Рутинное бритье промежности при поступлении в больницу во время родов
Referencias
References to studies included in this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Alternate allocation. | |
| Participants | 389 women in labour. USA. | |
| Interventions | Pubic shaving plus the usual skin preparation (scrubbing of the external genitalia and inner thighs with green soap and water and the pouring of sterile water, alcohol and a weak solution of bichloride of mercury over the vulva and adjoining area) (N = 196) versus clipping of long pubic hairs only (no skin preparation) (N = 193). | |
| Outcomes | Febrile puerperia. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Women alternately allocated to experimental or control group. No information on the timing of allocation, the personnel involved, or the number of exclusions during this process. |
| Allocation concealment (selection bias) | High risk | No sufficient detail about allocation sequence concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not possible due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | No mention of blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not possible to determine the completeness of data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement. |
| Other bias | Low risk | No other sources of bias identified. |
| Methods | Method of allocation not specified. | |
| Participants | 150 labouring women pre delivery. USA. | |
| Interventions | First comparison: shaving of the pudendal and perineal areas (N = 50) versus clipping of long pubic hairs (N = 50). In all women the pudendal and perineal region was washed with a diluted pHisoHex solution. | |
| Outcomes | Positive bacteriology cultures (gram positive and negative). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method for determining the randomisation sequence not mentioned; insufficient information about the sequence generation process. |
| Allocation concealment (selection bias) | High risk | Insufficient detail about allocation sequence concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not possible due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | No mention of blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not possible to determine the completeness of data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement. |
| Other bias | Low risk | No other sources of bias identified. |
| Methods | Random allocation from a table of random numbers with sequentially numbered, sealed envelopes. | |
| Participants | 500 pregnant women recruited from 1 hospital. 42 women excluded after randomisation due to caesarean section. Thailand. | |
| Interventions | Perineal shaving (N = 231) versus cutting of perineal hair, down to 0.5 cm above the skin (N = 227). In all women the perineal region was scrubbed with 4% chlorhexidine scrub and rinsed with savlon solution (1:100). | |
| Outcomes | Perineal wound infection; puerperal morbidity; puerperal infection; neonatal infection; satisfaction of the patients, accoucheurs and perineorrhaphy operators. | |
| Notes | All women were attended by nurses, externs and obstetrics‐gynaecology residents. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of a published table of random sequence generation. |
| Allocation concealment (selection bias) | Low risk | Use of sealed sequentially numbered envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not possible due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | No mention of blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement. |
| Other bias | Low risk | No other sources of bias identified. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postpartum maternal febrile morbidity Show forest plot | 3 | 997 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.73, 1.76] |
| Analysis 1.1 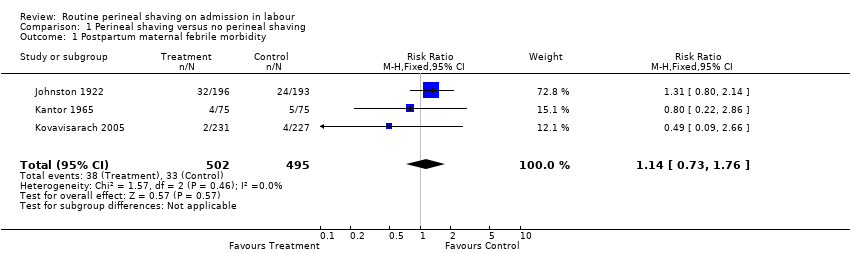 Comparison 1 Perineal shaving versus no perineal shaving, Outcome 1 Postpartum maternal febrile morbidity. | ||||
| 2 Colonisation Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Perineal shaving versus no perineal shaving, Outcome 2 Colonisation. | ||||
| 2.1 Gram‐positive | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.82, 1.64] |
| 2.2 Gram‐negative | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.70, 0.98] |
| 3 Neonatal infection Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.3 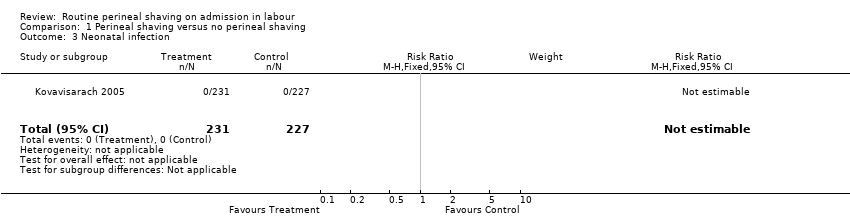 Comparison 1 Perineal shaving versus no perineal shaving, Outcome 3 Neonatal infection. | ||||
| 4 Wound infection Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.80, 2.70] |
| Analysis 1.4  Comparison 1 Perineal shaving versus no perineal shaving, Outcome 4 Wound infection. | ||||
| 5 Wound dehiscence Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.00] |
| Analysis 1.5  Comparison 1 Perineal shaving versus no perineal shaving, Outcome 5 Wound dehiscence. | ||||
| 6 Need for wound resuturing | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Discomfort | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Pain | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Maternal embarrassment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Maternal satisfaction continuous data Show forest plot | 1 | 458 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |
| Analysis 1.11  Comparison 1 Perineal shaving versus no perineal shaving, Outcome 11 Maternal satisfaction continuous data. | ||||
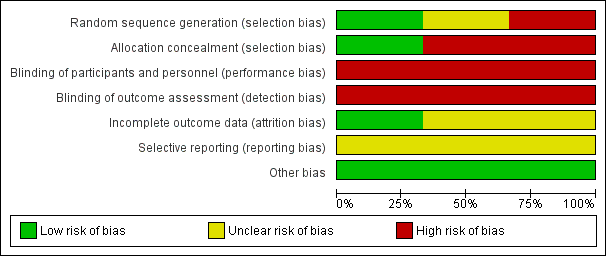
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
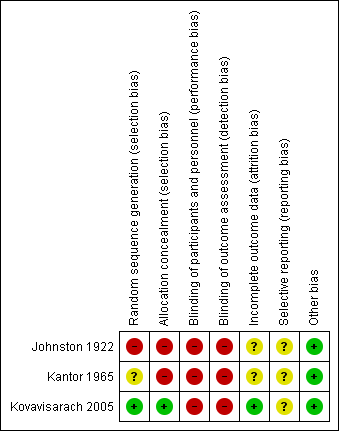
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 1 Postpartum maternal febrile morbidity.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 2 Colonisation.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 3 Neonatal infection.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 4 Wound infection.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 5 Wound dehiscence.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 11 Maternal satisfaction continuous data.
| Routine perineal shaving before childbirth for women in labour | ||||||
| Population: Women in labour | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Routine perineal shaving before childbirth | |||||
| Postpartum maternal febrile morbidity | Study population | RR 1.16 | 997 | ⊕⊝⊝⊝ | ||
| 67 per 1000 | 77 per 1000 | |||||
| Low | ||||||
| 18 per 1000 | 20 per 1000 | |||||
| High | ||||||
| 124 per 1000 | 141 per 1000 | |||||
| Neonatal infection | Study population | Not estimable | 458 | see comment | The outcome was reported with no events. | |
| See comment | See comment | |||||
| Moderate | ||||||
| Wound infection | Study population | RR 1.47 | 458 | ⊕⊕⊝⊝ | ||
| 70 per 1000 | 103 per 1000 | |||||
| Moderate | ||||||
| 70 per 1000 | 103 per 1000 | |||||
| Maternal satisfaction | The mean maternal satisfaction in the control groups was | The mean maternal satisfaction in the intervention groups was | MD 0.00 (‐0.13, 0.13) | 458 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most studies contributing data had serious design limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postpartum maternal febrile morbidity Show forest plot | 3 | 997 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.73, 1.76] |
| 2 Colonisation Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Gram‐positive | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.82, 1.64] |
| 2.2 Gram‐negative | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.70, 0.98] |
| 3 Neonatal infection Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Wound infection Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.80, 2.70] |
| 5 Wound dehiscence Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.00] |
| 6 Need for wound resuturing | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Discomfort | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Pain | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Maternal embarrassment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Maternal satisfaction continuous data Show forest plot | 1 | 458 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |

