Laparoscopic surgery for pelvic pain associated with endometriosis
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomisation by computer generated randomisation sequence. Allocation concealment not referred to within the text. Double blinded. Participant and observer. | |
| Participants | Location: Middlesbrough, UK. | |
| Interventions | Laparoscopic excision of areas of endometriosis. | |
| Outcomes | Pain symptoms were recorded by being asked to complete a visual analogue score before the intervention and again six months after the procedure. Participants were asked to complete a visual analogue score. Post‐operative complications were reported. | |
| Notes | Ethics committee approval was obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not referred to within the text. |
| Blinding (performance bias and detection bias) | Low risk | Double blinded. Participant and observer. |
| Incomplete outcome data (attrition bias) | Low risk | |
| Selective reporting (reporting bias) | Low risk | |
| Methods | Randomisation by computer generated randomisation sequence. Allocations contained within opaque envelopes. Double blinded. Participant and observer. | |
| Participants | Location: Calgary, Canada. | |
| Interventions | Laparoscopic excision of areas of endometriosis. | |
| Outcomes | Pain symptoms were recorded by being asked to complete daily visual analogue scales for one month at three month intervals post‐operatively for twelve months. The mean pain scores were reported by the study six and twelve months post operatively, however we have assumed the error bars of figure 5 represent standard deviation and not the standard error of the mean. | |
| Notes | Ethics committee approval was obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation sequence. |
| Allocation concealment (selection bias) | Low risk | Allocations contained within opaque envelopes. |
| Blinding (performance bias and detection bias) | Low risk | Double blinded. Participant and observer. |
| Incomplete outcome data (attrition bias) | Low risk | |
| Selective reporting (reporting bias) | Low risk | |
| Methods | Randomisation method was unclear. Allocation concealment not referred to within the text. Presence of blinded was unclear. | |
| Participants | Location: Limerick, Republic of Ireland. | |
| Interventions | Laparoscopic coagulation therapy of areas of endometriosis. | |
| Outcomes | Pain symptoms were recorded by being asked to complete a visual analogue score before the intervention and again three, six and twelve months after the procedure. Reported the mean operative time. | |
| Notes | Ethics committee approval was obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated as randomised. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not referred to within the text. |
| Blinding (performance bias and detection bias) | Unclear risk | Not referred to within the text. |
| Incomplete outcome data (attrition bias) | Low risk | |
| Selective reporting (reporting bias) | Low risk | |
| Methods | Randomisation by computer generated randomisation sequence. Double blinded. Participant and observer. Allocation concealment not referred to within the text.Not referred to within the text. | |
| Participants | Location Guildford UK, | |
| Interventions | Laser treatment including vaporisation of all visible endometriotic implants, adhesiolysis, and uterine nerve transection. | |
| Outcomes | Reported pain scores and 10cm linear analogue visual scale for dysmenorrhoea, dyspareunia, and pelvic pain, before the procedure and three and six months after the procedure. Post‐operative complications were reported. | |
| Notes | Ethics committee approval was obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not referred to within the text. |
| Blinding (performance bias and detection bias) | Low risk | Double blinded. Participant and observer. |
| Incomplete outcome data (attrition bias) | Low risk | 74 women entered the study. 63 completed to 6 month follow up. No reasons were stated for 4 participants. |
| Selective reporting (reporting bias) | Unclear risk | It is unclear how many women underwent one, two or all of the three potential interventions of laser ablation, adhesiolysis and uterine nerve ablation. |
| Methods | Randomisation method unclear. Allocation concealment not referred to within the text. Stated as single‐blinded, patient or research nurse blinded unclear. | |
| Participants | Location: Bucharest, Romania. | |
| Interventions | Laparoscopic excision or coagulation of areas of endometriosis. | |
| Outcomes | Pain symptoms were recorded by being asked to complete a visual analogue score before the intervention and again six and twelve months after the procedure. | |
| Notes | Infomed consent was obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated as randomised. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not referred to within the text. |
| Blinding (performance bias and detection bias) | Unclear risk | Not referred to within the text. |
| Incomplete outcome data (attrition bias) | Low risk | |
| Selective reporting (reporting bias) | Unclear risk | It is unclear how many women underwent one or two of the two potential interventions of laser ablation and coagulation. |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Comparison of two laparoscopic methods of treatment rather than comparison to non‐laparoscopic methods | |
| Comparison between two laparoscopic methods rather than laparoscopic methods with other treatment modalities | |
| Unpublished data. Comparison of laparoscopic laser ablation to laparoscopic laser ablation plus LUNA. No comparison to non‐laparoscopic treatment | |
| Randomised controlled study. Comparison of laparoscopy versus laparotomy for treatment of endometriomas. Outcome measures related to operating time and speed of recovery rather than improvement in symptoms. | |
| Abstract only. No data reported. Comparison of two laparoscopic techniques. | |
| Data not suitable for analysis of follow up as in most cases randomisation code was broken at six months and further surgery offered to expectant group. | |
| Comparison of two different laparoscopic methods rather than laparoscopic surgery with another treatment modality. | |
| Comparison of two different laparoscopic methods rather than laparoscopic surgery with another treatment modality. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain better or improved Show forest plot | 3 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Laparoscopic surgery versus no surgery, Outcome 1 Pain better or improved. | ||||
| 1.1 After 3 months | 1 | 63 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.36 [0.51, 3.64] |
| 1.2 After 6 months | 3 | 171 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 5.72 [3.09, 10.60] |
| 1.3 After 12 months | 1 | 69 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.72 [2.97, 20.06] |
| 2 Pain scores Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Laparoscopic surgery versus no surgery, Outcome 2 Pain scores. | ||||
| 2.1 6 months | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [0.31, 1.49] |
| 2.2 12 months | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 1.65 [1.11, 2.19] |
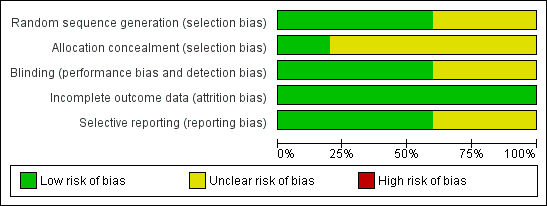
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
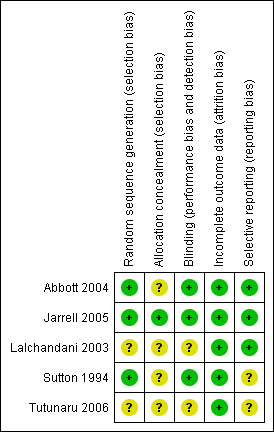
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
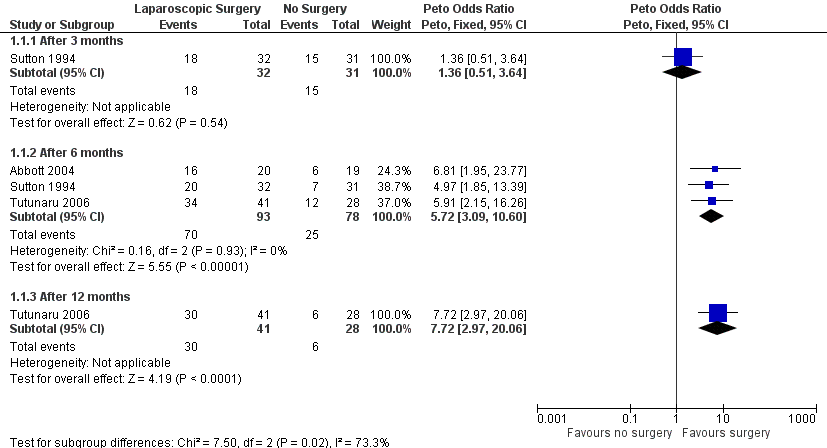
Forest plot of comparison: 1 Laparoscopic surgery versus no surgery, outcome: 1.1 Pain better or improved.

Comparison 1 Laparoscopic surgery versus no surgery, Outcome 1 Pain better or improved.

Comparison 1 Laparoscopic surgery versus no surgery, Outcome 2 Pain scores.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain better or improved Show forest plot | 3 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.1 After 3 months | 1 | 63 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.36 [0.51, 3.64] |
| 1.2 After 6 months | 3 | 171 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 5.72 [3.09, 10.60] |
| 1.3 After 12 months | 1 | 69 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.72 [2.97, 20.06] |
| 2 Pain scores Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 6 months | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [0.31, 1.49] |
| 2.2 12 months | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 1.65 [1.11, 2.19] |

