Pendidikan pesakit untuk mencegah ulser kaki kencing manis
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | 70 patients with type 2 diabetes mellitus ‐ randomised (intervention 38 vs control 32) | |
| Interventions | Intervention group: Control group: Adherence: not described | |
| Outcomes | Primary outcomes: not reported | |
| Duration and completion of follow‐up | 6 months; 62 people completed follow‐up (intervention 33 vs control 29) | |
| Types of assessment | Outcomes measured by multiple choice questions on knowledge and compliance. Number of questions and range of outcomes not reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) | Low risk | Foot care knowledge and foot care routine compliance were assessed with a questionnaire using multiple choice answers. Foot problems were scored by an independent podiatrist, who was not aware of the patients' experimental conditions |
| Incomplete outcome data (attrition bias) | High risk | 62 of 70 people completed 6 months' follow‐up (intervention 33 vs control 29). Reasons for missing outcome data are described and are unlikely to be related to the outcome No ITT analyses were undertaken |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | High risk | Baseline risk for foot ulceration: PVD, intervention 19 vs control 6 (P < 0.05) Co‐interventions were not described Adherence to the intervention was not described |
| Methods | RCT | |
| Participants | 749 insulin‐treated people with diabetes mellitus randomised: 345 consented to participate: Baseline risk for foot ulceration: Study setting: primary care, diabetes clinic in the USA | |
| Interventions | I: 9 group patient education sessions by nurse educator and nutritionist using film and card games and individual instruction. Content: 1 group session of education on foot care and skin hygiene, the other sessions on understanding diabetes, basic nutrition, weight loss, food purchasing, meal planning, insulin administration, emergencies, risk factors for macrovascular disease and individual diet instruction C: usual care. Content: not specified Adherence: 82 (50%) intervention group people completed 7 or more educational group sessions | |
| Outcomes | Primary outcomes: ulcer or amputations | |
| Duration and completion of follow‐up | Intervention 1.6 ± 0.3 years vs control 1.5 ± 0.3 years; 266 people completed follow‐up: intervention 127 vs control 139 | |
| Types of assessment | Behaviour assessment score: 7 questions of which 1 on foot care | |
| Notes | The reported outcome data on knowledge scores are not included in this review, because the assessment tool only included questions about diabetes in general, but not on foot care | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | 266 of 345 people completed follow‐up (intervention 127 vs control 139). Reasons for missing outcome data are described and are unlikely to be related to the outcome. Note: 749 people were originally randomised, but 193 did not attend the clinic during the period of the study and 211 of those who did attend to the clinic declined to participate, leaving only 345 study subjects No ITT analyses were undertaken |
| Selective reporting (reporting bias) | Unclear risk | Unclear. No study protocol available. The outcomes ulcer and amputation incidence, callus, nail dystrophy, fungal infection and behaviour assessment score were not prespecified in the methods section of the study report, but this is more likely to be a result of insufficient rather than selective reporting |
| Other bias | High risk | Baseline risk for foot ulceration: Co‐interventions were not described Adherence: 82 (50%) intervention group people completed 7 or more educational group sessions |
| Methods | RCT | |
| Participants | 167 people with type 2 diabetes randomised: intervention 55, only RA 55, control 57 Baseline risk for foot ulceration: no data provided Inclusion criteria: people with type 2 diabetes, age 40 years or older, residing within the country, presenting at the emergency department with non‐emergent health problems, not having active foot ulceration or other foot pathology, able to communicate verbally, agreeing on a home visit | |
| Interventions | Intervention group: Risk assessment group: lower extremity amputation risk assessment. Content: use of a monofilament Control group: No intervention Adherence: no data provided, but likely that all intervention group people received the single brief educational session directly after randomisation | |
| Outcomes | Primary outcomes: not reported | |
| Duration and completion of follow‐up | 1 month; 141 people completed follow‐up: intervention 47, RA 48, control 46 | |
| Types of assessment | Foot care knowledge scores: 5‐item foot care subscale from the Diabetes Knowledge Questionnaire 24 | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) | Low risk | The research assistant, who was the outcome assessor, was masked to group assignment |
| Incomplete outcome data (attrition bias) | High risk | 141 of 167 people completed 1‐month follow‐up (intervention 47, RA 48, control 46). Dropout was balanced in numbers across intervention groups, but reasons for missing data were not reported No ITT analyses were undertaken |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline risk for foot ulceration: no data provided There were no co‐interventions Adherence: no data provided, but likely that all intervention group people received the single brief educational session directly after randomisation |
| Methods | RCT | |
| Participants | 53 people with type 1 and 2 diabetes randomised: intervention 30 vs control 23 Baseline risk for foot ulceration: Baseline outcome measures: no data provided. Study setting: a unit of the National Health System (SUS) in Porto Alegre, Rio Grande do Sul, Brazil Study setting: community‐based care. Participants were selected from the National Health System (SUS) database Inclusion criteria: diabetes type 1 or 2, presence of neuropathy caused exclusively by diabetes mellitus as evidenced by inability to feel a Semmes‐Weinstein 5.07 monofilament in 2 of 3 of the following sites: digital pulp of the hallux, the head of the first metatarsal and the head of the fifth metatarsal | |
| Interventions | Intervention group:
Control group:
Adherence: of the 30 intervention group participants, 1 withdrew before completion of the education programme and 29 completed the education programme and received protective shoes. Of the 29 participants, 34.5% wore them daily up to 6 hours, 37.9% wore them daily for more than 6 hours and 27.6% did not wear the shoes daily | |
| Outcomes | Primary outcomes: foot ulceration, foot ulcer recurrence | |
| Duration and completion of follow‐up | 2 years. 35 participants completed follow‐up: intervention 21 vs control 14 | |
| Types of assessment | Inspection of the feet for the occurrence of neuropathic injury during individual consultations with the researcher, held quarterly in the first 18 months and after 2 years' follow‐up | |
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods are not described |
| Allocation concealment (selection bias) | Unclear risk | Methods are not described |
| Blinding (performance bias and detection bias) | High risk | Both participants and the outcome assessor were not blinded due to the nature of the intervention |
| Incomplete outcome data (attrition bias) | High risk | The proportion of people lost to follow‐up, although balanced between groups, could have induced clinically relevant bias. In I 9 out of 30 participants were censored (30%) and in C 9 out of 23 (39%) |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline risk for foot ulceration: the intervention group consisted of more men (intervention 70% vs control 52%), was older (mean age intervention 64.4 years vs control 59.8 years) and appeared to be at higher risk for foot ulceration (risk categories 1 to 4, intervention 20%, 50%, 10%, 20% vs control 43%, 30%, 13%, 13%). Baseline imbalances were not statistically significant and were not adjusted for Co‐interventions: not described Adherence: of the 30 participants, 1 withdrew before completion of the education programme and 29 completed the education programme and received protective shoes |
| Methods | RCT | |
| Participants | 40 people with type 2 diabetes mellitus randomised: intervention 20 vs control 20 Baseline risk for foot ulceration: Baseline outcome measures: no significant differences between groups Inclusion criteria: physically and mentally able to participate, able to read and understand English, age 18 years or older, no lower‐extremity ulcer, no history of lower‐extremity amputation | |
| Interventions | Intervention group: Control group: No intervention Adherence: 19 of 20 intervention group people attended the single education session | |
| Outcomes | Primary outcomes: not reported | |
| Duration and completion of follow‐up | 6 weeks after the intervention (people were enrolled in the study already 6 weeks prior to the intervention to ensure proper baseline measurements); 35 people completed follow‐up intervention 19 vs control 16 | |
| Types of assessment | Foot care knowledge assessment: 7 questions with 4 choices; foot care practice assessment: 7 questions with 4 choices; patients' self confidence assessment: 7 aspects of foot care rated on a 6‐point scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly drawing labelled consent forms, the sequence having been generated by shuffling |
| Allocation concealment (selection bias) | Low risk | Consent form labels were covered by opaque stickers and randomly shuffled |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | 35 of 40 people completed follow‐up (intervention 19 vs control 16). Reasons for missing data were not reported |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline foot risk assessment: 'no significant differences between groups' |
| Methods | RCT | |
| Participants | 100 people with type 2 diabetes mellitus randomised: intervention 50 vs control 50 Baseline risk for foot ulceration: Baseline outcome measures: Foot care knowledge scores: intervention 18.65 (SD 2.65) vs control 17.50 (SD 3.14), P = 0.056 Patients' behaviour assessment:
Study setting: primary care (mostly indigent) people with type 2 diabetes visiting a podiatrist in 1 of 2 designated community health centres associated with the Indiana University School of Medicine in Indianapolis, Indiana Inclusion criteria: > 65 years of age, no previous foot or leg amputation, access to a working telephone, able to understand English | |
| Interventions | Intervention group: Control group: Adherence: no data provided, but likely that all intervention group people received the single brief educational session directly after randomisation | |
| Outcomes | Primary outcomes: not reported | |
| Duration and completion of follow‐up | 4 weeks; 96 people completed follow‐up intervention 48 vs control 48 | |
| Types of assessment | Foot care knowledge: 26 items, with a ''true'', ''false'' or ''don't know'' answer (range 0 to 26) | |
| Notes | It was originally intended to report changes in 'weekly trimming of toenails', but this was abandoned, as all people were seen by a podiatrist for trimming of their toenails | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Papers with either 'group A' or 'group B' were drawn from an envelope |
| Allocation concealment (selection bias) | High risk | The envelope was not sealed |
| Blinding (performance bias and detection bias) | High risk | Outcomes were assessed by the research nurse, who also performed the educational intervention |
| Incomplete outcome data (attrition bias) | High risk | 96 of 100 people completed 4 weeks' follow‐up (intervention 48 vs control 48) |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline risk for foot ulceration: Co‐interventions were not described Adherence: no data provided, but likely that all intervention group people received the single brief educational session directly after randomisation |
| Methods | RCT | |
| Participants | 50 people with diabetes mellitus randomised: intervention 23 vs control 27 Inclusion criteria: diabetes duration at least 5 years (unclear which type of diabetes), no frank pathology, entering weekly hospital diabetes programme | |
| Interventions | Intervention group: Control group: Adherence: no data provided | |
| Outcomes | Primary outcomes: none reported | |
| Duration and completion of follow‐up | 6 months; 30 people completed follow‐up: intervention 15 vs control 15 | |
| Types of assessment | Foot status assessment: 67 items | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | People were allocated to intervention or control on the basis of the week that they entered the diabetes program. The experimental intervention group was developed similarly from the control group on alternate weeks |
| Allocation concealment (selection bias) | High risk | Alternation is not an adequate method of allocation concealment |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | 30 of 50 people completed 6 months' follow‐up (intervention 15 vs control 15). Reasons for dropping out were death (n = 2), not wanting to make an appointment at the scheduled time and moving without leaving a forwarding address (numbers not reported) |
| Selective reporting (reporting bias) | Low risk | Yes. No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline risk for foot ulceration: no data provided |
| Methods | RCT | |
| Participants | 178 people with diabetes and a newly healed foot ulcer randomised. Intervention 87 vs control 85. Excluded after randomisation: 6 Baseline risk for foot ulceration: Baseline outcome measures: Study setting: secondary outpatient care: specialist foot clinic in Nottingham, UK Inclusion criteria: people with newly healed diabetic foot ulcers (ulcer free for 28 days or more), not living in institutions, no history of dementia, no serious medical problems, English speaking or having an English speaking carer, living < 50 miles from the clinic, not included in any other study | |
| Interventions | Intervention group: Control group: Hand‐outs. Content: information about the causes of foot ulcers, foot care and ways to reduce the likelihood of accidents Adherence: no data provided, but likely that all intervention group people received the 1 hour at home education session | |
| Outcomes | Primary outcomes: ulcer incidence (recurrence), amputation rate Secondary outcomes: patients' behaviour assessment scores | |
| Duration and completion of follow‐up | 6 and 12 months; 168 people completed 12 months' follow‐up for primary outcomes. 138 people completed 12 months' follow‐up for secondary outcomes | |
| Types of assessment | Occurrence of new ulcers and amputation rate: hospital and foot clinic records, supported by questionnaires sent to the patient. At 12 months also corroborated by writing to participants' general practitioners | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was randomly generated by a computer in advance of the study |
| Allocation concealment (selection bias) | Low risk | People were allocated after telephoning an independent randomisation centre which held the sequence list |
| Blinding (performance bias and detection bias) | Low risk | Scoring of ulcer incidence and amputation rate was based on hospital and foot clinic records, supported by questionnaires sent to the patient. In case of discrepancy, the records were rechecked by a blinded observer. The success of blinding was not assessed but it was believed to be complete Patients' behaviour assessment score was based on questionnaires that were posted to participants and scored by a researcher who was blinded to participants' group allocation |
| Incomplete outcome data (attrition bias) | Low risk | 168 of 178 people completed 12 months' follow‐up for primary outcomes. 138 of 178 people completed 12 months' follow‐up for secondary outcomes. Reasons for dropping out were death (n = 10), illness (n = 2), erroneous double‐recruitment (n = 1), withdrawal of consent (n = 1), not fitting the eligibility criteria (n = 1), not returning questionnaires (n = 22) and incompleteness of the questionnaire answers (n = 2) |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Low risk | Baseline risk for foot ulceration: |
| Methods | RCT | |
| Participants | 227 people with diabetes mellitus and foot infection, ulceration or prior amputation ‐ randomised. 203 people included: intervention 103 vs control 100. Baseline risk for foot ulceration: although described as 'not significant', prior vascular reconstruction higher in control and incidence of foot callus higher in intervention (P < 0.05). No significant differences in foot deformities, neuropathy, gangrene, prior amputation or ulcer and level of distal pulses Study setting: secondary outpatient care, podiatric or vascular surgery care in the USA Inclusion criteria: people with diabetes (unclear which type) with foot infection, ulceration or prior amputation referred for podiatry or vascular surgery | |
| Interventions | Intervention group: Control group: Routine patient education. Content: routine diabetic teaching on diet, weight, exercise and medication Adherence: no data provided | |
| Outcomes | Primary outcomes: ulcer incidence, incidence of infections, amputation rate | |
| Duration and completion of follow‐up | Intervention mean 12 months, median 13.2 months (range 1 to 26 months) vs control mean 8 months, median 9.2 months (range 1 to 26 months); 182 people completed follow‐up: intervention 90 vs control 92 | |
| Types of assessment | No information provided | |
| Notes | Unit of randomisation: individual people. Unit of analyses: separate limbs | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were randomised into two groups based upon the odd or even last digit of their Social Security number" |
| Allocation concealment (selection bias) | High risk | Sequence generation was based upon the last digit of the persons social security number |
| Blinding (performance bias and detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | 182 of 227 people completed follow‐up (intervention 90 vs control 92). Reasons for dropping out were not fitting the eligibility criteria (n = 24), death (n = 13) and unspecified (n = 8) No ITT analyses were undertaken |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report listed the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline risk for foot ulceration: although described as 'not significant', prior vascular reconstruction higher in control and incidence of foot callus higher in intervention (P < 0.05). No significant differences in foot deformities, neuropathy, gangrene, prior amputation or ulcer and level of distal pulses |
| Methods | RCT | |
| Participants | 532 people with diabetes mellitus randomised intervention 263 vs control 269 Baseline risk for foot ulceration: no data provided Inclusion criteria: either 2 fasting blood glucose levels > 130 mg/dL or 1 > 150 mg/dL or 2‐hour value > 250 mg/dL, able to perform 2 basic self‐care tasks, no psychiatric or terminal illness, under care of an internal medicine resident, informed consent | |
| Interventions | Intervention group: Control group: Usual care. Content: including routine education Adherence: 139 of 208 (67%) people needing instruction on foot care completed this | |
| Outcomes | Primary outcomes: none reported | |
| Duration and completion of follow‐up | Median interval between instruction and follow‐up measurement 11.8 to 14.3 months; 275 people completed follow‐up: intervention 135 vs control 140 | |
| Types of assessment | Level of foot care knowledge: nurse‐administered patient history following predefined learning objectives | |
| Notes | Knowledge objectives unclear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) | High risk | Assessments were not conducted by personnel who were blind to subjects' experimental condition |
| Incomplete outcome data (attrition bias) | High risk | 275 of 532 people completed follow‐up (intervention 135 vs control 140). Reasons for dropping out were death (n = 30), physical or psychological incapacitation (n = 43), transfer to a senior staff physician (n = 32), relocation (n = 13), work conflict (n = 24), personal reasons (n = 45), failure to keep appointments (n = 11) and lost contact (n = 58) |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | High risk | Baseline risk for foot ulceration: no data provided |
| Methods | RCT | |
| Participants | 471 people with diabetes mellitus randomised intervention 228 vs control 243 Baseline risk for foot ulceration: no data provided Inclusion criteria: identified as diabetic inpatient of participating hospitals (unclear which type of diabetes), age < 65 years (at begin of study), no terminal illness, physician approval | |
| Interventions | Intervention group: Control group: Usual care. Content: not specified Adherence: no data provided | |
| Outcomes | Primary outcomes: none | |
| Duration and completion of follow‐up | 6 months; 373 people completed follow‐up: intervention 180 vs control 193 | |
| Types of assessment | Foot appearance assessment: nurse scored a 16‐item checklist | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) | Low risk | The staff nurses, who were the outcome assessors, were not aware of subject assignment at the time of the follow‐up visit |
| Incomplete outcome data (attrition bias) | High risk | 373 of 471 people completed follow‐up (intervention 180 vs control 193). Reasons for dropping out were deaths, violations of the protocol (such as an excessive number of home visits) and unspecified |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | Unclear risk | Baseline risk for foot ulceration: no data provided |
| Methods | RCT | |
| Participants | 530 people with diabetes mellitus randomised, intervention 267 vs control 263Baseline risk for foot ulceration: no data provided Baseline outcome measures: Study setting: community‐based care in the vicinity of Turku, Finland Inclusion criteria: included in the national drug imbursement register for receiving antidiabetic treatment, no obvious need for podiatry, no visit with podiatrist in previous 6 months, age between 10 to 79 years | |
| Interventions | Intervention group: Control group: Written information. Content: instructions on foot care Adherence: intervention mean number of podiatry visits 4.7 in first year. After first and before seventh follow‐up year at least 1 podiatry visit in 82.3% of people in intervention and in 49.7% in control | |
| Outcomes | Primary outcomes: amputation rate, ulcer incidence | |
| Duration and completion of follow‐up | 1 and 7 years; 459 completed 1 year of follow‐up: intervention 233 vs control 226 | |
| Types of assessment | Callus diameter in millimetres. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was performed separately for men and women and for people below and above 20 years of age. Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) | Unclear risk | The outcome assessor was blinded to the baseline characteristics, but no further information on blinding to the group allocation is provided |
| Incomplete outcome data (attrition bias) | High risk | Follow‐up was completed by only 63% of people in the intervention group and 62% of people in the control group at 7 years |
| Selective reporting (reporting bias) | Low risk | No study protocol available, but the trial report lists the outcomes of interest in both the methods and the results section |
| Other bias | High risk | Baseline risk for foot ulceration: no data provided |
BMI = body mass index, CI = confidence interval, HbA1c = glycated haemoglobin, HR = hazard ratio, ITT = intention to treat, PVD = peripheral vascular disease, RA = risk assessment, RCT = randomised controlled trial, RR = risk ratio, SD = standard deviation, SDSCA = Summary of Diabetes Self‐Care Activities.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a randomised controlled study design | |
| Not a randomised controlled study design and no educational programme that includes patient education aimed at reducing diabetic foot ulcers | |
| No educational programme that included patient education aimed at reducing diabetic foot ulcers, and no relevant outcomes reported | |
| No educational programme targeted at people that includes patient education aimed at reducing diabetic foot ulcers | |
| Education initially directed at wound healing. Patient education for preventing ulcer recurrence only offered to participants with healed index lesions | |
| No relevant outcomes reported | |
| Foot care education is part of the comprehensive intervention on foot ulceration but not the main contrast with the control | |
| Not a randomised controlled study design | |
| Foot care education is not the main contrast with the control | |
| Foot care education is not the main contrast with the control | |
| Foot care education is not the main contrast with the control | |
| Not a randomised controlled study design | |
| No educational programme targeted at people that includes patient education aimed at reducing diabetic foot ulcers, and education not the main contrast with the control | |
| No educational programme that includes patient education aimed at reducing diabetic foot ulcers | |
| Foot care education is not the main contrast with the control | |
| No educational programme that includes patient education aimed at reducing diabetic foot ulcers, and no relevant outcomes reported | |
| Not a randomised controlled study design | |
| Not a randomised controlled study design | |
| Only conference abstract. No full‐text article available. |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | The main result is planned to be presented at the Diabetic Foot Meeting in Haag 20‐23 May 2015, and a manuscript is submitted. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Foot ulcer incidence (1‐year follow‐up) Show forest plot | 1 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.14, 0.66] |
| Analysis 1.1  Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 1 Foot ulcer incidence (1‐year follow‐up). | ||||
| 2 Amputation Rate (1‐year follow‐up) Show forest plot | 1 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.15, 0.76] |
| Analysis 1.2 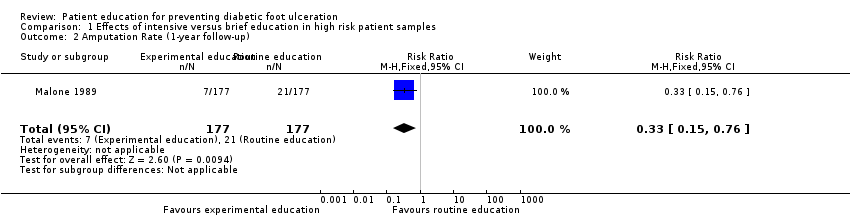 Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 2 Amputation Rate (1‐year follow‐up). | ||||
| 3 Foot ulcer incidence (1‐year follow‐up) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.44] |
| Analysis 1.3  Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 3 Foot ulcer incidence (1‐year follow‐up). | ||||
| 4 Amputation rate (1‐year follow‐up) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.41, 2.34] |
| Analysis 1.4  Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 4 Amputation rate (1‐year follow‐up). | ||||

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 1 Foot ulcer incidence (1‐year follow‐up).
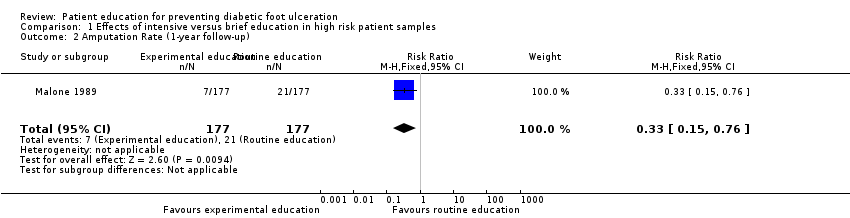
Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 2 Amputation Rate (1‐year follow‐up).
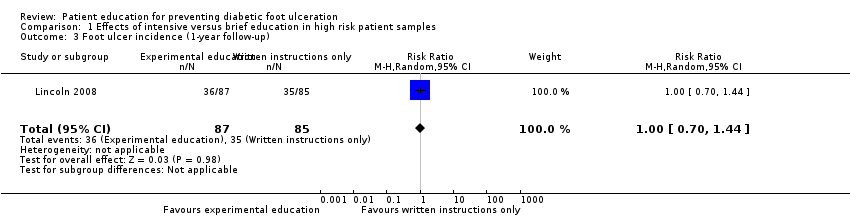
Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 3 Foot ulcer incidence (1‐year follow‐up).
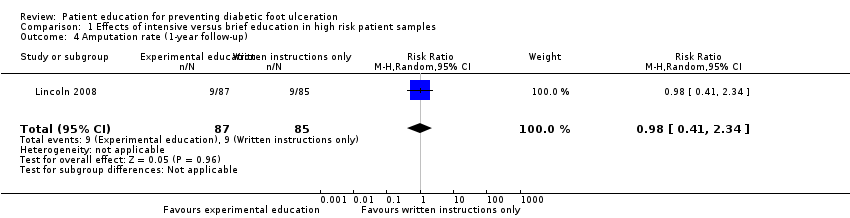
Comparison 1 Effects of intensive versus brief education in high risk patient samples, Outcome 4 Amputation rate (1‐year follow‐up).
| Study ID | Primary outcomes | Secondary outcomes |
| No primary outcomes reported | Foot problems requiring treatment: Foot care knowledge: Foot care routine compliance: | |
| Ulcer or amputation: people with callus, nail dystrophy or fungal infection at baseline: intervention 2/37 vs control 3/63 people with an ulcer or amputation at baseline: intervention 6/7 vs control 11/13 | Callus, nail dystrophy and fungal infection: Behaviour assessment scores: | |
| No primary outcomes reported | Patients' self‐reported behaviour assessment scores: Observed self‐care behaviour: Foot care knowledge scores: | |
| Ulcer incidence: people without a history of foot ulceration: intervention 8/21 vs control 8/14 (P = 0.317) Patient with a history of foot ulceration: intervention 1/8 vs control 5/8 (P = 0.119) All people: difference between the survival curves of intervention and control (P = 0.362) (HR not reported) | No secondary outcomes reported | |
| No primary outcomes reported | Foot care knowledge scores: Foot care practice scores: | |
| No primary outcomes reported | Foot care knowledge scores: Patients' behaviour assessment: | |
| No primary outcomes reported | Foot status: Foot care knowledge scores: Behaviour assessment: | |
| Ulcer incidence: Amputation rate: | Behaviour assessment scores: | |
| Ulcer incidence: Amputation rate: | No secondary outcomes reported | |
| No primary outcomes reported | Foot care knowledge scores: | |
| No primary outcomes reported | Foot appearance scores (mean ±standard error): Foot care knowledge scores: Foot care skills scores: | |
| Amputation: 7‐year follow‐up: intervention 1 vs control 0 Foot ulceration: 7‐year follow‐up: intervention 1 vs control 1 | Callus development: Calcaneal region:
Other regions:
7‐year follow‐up: Calcaneal region:
Other regions:
Foot care knowledge scores:
7‐year follow‐up:
Patients' behaviour assessment scores:
7‐year follow‐up:
| |
| Abbreviations: CI = confidence interval, ns = no statistical significance, RA = group that received risk assessment only, RR = risk ratio, SD = standard deviation. | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Foot ulcer incidence (1‐year follow‐up) Show forest plot | 1 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.14, 0.66] |
| 2 Amputation Rate (1‐year follow‐up) Show forest plot | 1 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.15, 0.76] |
| 3 Foot ulcer incidence (1‐year follow‐up) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.44] |
| 4 Amputation rate (1‐year follow‐up) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.41, 2.34] |

