbitone | Carbamazepine | |||||
| Time to treatment failure (any reason related to treatment) All participants Range of follow‐up: 0 to 4653 days | The median time to treatment failure was 1059 days in the phenobarbitone group | The median time to treatment failure was 2717 days (1658 days longer) in the carbamazepine group | HR 0.66 (0.50 to 0.86)a | 676 (4 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine. Treatment failure due to adverse events (HR 0.69, 95% CI 0.49 to 0.97, P = 0.03, I² = 55%), and due to lack of efficacy (HR 0.54, 95% CI 0.38 to 0.78, P = 0.0008, I² = 0%), also occurred significantly earlier on phenobarbitone compared to carbamazepine. |
| Time to treatment failure (any reason related to treatment) Subgroup: focal onset seizures Range of follow‐up: 0 to 4272 days | The median time to treatment failure was 913 days in the phenobarbitone group | The median time to treatment failure was 2422 days (1509 days longer) in the carbamazepine group | HR 0.66 (0.49 to 0.88) | 520 (4 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine. Treatment failure due to adverse events (HR 0.67, 95% CI 0.46 to 0.96, P = 0.03, I² = 70%), and due to lack of efficacy (HR 0.54, 95% CI 0.36 to 0.80, P = 0.002, I² = 0%), also occurred significantly earlier on phenobarbitone compared to carbamazepine. |
| Time to treatment failure (any reason related to treatment) Subgroup: generalised onset tonic‐clonic seizures Range of follow‐up: 0 to 4653 days | The 25th percentiled of time to treatment failure was 605 days in the phenobarbitone group | The 25th percentiled of time to treatment failure was 825 days (220 days longer) in the carbamazepine group | HR 0.65 (0.35 to 1.23) | 156 | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine. There was also no statistically significant difference between drugs in treatment failure due to adverse events (HR 0.84, 95% CI 0.35 to 2.00, P = 0.69, I² = 0%), or treatment failure due to lack of efficacy: HR 0.56 (95% CI 0.23 to 1.35, P = 0.20, I² = 0%). |
| *Illustrative risks in the carbamazepine and phenobarbitone groups are calculated at the median time to treatment failure (i.e. the time to 50% of participants failing or withdrawing from allocated treatment) within each group across all trials. The relative effect (pooled hazard ratio) shows the comparison of 'time to treatment failure' between the treatment groups. CI: 95% confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| aPooled HR for all participants adjusted for seizure type. | ||||||
| Carbamazepine compared with phenobarbitone for epilepsy (secondary outcomes) | ||||||
| Patient or population: adults and children with newly onset focal or generalised epilepsy Settings: outpatients Intervention: carbamazepine Comparison: phenobarbitone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Phenobarbitone | Carbamazepine | |||||
| Time to first seizure (post‐randomisation) All participants Range of follow‐up: 0 to 4108 days | The median time to first seizure post‐randomisation was 218 days in the phenobarbitone group | The median time to first seizure post‐randomisation was 113 days (105 days shorter) in the carbamazepine group | HR 1.13 (0.93 to 1.38)a | 822 (6 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine |
| Time to first seizure (post‐randomisation) Subgroup: focal onset seizures Range of follow‐up: 0 to 4108 days | The median time to first seizure post‐randomisation was 266 days in the phenobarbitone group | The median time to first seizure post‐randomisation was 84 days (182 days shorter) in the carbamazepine group | HR 1.31 (1.04 to 1.66) | 584 (6 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine |
| Time to first seizure (post‐randomisation) Subgroup: generalised onset tonic‐clonic seizures Range of follow‐up: 0 to 4070 days | The median time to first seizure post‐randomisation was 209 days in the phenobarbitone group | The median time to first seizure post‐randomisation was 303 days (94 days longer) in the carbamazepine group | HR 0.80 (0.55 to 1.15) | 238 (5 trials) | ⊕⊕⊝⊝ | HR < 1 indicates a clinical advantage for carbamazepine |
| Time to achieve 12‐month remission (seizure‐free period) All participants Range of follow‐up: 0 to 4222 days | The median time to achieve to 12‐month remission was 413 days in the phenobarbitone group | The median time to achieve to 12‐month remission was 446 days (33 days longer) in the carbamazepine group | HR 1.09 (0.84 to 1.40)a | 683 | ⊕⊕⊝⊝ | HR < 1 indicates a |
| Time to achieve 12‐month remission (seizure‐free period) Subgroup: focal onset seizures Range of follow‐up: 0 to 4222 days | The median time to achieve to 12‐month remission was 369 days in the phenobarbitone group | The median time to achieve to 12‐month remission was 531 days (162 days longer) in the carbamazepine group | HR 0.92 (0.67 to 1.25) | 525 | ⊕⊕⊝⊝ | HR < 1 indicates a |
| Time to achieve 12‐month remission (seizure‐free period) Subgroup: generalised onset tonic‐clonic seizures Range of follow‐up: 0 to 4163 days | The median time to achieve to 12‐month remission was 421 days in the phenobarbitone group | The median time to achieve to 12‐month remission was 366 days (55 days shorter) in the carbamazepine group | HR 1.56 (0.99 to 2.44) | 158 | ⊕⊕⊝⊝ | HR < 1 indicates a |
| *Illustrative risks in the carbamazepine and phenobarbitone groups are calculated at the median time to first seizure or time to 12‐month remission (i.e. the time to 50% of participants experiencing a first seizure or 12‐months of remission) within each group across all trials. The relative effect (pooled hazard ratio) shows the comparison of 'time to first seizure' or 'time to 12‐month remission' between the treatment groups. CI: 95% confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| aPooled HR for all participants adjusted for seizure type. | ||||||
Background
This is an updated version of the Cochrane Review previously published in Issue 12, 2016 of the Cochrane Database of Systematic Reviews (Nolan 2016a).
Description of the condition
Epilepsy is a common neurological condition in which abnormal electrical discharges from the brain cause recurrent unprovoked seizures. Epilepsy is a disorder of many heterogenous seizure types, with an estimated incidence of 33 to 57 per 100,000 person‐years worldwide (Annegers 1999; Hirtz 2007; MacDonald 2000; Olafsson 2005; Sander 1996), accounting for approximately 1% of the global burden of disease (Murray 1994).
The lifetime risk of epilepsy onset is estimated to be 1300 to 4000 per 100,000 person‐years (Hauser 1993; Juul‐Jenson 1983), and the lifetime prevalence could be as large as 70 million people worldwide (Ngugi 2010). It is believed that with effective drug treatment, up to 70% of individuals with active epilepsy have the potential to go into long‐term remission shortly after starting drug therapy (Cockerell 1995; Hauser 1993; Sander 2004), and around 70% of individuals can achieve seizure freedom using a single antiepileptic drug in monotherapy (Cockerell 1995). Current National Institute for Health and Care Excellence (NICE), guidelines recommend that both adults and children with epilepsy should be treated with monotherapy, wherever possible (NICE 2012). The remaining 30% of individuals experience refractory or drug‐resistant seizures, which often require treatment with combinations of antiepileptic drugs or alternative treatments, such as epilepsy surgery (Kwan 2000).
We studied two seizure types in this review: generalised onset seizures, in which electrical discharges begin in one part of the brain and move throughout the brain, and focal onset seizures, in which the seizure is generated in and affects one part of the brain (the whole hemisphere of the brain or part of a lobe of the brain).
Description of the intervention
Carbamazepine and phenobarbitone are among the most commonly used and earliest drugs licensed for the treatment of epileptic seizures; phenobarbitone has been used as monotherapy for focal seizures and generalised tonic‐clonic seizures for over 50 years (Gruber 1962), and carbamazepine, for over 30 years (Shakir 1980). Current NICE guidelines for adults and children recommend carbamazepine as a first‐line treatment for focal onset seizures and as a second‐line treatment for generalised tonic‐clonic seizures if first‐line treatments, sodium valproate and lamotrigine, are deemed unsuitable (NICE 2012). However, there is evidence that carbamazepine may exacerbate some other generalised seizure types, such as myoclonic and absence seizures (Liporace 1994; Shields 1983; Snead 1985).
Phenobarbitone is no longer considered a first‐line treatment in the USA and most of Europe because of concerns over short‐ and long‐term tolerability (Wallace 1997); particularly in children, there is concern about behavioural disturbance caused by phenobarbitone (Trimble 1988). One open‐label paediatric trial in the UK, de Silva 1996, withdrew the phenobarbitone arm of the trial because of concerns about behavioural problems and difficulties getting paediatricians to randomise individuals. However, the largest reported randomised controlled trial (RCT), investigating phenobarbitone as monotherapy in adults with focal seizures, Mattson 1985, did not find phenobarbitone to be more associated with adverse events than other trial drugs (carbamazepine, phenytoin, and primidone). In fact, phenobarbitone was significantly associated with the lowest incidence of motor disturbances (ataxia (lack of voluntary co‐ordination of muscle movements), incoordination, nystagmus, and tremor), and gastrointestinal problems.
Phenobarbitone is still used as a first‐line drug in low‐ and middle‐income countries (Banu 2007; Ogunrin 2005; Pal 1998). Two paediatric trials conducted in Bangladesh (Banu 2007), and rural India (Pal 1998), comparing phenobarbitone with carbamazepine and phenytoin, respectively, found no excess in behavioural side‐effects from phenobarbitone, but a trial in Nigerian adults (Ogunrin 2005), showed evidence of an association between phenobarbitone and worsening of cognitive impairments, particularly memory deficits.
Both carbamazepine and phenobarbitone have been shown to have teratogenic (disturbances to foetal development), effects (Bromley 2014; Weston 2016), where the risk is estimated to be two to three times that of the general population (Meador 2008; Morrow 2006); carbamazepine is associated particularly with neural tube defects (Matlow 2012), and has also been shown to be associated with negative neurodevelopmental outcomes, such as a lower developmental quotient compared to children born to women without epilepsy (Bromley 2014). Phenobarbitone is associated with low folic acid levels and megaloblastic anaemia (anaemia characterised by many large immature and dysfunctional red blood cells; Meador 2008). In addition to concerns over behavioural and cognitive adverse events, phenobarbitone is commonly associated with somnolence (sedation), and connective tissue abnormalities, such as Dupuytren's contracture and frozen shoulder (Baulac 2002), and exposure to phenobarbitone has also been shown to be associated with significantly higher rates of cardiac malformations compared to exposure to other antiepileptic drugs during pregnancy in a recent systematic review (Weston 2016).
How the intervention might work
Antiepileptic drugs suppress seizures by reducing neuronal excitability (MacDonald 1995). Phenobarbitone and carbamazepine are broad‐spectrum treatments suitable for many seizure types, and both have an anticonvulsant mechanism through blocking ion channels, binding with neurotransmitter receptors, or through inhibiting the metabolism or reuptake of neurotransmitters (Ragsdale 1991), and the modulation of gamma‐aminobutyric acid‐A (GABA‐A), receptors (Rho 1996).
Why it is important to do this review
The aim of this review was to summarise efficacy and tolerability data from existing trials comparing carbamazepine and phenobarbitone when used as monotherapy treatments. The adverse event profiles of the two drugs are well documented (see example references from Description of the intervention), and the largest reported RCT investigating carbamazepine and phenobarbitone as monotherapy in adults with focal seizures, Mattson 1985, found carbamazepine to be significantly better at controlling seizures than phenobarbitone, but other trials, including trials recruiting individuals with generalised onset seizures, have found no differences in efficacy between the two drugs (Banu 2007; Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mitchell 1987; Ogunrin 2005; Placencia 1993). Although individual trials have found no consistent differences in efficacy, the confidence intervals generated by these trials are wide, and they have not excluded important differences in efficacy, which synthesising the data of the individual trials may show.
There are difficulties in undertaking a systematic review of epilepsy monotherapy trials as the important efficacy outcomes require analysis of time‐to‐event data (for example, time to first seizure after randomisation). Although methods have been developed to synthesise time‐to‐event data using summary information (Parmar 1998; Williamson 2002), the appropriate statistics are not commonly reported in published epilepsy trials (Nolan 2013a; Williamson 2000). Furthermore, although most epilepsy monotherapy trials collect seizure data, there has been no uniformity in the definition and reporting of outcomes. For example, trials may report time to 12‐month remission but not time to first seizure or vice versa, or some trials may define time to first seizure from the date of randomisation while others use the date of achieving maintenance dose. Trial investigators have also adopted differing approaches to the analysis, particularly with respect to the censoring of time‐to‐event data. For these reasons, we performed this review using individual participant data (IPD), which helps to overcome these problems. This review is one in a series of Cochrane IPD reviews investigating pair‐wise monotherapy comparisons (Marson 2000; Nevitt 2017b; Nevitt 2018a; Nevitt 2018c; Nolan 2013c; Nolan 2016b; Nevitt 2018b). These data have also been included in IPD network meta‐analyses of antiepileptic drug monotherapy (Nevitt 2017a; Tudur Smith 2007).
Objectives
To review the time to treatment failure, remission and first seizure with carbamazepine compared with phenobarbitone when used as monotherapy in people with focal onset seizures (simple or complex focal and secondarily generalised), or generalised onset tonic‐clonic seizures (with or without other generalised seizure types).
Methods
Criteria for considering studies for this review
Types of studies
-
Randomised controlled trials (RCTs), using either an adequate method of allocation concealment (e.g. sealed, opaque envelopes), or a 'quasi' method of randomisation (e.g. allocation by date of birth).
-
Trials may have been double‐blind, single‐blind, or unblinded.
-
Trials must have included a comparison of carbamazepine monotherapy with phenobarbitone monotherapy in individuals with epilepsy.
Types of participants
-
We included children or adults with focal onset seizures (simple focal, complex focal or secondarily generalised tonic‐clonic seizures), or generalised onset tonic‐clonic seizures, with or without other generalised seizure types (in other words, those who had only generalised tonic‐clonic seizures and those who had both generalised onset tonic‐clonic seizures and generalised seizures of other types (e.g. absence, myoclonic etc.)).
-
We excluded individuals with other generalised seizure types alone without generalised tonic‐clonic seizures (e.g. those who had only absence seizures without any generalised clonic tonic‐seizures), due to differences in first‐line treatment guidelines for other generalised seizure types (NICE 2012).
-
We included individuals with a new diagnosis of epilepsy, or who had had a relapse following antiepileptic monotherapy withdrawal.
Types of interventions
Carbamazepine or phenobarbitone as monotherapy.
Types of outcome measures
Below is a list of outcomes investigated in this review. Reporting of these outcomes in the original trial report was not an eligibility requirement for this review.
Primary outcomes
Time to treatment failure (retention time). This was a combined outcome reflecting both efficacy and tolerability, as the following may have led to failure of treatment: continued seizures, side effects, non‐compliance or the initiation of additional add‐on treatment. This is an outcome to which the participant makes a contribution and is the primary outcome measure recommended by the Commission on Antiepileptic Drugs of the International League Against Epilepsy (ILAE 1998; ILAE 2006).
Time to treatment failure is considered according to three definitions:
-
Time to treatment failure for any treatment‐related reason (continued seizures, side effects, non‐compliance or the initiation of additional add‐on treatment)
-
Time to treatment failure due to adverse events (i.e. side effects)
-
Time to treatment failure due to lack of efficacy (i.e. continued seizures)
Secondary outcomes
-
Time to first seizure post‐randomisation
-
Time to achieve 12‐month remission (seizure‐free period)
-
Time to achieve six‐month remission (seizure‐free period)
-
Incidence of adverse events (all reported whether related or unrelated to treatment)
Search methods for identification of studies
Electronic searches
Searches were run for the original review in 2003 and subsequent searches were run in October 2013, September 2014, and August 2016. For the latest update we searched the following databases on 24 May 2018, with no language restrictions.
-
The Cochrane Register of Studies (CRS Web), which includes Cochrane Epilepsy's Specialized Register and the Cochrane Central Register of Controlled Trials (CENTRAL), using the search strategy outlined in Appendix 1
-
MEDLINE Ovid (1946‐24 May 2018), using the search strategy outlined in Appendix 2
-
US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov), using the search strategy outlined in Appendix 3
-
The World Health Organization International Clinical Trials Registry Platform (ICTRP), using the search strategy outlined in Appendix 4.
Previously we also searched SCOPUS (1823 to 18 September 2014), as an alternative to Embase, using the search strategy outlined in Appendix 5, but this is no longer necessary, because RCTs and quasi‐RCTs in Embase are now included in CENTRAL.
Searching other resources
In addition, we handsearched relevant journals, reviewed the reference lists of retrieved trials to search for additional reports of relevant trials, and contacted Novartis (manufacturers of carbamazepine), and experts in the field for information of any ongoing trials, as well as original investigators of relevant trials found.
Data collection and analysis
Selection of studies
Two review authors (SJN and AGM), independently assessed trials for inclusion, resolving any disagreements by mutual discussion.
Data extraction and management
We requested the following IPD for all trials meeting our inclusion criteria.
Trial methods
-
method of generation of random list
-
method of concealment of randomisation
-
stratification factors
-
blinding methods
Participant covariates
-
gender
-
age
-
seizure types
-
time between first seizure and randomisation
-
number of seizures prior to randomisation (with dates)
-
presence of neurological signs
-
electroencephalographic (EEG), results
-
computerised tomography/magnetic resonance imaging (CT/MRI), results
Follow‐up data
-
treatment allocation
-
date of randomisation
-
dates of follow‐up
-
dates of seizures post‐randomisation or seizure frequency data between follow‐up visits
-
dates of treatment failure and reasons for treatment failure
-
dose
-
dates of dose changes
For each trial for which we did not obtain IPD, we carried out an assessment to see whether any relevant aggregate‐level data had been reported or could be indirectly estimated using the methods of Parmar 1998 and Williamson 2002.
Three trials involving 804 participants, provided seizure data in terms of the number of seizures recorded between each follow‐up visit rather than specific dates of seizures (Feksi 1991; Mattson 1985; Placencia 1993). To enable the calculation of time‐to‐event outcomes, we applied linear interpolation to approximate dates of seizures between follow‐up visits. For example, if the trial recorded four seizures between two visits that occurred on 1 March 1990 and 1 May 1990 (interval of 61 days), then the date of first seizure would be approximately 13 March 1990. This allowed the computation of an estimate of the time to six‐month remission, 12‐month remission, and first seizure.
We calculated time to six‐month and 12‐month remission from the date of randomisation to the date (or estimated date), that the individual had first been free of seizures for six or 12 months, respectively. If the person had one or more seizures in the titration period, a six‐month or 12‐month seizure‐free period could also occur between the estimated date of the last seizure in the titration period and the estimated date of the first seizure in the maintenance period.
We calculated time to first seizure from the date of randomisation to the date that we estimated their first seizure to have occurred. If seizure data were missing for a particular visit, we censored these outcomes at the previous visit. We also censored these outcomes if the individual died or if follow‐up ceased prior to the occurrence of the event of interest. We used these methods in the remaining four trials involving 326 participants (Banu 2007; de Silva 1996; Heller 1995; Ogunrin 2005), for which we directly received outcome data (dates of seizures after randomisation).
In the Ogunrin 2005 trial, all 37 participants completed the 12‐week trial duration and no participants withdrew from the trial or from the allocated treatment. For four trials (685 participants), we extracted dates and reason for treatment failure or withdrawal from trial case report forms for the original review (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993).
Two review authors independently extracted data from all case report forms, resolving disagreements by reconsidering the case report forms at conference. For the analysis of time‐to‐event data, we defined an 'event' as either the failure of the allocated treatment because of poor seizure control, adverse events, or both. We also classed non‐compliance with the treatment regimen or the addition of another antiepileptic drug as 'events' for the outcome 'time to treatment failure.' We censored the outcome if treatment was stopped because the individual achieved a period of remission or if the individual was still on allocated treatment at the end of follow‐up.
For the Banu 2007 trial (108 participants), we were provided with the reason for treatment failure or treatment withdrawal and the date of last follow‐up visit. Treatment failure date did not always coincide with date of last follow‐up visit (i.e. several participants had the allocated treatment substituted for the other trial drug and continued to be followed up), and dates of treatment failure could not be provided. Therefore, we could not include participants from this trial in the outcome 'time to treatment failure'.
Assessment of risk of bias in included studies
Two review authors (SJN and JW), independently assessed all included trials for risk of bias according to the Cochrane 'Risk of bias' tool (Higgins 2017), resolving any disagreements by discussion. We rated each of the following six domains as low, unclear or high risk of bias: method of generating random sequence, allocation concealment, blinding methods, incomplete outcome data, selective outcome reporting and other sources of bias. Any discrepancies in the two authors' 'Risk of bias' judgements were resolved by discussion.
Measures of treatment effect
We measured all outcomes in this review as time‐to‐event outcomes with the hazard ratio (HR), and 95% confidence interval (CI), used as the measure of treatment effect. We calculated outcomes from IPD provided, where possible, or extracted from published trials if possible.
Unit of analysis issues
We did not have any unit of analysis issues. The unit of allocation and analysis was individual for all included trials, and no trials included in meta‐analysis were of a repeated measures (longitudinal), nature or of a cross‐over design.
Dealing with missing data
For each trial that supplied IPD, we reproduced results from trial results where possible and performed consistency checks.
-
We cross‐checked trial details against any published report of the trial and contacted original trial authors if we found missing data, errors, or inconsistencies.
-
If trial authors could not resolve inconsistencies between IPD and published data, depending on the extent of the inconsistencies, we performed sensitivity analysis (see Sensitivity analysis), or excluded the data from the meta‐analysis.
-
We reviewed the chronological randomisation sequence and checked the balance of prognostic factors, taking account of factors stratified for in the randomisation procedure.
Assessment of heterogeneity
We assessed heterogeneity statistically using the Q test (P < 0.10 for significance), and the I² statistic (greater than 50% indicating considerable heterogeneity; Higgins 2003), output produced using the generic inverse variance approach in Data and analyses, and visually by inspecting forest plots.
Assessment of reporting biases
Two review authors (SJN and JW), undertook all full quality and 'Risk of bias' assessments. In theory, a review using IPD should overcome issues of reporting biases, as unpublished data can be provided and unpublished outcomes calculated. Any selective reporting bias detected could be assessed with the Outcome Reporting Bias In Trials (ORBIT), classification system (Kirkham 2010).
Data synthesis
We carried out our analysis on an intention‐to‐treat basis (that is, we analysed participants in the group to which they were randomised, irrespective of which treatment they actually received). Therefore, for the time‐to‐event outcomes 'time to six‐month remission', 'time to 12‐month remission', and 'time to first seizure post‐randomisation', we did not censor participants if treatment was withdrawn or failed.
For all outcomes, we investigated the relationship between the time‐to‐event and treatment effect of the antiepileptic drugs. We used Cox proportional hazards regression models to obtain trial‐specific estimates of log (HR), or treatment effect and associated standard errors in Stata Statistical Software, version 14 (Stata 2015). The model assumes that the ratio of hazards (risks), between the two treatment groups is constant over time (i.e. hazards are proportional). We tested this proportional hazards assumption of the Cox regression model for each outcome of each trial by testing the statistical significance of a time‐varying covariate in the model. We evaluated overall estimates of HRs (with 95% confidence intervals (CIs)), using the generic inverse variance method in MetaView. We expressed results as a HR and a 95% CI.
By convention, a HR greater than 1 indicates that an event is more likely to occur earlier on carbamazepine than on phenobarbitone. Hence, for time to treatment failure or time to first seizure, a HR greater than 1 indicates a clinical advantage for phenobarbitone (e.g. a HR of 1.2 would suggest a 20% increase in risk of treatment failure from carbamazepine compared with phenobarbitone), and for time to six‐month and 12‐month remission, a HR greater than 1 indicates a clinical advantage for carbamazepine.
Subgroup analysis and investigation of heterogeneity
Because of the strong clinical belief that some antiepileptic drugs are more effective in some seizure types than others (see Description of the intervention and How the intervention might work), we stratified all analyses by seizure type (focal onset versus generalised onset), according to the classification of main seizure type at baseline. We classified focal seizures (simple or complex), and focal secondarily generalised seizures as focal epilepsy.
We classified primarily generalised seizures as generalised epilepsy. We conducted a Chi² test of interaction between treatment and seizure type. If we found significant statistical heterogeneity to be present, we performed meta‐analysis with a random‐effects model in addition to a fixed‐effect model, presenting the results of both models and performing sensitivity analyses to investigate differences in trial characteristics.
Sensitivity analysis
We performed several sensitivity analyses to test the robustness of our results to characteristics of the included trials.
-
Placencia 1993 concealed allocation via opaque sealed envelopes; however, the trial did not use this method for all trial participants. As inadequate allocation concealment could lead to biased selection of participants, we performed sensitivity analysis excluding data from Placencia 1993 for each outcome and observed any change to results and conclusions.
-
Following consistency checks of IPD for Placencia 1993 and Banu 2007, we found some inconsistencies between the data provided and the results in the publications in terms of treatment failure and seizure recurrences, respectively. Therefore, we performed sensitivity analyses for outcomes 'time to treatment failure' and 'time to first seizure', respectively, to investigate any impact of these inconsistencies on our results. For Placencia 1993, we compared reason for treatment failure in the data provided with reasons reported in the publication and performed a sensitivity analysis of those reasons that we classed as 'events' or 'censored observations' (see Effects of interventions for further details). Regarding Banu 2007, we did not have sufficient information to examine the classification of participants as 'events' and 'censored observations' in the analysis of 'time to first seizure'; therefore, we performed a simple sensitivity analysis excluding data from Banu 2007 from the outcome of 'time to first seizure' and observed any change to results and conclusions.
-
de Silva 1996 withdrew the phenobarbitone arm of the trial after 10 children were randomised to phenobarbitone due to concerns over unacceptable side‐effects. The trial did not randomise any further children to phenobarbitone and continued with the three other treatment arms: carbamazepine, phenytoin, and sodium valproate. For the primary and secondary outcomes of this review, we included all children randomised to carbamazepine (n = 54), and phenobarbitone (n = 10), from de Silva 1996, and to account for the imbalance between children randomised to the two drugs on this trial, we performed sensitivity analysis including only those children who were randomised before the withdrawal of the phenobarbitone arm from the trial. For sensitivity analysis, we analysed 20 children (10 boys and 10 girls), 10 randomised to each drug, nine with generalised seizures and 11 with focal seizures. We performed this sensitivity analysis for each outcome and observed any change to results and conclusions.
-
Misclassification of seizure type is a recognised problem in epilepsy, whereby some people with generalised seizures have been mistakenly classed as having focal onset seizures and vice versa. There is clinical evidence that individuals with generalised onset seizures are unlikely to have an 'age of onset' greater than 25 to 30 years (Malafosse 1994). Such misclassification affected the results of three reviews in our series of pair‐wise reviews for monotherapy in epilepsy comparing carbamazepine to phenobarbitone, phenytoin and sodium valproate in which around 30% to 50% of participants analysed may have had their seizure type misclassified as generalised onset (Marson 2000; Nevitt 2017b; Nevitt 2018b). Given the potential biases introduced into those reviews, we examined the distribution of age at onset for individuals with generalised seizures in the trials included in this review, to assess the potential impact of misclassification of seizure type on the outcomes.
-
22 out of 70 individuals (31%), with generalised onset seizures were over the age of 30 in Heller 1995,
-
19 out of 30 individuals (63%), with generalised onset seizures were over the age of 30 in Ogunrin 2005
-
24 out of 59 individuals (41%), with generalised onset seizures were over the age of 30 in Placencia 1993.
-
Banu 2007 and de Silva 1996 were paediatric trials, and Mattson 1985 recruited participants with focal seizures only, so there were no participants with new onset generalised seizures over the age of 30 in these trials. Therefore, out of 245 participants classified as experiencing generalised seizures from the six trials providing IPD, 65 (27%), may have been wrongly classified.
To investigate misclassification for each outcome, we undertook the following two analyses to investigate misclassification.
-
We reclassified all individuals with generalised seizures and age at onset greater than 30 into an 'uncertain seizure type' group.
-
We reclassified individuals with generalised seizures and age at onset greater than 30 as having focal onset seizures.
'Summary of findings' tables and quality of the evidence (GRADE)
For the 2016 update, we added two 'Summary of findings' tables to the review (outcomes in the tables decided before the update started based on clinical relevance).
summary of findings Table for the main comparison reports the primary outcome of 'time to treatment failure' in the subgroups of participants with focal onset seizures, generalised onset seizures and overall adjusted by seizure type.
summary of findings Table 2 reports the secondary outcomes of 'time to first seizure' and 'time to 12‐month remission' in the subgroups of participants with focal onset seizures, generalised onset seizures and overall adjusted by seizure type.
We determined the quality of the evidence using the GRADE approach, where we downgraded evidence in the presence of high risk of bias in at least one trial, indirectness of the evidence, unexplained heterogeneity or inconsistency, imprecision of results and high probability of publication bias. We downgraded evidence by one level if we considered the limitation serious and two levels for very serious.
Results
Description of studies
Results of the search
We identified 433 records from the databases and search strategies outlined in Electronic searches. We found one further record by searching other resources (handsearching). We removed 140 duplicate records and screened 294 records (title and abstract), for inclusion in the review. We excluded 272 records based on the title and abstract and assessed 22 full‐text articles for inclusion in the review. We excluded seven trials (see Excluded studies below), and included 13 trials (reported in 15 full‐text articles) in the review (see Included studies). See Figure 1 for a PRISMA study flow diagram (Moher 2009).
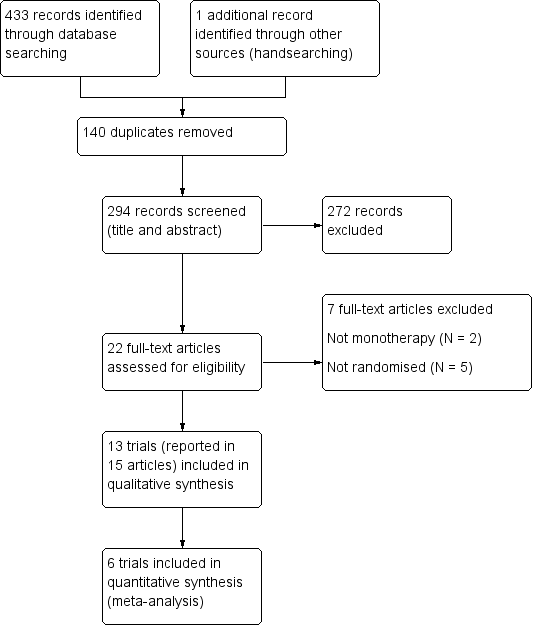
Study flow diagram
Included studies
We included 13 trials in this review (Banu 2007; Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985; Mitchell 1987; Ogunrin 2005; Placencia 1993). Two included trials were available in abstract form only (Bidabadi 2009; Czapinski 1997), and one included trial was published in Italian, which we translated into English (Cossu 1984).
Two trials recruited individuals of all ages (Feksi 1991; Placencia 1993); five trials recruited children only (de Silva 1996 defined children as under the age of 16, Banu 2007 and Chen 1996 defined children as under the age of 15, and Bidabadi 2009 and Mitchell 1987 defined children as under the age of 12), and the remaining six trials recruited adults only. Of the adults‐only trials, three defined adults to be individuals above the age of 18 (Cereghino 1974; Czapinski 1997; Mattson 1985), one trial classed adults as older than 13 years (Heller 1995), one trial classed adults as older than 14 years (Ogunrin 2005), and one trial classed adults as older than 15 years (Cossu 1984).
Seven trials recruited individuals with focal onset seizures and generalised onset seizures (Banu 2007; Chen 1996; de Silva 1996; Feksi 1991; Heller 1995; Ogunrin 2005; Placencia 1993), three trials recruited individuals with focal onset seizures only (Cereghino 1974; Mattson 1985; Mitchell 1987), one trial recruited individuals with focal seizures and secondarily generalised seizures (Bidabadi 2009), one trial recruited individuals with complex focal seizures only (Czapinski 1997), and one trial recruited individuals with temporal lobe epilepsy only (Cossu 1984). Ten trials recruited individuals with new onset seizures, or previously untreated seizures, or both (Banu 2007; Chen 1996; Cossu 1984; Czapinski 1997; de Silva 1996; Feksi 1991; Heller 1995; Mitchell 1987; Ogunrin 2005; Placencia 1993); one trial recruited institutionalised participants with uncontrolled seizures (Cereghino 1974); one trial recruited "previously untreated or under‐treated" individuals (Mattson 1985); and one trial (reported only in abstract form) provided no information regarding new onset of seizures in participants (Bidabadi 2009).
Four trials were conducted in Europe ( Cossu 1984; Czapinski 1997; de Silva 1996; Heller 1995); three trials were conducted in the USA (Cereghino 1974; Mattson 1985; Mitchell 1987); one trial was conducted in Iran (Bidabadi 2009), one trial was conducted in Taiwan (Chen 1996); and four trials were conducted in rural areas or low‐ or middle‐income countries, or both: one trial in Bangladesh (Banu 2007), one trial in Ecuador (Placencia 1993), one trial in Kenya (Feksi 1991), and one trial in Nigeria (Ogunrin 2005).
Individual participant data were provided by trial authors for six trials, which recruited a total of 836 participants, representing 57% of 1455 individuals from all 13 identified eligible trials. Four trials provided computerised data directly (Banu 2007; Mattson 1985; Ogunrin 2005; Placencia 1993), and the authors of two trials (de Silva 1996; Heller 1995), supplied a combination of both computerised and hard copy data (although mostly computerised).
Data were available for the following participant characteristics (percentage of 836 participants with data available): sex (99%, data missing for 6 participants in de Silva 1996 and 4 participants in Mattson 1985); seizure type (100%); drug randomised (99%, data missing for 6 participants in de Silva 1996); age at randomisation (99%, data missing for 1 participant in Heller 1995, 6 participants in de Silva 1996, and 4 participants in Mattson 1985); number of seizures in six months prior to randomisation (98%, data missing for 5 participants from Banu 2007, 1 participant in Heller 1995, 6 participants in de Silva 1996, and 7 participants in Mattson 1985); and time since first seizure to randomisation (94%, data missing for 2 participants in Heller 1995, 6 participants in de Silva 1996, 5 participants in Mattson 1985, and all 37 participants in Ogunrin 2005). See the Characteristics of included studies table and Table 1 for further details.
| Focal seizures: n (%)a | Male participants: n (%)a | Age at entry (years): Mean (SD), range | Aged > 30 and generalised seizures: n (%) | Epilepsy duration (years): mean (SD), range | Number of seizures in prior 6 months: median (range) | |||||||||||||
| CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | |
| 33 (61%) | 26 (48%) | 0 | 24 (44%) | 37 (69%) | 0 | 6.2 (3.6), 1 to 15 | 5.3 (3.3), 1 to 12 | 0 | 0 | 0 | 0 | 2.0 (2.4), 0 to 11.5 | 1.6 (2.0), 0 to 10 | 0 | 24 (1 to 7200) | 24 (2 to 4320) | 5 | |
| 29 (54%) | 5 (50%) | 0 | 30 (56%) | 4 (40%) | 6 | 9.2 (3.8), 2 to 15 | 9.1 (3.9), 3 to 14 | 6 | 0 | 0 | 0 | 1.7 (2.6), 0 to 12 | 1.3 (1.8), 0.1 to 5 | 6 | 3 (1 to 500) | 3 (1 to 170) | 6 | |
| 24 (39%) | 25 (43%) | 0 | 30 (49%) | 25 (43%) | 0 | 29.3 (14.1), 13 to 69 | 34.5 (15.1), 16 to 77 | 1 | 9 | 13 | 0 | 4.4 (7.4), 0.1 to 40 | 3.4 (6.6), 0 to 37 | 2 | 2 (1 to 354) | 3 (1 to 579) | 1 | |
| 155 (100%) | 155 (100%) | 0 | 133 (87%) | 135 (88%) | 4 | 42.1 (15.9), 18 to 82 | 40.1 (15.3), 18 to 75 | 4 | 0 | 0 | 0 | 5.9 (9.1), 0.5 to 55 | 5.7 (7.9), 0.5 to 36 | 5 | 1 (1 to 100) | 1 (1 to 14) | 7 | |
| 5 (26%) | 2 (11%) | 0 | 12 (63%) | 11 (61%) | 0 | 28.2 (5.8), 14 to 38 | 35.4 (6.2), 26 to 55 | 0 | 6 | 13 | 0 | NA | NA | 37 | 18 (6 to 36) | 12 (6 to 42) | 0 | |
| 69 (73%) | 64 (66%) | 0 | 37 (39%) | 30 (31%) | 0 | 29.3 (18.2), 2 to 68 | 28.7 (17.1), 2 to 68 | 0 | 11 | 13 | 0 | 9.5 (11.6), 0.5 to 54 | 9.8 (11.0), 0.5 to 48 | 0 | 1 (0 to 68) | 2 (0 to 100) | 0 | |
CBZ: carbamazepine; n: number of participants; NA: not available; PB: phenobarbitone; SD: standard deviation
aProportions (%) are calculated based on non‐missing data.
bRandomised drug missing for 6 participants in de Silva 1996.
Three trials provided the results of neurological examinations for 220 participants (27%), (de Silva 1996; Heller 1995; Ogunrin 2005). All participants had a normal neurological examination in Ogunrin 2005, 95% of participants and 94% of participants had a normal neurological examination in de Silva 1996 and Heller 1995 respectively.
Three trials provided electroencephalographic (EEG), results for 581 participants (69%), (103 participants from Banu 2007, 307 participants from Mattson 1985, and 192 participants from Placencia 1993). In Banu 2007, 52% of participants had an abnormal EEG, in Mattson 1985 71% of participants had an abnormal EEG and in Placencia 1993, 47% of participants had an abnormal EEG.
Four trials provided computerised tomography/magnetic resonance imaging (CT/MRI), results for 438 participants (52%), (26 from Banu 2007, 273 from Mattson 1985, 27 from Ogunrin 2005 and 112 from Placencia 1993). In Banu 2007, 19% of participants had an abnormal scan, in Mattson 1985 27% of participants had an abnormal scan, in Ogunrin 2005 no participants had an abnormal scan and in Placencia 1993, 33% of participants had an abnormal scan.
We did not obtain individual participant data (IPD), for six trials, with a total of 317 participants, as suitable seizure data for the outcomes examined in this review were not recorded (Chen 1996; Mitchell 1987), the trial authors no longer had a copy of the data (Cereghino 1974), or trial authors did not respond to our data requests (Bidabadi 2009; Cossu 1984; Czapinski 1997). A further trial, which randomised 302 participants (Feksi 1991), provided access to an IPD dataset, but this was not the final dataset used for the analysis published by the original authors. The pharmaceutical company that sponsored the trial, Ciba‐Geigy, who at that time held the product license for carbamazepine, held the final dataset. Since the trial was undertaken, there have been a number of mergers and restructures within the industry, and the current owners of the data are Novartis. Unfortunately, Novartis were unable to locate the data for this trial. The dataset that we had for this trial contained a number of problems and inconsistencies, and we therefore decided not to include this trial in the meta‐analysis. None of these seven trials reported the specific time‐to‐event outcomes chosen for this review, and we could not extract sufficient aggregate data from the trial publications in any other trial. Therefore, we could not include them in data synthesis. Table 2 contains full details of outcomes considered and summaries of results in each eligible trial for which IPD were not available.
| Trial | Outcomes reported | Summary of results |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
| PB (n = 123), CBZ (n = 126)
| |
|
|
|
CBZ: carbamazepine; IQ: intelligence quotient; PB: phenobarbitone; WISC‐R scale: the Wechsler Intelligence Scale for Children
Excluded studies
We excluded five trials that were not randomised controlled trials (RCTs), (Bird 1966; Castro‐Gago 1998; Hansen 1980; Kuzuya 1993; Sabers 1995), and we excluded two trials that did not use carbamazepine and phenobarbitone monotherapy (Marjerrison 1968; Meador 1990). See the 'Characteristics of excluded studies' tables for further details.
Risk of bias in included studies
For further details, see the 'Characteristics of included studies' tables, Figure 2, and Figure 3.

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included trials

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included trial
Allocation
Trials for which we received IPD
Three trials reported adequate methods of randomisation and allocation concealment and we judged all three to be at low risk of bias: two trials used permuted blocks to generate a random list and concealed allocation by using sealed opaque envelopes (de Silva 1996; Heller 1995); and one trial used number tables to generate a random list and concealed allocation by allocating the randomised drug on a different site to where participants were randomised (Ogunrin 2005). One trial reported only that participants were randomised with stratification for seizure type (Mattson 1985); no further information was provided in the trial publication or from the authors regarding the methods of generation of the random list and concealment of allocation and we judged this trial at unclear risk of bias. For two trials, neither the trial publication nor the authors provided the method of generation of the random list (Banu 2007; Placencia 1993), therefore these trials were judged to be at unclear risk of bias from random sequence generation. One of these trials reported that allocation was concealed using sealed envelopes prepared on a different site to recruitment of participants (Banu 2007, low risk of bias), and the other trial reported that allocation was concealed by sealed opaque envelopes, but this method was not used for all participants in the trial, therefore we judged this trial to be at high risk of bias for allocation concealment (Placencia 1993). This inadequate allocation concealment may have resulted in selection bias in this trial, so we performed sensitivity analyses for all outcomes excluding participants from this trial (see Sensitivity analysis and Effects of interventions).
Trials for which no IPD were available
Two trials reported adequate methods of randomisation (low risk of selection bias): random number tables (Cereghino 1974); and simple randomisation of block size three (Chen 1996), but they provided no details on concealment of allocation.
Three trials (Bidabadi 2009; Cossu 1984; Czapinski 1997) reported that the participants were 'randomised' or 'randomly allocated', etc. but did not provide information about the method of generation of the random list or allocation concealment (unclear risk of selection bias).
One trial ((Feksi 1991) reported that it concealed allocation by the use of sealed opaque envelopes (low risk of bias) but did not report the method of generation of the random list (unclear risk of bias), and one trial reported that it "randomised [children] using a scheme that balanced drug distribution by age and sex" but did not provide further details about the method of generation of the random list (Mitchell 1987). This trial also did not report any details on allocation concealment, and the trial used some non‐randomised children in some analyses (see Other potential sources of bias).
Blinding
Trials for which we received IPD
One trial (Mattson 1985) double‐blinded participants and personnel using an additional blank tablet (low risk of bias) ; however, it was unclear if this trial blinded the outcome assessor (unclear risk of bias). One trial blinded participants and the outcome assessors who performed cognitive testing but did not blind a research assistant recruiting participants and providing counselling on medication adherence (Ogunrin 2005). Similarly, another trial blinded participants and a psychologist and therapist throughout the trial, while not blinding the treating physician for practical and ethical reasons (Banu 2007). We judged that the open‐label elements of these two trials were unlikely to have influenced the results of these trials. However, the latter trial blinded a researcher throughout the trial duration, but unblinded the researcher for analysis, which may have impacted upon results.
One trial, Placencia 1993, did not report any information on blinding in the trial publication, and no information was available from the trial authors (unclear risk of bias). Two trials were unblinded for "practical and ethical reasons" (de Silva 1996; Heller 1995); however, it is likely that the unblinded design of de Silva 1996 contributed to the early withdrawal of the phenobarbitone arm, which is likely to have had an effect on the overall results of the trial. Further, as the two trials were conducted under the same protocol, the open design may have also contributed to the withdrawal rates in Heller 1995 and influenced the overall results; we judged both trials at high risk of performance and detection bias.
Trials for which no IPD were available
One trial was described as double‐blind (Cossu 1984), but it was unclear exactly who was blinded (participants, personnel, outcome assessors). One paediatric trial blinded participants (and parents), and psychometric testers but unblinded clinicians for follow‐up (Mitchell 1987). One trial described that cognitive testers were single‐blinded, Chen 1996, but gave no further details on blinding of participants and personnel.
The remaining four trials did not provide any information on masking of participants, personnel, or outcome assessors; we judged them to be at unclear risk of performance and detection bias (Bidabadi 2009; Cereghino 1974; Czapinski 1997; Feksi 1991).
Incomplete outcome data
Trials for which we received IPD
In theory, a review using IPD should overcome issues of attrition bias as unpublished data can be provided, unpublished outcomes calculated, and all randomised participants can be analysed by an intention‐to‐treat approach. All six trials provided IPD for all randomised individuals and reported the extent of follow‐up for each individual; we judged all six trials to be at low risk of attrition bias (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993). We queried any missing data with the original trial authors. From the information provided by the trial authors, we deemed the small amount of missing data present (included trials), to be missing at random and not affecting our analysis.
Trials for which no IPD were available
Two trials reported attrition rates and analysed all randomised participants using an intention‐to‐treat approach so were judged to be at low risk of bias (Cossu 1984; Mitchell 1987). Two trials reported attrition rates, but it was unclear if they analysed all participants (Cereghino 1974; Czapinski 1997), and one trial did not report attrition rates, and it was unclear if it analysed all participants (Bidabadi 2009). These three trials were judged to be at unclear risk of attrition bias.
Two trials included only those who completed the trial in the final analysis (Chen 1996; Feksi 1991), excluding 6% and 17.5% of participants, respectively, from the final results. This approach is not intention‐to‐treat, so we deemed these two trials to be at a high risk of attrition bias.
Selective reporting
We requested trial protocols in all IPD requests; however, protocols were not available for any of the 13 included trials, so we made a judgement of the risk of bias based on the information included in the publications or from the IPD we received (see the 'Characteristics of included studies' tables for more information).
Trials for which we received IPD
In theory, a review using IPD should overcome issues of reporting biases as unpublished data can be provided and unpublished outcomes calculated so all trials providing IPD were judged to be at low risk of reporting bias. We received sufficient IPD to calculate the four outcomes ('time to treatment failure', 'time to six‐month remission, 'time to 12‐month remission', and 'time to first seizure'), for four of the six trials (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993). The trial duration of Ogunrin 2005 was 12 weeks, and all randomised participants completed the trial; therefore, we could only calculate 'time to first seizure' for this trial. Banu 2007 did not record the dates of all seizures after randomisation and dates of treatment failure for allocated treatment for all participants; therefore, we could only calculate 'time to first seizure' for this trial.
Trials for which no IPD were available
Four trials reported either cognitive outcomes, seizure outcomes, adverse events, or a combination of these and were judged to be at low risk of reporting bias (Chen 1996; Cereghino 1974; Feksi 1991; Mitchell 1987). One trial reported cognitive outcomes only, but no adverse events or seizure outcomes (Cossu 1984); however, as no protocols were available for this trial, we do not know whether either seizure outcomes, recording of adverse events, or both, were planned a priori (unclear risk of reporting bias). Two trials were in abstract form only (Bidabadi 2009; Czapinski 1997) and did not provide sufficient information to assess selective reporting bias (unclear risk of reporting bias).
Other potential sources of bias
We detected another source of bias in six of the 13 included trials as described below (high risk of bias); the remaining seven trials were judged to be at low risk of other bias.
Following consistency checks of IPD for Placencia 1993 and Banu 2007, we found some inconsistencies between the data provided and the results in the publications in terms of treatment failure and seizure recurrences, respectively, which the authors could not resolve and we judged these trials to be at high risk of other bias. We performed sensitivity analysis to investigate the impact of the inconsistent data on our outcomes (see Sensitivity analysis and Effects of interventions). Furthermore, we received IPD for a seventh trial (Feksi 1991), but too many inconsistencies were present for this data to be usable (see Included studies for further details).
One trial had a cross‐over design (Cereghino 1974); such a design is unlikely to be appropriate for monotherapy treatment because of carryover effects from one treatment period into another (participants were also treated during washout periods with their 'regular medication'), and such a design does not allow long‐term outcomes, such as the time‐to‐event outcomes of interest in this review. For future updates of this review, we will exclude trials of a cross‐over design.
We included one trial with very small participant numbers (six participants randomised to each drug), and very short‐term follow‐up (three weeks), and it was unclear if this trial was adequately powered and of sufficient duration to detect differences (Cossu 1984). For future updates of this review, we will review our inclusion criteria in terms of participant numbers and trial duration.
Another trial had several potential sources of other bias (Mitchell 1987); there was evidence that the trial may have been underpowered to detect differences between the treatments, one of the tools for outcome assessment was not fully validated, and non‐randomised children from a related pilot trial were included in analysis for some of the outcomes.
Effects of interventions
See: Summary of findings for the main comparison Carbamazepine compared with phenobarbitone for epilepsy (time to treatment failure); Summary of findings 2 Carbamazepine compared with phenobarbitone for epilepsy (secondary outcomes)
We have provided a summary of the outcomes reported in trials for which no IPD were available in Table 2.
See Table 3 for details regarding the number of individuals contributing IPD to each analysis, summary of findings Table for the main comparison for a summary of the results for the primary outcome 'time to treatment failure' (stratified by seizure type), and summary of findings Table 2 for a summary of results for the secondary outcomes 'time to first seizure' and 'time to 12‐month remission'. Survival curve plots are shown in Figure 4; Figure 5; Figure 6; Figure 7; Figure 8; Figure 9; Figure 10; Figure 11; Figure 12; Figure 13; Figure 14 and Figure 15. We used Stata software version 14 to produce all survival curve plots using data from all trials providing IPD combined (Stata 2015).

Time to treatment failure ‐ any reason related to the treatment (CBZ: carbamazepine; PB: phenobarbitone)
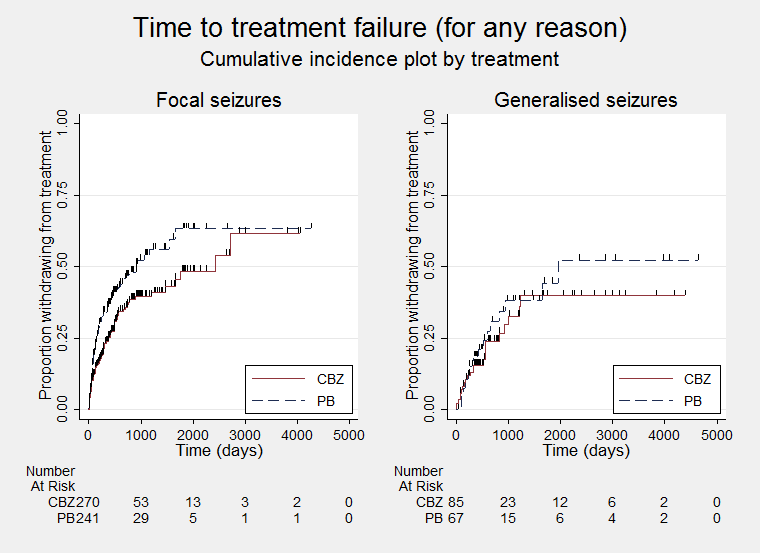
Time to treatment failure ‐ any reason related to the treatment, by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to treatment failure due to adverse events (CBZ: carbamazepine; PB: phenobarbitone)

Time to treatment failure due to adverse events, by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to treatment failure due to lack of efficacy (CBZ: carbamazepine; PB: phenobarbitone)
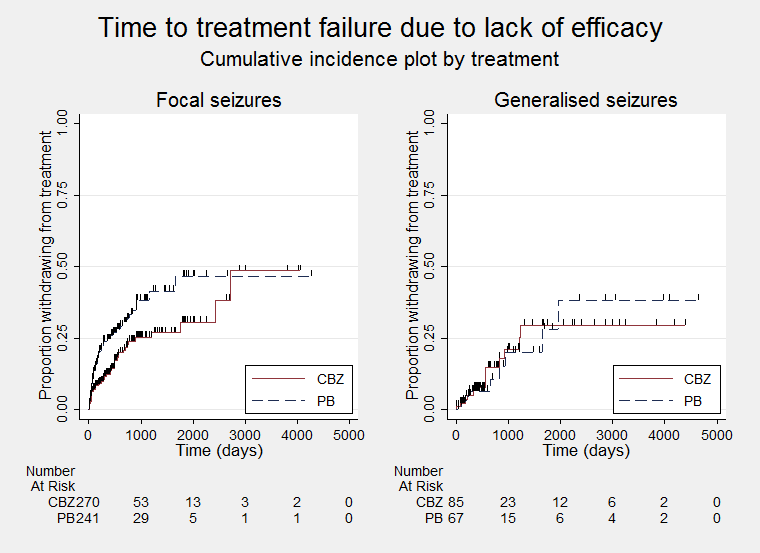
Time to treatment failure due to lack of efficacy, by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to first seizure post randomisation (CBZ: carbamazepine; PB: phenobarbitone)

Time to first seizure post randomisation ‐ by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to 12‐month remission (CBZ: carbamazepine; PB: phenobarbitone)

Time to 12‐month remission ‐ by seizure type (CBZ: carbamazepine; PB: phenobarbitone)
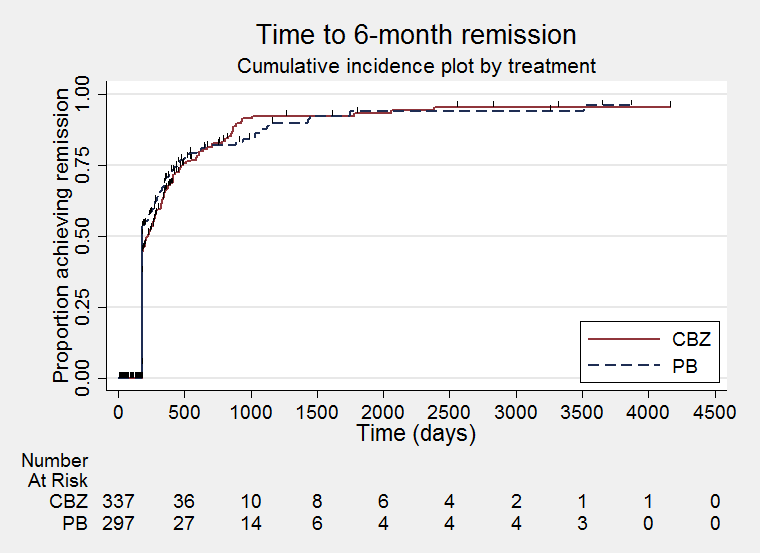
Time to six‐month remission (CBZ: carbamazepine; PB: phenobarbitone)

Time to six‐month remission ‐ by seizure type (CBZ: carbamazepine; PB: phenobarbitone)
| Trial | Number randomised | Time to treatment failure | Time to 12‐month remission | Time to six‐month remission | Time to first seizure | ||||||||||
| CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | |
| 54 | 54 | 108 | Data not available | Data not available | Data not available | 54 | 54 | 108 | |||||||
| 54 | 10 | 64 | 53 | 10 | 63 | 54 | 10 | 64 | 54 | 10 | 64 | 54 | 10 | 64 | |
| 61 | 58 | 119 | 60 | 55 | 115 | 61 | 58 | 119 | 61 | 58 | 119 | 61 | 58 | 119 | |
| 155 | 155 | 310 | 154 | 155 | 309 | 154 | 155 | 309 | 154 | 155 | 309 | 151 | 151 | 302 | |
| 19 | 18 | 37 | Data not available | Data not available | Data not available | 19 | 18 | 37 | |||||||
| 95 | 97 | 192 | 94 | 95 | 189 | 95 | 96 | 191 | 95 | 96 | 191 | 95 | 97 | 192 | |
| Total | 438 | 392 | 830 | 361 | 315 | 676 | 364 | 319 | 683 | 364 | 319 | 683 | 434 | 388 | 822 |
CBZ: carbamazepine; PB: phenobarbitone
aThe date of treatment failure was not recorded in all cases for Banu 2007, so we could not calculate 'time to treatment failure'. The date of first seizure after randomisation was recorded, but none of the dates of subsequent seizures were recorded; therefore, we could calculate 'time to first seizure', but we could not calculate 'time to six‐month remission' and 'time to 12‐month remission'.
bWe received individual participant data for 70 participants recruited in de Silva 1996; the randomised drug was not recorded in six participants. Reasons for treatment failure were not available for one participant randomised to CBZ; we did not include this participant in the analysis of 'time to treatment failure.'
cReasons for treatment failure were not available for four participants (one randomised to CBZ and three to PB), in Heller 1995; we did not include these participants in the analysis of 'time to treatment failure.'
dNo follow‐up data after randomisation were available for one participant randomised to CBZ in Mattson 1985. Dates of seizure recurrence were not available for seven participants (three randomised to CBZ and four to PB); we did not include these participants in the analysis of 'time to first seizure.'
eThe trial duration of Ogunrin 2005 was 12 weeks; therefore, six‐ and 12‐month remission of seizures could not be achieved, so we could not calculate these outcomes. All randomised participants completed the trial without withdrawing from treatment or treatment failing, so we could not analyse 'time to treatment failure.'
fReasons for treatment failure were not available for three participants (one randomised to CBZ and two randomised to PB) in Placencia 1993. We did not include these participants in the analysis of 'time to treatment failure.' Seizure data after occurrence of first seizure were not available for one participant randomised to PB, so we did not include this participant in the analyses of time to six‐month and time to 12‐month remission.
We note that participants with event times of zero (i.e. those who experienced treatment failure or experienced seizure recurrence on the day of randomisation), are not included in the 'Numbers at risk' on the graphs and that data are not stratified by trial within these survival curve plots. All figures are intended to provide a visual representation of outcomes, extent of follow‐up and visual differences between seizure types. These graphs are not intended to show statistical significance and numerical values may vary compared to the text due to differences in methodology.
We calculated all hazard ratios (HRs), presented below by generic inverse variance meta‐analysis. All analyses met the assumption of proportional hazards (addition of time‐varying covariate into the model non‐significant), unless otherwise stated.
Primary outcome
Time to treatment failure (retention time)
For this outcome, a HR less than one indicates a clinical advantage for carbamazepine.
Times to treatment failure and reasons for treatment failure were available for 676 participants from four of the six trials providing IPD (97.8% of 691 participants from de Silva 1996, Heller 1995, Mattson 1985, and Placencia 1993 (see Included studies and Table 3), and 46.4% of the total 1455 participants from the 13 included trials). See Table 4 for reasons for premature discontinuation of treatment (treatment failure), by treatment and how we classified these reasons in analysis.
| Reason for early termination | Total | ||||||||||||
| CBZ | PB | CBZ | PB | CBZ | PB | CBZ | PB | CBZ | PB | CBZ | PB | All | |
| Adverse events (event) | 3 | 2 | 8 | 12 | 11 | 5 | 5 | 5 | 0 | 0 | 27 | 24 | 51 |
| Lack of efficacy (event) | 12 | 2 | 5 | 7 | 3 | 11 | 0 | 0 | 8 | 6 | 28 | 26 | 54 |
| Both adverse events and lack of efficacy (event) | 6 | 4 | 4 | 3 | 31 | 46 | 0 | 0 | 0 | 0 | 41 | 53 | 94 |
| Non‐compliance/protocol violation (event) | 0 | 0 | 0 | 0 | 11 | 19 | 13 | 9 | 6 | 0 | 30 | 28 | 58 |
| Illness or death (not treatment‐related, censored) | 0 | 0 | 0 | 0 | 17 | 13 | 2 | 1 | 0 | 0 | 19 | 14 | 33 |
| Participant went into remission (censored) | 18 | 1 | 6 | 3 | 0 | 0 | 0 | 0 | 0 | 2 | 24 | 6 | 30 |
| Lost to follow‐up (censored) | 0 | 0 | 0 | 0 | 26 | 26 | 11 | 5 | 7 | 15 | 44 | 46 | 90 |
| Other (censored)d | 0 | 0 | 0 | 0 | 3 | 2 | 0 | 0 | 0 | 0 | 3 | 2 | 5 |
| Completed the trial (censored) | 14 | 1 | 37 | 30 | 52 | 33 | 63 | 75 | 33 | 31 | 199 | 170 | 369 |
| Total | 53 | 10 | 60 | 55 | 154 | 155 | 94 | 95 | 54 | 54 | 415 | 369 | 784 |
CBZ: carbamazepine; PB: phenobarbitone
aFour participants for Heller 1995 (one on CBZ and three on PB) and one for de Silva 1996 (CBZ) and one for Mattson 1985 (CBZ) had missing reasons for treatment failure.
bThere were inconsistencies between individual participant data and the publication of Placencia 1993; we performed sensitivity analysis (see Effects of interventions). There were missing reasons for treatment failure for three participants (one on CBZ and two on PB); we did not include these participants in the analysis.
cBanu 2007 provided reasons for treatment failure, but dates of treatment failure could not be provided for all participants, so we could not calculate 'time to treatment failure.'
dOther reasons from Mattson 1985: participants developed other medical disorders including neurological and psychiatric disorders.
Mattson 1985 did not record follow‐up data for one participant randomised to carbamazepine. de Silva 1996 did not record the randomised drug for six participants, and the reason for treatment failure was not available for one participant randomised to carbamazepine and could not be determined from the case notes. Similarly, in Heller 1995, for one participant randomised to carbamazepine and three participants randomised to phenobarbitone and in Placencia 1993, for one participant randomised to carbamazepine and two participants randomised to phenobarbitone, the reason for treatment failure was not available and could not be determined from the case notes. We did not include these 15 participants with missing outcome data in the analysis of 'time to treatment failure.' All participants completed the 12‐week trial in Ogunrin 2005 and so could not contribute to the analysis of 'time to treatment failure.' From the IPD provided by Banu 2007, we were able to establish reasons for treatment failure for all participants (see Table 4), but the date of treatment failure was not available for all participants (see Data extraction and management for further details); therefore, we could not calculate the 'time to treatment failure' for this trial.
Out of the 784 participants for whom we had reasons for treatment failure or withdrawal (Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993), 415 participants prematurely withdrew from treatment (53% of total participants): 216 out of 415 participants randomised to carbamazepine (52%), and 199 out of 369 participants randomised to phenobarbitone (54%)
We deemed 257 participants (62% of total treatment failures), to have withdrawn for reasons related to the trial drug, 126 (58%), on carbamazepine and 131 (66%), on phenobarbitone, and we classed these reasons as 'events' in analysis. The most common treatment‐related reason for treatment failure was a combination of adverse events and lack of efficacy: 94 withdrawals (23% of total treatment failures), 41 (19% of total treatment failures), on carbamazepine and 53 (27% of total treatment failures), on phenobarbitone. Non‐compliance with treatment or patient choice was the treatment‐related reason in 14% of total treatment failures, lack of efficacy in 13% of total treatment failures and adverse events in 12% of total treatment failures.
We classed the other 158 reasons (90 on carbamazepine and 68 on phenobarbitone), which were mostly losses to follow‐up (57% of other withdrawals), to be not related to the treatment and censored these participants in the analysis, in addition to the 369 participants (199 on carbamazepine and 170 on phenobarbitone), who completed the trial without withdrawing or failing treatment.
Considering time to treatment failure for any reason related to the treatment, the overall pooled HR (for 676 participants), was 0.66 (95% confidence interval (CI), 0.51 to 0.86; P = 0.002; fixed‐effect meta‐analysis; Analysis 1.1), indicating a statistically significant advantage for carbamazepine; in other words, treatment failure occurred significantly earlier on phenobarbitone than carbamazepine in the four included trials.
There was a considerable amount of statistical heterogeneity between trials (I² = 58%, see Analysis 1.1). When we repeated the analysis using random‐effects meta‐analysis, the pooled HR was 0.66 (95% CI 0.42 to 1.04; P = 0.08), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant. We have investigated the heterogeneity present within the analysis in subgroup and sensitivity analyses described below.
Considering time to treatment failure due to adverse events (all other reasons for treatment failure or treatment withdrawal censored in analysis), the overall pooled HR (for 676 participants), was 0.67 (95% CI 0.48 to 0.93; P = 0.02; fixed‐effect meta‐analysis; Analysis 1.2), indicating a statistically significant advantage for carbamazepine; in other words, treatment failure due to adverse events occurred significantly earlier on phenobarbitone than carbamazepine in the four included trials. However, again a moderate amount of heterogeneity was present in analysis (I² = 57%, see Analysis 1.2), and when we repeated the analysis with random‐effects meta‐analysis, the pooled HR was 0.59 (95% CI 0.32 to 1.09, P = 0.09), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant.
Considering time to treatment failure due to lack of efficacy (all other reasons for treatment failure or treatment withdrawal censored in analysis), 487 participants provided IPD from three trials; no participants withdrew due to lack of efficacy in one of the trials (Placencia 1993, see Table 4). The overall pooled HR was 0.54 (95% CI 0.38 to 0.77; P = 0.0007; fixed‐effect meta‐analysis; Analysis 1.3), indicating a statistically significant advantage for carbamazepine; in other words, treatment failure due to lack of efficacy occurred significantly earlier on phenobarbitone than carbamazepine in the three included trials. There was no evidence of statistical heterogeneity between trials (I² = 0%).
Subgroup analyses: seizure type (focal versus generalised onset)
Considering time to treatment failure for any reason related to the treatment, for participants with focal onset seizures (520 participants from four trials), the pooled HR was 0.66 (95% CI 0.49 to 0.88, P = 0.005; low‐quality evidence, fixed‐effect meta‐analysis; Analysis 1.4), indicating a statistically significant advantage for carbamazepine, but a large amount of statistical heterogeneity was present between trials (I² = 66%). When we repeated the analysis using random‐effects meta‐analysis, the pooled HR for participants with focal onset seizures was 0.63 (95% CI 0.32 to 1.22, P = 0.17), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant. For participants with generalised onset seizures (156 participants from three trials), the pooled HR was 0.65 (95% CI 0.35 to 1.23, P = 0.19; low‐quality evidence, fixed‐effect meta‐analysis; Analysis 1.4), suggesting an advantage for carbamazepine that was not statistically significant. There was no evidence of statistical heterogeneity between trials (I² = 0%).
The test for subgroup differences between focal and generalised onset seizures was not statistically significant (P = 0.99, I² = 0% for variability due to subgroup differences; Analysis 1.4). The overall pooled HR (adjusted by seizure type for 676 participants from four trials), was 0.66 (95% CI 0.50 to 0.86; P = 0.002; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.4), indicating a statistically significant advantage for carbamazepine. Numerical results in this analysis adjusted for seizure type are very similar to the unadjusted analysis (Analysis 1.1), and heterogeneity present within analysis is reduced within the adjusted analysis (I² = 35% in Analysis 1.4 compared to I² = 58% in Analysis 1.1).
Considering time to treatment failure due to adverse events, 619 participants provided IPD from four trials; no participants in the carbamazepine group with generalised onset seizures withdrew due to adverse events in one of the trials (Placencia 1993), so we could not calculate a hazard ratio. For participants with focal onset seizures (520 participants from four trials), the pooled HR was 0.67 (95% CI 0.46 to 0.96, P = 0.03; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.5), indicating a statistically significant advantage for carbamazepine, but a large amount of statistical heterogeneity was present between trials (I² = 70%). When we repeated the analysis using random‐effects meta‐analysis, the pooled HR for participants with focal onset seizures was 0.53 (95% CI 0.20 to 1.44, P = 0.21), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant. For participants with generalised onset seizures (99 participants from two trials), the pooled HR was 0.84 (95% CI 0.35 to 2.00, P = 0.69; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.5), suggesting an advantage for carbamazepine that was not statistically significant. There was no evidence of statistical heterogeneity between trials in the subgroup of participants with generalised onset seizures (I² = 0%).
The test for subgroup differences between focal and generalised onset seizures was not statistically significant (P = 0.64, I² = 0% for variability due to subgroup differences; Analysis 1.5). The overall pooled HR (adjusted by seizure type for 619 participants from four trials), was 0.69 (95% CI 0.49 to 0.97; P = 0.03; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.5), indicating a statistically significant advantage for carbamazepine. Numerical results in this analysis adjusted for seizure type are very similar to the unadjusted analysis (Analysis 1.2), but a similar amount of heterogeneity is present within this adjusted analysis (I² = 55%). When we repeated the analysis using random‐effects meta‐analysis, the pooled HR for participants with focal onset seizures was 0.60 (95% CI 0.31 to 1.17, P = 0.14), still indicating an advantage for carbamazepine, but this advantage was no longer statistically significant.
Considering time to treatment failure due to lack of efficacy, for participants with focal onset seizures (388 participants from three trials), the pooled HR was 0.54 (95% CI 0.36 to 0.80, P = 0.002; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.6), indicating a statistically significant advantage for carbamazepine. There was no evidence of statistical heterogeneity between trials in the subgroup of participants with focal onset seizures (I² = 0%). For participants with generalised onset seizures (99 participants from two trials), the pooled HR was 0.56 (95% CI 0.23 to 1.35, P = 0.20; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.6), suggesting an advantage for carbamazepine that was not statistically significant. There was no evidence of statistical heterogeneity between trials in the subgroup of participants with generalised onset seizures (I² = 0%).
The test for subgroup differences between focal and generalised onset seizures was not statistically significant (P = 0.94, I² = 0% for variability due to subgroup differences; Analysis 1.6). The overall pooled HR (adjusted by seizure type for 487 participants from three trials), was 0.54 (95% CI 0.38 to 0.78; P = 0.0008; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.6), indicating a statistically significant advantage for carbamazepine. Numerical results in this analysis adjusted for seizure type are very similar to the unadjusted analysis (Analysis 1.3), and there was no evidence of statistical heterogeneity between trials in this adjusted analysis (I² = 0%).
Sensitivity analysis
We used fixed‐effect meta‐analysis to performed all sensitivity analyses.
We performed sensitivity analysis excluding participants from Placencia 1993 from the analysis of time to treatment failure for any reason related to treatment because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 5). This sensitivity analysis resulted in a slightly larger advantage for carbamazepine with a pooled HR of 0.59 (95% CI 0.44 to 0.79, P = 0.0003, adjusted for seizure type; fixed‐effect meta‐analysis), and reduced heterogeneity (I² = 6%), compared to the original analysis (see Table 5), but no change to conclusions.
| Analysisa | Time to treatment failureb | Time to first seizured | Time to 12‐month remission | Time to six‐month remission | |
| Original analysis (adjusted for seizure type) | Participants | Overall: 676 (Foc: 520; Gen: 156) | Overall: 822 (Foc: 584; Gen 238) | Overall: 683 (Foc: 525; Gen:158) | Overall: 683 (Foc: 525; Gen:158) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.66 (0.49 to 0.88) P = 0.005, I² = 66% Gen: 0.65 (0.35 to 1.23) P = 0.19, I² = 0% Overall: 0.66 (0.50 to 0.86) P = 0.002, I² = 35% | Foc: 1.31 (1.04 to 1.66) P = 0.02, I² = 0% Gen: 0.80 (0.55 to 1.15) P = 0.22, I² = 54% Overall: 1.13 (0.93 to 1.38) P = 0.22, I² = 46% | Foc: 0.92 (0.67 to 1.25) P = 0.59, I² = 63% Gen: 1.56 (0.99 to 2.44) P = 0.05, I² = 0% Overall: 1.09 (0.84 to 1.40) P = 0.52, I² = 51% | Foc: 0.86 (0.67 to 1.11) P = 0.24, I² = 62% Gen: 1.45 (0.99 to 2.12) P = 0.06, I² = 0% Overall: 1.01 (0.81 to 1.24) P = 0.95, I² = 58% | |
| Sensitivity analysis excluding Placencia 1993b | Participants | Overall: 487 (Foc: 388; Gen 99) | Overall: 630 (Foc: 451; Gen: 179) | Overall: 492 (Foc: 392; Gen:100) | Overall: 492 (Foc: 392; Gen:100) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.58 (0.42 to 0.79) P = 0.0006, I² = 45% Gen: 0.66 (0.32 to 1.32) P = 0.24, I² = 0% Overall: 0.59 (0.44 to 0.79) P = 0.0003, I² = 6% | Foc: 1.22 (0.94 to 1.58) P = 0.13, I² = 0% Gen: 0.86 (0.57 to 1.28) P = 0.46, I² = 62% Overall: 1.10 (0.89 to 1.37) P = 0.38, I² = 39% | Foc: 1.14 (0.80 to 1.62) P = 0.47, I² = 0% Gen: 1.41 (0.84 to 2.37) P = 0.19, I² = 0% Overall: 1.22 (0.91 to 1.63) P = 0.18; I² = 0% | Foc: 1.10 (0.81 to 1.49) P = 0.56, I² = 0% Gen: 1.23 (0.76 to 1.99) P = 0.40, I² = 0% Overall: 1.13 (0.87 to 1.47) P = 0.34, I² = 0% | |
| Sensitivity analysis for de Silva 1996c | Participants | Overall: 633 (Foc: 498: Gen: 135) | Overall: 779 (Foc: 562; Gen: 217) | Overall: 640 (Foc: 503; Gen: 137) | Overall: 640 (Foc: 503; Gen: 137) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.69 (0.51 to 0.93) P = 0.01, I² = 47% Gen: 0.73 (0.37 to 1.45) P = 0.37, I² = 0% Overall: 0.69 (0.53 to 0.91) P = 0.009, I² = 0% | Foc: 1.30 (1.02 to 1.64) P = 0.03; I² = 0% Gen: 0.81 (0.56 to 1.19) P = 0.29, I² = 53% Overall: 1.14 (0.93 to 1.39) P = 0.21; I² = 42% | Foc: 0.94 (0.68 to 1.29) P = 0.69, I² = 62% Gen: 1.68 (1.06 to 2.69) P = 0.03, I² = 0% Overall: 1.13 (0.87 to 1.46) P = 0.37, I² = 51% | Foc: 0.87 (0.67 to 1.13) P = 0.31; I² = 65% Gen: 1.51 (1.02 to 2.23) P = 0.04, I² = 0% Overall: 1.03 (0.83 to 1.28) P = 0.79, I² = 65% | |
| Sensitivity analysis classifying generalised onset seizures and age at onset > 30 as focal onset seizures | Participants | Overall: 676 (Foc: 566; Gen: 110) | Overall: 822 (Foc: 649; Gen: 173) | Overall: 683 (Foc: 571; Gen: 112) | Overall: 683 (Foc: 569; Gen: 114) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.66 (0.49 to 0.88), P = 0.005, I² = 63% Gen: 0.67 (0.35 to 1.28) P = 0.22, I² = 0% Overall: 0.66 (0.5 to 0.86) P = 0.002, I² = 31% | Foc: 1.29 (1.04 to 1.62) P = 0.02, I² = 0% Gen: 0.70 (0.45 to 1.07) P = 0.10, I² = 0% Overall: 1.14 (0.93 to 1.39) P = 0.20, I² = 17% | Foc: 0.97 (0.73 to 1.30) P = 0.85, I² = 52% Gen: 1.53 (0.96 to 2.44) P = 0.08, I² = 0% Overall: 1.10 (0.86 to 1.40) P = 0.45, I² = 41% | Foc: 0.91 (0.71 to 1.15) P = 0.41, I² = 43% Gen: 1.30 (0.82 to 2.08) P = 0.27, I² = 0% Overall: 0.97 (0.79 to 1.20) P = 0.81, I² = 21% | |
| Sensitivity analysis classifying generalised onset seizures and age at onset > 30 as uncertain seizure type | Participants | Overall: 676 (Foc: 520; Gen: 110; Unc: 46) | Overall: 822 (Foc: 584; Gen: 173; Unc: 65) | Overall: 683 (Foc: 525; Gen:112; Unc: 46) | Overall: 683 (Foc: 525; Gen:112; Unc: 46) |
| Pooled HR (95% CI) P value, I² (%) | Foc: 0.66 (0.49 to 0.88) P = 0.005, I² = 66% Gen: 0.67 (0.35 to 1.28) P = 0.22, I² = 0% Unc: 0.77 (0.18 to 3.27) P = 0.72, I² = 0% Overall: 0.66 (0.51 to 0.86) P = 0.002, I² = 16% | Foc: 1.31 (1.04 to 1.66) P = 0.02, I² = 0% Gen: 0.70 (0.45 to 1.07) P = 0.10, I² = 0% Unc: 0.82 (0.40 to 1.69) P = 0.59, I² = 58% Overall: 1.11 (0.91 to 1.35) P = 0.32, I² = 30% | Foc: 0.92 (0.67 to 1.25) P = 0.59, I² = 63% Gen: 1.53 (0.96 to 2.44) P = 0.08, I² = 0% Unc: 1.85 (0.77 to 4.42) P = 0.17, I² = 0% Overall: 1.12 (0.87 to 1.43) P = 0.42, I² = 42% | Foc: 0.86 (0.67 to 1.11) P = 0.24, I² = 62% Gen: 1.30 (0.82 to 2.08) P = 0.27, I² = 0% Unc:1.67 (0.85 to 3.28) P = 0.14, I² = 3% Overall: 1.00 (0.81 to 1.23) P = 0.27, I² = 0% | |
CI: confidence interval; Foc: focal onset seizures; Gen: generalised onset seizures; HR: hazard ratio; Unc: uncertain seizure type
aFor time to treatment failure and time to first seizure, HR < 1 indicates a clinical advantage for carbamazepine and for time to 12‐month and six‐month remission, HR < 1 indicates a clinical advantage for phenobarbitone. All results presented are calculated from fixed‐effect meta‐analysis.
bWe performed sensitivity analysis excluding all randomised participants in Placencia 1993 because of inadequate allocation concealment in the trial. We performed further sensitivity analysis for the outcome 'time to treatment failure' because of inconsistencies between published data and individual participant data for Placencia 1993 and for the outcome 'time to treatment failure due to adverse events' (see Sensitivity analysis and Effects of interventions for full details).
cWe performed sensitivity analysis including only the participants in de Silva 1996, who were randomised before the phenobarbitone arm was withdrawn. We also performed this sensitivity analysis for the outcomes 'time to treatment failure due to adverse events' and 'time to treatment failure due to lack of efficacy (see Sensitivity analysis and Effects of interventions for full details).
dWe performed sensitivity analyses due to inconsistencies between published data and individual participant data for Banu 2007 (see Sensitivity analysis and Effects of interventions for full details).
We also performed sensitivity analysis excluding Placencia 1993 from time to treatment failure due to adverse events; results were very similar to the Analysis 1.5, heterogeneity was still present in analysis and conclusions unchanged (result unchanged for individuals with generalised seizures (no participants with generalised seizures withdrew from carbamazepine due to adverse events in Placencia 1993), for individuals with focal onset seizures, pooled HR 0.63, (95% CI 0.43, 0.91; P = 0.01; I² = 73%), and overall pooled HR adjusted for seizure type, 0.65 (95% CI 0.46 to 0.92; P = 0.02, I² = 55%). No participants withdrew from Placencia 1993 due to lack of efficacy so we did not perform any sensitivity analysis excluding Placencia 1993 for time to treatment failure due to adverse events.
Further, in Placencia 1993, we also found inconsistencies (between IPD dataset and published results), in the number of participants who failed treatment or withdrew from treatment for certain reasons, which the trial authors could not resolve. These inconsistencies were as follows.
-
Results from the IPD dataset: treatment failed in 51 participants, 31 from carbamazepine and 20 from phenobarbitone: 16 participants left the area (lost to follow‐up), 10 failed due to adverse effects, 22 withdrew from treatment for personal reasons or no stated reason (classed as an event), and three died (cause of death not related to treatment, censored in analysis). See Table 4 for further details.
-
Results in the trial report: 53 participants failed treatment, 31 from carbamazepine and 22 from phenobarbitone: 18 participants left the area (lost to follow‐up), five failed because of adverse effects, three died, and 27 withdrew from treatment for personal reasons or no stated reason.
As the overall number of events and censored observations was similar (results from the IPD dataset: 51 withdrew, 32 events, 19 censored; and results in the trial report: 53 withdrew, 32 events, 21 censored), and as our sensitivity analysis excluding results of Placencia 1993 gave similar results and an unchanged conclusion, we felt that these inconsistencies were minor and were unlikely to have had a large impact on the overall results.
In the primary analysis of Placencia 1993, we classed those who withdrew for 'no clearly articulated reason' as events in the analysis; in other words, the treatment failure was due to the trial drug. However, it is also possible that these participants may have withdrawn for reasons not related to the trial drug, and we therefore should have censored them in the analysis. We performed a further sensitivity analysis censoring the 19 participants who withdrew for 'no clearly articulated reason'. Again, the results of the sensitivity analysis were similar to the primary analysis, showing a statistically significant advantage for carbamazepine (pooled HR 0.61, 95% CI 0.46 to 0.81, P = 0.0006, adjusted for seizure type; fixed‐effect meta‐analysis), and again, heterogeneity was substantially reduced after censoring these participants (I² = 6%). Heterogeneity was also reduced in the subgroup with focal onset seizures, pooled HR 0.60 (95% CI 0.44 to 0.82, P = 0.001, I² = 38%), compared to Analysis 1.4.
The sensitivity analysis of 'time to treatment failure for any reason related to treatment' including only the 20 participants randomised in de Silva 1996 before the withdrawal of the phenobarbitone arm gave similar results with a pooled HR (adjusted for seizure type for 633 participants), of 0.69 (95% CI 0.53 to 0.91, P = 0.009), and heterogeneity between trials was reduced to I² = 0% in this analysis. Results within each seizure group were also very similar in this sensitivity analysis (see Table 5 for further details). Results were also very similar for 'time to treatment failure due to adverse events' (pooled HR adjusted for seizure type, 0.56 (95% CI 0.38 to 0.81); P = 0.002, I² = 0%; fixed‐effect meta‐analysis), and conclusions unchanged, but for 'time to treatment failure due to adverse events', the clinical advantage for carbamazepine was no longer statistically significant in this sensitivity analysis (pooled HR adjusted for seizure type, 0.71 (95% CI 0.49 to 1.01); P = 0.06, I² = 12%; fixed‐effect meta‐analysis).
In the sensitivity analyses to investigate misclassification of seizure type, following reclassification of the 46 participants aged 30 or older in Heller 1995 and Placencia 1993 with new onset generalised seizures reclassified to focal onset seizures or an uncertain seizure type, results were very similar and conclusions were unchanged (see Table 5).
Summary of results for the primary outcome
Results for the primary outcome 'time to treatment failure for any reason related to treatment', in addition to the outcomes 'time to treatment failure due to adverse events' and 'time to treatment failure due to lack of efficacy' suggest a statistically significant advantage to carbamazepine; in other words, treatment failure may occur significantly earlier on phenobarbitone than carbamazepine. A statistically significant advantage for carbamazepine is also observed in the subgroup of participants experiencing new focal onset seizures and a potential (non‐statistically significant), advantage for the smaller subgroup of individuals experiencing generalised onset seizures (23% of total participants). There was no evidence of any interaction between treatment and seizure type.
Inadequate allocation concealment in Placencia 1993 may have influenced withdrawal rates if participants or personnel, or both, were aware of which drug the participants had been assigned; from the data we received, 19% of participants withdrew from the carbamazepine arm, and 15% of participants withdrew from the phenobarbitone arm while the other three trials included in the analysis showed more participants withdrawing from the phenobarbitone arm than the carbamazepine arm. Furthermore, inconsistencies between published data and data provided to us and unclear definitions for reason of treatment failure (participants withdrew for 'no clearly articulated reason'), was likely to have influenced the results of our analysis. These factors in the Placencia 1993 trial, in addition to the continuation of the carbamazepine arm in de Silva 1996 after the withdrawal of the phenobarbitone arm, are all factors that are likely to have contributed to the heterogeneity in Analysis 1.1 and Analysis 1.4. These factors may have confounded the results of our primary analyses in this review.
Secondary outcomes
Time to first seizure post‐randomisation
For this outcome, a HR less than one indicates a clinical advantage for carbamazepine.
We had data for 822 participants from six trials (98.3% of 836 participants from Banu 2007; de Silva 1996; Heller 1995; Mattson 1985; Ogunrin 2005 and Placencia 1993 (see Included studies and Table 3)). de Silva 1996 did not record the randomised drug for six participants, and dates of seizure recurrence were not available for eight participants (4 randomised to carbamazepine and 4 to phenobarbitone), in Mattson 1985; therefore, we did not include these 14 participants in the analysis.
Four hundred and fifty‐three out of 822 participants (55%), experienced seizure recurrence, 264 out of 434 (61%), on carbamazepine and 189 out of 388 (49%), on phenobarbitone. The overall pooled HR (for 822 participants), was 1.15 (95% CI 0.95 to 1.40, P = 0.15; fixed‐effect meta‐analysis; Analysis 1.7), suggesting a potential advantage for phenobarbitone (i.e. that first seizure recurrence may occur later on phenobarbitone compared to carbamazepine), that was not statistically significant. There was no evidence of any important statistical heterogeneity between trials (I² = 30%).
Subgroup analyses: seizure type (focal versus generalised onset)
For participants with focal onset seizures (584 participants from six trials), the pooled HR of 1.31 (95% CI 1.04 to 1.66, P = 0.02; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.8), suggested a statistically significant advantage for phenobarbitone; in other words that first seizure recurrence occurs later on phenobarbitone compared to carbamazepine. There was no evidence of statistical heterogeneity between trials for participants with focal onset seizures (I² = 0%). For participants with generalised onset seizures (238 participants from five trials), the pooled HR was 0.80 (95% CI 0.55 to 1.15, P = 0.22; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.8), suggesting a potential advantage for carbamazepine that was not statistically significant. A considerable amount of statistical heterogeneity was present between trials for participants with generalised onset seizures (I² = 54%). When we repeated the analysis with random‐effects meta‐analysis, the pooled HR of 0.85 (95% CI 0.48 to 1.50, P = 0.58), still showed an advantage for carbamazepine that was not statistically significant. There was a statistically significant interaction between treatment and seizure type (generalised versus focal onset; test for subgroup differences: P = 0.02, I² = 80.2% variability due to subgroup differences; Analysis 1.8, calculated with fixed‐effect meta‐analysis). In other words, phenobarbitone may have an advantage over carbamazepine for individuals with focal seizures and vice versa for individuals with generalised onset seizures.
Overall, the pooled HR (adjusted for seizure type for 822 participants, fixed‐effect), was 1.13 (95% CI 0.93 to 1.38, P = 0.22; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.8), suggesting a potential advantage for phenobarbitone that was not statistically significant. A moderate amount of heterogeneity was present between trials (I² = 46%). When we repeated the analysis with random‐effects meta‐analysis, the results were similar and conclusions unchanged (pooled HR adjusted for seizure type 1.11, 95% CI 0.82 to 1.51, P = 0.22).
Sensitivity analysis
We used fixed‐effect meta‐analysis to perform all sensitivity analyses.
We performed sensitivity analysis excluding participants from Placencia 1993 from analysis because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 5). This sensitivity analysis suggested in a potential advantage for phenobarbitone which was not statistically significant; overall pooled HR of 1.10 (95% CI 0.89 to 1.37, P = 0.38, adjusted for seizure type, fixed‐effect meta‐analysis), and slightly reduced heterogeneity (I² = 39% reduced from I² = 46% in Analysis 1.8; see Table 5). Results for individuals with focal seizures also suggested a potential advantage for phenobarbitone that was not statistically significant; pooled HR of 1.22 (95% CI 0.94 to 1.58, P = 0.13; fixed‐effect meta‐analysis); there was no heterogeneity present in the original analysis (Analysis 1.8), or within sensitivity analysis (I² = 0%). For individuals with generalised onset seizures, the sensitivity analysis suggested a potential advantage for carbamazepine, which was not statistically significant; pooled HR of 0.86 (95% CI 0.57 to 1.28; P = 0.46; fixed‐effect meta‐analysis), but a slight increase in heterogeneity (I² = 62% reduced from I² = 54% in Analysis 1.8; see Table 5). Following sensitivity analysis, there was no significant evidence of an interaction between treatment and seizure type (test for subgroup differences: P = 0.15, I² = 52% variability due to subgroup differences)
In Banu 2007, we found inconsistencies (between the IPD dataset and published results), which the trial authors could not resolve; the publication reported that only seven participants not had experienced any seizures from the start of treatment (three participants randomised to phenobarbitone and four randomised to carbamazepine); however, from IPD provided, 21 participants did not experience any seizures from the start of treatment (12 randomised to phenobarbitone and nine randomised to carbamazepine). Given these inconsistencies and the limited data available on seizure recurrence, we performed sensitivity analysis excluding the participants from Banu 2007 from Analysis 1.8. This sensitivity analysis resulted in a pooled HR of 1.20 (95% CI 0.97 to 1.48, P = 0.31; adjusted for seizure type; fixed‐effect meta‐analysis), suggesting a slightly larger advantage to phenobarbitone, which was still not statistically significant. There was also a slight increase in heterogeneity (I² = 52% reduced from I² = 46% in Analysis 1.8). For individuals with focal onset seizures, following sensitivity analysis, results were numerically similar and conclusions unchanged (pooled HR 1.38, 95% CI 1.08 to 1.78; P = 0.01; I² = 0%). For individuals with generalised seizures, the sensitivity analysis resulted in similar numerical results and unchanged conclusions (pooled HR 0.81, 95% CI 0.54 to 1.22; P = 0.31), but again slightly increased heterogeneity (I² = 65% reduced from I² = 54% in Analysis 1.8). There was a statistically significant interaction between treatment and seizure type (generalised versus focal onset), in this sensitivity analysis (test for subgroup differences: P = 0.03, I² = 78.9% variability due to subgroup differences).
The sensitivity analysis including only the 20 participants randomised in de Silva 1996 before the withdrawal of the phenobarbitone arm gave very similar numerical results and no change to conclusions or the amount of heterogeneity present in analysis overall in both seizure type subgroups for individuals with focal onset seizures (see Table 5 for further details). There was a statistically significant interaction between treatment and seizure type (generalised versus focal onset), in this sensitivity analysis (test for subgroup differences: P = 0.04, I² = 76.1% variability due to subgroup differences).
In the sensitivity analyses to investigate misclassification of seizure type, following reclassification of the 65 participants aged 30 or older with new onset generalised seizures in Heller 1995, Ogunrin 2005 and Placencia 1993 to focal onset seizures or an uncertain seizure type, in both sensitivity analyses, heterogeneity within the subgroup of individuals with generalised seizures is reduced to I² = 0% (compared to I² = 54% in Analysis 1.8, see Table 5). From visual inspection of forest plots in Analysis 1.8, it was clear that Ogunrin 2005 appears to be the main source of the heterogeneity between trials in the subgroup of participants with generalised onset seizures. The other four trials showed moderate, non‐significant advantages to carbamazepine, while Ogunrin 2005 showed a large, significant effect size in favour of phenobarbitone. This effect was not observed in the subgroup of participants with focal onset seizures in Ogunrin 2005. Following reclassification of 19 participants aged 30 or older with new onset generalised seizures in Ogunrin 2005 to an uncertain seizure type, a large, but imprecise effect towards phenobarbitone is also shown (Analysis 1.9), therefore it appears to be these participants introducing inconsistency into Analysis 1.8. Within the remaining 11 participants classified as experiencing new onset seizures (over the age of 30 at seizure onset), no participants on phenobarbitone experienced first seizure recurrence, therefore we could not calculate a hazard ratio for this reclassified subgroup (see Analysis 1.9). For both of the analyses reclassifying seizure type, there was statistically significant evidence of an interaction between treatment and seizure type (test for subgroup differences: P = 0.01, I² = 83.9% variability due to subgroup differences for generalised onset and over the age of 30 at onset reclassified to focal onset, and test for subgroup differences: P = 0.03, I² = 71.6% variability due to subgroup differences for generalised onset and over the age of 30 at onset reclassified to uncertain seizure type); in other words phenobarbitone may have an advantage over carbamazepine for individuals with focal seizures and vice versa for individuals with generalised onset seizures.
Summary of results for time to first seizure post‐randomisation
Overall, the results for secondary outcome 'time to first seizure post‐randomisation' suggest that there may be a difference in efficacy of the drugs (in terms of time to first seizure recurrence after randomisation), by seizure type. That is, that participants with generalised seizures experience seizure recurrence later on carbamazepine than phenobarbitone, and that participants with focal onset seizures experience seizure recurrence later on phenobarbitone than carbamazepine. The overall trend towards a slight potential advantage for phenobarbitone for all included participants probably reflects that the majority of participants included in this analysis had focal onset seizures (71% of 822 included participants). However, heterogeneity was present within some analyses, and results were robust to all sensitivity analyses. It was possible that inconsistencies in data provided to us (Banu 2007), and misclassification of seizure type in participants over the age of 30 (Heller 1995;Ogunrin 2005; Placencia 1993), inadequate allocation concealment in the Placencia 1993 trial, in addition to the continuation of the carbamazepine arm in de Silva 1996 after the withdrawal of the phenobarbitone arm may have confounded the results of this analysis. However, within some sensitivity analyses to take account of these confounding factors, particularly within the sensitivity analyses to take account of misclassification of seizure type, heterogeneity was greatly reduced and the association between treatment and seizure type still existed and therefore could be a true association.
Time to achieve 12‐month remission
For this outcome, a HR less than one indicates a clinical advantage for phenobarbitone.
Data for 683 participants from four trials were available for analyses of time to 12‐month remission and time to six‐month remission (98.8% of 691 participants from de Silva 1996; Heller 1995; Mattson 1985 and Placencia 1993 (see Included studies and Table 3), and 46.9% of the total 1455 participants from the 13 included trials). Mattson 1985 recorded no follow‐up data for one participant randomised to carbamazepine. de Silva 1996 did not record the randomised drug for six participants, and in Placencia 1993, seizure data after occurrence of first seizure were not available for one participant randomised to phenobarbitone, so we did not include this participant in the analyses. The trial duration of Ogunrin 2005 was 12 weeks, so 12‐month remission was not possible among participants in this trial. Banu 2007 recorded the date of first seizure after randomisation, but all dates of subsequent seizures were not available; therefore, we could calculate 'time to first seizure' but not 'time to six‐month remission' and 'time to 12‐month remission'.
Two hundred and eighty out of 683 participants (41%), achieved 12‐month remission; 163 out of 384 (45%), on carbamazepine and 117 out of 319 (37%), on phenobarbitone. The overall pooled HR (for 683 participants), was 1.09 (95% CI 0.85 to 1.40, P = 0.51; fixed‐effect meta‐analysis; Analysis 1.10), suggesting no clear advantage for either drug. There was no evidence of statistical heterogeneity between trials (I² = 0%).
Subgroup analyses: seizure type (focal versus generalised onset)
For participants with focal onset seizures (525 participants from four trials), the pooled HR was 0.92 (95% CI 0.67 to 1.25, P = 0.59; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.11), suggesting no clear advantage for either drug. A considerable amount of statistical heterogeneity was present between trials for participants with focal onset seizures (I² = 67%). When we repeated the analysis with random‐effects, the pooled HR was 1.24 (95% CI 0.69 to 2.22, P = 0.49), suggesting a potential advantage to phenobarbitone that was not statistically significant; in other words, six‐month remission may occur earlier on phenobarbitone that carbamazepine but confidence intervals are wide so we cannot rule out an advantage to carbamazepine or no differences between the drugs. For participants with generalised onset seizures (158 participants from three trials), the pooled HR was 1.56 (95% CI 0.99 to 2.44, P = 0.05; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.11), suggesting a borderline statistically significant advantage for carbamazepine. There was no evidence of statistical heterogeneity between trials for participants with generalised seizures (I² = 0%). There was potential evidence of an interaction between treatment and seizure type (generalised onset versus focal onset), (test for subgroup differences: P = 0.06, I² = 72.2% variability due to subgroup differences, see Analysis 1.11, calculated with fixed‐effect meta‐analysis).
Overall, the pooled HR (adjusted for seizure type for 683 participants), was 1.09 (95% CI 0.84 to 1.40, P = 0.52; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.11), suggesting no clear overall advantage for either drug, but a considerable amount of heterogeneity was present between trials (I² = 51%). When we repeated the analysis with random‐effects, results were similar and conclusions unchanged (pooled HR 1.06 (95% CI 0.72 to 1.57, P = 0.77).
Sensitivity analysis
We used fixed‐effect meta‐analysis to perform all sensitivity analyses.
We performed sensitivity analysis excluding participants from Placencia 1993 from the analysis of 'time to treatment failure for any reason related to treatment' because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 5). This sensitivity analysis suggested a potential advantage for carbamazepine, which was not statistically significant; overall pooled HR of 1.22 (95% CI 0.91 to 1.63, P = 0.18, adjusted for seizure type, fixed‐effects meta‐analysis), and greatly reduced heterogeneity (I² = 0% reduced from I² = 51% in Analysis 1.11; see Table 5). Results for individuals with focal seizures also suggested a potential advantage for carbamazepine, which was not statistically significant; pooled HR of 1.14 (95% CI 0.80 to 1.62, P = 0.47; fixed‐effect meta‐analysis), and greatly reduced heterogeneity (I² = 0% reduced from I² = 63% in Analysis 1.11; see Table 5). For individuals with generalised onset seizures, there was no heterogeneity present in the original analysis (Analysis 1.11), or within sensitivity analysis (I² = 0%). The sensitivity analysis suggested a potential advantage for carbamazepine, which was not statistically significant; pooled HR of 1.41 (95% CI 0.84 to 2.37; P = 0.19; fixed‐effect meta‐analysis). Following sensitivity analysis, there was no evidence of an interaction between treatment and seizure type (test for subgroup differences: P = 0.50, I² = 0% variability due to subgroup differences)
Also, within Placencia 1993, there was evidence that the proportional hazards assumption of the Cox model may have been violated; the P value of the time‐varying covariate was < 0.001. On closer inspection of the participants in Placencia 1993, all 60 participants who achieved 12‐month remission achieved immediate remission (i.e. did not have any seizures at all in the first 12 months of follow‐up). The trial followed up a further 42 participants for more than 365 days (up to 548 days); however, none of these participants achieved a 12‐month period of seizure freedom during the trial, so we censored them all at their last follow‐up date (after 365 days). This observation would explain the apparent change in treatment effect over time in Placencia 1993, and therefore the violation of the proportional hazards assumption. When we analysed separately those who achieved immediate 12‐month remission, the proportional hazards assumption was satisfied (P value of time‐varying covariate was 0.872). The proportional hazards assumption of the Cox model were satisfied for all other trials included in the analysis.
The sensitivity analysis including only the 20 participants randomised in de Silva 1996 before the withdrawal of the phenobarbitone arm gave very similar numerical results and no change to conclusions or the amount of heterogeneity present in analysis overall and for individuals with focal onset seizures. For individuals with generalised onset seizures, results were numerically similar, but sensitivity analysis showed a statistically significant advantage to carbamazepine, pooled HR for 137 participants, 1.68 (95% CI 1.06 to 2.69; P = 0.03, I² = 0%; fixed‐effect meta‐analysis); in other words, 12‐month remission occurred significantly earlier on carbamazepine than phenobarbitone for individuals with generalised seizures (see Table 5 for further details).
In the sensitivity analyses to investigate misclassification of seizure type, following reclassification of the 46 participants aged 30 or older with new onset generalised seizures in Heller 1995 and Placencia 1993 to focal onset seizures or an uncertain seizure type, results were very similar and there was no change to conclusions or the amount of heterogeneity present in analysis overall and for individuals with focal onset seizures. For the subgroup of individuals with generalised seizures (following reclassification), the potential advantage to carbamazepine was no longer statistically significant (see Table 5). For both of the analyses reclassifying seizure type, there was no evidence of an interaction between treatment and seizure type (test for subgroups differences: P = 0.11, I² = 61.4% variability due to subgroup differences for generalised onset and over the age of 30 at onset reclassified to focal onset and test for subgroups differences: P = 0.10, I² = 57.4% variability due to subgroup differences for generalised onset and over the age of 30 at onset reclassified to uncertain seizure type.)
Summary of results for time to achieve 12‐month remission
Overall, the results for secondary outcome 'time to 12‐month remission' do not show consistent or clear differences between the drugs and heterogeneity between may have confounded the results. Subgroup analyses by seizure type and sensitivity analyses suggest a potential advantage for carbamazepine, that is, that 12‐month remission may be achieved more quickly on carbamazepine than phenobarbitone but these results are not statistically significant.
From visual inspection of forest plots and sensitivity analysis, it was clear that Placencia 1993 was the main source of the heterogeneity between trials in the subgroup of participants with focal onset seizures and overall in all participants. The other three trials showed moderate, non‐significant effect sizes, while Placencia 1993 showed a large, significant effect size in favour of phenobarbitone (see Analysis 1.11). This effect was not shown in the subgroup of participants with generalised onset seizures in participants in Placencia 1993 and when we excluded Placencia 1993 from the meta‐analysis in sensitivity analysis, the heterogeneity present in analysis was reduced to zero. This could have been a knock‐on effect of the inadequate allocation concealment in this trial, which was likely to have influenced the withdrawal rates in this trial, and in turn the number of participants remaining in the trial who could achieve 12‐month remission. Furthermore, the distribution of 12‐month remission times in Placencia 1993 (all participants who achieved 12 month remission achieved it immediately, and all those who did not were censored), may have influenced the result of this trial. As for our primary outcome, we conclude that the inclusion of this trial may have confounded the results of this outcome.
Time to achieve six‐month remission
For this outcome, a HR less than one indicates a clinical advantage for phenobarbitone.
Time to six‐month remission was available for 683 participants from four of the trials providing IPD (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993; see 'time to 12‐month remission' for further details of available data). Three hundred and eighty‐seven out of 683 participants (57%), achieved six‐month remission, 213 out of 384 (59%), on carbamazepine and 117 out of 319 (55%), on phenobarbitone. The overall pooled HR (for 683 participants), was 0.98 (95% CI 0.80 to 1.21, P = 0.86; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.12), suggesting no clear advantage for either drug. There was no evidence of statistical heterogeneity between trials (I² = 17%).
Subgroup analyses: seizure type (focal versus generalised onset)
For participants with focal onset seizures (525 participants from four trials), the pooled HR of 0.86 (95% CI 0.67 to 1.11, P = 0.24; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.13), which suggests a potential advantage for phenobarbitone that was not statistically significant. A considerable amount of statistical heterogeneity was present between trials for participants with focal onset seizures (I² = 62%). When we repeated the analysis with random‐effects, the pooled HR of 0.87 (95% CI 0.55 to 1.37, P = 0.54), results were similar and conclusions unchanged. For participants with generalised onset seizures (158 participants from three trials), the pooled HR was 1.45 (95% CI 0.99 to 2.12, P = 0.06; moderate‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.13), suggesting a potential advantage for carbamazepine, which is not statistically significant. There was no evidence of statistical heterogeneity between trials for participants with generalised seizures (I² = 0%). There was statistically significant evidence of an interaction between treatment and seizure type (generalised versus focal onset; P = 0.03, I² = 80.0% variability due to subgroup differences, see Analysis 1.13, calculated with fixed‐effect meta‐analysis).
Overall, the pooled HR (adjusted for seizure type for 683 participants, fixed‐effect meta‐analysis), was 1.01 (95% CI 0.81 to 1.24, P = 0.95; low‐quality evidence; fixed‐effect meta‐analysis; Analysis 1.13), suggesting no clear advantage for either drug, but a considerable amount of heterogeneity was present between trials (I² = 58%). When we repeated the analysis with random‐effects meta‐analysis, results were similar and conclusions unchanged (pooled HR 1.06 (95% CI 0.74 to 1.51, P = 0.75).
Sensitivity analysis
We used fixed‐effect meta‐analysis to perform all sensitivity analyses.
We performed sensitivity analysis excluding participants from Placencia 1993 from the analysis of 'time to treatment failure for any reason related to treatment' because of high risk of selection bias due to inadequate allocation concealment (see Allocation (selection bias) and Table 5). This sensitivity analysis suggested a potential advantage for carbamazepine, which was not statistically significant; overall pooled HR of 1.13 (95% CI 0.87 to 1.47, P = 0.34, adjusted for seizure type; fixed‐effect meta‐analysis), and greatly reduced heterogeneity (I² = 0% reduced from I² = 58% in Analysis 1.13; see Table 5). Results for individuals with focal seizures also suggested a potential advantage for carbamazepine, which was not statistically significant; pooled HR of 1.10 (95% CI 0.81 to 1.49, P = 0.56; fixed‐effect meta‐analysis), and greatly reduced heterogeneity (I² = 0% reduced from I² = 62% in Analysis 1.13; see Table 5). For individuals with generalised onset seizures, there was no heterogeneity present in the original analysis (Analysis 1.13), or within sensitivity analysis (I² = 0%). The sensitivity analysis suggested a potential advantage for carbamazepine, which was not statistically significant; pooled HR of 1.23 (95% CI 0.76 to 1.99; P = 0.40; fixed‐effect meta‐analysis). Following sensitivity analysis, there was no evidence of an interaction between treatment and seizure type (test for subgroup differences: P = 0.69, I² = 0% variability due to subgroup differences)
The sensitivity analysis including only the 20 participants randomised in de Silva 1996 before the withdrawal of the phenobarbitone arm gave very similar numerical results and no change to conclusions or the amount of heterogeneity present in analysis overall and for individuals with focal onset seizures. For individuals with generalised onset seizures, results were numerically similar, but sensitivity analysis showed a statistically significant advantage to carbamazepine, pooled HR for 137 participants, 1.51 (95% CI 1.02 to 2.23; P = 0.04, I² = 0%; fixed‐effect meta‐analysis); in other words, six‐month remission occurred significantly earlier on carbamazepine than phenobarbitone for individuals with generalised seizures (see Table 5 for further details).
In the sensitivity analyses to investigate misclassification of seizure type, following reclassification of the 46 participants aged 30 or older with new onset generalised seizures in Heller 1995 and Placencia 1993 to focal onset seizures or an uncertain seizure type, results were very similar and there was no change to conclusions or the amount of heterogeneity present in analysis overall and for individuals with focal onset seizures. For the subgroup of individuals with generalised seizures (following reclassification), the potential advantage to carbamazepine was no longer statistically significant (see Table 5). For both of the analyses reclassifying seizure type, there was no evidence of an interaction between treatment and seizure type (test for subgroups differences: P = 0.17, I² = 46.1% variability due to subgroup differences for generalised onset and over the age of 30 at onset reclassified to focal onset, and test for subgroups differences: P = 0.09, I² = 58.5% variability due to subgroup differences for generalised onset and over the age of 30 at onset reclassified to uncertain seizure type.
Summary of results for time to achieve six‐month remission
Overall, the results for secondary outcome 'time to six‐month remission' are very similar to results for 'time to 12‐month remission.' No consistent or clear differences between the drugs have been shown and heterogeneity between them may have confounded the results. Subgroup analyses by seizure type suggest a potential interaction between treatment and seizure type (that phenobarbitone may have an advantage over carbamazepine for individuals with focal seizures and vice versa for individuals with generalised onset seizures). However, this potential interaction was not robust to sensitivity analysis (excluding Placencia 1993 from analysis and reclassification of seizure type).
As for the analysis of 'time to six‐month remission,' from visual inspection of forest plots and sensitivity analysis, it was clear that Placencia 1993 was the main source of the heterogeneity between trials in the subgroup of participants with focal onset seizures and overall in all participants. The other three trials showed moderate, non‐significant effect sizes, while Placencia 1993 showed a large, significant effect size in favour of phenobarbitone (see Analysis 1.13). This effect was not shown in the subgroup of participants with generalised onset seizures in participants in Placencia 1993, and when Placencia 1993 was excluded from the meta‐analysis in sensitivity analysis, the heterogeneity present in analysis was reduced to zero. This could have been a knock‐on effect of the inadequate allocation concealment in this trial, which was likely to have influenced the withdrawal rates in this trial, and in turn the number of participants remaining in the trial who could achieve six‐month remission. As for other outcomes of this review, we conclude that the inclusion of this trial may have confounded the results of this outcome.
Incidence of adverse events
We extracted all reported information related to adverse events from the trial publications. Cossu 1984 did not report any findings related to adverse events, and without access to protocols we are uncertain if these data were collected (see Selective reporting (reporting bias)). See Table 6 for details of all adverse event data provided in the other 12 trials included in this review. Two trials reported only numbers of withdrawals from the trial due to adverse events (Chen 1996; Czapinski 1997), and two reported the rate of adverse events/number of participants reporting adverse events (Bidabadi 2009; Placencia 1993); these four trials did not report specific adverse events. It was difficult to summarise the 'most common' adverse events overall across the 12 trials or deduce whether carbamazepine or phenobarbitone were most associated with specific adverse events because of the differences in methods of reporting adverse event data across the trials. For the eight trials that did report specific adverse events, the events reported by two or more trials were as follows.
| Trial | Adverse event dataa | Summary of reported results | |
| CBZ | PB | ||
| Reported list of 'problems' at the last visit (provided as IPD) | n = 54
| n = 54
| |
| Rate of drug side‐effects | No statistical significant difference was seen after treatment between 2 groups in the rate of drug side‐effects | No statistical significant difference was seen after treatment between 2 groups in the rate of drug side‐effects | |
| Most frequently observed side‐effects | Gastrointestinal side‐effects and "impaired function" (general malaise). Frequency not clearly stated | Gastrointestinal side‐effects and "impaired function" (general malaise). Frequency not clearly stated | |
| Withdrawal from the trial due to 'allergic reactions' | n = 24 1 participant withdrew due to an allergic reaction | n = 23 2 participants withdrew due to allergic reactions | |
| No adverse events reported | Not reported | Not reported | |
| "Exclusions due to adverse events or no efficacy" | n = 30 Proportion "excluded": 30% | n = 30 Proportion "excluded": 33.3% | |
| "Unacceptable" adverse events leading to drug withdrawal | n = 54
| n = 10
| |
| Reports of minor adverse events and side‐effects leading to drug withdrawal | n = 150
| n = 152
| |
| "Unacceptable" adverse events leading to drug withdrawal | n = 61
| n = 58
| |
| Narrative report of "adverse effects" and "serious side‐effects" | n = 155
No serious side‐effects | n = 155
No serious side‐effects | |
| Systemic side‐effects and side‐effects leading to drug change | n = 15 4 participants switched from CBZ to PB; 3 due to systemic side‐effects (1 with persistent rashes and 1 with marked granulocytopenia (decrease of granulocytes (white blood cells)) and 1 due to behavioural changes | n = 18 1 participant switched from PB to CBZ due to substantial behavioural side‐effects | |
| Participant‐reported symptomatic complaints (provided as IPD) | n = 19
| n = 18
| |
| Number of participants reporting side‐effects | n = 95 53 participants reported at least 1 side‐effect | n = 97 50 participants reported at least 1 side‐effect | |
CBZ: carbamazepine; IPD: individual participant data; n: number; PB: phenobarbitone
aWe recorded adverse event data as reported narratively in the publications; therefore, exact definition of a symptom may vary. Adverse event data were supplied as IPD for Banu 2007 and Ogunrin 2005. Adverse event data were not requested in original IPD requests (de Silva 1996; Heller 1995; Mattson 1985; Placencia 1993).
bParticipants may report more than one adverse event.
cBidabadi 2009 and Czapinski 1997 are abstracts only so reported very little information.
dNote that the recruited participants in this trial were institutionalised; therefore, the "precise nature of side‐effects was not always determinable". The two most frequently occurring side‐effects were reported as the frequency of participants reporting the side‐effect on each day of the treatment period; however, overall totals of participants reporting each side‐effect were not reported.
eParticipants may have withdrawn due to adverse event alone or a combination of adverse events and poor efficacy (seizures).
fThe phenobarbitone arm of de Silva 1996 was stopped prematurely after 10 children were randomised to this arm because of concerns over behavioural adverse events (see the 'Characteristics of included studies' tables).
Adverse events with carbamazepine
-
Gastrointestinal side effects including abdominal pain, nausea, and vomiting (Cereghino 1974; Mattson 1985)
-
Drowsiness/tiredness/fatigue/sedation (Banu 2007; de Silva 1996; Heller 1995)
-
Headaches (Banu 2007; Heller 1995)
-
Motor disturbance (including ataxia, incoordination, nystagmus, tremor, slowing of mental function, inattention, psychomotor retardation), (Banu 2007; Mattson 1985; Ogunrin 2005)
-
Dysmorphic and idiosyncratic side effects (rash, gum hypertrophy, hirsutism, acne, other skin problems), (Feksi 1991; Heller 1995; Mattson 1985; Mitchell 1987; Ogunrin 2005)
-
Cognitive side effects and impairments including depression and memory problems (Banu 2007; Feksi 1991; Heller 1995; Ogunrin 2005)
-
Behaviour‐related side effects (aggression, behavioural changes, etc.), (Banu 2007; Feksi 1991; Mitchell 1987)
Adverse events with phenobarbitone
-
Gastrointestinal side effects including abdominal pain, nausea, and vomiting (Banu 2007; Cereghino 1974; Heller 1995; Mattson 1985)
-
Drowsiness/tiredness/fatigue/sedation (Banu 2007; de Silva 1996; Heller 1995)
-
Motor disturbance (including ataxia, incoordination, nystagmus, tremor, slowing of mental function, inattention, psychomotor retardation), (Banu 2007; Mattson 1985; Ogunrin 2005)
-
Dysmorphic and idiosyncratic side effects (rash, gum hypertrophy, hirsutism, acne, other skin problems), (de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985)
-
Cognitive side effects and impairments, including depression and memory problems (Banu 2007; Feksi 1991; Ogunrin 2005)
-
Behaviour‐related side effects (aggression, behavioural changes, etc.), (Banu 2007; de Silva 1996; Mitchell 1987)
Discussion
Summary of main results
The results of this review provide statistically significant, moderate‐quality evidence of an advantage for carbamazepine over phenobarbitone for our primary global effectiveness outcome 'time to treatment failure'. In other words, treatment failure may occur significantly earlier on phenobarbitone than carbamazepine.
Considering time to treatment failure for any reason related to treatment, for 676 participants providing IPD from four trials, the pooled HR adjusted for seizure type was 0.66 (95% CI 0.50 to 0.86; P = 0.002; adjusted for seizure type; moderate‐quality evidence). This advantage was also present for time to treatment failure due to adverse events (pooled HR adjusted for seizure type: 0.69 (95% CI 0.49 to 0.97; P = 0.03; low‐quality evidence), and time to treatment failure due to lack of efficacy (pooled HR adjusted for seizure type: 0.54 (95% CI 0.38 to 0.78; P = 0.0008; moderate‐quality evidence).
A statistically significant advantage for carbamazepine is also observed in the subgroup of participants experiencing new focal onset seizures and a potential (non‐statistically significant), advantage for the smaller subgroup of individuals experiencing generalised onset seizures (23% of total participants); there was no evidence of any interaction between treatment and seizure type. However, a substantial amount of heterogeneity was present between results for individuals with focal seizures, which is likely to have originated from inadequate allocation concealment, which may have influenced withdrawal rates in one trial precutting 192 participants (Placencia 1993, contributing 28% of data to this meta‐analysis), and the early withdrawal of the phenobarbitone arm in another trial due to concerns of serious behavioural adverse events (de Silva 1996), and may have confounded the results the primary outcomes of this review.
For our secondary outcomes, 'time to first seizure post‐randomisation', 'time to 12‐month remission' and 'time to six‐month remission'), we did not find any statistically significant differences between carbamazepine and phenobarbitone overall and evidence for these outcomes was moderate to low quality. Any differences found by seizure type were not consistent or robust to sensitivity analysis and some subgroup analyses were likely confounded by heterogeneity. For all of these outcomes, over 70% of included participants were classified as experiencing new onset focal seizures, therefore the direction of overall results (adjusted by seizure type), are likely influenced by this majority seizure type.
Results of these outcomes suggest that there may be an association between treatment effect in terms of efficacy and seizure type; that is, that participants with focal onset seizures experience seizure recurrence later and hence remission of seizures earlier on phenobarbitone than carbamazepine, and vice versa for individuals with generalised seizures. It is likely that the analyses of these outcomes were confounded by several methodological issues, which could have introduced the heterogeneity and inconsistency; such as misclassification of seizure type in participants over the age of 30 in these trials (Heller 1995;Ogunrin 2005; Placencia 1993), which seems to have had a particular impact on the results of Ogunrin 2005, inconsistencies in IPD provided to us (Banu 2007), in addition to the methodological issues within de Silva 1996 and Placencia 1993 described above. Therefore it is unknown whether this apparent association between treatment efficacy and seizure type is a true association or not.
Limited information was available regarding adverse events in the trials and we were unable to compare the rates of adverse events between carbamazepine and phenobarbitone. Some adverse events reported on both drugs were abdominal pain, nausea, and vomiting, drowsiness, motor and cognitive disturbances, dysmorphic side effects (such as rash), and behavioural side effects in three paediatric trials.
Overall completeness and applicability of evidence
We have gratefully received IPD for 1138 individuals (78% of individuals from all eligible trials), from the authors of seven trials (Banu 2007; de Silva 1996; Feksi 1991; Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993), which included a comparison of phenobarbitone with carbamazepine for the treatment of epilepsy. However, we were not able to include the data from one trial (Feksi 1991), recruiting 302 participants (representing 21% of the total number in the 13 eligible trials and 27% of the total number of participants from the trials for which we received IPD), because of many inconsistencies in the dataset that could not be resolved and we felt were too extensive to account for in sensitivity analysis (see Included studies).
We also could not include 317 individuals (22%), from the other six relevant trials (Bidabadi 2009; Cereghino 1974; Chen 1996; Cossu 1984; Czapinski 1997; Mitchell 1987), in any analysis, as IPD were not available and the published reports did not report outcomes of interest. Therefore, we could include IPD for 836 participants in at least one outcome of this review, representing 57% of 1455 individuals from all 13 identified eligible trials.
While we received IPD for 836 participants, we were not able to include all data in all of our analyses. Because of the short, three‐month duration of the trial, we were unable to include 37 participants from Ogunrin 2005 in our remission analyses, and in this short follow‐up time, no participants withdrew from treatment; therefore, this trial could not contribute to our primary outcome of 'time to treatment failure' either. We were also unable to include 108 participants from Banu 2007 in analyses of treatment failure and remission as we did not receive dates of treatment failures and subsequent seizures after first seizure recurrence. Therefore, our primary outcome was, in fact, based on 676 participants (47% of individuals from all eligible trials).
Having to exclude data from nearly half of the eligible participants due to lack of IPD and insufficient reporting in trial publications was likely to have had an impact on the applicability of the evidence; therefore, we encourage caution in the interpretation of all results in this review. However, it was difficult to quantify exactly how large this impact was on the results of this review (see Potential biases in the review process).
Four trials contributing around 80% of the participant data to this review recruited adults only (Heller 1995; Mattson 1985; Ogunrin 2005; Placencia 1993); the other two trials contributing around 20% of data were paediatric trials (Banu 2007; de Silva 1996). Also, the largest single trial contributing over a third of the participant data to this review, Mattson 1985, recruited individuals with focal onset seizures only. Therefore, only around 30% of participants included in this review were experiencing generalised onset seizures. Furthermore, there is evidence within this review to suggest that up to 27% of individuals with newly onset generalised seizures may have had their seizure type misclassified. For these reasons, the results of this review may not be fully generalisable to children or to individuals with generalised onset seizures, and more evidence recruiting these types of participants is required.
The adverse event profiles of the two drugs, particularly phenobarbitone with relation to behavioural changes in children, are well documented (see Description of the intervention). Results of this review suggest that phenobarbitone may be more likely to be failed earlier than carbamazepine for any treatment‐related reason and due to adverse events; however, results across trials were variable and should be interpreted with caution. While we found no consistent differences between the two drugs in terms of efficacy; results of this review suggest a potential association between treatment efficacy and seizure type (see Summary of main results); yet the direction of this association (advantage for carbamazepine for generalised seizures and advantage for phenobarbitone for focal seizures), was unexpected given documented evidence that carbamazepine may exacerbate some generalised seizure types, such as myoclonic and absence seizures (Liporace 1994; Shields 1983; Snead 1985), and that current guidelines recommend carbamazepine as a first‐line drug for the treatment of focal seizures (NICE 2012).
Evidence from previous reviews conducted by Cochrane Epilepsy as part of this series of pair‐wise reviews for monotherapy in epilepsy (Marson 2000; Nevitt 2018b; Nevitt 2017b), suggests that misclassification of seizure type is an important issue in epilepsy trials (Malafosse 1994). We believe that the results of the original trials, and hence the results of the outcome 'time to first seizure' in this review, are likely to have been confounded by classification bias, particularly the 19 individuals from Ogunrin 2005 classified with new onset generalised seizures over the age of 30, and contributing a large amount of variability to the analysis.
Ogunrin 2005 classified generalised and focal onset seizures according to the International League Against Epilepsy (ILAE), classification of 1981 (Commission 1981), rather than the revised ILAE classification in 1989 (Commission 1989), which may have led to misclassification. Furthermore, Ogunrin 2005 was conducted in Nigeria, a lower middle‐income country without access to the same facilities as trials conducted in the USA and Europe; therefore, seizure types were classified clinically, and electroencephalographics (EEGs)/magnetic resonance images (MRIs), were not required for diagnosis of epilepsy. Clinical classification may also have contributed to potential misclassification in this trial.
As described in Summary of main results, results of this review are likely to be confounded by heterogeneity and methodological inadequacies of the included trials. Therefore, this apparent association may not be a true association and all results of this review should be interpreted with caution. We would not advocate basing a choice between these two drugs on the results of this review alone.
Quality of the evidence
The six trials for which IPD were made available were generally of relatively good methodological quality; however, four out of the six trials for which we received IPD were at high risk of bias for at least one aspect (see Figure 3), which may have introduced bias into analyses. While an IPD approach to analysis allows us to use unpublished data, therefore reducing attrition and reporting bias, for two of the trials contributing 36% of participant data, we found inconsistencies between published data and participant data provided to us in terms of treatment failure information and seizure recurrence, respectively (Banu 2007; Placencia 1993), which the trial authors could not resolve. In both cases, it was likely that the inconsistencies within these trials contributed to the considerable heterogeneity present within the analyses in this review.
Three of the trials contributing 27% of the participant data to this review described adequate methods of randomisation and allocation concealment (de Silva 1996; Heller 1995; Ogunrin 2005); however, the other two largest single trials contributing 50% of participant data to this review did not describe the method of randomisation or allocation concealment used, or both, and this information was not available from trial authors (Banu 2007; Mattson 1985). We are uncertain whether this lack of information has affected the results of this review. One trial contributing 23% of participant data to this review reported that an adequate method of allocation concealment was not used for all randomised participants, and following sensitivity analyses, we believe this inadequate allocation concealment may have influenced rates of withdrawal if participants, or clinicians, or both, were aware of the allocated treatment, which may have had a further knock‐on effect on our seizure and remission outcomes.
Three of the trials providing IPD blinded participants and outcome assessors (Banu 2007; Mattson 1985; Ogunrin 2005); and the other two trials, de Silva 1996 and Heller 1995, were designed as pragmatic open‐label trials, as masking of treatment would not be "practicable or ethical", would "undermine compliance", and would "introduce bias due to a very large dropout rate" as blinding does not conform to standard clinical practice of increasing drug doses to therapeutic ranges (Heller 1995). Despite this reasoning, considering the largest trials conducted within the USA and Europe, the rates of treatment failure for reasons related to the trial drug across the double‐blind (Mattson 1985), and open‐label (de Silva 1996; Heller 1995), trials included in 'time to treatment failure' were quite similar (see Table 4 for further details):
-
44% of participants failed treatment in Mattson 1985 (52% randomised to phenobarbitone and 36% randomised to carbamazepine);
-
34% of participants failed treatment in Heller 1995 (40% randomised to phenobarbitone and 28% randomised to carbamazepine);
-
46% of participants failed treatment in de Silva 1996 (80% from phenobarbitone and 40% from carbamazepine).
It is however, debatable whether double‐blind design is the most appropriate for trials of monotherapy in epilepsy of long duration, and whether such a design does have an impact upon the dropout rate, and therefore, the results of the trial. The overall treatment failure rate in de Silva 1996 was greatly influenced by the high treatment failure rate of children randomised to phenobarbitone (80%), which led to the withdrawal of that treatment arm from the four‐treatment trial because of concerns of serious adverse events. It is difficult to know if preconceptions of phenobarbitone and documented associations of the drug with adverse behavioural effects in children directly led to the withdrawal of the drug, and if the same outcome would have occurred if the trial had been double‐blinded. It is also interesting to note that within the other paediatric trial within this review, which was blinded and conducted in a rural area of Bangladesh (Banu 2007), there were no documented failures of the allocated treatment (carbamazepine or phenobarbitone), due to adverse events, and in fact, in this trial, significantly more children withdrew from carbamazepine than phenobarbitone for reasons related to the trial drug (11% withdrew from phenobarbitone, 26% withdrew from carbamazepine, Chi² test, P = 0.05, see Table 4). Unfortunately, we could not include this trial in the analysis of 'time to treatment failure' as dates of treatment failure were not available for all participants. Furthermore, a trial comparing phenobarbitone with phenytoin conducted in India (Pal 1998), in which phenobarbitone was concluded to be an "effective and acceptable antiepileptic drug for rural Indian children" did not report concerns regarding adverse events of phenobarbitone in children.
We note the influence of country of recruitment over the methodological design and perhaps the results of the trial. Within the USA and Europe, where many treatment options are available, phenobarbitone is no longer considered to be a first‐line agent, in favour of more tolerable first‐line agents, such as carbamazepine and lamotrigine (NICE 2012), whereas in low‐ and middle‐income countries or rural regions, where income is limited and newer generation antiepileptic drugs are not readily available or affordable, older and cheaper drugs, such as phenobarbitone, are more likely to be used as comparators.
Trials for which no IPD were available were generally of poorer quality than those for which we received IPD. A lot of methodological information in these trials was not reported or was unclear. Two trials presented incomplete outcome data following exclusion of participants (Chen 1996; Feksi 1991); one trial used an inadequate cross‐over design for investigating monotherapy treatments (Cereghino 1974); two trials were likely to have been underpowered to detect a difference between the drugs (Cossu 1984; Mitchell 1987); one trial may have been underpowered, too; and two trials available only in abstract or summary form, provided only very limited information on trial methodology (Bidabadi 2009; Czapinski 1997).
Overall, due to the documented methodological issues that may have introduced heterogeneity, biases and imprecision into our meta‐analyses, we rated the evidence provided in this review as moderate to low quality according to GRADE criteria (See summary of findings Table for the main comparison and summary of findings Table 2), and would not advocate use of the evidence in this review for clinical decision‐making between the two drugs.
Potential biases in the review process
We were able to include IPD for 836 out of 1455 eligible participants (57%), from six out of 13 trials in this review and conducted all analyses as IPD analyses. Such an approach has many advantages, such as allowing the standardisation of definitions of outcomes across trials, and attrition and reporting biases are reduced, as we can perform additional analyses and calculate additional outcomes from unpublished data. For the outcomes we used in this review that are of a time‐to‐event nature, an IPD approach is considered to be the 'gold standard' approach to analysis (Parmar 1998).
However, despite the advantages of this approach, for reasons out of our control, we were not able to obtain IPD for 619 participants from seven eligible trials, and no aggregate data were available for our outcomes of interest in trial publications. We therefore had to exclude 43% of eligible participants from our analyses, which may have introduced bias into the review. Given that no statistically significant differences were found between the drugs in terms of proportions of participants seizure‐free and proportions of participants withdrawing from allocated treatment in the seven trials for which IPD were not available (where recorded, see Table 2), we do not believe that our conclusions would have changed for the outcomes of this review had the IPD for the seven trials been available. We do however, recommend caution when interpreting results of analyses of this review because of potential retrieval bias from the exclusion of 43% of eligible participants from seven trials in this review.
Furthermore, five out of the seven trials that we were not able to include in meta‐analysis were at high risk of bias for at least one methodological aspect (see Figure 3 and Risk of bias in included studies); therefore, inclusion of this data may have introduced bias into our results. We also judged four out of the six trials with IPD provided for analysis to be at high risk of bias for at least one methodological element. We addressed these issues in sensitivity analysis and discussed each analysis at length (see Sensitivity analysis and Effects of interventions).
Finally, we made some assumptions in the statistical methodology used in this review. Firstly, when we received only follow‐up dates and seizure frequencies, we used linear interpolation to estimate seizure times. We are aware that an individual's seizure patterns may be non‐linear; therefore, we recommend caution when interpreting the numerical results of the seizure‐related outcomes. We also made an assumption that treatment effect for each outcome did not change over time (proportional hazards assumption, see Data synthesis). We are aware that in trials of long duration (e.g. de Silva 1996, Heller 1995 and Mattson 1985 followed up participants for between 3 and 10 years), the assumption of treatment effect remaining constant over time may not be appropriate. For example, there is likely to be a difference between participants who achieve immediate remission compared with participants who achieve later remission, and we encourage that results should be interpreted with this limitation in mind.
Agreements and disagreements with other studies or reviews
To our knowledge, together with previous versions of this review, this is the only systematic review and meta‐analysis that compares phenobarbitone and carbamazepine monotherapy for focal onset seizures and generalised onset tonic‐clonic seizures. A network meta‐analysis has been published (Nevitt 2017a), comparing all direct and indirect evidence from phenobarbitone, carbamazepine, and other standard and new antiepileptic drugs licensed for monotherapy. The results of this review generally agree with the results of the network meta‐analysis; results of this network meta‐analysis showed a statistically significant advantage for carbamazepine compared with phenobarbitone for 'time to treatment failure' for participants with focal onset seizures and a statistically significant advantage for phenobarbitone compared with carbamazepine for 'time to first seizure' for participants with focal onset seizures. No statistically significant differences were found between the drugs for participants with generalised onset seizures.

Study flow diagram

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included trials
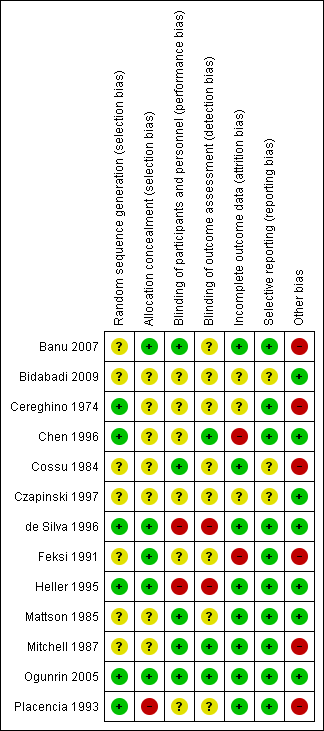
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included trial
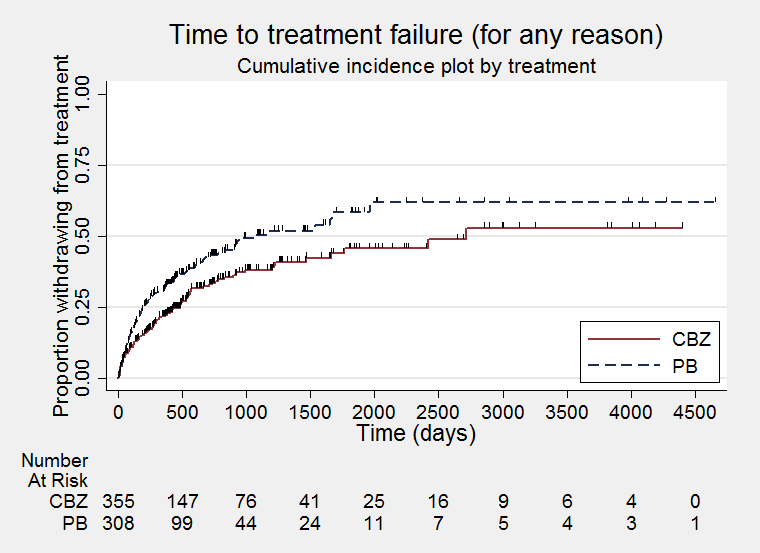
Time to treatment failure ‐ any reason related to the treatment (CBZ: carbamazepine; PB: phenobarbitone)

Time to treatment failure ‐ any reason related to the treatment, by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to treatment failure due to adverse events (CBZ: carbamazepine; PB: phenobarbitone)
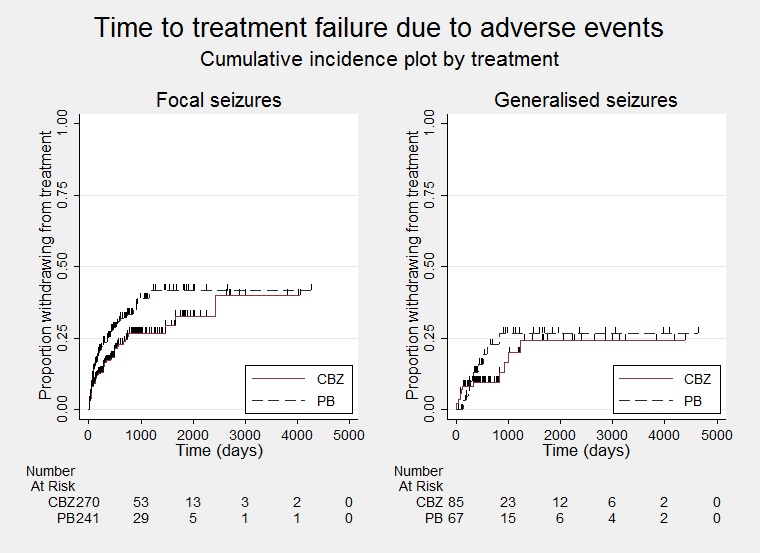
Time to treatment failure due to adverse events, by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to treatment failure due to lack of efficacy (CBZ: carbamazepine; PB: phenobarbitone)
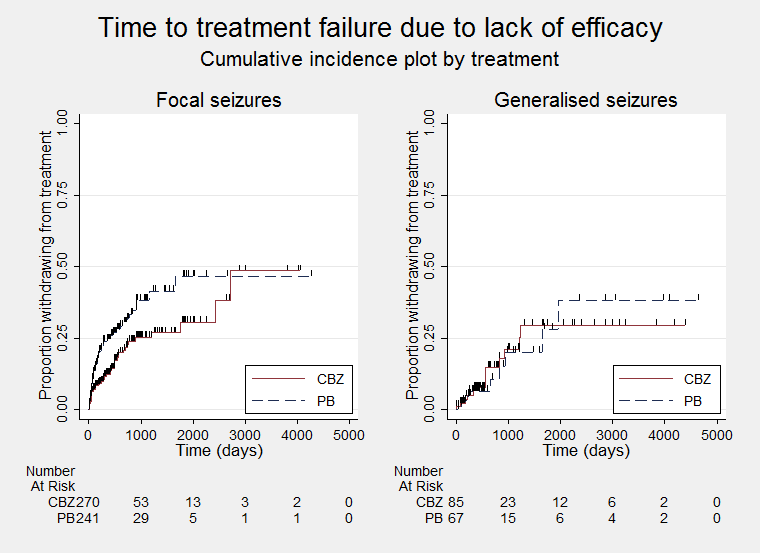
Time to treatment failure due to lack of efficacy, by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to first seizure post randomisation (CBZ: carbamazepine; PB: phenobarbitone)

Time to first seizure post randomisation ‐ by seizure type (CBZ: carbamazepine; PB: phenobarbitone)
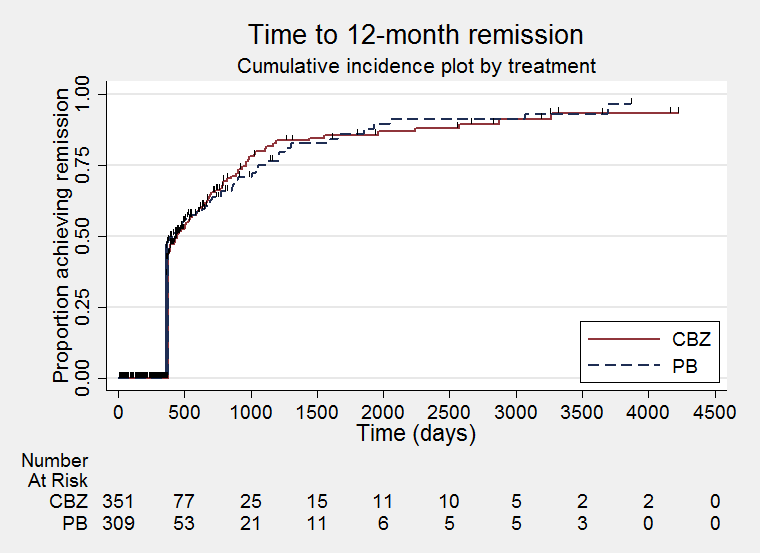
Time to 12‐month remission (CBZ: carbamazepine; PB: phenobarbitone)

Time to 12‐month remission ‐ by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Time to six‐month remission (CBZ: carbamazepine; PB: phenobarbitone)

Time to six‐month remission ‐ by seizure type (CBZ: carbamazepine; PB: phenobarbitone)

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 1 Time to treatment failure (any reason related to the treatment).

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 2 Time to treatment failure due to adverse events.

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 3 Time to treatment failure due to lack of efficacy.
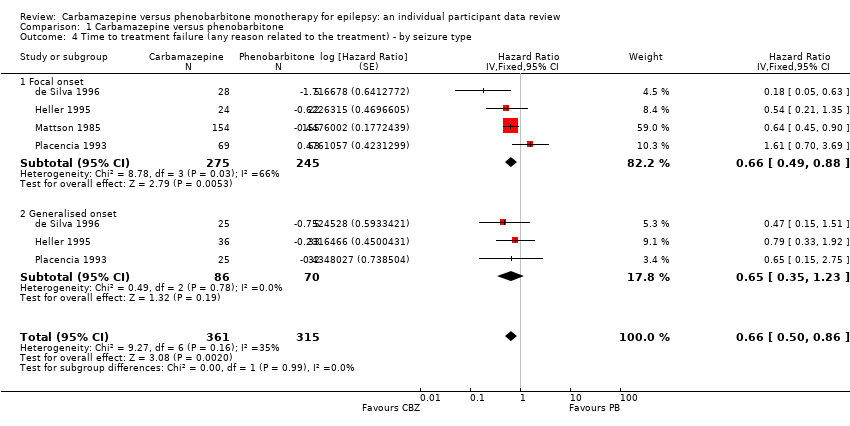
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 4 Time to treatment failure (any reason related to the treatment) ‐ by seizure type.
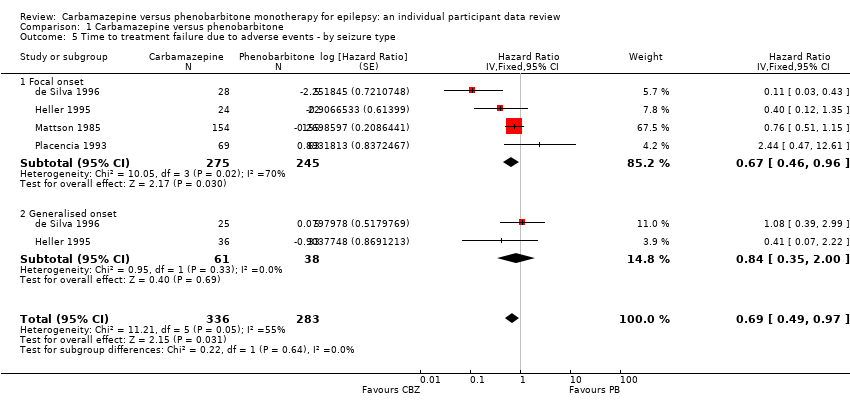
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 5 Time to treatment failure due to adverse events ‐ by seizure type.

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 6 Time to treatment failure due to lack of efficacy ‐ by seizure type.

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 7 Time to first seizure.

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 8 Time to first seizure ‐ by seizure type.

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 9 Time to first seizure ‐ sensitivity analysis.

Comparison 1 Carbamazepine versus phenobarbitone, Outcome 10 Time to 12‐month remission.
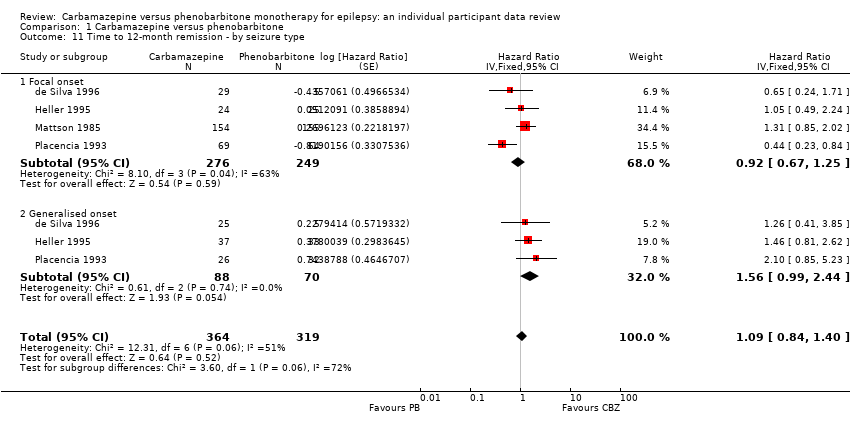
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 11 Time to 12‐month remission ‐ by seizure type.
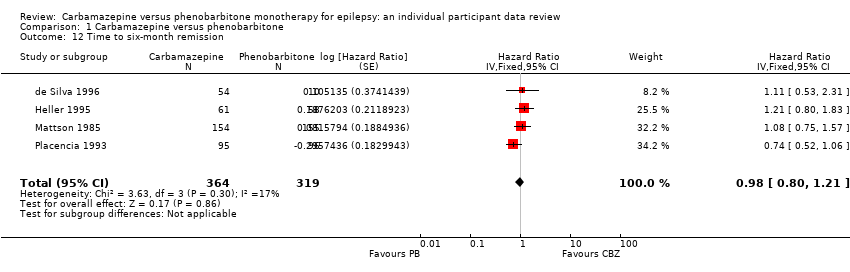
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 12 Time to six‐month remission.
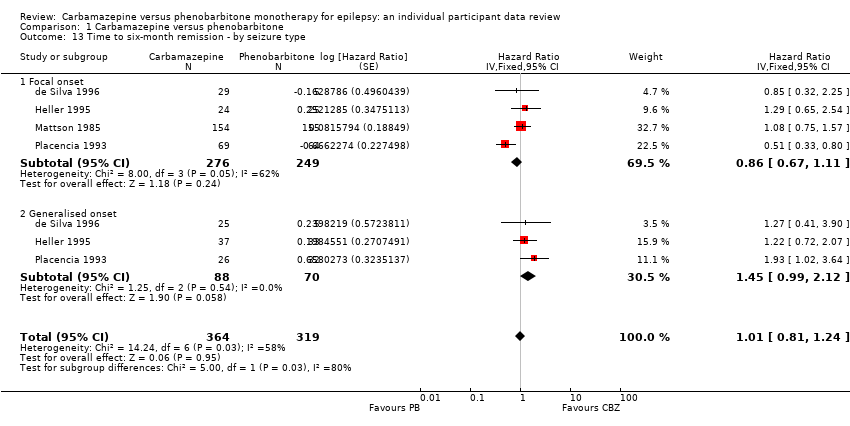
Comparison 1 Carbamazepine versus phenobarbitone, Outcome 13 Time to six‐month remission ‐ by seizure type.
| Carbamazepine compared with phenobarbitone for epilepsy (time to treatment failure) | ||||||
| Patient or population: adults and children with newly onset focal or generalised epilepsy Settings: outpatients Intervention: carbamazepine Comparison: phenobarbitone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Phenobarbitone | Carbamazepine | |||||
| Time to treatment failure (any reason related to treatment) All participants Range of follow‐up: 0 to 4653 days | The median time to treatment failure was 1059 days in the phenobarbitone group | The median time to treatment failure was 2717 days (1658 days longer) in the carbamazepine group | HR 0.66 (0.50 to 0.86)a | 676 (4 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine. Treatment failure due to adverse events (HR 0.69, 95% CI 0.49 to 0.97, P = 0.03, I² = 55%), and due to lack of efficacy (HR 0.54, 95% CI 0.38 to 0.78, P = 0.0008, I² = 0%), also occurred significantly earlier on phenobarbitone compared to carbamazepine. |
| Time to treatment failure (any reason related to treatment) Subgroup: focal onset seizures Range of follow‐up: 0 to 4272 days | The median time to treatment failure was 913 days in the phenobarbitone group | The median time to treatment failure was 2422 days (1509 days longer) in the carbamazepine group | HR 0.66 (0.49 to 0.88) | 520 (4 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine. Treatment failure due to adverse events (HR 0.67, 95% CI 0.46 to 0.96, P = 0.03, I² = 70%), and due to lack of efficacy (HR 0.54, 95% CI 0.36 to 0.80, P = 0.002, I² = 0%), also occurred significantly earlier on phenobarbitone compared to carbamazepine. |
| Time to treatment failure (any reason related to treatment) Subgroup: generalised onset tonic‐clonic seizures Range of follow‐up: 0 to 4653 days | The 25th percentiled of time to treatment failure was 605 days in the phenobarbitone group | The 25th percentiled of time to treatment failure was 825 days (220 days longer) in the carbamazepine group | HR 0.65 (0.35 to 1.23) | 156 | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine. There was also no statistically significant difference between drugs in treatment failure due to adverse events (HR 0.84, 95% CI 0.35 to 2.00, P = 0.69, I² = 0%), or treatment failure due to lack of efficacy: HR 0.56 (95% CI 0.23 to 1.35, P = 0.20, I² = 0%). |
| *Illustrative risks in the carbamazepine and phenobarbitone groups are calculated at the median time to treatment failure (i.e. the time to 50% of participants failing or withdrawing from allocated treatment) within each group across all trials. The relative effect (pooled hazard ratio) shows the comparison of 'time to treatment failure' between the treatment groups. CI: 95% confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| aPooled HR for all participants adjusted for seizure type. | ||||||
| Carbamazepine compared with phenobarbitone for epilepsy (secondary outcomes) | ||||||
| Patient or population: adults and children with newly onset focal or generalised epilepsy Settings: outpatients Intervention: carbamazepine Comparison: phenobarbitone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Phenobarbitone | Carbamazepine | |||||
| Time to first seizure (post‐randomisation) All participants Range of follow‐up: 0 to 4108 days | The median time to first seizure post‐randomisation was 218 days in the phenobarbitone group | The median time to first seizure post‐randomisation was 113 days (105 days shorter) in the carbamazepine group | HR 1.13 (0.93 to 1.38)a | 822 (6 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine |
| Time to first seizure (post‐randomisation) Subgroup: focal onset seizures Range of follow‐up: 0 to 4108 days | The median time to first seizure post‐randomisation was 266 days in the phenobarbitone group | The median time to first seizure post‐randomisation was 84 days (182 days shorter) in the carbamazepine group | HR 1.31 (1.04 to 1.66) | 584 (6 trials) | ⊕⊕⊕⊝ | HR < 1 indicates a clinical advantage for carbamazepine |
| Time to first seizure (post‐randomisation) Subgroup: generalised onset tonic‐clonic seizures Range of follow‐up: 0 to 4070 days | The median time to first seizure post‐randomisation was 209 days in the phenobarbitone group | The median time to first seizure post‐randomisation was 303 days (94 days longer) in the carbamazepine group | HR 0.80 (0.55 to 1.15) | 238 (5 trials) | ⊕⊕⊝⊝ | HR < 1 indicates a clinical advantage for carbamazepine |
| Time to achieve 12‐month remission (seizure‐free period) All participants Range of follow‐up: 0 to 4222 days | The median time to achieve to 12‐month remission was 413 days in the phenobarbitone group | The median time to achieve to 12‐month remission was 446 days (33 days longer) in the carbamazepine group | HR 1.09 (0.84 to 1.40)a | 683 | ⊕⊕⊝⊝ | HR < 1 indicates a |
| Time to achieve 12‐month remission (seizure‐free period) Subgroup: focal onset seizures Range of follow‐up: 0 to 4222 days | The median time to achieve to 12‐month remission was 369 days in the phenobarbitone group | The median time to achieve to 12‐month remission was 531 days (162 days longer) in the carbamazepine group | HR 0.92 (0.67 to 1.25) | 525 | ⊕⊕⊝⊝ | HR < 1 indicates a |
| Time to achieve 12‐month remission (seizure‐free period) Subgroup: generalised onset tonic‐clonic seizures Range of follow‐up: 0 to 4163 days | The median time to achieve to 12‐month remission was 421 days in the phenobarbitone group | The median time to achieve to 12‐month remission was 366 days (55 days shorter) in the carbamazepine group | HR 1.56 (0.99 to 2.44) | 158 | ⊕⊕⊝⊝ | HR < 1 indicates a |
| *Illustrative risks in the carbamazepine and phenobarbitone groups are calculated at the median time to first seizure or time to 12‐month remission (i.e. the time to 50% of participants experiencing a first seizure or 12‐months of remission) within each group across all trials. The relative effect (pooled hazard ratio) shows the comparison of 'time to first seizure' or 'time to 12‐month remission' between the treatment groups. CI: 95% confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| aPooled HR for all participants adjusted for seizure type. | ||||||
| Focal seizures: n (%)a | Male participants: n (%)a | Age at entry (years): Mean (SD), range | Aged > 30 and generalised seizures: n (%) | Epilepsy duration (years): mean (SD), range | Number of seizures in prior 6 months: median (range) | |||||||||||||
| CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | CBZ | PB | Missing | |
| 33 (61%) | 26 (48%) | 0 | 24 (44%) | 37 (69%) | 0 | 6.2 (3.6), 1 to 15 | 5.3 (3.3), 1 to 12 | 0 | 0 | 0 | 0 | 2.0 (2.4), 0 to 11.5 | 1.6 (2.0), 0 to 10 | 0 | 24 (1 to 7200) | 24 (2 to 4320) | 5 | |
| 29 (54%) | 5 (50%) | 0 | 30 (56%) | 4 (40%) | 6 | 9.2 (3.8), 2 to 15 | 9.1 (3.9), 3 to 14 | 6 | 0 | 0 | 0 | 1.7 (2.6), 0 to 12 | 1.3 (1.8), 0.1 to 5 | 6 | 3 (1 to 500) | 3 (1 to 170) | 6 | |
| 24 (39%) | 25 (43%) | 0 | 30 (49%) | 25 (43%) | 0 | 29.3 (14.1), 13 to 69 | 34.5 (15.1), 16 to 77 | 1 | 9 | 13 | 0 | 4.4 (7.4), 0.1 to 40 | 3.4 (6.6), 0 to 37 | 2 | 2 (1 to 354) | 3 (1 to 579) | 1 | |
| 155 (100%) | 155 (100%) | 0 | 133 (87%) | 135 (88%) | 4 | 42.1 (15.9), 18 to 82 | 40.1 (15.3), 18 to 75 | 4 | 0 | 0 | 0 | 5.9 (9.1), 0.5 to 55 | 5.7 (7.9), 0.5 to 36 | 5 | 1 (1 to 100) | 1 (1 to 14) | 7 | |
| 5 (26%) | 2 (11%) | 0 | 12 (63%) | 11 (61%) | 0 | 28.2 (5.8), 14 to 38 | 35.4 (6.2), 26 to 55 | 0 | 6 | 13 | 0 | NA | NA | 37 | 18 (6 to 36) | 12 (6 to 42) | 0 | |
| 69 (73%) | 64 (66%) | 0 | 37 (39%) | 30 (31%) | 0 | 29.3 (18.2), 2 to 68 | 28.7 (17.1), 2 to 68 | 0 | 11 | 13 | 0 | 9.5 (11.6), 0.5 to 54 | 9.8 (11.0), 0.5 to 48 | 0 | 1 (0 to 68) | 2 (0 to 100) | 0 | |
| CBZ: carbamazepine; n: number of participants; NA: not available; PB: phenobarbitone; SD: standard deviation aProportions (%) are calculated based on non‐missing data. | ||||||||||||||||||
| Trial | Outcomes reported | Summary of results |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
| PB (n = 123), CBZ (n = 126)
| |
|
|
| |
| CBZ: carbamazepine; IQ: intelligence quotient; PB: phenobarbitone; WISC‐R scale: the Wechsler Intelligence Scale for Children | ||
| Trial | Number randomised | Time to treatment failure | Time to 12‐month remission | Time to six‐month remission | Time to first seizure | ||||||||||
| CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | CBZ | PB | Total | |
| 54 | 54 | 108 | Data not available | Data not available | Data not available | 54 | 54 | 108 | |||||||
| 54 | 10 | 64 | 53 | 10 | 63 | 54 | 10 | 64 | 54 | 10 | 64 | 54 | 10 | 64 | |
| 61 | 58 | 119 | 60 | 55 | 115 | 61 | 58 | 119 | 61 | 58 | 119 | 61 | 58 | 119 | |
| 155 | 155 | 310 | 154 | 155 | 309 | 154 | 155 | 309 | 154 | 155 | 309 | 151 | 151 | 302 | |
| 19 | 18 | 37 | Data not available | Data not available | Data not available | 19 | 18 | 37 | |||||||
| 95 | 97 | 192 | 94 | 95 | 189 | 95 | 96 | 191 | 95 | 96 | 191 | 95 | 97 | 192 | |
| Total | 438 | 392 | 830 | 361 | 315 | 676 | 364 | 319 | 683 | 364 | 319 | 683 | 434 | 388 | 822 |
| CBZ: carbamazepine; PB: phenobarbitone | |||||||||||||||
| Reason for early termination | Total | ||||||||||||
| CBZ | PB | CBZ | PB | CBZ | PB | CBZ | PB | CBZ | PB | CBZ | PB | All | |
| Adverse events (event) | 3 | 2 | 8 | 12 | 11 | 5 | 5 | 5 | 0 | 0 | 27 | 24 | 51 |
| Lack of efficacy (event) | 12 | 2 | 5 | 7 | 3 | 11 | 0 | 0 | 8 | 6 | 28 | 26 | 54 |
| Both adverse events and lack of efficacy (event) | 6 | 4 | 4 | 3 | 31 | 46 | 0 | 0 | 0 | 0 | 41 | 53 | 94 |
| Non‐compliance/protocol violation (event) | 0 | 0 | 0 | 0 | 11 | 19 | 13 | 9 | 6 | 0 | 30 | 28 | 58 |
| Illness or death (not treatment‐related, censored) | 0 | 0 | 0 | 0 | 17 | 13 | 2 | 1 | 0 | 0 | 19 | 14 | 33 |
| Participant went into remission (censored) | 18 | 1 | 6 | 3 | 0 | 0 | 0 | 0 | 0 | 2 | 24 | 6 | 30 |
| Lost to follow‐up (censored) | 0 | 0 | 0 | 0 | 26 | 26 | 11 | 5 | 7 | 15 | 44 | 46 | 90 |
| Other (censored)d | 0 | 0 | 0 | 0 | 3 | 2 | 0 | 0 | 0 | 0 | 3 | 2 | 5 |
| Completed the trial (censored) | 14 | 1 | 37 | 30 | 52 | 33 | 63 | 75 | 33 | 31 | 199 | 170 | 369 |
| Total | 53 | 10 | 60 | 55 | 154 | 155 | 94 | 95 | 54 | 54 | 415 | 369 | 784 |
| CBZ: carbamazepine; PB: phenobarbitone | |||||||||||||
| Analysisa | Time to treatment failureb | Time to first seizured | Time to 12‐month remission | Time to six‐month remission | |
| Original analysis (adjusted for seizure type) | Participants | Overall: 676 (Foc: 520; Gen: 156) | Overall: 822 (Foc: 584; Gen 238) | Overall: 683 (Foc: 525; Gen:158) | Overall: 683 (Foc: 525; Gen:158) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.66 (0.49 to 0.88) P = 0.005, I² = 66% Gen: 0.65 (0.35 to 1.23) P = 0.19, I² = 0% Overall: 0.66 (0.50 to 0.86) P = 0.002, I² = 35% | Foc: 1.31 (1.04 to 1.66) P = 0.02, I² = 0% Gen: 0.80 (0.55 to 1.15) P = 0.22, I² = 54% Overall: 1.13 (0.93 to 1.38) P = 0.22, I² = 46% | Foc: 0.92 (0.67 to 1.25) P = 0.59, I² = 63% Gen: 1.56 (0.99 to 2.44) P = 0.05, I² = 0% Overall: 1.09 (0.84 to 1.40) P = 0.52, I² = 51% | Foc: 0.86 (0.67 to 1.11) P = 0.24, I² = 62% Gen: 1.45 (0.99 to 2.12) P = 0.06, I² = 0% Overall: 1.01 (0.81 to 1.24) P = 0.95, I² = 58% | |
| Sensitivity analysis excluding Placencia 1993b | Participants | Overall: 487 (Foc: 388; Gen 99) | Overall: 630 (Foc: 451; Gen: 179) | Overall: 492 (Foc: 392; Gen:100) | Overall: 492 (Foc: 392; Gen:100) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.58 (0.42 to 0.79) P = 0.0006, I² = 45% Gen: 0.66 (0.32 to 1.32) P = 0.24, I² = 0% Overall: 0.59 (0.44 to 0.79) P = 0.0003, I² = 6% | Foc: 1.22 (0.94 to 1.58) P = 0.13, I² = 0% Gen: 0.86 (0.57 to 1.28) P = 0.46, I² = 62% Overall: 1.10 (0.89 to 1.37) P = 0.38, I² = 39% | Foc: 1.14 (0.80 to 1.62) P = 0.47, I² = 0% Gen: 1.41 (0.84 to 2.37) P = 0.19, I² = 0% Overall: 1.22 (0.91 to 1.63) P = 0.18; I² = 0% | Foc: 1.10 (0.81 to 1.49) P = 0.56, I² = 0% Gen: 1.23 (0.76 to 1.99) P = 0.40, I² = 0% Overall: 1.13 (0.87 to 1.47) P = 0.34, I² = 0% | |
| Sensitivity analysis for de Silva 1996c | Participants | Overall: 633 (Foc: 498: Gen: 135) | Overall: 779 (Foc: 562; Gen: 217) | Overall: 640 (Foc: 503; Gen: 137) | Overall: 640 (Foc: 503; Gen: 137) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.69 (0.51 to 0.93) P = 0.01, I² = 47% Gen: 0.73 (0.37 to 1.45) P = 0.37, I² = 0% Overall: 0.69 (0.53 to 0.91) P = 0.009, I² = 0% | Foc: 1.30 (1.02 to 1.64) P = 0.03; I² = 0% Gen: 0.81 (0.56 to 1.19) P = 0.29, I² = 53% Overall: 1.14 (0.93 to 1.39) P = 0.21; I² = 42% | Foc: 0.94 (0.68 to 1.29) P = 0.69, I² = 62% Gen: 1.68 (1.06 to 2.69) P = 0.03, I² = 0% Overall: 1.13 (0.87 to 1.46) P = 0.37, I² = 51% | Foc: 0.87 (0.67 to 1.13) P = 0.31; I² = 65% Gen: 1.51 (1.02 to 2.23) P = 0.04, I² = 0% Overall: 1.03 (0.83 to 1.28) P = 0.79, I² = 65% | |
| Sensitivity analysis classifying generalised onset seizures and age at onset > 30 as focal onset seizures | Participants | Overall: 676 (Foc: 566; Gen: 110) | Overall: 822 (Foc: 649; Gen: 173) | Overall: 683 (Foc: 571; Gen: 112) | Overall: 683 (Foc: 569; Gen: 114) |
| Pooled HR (95% CI), P value, I² (%) | Foc: 0.66 (0.49 to 0.88), P = 0.005, I² = 63% Gen: 0.67 (0.35 to 1.28) P = 0.22, I² = 0% Overall: 0.66 (0.5 to 0.86) P = 0.002, I² = 31% | Foc: 1.29 (1.04 to 1.62) P = 0.02, I² = 0% Gen: 0.70 (0.45 to 1.07) P = 0.10, I² = 0% Overall: 1.14 (0.93 to 1.39) P = 0.20, I² = 17% | Foc: 0.97 (0.73 to 1.30) P = 0.85, I² = 52% Gen: 1.53 (0.96 to 2.44) P = 0.08, I² = 0% Overall: 1.10 (0.86 to 1.40) P = 0.45, I² = 41% | Foc: 0.91 (0.71 to 1.15) P = 0.41, I² = 43% Gen: 1.30 (0.82 to 2.08) P = 0.27, I² = 0% Overall: 0.97 (0.79 to 1.20) P = 0.81, I² = 21% | |
| Sensitivity analysis classifying generalised onset seizures and age at onset > 30 as uncertain seizure type | Participants | Overall: 676 (Foc: 520; Gen: 110; Unc: 46) | Overall: 822 (Foc: 584; Gen: 173; Unc: 65) | Overall: 683 (Foc: 525; Gen:112; Unc: 46) | Overall: 683 (Foc: 525; Gen:112; Unc: 46) |
| Pooled HR (95% CI) P value, I² (%) | Foc: 0.66 (0.49 to 0.88) P = 0.005, I² = 66% Gen: 0.67 (0.35 to 1.28) P = 0.22, I² = 0% Unc: 0.77 (0.18 to 3.27) P = 0.72, I² = 0% Overall: 0.66 (0.51 to 0.86) P = 0.002, I² = 16% | Foc: 1.31 (1.04 to 1.66) P = 0.02, I² = 0% Gen: 0.70 (0.45 to 1.07) P = 0.10, I² = 0% Unc: 0.82 (0.40 to 1.69) P = 0.59, I² = 58% Overall: 1.11 (0.91 to 1.35) P = 0.32, I² = 30% | Foc: 0.92 (0.67 to 1.25) P = 0.59, I² = 63% Gen: 1.53 (0.96 to 2.44) P = 0.08, I² = 0% Unc: 1.85 (0.77 to 4.42) P = 0.17, I² = 0% Overall: 1.12 (0.87 to 1.43) P = 0.42, I² = 42% | Foc: 0.86 (0.67 to 1.11) P = 0.24, I² = 62% Gen: 1.30 (0.82 to 2.08) P = 0.27, I² = 0% Unc:1.67 (0.85 to 3.28) P = 0.14, I² = 3% Overall: 1.00 (0.81 to 1.23) P = 0.27, I² = 0% | |
| CI: confidence interval; Foc: focal onset seizures; Gen: generalised onset seizures; HR: hazard ratio; Unc: uncertain seizure type aFor time to treatment failure and time to first seizure, HR < 1 indicates a clinical advantage for carbamazepine and for time to 12‐month and six‐month remission, HR < 1 indicates a clinical advantage for phenobarbitone. All results presented are calculated from fixed‐effect meta‐analysis. | |||||
| Trial | Adverse event dataa | Summary of reported results | |
| CBZ | PB | ||
| Reported list of 'problems' at the last visit (provided as IPD) | n = 54
| n = 54
| |
| Rate of drug side‐effects | No statistical significant difference was seen after treatment between 2 groups in the rate of drug side‐effects | No statistical significant difference was seen after treatment between 2 groups in the rate of drug side‐effects | |
| Most frequently observed side‐effects | Gastrointestinal side‐effects and "impaired function" (general malaise). Frequency not clearly stated | Gastrointestinal side‐effects and "impaired function" (general malaise). Frequency not clearly stated | |
| Withdrawal from the trial due to 'allergic reactions' | n = 24 1 participant withdrew due to an allergic reaction | n = 23 2 participants withdrew due to allergic reactions | |
| No adverse events reported | Not reported | Not reported | |
| "Exclusions due to adverse events or no efficacy" | n = 30 Proportion "excluded": 30% | n = 30 Proportion "excluded": 33.3% | |
| "Unacceptable" adverse events leading to drug withdrawal | n = 54
| n = 10
| |
| Reports of minor adverse events and side‐effects leading to drug withdrawal | n = 150
| n = 152
| |
| "Unacceptable" adverse events leading to drug withdrawal | n = 61
| n = 58
| |
| Narrative report of "adverse effects" and "serious side‐effects" | n = 155
No serious side‐effects | n = 155
No serious side‐effects | |
| Systemic side‐effects and side‐effects leading to drug change | n = 15 4 participants switched from CBZ to PB; 3 due to systemic side‐effects (1 with persistent rashes and 1 with marked granulocytopenia (decrease of granulocytes (white blood cells)) and 1 due to behavioural changes | n = 18 1 participant switched from PB to CBZ due to substantial behavioural side‐effects | |
| Participant‐reported symptomatic complaints (provided as IPD) | n = 19
| n = 18
| |
| Number of participants reporting side‐effects | n = 95 53 participants reported at least 1 side‐effect | n = 97 50 participants reported at least 1 side‐effect | |
| CBZ: carbamazepine; IPD: individual participant data; n: number; PB: phenobarbitone | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to treatment failure (any reason related to the treatment) Show forest plot | 4 | 676 | Hazard Ratio (Fixed, 95% CI) | 0.66 [0.51, 0.86] |
| 2 Time to treatment failure due to adverse events Show forest plot | 4 | 676 | Hazard Ratio (Fixed, 95% CI) | 0.67 [0.48, 0.93] |
| 3 Time to treatment failure due to lack of efficacy Show forest plot | 3 | 487 | Hazard Ratio (Fixed, 95% CI) | 0.54 [0.38, 0.77] |
| 4 Time to treatment failure (any reason related to the treatment) ‐ by seizure type Show forest plot | 4 | 676 | Hazard Ratio (Fixed, 95% CI) | 0.66 [0.50, 0.86] |
| 4.1 Focal onset | 4 | 520 | Hazard Ratio (Fixed, 95% CI) | 0.66 [0.49, 0.88] |
| 4.2 Generalised onset | 3 | 156 | Hazard Ratio (Fixed, 95% CI) | 0.65 [0.35, 1.23] |
| 5 Time to treatment failure due to adverse events ‐ by seizure type Show forest plot | 4 | 619 | Hazard Ratio (Fixed, 95% CI) | 0.69 [0.49, 0.97] |
| 5.1 Focal onset | 4 | 520 | Hazard Ratio (Fixed, 95% CI) | 0.67 [0.46, 0.96] |
| 5.2 Generalised onset | 2 | 99 | Hazard Ratio (Fixed, 95% CI) | 0.84 [0.35, 2.00] |
| 6 Time to treatment failure due to lack of efficacy ‐ by seizure type Show forest plot | 3 | 487 | Hazard Ratio (Fixed, 95% CI) | 0.54 [0.38, 0.78] |
| 6.1 Focal onset | 3 | 388 | Hazard Ratio (Fixed, 95% CI) | 0.54 [0.36, 0.80] |
| 6.2 Generalised onset | 2 | 99 | Hazard Ratio (Fixed, 95% CI) | 0.56 [0.23, 1.35] |
| 7 Time to first seizure Show forest plot | 6 | 822 | Hazard Ratio (Fixed, 95% CI) | 1.15 [0.95, 1.40] |
| 8 Time to first seizure ‐ by seizure type Show forest plot | 6 | 822 | Hazard Ratio (Fixed, 95% CI) | 1.13 [0.93, 1.38] |
| 8.1 Focal onset | 6 | 584 | Hazard Ratio (Fixed, 95% CI) | 1.31 [1.04, 1.66] |
| 8.2 Generalised onset | 5 | 238 | Hazard Ratio (Fixed, 95% CI) | 0.80 [0.55, 1.15] |
| 9 Time to first seizure ‐ sensitivity analysis Show forest plot | 6 | 822 | Hazard Ratio (Fixed, 95% CI) | 1.11 [0.91, 1.35] |
| 9.1 Focal onset | 6 | 584 | Hazard Ratio (Fixed, 95% CI) | 1.31 [1.04, 1.66] |
| 9.2 Generalised onset | 5 | 173 | Hazard Ratio (Fixed, 95% CI) | 0.70 [0.45, 1.07] |
| 9.3 Uncertain seizure type | 3 | 65 | Hazard Ratio (Fixed, 95% CI) | 0.82 [0.40, 1.69] |
| 10 Time to 12‐month remission Show forest plot | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 1.09 [0.85, 1.40] |
| 11 Time to 12‐month remission ‐ by seizure type Show forest plot | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 1.09 [0.84, 1.40] |
| 11.1 Focal onset | 4 | 525 | Hazard Ratio (Fixed, 95% CI) | 0.92 [0.67, 1.25] |
| 11.2 Generalised onset | 3 | 158 | Hazard Ratio (Fixed, 95% CI) | 1.56 [0.99, 2.44] |
| 12 Time to six‐month remission Show forest plot | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 0.98 [0.80, 1.21] |
| 13 Time to six‐month remission ‐ by seizure type Show forest plot | 4 | 683 | Hazard Ratio (Fixed, 95% CI) | 1.01 [0.81, 1.24] |
| 13.1 Focal onset | 4 | 525 | Hazard Ratio (Fixed, 95% CI) | 0.86 [0.67, 1.11] |
| 13.2 Generalised onset | 3 | 158 | Hazard Ratio (Fixed, 95% CI) | 1.45 [0.99, 2.12] |

