Preparación mecánica del intestino para la cirugía colorrectal electiva
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomisation was performed centrally via an interactive voice randomisation system. Single‐blinded: the surgeon was blinded to the randomisation process and the preparation status of all patients. Withdrawal/dropout:7 patients were excluded (5 missing consent form, 1 refusal of surgical treatment, 1 loss of follow‐up). Follow‐up: 30 days postoperative. | |
| Participants | Inclusion criteria: all the patients aged 18 years or old with rectal cancer who underwent laparoscopic or open elective rectal resection with mesorectal excision and sphincter preservation. Exclusion criteria: very low tumours (abdominal perineal excision): metastasis in the liver or lungs; T4 rectal cancer; synchronous adenocarcinoma; and/or gastrointestinal disease, refusing extensive colonic surgery. Diseases: rectal cancer. Number of participants: 178 (102 male; 76 female). Age: 54 ‐ 71 years. Location of study: 8 french hospitals (Paris (2 hospitals), Bordeaux, Montpellier, Marseilles, Toulouse, Boulogne Billancourt, Clermont‐Ferrand). Antibiotics: 500 mg of metronidazole + 1 g of ceftriaxone at anaesthetic induction and were continued every 2 hours during the surgical procedure. | |
| Interventions | Group A ‐ MBP (n = 89): oral laxatives and retrograde enemas ‐ senna solution. After the preparation diet was confined to clear fluids. Group B ‐ no MBP (n = 89): no preoperative dietary restrictions. | |
| Outcomes | Anastomotic leakage: Group A = 8, Group B ‐ 17 ‐ Asymptomatic anastomotic leakage: Group A = 2, Group B = 3; ‐ Clinical anastomotic leakage: Group A = 6, Group B = 14. Wound abscess: Group A = 3, Group B = 1. Pelvic abscess: Group A = 1, Group B = 7. Peritonitis: Group A = 2, Group B = 6. Reoperation: Group A = 12, Group B = 5. Infectious abdominal complications: Group A = 15, Group B = 34. Infectious extra abdominal complications: Group A = 1, Group B = 1. Non infectious abdominal complications: Group A = 7, Group B = 14. Non infectious extra abdominal complications: Group A = 5, Group B = 1. Necessity to rectal stump washout intra operatively for pool preparation: Group A = 43, Group B = 47. Intraoperative faecal spillage: Group A = 2, Group B = 7. | |
| Notes | A multicenter study: 8 participating national (France) hospitals. Included patients with preoperative radiotherapy and chemiotherapy. Intention‐to‐treat analysis was performed. The sample size was calculated (n = 90 participants, in each group). Temporaly ileostomy: Group A = 71, Group B = 74. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Stated that randomised, but no details provided about randomisation method. | |
| Participants | Inclusion criteria: participants undergoing elective colorectal surgery. Exclusion criteria: no details. Diseases: colorectal cancer: 164/179; other: 14/179. Age: no details. Location of study: Liverpool, UK. | |
| Interventions | Group A ‐ MPB (n = 86); Antibiotics: perioperative intravenous (no more details). | |
| Outcomes | Wound infection: Group A = 5, Group B = 7. | |
| Notes | Conference proceeding only ‐ never published as article, so results obtained from abstract. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Randomisation: computer‐generated. | |
| Participants | Inclusion criteria: elective left‐sided colorectal surgery; participants aged 18 years or more; no MBP or antibiotics the week before inclusion. | |
| Interventions | Group A ‐ MBP (n = 78): 3 litres PEG 12‐16 h before surgery. | |
| Outcomes | Anastomotic leakage: Group A = 5, Group B = 1. | |
| Notes | Published data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Stated that randomised, but no details provided about randomisation method. On a day 7 before surgery, the colorectal anastomosis was checked, in the first half of the series. | |
| Participants | Inclusion criteria: participants admitted for elective colorectal surgery with primary anastomosis. | |
| Interventions | Group A ‐ MBP group (n = 82): sodium picosulphate 10 mg, the day before surgery (dose in morning and afternoon). | |
| Outcomes | Death: Group A =2; Group B = 0. | |
| Notes | Representative sample: consecutive participants. The outcome "Anastomotic leakage" was stratified, by the author: | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Randomisation: computer‐generated randomisation list; participants were allocated to each intervention by means of numbered sealed envelopes that corresponded to the randomisation list. Blinding: none. Withdrawal/dropouts: 77 participants excluded. Follow up: 24 days (17 ‐ 34 days). | |
| Participants | Inclusion criteria: indication for elective colorectal surgery with primary anastomosis. Exclusion criteria: acute laparotomy; laparoscopic colorectal surgery; contraindication for MBP; ileal stoma; younger than 18 years. Diseases: colorectal cancer, inflammatory bowel disease, radiation induced stenosis, endometriosis, correction of Hartmann's. Age: mean age 67 years. Location of study: 13 participating hospitals in the Netherlands. Date: April 1998‐February 2004. Antibiotics: according to the guideline of each hospital: cefuroxime + metronidazole, cefazolin + metronidazole, cefamandole + metronidazole, gentamycin + metronidazole, amoxicillin + clavulanate, and others. | |
| Interventions | Group A ‐ MBP (n = 670): PEG + bisacodyl (11 hospitals) or sodium phosphate solution (2 hospitals); fluid diet on the day before surgery. | |
| Outcomes | Anastomotic leakage: Group A = 32, Group B = 37. Outcomes measured in days (postoperatives): No postoperative complications: Group A = 462, Group B = 452. | |
| Notes | A multicenter study. In 2010 subgroup analysis is published by van't Sant the authors of this review made the calculus: Colonic surgery (n = 905): Group A = 434; Group B = 471. ‐ Anastomotic leakage: Group A = 14; Group B = 23. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Central trial office of randomisation, computer generated. | |
| Participants | Inclusion criteria: elective colon surgery. | |
| Interventions | Group A ‐ MBP (n = 125): 4 litres of PEG. | |
| Outcomes | Anastomotic leakage: Group A = 7, Group B = 6; Reoperation: Group A = 13, Group B = 11. | |
| Notes | Primary data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: no details. Follow up: 30 days after surgery. | |
| Participants | Inclusion criteria: participants admitted for elective colorectal surgery with primary anastomosis. Antibiotics: metronidazole + gentamicin 1 h before surgery, and then for 48 h. | |
| Interventions | Group A ‐ MBP (n = 30): 500 ml mannitol 20% + 500 ml orange juice. | |
| Outcomes | Wound infection: Group A = 1; Group B = 2. ‐Mechanical obstruction: Group A = 0; Group B = 1. ‐Dehiscence of wall suture: Group A = 0; Group B = 1. ‐Pulmonary embolism: Group A = 1; Group B = 0. Extra‐abdominal complications (infections): ‐Pneumonia: Group A = 1; Group B = 1. ‐Urinary infection: Group A = 1; Group B = 2. | |
| Notes | The sample size was calculated, but no details given. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: Central randomisation; random numbers. | |
| Participants | Inclusion criteria: participants undergoing elective open surgery for cancer, adenoma or diverticular disease of the rectum, involving an anastomosis; aged between 18‐85 years with an ASA grade of I, II or III. | |
| Interventions | Group A ‐ MBP (n = 27): PEG or sodium phosphate. | |
| Outcomes | Anastomotic dehiscence: Group A = 3, Group B = 0. | |
| Notes | A multicenter study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: central randomisation; random numbers. | |
| Participants | Inclusion criteria: participants undergoing elective open surgery for cancer, adenoma or diverticular disease of the colon, involving an anastomosis; aged between 18‐85 years with an ASA grade of I, II or III. | |
| Interventions | Group A ‐ MBP (n = 686): PEG or sodium phosphate. | |
| Outcomes | Anastomotic dehiscence: Group A = 13, Group B = 17. Reoperation: Group A = 30, Group B = 35. | |
| Notes | A multicenter study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: sealed envelopes at the time of the assignment of the surgical date. Blinding: not described. Withdrawal/Dropout: not described. Duration of follow‐up: not related. | |
| Participants | Inclusion criteria: all the consecutives electives surgeries with colonic anastomosis (ileocolonic, colonic, colorectal), including colonic transit reestablishment. Exclusion criteria: patients with immediately postoperative death without relation an intraabdominal sepsis or anastomotic leakage; patients whom refused to be operated without mechanical bowel preparation; patients submitted to bowel preparation for colonoscopy within 4 days prior to surgery. Diseases: benign or malignant colorectal pathology. Number of participants: 129 (77 male; 52 female). Age: 15 ‐ 85 years. Location of study: Hospital General de Agudos and private clinic, Lanus, province of Buenos Aires. Time os study: 2005 (March) ‐ 2006 (September). Antibiotics: ciprofloxacin 500 mg + metronidazole 500 mg. | |
| Interventions | Group A ‐ MBP (n = 64): upon availability dibasic‐monobasic sodium phosphate or polyethylene glycol. Group B ‐ no MBP (n = 65). | |
| Outcomes | Anastomotic leakage: Group A = 3 (in 53 patients), Group B = 9 (in 59 patients) ‐ Leakage in anastomosis intraperitoneal: Group A = 2 (in 43 patients), Group B = 5 (in 42 patients); ‐ Leakage in anastomosis extraperitoneal: Group A = 1 (in 10 patients), Group B = 4 (in 17 patients). Reoperation: Group A = 3, Group B = 5 ‐ Reoperation for leakage: Group A = 3, Group B = 4. Mortality: Group A = 1, Group B = 2. Wound infection: Group A = 10, Group B = 10. Peritonits: Group A = 3, Group B = 4. Intraabdominal abscess: Group A = 1, Group B = 0. | |
| Notes | Sample size was not calculated. Excluded patients without anastomosis in the outcome "Anastomotic leakage". Patients without anastomosis: Group A = 6 abdominoperineal amputation, 5 Hartmann's procedure; Group B = 4 abdominoperineal amputation, 2 Hartmann's procedure. Anastomosis and dehiscence: ‐ Right: Group A (25) = 1, Group B (21) = 2; ‐ Left: Group A (18) = 1, Group B (21) = 2; ‐ Low: Group A (10) = 1, Group B (17) = 4. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: sealed envelopes; consecutive adult participants. | |
| Participants | Inclusion criteria: all consecutive adults admitted for elective colorectal surgery. Disease: colorectal cancer (134); benign tumours (24); inflammatory bowel disease (32); diverticular disease (58); other (19). Number: 267 (130 male; 137 female). Age: 16‐97 years. Location: Kuopio + Oulu, Finland. Date: 1994‐1996. Antibiotics: ceftriaxone 2 g + metronidazole 1 g at the induction of anaesthesia. | |
| Interventions | Group A ‐ MBP (n = 138): PEG electrolyte solution, and no solid food on the preoperative day. | |
| Outcomes | Wound infection: Group A = 5; Group B = 3. | |
| Notes | Low colonic anastomosis/leakage: Group A = 9/3; Group B = 14/2. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: sealed envelops. Blinding: not described. Withdrawal/Dropout: not described. Follow‐up: 30 days after surgery. | |
| Participants | Inclusion criteria: elective colorectal surgery with primary anastomosis. Exclusion criteria: colorectal cancer smaller than 2 cm not marked by colonoscopy, those who were found to have an abscess of the tumour, diverticulitis, patients who refused to be randomised. Diseases: benign and malign colorectal diseases. Number: 139 (50 male; 89 female). Age: 68 ‐ 70 years. Location: Barcelona, Spain Time: May 2005 ‐ Agost 2007. Antibiotics: ‐ Oral (single dose 24 hours before the surgery): neomycin + metronidazole; ‐ Parenteral (single dose at the induction of anaesthesia): ceftriaxone + metronidazole. | |
| Interventions | Group A ‐ MBP (n = 69): monobasic sodium phosphate + dibasic sodium phosphate or polyethylene glycol Group B ‐ no MBP (n = 70): 2 cleansing enemas ‐ the day before the surgery (at 21:00 PM), ‐ 2 hours before the surgery. | |
| Outcomes | Overall anastomotic leakage: Group A = 5; Group B = 4 ‐ colorectal anastomosis: Group A = 0 (in 31 patients); Group B = 3 (in 19 patients), ‐ colonic anastomosis: Group A = 5 (in 38 patients); Group B = 1 (in 51 patients). Mortality: Group A = 2; Group B = 0; Overall wound infection: Group A = 8; Group B = 4 ‐ colorectal surgery: Group A = 3 (in 31 patients); Group B = 0 (in 19 patients), ‐ colonic surgery: Group A = 5 (in 38 patients); Group B = 4 (in 51 patients). | |
| Notes | Sample size was calculated. Colonic anastomosis: Group A = 38; Group B = 51; Colorectal anastomosis: Group A = 31; Group B = 19. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: computer‐generated numbers. | |
| Participants | Inclusion criteria: all participants scheduled to undergo an elective colon or proximal rectal resection with primary anastomosis by the same surgeon; without intraoperative colonoscopy; had not had endoscopic exploration in the prior week; were 18 years of age or older; had given informed consent. | |
| Interventions | Group A ‐ MBP (n = 48): 3 litres of oral PEG lavage solution plus conventional enemas over 24 h. | |
| Outcomes | Anastomotic failure: Group A = 4, Group B = 2. | |
| Notes | Sample size was calculated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: random numbers. Blinding: single‐blind (the treating surgeon was blinded). Withdrawal/Dropout: 41 exclusion after randomisation ‐ Group A: 23 resections of the colon and/or rectum without anastomosis; ‐ Group B: 16 resections, without anastomosis + 2 no resections performed. Follow‐up: 6 weeks after surgery. | |
| Participants | Inclusion criteria: all patients over the age of 18 years undergoing elective resection of the colon and/or rectum with anastomosis and with or without defunctioning stoma. Exclusion criteria: patients had undergone mechanical bowel preparation within 2 days of operation date, and patients submitted to laparoscopic procedure. Diseases: colorectal adenoma and cancer, inflammatory bowel disease, diverticular disease, rectal pathology. Number: 294 (M:F = Group A: 1: 8, Group B: 1:9). Age: 21 ‐ 93 years. Location of study: Perth, Western Australia ‐ Australia. Date: January 2000 ‐ February 2005. Antibiotics: ticarcillin disodium and clavulanate potassium (3‐1 g) with induction of anaesthesia or gentamicin (2 mg/kg) + metronidazole (500 mg). | |
| Interventions | Group A ‐ MBP (n = 147): polyethylene glycol Group B no MBP (n = 147): single sodium phosphate enema 2 ‐ 4 hours before surgery. | |
| Outcomes | Anastomotic leaks: Group A = 3; Group B = 7. Reoperation: Group A = 0; Group B = 6; Mortality: Group A = 0; Group B = 1. Wound infection: Group A = 19; Group B = 21. Intra‐abdominal abscess: Group A = 1; Group B = 1. | |
| Notes | The sample size was calculated. There was a significant difference in severity of the leaks: "the presence of a high volume faecal residue is likely to increase the chance of clinically significant anastomotic leak that will require reoperation". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: participants with even numbers received MBP (Group 1); participants with odd numbers did not receive MBP (Group 2). | |
| Participants | Inclusion criteria: adult participants admitted for elective colorectal surgery. | |
| Interventions | Group A ‐ MBP (n = 164): 2.4 g monobasic sodium phosphate + 0.9 g dibasic sodium phosphate + low‐residue diet 1 day before surgery. | |
| Outcomes | Mortality: Group A = 2, Group B = 2. | |
| Notes | There were more men than women in both groups, but no statistical difference was found between the two groups (sex, age and diagnosis). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Methods | Randomisation: participants were allocated by a randomised cards. Blinding: not described. | |
| Participants | Inclusion criteria: participants admitted for elective colorectal surgery. | |
| Interventions | Group A ‐ MBP (n = 72): laxative or enema: | |
| Outcomes | Wound infection: Group A = 17; Group B = 9. Anastomotic dehiscence: Group A = 7; Group B = 4. Reoperation: Group A = 4; Group B = 1. | |
| Notes | Representative sample not described. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: patients were prospectively randomised by individual computer‐generated randomisation into two groups. Blinding: not described. Withdrawal/dropout: 62 patients were excluded after randomisation due to the exclusion criteria. Duration of follow‐up: 30 days postoperative. | |
| Participants | Inclusion criteria: patients undergoing elective colon and rectal surgery with primary anastomosis. Exclusion criteria: abdominal perineal resection, transanal resection for T1, total mesorectal excision with sphincter saving procedure after neo‐adjuvant therapy for middle or low rectal cancer, R2‐ resection, randomisation in other studies, urgency or emergency procedures, patients who required a diverting stoma proximal to the anastomosis and those who were found to have an abdominal abscess at the time of surgery. Diseases: colorectal cancer. Number of participants: 244 (125 male; 110 female). Age: 60 ‐ 80 years. Location of study: Oncologic Unit Surgery, San Martino Hospital, Genoa, Italy. Time of study: 2005 (July) ‐ 2009 (September). Antibiotics: cephalosporin 2 g + metronidazole 500 mg. | |
| Interventions | Group A ‐ MBP (n = 120): 12 to 16 hours before surgery with polyethylene glycol. Group B ‐ no MBP (n = 124). Patients undergoing rectal surgery were given one enema one day before surgery. | |
| Outcomes | Anastomotic leakage: Group A = 7, Group B = 5. ‐ Colon: Group A = 2, Group B = 2. ‐ Rectum: Group A = 5, Group B = 3. Wound infection: Group A = 11, Group B = 6. Abdominal abscess: Group A = 6, Group B = 3. Total of infectious complications: Group A = 24, Group B = 14. | |
| Notes | Surgery localization: ‐ Colon: Group A = 87, Group B = 95. ‐ Rectum (upper): Group A = 33, Group B = 29. Surgical procedure: ‐ Right colectomy: Group A = 40, Group B = 50. ‐ Transverse colectomy: Group A = 9, Group B = 4. ‐ Left colectomy: Group A = 13, Group B = 26. ‐ Sigmoidectomy: Group A = 25, Group B = 15. ‐ Anterior resection: Group A = 33, Group B = 29. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation, blinding, withdrawal and dropouts: no details. Follow up: until hospital discharge (not specified). | |
| Participants | Inclusion criteria: participants with colorectal cancer, submitted for elective colorectal surgery. Exclusion criteria: no details. Diseases: colorectal cancer. Number: 47 (21 male, 26 female). Age: 22‐87 years. Location of study: Lima, Peru. Date: October 1999‐January 2001. Antibiotics: intravenously, against anaerobic and Gram‐negative bacteria, 30 minutes before surgery. | |
| Interventions | Group A ‐ MBP (n = 24): mannitol or PEG electrolyte solution + liquid diet 48 h before surgery. | |
| Outcomes | Wound infection: Group A = 2; Group B = 0. | |
| Notes | Length of hospital stay: Group A = 17‐19 days (mean 14); Group B = 6‐15 days (mean 11). Analysed only the complications related with the surgery. Participants without anastomosis (2 in Group A; 3 in Group B). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | It is a subgroup analysis of a prior large multicenter performed by Contant et al. Randomisation: computer‐generated randomisation list; participants were allocated to each intervention by means of numbered sealed envelopes that corresponded to the randomisation list. Blinding: none. Withdrawal/dropouts: not described. Follow‐up: first outpatients visit after discharge from the hospital which usually occurred after 2 weeks. | |
| Participants | Inclusion criteria: elective low anterior resection with primary anastomosis. Exclusion criteria: acute laparotomy, laparoscopic colorectal surgery, contraindications for the use of mechanical bowel preparation, an a priori diverting ileostomy, and age less than 18 years old. Diseases: colorectal cancer, inflammatory bowel disease, other. Participants: 449 (no details about gender). Age: not described. Location of study: Netherlands (13 hospitals). Date: April 1998 ‐ February 2004. Antibiotics: according to the guideline of each hospital: cefuroxime + metronidazole, cefazolin + metronidazole, cefamandole + metronidazole, gentamycin + metronidazole, amoxicillin + clavulanate, and others. | |
| Interventions | Group A ‐ Mechanical bowel preparation (n = 236): PEG + bisacodyl (11 hospitals) or sodium phosphate solution (2 hospitals); fluid diet on the day before surgery. | |
| Outcomes | Anastomotic dehiscence: Group A = 18; Group B = 14. Wound infection: Group A = 39; Group B = 36. Intraabdominal abscess: Group A = 6; Group B = 9. Mortality: Group A = 7; Group B = 9. Urinary tract infection: Group A = 34; Group B = 26. Pneumonia: Group A = 16; Group B = 20. Fascia dehiscence: Group A = 7; Group B = 2. Overall complications: Group A = 92 (39%); Group B = 83 (39%). | |
| Notes | Diverting ileostomy: n = 48 (no stoma = 401). Stoma: Group A = 27; Group B = 21. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomisation: Computer‐generated randomisation. | |
| Participants | Inclusion criteria: participants undergoing elective colon and rectal surgery with primary anastomosis. | |
| Interventions | Group A ‐ MBP (n = 187): 1 gallon PEG 12‐16 h before surgery. | |
| Outcomes | Wound infection: Group A = 12, Group B = 11. Overall non surgical complications: Group A = 53, Group B = 54. | |
| Notes | Extra data after stratification had been obtained with personal communication with the author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Abbreviations
ASA = American Society of Anaesthesiologists
h = hour(s)
MBP = mechanical bowel preparation
n = number of participants
PEG = polyethylene glycol
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| A case‐control study; unselected group of participants who underwent elective rectal surgery. Included laparoscopic surgeries. | |
| Series of consecutive participants. | |
| A survey with no control group. | |
| Published data in a conference proceeding. | |
| No control group. | |
| This trial not tested mechanical bowel preparation, but antimicrobials. | |
| A retrospective, non‐randomised study. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effect of Mechanical Bowel Preparation With Polyethylene Glycol Plus Bowel Enema (Glycerine 5%) vs Bowel Enema Alone in Patients Candidates to Colorectal Resection for Malignancy. Prospective, Randomized Clinical Trial |
| Methods | Inteventional and randomised |
| Participants | Patients candidates to colorectal surgery for histologically confirmed colorectal cancer; age 18‐80 years |
| Interventions | Other: mechanical bowel preparation |
| Outcomes | Anastomotic leakage, wound infection, post surgery extra abdominal complications, patient's symptoms (through questionnaire) |
| Starting date | October 2007 |
| Contact information | Emilio Bertani ([email protected])
|
| Notes | ClinicalTrials.gov Identifier: NCT00940030 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anastomosis leakage stratified for colonic or rectal surgery Show forest plot | 11 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 1 Anastomosis leakage stratified for colonic or rectal surgery. | ||||
| 1.1 Leakage after low anterior resection | 7 | 846 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.88 [0.55, 1.40] |
| 1.2 Leakage after colonic surgery | 8 | 3147 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.85 [0.58, 1.26] |
| 2 Overall anastomotic leakage for colorectal surgery Show forest plot | 13 | 4533 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.99 [0.74, 1.31] |
| Analysis 1.2  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 2 Overall anastomotic leakage for colorectal surgery. | ||||
| 3 Mortality Show forest plot | 11 | 4166 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.93 [0.58, 1.47] |
| Analysis 1.3  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 3 Mortality. | ||||
| 4 Peritonitis Show forest plot | 10 | 3983 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.74 [0.50, 1.08] |
| Analysis 1.4  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 4 Peritonitis. | ||||
| 5 Reoperation Show forest plot | 11 | 4319 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.04 [0.81, 1.34] |
| Analysis 1.5  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 5 Reoperation. | ||||
| 6 Wound infection Show forest plot | 13 | 4595 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.16 [0.95, 1.42] |
| Analysis 1.6  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 6 Wound infection. | ||||
| 7 Infectious extra‐abdominal complications Show forest plot | 6 | 3575 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.05 [0.85, 1.30] |
| Analysis 1.7  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 7 Infectious extra‐abdominal complications. | ||||
| 8 Non‐infectious extra‐abdominal complications Show forest plot | 6 | 2346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.98 [0.71, 1.36] |
| Analysis 1.8  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 8 Non‐infectious extra‐abdominal complications. | ||||
| 9 Sensitivity analysis 1 ‐ Including only studies with adequate randomisation Show forest plot | 9 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 9 Sensitivity analysis 1 ‐ Including only studies with adequate randomisation. | ||||
| 9.1 Overall anastomotic leakage for colorectal surgery | 9 | 3854 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.64, 1.23] |
| 9.2 Wound infection | 9 | 3875 | Odds Ratio (M‐H, Random, 95% CI) | 1.13 [0.91, 1.40] |
| 10 Sensitivity analysis 2 ‐ Studies including only patients with anastomosis Show forest plot | 8 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.10  Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 10 Sensitivity analysis 2 ‐ Studies including only patients with anastomosis. | ||||
| 10.1 Overall anastomotic leakage for colorectal surgery | 8 | 3792 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.60, 1.41] |
| 10.2 Wound infection | 8 | 3837 | Odds Ratio (M‐H, Random, 95% CI) | 1.07 [0.86, 1.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anastomotic leakage for colorectal surgery Show forest plot | 3 | 763 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.71, 2.87] |
| Analysis 2.1  Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 1 Anastomotic leakage for colorectal surgery. | ||||
| 1.1 Leakage after rectal surgery | 3 | 195 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.34, 2.52] |
| 1.2 Leakage after colonic surgery | 3 | 568 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.15 [0.79, 5.84] |
| 2 Overall anastomotic leakage Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.74, 2.36] |
| Analysis 2.2  Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 2 Overall anastomotic leakage. | ||||
| 3 Mortality Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.56, 3.90] |
| Analysis 2.3  Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 3 Mortality. | ||||
| 4 Peritonitis / Abscess Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.64, 2.93] |
| Analysis 2.4  Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 4 Peritonitis / Abscess. | ||||
| 5 Reoperation Show forest plot | 2 | 447 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.32, 2.33] |
| Analysis 2.5  Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 5 Reoperation. | ||||
| 6 Wound infection Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.85, 1.88] |
| Analysis 2.6  Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 6 Wound infection. | ||||
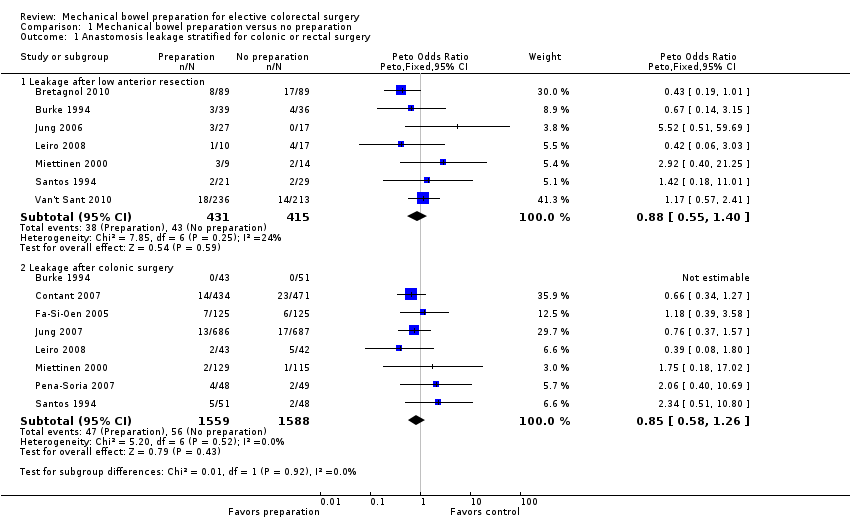
Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 1 Anastomosis leakage stratified for colonic or rectal surgery.

Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 2 Overall anastomotic leakage for colorectal surgery.

Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 3 Mortality.
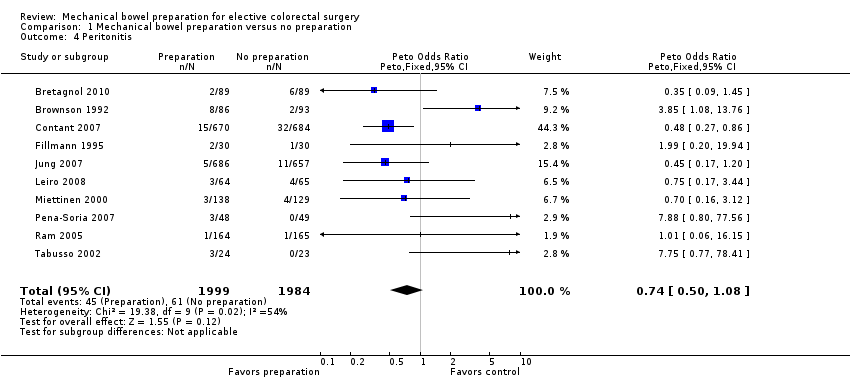
Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 4 Peritonitis.
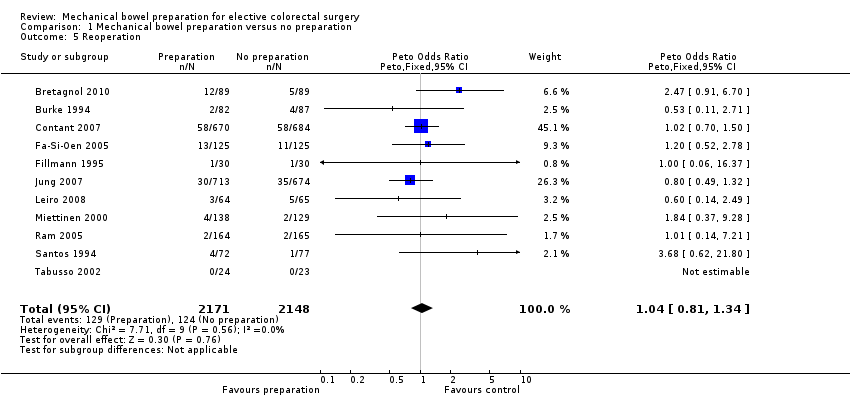
Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 5 Reoperation.
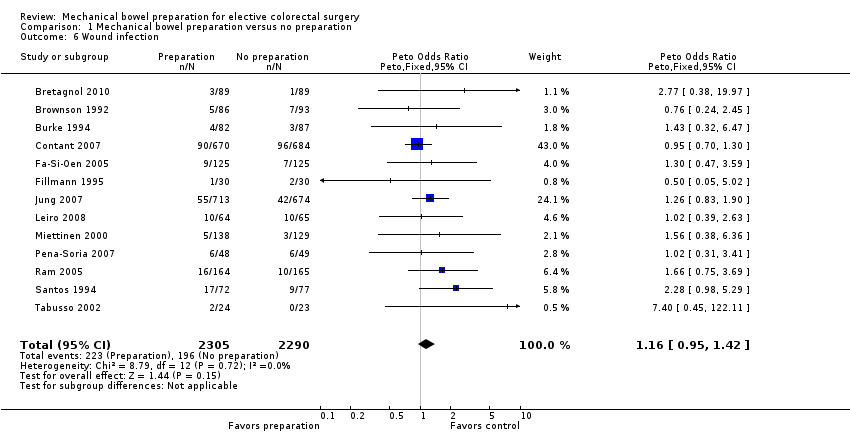
Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 6 Wound infection.

Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 7 Infectious extra‐abdominal complications.

Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 8 Non‐infectious extra‐abdominal complications.

Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 9 Sensitivity analysis 1 ‐ Including only studies with adequate randomisation.

Comparison 1 Mechanical bowel preparation versus no preparation, Outcome 10 Sensitivity analysis 2 ‐ Studies including only patients with anastomosis.
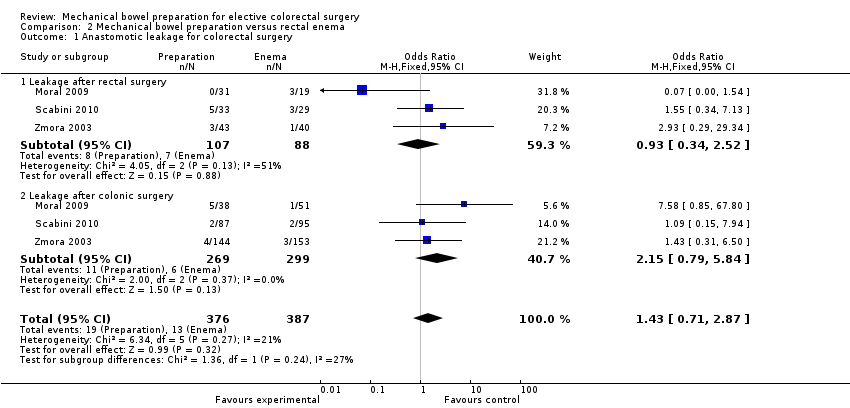
Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 1 Anastomotic leakage for colorectal surgery.
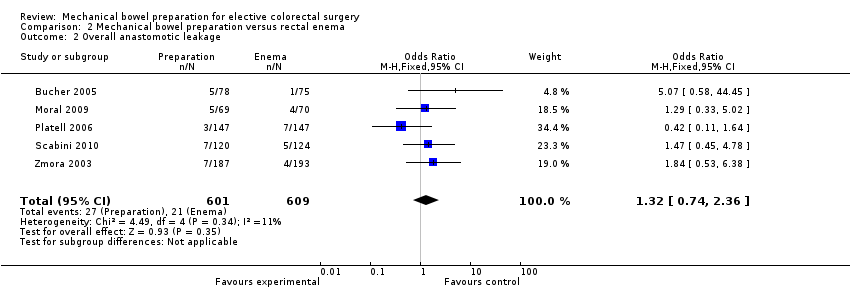
Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 2 Overall anastomotic leakage.
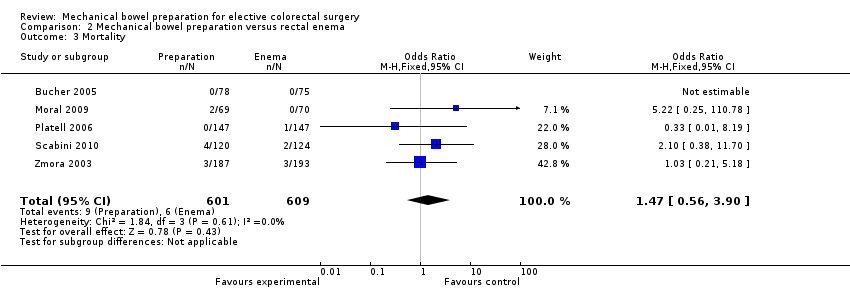
Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 3 Mortality.
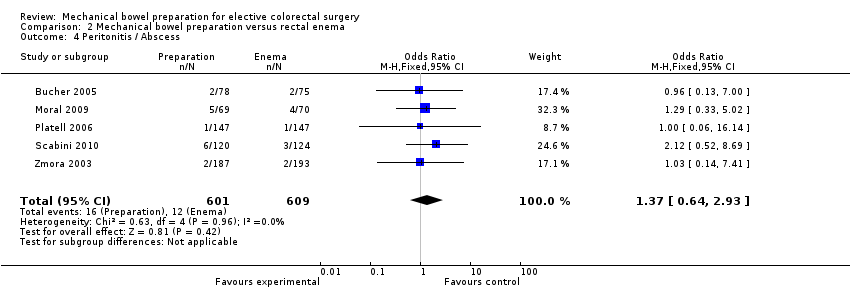
Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 4 Peritonitis / Abscess.
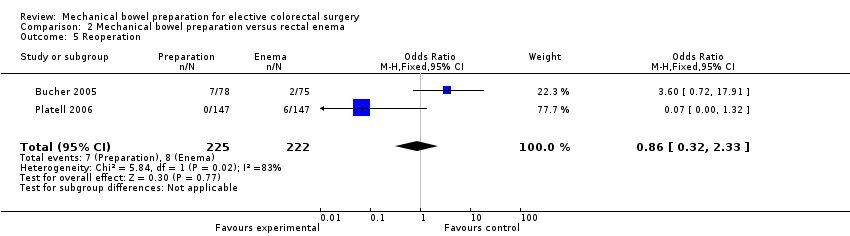
Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 5 Reoperation.

Comparison 2 Mechanical bowel preparation versus rectal enema, Outcome 6 Wound infection.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anastomosis leakage stratified for colonic or rectal surgery Show forest plot | 11 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.1 Leakage after low anterior resection | 7 | 846 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.88 [0.55, 1.40] |
| 1.2 Leakage after colonic surgery | 8 | 3147 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.85 [0.58, 1.26] |
| 2 Overall anastomotic leakage for colorectal surgery Show forest plot | 13 | 4533 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.99 [0.74, 1.31] |
| 3 Mortality Show forest plot | 11 | 4166 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.93 [0.58, 1.47] |
| 4 Peritonitis Show forest plot | 10 | 3983 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.74 [0.50, 1.08] |
| 5 Reoperation Show forest plot | 11 | 4319 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.04 [0.81, 1.34] |
| 6 Wound infection Show forest plot | 13 | 4595 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.16 [0.95, 1.42] |
| 7 Infectious extra‐abdominal complications Show forest plot | 6 | 3575 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.05 [0.85, 1.30] |
| 8 Non‐infectious extra‐abdominal complications Show forest plot | 6 | 2346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.98 [0.71, 1.36] |
| 9 Sensitivity analysis 1 ‐ Including only studies with adequate randomisation Show forest plot | 9 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Overall anastomotic leakage for colorectal surgery | 9 | 3854 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.64, 1.23] |
| 9.2 Wound infection | 9 | 3875 | Odds Ratio (M‐H, Random, 95% CI) | 1.13 [0.91, 1.40] |
| 10 Sensitivity analysis 2 ‐ Studies including only patients with anastomosis Show forest plot | 8 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1 Overall anastomotic leakage for colorectal surgery | 8 | 3792 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.60, 1.41] |
| 10.2 Wound infection | 8 | 3837 | Odds Ratio (M‐H, Random, 95% CI) | 1.07 [0.86, 1.35] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anastomotic leakage for colorectal surgery Show forest plot | 3 | 763 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.71, 2.87] |
| 1.1 Leakage after rectal surgery | 3 | 195 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.34, 2.52] |
| 1.2 Leakage after colonic surgery | 3 | 568 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.15 [0.79, 5.84] |
| 2 Overall anastomotic leakage Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.74, 2.36] |
| 3 Mortality Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.56, 3.90] |
| 4 Peritonitis / Abscess Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.64, 2.93] |
| 5 Reoperation Show forest plot | 2 | 447 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.32, 2.33] |
| 6 Wound infection Show forest plot | 5 | 1210 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.85, 1.88] |

