Cirugía para la espondilosis lumbar degenerativa
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Random number table | |
| Participants | 31 participents; 16 m, 15 f; | |
| Interventions | Exp: Decompression | |
| Outcomes | 2nd procedure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomization by computer programme. | |
| Participants | 28 participants; 10 m, 18 f; | |
| Interventions | Exp: IDET | |
| Outcomes | Observer rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: not stated | |
| Participants | 44 participants; 10 m, 34 f; age 44 to 79 yrs; | |
| Interventions | Exp: | |
| Outcomes | Spondylolisthesis progression | |
| Notes | Non‐randomized allocation of patients with radiological instability | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Centralized randomization | |
| Participants | 60 participants; | |
| Interventions | Exp: Posterolateral instrumented fusion (pedicle systems) | |
| Outcomes | Patient rating | |
| Notes | Treatment post laminectomy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Block randomization from computer generated list | |
| Participants | 60 participants | |
| Interventions | Exp: Posterolateral instrumented fusion (pedicle systems) | |
| Outcomes | Independent observer rating | |
| Notes | Treatment post discectomy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomisation method: sealed envelopes containing random numbers. | |
| Participants | 42 participants; 26 m, 16 f; age 19 to 51 yrs; | |
| Interventions | Exp: | |
| Outcomes | Back pain rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization by consecutively numbered sealed envelopes | |
| Participants | 148 participants; 88 m, 58 f | |
| Interventions | Dubousset system | |
| Outcomes | Dallas pain questionnaire | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Central randomization ratio 2:1 | |
| Participants | 53 participants; 30 m, 25 f | |
| Interventions | Exp: ProDisc artificial lumbar disc replacement | |
| Outcomes | ODI | |
| Notes | Interim analysis from one center out of US multi‐center trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: closed envelope technique | |
| Participants | 76 participants; 17 m, 59 f; age 52 to 86 yrs; Degenerative spondylolisthesis and spinal stenosis | |
| Interventions | Exp: Instrumented posterolateral fusion (Steffee system) | |
| Outcomes | Back pain scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: not stated | |
| Participants | 83 participants; 58 m, 25 f; age 19 to 76 yrs; Heterogeneous conditions | |
| Interventions | Exp: Instrumented posterolateral fusion (Steffee system) | |
| Outcomes | Back pain scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomization method: 2:1 Exp:Ctl | |
| Participants | 57 participants | |
| Interventions | Exp: IDET | |
| Outcomes | LBOS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | Randomization blindly from computer generated list | |
| Participants | 294 participants; 50% m; | |
| Interventions | Exp: Surgical | |
| Outcomes | Patient rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: not stated | |
| Participants | 179 participants at follow‐up; 97 m, 82 f; age 21 to 76 yrs; | |
| Interventions | Exp: Electrical stimulation | |
| Outcomes | Surgeon rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomization method: quasi by date of admission to hospital | |
| Participants | 45 participants; 21 m, 24 f; age 48 to 87 yrs; Spinal stenosis | |
| Interventions | Exp: Decompression with arthrodesis (both mono + multi‐segmental) | |
| Outcomes | Patient rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Quasi‐randomized: alternately assigned to treatment | |
| Participants | 50 participants; 14 m, 36 f; age 52 to 84 yrs; Degenerative spondylolisthesis | |
| Interventions | Exp: Decompression + fusion | |
| Outcomes | Back pain scale Leg pain scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Computer generated randomization | |
| Participants | 61 participants; 32 m, 29 f; | |
| Interventions | Exp: Pulsed electromagnetic field therapy (external coil) | |
| Outcomes | Fusion failure | |
| Notes | Also measurements of fusion mass | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomization method: not stated | |
| Participants | 62 participants; Degenerative spondylolisthesis | |
| Interventions | Exp: Instrumented posterolateral (pedicle system) and posterior interbody fusin (autogenous graft) | |
| Outcomes | Fusion | |
| Notes | Abstract of data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomized from computer generated randomisation code provided by independent third party. | |
| Participants | 243 participants; mean age 57 yrs | |
| Interventions | Exp: Active stimulation 30 min/day for 2 months | |
| Outcomes | Fusion by CT and/or lateral Flex/Ext radiographs | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization from chits drawn from box | |
| Participants | 55 participants; 29 m, 26 f; age range 25 to 70 yrs | |
| Interventions | Exp: Ligamentoplasty (Graf system) | |
| Outcomes | VAS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Random number generator in ratio 2:1 | |
| Participants | 60 participants, 30 m, 30 f; | |
| Interventions | Exp: SB Charite artificial lumbar disc replacement | |
| Outcomes | ODI | |
| Notes | Pilot study only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: not stated | |
| Participants | 27 participants; 23 m, 4 f; age 24 to 42 yrs; | |
| Interventions | Exp: Postero‐lateral fusion (Steffee system) | |
| Outcomes | Fusion, | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomization method: blindly selected choice of three. Allocation concealment: A | |
| Participants | 111 participants; 57 m, 54 f ; 18 to 55 yrs; Isthmic spondylolisthesis of all grades | |
| Interventions | Exp.1: Instrumented posterolateral fusion (CD system) | |
| Outcomes | Disability rating index | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: not stated | |
| Participants | 195 participants | |
| Interventions | Exp: Electromagnetic brace ‐ 8 hrs/day | |
| Outcomes | Surgeons rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Computer generated random numbers | |
| Participants | 64 participants from a potential of 1360 | |
| Interventions | Exp: IDET to 90ºC | |
| Outcomes | VAS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomization method: Allocation by pathology and then assigned alternately | |
| Participants | 70 participants; 34 m, 36 f; age 43 to 79 yrs; | |
| Interventions | Exp: Multiple laminotomy | |
| Outcomes | Patient rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Randomization method not stated. | |
| Participants | 140 participants; 63 m, 76 f; | |
| Interventions | Exp: Threaded fusion device (Interfix system) | |
| Outcomes | Radiographic fusion | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomization by odd and even file numbers. | |
| Participants | 53 participants; 27 m, 21 f; | |
| Interventions | Exp: 360º fusion (TSRH system plus allograft ring, plus autogenous posterolateral graft) | |
| Outcomes | Pain | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | Randomization from consecutively numbered closed envelopes | |
| Participants | 130 participants; 60 m, 69 f; age 20 to 67 yrs; Chronic low back pain | |
| Interventions | Exp: Instrumented posterolateral fusion (CD system) | |
| Outcomes | Functional scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Random number generator | |
| Participants | 124participants; age 20 to 80 yrs; Heterogeneous conditions | |
| Interventions | Exp: | |
| Outcomes | Surgeons rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Randomized from central office | |
| Participants | 39 participants from 1 of 19 participating centers ‐ ratio 28 Exp. to 11Ctl; age 18 to 60 yrs; | |
| Interventions | Exp: ProDisc implant | |
| Outcomes | VAS | |
| Notes | Results from 1 of 19 centers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Block randomization by centre | |
| Participants | 200 pts; mean age 69 yrs | |
| Interventions | Exp. Interspinous spacer (X‐stop system) | |
| Outcomes | SF‐36 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Exp = Experimental
Ctl = Control
m = male
f = female
yrs = years
wks = weeks
ODI ‐ Oswestry Disability Index
PLIF = posterior lumbar interbody fusion
ALIF = anterior lumbar interbody fusion
CD system = Cotrel‐Dubousset instrumentation
ZCI = Zurich claudication questionnaire
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Study of human bone morphogenetic protein | |
| Study of rehabilitation following surgery | |
| No subsequent data produced following abstract in 1995 | |
| Comparison of two durations of intradiscal radiofrequency thermocoagulation | |
| Study of method of achieving better fusion (allograft versus autograft) | |
| Study of osteogenic protein‐1 | |
| Medical treatment for discogenic back pain (steroid vs. saline placebo injection). | |
| Randomly selected group of patients divided according to their surgery | |
| Study of technique ‐ computer assistance in placement of pedicle screws | |
| Study of varying surgical technique | |
| Initial report of 8 patients published in 1995. No complete data. | |
| Preliminary data comparing the effectiveness of an implanted electrode to diminish persistent radicular and back pain after lumbosacral spine surgery with reoperation | |
| No further data published after abstract in 1995 | |
| Study of technique | |
| Variation of surgical technique ‐ hydroxyapatite coating of pedicle screws | |
| Study of post spinal fusion rehabilitation programmes | |
| Study of bone morphogenetic proteins | |
| Study of two different screw types | |
| No subsequent data produced following abstract in 1996 | |
| Study of variation within a given procedure |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A Prospective randomised trial comparing femoral ring allograft versus a titanium cage for circumferential spinal fusion: two year functional and radiological outcome |
| Methods | |
| Participants | 62 participants |
| Interventions | Exp: Titanium interbody cage |
| Outcomes | ODI |
| Starting date | 2001 |
| Contact information | Centre for spinal surgery, Queens Medical Centre, Nottingham, UK |
| Notes |
| Trial name or title | |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
| Trial name or title | Spinal fusion in patients with single level degenerate disc disease and neural compression ‐ a prospective randomised study |
| Methods | |
| Participants | 40 participants; age 39 to 74 yrs |
| Interventions | Exp 1: Transforaminal interbody fusion plus instrumented posterolateral fusion |
| Outcomes | Roland & Morris |
| Starting date | 1999 |
| Contact information | |
| Notes |
| Trial name or title | |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
| Trial name or title | Operative treatment for moderately severe lumbar spinal stenosis: a randomized controlled trial |
| Methods | |
| Participants | 94 participants |
| Interventions | Exp: Segmental decompression and undercutting facetectomy |
| Outcomes | VAS |
| Starting date | 2001 |
| Contact information | Finnish Institute of Occupational Health, Helsinki |
| Notes |
| Trial name or title | |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Secondary surgery by 4 years Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 0.89] |
| Analysis 1.1  Comparison 1 DECOMPRESSION vs CONSERVATIVE, Outcome 1 Secondary surgery by 4 years. | ||||
| 2 Bad result at 10 years Show forest plot | 1 | 19 | Odds Ratio (M‐H, Random, 95% CI) | 2.43 [0.09, 67.57] |
| Analysis 1.2  Comparison 1 DECOMPRESSION vs CONSERVATIVE, Outcome 2 Bad result at 10 years. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No success: combined patient / surgeon rating Show forest plot | 1 | 67 | Odds Ratio (M‐H, Random, 95% CI) | 0.85 [0.25, 2.88] |
| Analysis 2.1  Comparison 2 MULTIPLE LAMINOTOMY vs LAMINECTOMY, Outcome 1 No success: combined patient / surgeon rating. | ||||
| 2 Spondylolisthesis progression Show forest plot | 1 | 67 | Odds Ratio (M‐H, Random, 95% CI) | 0.56 [0.16, 2.03] |
| Analysis 2.2  Comparison 2 MULTIPLE LAMINOTOMY vs LAMINECTOMY, Outcome 2 Spondylolisthesis progression. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result 18‐24 months ‐ Surgeon rating Show forest plot | 3 | 138 | Odds Ratio (M‐H, Random, 95% CI) | 0.44 [0.13, 1.48] |
| Analysis 3.1  Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 1 Poor result 18‐24 months ‐ Surgeon rating. | ||||
| 2 Re‐operation 2‐4 years Show forest plot | 2 | 64 | Odds Ratio (M‐H, Random, 95% CI) | 4.69 [0.51, 42.83] |
| Analysis 3.2  Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 2 Re‐operation 2‐4 years. | ||||
| 3 Spondylolisthesis progression Show forest plot | 2 | 93 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.00, 2.07] |
| Analysis 3.3  Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 3 Spondylolisthesis progression. | ||||
| 4 No improvement in walking distance Show forest plot | 1 | 39 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.06, 2.21] |
| Analysis 3.4  Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 4 No improvement in walking distance. | ||||
| 5 Good result at 18‐24 months Show forest plot | 2 | 93 | Odds Ratio (M‐H, Random, 95% CI) | 4.41 [1.09, 17.76] |
| Analysis 3.5  Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 5 Good result at 18‐24 months. | ||||
| 6 No spondylolisthesis progression Show forest plot | 2 | 93 | Odds Ratio (M‐H, Random, 95% CI) | 11.53 [0.48, 275.52] |
| Analysis 3.6  Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 6 No spondylolisthesis progression. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result as rated by patient ‐ at 2yrs Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 5.74 [0.25, 130.37] |
| Analysis 4.1  Comparison 4 LAMINECTOMY PLUS MULTI‐LEVEL FUSION vs LAMINECTOMY, Outcome 1 Poor result as rated by patient ‐ at 2yrs. | ||||
| 2 Poor result as rated by independent assessor ‐ at 2yrs Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 8.68 [0.41, 184.28] |
| Analysis 4.2  Comparison 4 LAMINECTOMY PLUS MULTI‐LEVEL FUSION vs LAMINECTOMY, Outcome 2 Poor result as rated by independent assessor ‐ at 2yrs. | ||||
| 3 Re‐operation by 28mths Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 3.21 [0.12, 85.20] |
| Analysis 4.3  Comparison 4 LAMINECTOMY PLUS MULTI‐LEVEL FUSION vs LAMINECTOMY, Outcome 3 Re‐operation by 28mths. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No fusion at 4.5yrs Show forest plot | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 15.21 [0.76, 303.32] |
| Analysis 5.1  Comparison 5 LAMINECTOMY vs NO LAMINECTOMY (Isthmic spondylolisthesis), Outcome 1 No fusion at 4.5yrs. | ||||
| 2 No success ‐ Patient rating at 4.5yrs Show forest plot | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 11.5 [1.24, 106.85] |
| Analysis 5.2  Comparison 5 LAMINECTOMY vs NO LAMINECTOMY (Isthmic spondylolisthesis), Outcome 2 No success ‐ Patient rating at 4.5yrs. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result as rated by surgeon ‐ at 36 mths (ave) Show forest plot | 1 | 50 | Odds Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 4.04] |
| Analysis 6.1  Comparison 6 LAMINECTOMY PLUS ONE LEVEL FUSION (No instrumentation, spinal stenosis + degen spondylolisthesis vs LAMINECT, Outcome 1 Poor result as rated by surgeon ‐ at 36 mths (ave). | ||||
| 2 Spondylolisthesis progression at 6 months Show forest plot | 1 | 19 | Odds Ratio (M‐H, Random, 95% CI) | 4.67 [0.67, 32.36] |
| Analysis 6.2  Comparison 6 LAMINECTOMY PLUS ONE LEVEL FUSION (No instrumentation, spinal stenosis + degen spondylolisthesis vs LAMINECT, Outcome 2 Spondylolisthesis progression at 6 months. | ||||
| 3 Re‐operation required within 4 years Show forest plot | 1 | 19 | Odds Ratio (M‐H, Random, 95% CI) | 3.00 [0.11, 83.36] |
| Analysis 6.3  Comparison 6 LAMINECTOMY PLUS ONE LEVEL FUSION (No instrumentation, spinal stenosis + degen spondylolisthesis vs LAMINECT, Outcome 3 Re‐operation required within 4 years. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fair or Poor outcome (independent observer rated) Show forest plot | 1 | 262 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.13, 0.52] |
| Analysis 7.1  Comparison 7 LUMBAR FUSION vs CONSERVATIVE (PHYSICAL) THERAPY, Outcome 1 Fair or Poor outcome (independent observer rated). | ||||
| 2 Not back to work at 2 years Show forest plot | 1 | 208 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.10, 0.64] |
| Analysis 7.2  Comparison 7 LUMBAR FUSION vs CONSERVATIVE (PHYSICAL) THERAPY, Outcome 2 Not back to work at 2 years. | ||||
| 3 Unchanged / worse at two years (patient rating) Show forest plot | 1 | 257 | Odds Ratio (M‐H, Random, 95% CI) | 0.28 [0.15, 0.53] |
| Analysis 7.3  Comparison 7 LUMBAR FUSION vs CONSERVATIVE (PHYSICAL) THERAPY, Outcome 3 Unchanged / worse at two years (patient rating). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure (patient rating) at 1 year Show forest plot | 1 | 61 | Odds Ratio (M‐H, Random, 95% CI) | 0.76 [0.25, 2.25] |
| Analysis 8.1  Comparison 8 LUMBAR FUSION vs COGNITIVE EXERCISES (Degenerate disc), Outcome 1 Failure (patient rating) at 1 year. | ||||
| 2 Failure (independent assessor) at 1 year Show forest plot | 2 | 63 | Odds Ratio (M‐H, Random, 95% CI) | 1.53 [0.48, 4.87] |
| Analysis 8.2  Comparison 8 LUMBAR FUSION vs COGNITIVE EXERCISES (Degenerate disc), Outcome 2 Failure (independent assessor) at 1 year. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure (patient rating) Show forest plot | 1 | 57 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.38, 3.03] |
| Analysis 9.1  Comparison 9 INSTRUMENTED FUSION vs COGNITIVE EXERCISES (Post discectomy), Outcome 1 Failure (patient rating). | ||||
| 2 Failure (Independent observer rating) Show forest plot | 1 | 57 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.49, 4.08] |
| Analysis 9.2  Comparison 9 INSTRUMENTED FUSION vs COGNITIVE EXERCISES (Post discectomy), Outcome 2 Failure (Independent observer rating). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
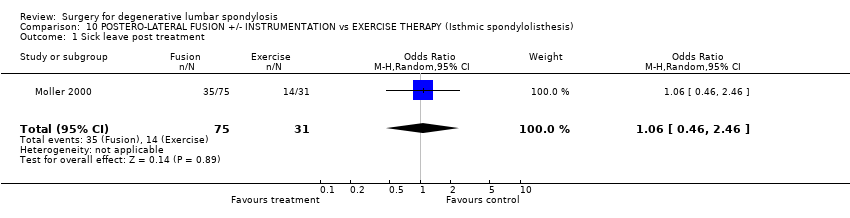
| 1 Sick leave post treatment Show forest plot | 1 | 106 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.46, 2.46] |
| Analysis 10.1  Comparison 10 POSTERO‐LATERAL FUSION +/‐ INSTRUMENTATION vs EXERCISE THERAPY (Isthmic spondylolisthesis), Outcome 1 Sick leave post treatment. | ||||
| 2 Failure ‐ patient rating Show forest plot | 1 | 109 | Odds Ratio (M‐H, Random, 95% CI) | 0.23 [0.10, 0.53] |
| Analysis 10.2  Comparison 10 POSTERO‐LATERAL FUSION +/‐ INSTRUMENTATION vs EXERCISE THERAPY (Isthmic spondylolisthesis), Outcome 2 Failure ‐ patient rating. | ||||
| 3 Failure ‐ Assessor rating Show forest plot | 1 | 109 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.03, 0.23] |
| Analysis 10.3  Comparison 10 POSTERO‐LATERAL FUSION +/‐ INSTRUMENTATION vs EXERCISE THERAPY (Isthmic spondylolisthesis), Outcome 3 Failure ‐ Assessor rating. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
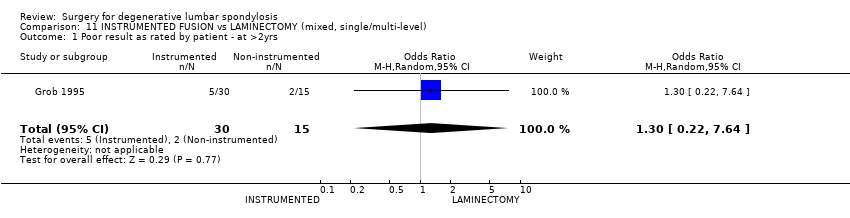
| 1 Poor result as rated by patient ‐ at >2yrs Show forest plot | 1 | 45 | Odds Ratio (M‐H, Random, 95% CI) | 1.3 [0.22, 7.64] |
| Analysis 11.1  Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 1 Poor result as rated by patient ‐ at >2yrs. | ||||
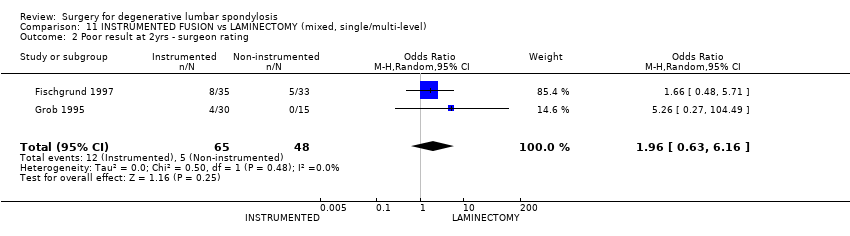
| 2 Poor result at 2yrs ‐ surgeon rating Show forest plot | 2 | 113 | Odds Ratio (M‐H, Random, 95% CI) | 1.96 [0.63, 6.16] |
| Analysis 11.2  Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 2 Poor result at 2yrs ‐ surgeon rating. | ||||
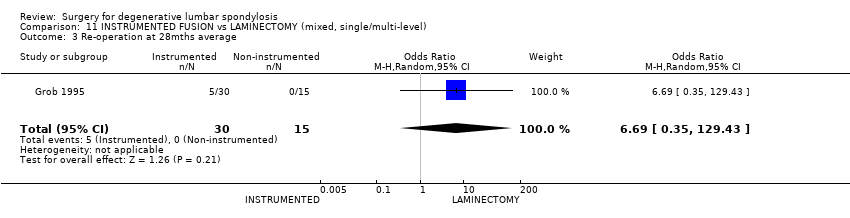
| 3 Re‐operation at 28mths average Show forest plot | 1 | 45 | Odds Ratio (M‐H, Random, 95% CI) | 6.69 [0.35, 129.43] |
| Analysis 11.3  Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 3 Re‐operation at 28mths average. | ||||
| 4 Spondylolisthesis progression Show forest plot | 1 | 33 | Odds Ratio (M‐H, Random, 95% CI) | 0.05 [0.00, 0.60] |
| Analysis 11.4  Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 4 Spondylolisthesis progression. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fair/Poor outcome at 1 ‐ 2yr ‐ Surgeon rating Show forest plot | 3 | 193 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.08, 4.26] |
| Analysis 12.1  Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 1 Fair/Poor outcome at 1 ‐ 2yr ‐ Surgeon rating. | ||||
| 2 2nd procedure by 2yrs Show forest plot | 7 | 494 | Odds Ratio (M‐H, Random, 95% CI) | 1.05 [0.40, 2.73] |
| Analysis 12.2  Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 2 2nd procedure by 2yrs. | ||||
| 3 No fusion at 2 yrs Show forest plot | 8 | 638 | Odds Ratio (M‐H, Random, 95% CI) | 0.43 [0.21, 0.91] |
| Analysis 12.3  Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 3 No fusion at 2 yrs. | ||||
| 4 Poor clinical outcome Show forest plot | 8 | 653 | Odds Ratio (M‐H, Random, 95% CI) | 0.49 [0.28, 0.84] |
| Analysis 12.4  Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 4 Poor clinical outcome. | ||||
| 5 Re‐operation at 5 years Show forest plot | 1 | 120 | Odds Ratio (M‐H, Random, 95% CI) | 2.65 [1.08, 6.51] |
| Analysis 12.5  Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 5 Re‐operation at 5 years. | ||||
| 6 Pain score at 5 years Show forest plot | 1 | 109 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.12, 1.18] |
| Analysis 12.6  Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 6 Pain score at 5 years. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure ‐ Patient rating at 2 yr Show forest plot | 1 | 75 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.12, 1.12] |
| Analysis 13.1  Comparison 13 INSTRUMENTED FUSION vs NON‐INSTRUMENTED FUSION (Isthmic spondylolisthesis), Outcome 1 Failure ‐ Patient rating at 2 yr. | ||||
| 2 Failure ‐ Assessor rating Show forest plot | 1 | 75 | Odds Ratio (M‐H, Random, 95% CI) | 0.70 [0.25, 1.92] |
| Analysis 13.2  Comparison 13 INSTRUMENTED FUSION vs NON‐INSTRUMENTED FUSION (Isthmic spondylolisthesis), Outcome 2 Failure ‐ Assessor rating. | ||||
| 3 Failed fusion (definitely not solid) Show forest plot | 1 | 74 | Odds Ratio (M‐H, Random, 95% CI) | 0.51 [0.18, 1.43] |
| Analysis 13.3  Comparison 13 INSTRUMENTED FUSION vs NON‐INSTRUMENTED FUSION (Isthmic spondylolisthesis), Outcome 3 Failed fusion (definitely not solid). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fusion failure Show forest plot | 2 | 201 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.51, 2.29] |
| Analysis 14.1  Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 1 Fusion failure. | ||||
| 2 Complications Show forest plot | 2 | 201 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.24, 4.17] |
| Analysis 14.2  Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 2 Complications. | ||||
| 3 Not much better Show forest plot | 1 | 149 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.59, 2.33] |
| Analysis 14.3  Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 3 Not much better. | ||||
| 4 Re‐operation Show forest plot | 1 | 139 | Odds Ratio (M‐H, Random, 95% CI) | 0.25 [0.09, 0.74] |
| Analysis 14.4  Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 4 Re‐operation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fusion failure Show forest plot | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 2.35 [0.40, 13.90] |
| Analysis 15.1  Comparison 15 ALIF PLUS POSTEROLATERAL INSTRUMENTED vs ALIF plus INSTRUMENTED, Outcome 1 Fusion failure. | ||||
| 2 Re‐operation Show forest plot | 1 | 48 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.28, 2.96] |
| Analysis 15.2  Comparison 15 ALIF PLUS POSTEROLATERAL INSTRUMENTED vs ALIF plus INSTRUMENTED, Outcome 2 Re‐operation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Re‐operation Show forest plot | 1 | 56 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 8.24] |
| Analysis 16.1  Comparison 16 GRAF LIGAMENTOPLASTY vs ANTERIOR LUMBAR CAGED FUSION, Outcome 1 Re‐operation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure of fusion Show forest plot | 1 | 118 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.01, 0.15] |
| Analysis 17.1  Comparison 17 ANTERIOR THREADED CAGE vs FEMORAL RING FUSION, Outcome 1 Failure of fusion. | ||||
| 2 Secondary procedure Show forest plot | 1 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.18, 0.76] |
| Analysis 17.2  Comparison 17 ANTERIOR THREADED CAGE vs FEMORAL RING FUSION, Outcome 2 Secondary procedure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No success (observer rated) ‐ at 8 weeks Show forest plot | 1 | 28 | Odds Ratio (M‐H, Random, 95% CI) | 1.85 [0.15, 23.07] |
| Analysis 18.1  Comparison 18 IDET vs SHAM, Outcome 1 No success (observer rated) ‐ at 8 weeks. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure of fusion with internal fixation Show forest plot | 3 | 290 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.15, 2.30] |
| Analysis 19.1  Comparison 19 ANY FORM OF ELECTRICAL STIMULATION vs PLACEBO, Outcome 1 Failure of fusion with internal fixation. | ||||
| 2 Failure of fusion without internal fixation Show forest plot | 3 | 268 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.22, 0.64] |
| Analysis 19.2  Comparison 19 ANY FORM OF ELECTRICAL STIMULATION vs PLACEBO, Outcome 2 Failure of fusion without internal fixation. | ||||
| 3 Poor clincical outcome Show forest plot | 3 | 357 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.27, 1.24] |
| Analysis 19.3  Comparison 19 ANY FORM OF ELECTRICAL STIMULATION vs PLACEBO, Outcome 3 Poor clincical outcome. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Secondary surgery Show forest plot | 1 | 196 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.09, 0.73] |
| Analysis 20.1  Comparison 20 X‐STOP INTERSPINOUS IMPLANT vs CONTROL, Outcome 1 Secondary surgery. | ||||
| 2 Moderate or severe pain Show forest plot | 1 | 167 | Odds Ratio (M‐H, Random, 95% CI) | 0.14 [0.07, 0.29] |
| Analysis 20.2  Comparison 20 X‐STOP INTERSPINOUS IMPLANT vs CONTROL, Outcome 2 Moderate or severe pain. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oswestry Disability Index at 2 years Show forest plot | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐4.30 [‐10.28, 1.68] |
| Analysis 21.1  Comparison 21 CHARITE DISC REPLACEMENT vs BAK ANTERIOR INTERBODY FUSION, Outcome 1 Oswestry Disability Index at 2 years. | ||||
| 2 VAS‐pain Show forest plot | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐5.70 [‐13.71, 2.31] |
| Analysis 21.2  Comparison 21 CHARITE DISC REPLACEMENT vs BAK ANTERIOR INTERBODY FUSION, Outcome 2 VAS‐pain. | ||||
| 3 Device failure Show forest plot | 1 | 304 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.32, 2.45] |
| Analysis 21.3  Comparison 21 CHARITE DISC REPLACEMENT vs BAK ANTERIOR INTERBODY FUSION, Outcome 3 Device failure. | ||||
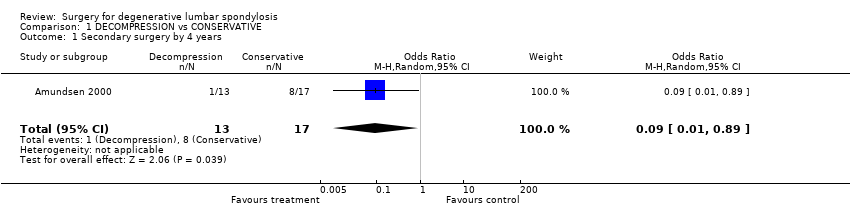
Comparison 1 DECOMPRESSION vs CONSERVATIVE, Outcome 1 Secondary surgery by 4 years.
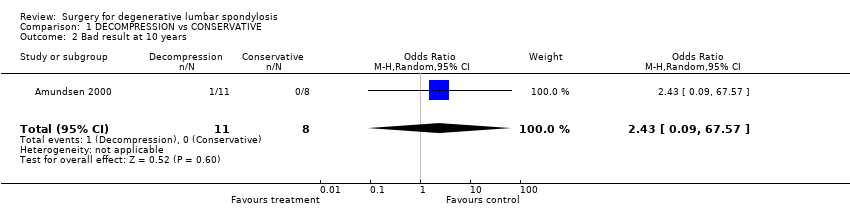
Comparison 1 DECOMPRESSION vs CONSERVATIVE, Outcome 2 Bad result at 10 years.

Comparison 2 MULTIPLE LAMINOTOMY vs LAMINECTOMY, Outcome 1 No success: combined patient / surgeon rating.
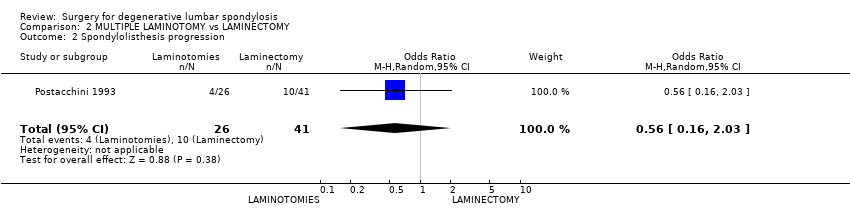
Comparison 2 MULTIPLE LAMINOTOMY vs LAMINECTOMY, Outcome 2 Spondylolisthesis progression.
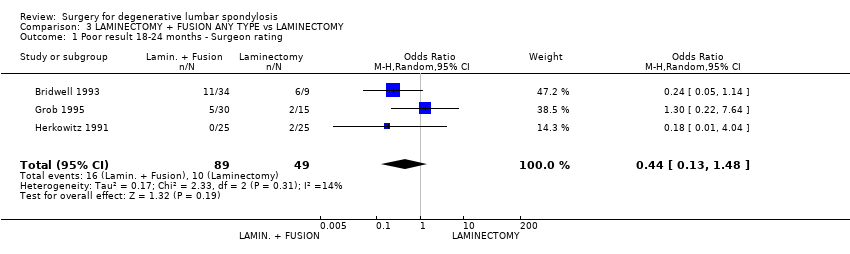
Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 1 Poor result 18‐24 months ‐ Surgeon rating.

Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 2 Re‐operation 2‐4 years.

Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 3 Spondylolisthesis progression.
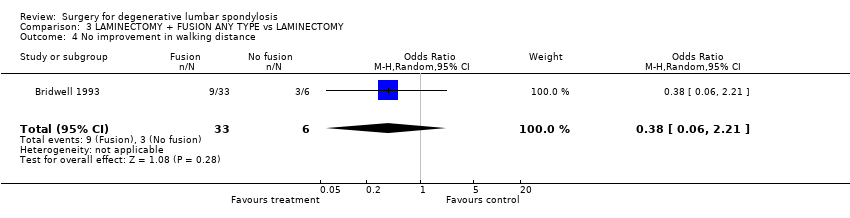
Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 4 No improvement in walking distance.

Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 5 Good result at 18‐24 months.
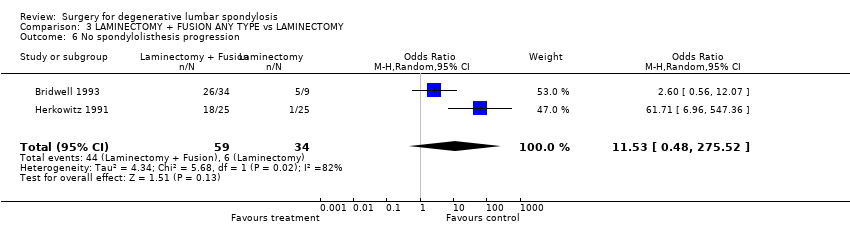
Comparison 3 LAMINECTOMY + FUSION ANY TYPE vs LAMINECTOMY, Outcome 6 No spondylolisthesis progression.

Comparison 4 LAMINECTOMY PLUS MULTI‐LEVEL FUSION vs LAMINECTOMY, Outcome 1 Poor result as rated by patient ‐ at 2yrs.

Comparison 4 LAMINECTOMY PLUS MULTI‐LEVEL FUSION vs LAMINECTOMY, Outcome 2 Poor result as rated by independent assessor ‐ at 2yrs.
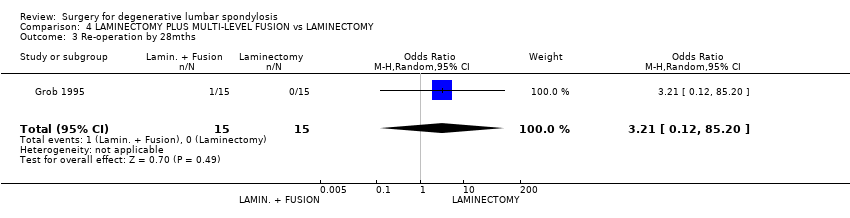
Comparison 4 LAMINECTOMY PLUS MULTI‐LEVEL FUSION vs LAMINECTOMY, Outcome 3 Re‐operation by 28mths.

Comparison 5 LAMINECTOMY vs NO LAMINECTOMY (Isthmic spondylolisthesis), Outcome 1 No fusion at 4.5yrs.

Comparison 5 LAMINECTOMY vs NO LAMINECTOMY (Isthmic spondylolisthesis), Outcome 2 No success ‐ Patient rating at 4.5yrs.
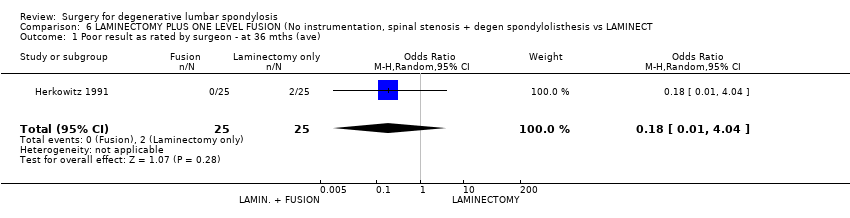
Comparison 6 LAMINECTOMY PLUS ONE LEVEL FUSION (No instrumentation, spinal stenosis + degen spondylolisthesis vs LAMINECT, Outcome 1 Poor result as rated by surgeon ‐ at 36 mths (ave).

Comparison 6 LAMINECTOMY PLUS ONE LEVEL FUSION (No instrumentation, spinal stenosis + degen spondylolisthesis vs LAMINECT, Outcome 2 Spondylolisthesis progression at 6 months.
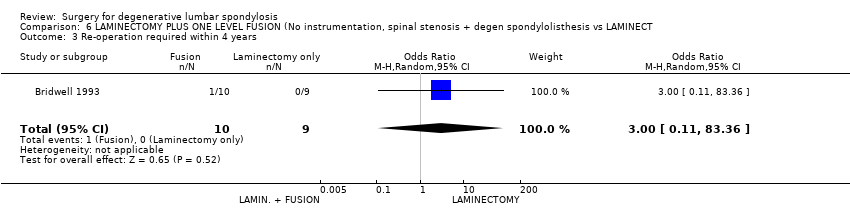
Comparison 6 LAMINECTOMY PLUS ONE LEVEL FUSION (No instrumentation, spinal stenosis + degen spondylolisthesis vs LAMINECT, Outcome 3 Re‐operation required within 4 years.

Comparison 7 LUMBAR FUSION vs CONSERVATIVE (PHYSICAL) THERAPY, Outcome 1 Fair or Poor outcome (independent observer rated).

Comparison 7 LUMBAR FUSION vs CONSERVATIVE (PHYSICAL) THERAPY, Outcome 2 Not back to work at 2 years.
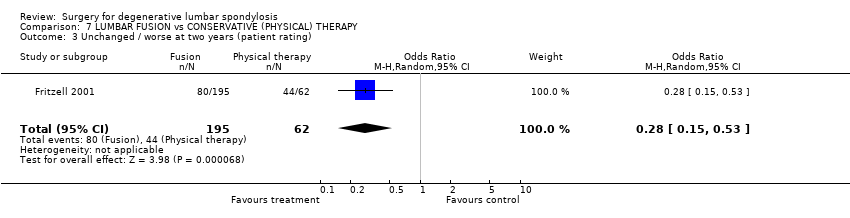
Comparison 7 LUMBAR FUSION vs CONSERVATIVE (PHYSICAL) THERAPY, Outcome 3 Unchanged / worse at two years (patient rating).

Comparison 8 LUMBAR FUSION vs COGNITIVE EXERCISES (Degenerate disc), Outcome 1 Failure (patient rating) at 1 year.

Comparison 8 LUMBAR FUSION vs COGNITIVE EXERCISES (Degenerate disc), Outcome 2 Failure (independent assessor) at 1 year.
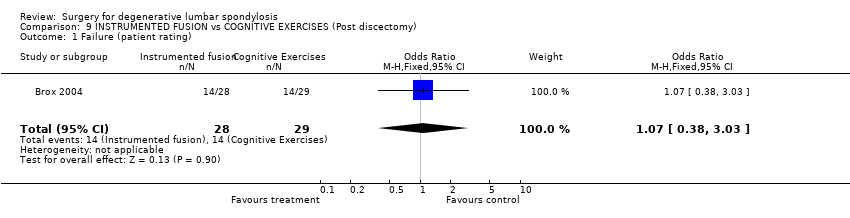
Comparison 9 INSTRUMENTED FUSION vs COGNITIVE EXERCISES (Post discectomy), Outcome 1 Failure (patient rating).
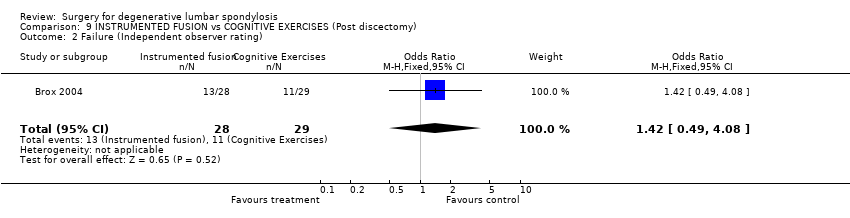
Comparison 9 INSTRUMENTED FUSION vs COGNITIVE EXERCISES (Post discectomy), Outcome 2 Failure (Independent observer rating).
Comparison 10 POSTERO‐LATERAL FUSION +/‐ INSTRUMENTATION vs EXERCISE THERAPY (Isthmic spondylolisthesis), Outcome 1 Sick leave post treatment.

Comparison 10 POSTERO‐LATERAL FUSION +/‐ INSTRUMENTATION vs EXERCISE THERAPY (Isthmic spondylolisthesis), Outcome 2 Failure ‐ patient rating.

Comparison 10 POSTERO‐LATERAL FUSION +/‐ INSTRUMENTATION vs EXERCISE THERAPY (Isthmic spondylolisthesis), Outcome 3 Failure ‐ Assessor rating.
Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 1 Poor result as rated by patient ‐ at >2yrs.
Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 2 Poor result at 2yrs ‐ surgeon rating.
Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 3 Re‐operation at 28mths average.

Comparison 11 INSTRUMENTED FUSION vs LAMINECTOMY (mixed, single/multi‐level), Outcome 4 Spondylolisthesis progression.
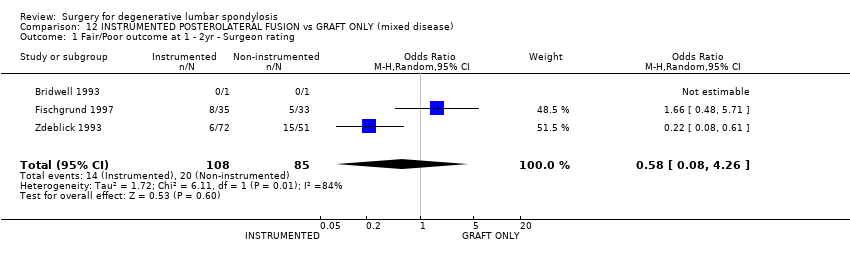
Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 1 Fair/Poor outcome at 1 ‐ 2yr ‐ Surgeon rating.

Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 2 2nd procedure by 2yrs.
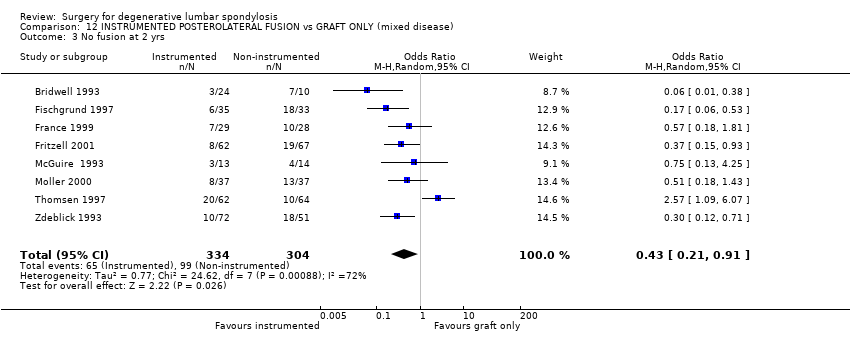
Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 3 No fusion at 2 yrs.

Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 4 Poor clinical outcome.

Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 5 Re‐operation at 5 years.

Comparison 12 INSTRUMENTED POSTEROLATERAL FUSION vs GRAFT ONLY (mixed disease), Outcome 6 Pain score at 5 years.
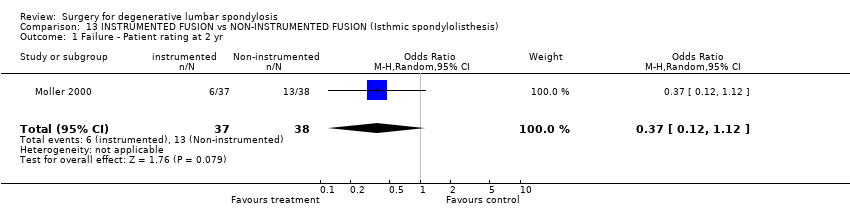
Comparison 13 INSTRUMENTED FUSION vs NON‐INSTRUMENTED FUSION (Isthmic spondylolisthesis), Outcome 1 Failure ‐ Patient rating at 2 yr.
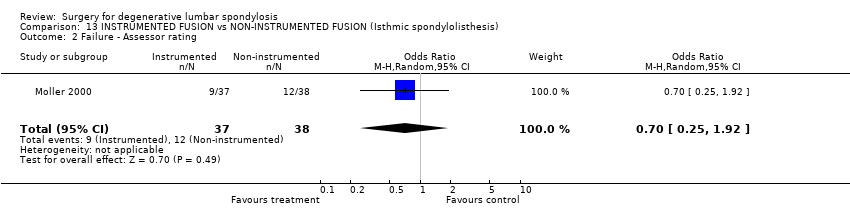
Comparison 13 INSTRUMENTED FUSION vs NON‐INSTRUMENTED FUSION (Isthmic spondylolisthesis), Outcome 2 Failure ‐ Assessor rating.
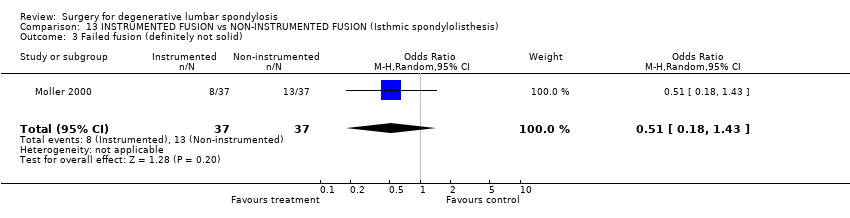
Comparison 13 INSTRUMENTED FUSION vs NON‐INSTRUMENTED FUSION (Isthmic spondylolisthesis), Outcome 3 Failed fusion (definitely not solid).

Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 1 Fusion failure.

Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 2 Complications.
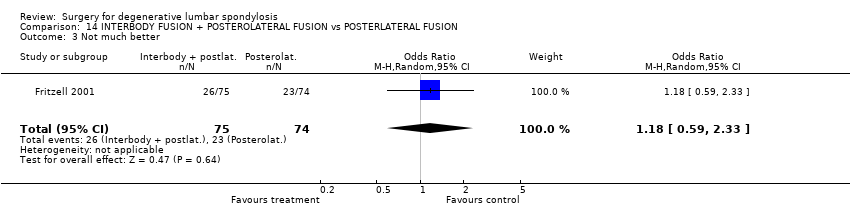
Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 3 Not much better.
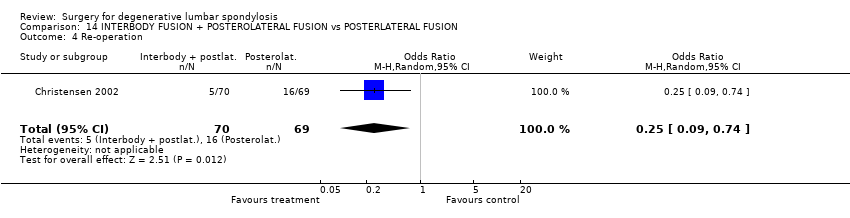
Comparison 14 INTERBODY FUSION + POSTEROLATERAL FUSION vs POSTERLATERAL FUSION, Outcome 4 Re‐operation.
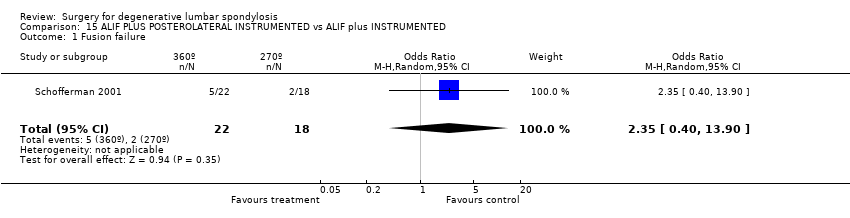
Comparison 15 ALIF PLUS POSTEROLATERAL INSTRUMENTED vs ALIF plus INSTRUMENTED, Outcome 1 Fusion failure.

Comparison 15 ALIF PLUS POSTEROLATERAL INSTRUMENTED vs ALIF plus INSTRUMENTED, Outcome 2 Re‐operation.
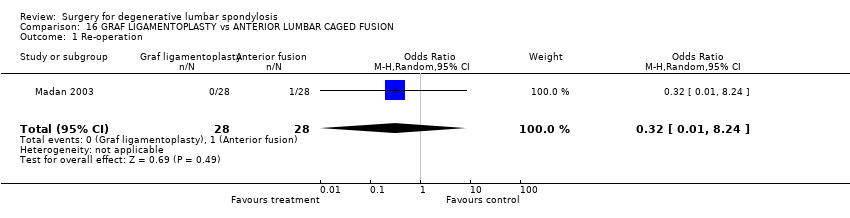
Comparison 16 GRAF LIGAMENTOPLASTY vs ANTERIOR LUMBAR CAGED FUSION, Outcome 1 Re‐operation.
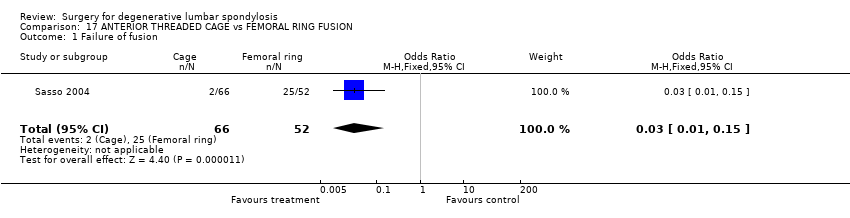
Comparison 17 ANTERIOR THREADED CAGE vs FEMORAL RING FUSION, Outcome 1 Failure of fusion.

Comparison 17 ANTERIOR THREADED CAGE vs FEMORAL RING FUSION, Outcome 2 Secondary procedure.
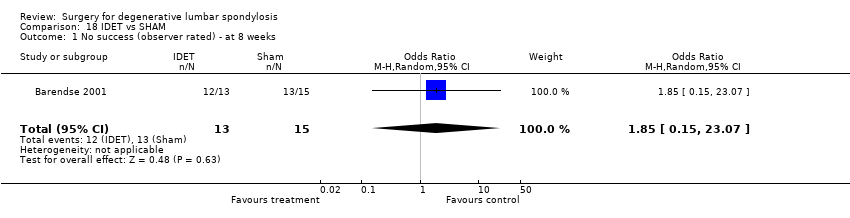
Comparison 18 IDET vs SHAM, Outcome 1 No success (observer rated) ‐ at 8 weeks.

Comparison 19 ANY FORM OF ELECTRICAL STIMULATION vs PLACEBO, Outcome 1 Failure of fusion with internal fixation.

Comparison 19 ANY FORM OF ELECTRICAL STIMULATION vs PLACEBO, Outcome 2 Failure of fusion without internal fixation.
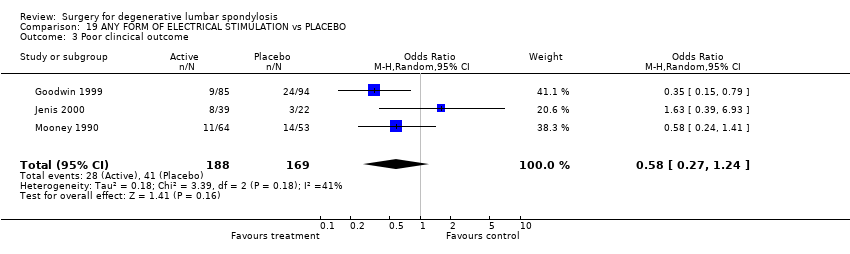
Comparison 19 ANY FORM OF ELECTRICAL STIMULATION vs PLACEBO, Outcome 3 Poor clincical outcome.
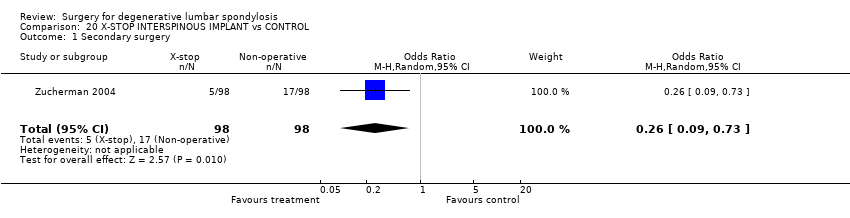
Comparison 20 X‐STOP INTERSPINOUS IMPLANT vs CONTROL, Outcome 1 Secondary surgery.
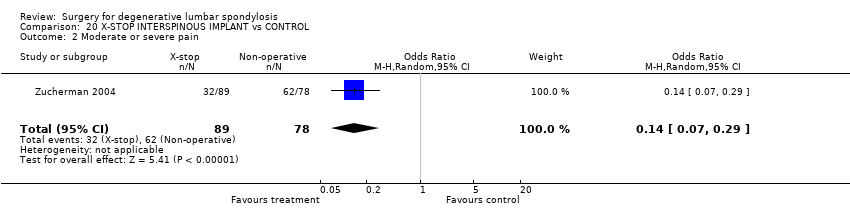
Comparison 20 X‐STOP INTERSPINOUS IMPLANT vs CONTROL, Outcome 2 Moderate or severe pain.
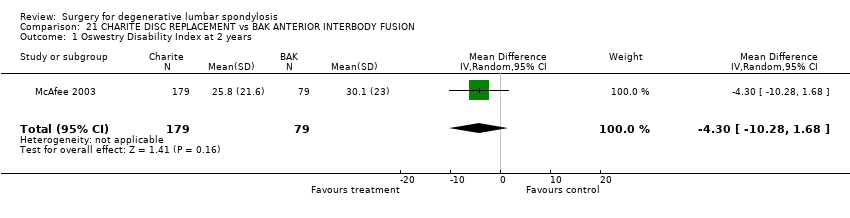
Comparison 21 CHARITE DISC REPLACEMENT vs BAK ANTERIOR INTERBODY FUSION, Outcome 1 Oswestry Disability Index at 2 years.
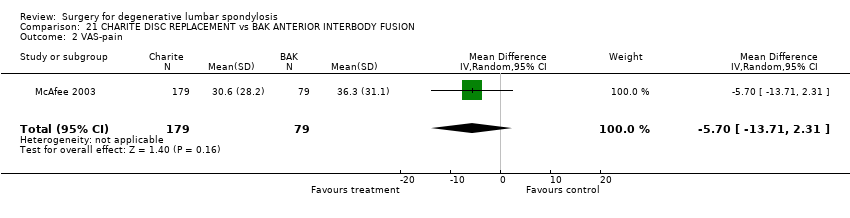
Comparison 21 CHARITE DISC REPLACEMENT vs BAK ANTERIOR INTERBODY FUSION, Outcome 2 VAS‐pain.

Comparison 21 CHARITE DISC REPLACEMENT vs BAK ANTERIOR INTERBODY FUSION, Outcome 3 Device failure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Secondary surgery by 4 years Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 0.89] |
| 2 Bad result at 10 years Show forest plot | 1 | 19 | Odds Ratio (M‐H, Random, 95% CI) | 2.43 [0.09, 67.57] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No success: combined patient / surgeon rating Show forest plot | 1 | 67 | Odds Ratio (M‐H, Random, 95% CI) | 0.85 [0.25, 2.88] |
| 2 Spondylolisthesis progression Show forest plot | 1 | 67 | Odds Ratio (M‐H, Random, 95% CI) | 0.56 [0.16, 2.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result 18‐24 months ‐ Surgeon rating Show forest plot | 3 | 138 | Odds Ratio (M‐H, Random, 95% CI) | 0.44 [0.13, 1.48] |
| 2 Re‐operation 2‐4 years Show forest plot | 2 | 64 | Odds Ratio (M‐H, Random, 95% CI) | 4.69 [0.51, 42.83] |
| 3 Spondylolisthesis progression Show forest plot | 2 | 93 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.00, 2.07] |
| 4 No improvement in walking distance Show forest plot | 1 | 39 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.06, 2.21] |
| 5 Good result at 18‐24 months Show forest plot | 2 | 93 | Odds Ratio (M‐H, Random, 95% CI) | 4.41 [1.09, 17.76] |
| 6 No spondylolisthesis progression Show forest plot | 2 | 93 | Odds Ratio (M‐H, Random, 95% CI) | 11.53 [0.48, 275.52] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result as rated by patient ‐ at 2yrs Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 5.74 [0.25, 130.37] |
| 2 Poor result as rated by independent assessor ‐ at 2yrs Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 8.68 [0.41, 184.28] |
| 3 Re‐operation by 28mths Show forest plot | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 3.21 [0.12, 85.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No fusion at 4.5yrs Show forest plot | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 15.21 [0.76, 303.32] |
| 2 No success ‐ Patient rating at 4.5yrs Show forest plot | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 11.5 [1.24, 106.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result as rated by surgeon ‐ at 36 mths (ave) Show forest plot | 1 | 50 | Odds Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 4.04] |
| 2 Spondylolisthesis progression at 6 months Show forest plot | 1 | 19 | Odds Ratio (M‐H, Random, 95% CI) | 4.67 [0.67, 32.36] |
| 3 Re‐operation required within 4 years Show forest plot | 1 | 19 | Odds Ratio (M‐H, Random, 95% CI) | 3.00 [0.11, 83.36] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fair or Poor outcome (independent observer rated) Show forest plot | 1 | 262 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.13, 0.52] |
| 2 Not back to work at 2 years Show forest plot | 1 | 208 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.10, 0.64] |
| 3 Unchanged / worse at two years (patient rating) Show forest plot | 1 | 257 | Odds Ratio (M‐H, Random, 95% CI) | 0.28 [0.15, 0.53] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure (patient rating) at 1 year Show forest plot | 1 | 61 | Odds Ratio (M‐H, Random, 95% CI) | 0.76 [0.25, 2.25] |
| 2 Failure (independent assessor) at 1 year Show forest plot | 2 | 63 | Odds Ratio (M‐H, Random, 95% CI) | 1.53 [0.48, 4.87] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure (patient rating) Show forest plot | 1 | 57 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.38, 3.03] |
| 2 Failure (Independent observer rating) Show forest plot | 1 | 57 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.49, 4.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sick leave post treatment Show forest plot | 1 | 106 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.46, 2.46] |
| 2 Failure ‐ patient rating Show forest plot | 1 | 109 | Odds Ratio (M‐H, Random, 95% CI) | 0.23 [0.10, 0.53] |
| 3 Failure ‐ Assessor rating Show forest plot | 1 | 109 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.03, 0.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Poor result as rated by patient ‐ at >2yrs Show forest plot | 1 | 45 | Odds Ratio (M‐H, Random, 95% CI) | 1.3 [0.22, 7.64] |
| 2 Poor result at 2yrs ‐ surgeon rating Show forest plot | 2 | 113 | Odds Ratio (M‐H, Random, 95% CI) | 1.96 [0.63, 6.16] |
| 3 Re‐operation at 28mths average Show forest plot | 1 | 45 | Odds Ratio (M‐H, Random, 95% CI) | 6.69 [0.35, 129.43] |
| 4 Spondylolisthesis progression Show forest plot | 1 | 33 | Odds Ratio (M‐H, Random, 95% CI) | 0.05 [0.00, 0.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fair/Poor outcome at 1 ‐ 2yr ‐ Surgeon rating Show forest plot | 3 | 193 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.08, 4.26] |
| 2 2nd procedure by 2yrs Show forest plot | 7 | 494 | Odds Ratio (M‐H, Random, 95% CI) | 1.05 [0.40, 2.73] |
| 3 No fusion at 2 yrs Show forest plot | 8 | 638 | Odds Ratio (M‐H, Random, 95% CI) | 0.43 [0.21, 0.91] |
| 4 Poor clinical outcome Show forest plot | 8 | 653 | Odds Ratio (M‐H, Random, 95% CI) | 0.49 [0.28, 0.84] |
| 5 Re‐operation at 5 years Show forest plot | 1 | 120 | Odds Ratio (M‐H, Random, 95% CI) | 2.65 [1.08, 6.51] |
| 6 Pain score at 5 years Show forest plot | 1 | 109 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.12, 1.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure ‐ Patient rating at 2 yr Show forest plot | 1 | 75 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.12, 1.12] |
| 2 Failure ‐ Assessor rating Show forest plot | 1 | 75 | Odds Ratio (M‐H, Random, 95% CI) | 0.70 [0.25, 1.92] |
| 3 Failed fusion (definitely not solid) Show forest plot | 1 | 74 | Odds Ratio (M‐H, Random, 95% CI) | 0.51 [0.18, 1.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fusion failure Show forest plot | 2 | 201 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.51, 2.29] |
| 2 Complications Show forest plot | 2 | 201 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.24, 4.17] |
| 3 Not much better Show forest plot | 1 | 149 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.59, 2.33] |
| 4 Re‐operation Show forest plot | 1 | 139 | Odds Ratio (M‐H, Random, 95% CI) | 0.25 [0.09, 0.74] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fusion failure Show forest plot | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 2.35 [0.40, 13.90] |
| 2 Re‐operation Show forest plot | 1 | 48 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.28, 2.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Re‐operation Show forest plot | 1 | 56 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 8.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure of fusion Show forest plot | 1 | 118 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.01, 0.15] |
| 2 Secondary procedure Show forest plot | 1 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.18, 0.76] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No success (observer rated) ‐ at 8 weeks Show forest plot | 1 | 28 | Odds Ratio (M‐H, Random, 95% CI) | 1.85 [0.15, 23.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure of fusion with internal fixation Show forest plot | 3 | 290 | Odds Ratio (M‐H, Random, 95% CI) | 0.59 [0.15, 2.30] |
| 2 Failure of fusion without internal fixation Show forest plot | 3 | 268 | Odds Ratio (M‐H, Random, 95% CI) | 0.38 [0.22, 0.64] |
| 3 Poor clincical outcome Show forest plot | 3 | 357 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.27, 1.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Secondary surgery Show forest plot | 1 | 196 | Odds Ratio (M‐H, Random, 95% CI) | 0.26 [0.09, 0.73] |
| 2 Moderate or severe pain Show forest plot | 1 | 167 | Odds Ratio (M‐H, Random, 95% CI) | 0.14 [0.07, 0.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oswestry Disability Index at 2 years Show forest plot | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐4.30 [‐10.28, 1.68] |
| 2 VAS‐pain Show forest plot | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐5.70 [‐13.71, 2.31] |
| 3 Device failure Show forest plot | 1 | 304 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.32, 2.45] |

