Rasurado perineal sistemático al ingreso en trabajo de parto
Información
- DOI:
- https://doi.org/10.1002/14651858.CD001236.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 14 noviembre 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Vittorio Basevi wrote the protocol and Tina Lavender commented. Tina Lavender and Vittorio Basevi wrote the review. Vittorio Basevi extracted the data and Tina Lavender checked the data.
Vittorio Basevi drafted the 2014 updated and Tina Lavender commented on drafts.
Sources of support
Internal sources
-
Direzione generale sanità e politiche sociali,Regione Emilia‐Romagna,Bologna, Italy.
External sources
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
None known.
Acknowledgements
This Cochrane review updates the pre‐Cochrane review undertaken by Prof Mary Renfrew in 1995 (Renfrew 1995).
We acknowledge Prof Zarko Alfirevic for his support and guidance and Dr Simona Di Mario for her support on the previous update of this review (Basevi 2000).
We would like to thank Erika Ota for her support in the creation of the 'Summary of findings' table for this update. Erika Ota's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Nov 14 | Routine perineal shaving on admission in labour | Review | Vittorio Basevi, Tina Lavender | |
| 2000 Oct 23 | Routine perineal shaving on admission in labour | Review | Vittorio Basevi, Tina Lavender | |
Differences between protocol and review
The methods have been updated for the 2014 update and the quality of the evidence assessed using GRADE in order to assess the quality of the body of evidence relating to key outcomes. We added 'side‐effects' as a non‐prespecified outcome.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICO
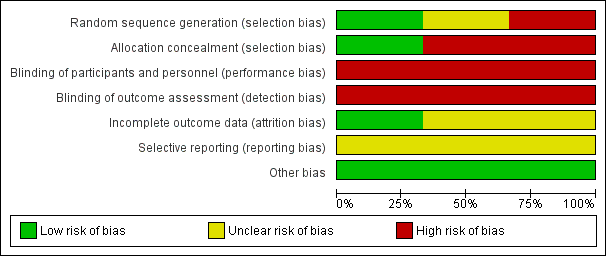
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
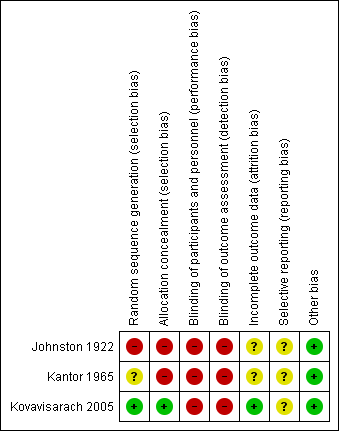
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 1 Postpartum maternal febrile morbidity.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 2 Colonisation.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 3 Neonatal infection.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 4 Wound infection.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 5 Wound dehiscence.

Comparison 1 Perineal shaving versus no perineal shaving, Outcome 11 Maternal satisfaction continuous data.
| Routine perineal shaving before childbirth for women in labour | ||||||
| Population: Women in labour | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Routine perineal shaving before childbirth | |||||
| Postpartum maternal febrile morbidity | Study population | RR 1.16 | 997 | ⊕⊝⊝⊝ | ||
| 67 per 1000 | 77 per 1000 | |||||
| Low | ||||||
| 18 per 1000 | 20 per 1000 | |||||
| High | ||||||
| 124 per 1000 | 141 per 1000 | |||||
| Neonatal infection | Study population | Not estimable | 458 | see comment | The outcome was reported with no events. | |
| See comment | See comment | |||||
| Moderate | ||||||
| Wound infection | Study population | RR 1.47 | 458 | ⊕⊕⊝⊝ | ||
| 70 per 1000 | 103 per 1000 | |||||
| Moderate | ||||||
| 70 per 1000 | 103 per 1000 | |||||
| Maternal satisfaction | The mean maternal satisfaction in the control groups was | The mean maternal satisfaction in the intervention groups was | MD 0.00 (‐0.13, 0.13) | 458 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most studies contributing data had serious design limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postpartum maternal febrile morbidity Show forest plot | 3 | 997 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.73, 1.76] |
| 2 Colonisation Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Gram‐positive | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.82, 1.64] |
| 2.2 Gram‐negative | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.70, 0.98] |
| 3 Neonatal infection Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Wound infection Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.80, 2.70] |
| 5 Wound dehiscence Show forest plot | 1 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.00] |
| 6 Need for wound resuturing | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Discomfort | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Pain | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Maternal embarrassment | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Maternal satisfaction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Maternal satisfaction continuous data Show forest plot | 1 | 458 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |

