Antibióticos para el aborto incompleto
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised into two groups using sealed envelopes containing the treatment modality. | |
| Participants | 140 women admitted with a diagnosis of incomplete abortion to a tertiary care hospital inHarare, Zimbabwe. Included women with clinical evidence of an incomplete abortion; oral temperature not higher than 37°C; absence of a foul‐smelling vaginal discharge; absence of abdominal tenderness, and a negative cervical excitation test | |
| Interventions | Experimental: Tetracycline 500 mg four times daily for one week and evacuation | |
| Outcomes | Postabortal sepsis based on the presence of at least 3 out of 5 parameters: 1) history of chills, fever, headache,or lower abdominal pain; 2) oral temperature of greater than 37°C; 3) abdominal tenderness; 4) positive cervical excitation test; 5) presence of a foul smelling vaginal discharge. | |
| Notes | Post‐experimental exclusions: None reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| The study was excluded since it was on women undergoing induced abortion | |
| Descriptive study ‐ not RCT | |
| The study was on women with septic abortion. | |
| Randomised double‐blind placebo‐controlled trial, but for women with bacterial vaginosis for induced abortion | |
| The study was excluded since it was on women undergoing induced abortion. | |
| Cluster RCT for induced abortion , not for incomplete abortion | |
| Descriptive study on magnitude of abortion complications in Kenya | |
| The study was excluded since it was on women with a history of pelvic inflammatory disease undergoing first‐trimester abortion. | |
| Excluded since the study was on women admitted for legal termination of pregnancy at 12 weeks or less of gestation. | |
| The study was excluded since it was on patients undergoing first trimester abortions. | |
| The study was excluded since it was on women who were seeking induced abortions. | |
| RCT but for surgical abortion, not for incomplete abortion | |
| Randomised trial, but on women with bacterial vaginosis | |
| Study excluded because it was on women undergoing induced abortion | |
| This study had a high allocation concealment quality score (A); the generation of allocation sequence was reported and adequate; power calculation was done; and blinding of outcome assessment was presumably but not specifically done. There was no blinding of providers nor patients. However, the randomization schedule for each patient was not known by the examining physician at the time of the 2‐week follow‐up pelvic examination. Post‐experimental exclusions and protocol deviation was not reported. However, there was a loss to follow‐up of 30.5% which was 0.5% higher than the 30% which the reviewers had specified for the exclusion criteria, which was the reason for exclusion of the study. The study was conducted on 345 consenting women with an estimated gestational age of 6 ‐ 14 weeks with an incomplete abortion at a tertiary care hospital in Texas, U.S.A. Exclusion criteria were: haemodynamically unstable; allergic to doxycline; had evidence of a septic abortion or urinary tract or pelvic infection. Interventions were Doxycycline 100 mg intravenously and suction curettage for the experimental group and normal saline and suction curettage for the control group. Follow up was after 2‐3 weeks. Outcome assessed was infectious morbidity which was diagnosed if any two or more of the following symptoms were found: 1) low abdominal pain; 2) uterine, adnexal or cervical motion tenderness; 3) purulent leukorrhoea; 4) leukocytosis of more than 15,000/cu. mm.; or 5) fever above 100.4°F. The authors concluded that in their population of patients with incomplete abortion, prophylactic doxycycline did not decrease the rate of postoperative febrlle morbidity. This study was methodologically sound and the trial was done according to the protocol. If it had not been for the loss to follow‐up which exceeded the reviewers' criteria by 0.5%, it would have been included. | |
| Cost‐effective analysis ‐ not RCT | |
| The study was excluded since it was on women having induced first‐trimester abortions. | |
| The study was excluded since it was on women undergoing second trimester intraamniotic injection abortions. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 postabortion infection Show forest plot | 1 | 135 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.61 [0.79, 3.26] |
| Analysis 1.1  Comparison 1 Any antibiotic vs nothing, Outcome 1 postabortion infection. | ||||
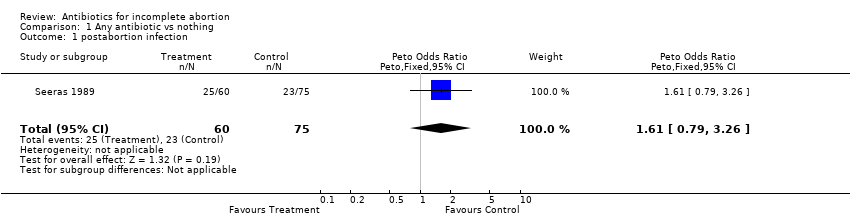
Comparison 1 Any antibiotic vs nothing, Outcome 1 postabortion infection.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 postabortion infection Show forest plot | 1 | 135 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.61 [0.79, 3.26] |

