| Study | Participants | Procedure | Interventions | Outcomes | Metrics used | Results |
| Altun‐Koroglu 2010 | 75 full‐term infants | Heel lance | 3 mL of hind milk (N = 25) 3 mL of 12.5% sucrose solution (N = 25) 3 mL of distilled water (N = 25) | NFCS, crying time, duration of crying, HR | Median and IQR | Median crying time, duration of first cry and tachycardia, and time needed to return to baseline = longest in the distilled water group. Significantly shorter in the hind milk group when compared to distilled water group (P = 0.022, P = 0.008, P 0.009 and P = 0.038, respectively) No statistically significant differences observed between the hind milk and sucrose group Maximum HR in hind milk group was significantly lower than distilled water group (184 bpm vs. 196 bpm, P = 0.031) Significant reduction in average NFCS score. 1st minute NFCS score and 5th minute NFCS score in the hind milk group compared to the distilled water group (P = 0.006, P = 0.017 and P = 0.021, respectively) |
| Blass 1997 | 72 infants, 22 to 40 h old | Heel lance | 2 mL of either of the following solutions: water 12% sucrose protein mixture 7% lactose dilute fat (coconut and soy oil) concentrated fat fat and lactose mixture RSF (water, protein, lactose, fat) milk N = 8 for all groups | Crying time (%) during blood collection and 1, 2 and 3 min after heel lance Mean % of crying time per min at 1, 2 and 3 min after heel lance (recovery period) | Mean proportions Graphically reported | Significantly less crying time during blood collection in the sucrose group (47%) compared to the water group (92%, P = 0.015) |
| Blass 1999 | 40 term newborn infants, 34 to 55 h old | Heel lance | 2 mL of 12% sucrose over 2 min via syringe (N = 10) 2 mL of water via syringe over 2 min (N = 10) Pacifier dipped every 30 s in 12% sucrose solution for 2 min (N = 10) Pacifier dipped in water every 30 s for 2 min (N = 10) prior to heel lance | % time crying 3 min after heel lance Mean change in HR % time grimacing | Mean percentage Mean change (bpm) Mean percentage | 2 mL of 12% (0.24 g) sucrose alone diminished cry duration from heel lance compared to water (8% vs. 50%, P = 0.003) and water with pacifier (8% vs. 35%, P = 0.002). Pacifier with 12% sucrose more effective in reducing cry duration compared to water with pacifier (5% vs. 35%, P = 0.001) or water alone (50%, P = 0.002) Mean HR increased significantly from treatment to heel lance in infants receiving water alone (mean increase of 17 bpm, P = 0.002) and water with pacifier (mean increase of 20 bpm, P = 0.005). Mean increase in HR also increased for the 2 mL of 12% (0.24 g) sucrose and pacifier group (mean difference of 7.4 bpm, P = 0.05) but not for infants receiving 2 mL of 12% (0.24 g) sucrose alone (mean difference of 5.9 bpm, P = 0.142) 2 mL of 12% (0.24 g) sucrose reduced grimacing compared to water (P = 0.0003). 12% (0.24 g) sucrose with pacifier reduced grimacing compared to water (P = 0.001) and pacifier alone (P = 0.04) |
| Bucher 1995 | 16 preterm infants, 27 to 34 weeks' GA, postnatal age approximately 42 days | Heel lance | 2 mL of 50% sucrose via syringe into the mouth 2 min before heel lance 2 mL of distilled water via syringe into the mouth 2 min before heel lance (N = 16, cross‐over design) | % time crying Recovery time until crying stopped Increase in HR Recovery time for HR TcpO2 (max increase ‐ kPa); TcpO2 (max decrease ‐ kPa); TcpO2 (difference between baseline and 10 min after end of intervention ‐ kPa); TcpCO2 (max decrease ‐ kPa); TcpCO2 (difference between baseline and 10 min after the end of intervention), recovery time for respirations | Not reported Median, IQR Median, IQR | Cry duration (% of total duration of intervention) significantly reduced in 2 mL of 50% (1.0 g) sucrose group (71.5%) compared to control group (93.5%, P = 0.002) Median increase in HR (bpm) after heel lance were significantly reduced in the 2 mL of 50% (1.0 g) of sucrose group (35 bpm) compared to water (51 bpm), P = 0.005 No significant differences between groups with respect to measures for TcpO2 (P = 0.05) and TcpCO2 (P = 0.21) |
| Codipietro 2008 | 101 term infants, 39.3 to 39.4 weeks GA | Heel lance | Breastfeeding prior to heel lance (N = 51) 1 mL 25% sucrose via syringe (N = 50) | Duration of first cry, % crying time in first 2 min, and % crying time during blood sampling HR increase from baselines at 30 s following commencement of procedure SpO2 decrease PIPP during blood sampling, 2 min after heel lance | Median, range | Median duration of first cry: breastfeeding group (3 (0 to 12)) compared to sucrose (21 (0 to 120)), P = 0.004 % crying during first 2 min: breastfeeding group (4 (0 to 100) compared to sucrose (45 (0 to 100) (P < 0.001) % crying during sampling: breastfeeding group (8 (0 to 100) compared to sucrose (56.5 (0 to 100) (P = 0.0003) Median increase in HR from baseline to 30 s after start of heel lance was significantly lower in breastfeeding group (13 (‐12 to 54)) compared to sucrose group (22 (‐32 to 65)) (P = 0.005) Median decrease in SpO2 from baseline to 30 s after start of heel lance was significantly greater in sucrose group (‐3 (‐30 to 1)) compared to breastfeeding group (‐1 (‐14 to 2)) (P= 0.001) Median PIPP scores significantly lower in breastfeeding group (3.0) compared to sucrose group (8.5) (P < 0.0001) |
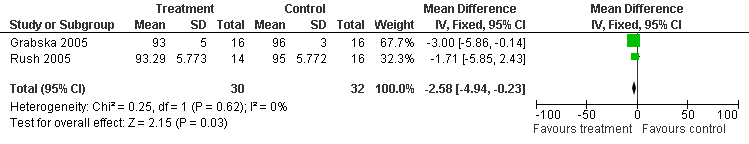
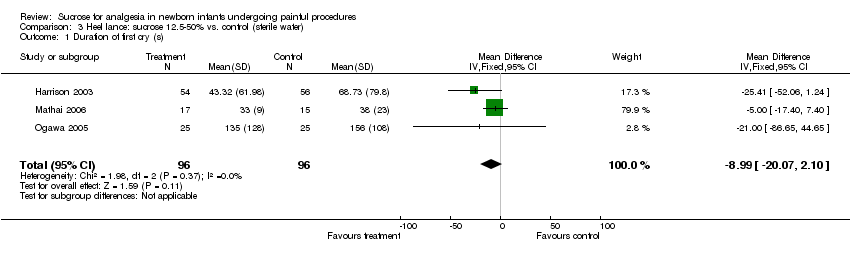
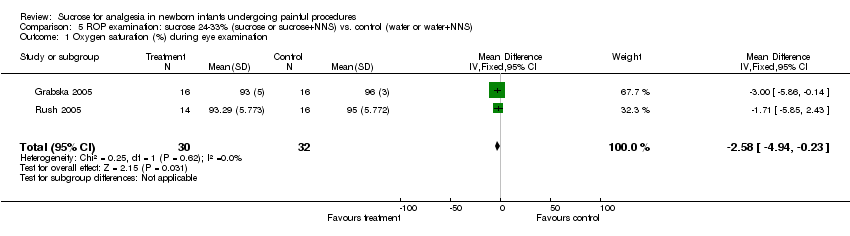
| Gibbins 2002 | 190 preterm and term infants, mean GA of 33.7 weeks, < 7 days postnatal age | Heel lance | 0.5 mL of 24% sucrose via syringe to the anterior surface of the tongue followed by pacifier (N = 64)
0.5 mL 24% sucrose without pacifier (N = 62)
0.5 mL sterile water with pacifier (N = 64)
2 min prior to heel lance | PIPP scores at 30 and 60 s after heel lance | Reported means, SD | Statistically significant difference in mean PIPP scores at both 30 s (F = 8.23, P < 0.001) and 60 s (F = 8.49, P < 0.001) after heel lance in favour of 0.5 mL of 24% (0.12 g) sucrose group and 0.5 mL of 24% (0.12 g) sucrose with pacifier group. Post‐hoc Tukey tests showed infants who received sucrose and pacifier had significantly lower PIPP scores after heel lance at 30 s (mean 8.16, SD 3.24) compared to infants receiving sucrose alone (mean 9.77, SD 3.04, P = 0.007) and water with pacifier (mean 10.19, SD 2.67, P < 0.001). At 60 s after heel lance, PIPP scores were significantly lower for 0.5 mL of 24% (0.12 g) sucrose with pacifier group (mean 8.78, SD 4.03) compared to the 0.5 mL of 24% (0.12 g) sucrose alone group (mean 11.20, SD 3.25, P = 0.005) and water with pacifier group (mean 11.20, SD 3.47, P = 0.007). No significant differences in PIPP scores found between 0.5 mL of 24% (0.12 g) sucrose alone group or water with pacifier group at both follow‐up times |
| Gormally 2001 | 94 term newborns, mean GA 39.4 weeks on 2nd or 3rd day of life | Heel lance | No holding and sterile water given by pipette (N = 21) No holding and 0.250 mL of 24% sucrose solution given by pipette (N = 22) Holding and sterile water given by pipette (N = 20) Holding and 0.250 mL of 24% sucrose solution by pipette (N = 22) All solutions given 3 times at 30‐s intervals | % time crying 1, 2, 3 min after heel lance Mean HR before intervention, 1, 2, 3 min after heel lance, mean vagal tone index before intervention, 1, 2, 3 min after heel lance Pain concatenation scores for facial activity before intervention, 1, 2, 3 min after heel lance | Not reported | Crying decreased over time (F(2,80) = 10.0, P < 0.001) but no significant interaction noted for time with holding, taste or holding and taste. Effect of taste on crying was significant (F(1,81) = 4.1, P < 0.05) in favour of 0.25 mL of 24% (0.18 g) sucrose. Effect of holding not statistically significant (F(1,81) = 3.0, P = 0.09)). No statistically significant interaction between taste and holding to reduce crying (F(1,81) = 0.80, P = 0.37). Effect of combined interventions was additive Although no significant differences in mean HR due to holding or sucrose as main effects, there was significant interaction between holding and taste (F(1,61) = 8.89, P < 0.004), indicating synergistic effect that was also dependent on pre‐intervention HR (F(1,61) = 9.23, P < 0.004). No significant main effects noted for vagal tone; as with HR, effect of vagal tone was dependent on pre‐intervention vagal tone for both holding and taste interventions (F(1,60) = 4.82, P < 0.03). Pre‐intervention levels interacted to decrease HR and vagal tone in infants who had higher rates before interventions Pain concatenation scores measuring facial expressions of pain decreased over time (F(1,65) = 28.5, P < 0.001). Only the effect of holding reduced pain scores (F(1,65) = 5.6, P <0.02). No difference as to whether infant received sucrose (taste main effect F(1,65) 0.17, P = 0.68 |
| Greenberg 2002 | 84 term newborns, approximately 17 to 19 h old | Heel lance | Sugar‐coated pacifier (N = 21) water‐moistened pacifier (N = 21) 2 mL of 12% sucrose (n =21) routine care (N = 21) | Duration of cry from procedure phase to 3 min post‐procedure Vagal tone and vagal tone index Salivary cortisol levels | Not reported | Significant decrease in duration of cry for the sugar‐coated pacifier group compared to the control group (P = 0.001) and the water‐moistened pacifier group (P = 0.001). Lower vagal tone during heel lance in the sugar‐coated pacifier group compared to the control group (P = 0.008) and oral sucrose group (P = 0.018). Lower vagal tone index in the sugar‐coated pacifier group compared to control group at heel lance (P = 0.019), and 6 to 10 min after (P = 0.007) and 11 to 15 min (P = 0.049) after heel lance No significant differences were found in salivary cortisol levels across groups (no P value reported). |
| Guala 2001 | 140 term, 38 to 41 weeks' GA | Heel lance | Nothing (N = 20) Water (N = 20) 5% Glucose (N = 20) 33% Glucose (N = 20 50% Glucose (N = 20) 33% Sucrose (N = 20) 50% Sucrose (N = 20) | HR before, during and 3 min after heel lance | Mean, SD | No significant differences were found between groups for differences in HR at each of the 3 phases of the heel lance (P value reported for 3 min after heel lance, P = 0.087; the difference between 3 min after heel lance and during heel lance, P = 0.068) |
| Haouari 1995 | 60 term infants, 37 to 42 weeks' gestation, 1 to 6 days of age | Heel lance | 2 mL of 12.5% sucrose 2 min prior to heel lance (N = 15) 2 mL of 25% sucrose 2 min prior to heel lance (N = 15) 2 mL of 50 % sucrose 2 min prior to heel lance (N = 15) 2 mL of sterile water 2 min prior to heel lance (N = 15) All solutions were given by syringe on the tongue over < 1 min | Total time crying over 3 min. Time of first cry after lance % change in HR at 1, 3, 5 min after heel lance | Median, IQR Reported Means and SEM | After heel lance, significant decreases in total crying time and duration of first cry in 2 mL of 50% (1.0 g) sucrose group compared with water (P = 0.02). Significant reduction in median time crying at end of first minute (P < 0.02) in 2 mL of 50% (1.0 g) sucrose group (35 s; range 14 to 60) compared with water (60 s; range 50 to 60). In second minute, duration of cry was significantly less in 2 mL of 50% (1.0 g) sucrose group (0 s; range 0 to 25) and in 2 mL of 25% (0.5 g) sucrose group (18 s; range 0 to 55) compared to water (60 s; range 40 to 60), P = 0.003 and P = 0.02, respectively Significant decrease in % change in HR 3 min after heel lancing (P = 0.02) in the 2 mL of 50% (1.0 g) sucrose group (mean 0.1%, SEM 3.3) compared to water group (mean 17.5%, SEM 6.0) |
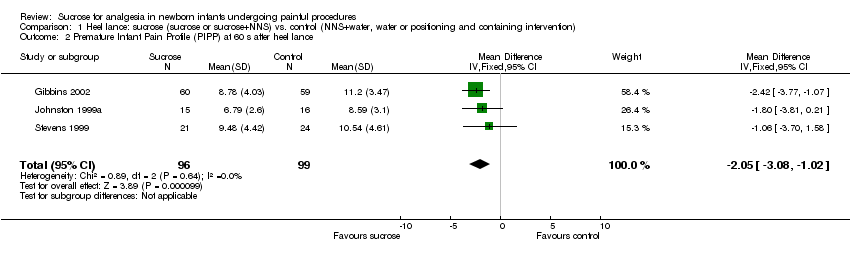
| Harrison 2003 | 99 sick hospitalised infants, mean (SD) gestation age 36.7 weeks (3.3) (treatment), 36.8 weeks (3.7) (control) (author provided data on a subset of infants from a larger study (N = 128) that fulfilled our inclusion criteria) | Heel lance | 1 mL of water (N = 46) 1 mL of 25% sucrose (N = 53) For infants weighing ≤ 1500 g the dose was reduced to 0.5 mL | Duration of cry until 5 second pause, incidence and duration of crying time during the heel lance and squeeze and during the 3‐minute recovery period HR at baseline, heel lance, during heel lance and 1, 2, 3 min post heel lance SpO2 at baseline, heel lance, during heel lance and 1, 2, 3 min post heel lance 4‐point subset of the NFCS (brow bulge, eye squeeze, nasolabial furrow, stretch mouth) at heel lance, during heel lance and 1, 2, 3 min post heel lance | Mean, SD (collected from authors) | Mean length of first cry was higher in the water group (70.5 (83.6)) compared to the sucrose group (46.8 (63.1)). The sucrose group cried 57.1% of the procedure time compared to 58.8% in the water group. The mean total duration of cry during the heel lance was 84.7 s (68.8) in the sucrose group and 87.4 s (87.1) in the water group. The mean (SD) HR upon heel lance was 163.0 (17.9) bpm in the sucrose group and 159.5 (19.2) bpm in the water group. HR at 30 s from the beginning of the procedure was 175.4 (22.2) and 172.8 (23.6) bpm in the sucrose and water groups, respectively. The HR in both groups decreased after the procedure to 152.1 (22.5) bpm in the sucrose group and 154.2 (29.1) bpm in the water group 2 min post heel lance Results of SpO2 were similar between the 2 groups Mean facial scores were significantly reduced at heel lance (2.74 (1.8)) in the sucrose group compared to the water group (2.94 (1.6)) (P = 0.02) and at 1 min (P = 0.04) and 2 min (P = 0.046) post‐heel lance. No significant differences occurred at 3 min post heel lance |
| Isik 2000a | 113 healthy term newborns GAs 37 to 42 weeks, median post natal age 2 days, range 2 to 5 days | Heel lance | 2 mL of 30% sucrose (N = 28) 2 mL of 10% glucose (N = 29) 2 mL of 30% glucose (N = 28) 2 mL of distilled water (N = 28) syringed into the anterior third of the tongue for 1 and 2 min prior to heel lance | Mean cry time during 3 min after lance Mean maximum HR 3 min from heel lance Mean recovery time for HR % change in HR at 1, 2, 3 min after heel lance | Reported means, SD Reported means and SEM | Infants who received 2 mL of 30% (0.6 g) sucrose (mean crying time of 61 s) cried significantly less than those who received 30% glucose (mean crying time of 95 s), 10% glucose (mean crying time of 103 s) or sterile water (mean crying time of 105 s)(P = 0.02) No significant difference between groups with respect to maximum HR after heel lance (P = 0.71), or mean recovery time (P = 0.09). No significant difference found in % change in HR at 1 or 3 min after heel lance (P = 0.14, P = 0.53, respectively). At 2 min after heel lance, % change in HR favoured group receiving sucrose (P = 0.05) compared to other groups |
| Johnston 1997a | 85 preterm infants, 25 ‐ 34 weeks' GA, 2 to 10 days of age | Heel lance | 0.05 mL of 24% sucrose via syringe into the mouth just prior to heel lance (N = 27)
0.05 mL of 24% sucrose via syringe into the mouth just prior to heel lance and simulated rocking 15 min prior to heel lance (N = 14)
0.05 mL of sterile water via syringe into the mouth just prior to heel lance and simulated rocking 15 min prior to heel lance (N = 24)
0.05 mL of sterile water via syringe into the mouth just prior to heel lance | HR at baseline and 3 x 30‐second blocks Behavioural facial actions (NFCS) at baseline and 3 x 30‐second blocks | Not reported | Although HR increased across all phases of procedure (F(3,59) = 2.94, P < 0.04), there was no significant differences noted between groups (F(3,59) = 0.682, P = 0.566) Decrease in % facial action in 0.05 mL of 24% (0.012 g) sucrose alone group and combined 0.05 mL of 24% (0.012 g) sucrose and rocking group compared to water group (F(6, 150) = 2.765, P < 0.02) |
| Johnston 1999a | 48 preterm neonates mean GA of 31 weeks, range 25 to 34 weeks, within 10 days of birth | Heel lance | 0.05 mL of 24% sucrose as a single dose, followed by 2 doses of sterile water (N = 15)
3 doses of 0.05 mL of 24% sucrose (N = 17)
3 doses of 0.05 mL of sterile water (N = 16)
given by syringe to anterior surface of the tongue at:
2 min prior to heel lance,
just prior to lancing and
2 min after lancing | PIPP scores in 5 x 30 second blocks | Reported means, SD | Statistically significant difference between groups (F = 9.143, P < 0.0001) for mean PIPP scores. Post‐hoc analysis found significantly lower PIPP scores with repeated doses of 0.05 mL of 24% (0.012 g) sucrose compared to placebo groups across all blocks of time, P < 0.05. PIPP scores for repeated doses of 0.05 mL of 24% (0.012 g) sucrose were significantly lower compared to single doses of 0.05 mL of 24% (0.012 g) sucrose (8.25 vs. 6.25) only at last block of time, P < 0.05. PIPP scores for single doses of 0.05 mL of 24% (0.012 g) sucrose compared to placebo showed trend towards statistical significance in favour of 0.05 mL of 24% (0.012 g) sucrose (F = 3.465, P = 0.07) |
| Mathai 2006 | 104 term neonates, postnatal age > 24 h, sucrose group mean postnatal age 48 h, distilled water groups mean postnatal age 44 h | Heel lance | 2 mL 20% sucrose instilled into mouth via a dropper (N = 17) 2 mL distilled water instilled into mouth via a dropper (N = 15) Rocking (N = 17) Massage (N = 17) Expressed breast milk (N = 18) NNS (N = 18) | Time of first cry in seconds, total cry in seconds HR before heel lance, 2 min after heel lance and 4 min after heel lance SpO2 before heel lance, 2 min after heel lance and 4 min after heel lance DAN scale before the heel lance and 30 s, 1 min, 2 min, 4 min after heel lance | Reported means, SD Not reported Mean, SD | No significant difference between sucrose group and any other group for time of first cry NNS and rocking significantly reduced total duration of cry, P < 0.05 No significant difference in HR between the groups at any time point No significant difference in SpO2 between the groups at any time point Significantly reduced DAN scores at 30 s after the heel lance for the sucrose group (mean 7.6, SD 14, P < 0.05); however, this was not sustained at 1, 2 and 4 min NNS and rocking significantly decreased the DAN scores at 2 and 4 min post heel lance, P < 0.05 |
| Okan 2007 | 31 healthy preterm newborns, mean GA 30.5 weeks, mean postmenstrual age 32.3 weeks | Heel lance | 2 mL of 20% sucrose 2 mL of 20% glucose 2 mL of water Infants received all 3 interventions at different times | Duration of first cry and total crying time HR at baseline, during heel lance and 1, 2, 3, 4 and 5 min post heel lance SpO2 and respiratory rate at baseline, during heel lance and 1, 2, 3, 4 and 5 min after heel lance NFCS scores during heel lance and 1, 2, 3, 4 and 5 min post heel lance | Mean, SD | Significantly increased duration of first cry and total crying time in the water group compared to the sucrose and glucose groups (P = 0.005 and P = 0.007, respectively). No significant differences in cry characteristics were observed between the sucrose and glucose groups Significantly higher HR in the water group (mean 175, SD 20.8) compared to the sucrose (mean 166, SD 17.6) and glucose groups (mean 165, SD 17.5) at 1 min following heel lance (P = 0.007). No significant differences between the sucrose and glucose groups Significantly higher NFCS score in the placebo group in the 4th minute following heel lance (mean 1.3, SD 2.0) and 5th minute following heel lance (mean 1.0, SD 1.0) compared to the sucrose (mean 0.5, SD 1.7; mean 0.3, SD 1.3, respectively) and glucose groups (mean 0.2, SD 0.5; mean 0.1, SD 0.3, respectively) (P = 0.009 at 4th minute and P = 0.049 at 5th minute. There were no significant differences between the sucrose and glucose groups |
| Ors 1999 | 102 healthy term infants, GA 37 to 42 weeks, median postnatal age 1.6 days, range 1 to 15 days | Heel lance | 2 mL of 25% sucrose (N = 35) 2 mL of human milk (N = 33) 2 mL of sterile water (N = 34) All solutions syringed onto anterior part of tongue for 1 min Heel prick performed 2 min after intervention | Median cry time during 3 min after lance % change HR 1, 2 and 3 min after heel lance | Median, IQR | Significant decrease in crying times for 2 mL of 25% (0.5 g) sucrose group (median 36, IQR 18 to 43) compared to human milk (median 62, IQR 29 to 107) and sterile water [(median 52, IQR 32 to 158) (P = 0.0009). Recovery time for crying was significantly reduced in 2 mL of 25% (0.5 g) sucrose group (median 72, IQR 48 to 116) compared to human milk (median 112, IQR 72 to 180) and sterile water (median 124, IQR 82 to 180) (P = 0.004) % change in HR after heel lance was significantly lower in the group receiving 2 mL of 25% (0.5 g) sucrose compared to groups receiving human milk and sterile water at 1, 2 and 3 min (P = 0.008, P = 0.01, P = 0.002, respectively) |
| Overgaard 1999 | 100 newborn term infants, mean age 6 days, range 4 to 9 | Heel lance | 2 mL of 50% sucrose solution via syringe into the mouth over 30 s 2 min prior to heel lance 2 mL of sterile water via syringe into the mouth over 30 s 2 min prior to heel lance | Median crying time during heel lance, fraction of crying during sampling, crying time during first minute after end of sampling, total crying time Change HR 0 and 1 min SpO2 at 0 and 1 min NIPS scores 1 min after heel lance and 1 min after blood sampling | Median, 5th and 95th percentiles | Median duration of first cry in group receiving 2 mL of 50% (1 g) sucrose was significantly lower (18 s (2 to 75)) compared to placebo group (22 s (11 to 143)) (P = 0.03). Median crying time during heel lance in the sucrose group was lower (26 s (2 to 183)) compared to placebo group (40 s (12 to 157)) (P = 0.07). Median fraction of crying during sampling in 2 mL of 50% (1 g) sucrose group was significantly lower (43% (4 to 100)) compared to placebo group (83% (20 to 100)) (P = 0.004). Median crying time during first minute after end of sampling in 2 mL of 50% (1 g) sucrose group was significantly lower (3 s (0 ‐ 58)) compared to placebo group (16 s (0 to 59)) (P = 0.004). Median total time crying in 2 mL of 50% (1 g) sucrose group was significantly lower (30 s (2 to 217)) compared to placebo group (71 s (13 to 176)) (P = 0.007) No significant in HR differences between groups (P = 0.05) No significant differences between groups with respect to changes in SpO2 (P = 0.8) Median NIPS scores 1 min after heel lance were lower in 2 mL of 50% (1.0 g) sucrose group compared to placebo group (3 (0 to 7) and 6 (0 to 7), respectively; P = 0.04). Median NIPS scores 1 min after end of blood sampling were lower in 2 mL of 50% (1.0 g) sucrose group (0 (0 to 7)) compared to placebo group (2 (0 to 7)) (P = 0.05) |
| Ozdogan 2010 | 142 healthy term newborns | Heel lance | 6 groups Single‐dose breast milk Single‐dose sterile water Single‐dose 12.5% sucrose 2 doses breast milk 2 doses sterile water 2 doses 12.5% sucrose | Median crying time; NFCS | Medians | Significant difference between single‐dose sucrose vs. water (P = 0.002) in favour of sucrose. Double doses of sucrose were not superior to single doses; single doses or double doses of breast milk were not effective in reducing pain No significant differences between groups on crying time |
| Ramenghi 1996a | 15 preterm infants, 32 to 34 weeks' gestation, > 24 h of age | Heel lance | 1 mL of 25% sucrose
1 mL of sterile water | Duration of first cry and % time crying 5 min after lance HR (at ‐2, 0, 1, 3 and 5 min from heel lance) Behavioural scores (4 facial expressions and the presence of crying) ‐2, ‐1 , 0, 1, 2, 3 and 5 min Quality/intensity of sucking | Median, IQR Not reported Not reported | Significant decrease in total % of time crying over 5 min (median 6%, IQR 3.3 to 15.3) in the 1 mL of 25% (0.25 g) sucrose group compared with water group (median 16.6%, range 5 to 27.3) (P = 0.018). Duration of first cry was significantly decreased in the 1 mL of 25% (0.25 g) sucrose group (median 12 s, IQR 8 to 22) compared to control group (median 23 s, IQR 15 to 45) (P = 0.004) No significant differences in HR between groups, P value not reported Mean pain scores were significantly lower in the groups receiving 1 mL of 25% sucrose (0.25 g) of sucrose at both 1 and 3 min after heel lance (P = 0.01, P = 0.03, respectively) The clinical interpretation of the quality of sucking was significantly more intense in the 1 mL of 25% (0.25 g) sucrose group than in the water group (P = 0.04) |
| Ramenghi 1996b | 60 term infants, 37 to 42 weeks GA, 2‐ to 5‐day old | Heel lance | 2 mL of 25% (0.5 g) sucrose 2 mL of 50% (1.0 g) sucrose Calpol Single‐dose sterile water | Duration of first cry after lance, % time crying over 3 min after heel lance % change in HR over 5 min (at ‐2, 0, 1, 3 and 5 min from heel lance) Behavioural scores (4 facial expressions and the presence of crying) ‐2, ‐1, 0, 1, 2, 3 and 5 min | Median, IQR Not reported Median, IQR | Significant decrease in duration of first cry and % crying during 3 min after heel lance in the 2 mL of 25% (0.5 g) sucrose, 2 mL of 50% (1.0 g) sucrose and Calpol groups (P = 0.02) (data in graph form only) Significant increase in HR for 3 min after heel lance in water group compared with 2 mL of 50% (1.0 g) sucrose group and Calpol group (P = 0.009) Pain score (0 to 5) was significantly higher in water group (score = 2, range 1 to 5) than in other 3 groups: 2 mL of 50% (1 g) sucrose group (score = 0, range 0 to 3); 2 mL of 25% (0.5 g) sucrose group (score = 0, range 0 to 2); Calpol group (score = 0, range 0 to 1) (P = 0.05) |
| Ramenghi 1999 | 30 preterm infants, GA 32 to 36 weeks, postnatal age < 24 h | Heel lance | 25% sucrose solution (volume not reported) was given via syringe into the mouth or via NG tube 2 min prior to first heel lance (N = 15), and via the alternate route for the second heel lance within 48 h Sterile water via syringe into the mouth or via NG tube 2 min prior to first heel lance and for the second heel lance the alternate route within 48 h (cross‐over design, N = 30) | % cry over 5 min after sampling Behavioural scores (4 facial expressions and the presence of cry) at 1, 3 and 5 min after the lance for a total behavioural score | Median, IQR | Median % cry in intraoral water group was 22% (IQR 10.6 to 40) and 27% (IQR 11.6 to 47) for infants in NG tube water group. Median % cry in intraoral 25% sucrose group was 6% (IQR 0.6 to 15) and 18.3% (IQR 11.6 to 41.6) for NG tube 25% sucrose group. Significant reduction in crying time (P = 0.006) noted in the 25% sucrose group compared with water group when infants received 25% sucrose intraorally, not via NG‐tube route. For infants in 25% sucrose group, significant reduction in crying time noted (P = 0.008) when solution given intraorally compared to NG tube route Behavioural scores for the intraoral water group was 9 (IQR 6 to 12) and 10 (IQR 6 to 14) for NG tube water group. Behavioural scores for intraoral 25% sucrose group was 5 (IQR 3 to 6) and 9 (IQR 8 to 10) for NG tube sucrose group. Significant reduction in behavioural scores noted in 25% sucrose group (P = 0.002) compared with water group when infants received 25% sucrose intraorally but not via NG route. For infants in 25% sucrose group, there was significant reduction in behavioural score (P = 0.001) when solution was given intraorally compared to via NG tube |
| Rushforth 1993 | 52 term infants, 37 to 42 weeks, GA, 2 to 7 days of age | Heel lance | 2 mL of 7.5% sucrose administered by a dropper into the mouth over a 1‐minute period prior to heel lance (N = 26) 2 mL of sterile water administered by dropper into the mouth over a 1‐minute period prior to heel lance (N = 26) | % cry over 3 min after sampling | Median only | No significant differences in median % time crying between group receiving 2 mL of 7.5% (0.15 g) sucrose (74.3%) compared to group receiving water (73.2%). No significant differences between groups in duration of cry after 1 min (P = 0.65), 2 min (P = 0.52) and 3 min (P = 0.72). No difference in time to cessation of crying (P = 0.16) |
| Slater 2010 | 44 term infants, 37 to 43 GA, < 8 days old | Heel lance | 0.5 mL of 24% sucrose given via syringe (N = 20) 0.5 mL of sterile water (N = 24) | HR change, PIPP score, nociceptive‐specific brain activity, latency to change in facial expression (s), facial non‐responders, nociceptive reflex withdrawal activity | Mean, SD, mean weight | Only mean baseline HR given: 0.5 mL of 24% sucrose 132. 6 bpm (124.3 to 140.9); 0.5 mL of sterile water 131.8 (122.2 to 141.5) (P = 0.90) Only mean baseline SpO2 given: 0.5 mL of 24% sucrose 99.4 (98.8 to 100.1); 0.5 mL of sterile water 97.4 (95.0 to 99.8) (P = 0.13) PIPP score during insertion: baseline PIPP score: 0.5 mL of 24% sucrose 1.3 (0.8 to 1.7), 0.5 mL of sterile water 1.3 (0.8 to 1.8) (P = 0.13); PIPP during procedure: 0.5 mL of 24% sucrose 5.8 (3.7 to 7.8), 0.5 mL of sterile water 8.5 (7.3 to 9.8) (P = 0.02) No significant differences in nociceptive‐specific brain activity (P = 0.46) latency to change in facial expression (P = 0.86), mean nociceptive reflex withdrawal activity (P = 0,49) or mean latency to nociceptive reflex withdrawal activity (P = 0.56); significant difference in facial non‐responder (P < 0.0001). |
| Stevens 1999 | 122 neonates, 27 to 31 weeks' GA, < 28 days of age | Heel lance | Prone positioning 30 min prior to heel lance Pacifier dipped in sterile water and placed into the mouth 2 min prior to heel lance Pacifier dipped in 24% sucrose and placed into the mouth 2 min prior to heel lance Control: Containment in SnuggleUp device (N = 122) NB: all infants were contained in SnuggleUp device | PIPP scores at 30 and 60 s | Reported means, SD | Main effect of treatment for mean PIPP scores (F(16.20), P < 0.0001). Post‐hoc analysis revealed significant reduction in PIPP scores 30 s after heel lance in sucrose group (pacifier dipped in 24% sucrose ‐ estimated at 0.02 g), (mean 7.87, SD 3.35), compared to control group (mean 9.80, SD 3.55) (F(24.09), P < 0.0001). Statistically significant reduction in PIPP scores in pacifier and water group (mean 8.44, SD 3.55) compared to control group (mean 9.80, SD 3.55) (F(9.00), P = 0.003). Trend towards lower PIPP scores with sucrose and pacifier group compared to water and pacifier group (F(3.62), P < 0.05) |
| Stevens 2005 | 66 preterm infants, 26 to 30 weeks, postnatal age 72 h | Heel lance | Standard care‐positioning and swaddling (N = 21) Standard care‐positioning and swaddling and 0.1 mL sterile water via syringe into the mouth immediately followed by a pacifier 2 min prior to painful procedure (N = 23) Standard care‐positioning and swaddling and 0.1 mL 24% sucrose via syringe into the mouth immediately followed by a pacifier 2 min prior to painful procedure (N = 22) These interventions were given every time there was a painful procedure during the first 28 days of life | PIPP at day 7, 14, 21 and 28 at routine heel lance | Not reported | Significant main effect of group (P = 0.03) with differences occurring between the sucrose + pacifier group and standard care group (t(60) = ‐2.54; P = 0.01). Mean PIPP scores were generally higher in the standard care group No significant main effect of time Adverse effects: no group differences for adverse events, clinical outcomes or neurobiological risk status |
| Storm 2002 | 48 preterm, median GA of 32 weeks, median postnatal age of 14 days | Heel lance | 2 mL of 15% sucrose, N = 12
1 mL of 25% sucrose, N =12
Milk via NG tube N = 12
Milk via NG tube + 25% sucrose, N = 12
All infants were given water prior to a second heel lance | Differences in crying time for pre‐heel lance to heel lance procedure Changes in HR from pre‐heel lance to heel lance procedure Difference in skin conductance from pre‐heel lance to heel lance procedure | Not reported | Significantly less crying in infants receiving 1 mL of 25% sucrose (P < 0.05) and food (milk) + 1 mL of 25% sucrose (P < 0.05) No significant differences between groups in changes in HR from pre‐heel lance to heel lance procedure (P value not reported) No statistically significant smaller increase in skin conductance variables compared to their water control session (P value not reported) |
| Unceta‐Barranechea 2008 | 150 term infants | Heel lance | Facilitated tucking NNS + water NNS + 2 mL 24% sucrose | Mean crying time between groups Modified NFCS | Mean, SD | Statistically significant differences in crying time between control group and 2 intervention groups (P < 0.001). No significant difference between sucking with placebo and sucking with sucrose groups (P = 0.735). Statistically significant differences in pain score between control group and 2 intervention groups (P < 0.001). No significant difference between sucking with placebo and sucking with sucrose groups (P = 0.105) |
| Yilmaz 2011 | 120 infants GA 37 to 42 weeks Control group (N = 30): mean GA (SD) = 39.67 (0.80) Mother’s milk group (N = 30): mean GA (SD) = 39.10 (1.03) Sucrose group (N = 30): mean GA (SD) =39.10 (0.71) Pacifier group (N = 30): mean GA (SD) = 39.20 (0.93) | Heel lance | Control group: newborns were in their mothers’ lap; no interventions were made before the painful procedure Mother's milk group: 2 mL mother’s milk 2 min before the procedure by using a syringe with the needle removed and avoiding contact of the syringe with the mouth and lips Sucrose group: 2 mL sucrose of 20% by using a syringe 2 min before the procedure Pacifier group: given a pacifier | NIPS score, HR, respiratory rate, crying time | Mean, SD | No differences in HR and O2 saturation between groups After the procedure, the mean crying time of the sucrose group was shorter than those of the other groups. Comparing the crying times of the control and experimental groups according to the procedure time showed no statistically significant differences between the values for before and during the procedure (F = 1.50, P > 0.05); (F = 2.43, P > 0.05) Before the procedure, the lowest NIPS mean was in the sucrose group and the highest NIPS mean was in the pacifier group. During the procedure, no statistically significant differences were found between the groups for NIPS means (P > 0.05). After the procedure, the sucrose group showed the lowest response to pain, while the mother's milk group had the highest response. Comparing the NIPS means of the control and experimental groups according to the procedure times, statistically significant differences were found between the groups for values obtained before and after the procedure (F = 3.49, P < 0.05); (F = 6.71, P < 0.05) |