Interventions for preventing and treating pelvic and back pain in pregnancy
Información
- DOI:
- https://doi.org/10.1002/14651858.CD001139.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 01 agosto 2013see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
For the 2013 update, Victoria Pennick (VEP) and Dianne Liddle (SDL) selected and assessed the risk of bias of the articles and extracted and analysed the data. They both contributed to the writing of the review. Gavin Young remained available to assist as necessary, but was not involved in the actual production of this review.
For the 2007 update: Victoria Pennick (VEP) and Gavin Young (GY) selected and assessed the methodological quality of the articles and extracted and analysed the data. VEP wrote the first draft of the review; GY reviewed and offered his comments.
For the original review and 2002 update: both review authors, GY and David Jewell, assessed all articles and contributed to the analyses. GY entered the data and wrote the text.
Sources of support
Internal sources
-
Institute for Work and Health, Canada.
External sources
-
Royal College of General Practitioners, UK.
Declarations of interest
None known.
Acknowledgements
The authors would like to thank the Scientific Foundation Board of the Royal College of General Practitioners for the grant which made the 2002 updating of this review possible. Gavin Young would like to thank Paul Shekelle of the Cochrane Back Review Group for helping with the 2002 analyses and Victoria Pennick would like to thank Andrea Furlan for her helpful comments and help with translation in the 2007 version.
We would like to acknowledge the contributions made by David Jewell to the first two versions of this review and Gavin Young for his contributions to the first three versions. We were able to exclude trials and include data from non‐English trials due to the gracious assistance of Andrea Furlan, Ivan Steenstra, Jacob Etches, Ayako Kitta, Reza Yousefi‐Nooraie and Tomasz Kotwicki. Thanks also to Kelly An who helped with 'Risk of bias' assessment and data extraction, and Lynn Hampson and Rachel Couban who helped identify and obtain copies of the studies.
A special thank you goes to Stephanie McKeown whose encouragement and support made it possible for Dianne Liddle to participate in this review.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Pregnancy and Childbirth Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Sep 30 | Interventions for preventing and treating low‐back and pelvic pain during pregnancy | Review | Sarah D Liddle, Victoria Pennick | |
| 2013 Aug 01 | Interventions for preventing and treating pelvic and back pain in pregnancy | Review | Victoria Pennick, Sarah D Liddle | |
| 2007 Apr 18 | Interventions for preventing and treating pelvic and back pain in pregnancy | Review | Victoria Pennick, Gavin Young | |
| 2002 Jan 21 | Interventions for preventing and treating pelvic and back pain in pregnancy | Review | Gavin Young, David Jewell | |
Differences between protocol and review
The protocol was originally written in the 1990s. The methodology for conducting Cochrane reviews has changed substantially since then; this update reflects those changes.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Acupuncture Therapy;
- Back Pain [prevention & control, *therapy];
- Braces;
- *Exercise Therapy;
- Low Back Pain [prevention & control, therapy];
- Manipulation, Osteopathic;
- Pelvic Pain [prevention & control, *therapy];
- Pregnancy Complications [prevention & control, *therapy];
- Randomized Controlled Trials as Topic;
- Sick Leave [statistics & numerical data];
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICO

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
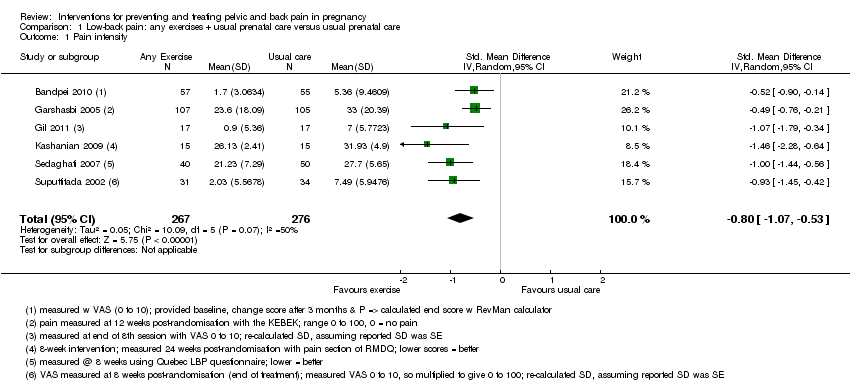
Comparison 1 Low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 1 Pain intensity.

Comparison 1 Low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 2 Disability.

Comparison 2 Low‐back pain: water gymnastics + usual prenatal care versus usual prenatal care, Outcome 1 Number of women taking sick leave because of back pain after 32 weeks' gestation.

Comparison 3 Low‐back pain: support belts, Outcome 1 Low‐back pain, measured with VAS; 0 to 10; 0 = no pain.
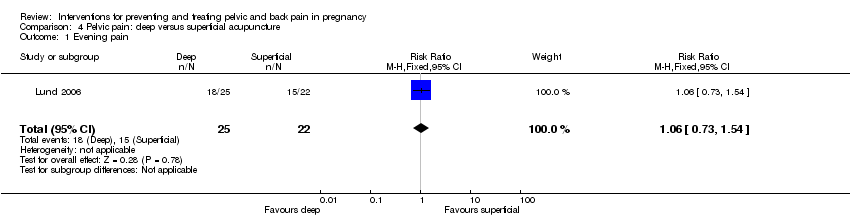
Comparison 4 Pelvic pain: deep versus superficial acupuncture, Outcome 1 Evening pain.

Comparison 5 Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 1 Women who reported pain on Visual Analogue Scale.
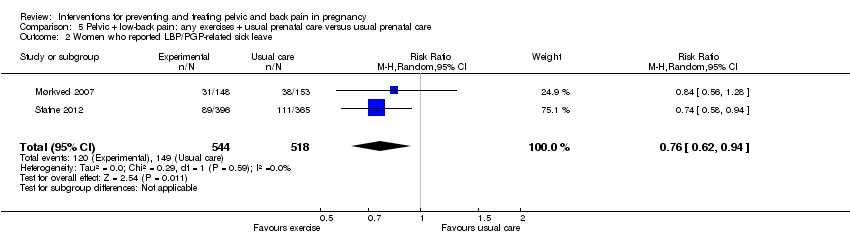
Comparison 5 Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care, Outcome 2 Women who reported LBP/PGP‐related sick leave.

Comparison 6 Pelvic + low‐back pain: acupuncture + usual prenatal care versus usual prenatal care, Outcome 1 Number of women who reported decreased pain.
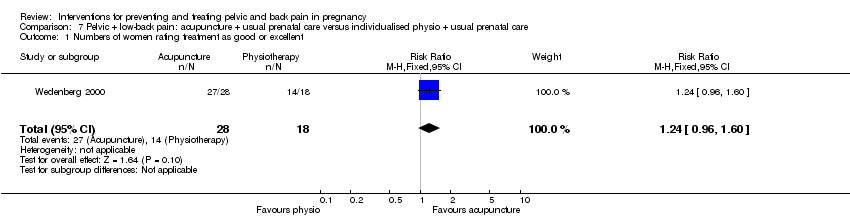
Comparison 7 Pelvic + low‐back pain: acupuncture + usual prenatal care versus individualised physio + usual prenatal care, Outcome 1 Numbers of women rating treatment as good or excellent.
| Low‐back pain: any exercises + usual prenatal care versus usual prenatal care for treating back pain in pregnancy | ||||||
| Patient or population: pregnant women with back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Low‐back pain: any exercises + usual prenatal care versus usual prenatal care | |||||
| Pain intensity measured by a number of different measurements; lower score = better | The mean pain intensity in the control groups was18.75 | The mean pain intensity in the intervention groups was | SMD ‐0.80 (‐1.07, ‐0.53) | 543 | ⊕⊕⊝⊝ | |
| Disability measured by Roland Morris Disability Questionnaire and Oswestry Disability Index | The mean disability in the control groups was 26.6 | The mean disability in the intervention groups was | SMD ‐0.56 (‐0.89 to ‐0.23) | 146 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 poor or no description of randomisation process, allocation concealment, blinding of research personnel | ||||||
| Low‐back pain: water gymnastics + usual prenatal care versus usual prenatal care for treating back pain in pregnancy | ||||||
| Patient or population: pregnant women with back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (usual care) | water gymnastics | |||||
| Number of women taking sick leave because of back pain after 32 weeks' gestation | Study population | RR 0.4 | 241 | ⊕⊕⊝⊝ | ||
| 144 per 1000 | 58 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 unclear methods of randomisation; research personnel not blinded | ||||||
| Low‐back pain: support belts for preventing and treating pelvic and back pain in pregnancy | ||||||
| Patient or population: pregnant women with back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Low‐back pain: support belts | |||||
| BellyBra versus Tubigrip ‐ Low‐back Pain | The mean Bellybra versus Tubigrip back pain in the control group was 4.7, measured on VAS 0 to 10 | The mean Bellybra versus Tubigrip ‐ back pain in the intervention group was 0.2 lower (1.19 lower to 0.79 higher) | MD ‐0.20 (95% CI ‐1.19 to 0.79) | 94 | ⊕⊕⊝⊝ | |
| BellyBra versus Tubigrip ‐ ADL | The mean Bellybra versus Tubigrip ability to perform activities of daily living in the control group was 5.6, measured as a total of several activities | The mean Bellybra versus Tubigrip ability to perform activities of daily living in the intervention group was 0.9 lower | MD ‐0.90 (95% CI ‐1.81 to 0.01) | 94 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 no blinding of research personnel described; no explanation provided for lost‐to‐follow‐up data; different co‐interventions and compliance between groups | ||||||
| Pelvic pain: deep versus superficial acupuncture for preventing and treating pelvic and back pain in pregnancy | ||||||
| Patient or population: pregnant women with pelvic pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (superficial) | Intervention (deep) | |||||
| evening pain, reported as better, based on women's report on Visual Analogue Scale | Study population | RR 1.06 | 47 | ⊕⊕⊝⊝ | ||
| 682 per 1000 | 723 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 randomisation process and attrition rate/explanations not described | ||||||
| Pelvic + low‐back pain: any exercises + usual prenatal care versus usual prenatal care for preventing and treating pelvic and back pain in pregnancy | ||||||
| Patient or population: pregnant women with, or at risk of developing, pelvic and back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (usual prenatal care) | Any exercises + usual prenatal care | |||||
| Number of women who reported pain on Visual Analogue Scale | Study population | RR 0.85 | 1344 | ⊕⊕⊕⊝ | ||
| 747 per 1000 | 635 per 1000 | |||||
| Number of women who reported LBP/PGP‐related sick leave | Study population | RR 0.76 | 1062 (2 studies) | ⊕⊕⊕⊝ | ||
| 288 per 1000 | 219 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 there was a mix of potential biases among the four studies: no allocation concealment (1); no blinding of research personnel (all); poor/no description of drop‐outs, co‐interventions and baseline inequality (mixed) | ||||||
| Pelvic + low‐back pain: acupuncture + usual prenatal care versus usual prenatal care for preventing and treating pelvic and back pain in pregnancy | ||||||
| Patient or population: pregnant women with, or at risk of developing, pelvic and back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Pelvic + low‐back pain: acupuncture + usual prenatal care versus usual prenatal care | |||||
| Number of women who reported decreased pain | Study population | RR 4.16 | 72 | ⊕⊕⊝⊝ | ||
| 143 per 1000 | 594 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 no blinding of research personnel, over 20% attrition, different co‐interventions | ||||||
| Pelvic + low‐back pain: acupuncture + usual prenatal care versus individualised physio + usual prenatal care for preventing and treating pelvic and back pain in pregnancy | ||||||
| Patient or population: pregnant women with, or at risk of developing, pelvic and back pain | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (individualised physio + usual prenatal care) | acupuncture + usual prenatal care | |||||
| Numbers of women rating treatment as good or excellent | Study population | RR 1.24 | 46 | ⊕⊕⊝⊝ | ||
| 778 per 1000 | 964 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 no description of randomisation process, no blinding of research personnel described, uneven attrition (12 dropped out of physio group, while none dropped out of the acupuncture group) and co‐interventions between groups | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 6 | 543 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.07, ‐0.53] |
| 2 Disability Show forest plot | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.89, ‐0.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women taking sick leave because of back pain after 32 weeks' gestation Show forest plot | 1 | 241 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.17, 0.92] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Low‐back pain, measured with VAS; 0 to 10; 0 = no pain Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Low‐back Pain | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.19, 0.79] |
| 1.2 ADL | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.81, 0.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Evening pain Show forest plot | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.73, 1.54] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Women who reported pain on Visual Analogue Scale Show forest plot | 4 | 1344 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.73, 1.00] |
| 2 Women who reported LBP/PGP‐related sick leave Show forest plot | 2 | 1062 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.62, 0.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who reported decreased pain Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.16 [1.77, 9.78] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Numbers of women rating treatment as good or excellent Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.96, 1.60] |

