Monoterapia con lamotrigina versus carbamazepina para la epilepsia: una revisión de datos de participantes individuales
Información
- DOI:
- https://doi.org/10.1002/14651858.CD001031.pub4Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 28 junio 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Epilepsia
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
SJ Nevitt assessed studies for inclusion in the review update, obtained individual participant data from trial investigators for the review update, assessed risk of bias in all included studies, performed analyses in Stata version 14, added survival plots and a 'Summary of findings' table, and updated the text of the review.
C Tudur Smith provided statistical supervision and was involved with data analysis in the original review.
AG Marson independently assessed studies for inclusion, obtained individual participant data from trial investigators, provided guidance with the clinical interpretation of results, assessed eligibility and methodological quality of individual studies, and co‐wrote the original review.
J Weston independently assessed risk of bias in all included studies.
Sources of support
Internal sources
-
University of Liverpool, UK.
External sources
-
National Institute for Health Research (NIHR), UK.
Declarations of interest
SJ Nevitt: none known.
J Weston: none known.
AG Marson was Chief Investigator of SANAD A 2007. A consortium of pharmaceutical companies (GSK, EISAI, UCB Pharma) funded the National Audit of Seizure Management in Hospitals (NASH) through grants paid to the University of Liverpool. Professor Tony Marson is part funded by National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care North West Coast (NIHR CLAHRC NWC).
C Tudur Smith was involved in the statistical analysis of SANAD A 2007.
Acknowledgements
This review update was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Epilepsy Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS of the Department of Health.
We are greatly indebted to all of the original trialists that provided individual participant data and input into this review.
We are grateful to the Cochrane Epilepsy Group Information Specialist, Graham Chan, for performing all electronic searches.
We would like to thank Sarah White for her input into the original protocol, and to Carrol Gamble and Paula Williamson for contributions to the original review.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Jun 28 | Lamotrigine versus carbamazepine monotherapy for epilepsy: an individual participant data review | Review | Sarah J Nevitt, Catrin Tudur Smith, Jennifer Weston, Anthony G Marson | |
| 2016 Nov 14 | Lamotrigine versus carbamazepine monotherapy for epilepsy: an individual participant data review | Review | Sarah J Nevitt, Catrin Tudur Smith, Jennifer Weston, Anthony G Marson | |
| 2006 Jan 25 | Lamotrigine versus carbamazepine monotherapy for epilepsy | Review | Carrol L Gamble, Paula R Williamson, Anthony G Marson | |
| 2002 Oct 21 | Lamotrigine versus carbamazepine monotherapy for epilepsy | Protocol | Carrol L Preston, A G Marson, Paula R Williamson, Tony G Marson | |
Differences between protocol and review
For the 2018 update, 'Time to withdrawal of allocated treatment' was re‐defined as 'Time to treatment failure' due to feedback received from the Cochrane Editorial Unit regarding potential confusion regarding 'withdrawal' as a positive or negative outcome of anti‐epileptic monotherapy.
Additional analyses of 'Time to treatment failure' (due to lack of efficacy and due to adverse events) following feedback on published anti‐epileptic drug monotherapy reviews that these sub‐outcomes would be useful for clinical practice.
The term 'partial' has been replaced by 'focal', in accordance with the most recent classification of epilepsies of the International League Against Epilepsy (Scheffer 2017).
For the 2016 update, in a posthoc change, 'Summary of findings' tables were added to the review
December 2014: the title was changed to specify that the review uses individual participant data.
Notes
Sarah J Nolan (lead author of the 2016 update) is now Sarah J Nevitt.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Anticonvulsants [adverse effects, *therapeutic use];
- Carbamazepine [adverse effects, *therapeutic use];
- Epilepsies, Partial [*drug therapy];
- Epilepsy, Generalized [drug therapy];
- Epilepsy, Tonic‐Clonic [*drug therapy];
- Lamotrigine;
- Randomized Controlled Trials as Topic;
- Recurrence;
- Time Factors;
- Treatment Failure;
- Triazines [*therapeutic use];
- Withholding Treatment;
Medical Subject Headings Check Words
Adult; Child; Humans;
PICO
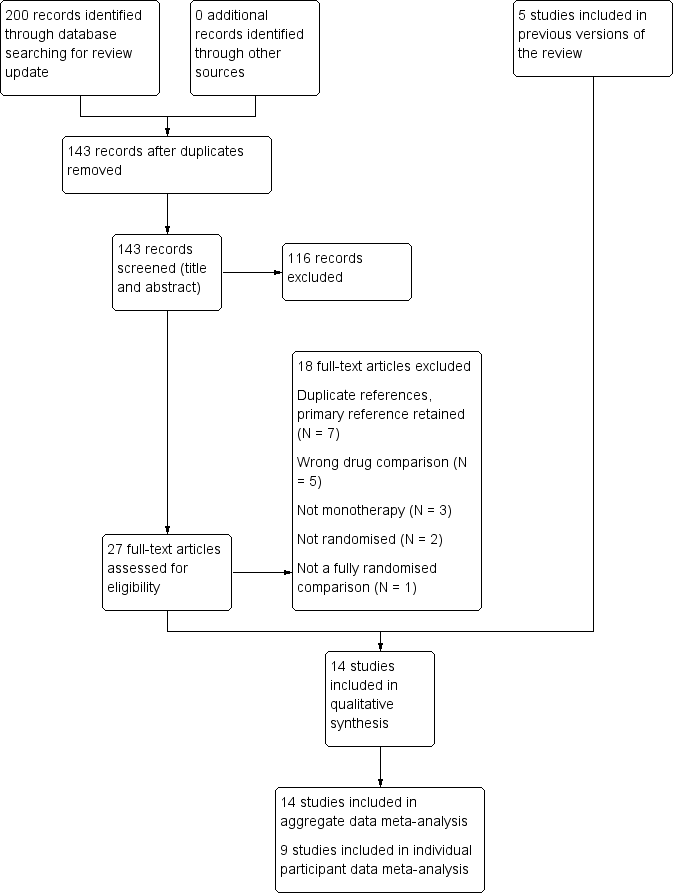
Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
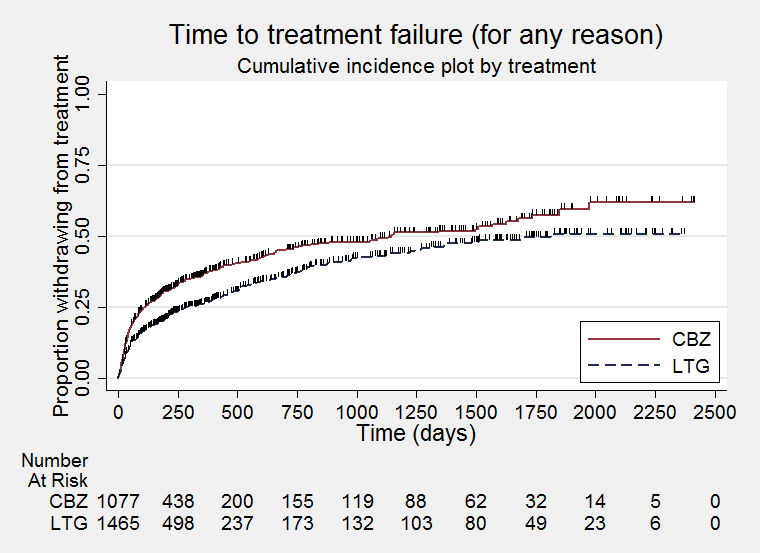
Time to treatment failure for any reason related to treatment (CBZ: Carbamazepine; LTG: Lamotrigine)

Time to treatment failure due to adverse effects (CBZ: Carbamazepine; LTG: Lamotrigine)

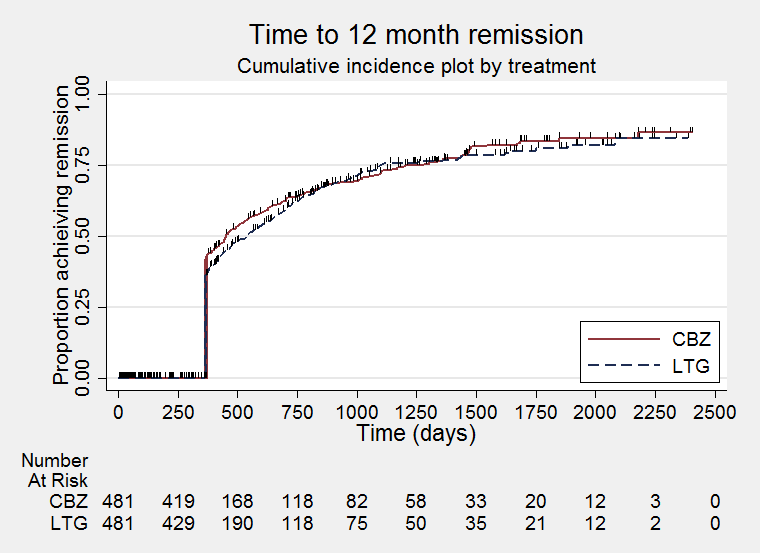
Time to treatment failure due to lack of efficacy (CBZ: Carbamazepine; LTG: Lamotrigine)

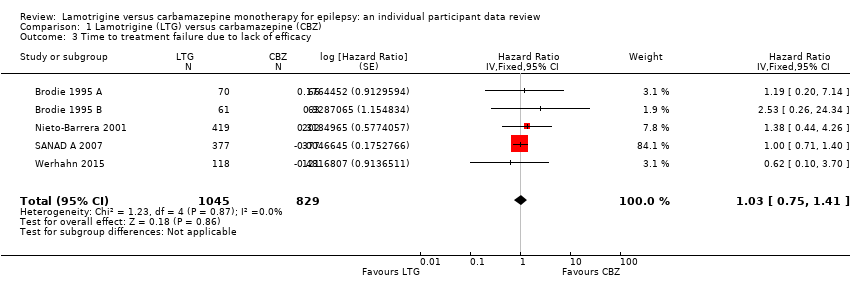
Time to treatment failure for any reason related to treatment ‐ by seizure type (CBZ: Carbamazepine; LTG: Lamotrigine)

Time to treatment failure for due to adverse events ‐ by seizure type (CBZ: Carbamazepine; LTG: Lamotrigine)
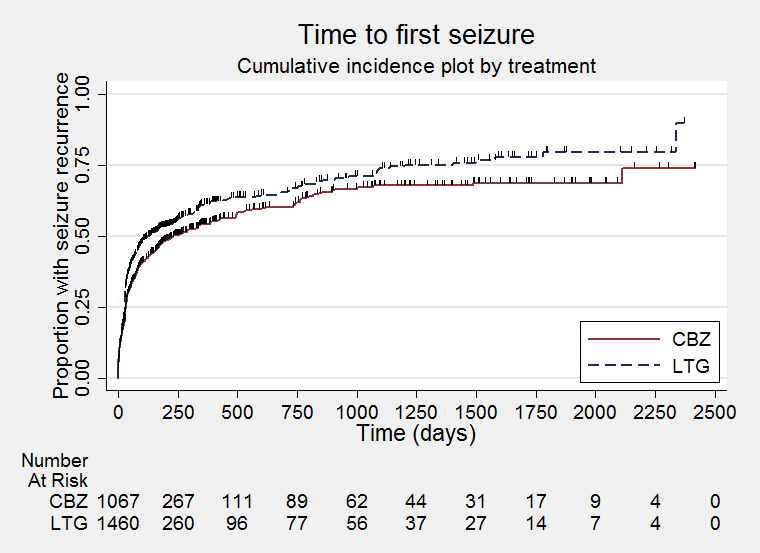
Time to first seizure (CBZ: Carbamazepine; LTG: Lamotrigine)
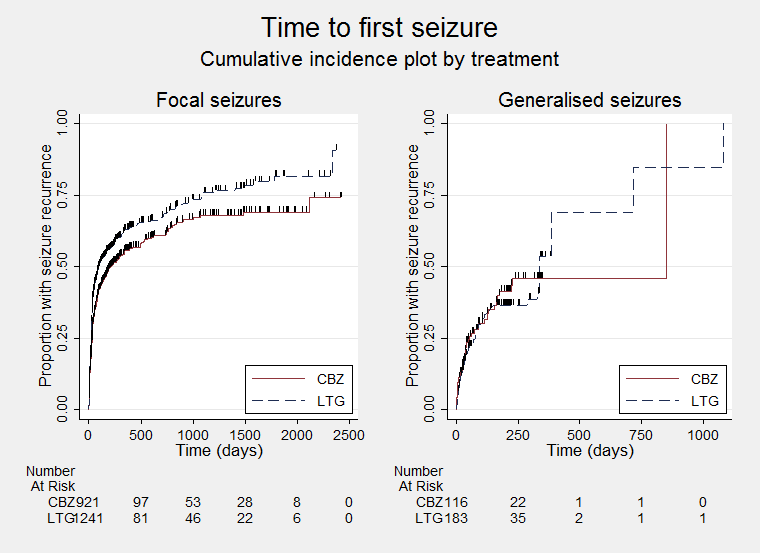
Time to first seizure ‐ by seizure type (CBZ: Carbamazepine; LTG: Lamotrigine)
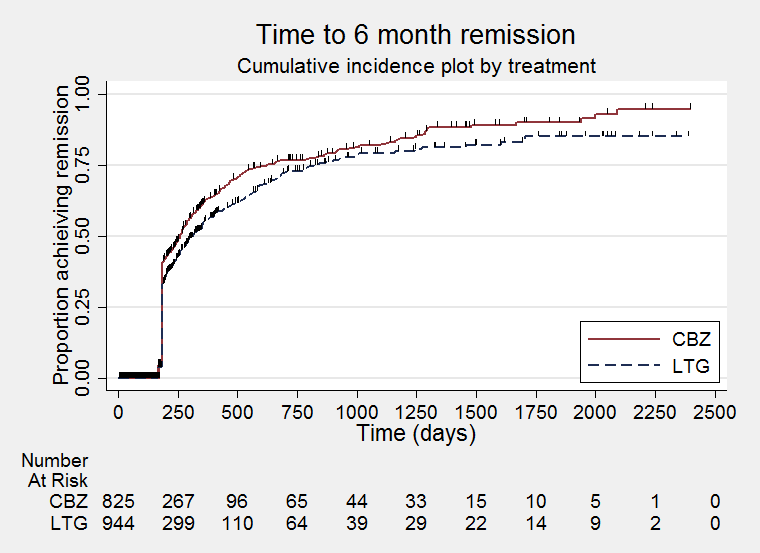
Time to six‐month remission (CBZ: Carbamazepine; LTG: Lamotrigine)

Time to six‐month remission ‐ by seizure type (CBZ: Carbamazepine; LTG: Lamotrigine)
Time to 12‐month remission (CBZ: Carbamazepine; LTG: Lamotrigine)

Time to 24‐month remission (CBZ: Carbamazepine; LTG: Lamotrigine)

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 1 Time to treatment failure (any reason related to the treatment).

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 2 Time to treatment failure due to adverse events.
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 3 Time to treatment failure due to lack of efficacy.
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 4 Time to treatment failure (any reason related to the treatment) ‐ by seizure type.
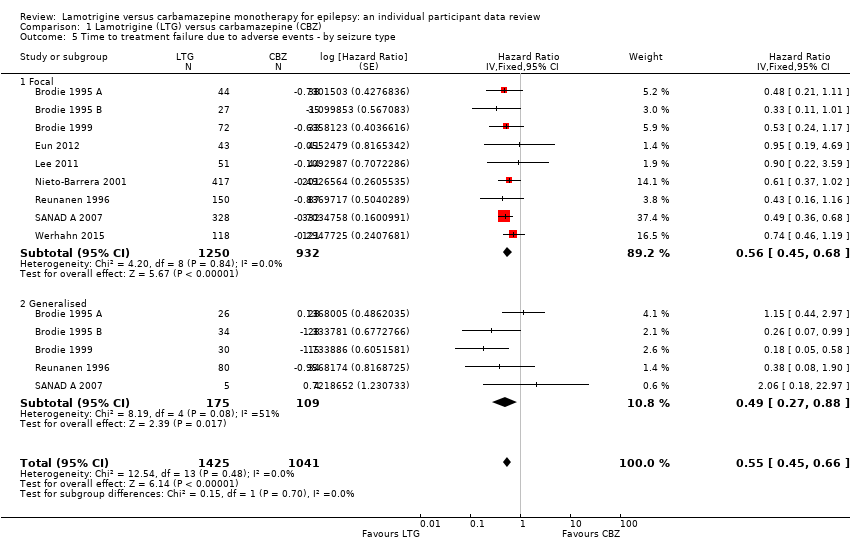
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 5 Time to treatment failure due to adverse events ‐ by seizure type.
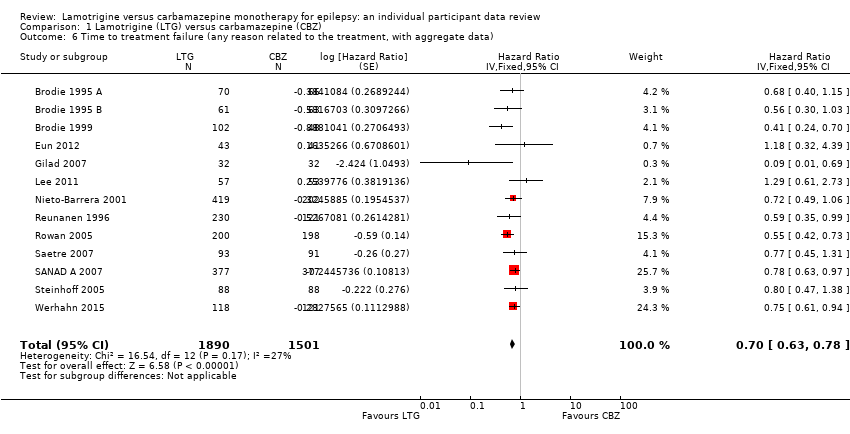
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 6 Time to treatment failure (any reason related to the treatment, with aggregate data).

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 7 Time to treatment failure (any reason related to the treatment) ‐ subgroup analysis (blinding).

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 8 Time to first seizure.

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 9 Time to first seizure by seizure type.
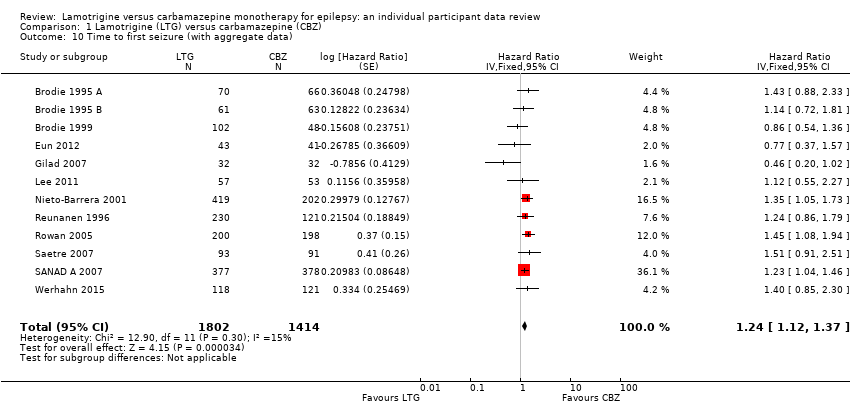
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 10 Time to first seizure (with aggregate data).
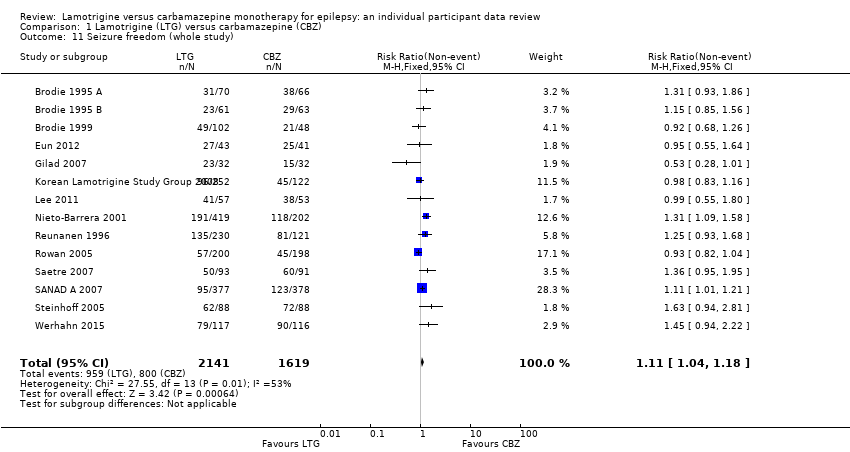
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 11 Seizure freedom (whole study).

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 12 Time to 6‐month remission.
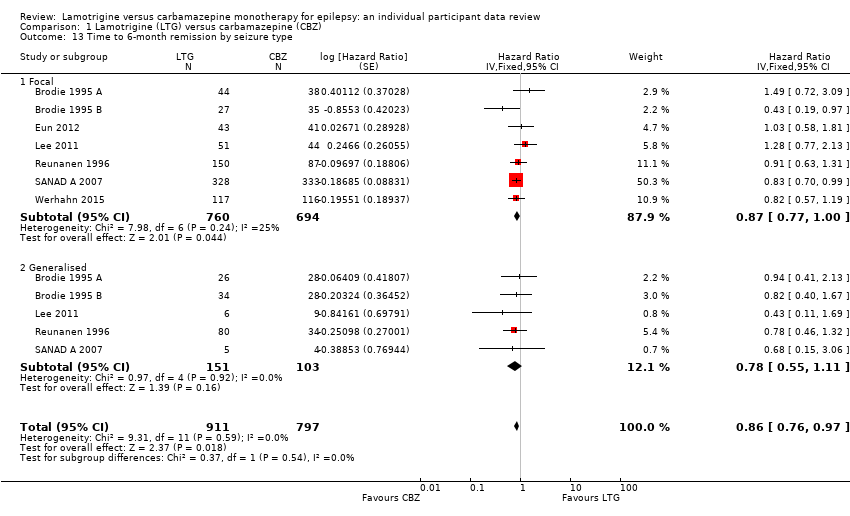
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 13 Time to 6‐month remission by seizure type.

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 14 Seizure freedom at 6 months.
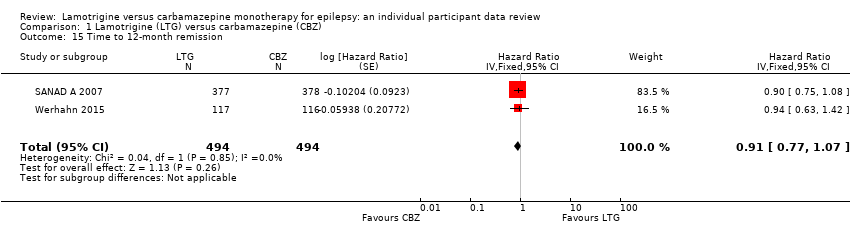
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 15 Time to 12‐month remission.

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 16 Time to 12‐month remission by seizure type.

Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 17 Time to 24‐month remission.
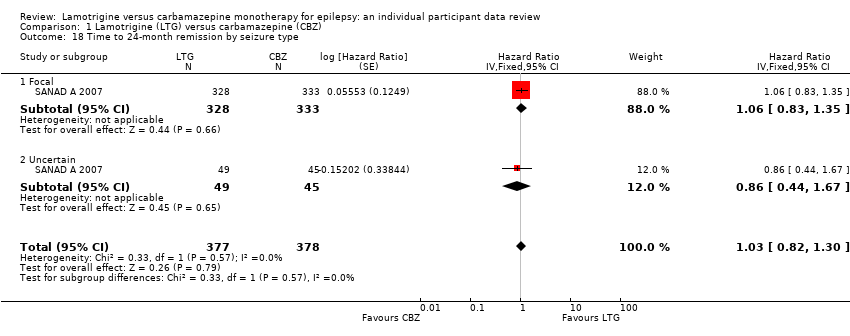
Comparison 1 Lamotrigine (LTG) versus carbamazepine (CBZ), Outcome 18 Time to 24‐month remission by seizure type.
| Lamotrigine compared with carbamazepine for epilepsy | ||||||
| Patient or population: adults and children with focal onset or generalised onset seizures (generalised tonic‐clonic with or without other generalised seizure types) Settings: outpatients Intervention: lamotrigine Comparison: carbamazepine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Carbamazepine | Lamotrigine | |||||
| Time to treatment failure (any reason related to treatment) All participants Range of follow‐up: 0 to 2420 days | The median time to treatment failure was 1144 days in the carbamazepine group | The median time to treatment failure was 1813 days (669 days longer) in the lamotrigine group | HR 0.71 (0.62 to 0.82)a | 2481 (9 trials) | ⊕⊕⊕⊝ | HR of less than 1 indicates an advantage for lamotrigine. Treatment failure due to adverse events also occurred significantly earlier on carbamazepine compared to lamotrigine: HR 0.54 (95% CI 0.45 to 0.65, P<0.00001). There was no difference between lamotrigine and carbamazepine in terms of treatment failure due to lack of efficacy: HR 1.03 (95% CI 0.75 to 1.41, P=0.86) |
| Time to treatment failure (any reason related to treatment) Subgroup: focal onset seizures Range of follow‐up: 0 to 2420 days | The median time to treatment failure was 1149 days in the carbamazepine group | The median time to treatment failure was 1699 days (550 days longer) in the lamotrigine group | HR 0.74 (0.64 to 0.86) | 2182 (9 trials) | ⊕⊕⊕⊝ | HR of less than 1 indicates an advantage for lamotrigine. Treatment failure due to adverse events also occurred significantly earlier on carbamazepine compared to lamotrigine: HR 0.56 (95% CI 0.45 to 0.68, P<0.00001). Treatment failure due to lack of efficacy was not calculated for focal onset seizures subgroup due to small numbers of individuals withdrawing from treatment for lack of efficacy. |
| Time to treatment failure (any reason related to treatment) Subgroup: generalised onset seizures Range of follow‐up: 0 to 1446 days | The 25th percentile** of time to treatment failure was 57 days in the carbamazepine group | The 25th percentile** of time to treatment failure was 510 days (453 days longer) in the lamotrigine group | HR 0.51 (0.33 to 0.78) | 299 (6 trials) | ⊕⊕⊝⊝ | HR of less than 1 indicates an advantage for lamotrigine Treatment failure due to adverse events also occurred significantly earlier on carbamazepine compared to lamotrigine: HR 0.49 (95% CI 0.27 to 0.88, P=0.02). Treatment failure due to lack of efficacy was not calculated for focal onset seizures subgroup due to small numbers of individuals withdrawing from treatment for lack of efficacy. |
| * Illustrative risks in the carbamazepine and lamotrigine groups are calculated at the median time to treatment failure (i.e. the time to 50% of participants failing or withdrawing from allocated treatment) within each group across all trials. The relative effect (pooled hazard ratio) shows the comparison of 'time to treatment failure' between the treatment groups. ** The 25th percentile of time to treatment failure (i.e. the time to 50% of participants failing or withdrawing from allocated treatment) is presented for the subgroup with generalised seizures as less than 50% of participants failed / withdrew from treatment, therefore the median time could not be calculated. Abbreviations: 95% CI: 95% confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| a. Pooled hazard ratio for all participants adjusted for seizure type. b. Downgraded once due to high risk of bias due to the open‐label design of five trials included in the analysis (Eun 2012; Lee 2011; Nieto‐Barrera 2001; Reunanen 1996; SANAD A 2007); the design of the trial may have influenced the withdrawal rates. c. Downgraded once due to high risk of bias due to the open‐label design of three trials included in the analysis (Lee 2011; Reunanen 1996; SANAD A 2007); the design of the trial may have influenced the withdrawal rates. d. Downgraded once due to potential misclassification of generalised onset seizures in up to 50% of participants in the trials. | ||||||
| Lamotrigine compared with carbamazepine for epilepsy | ||||||
| Patient or population: adults and children with focal onset or generalised onset seizures (generalised tonic‐clonic with or without other generalised seizure types) Settings: outpatients Intervention: lamotrigine Comparison: carbamazepine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Carbamazepine | Lamotrigine | |||||
| Time to first seizure All participants Range of follow‐up: 0 to 2420 days | The median time to first seizure was 232 days in the carbamazepine group | The median time to first seizure was 134 days (98 days shorter) in the lamotrigine group | HR 1.26 (1.12 to 1.41)a | 2476 (9 trials) | ⊕⊕⊕⊕ | HR of less than 1 indicates an advantage for lamotrigine |
| Time to first seizure Subgroup: focal onset seizures Range of follow‐up: 0 to 2420 days | The median time to first seizure was 208 days in the carbamazepine group | The median time to first seizure was 96 days (112 days shorter) in the lamotrigine group | HR 1.29 (1.14 to 1.45) | 2177 (9 trials) | ⊕⊕⊕⊕ | HR of less than 1 indicates an advantage for lamotrigine |
| Time to first seizure Subgroup: generalised onset seizures Range of follow‐up: 0 to 853 days | The median time to first seizure was 853 days in the carbamazepine group | The median time to first seizure was 337 days (516 days longer) in the lamotrigine group | HR 0.98 (0.65 to 1.48) | 277 (6 trials) | ⊕⊕⊝⊝ | HR of less than 1 indicates an advantage for lamotrigine |
| Time to 12‐month remission All participants Range of follow‐up: 0 to 2420 days | The median time to 12‐month remission was 452 days in the carbamazepine group | The median time to 12‐month remission was 538 days (86 days longer) in the lamotrigine group | HR 0.91 (0.77 to 1.07) | 988 (2 trials) | ⊕⊕⊕⊕ | HR of less than 1 indicates an advantage for carbamazepine Time to 12‐month remission not presented by seizure type due to small numbers of participants with generalised onset seizures in the two trials |
| * Illustrative risks in the carbamazepine and lamotrigine groups are calculated at the median time to first seizure or time to 12‐month remission (i.e. the time to 50% of participants experiencing a first seizure or 12‐months of remission) within each group across all trials. The relative effect (pooled hazard ratio) shows the comparison of 'time to first seizure' or 'time to 12‐month remission' between the treatment groups. Abbreviations: 95% CI: 95% confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| a. Pooled hazard ratio for all participants adjusted for seizure type. b. High risk of bias due to the open‐label design in some of the included trials, however outcomes are objective and unlikely to be influenced by knowledge of drug allocation. No downgrade made. c. Downgraded once due to potential misclassification of generalised onset seizures in up to 50% of participants in the trials. | ||||||
| Focal seizures: n (%) | Male gender: n (%) | Age at entry (years): Mean (SD), range | Aged > 30 and generalised seizures: n (%) | Epilepsy duration (years): Mean (SD), range | Number of seizures in prior 6 months: median (range) | |||||||||||||
| LTG | CBZ | Missing | LTG | CBZ | Missing | LTG | CBZ | Missing | LTG | CBZ | Missing | LTG | CBZ | Missing | LTG | CBZ | Missing | |
| 44 (63%) | 38 (58%) | 0 | 28 (40%) | 28 (42%) | 0 | 35.3 (17.1), 15 to 71 | 32.5 (14.4), 13 to 69 | 0 | 11 | 9 | 0 | 2.2 (3.3), 0 to 17.9 | 1.8 (2.3), 0.3 to 11.0 | 0 | 4 (1 to 490) | 3 (1 to 960) | 0 | |
| 27 (44%) | 35 (56%) | 0 | 26 (43%) | 30 (48%) | 0 | 30.9 (14.5), 14 to 86 | 29.1 (13.9), 14 to 81 | 0 | 12 | 11 | 0 | 1.4 (3.2), 0 to 19.4 | 1.2 (1.8), 0 to 7.1 | 0 | 3 (1 to 1020) | 3 (2 to 122) | 0 | |
| 72 (71%) | 33 (69%) | 0 | 55 (54%) | 28 (58%) | 0 | 77.3 (6.1), 65 to 94 | 76.2 (5.9), 66 to 88 | 0 | 30 | 15 | 0 | NA | NA | 150 | 3 (1 to 163) | 4.5 (1 to 108) | 0 | |
| 43 (100%) | 41 (100%) | 0 | 24 (56%) | 24 (59%) | 0 | 9.2 (2.0), 6 to 13 | 8.3 (2.1), 5 to 12 | 0 | 0 | 0 | 0 | 0.6 (0.9), 0 to 4.5 | 0.5 (0.3), 0 to 1.4 | 1 | 3(2 to 11) | 3 (2 to 11) | 0 | |
| 51 (89%) | 44 (83%) | 0 | 24 (42%) | 33 (62%) | 0 | 33.6 (12.6), 16 to 60 | 38.3 (11.5), 16 to 60 | 0 | 2 | 7 | 0 | NA | NA | 110 | 2(0 to 60) | 2 (0 to 200) | 0 | |
| 418 (99.5%) | 201 (99.5%) | 0 | 222 (53%) | 107 (53%) | 0 | 27.1 (21.7), 2 to 84 | 27.5 (21.0), 2 to 77 | 1 | 1 | 1 | 0 | NA | NA | 622 | 4 (1 to 9000) | 3 (1 to 3600) | 0 | |
| 150 (65%) | 87 (72%) | 0 | 127 (55%) | 61 (50%) | 0 | 31.8 (14.0), 12 to 71 | 32.7 (14.6), 13 to 71 | 2 | 31 | 12 | 0 | 2.2 (3.2), 0 to 17.1 | 2.2 (3.7), 0.26 to 8 | 3 | 3(1 to 133) | 3 (1 to 145) | 1 | |
| 329 (99%) | 333 (99%) | 85 | 205 (55%) | 204 (55%) | 18 | 36.8 (18.4), 6 to 83 | 39.3 (18.4), 5 to 82 | 18 | 46 | 42 | 0 | NA | NA | 727 | 2(0 to 1185) | 4 (0 to 466) | 19 | |
| 118 (100%) | 121 (100%) | 0 | 69 (59%) | 65 (54%) | 0 | 70.8 (7.5), 60 to 88 | 71.8 (6.7), 60 to 89 | 0 | 0 | 0 | 0 | NA | NA | 239 | 2 (1 to 20) | 2 (1 to 90) | 6 | |
| CBZ = carbamazepine, LTG = lamotrigine; n = number of participants; NA = not applicable; SD = standard deviation | ||||||||||||||||||
| EEG normal: n (%) | CT scan normal: n (%) | Neurological exam normal: n (%) | |||||||
| LTG | CBZ | Missing | LTG | CBZ | Missing | LTG | CBZ | Missing | |
| 32 (46%) | 30 (46%) | 2 | 38 (84%) | 44 (90%) | 42 | 62 (89%) | 61 (92%) | 0 | |
| 42 (73%) | 34 (56%) | 6 | 34 (77%) | 38 (79%) | 32 | 56 (92%) | 52 (83%) | 0 | |
| NA | NA | 150 | 39 (39%) | 23 (48%) | 1 | 59 (58%) | 31 (65%) | 0 | |
| 3 (7%) | 3 (7%) | 0 | 38 (88%) | 37(90%) | 0 | 43 (100%) | 40 (98%) | 0 | |
| 31 (54%) | 27 (51%) | 0 | 36 (63%) | 38 (72%) | 0 | 57 (100%) | 53 (100%) | 0 | |
| NA | NA | 622 | NA | NA | 622 | NA | NA | 622 | |
| 9 (53%) | 4 (44%) | 325 | 11 (73%) | 5 (83%) | 330 | 202 (89%) | 103 (85%) | 0 | |
| NA | NA | 756 | NA | NA | 756 | 277 (75%) | 281 (76%) | 18 | |
| 45 (38%) | 37 (31%) | 1 | 26 (22%) | 26 (21%) | 1 | NA | NA | 239 | |
| CBZ = carbamazepine; CT = computerised tomography; EEG = electroencephalogram; LTG = lamotrigine; n = number of participants; NA = not applicable | |||||||||
| Number randomised | Time to treatment failure | Time to first seizure | Time to 6‐ month remission1 | Time to 12‐ month remission | Time to 24‐ month remission | |||||||||||||
| LTG | CBZ | Total | LTG | CBZ | Total | LTG | CBZ | Total | LTG | CBZ | Total | LTG | CBZ | Total | LTG | CBZ | Total | |
| 70 | 66 | 136 | 70 | 66 | 136 | 70 | 66 | 136 | 70 | 66 | 136 | NA | NA | NA | NA | NA | NA | |
| 61 | 63 | 124 | 61 | 63 | 124 | 61 | 63 | 124 | 61 | 63 | 124 | NA | NA | NA | NA | NA | NA | |
| 102 | 48 | 150 | 102 | 48 | 150 | 102 | 48 | 150 | 102 | 48 | 150 | NA | NA | NA | NA | NA | NA | |
| 43 | 41 | 84 | 43 | 41 | 84 | 43 | 41 | 84 | 43 | 41 | 84 | NA | NA | NA | NA | NA | NA | |
| 57 | 53 | 110 | 57 | 53 | 110 | 57 | 53 | 110 | 57 | 53 | 110 | NA | NA | NA | NA | NA | NA | |
| 420 | 202 | 622 | 419 | 202 | 621 | 419 | 202 | 621 | 419 | 202 | 621 | NA | NA | NA | NA | NA | NA | |
| 230 | 121 | 351 | 230 | 121 | 351 | 230 | 121 | 351 | 230 | 121 | 351 | NA | NA | NA | NA | NA | NA | |
| 378 | 378 | 756 | 377 | 377 | 754 | 377 | 378 | 755 | 377 | 378 | 755 | 377 | 378 | 755 | 377 | 378 | 755 | |
| 118 | 121 | 239 | 118 | 121 | 239 | 117 | 116 | 233 | 117 | 116 | 233 | 117 | 116 | 233 | NA | NA | NA | |
| Total | 1479 | 1093 | 2572 | 1477 | 1092 | 2569 | 1476 | 1088 | 2564 | 1476 | 1088 | 2564 | 494 | 494 | 988 | 377 | 378 | 755 |
| CBZ = carbamazepine; LTG = lamotrigine; NA: not applicable (trial duration not sufficient to measure the outcome). 1. Brodie 1999, and Nieto‐Barrera 2001, are of 24 weeks duration (approximately six months). The two trials are not included in the analyses of time to six‐month remission but are included in sensitivity analysis of seizure freedom at six months. 2. Follow‐up data are missing for one participant in Nieto‐Barrera 2001. 3. Treatment failure time missing for two participants and seizure data after follow‐up missing for one participant in SANAD A 2007. 4. Seizure data after follow‐up missing for six participants in Werhahn 2015. | ||||||||||||||||||
| Reason for early termination1 | Classification in time‐to‐event analyses: Event | Classification in time‐to‐event analyses: Censored | Total | ||||||||||
| Adverse events | Inadequate response/seizure recurrence | Both adverse events and inadequate response | Protocol violation/non‐compliance | Withdrew consent/participant choice3 | Other (treatment‐related)4 | Illness or death (not treatment‐related) | Remission of seizures | Lost to follow‐up | Other (not treatment‐related)5 | Completed trial | |||
| LTG | 18 | 3 | 0 | 3 | 1 | 0 | 1 | 0 | 1 | 0 | 43 | 70 | |
| CBZ | 22 | 2 | 0 | 6 | 1 | 0 | 0 | 0 | 2 | 0 | 33 | 66 | |
| LTG | 7 | 3 | 0 | 5 | 2 | 0 | 0 | 0 | 1 | 0 | 43 | 61 | |
| CBZ | 23 | 1 | 0 | 3 | 1 | 0 | 0 | 0 | 1 | 0 | 34 | 63 | |
| LTG | 18 | 0 | 0 | 7 | 3 | 0 | 1 | 0 | 2 | 0 | 71 | 102 | |
| CBZ | 20 | 0 | 0 | 3 | 2 | 2 | 0 | 0 | 1 | 0 | 20 | 48 | |
| LTG | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 34 | 43 | |
| CBZ | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 35 | 41 | |
| LTG | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 31 | 32 | |
| CBZ | 10 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 21 | 32 | |
| LTG | 24 | 11 | 0 | 0 | 0 | 52 | 0 | 0 | 0 | 0 | 165 | 252 | |
| CBZ | 13 | 2 | 0 | 0 | 0 | 22 | 0 | 0 | 0 | 0 | 85 | 122 | |
| LTG | 4 | 3 | 0 | 2 | 7 | 0 | 0 | 0 | 2 | 0 | 39 | 57 | |
| CBZ | 7 | 0 | 0 | 3 | 2 | 0 | 0 | 0 | 7 | 0 | 34 | 53 | |
| LTG | 34 | 12 | 0 | 6 | 16 | 0 | 0 | 0 | 13 | 0 | 339 | 420 | |
| CBZ | 26 | 4 | 0 | 11 | 2 | 0 | 0 | 0 | 3 | 0 | 156 | 202 | |
| LTG | 10 | 1 | 0 | 17 | 3 | 3 | 4 | 0 | 0 | 0 | 192 | 230 | |
| CBZ | 12 | 0 | 0 | 11 | 6 | 0 | 2 | 0 | 0 | 0 | 90 | 121 | |
| LTG | 20 | 7 | 0 | 15 | 24 | 0 | 7 | 0 | 10 | 5 | 112 | 200 | |
| CBZ | 54 | 3 | 0 | 14 | 28 | 0 | 14 | 0 | 4 | 10 | 71 | 198 | |
| LTG | 13 | 0 | 0 | 2 | 0 | 10 | 0 | 0 | 0 | 0 | 68 | 93 | |
| CBZ | 23 | 0 | 0 | 1 | 0 | 6 | 0 | 0 | 0 | 0 | 61 | 91 | |
| LTG | 61 | 60 | 11 | 1 | 4 | 16 | 7 | 23 | 0 | 14 | 181 | 378 | |
| CBZ | 104 | 43 | 20 | 2 | 1 | 7 | 10 | 25 | 0 | 15 | 151 | 378 | |
| LTG | 7 | 1 | 0 | 0 | 13 | 3 | 0 | 0 | 0 | 0 | 64 | 88 | |
| CBZ | 17 | 0 | 0 | 0 | 7 | 5 | 0 | 0 | 0 | 0 | 59 | 88 | |
| LTG | 31 | 2 | 0 | 6 | 13 | 1 | 0 | 0 | 0 | 0 | 65 | 118 | |
| CBZ | 39 | 3 | 0 | 4 | 20 | 0 | 0 | 0 | 0 | 0 | 55 | 121 | |
| Total LTG | 251 | 105 | 11 | 64 | 86 | 85 | 20 | 23 | 33 | 19 | 1447 | 2144 | |
| Total CBZ | 373 | 58 | 20 | 58 | 71 | 42 | 27 | 25 | 20 | 25 | 905 | 1624 | |
| Total (all) | 624 | 163 | 31 | 122 | 157 | 127 | 47 | 48 | 53 | 44 | 2352 | 3768 | |
| 1. Primary reason for discontinuation specified ‐ participants may have withdrawn from allocated treatment for a combination of reasons. 2. Reasons for treatment failure extracted from trial publications for Gilad 2007, Korean Lamotrigine Study Group 2008; Rowan 2005, Saetre 2007, and Steinhoff 2005. Individual participant data for reasons for treatment failure provided for other trials. 3. Withdrawal of consent/participant choice classified as an event in this review but censored in included trial (SANAD A 2007). Sensitivity analysis classifying withdrawal of consent as a censored observation did not change the conclusions (results available on request). 4. Other treatment‐related reasons: investigator choice (Werhahn 2015), drug‐related death, pregnancy or perceived remission (SANAD A 2007). Specified only as 'other reason' for Brodie 1999; Reunanen 1996; Korean Lamotrigine Study Group 2008; Saetre 2007 and Steinhoff 2005. 5. Other reasons (not treatment‐related): epilepsy diagnosis changed (SANAD A 2007). Specified only as 'other reason' for Rowan 2005, and for seven participants in SANAD A 2007. 6. No information on whether participants withdrew from treatment or completed the study available for 19 participants 7. One participant (randomised to LTG) with date and reason for treatment failure missing. 8. Two participants with date of treatment failure missing so not included in analysis of time to treatment failure but with reasons for treatment failure provided (both censored: one withdrew from LTG due to remission of seizures, one withdrew from CBZ due to 'other' non‐treatment‐related reason). | |||||||||||||
| Treatment | N | Comparator | N | Total | Time to treatment failure | Time to first seizure | Time to 6‐month remission | |||
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | |||||
| Lamotrigine (both arms) | 230 | Carbamazepine | 121 | 351 | 0.59 (0.35 to 0.99) | 0.04 | 1.24 (0.86 to 1.79) | 0.25 | 0.84 (0.36 to 1.95) | 0.68 |
| Lamotrigine 200 mg | 115 | Lamotrigine 100 mg + carbamazepine | 236 | 351 | 0.47 (0.25 to 0.86) | 0.02 | 0.96 (0.67 to 1.36) | 0.8 | 0.62 (0.24 to 1.58) | 0.32 |
| Lamotrigine 100 mg | 115 | Lamotrigine 200 mg + carbamazepine | 236 | 351 | 1.05 (0.63 to 1.75) | 0.85 | 1.29 (0.91 to 1.83) | 0.15 | 1.33 (0.56 to 3.17) | 0.52 |
| Lamotrigine 200 mg | 115 | Carbamazepine | 121 | 236 | 0.41 (0.21 to 0.78) | 0.007 | 1.12 (0.73 to 1.72) | 0.59 | 0.63 (0.22 to 1.78) | 0.39 |
| Lamotrigine 100 mg | 115 | Carbamazepine | 121 | 236 | 0.73 (0.43 to 1.26) | 0.26 | 1.37 (0.90 to 2.07) | 0.14 | 1.10 (0.41 to 2.92) | 0.86 |
| mg= milligrams per day; HR = hazard ratio; 95% CI = 95% confidence interval | ||||||||||
| Time to treatment failure | Time to first seizure | Time to 6‐month remission | |
| Original analysis | F: HR 0.74, 95% CI (0.64 to 0.86) G: HR 0.51, 95% CI (0.33 to 0.78) O: HR 0.71, 95% CI (0.62 to 0.82) | F: HR 1.29, 95% CI (1.14 to 1.45) G: HR 0.98, 95% CI (0.65 to 1.48) O: HR 1.26, 95% CI (1.12 to 1.41) | F: HR 0.87, 95% CI (0.77 to 1.00) G: HR 0.78, 95% CI (0.55 to 1.11) O: HR 0.86, 95% CI (0.76 to 0.97) |
| Test of subgroup differences | Chi² = 2.73, df = 1 (P = 0.10), I² = 63.4% | Chi² = 1.53, df = 1 (P = 0.22), I² = 34.5% | Chi² = 0.37, df = 1 (P = 0.54), I² = 0% |
| Generalised onset and age at onset > 30 reclassified | F: HR 0.72, 95% CI (0.62 to 0.83) G: HR 0.58, 95% CI (0.32 to 1.06) O: HR 0.71, 95% CI (0.62 to 0.82) | F: HR 1.25, 95% CI (1.11 to 1.41) G: HR 1.17, 95% CI (0.67 to 2.04) O: HR 1.25, 95% CI (1.11 to 1.40) | F: HR 0.85, 95% CI (0.75 to 0.97) G: HR 0.69, 95% CI (0.44 to 1.08) O: HR 0.84, 95% CI (0.74 to 0.95) |
| Test of subgroup differences | Chi² = 0.45, df = 1 (P = 0.50), I² = 0% | Chi² = 0.06, df = 1 (P = 0.81), I² = 0% | Chi² = 0.80, df = 1 (P = 0.37), I² = 0% |
| Generalised onset and age at onset > 30 reclassified | F: HR 0.74, 95% CI (0.64 to 0.86) G: HR 0.58, 95% CI (0.32 to 1.06) U: HR 0.62, 95% CI (0.39 to 0.97) O: HR 0.72, 95% CI (0.63 to 0.83) | F: HR 1.29, 95% CI (1.14 to 1.45) G: HR 1.17, 95% CI (0.67 to 2.04) U: HR 0.88, 95% CI (0.58 to 1.33) O: HR 1.24, 95% CI (1.11 to 1.39) | F: HR 0.87, 95% CI (0.77 to 1.00) G: HR 0.69, 95% CI (0.44 to 1.08) U: HR 0.89, 95% CI (0.60 to 1.31) O: HR 0.86, 95% CI (0.76 to 0.97) |
| Test of subgroup differences | Chi² = 1.15, df = 2 (P = 0.56), I² = 0% | Chi² = 3.03, df = 2 (P = 0.22), I² = 33.9% | Chi² = 1.02, df = 2 (P = 0.60), I² = 0% |
| CI = confidence interval; F = focal onset seizures; G = generalised onset seizures; HR = hazard ratio; O = overall pooled result adjusted by seizure type; U = uncertain seizure type. | |||
| Trial | Number experiencing adverse events | Number of adverse events | Number of adverse events per person (range) | Number of drug‐related adverse events1 | Number of adverse events requiring action/ treatment change | Number of patients needing a treatment change/dose change | |||||||||||
| LTG | CBZ | Total | LTG | CBZ | Total | LTG | CBZ | LTG | CBZ | Total | LTG | CBZ | Total | LTG | CBZ | Total | |
| 62 | 58 | 120 | 388 | 322 | 710 | 1 to 30 | 1 to 17 | 94 | 124 | 218 | 167 | 111 | 278 | 22 | 32 | 54 | |
| 54 | 58 | 112 | 285 | 291 | 576 | 1 to 14 | 1 to 18 | 81 | 125 | 206 | 98 | 81 | 179 | 20 | 40 | 60 | |
| 91 | 41 | 132 | 338 | 173 | 511 | 1 to 12 | 1 to 10 | 109 | 73 | 182 | 92 | 66 | 158 | 39 | 27 | 66 | |
| 3 | 6 | 9 | 5 | 8 | 13 | 1 to 30 | 1 to 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| 4 | 6 | 10 | NA | NA | NA | NA | NA | 4 | 5 | 9 | NA | NA | NA | NA | NA | NA | |
| 218 | 120 | 338 | 524 | 277 | 801 | 1 to 10 | 1 to 11 | 238 | 152 | 390 | 116 | 82 | 198 | 70 | 54 | 124 | |
| 124 | 77 | 201 | 451 | 243 | 694 | 1 to 14 | 1 to 8 | 138 | 169 | 307 | 156 | 52 | 208 | 23 | 36 | 59 | |
| 229 | 260 | 489 | 1038 | 1339 | 2377 | 1 to 25 | 1 to 37 | NA | NA | NA | 447 | 665 | 1112 | 120 | 173 | 293 | |
| 120 | 110 | 230 | 779 | 770 | 1549 | 1 to 53 | 1 to 30 | 291 | 382 | 673 | 147 | 159 | 306 | 64 | 65 | 129 | |
| CBZ = carbamazepine; LTG = lamotrigine; NA = information not available. 1. In Brodie 1995 A, Brodie 1995 B and Reunanen 1996 adverse events that are "definitely related", in Brodie 1999 and Nieto‐Barrera 2001 "a reasonable possibility" that adverse events are treatment‐related and in Werhahn 2015 adverse events are "related, probably related or possibility related". | |||||||||||||||||
| Most commonly occurring adverse events | ||||||||||||||||
| LTG | CBZ | LTG | CBZ | LTG | CBZ | LTG | CBZ | |||||||||
| Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | |
| Accidental injury/fracture | 2 | 2 | 1 | 1 | 3 | 3 | 2 | 2 | 19 | 12 | 4 | 3 | 7 | 7 | 1 | 1 |
| Aggression | 8 | 6 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 3 | 3 | 2 | 2 |
| Anorexia/weight loss | 2 | 2 | 0 | 0 | 6 | 4 | 0 | 0 | 2 | 2 | 1 | 1 | 6 | 5 | 0 | 0 |
| Anxiety/depression | 12 | 5 | 7 | 5 | 6 | 3 | 10 | 7 | 3 | 3 | 0 | 0 | 8 | 8 | 2 | 2 |
| Aphasia | 0 | 0 | 3 | 3 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 2 | 1 | 1 | 0 | 0 |
| Ataxia | 2 | 2 | 6 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 3 | 3 |
| Chest infection/bronchitis | 11 | 6 | 12 | 8 | 3 | 3 | 1 | 1 | 16 | 12 | 4 | 4 | 18 | 15 | 8 | 8 |
| Cold/influenza | 17 | 15 | 4 | 4 | 8 | 8 | 10 | 9 | 7 | 7 | 1 | 1 | 25 | 19 | 11 | 11 |
| Concentration | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 4 | 4 | 1 | 1 |
| Confusion | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 0 |
| Cough/wheeze | 5 | 5 | 5 | 5 | 2 | 2 | 1 | 1 | 6 | 5 | 1 | 1 | 6 | 5 | 6 | 5 |
| Dental | 3 | 3 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | 6 | 3 | 3 |
| Dizzy/faint | 16 | 9 | 16 | 11 | 12 | 9 | 22 | 14 | 26 | 18 | 16 | 14 | 43 | 34 | 16 | 15 |
| Drowsy/fatigued | 32 | 21 | 52 | 31 | 34 | 20 | 49 | 36 | 25 | 17 | 21 | 15 | 36 | 34 | 45 | 40 |
| Gastrointestinal disturbances | 14 | 7 | 10 | 8 | 6 | 6 | 7 | 5 | 29 | 22 | 14 | 11 | 36 | 28 | 17 | 17 |
| Hair loss | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Headache/migraine | 77 | 27 | 31 | 17 | 48 | 24 | 52 | 22 | 14 | 10 | 8 | 8 | 56 | 46 | 16 | 14 |
| Impotence | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Increased/worsened seizures | 1 | 1 | 2 | 2 | 1 | 1 | 0 | 0 | 4 | 4 | 2 | 2 | 14 | 12 | 4 | 4 |
| Kidney/urinary problems | 3 | 2 | 2 | 2 | 4 | 4 | 1 | 1 | 12 | 10 | 4 | 4 | 4 | 4 | 1 | 1 |
| Memory problems | 7 | 5 | 2 | 2 | 5 | 3 | 3 | 2 | 4 | 4 | 0 | 0 | 2 | 2 | 1 | 1 |
| Menstrual problems | 3 | 3 | 16 | 12 | 0 | 0 | 4 | 4 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| Mood/behavioural change | 9 | 5 | 6 | 5 | 1 | 1 | 6 | 6 | 5 | 4 | 0 | 0 | 7 | 7 | 4 | 4 |
| Nausea/vomiting | 17 | 13 | 15 | 11 | 26 | 18 | 21 | 9 | 21 | 17 | 8 | 6 | 26 | 23 | 13 | 11 |
| Pain | 19 | 13 | 9 | 6 | 23 | 13 | 7 | 5 | 20 | 17 | 7 | 7 | 13 | 8 | 4 | 2 |
| Pins and needles/tingling | 2 | 1 | 3 | 2 | 3 | 3 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
| Rash/skin problems | 25 | 21 | 20 | 13 | 32 | 15 | 32 | 23 | 31 | 19 | 30 | 14 | 49 | 46 | 32 | 30 |
| Sleep problems/dreams | 4 | 3 | 4 | 4 | 8 | 5 | 12 | 5 | 9 | 8 | 0 | 0 | 19 | 19 | 1 | 1 |
| Throat/tonsil infection | 11 | 7 | 7 | 6 | 6 | 5 | 3 | 3 | 1 | 1 | 0 | 0 | 15 | 14 | 7 | 7 |
| Tremor/twitch | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 2 | 2 |
| Visual disturbance/nystagmus | 8 | 4 | 6 | 5 | 2 | 2 | 9 | 6 | 1 | 1 | 4 | 3 | 7 | 7 | 3 | 2 |
| Weight gain | 3 | 3 | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 3 | 3 | 3 |
| Table of most commonly occurring adverse events split into two for formatting reasons. Events = number of adverse events reported; Ppts = number of participants reporting the adverse event (a participant could report the same type of adverse event multiple times). LTG = lamotrigine; CBZ = carbamazepine Most common adverse events are defined as events reported 10 or more times in at least one of the seven trials (Brodie 1995 A; Brodie 1995 B; Brodie 1999; Nieto‐Barrera 2001; Reunanen 1996; SANAD A 2007; Werhahn 2015). Less commonly reported adverse events are not summarised in this table but details are available on request from the review authors. General terminology for the type of adverse events was defined by the review authors based on the individual participant data provided. | ||||||||||||||||
| Most commonly occurring adverse events | Total (across seven studies) | |||||||||||||||
| LTG | CBZ | LTG | CBZ | LTG | CBZ | LTG | CBZ | |||||||||
| Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | Events | Ppts | |
| Accidental injury/fracture | 2 | 2 | 0 | 0 | 29 | 19 | 10 | 10 | 16 | 15 | 14 | 7 | 78 | 60 | 32 | 24 |
| Aggression | 1 | 1 | 0 | 0 | 25 | 18 | 41 | 21 | 1 | 1 | 1 | 1 | 40 | 31 | 46 | 26 |
| Anorexia/weight loss | 3 | 2 | 0 | 0 | 12 | 11 | 16 | 13 | 1 | 1 | 0 | 0 | 32 | 27 | 17 | 14 |
| Anxiety/depression | 4 | 4 | 2 | 2 | 48 | 34 | 46 | 34 | 17 | 14 | 17 | 10 | 98 | 71 | 84 | 60 |
| Aphasia | 1 | 1 | 0 | 0 | 7 | 4 | 11 | 8 | 1 | 1 | 7 | 5 | 11 | 8 | 23 | 18 |
| Ataxia | 0 | 0 | 3 | 3 | 38 | 20 | 30 | 22 | 1 | 1 | 0 | 0 | 43 | 25 | 42 | 33 |
| Chest infection/bronchitis | 3 | 3 | 1 | 1 | 2 | 1 | 6 | 5 | 8 | 8 | 3 | 3 | 61 | 48 | 35 | 30 |
| Cold/influenza | 9 | 8 | 2 | 2 | 1 | 1 | 3 | 3 | 11 | 9 | 20 | 15 | 78 | 67 | 51 | 45 |
| Concentration | 3 | 3 | 4 | 3 | 8 | 7 | 11 | 11 | 5 | 5 | 3 | 3 | 20 | 19 | 21 | 20 |
| Confusion | 0 | 0 | 0 | 0 | 30 | 19 | 33 | 22 | 4 | 4 | 5 | 5 | 37 | 26 | 39 | 28 |
| Cough/wheeze | 3 | 3 | 0 | 0 | 4 | 4 | 1 | 1 | 14 | 11 | 13 | 11 | 40 | 35 | 27 | 24 |
| Dental | 6 | 5 | 0 | 0 | 7 | 7 | 16 | 11 | 3 | 2 | 2 | 2 | 27 | 25 | 25 | 20 |
| Dizzy/faint | 17 | 13 | 20 | 13 | 55 | 32 | 64 | 37 | 74 | 46 | 62 | 41 | 243 | 161 | 216 | 145 |
| Drowsy/fatigued | 56 | 40 | 77 | 47 | 125 | 72 | 267 | 123 | 30 | 24 | 51 | 46 | 338 | 228 | 562 | 338 |
| Gastrointestinal disturbances | 21 | 17 | 10 | 8 | 48 | 31 | 49 | 35 | 45 | 34 | 65 | 42 | 199 | 145 | 172 | 126 |
| Hair loss | 0 | 0 | 0 | 0 | 6 | 4 | 15 | 6 | 3 | 3 | 3 | 3 | 10 | 8 | 20 | 11 |
| Headache/migraine | 74 | 42 | 20 | 13 | 95 | 49 | 97 | 43 | 48 | 31 | 40 | 29 | 412 | 229 | 264 | 146 |
| Impotence | 1 | 1 | 0 | 0 | 5 | 4 | 17 | 5 | 0 | 0 | 0 | 0 | 6 | 5 | 17 | 5 |
| Increased/worsened seizures | 1 | 1 | 0 | 0 | 29 | 21 | 41 | 25 | 86 | 35 | 58 | 27 | 136 | 75 | 107 | 60 |
| Kidney/urinary problems | 4 | 3 | 2 | 2 | 4 | 3 | 10 | 8 | 16 | 16 | 18 | 17 | 47 | 42 | 38 | 35 |
| Memory problems | 4 | 4 | 3 | 3 | 38 | 23 | 71 | 34 | 7 | 6 | 7 | 7 | 67 | 47 | 87 | 49 |
| Menstrual problems | 15 | 9 | 13 | 7 | 4 | 4 | 3 | 2 | 0 | 0 | 0 | 0 | 22 | 16 | 37 | 26 |
| Mood/behavioural change | 5 | 5 | 4 | 1 | 32 | 22 | 56 | 34 | 2 | 2 | 6 | 5 | 61 | 46 | 82 | 55 |
| Nausea/vomiting | 21 | 15 | 15 | 11 | 38 | 23 | 54 | 35 | 30 | 23 | 37 | 24 | 179 | 132 | 163 | 107 |
| Pain | 18 | 15 | 1 | 1 | 14 | 9 | 15 | 12 | 55 | 28 | 28 | 20 | 162 | 103 | 71 | 53 |
| Pins and needles/tingling | 3 | 2 | 0 | 0 | 13 | 13 | 23 | 13 | 4 | 4 | 3 | 3 | 27 | 25 | 29 | 18 |
| Rash/skin problems | 33 | 26 | 17 | 14 | 65 | 36 | 99 | 65 | 23 | 20 | 39 | 32 | 258 | 183 | 269 | 191 |
| Sleep problems/dreams | 27 | 19 | 3 | 2 | 46 | 32 | 24 | 12 | 19 | 18 | 10 | 9 | 132 | 104 | 54 | 33 |
| Throat/tonsil infection | 13 | 10 | 1 | 1 | 2 | 2 | 1 | 1 | 6 | 4 | 4 | 3 | 54 | 43 | 23 | 21 |
| Tremor/twitch | 7 | 6 | 0 | 0 | 28 | 12 | 13 | 10 | 16 | 8 | 10 | 9 | 53 | 28 | 27 | 22 |
| Visual disturbance/nystagmus | 6 | 4 | 7 | 5 | 34 | 22 | 33 | 22 | 13 | 10 | 8 | 4 | 71 | 50 | 70 | 47 |
| Weight gain | 1 | 1 | 0 | 0 | 21 | 13 | 42 | 21 | 4 | 4 | 3 | 3 | 34 | 25 | 49 | 28 |
| Table of most commonly occurring adverse events split into two for formatting reasons. Events = number of adverse events reported; Ppts = number of participants reporting the adverse event (a participant could report the same type of adverse event multiple times). LTG = lamotrigine; CBZ = carbamazepine Most common adverse events are defined as events reported 10 or more times in at least one of the seven trials (Brodie 1995 A; Brodie 1995 B; Brodie 1999; Nieto‐Barrera 2001; Reunanen 1996; SANAD A 2007; Werhahn 2015). Less commonly reported adverse events are not summarised in this table but details are available on request from the review authors. General terminology for the type of adverse events was defined by the review authors based on the individual participant data provided. | ||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to treatment failure (any reason related to the treatment) Show forest plot | 9 | 2569 | Hazard Ratio (Fixed, 95% CI) | 0.73 [0.64, 0.82] |
| 2 Time to treatment failure due to adverse events Show forest plot | 9 | 2569 | Hazard Ratio (Fixed, 95% CI) | 0.54 [0.45, 0.65] |
| 3 Time to treatment failure due to lack of efficacy Show forest plot | 5 | 1874 | Hazard Ratio (Fixed, 95% CI) | 1.03 [0.75, 1.41] |
| 4 Time to treatment failure (any reason related to the treatment) ‐ by seizure type Show forest plot | 9 | 2481 | Hazard Ratio (Fixed, 95% CI) | 0.71 [0.62, 0.82] |
| 4.1 Focal | 9 | 2182 | Hazard Ratio (Fixed, 95% CI) | 0.74 [0.64, 0.86] |
| 4.2 Generalised | 6 | 299 | Hazard Ratio (Fixed, 95% CI) | 0.51 [0.33, 0.78] |
| 5 Time to treatment failure due to adverse events ‐ by seizure type Show forest plot | 9 | 2466 | Hazard Ratio (Fixed, 95% CI) | 0.55 [0.45, 0.66] |
| 5.1 Focal | 9 | 2182 | Hazard Ratio (Fixed, 95% CI) | 0.56 [0.45, 0.68] |
| 5.2 Generalised | 5 | 284 | Hazard Ratio (Fixed, 95% CI) | 0.49 [0.27, 0.88] |
| 6 Time to treatment failure (any reason related to the treatment, with aggregate data) Show forest plot | 13 | 3391 | Hazard Ratio (Fixed, 95% CI) | 0.70 [0.63, 0.78] |
| 7 Time to treatment failure (any reason related to the treatment) ‐ subgroup analysis (blinding) Show forest plot | 13 | 3391 | Hazard Ratio (Fixed, 95% CI) | 0.70 [0.63, 0.78] |
| 7.1 Double‐blind | 6 | 1231 | Hazard Ratio (Fixed, 95% CI) | 0.65 [0.56, 0.75] |
| 7.2 Open‐label | 7 | 2160 | Hazard Ratio (Fixed, 95% CI) | 0.76 [0.65, 0.90] |
| 8 Time to first seizure Show forest plot | 9 | 2564 | Hazard Ratio (Fixed, 95% CI) | 1.22 [1.09, 1.37] |
| 9 Time to first seizure by seizure type Show forest plot | 9 | 2476 | Hazard Ratio (Fixed, 95% CI) | 1.26 [1.12, 1.41] |
| 9.1 Focal | 9 | 2177 | Hazard Ratio (Fixed, 95% CI) | 1.29 [1.14, 1.45] |
| 9.2 Generalised | 6 | 299 | Hazard Ratio (Fixed, 95% CI) | 0.98 [0.65, 1.48] |
| 10 Time to first seizure (with aggregate data) Show forest plot | 12 | 3216 | Hazard Ratio (Fixed, 95% CI) | 1.24 [1.12, 1.37] |
| 11 Seizure freedom (whole study) Show forest plot | 14 | 3760 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [1.04, 1.18] |
| 12 Time to 6‐month remission Show forest plot | 7 | 1793 | Hazard Ratio (Fixed, 95% CI) | 0.84 [0.74, 0.94] |
| 13 Time to 6‐month remission by seizure type Show forest plot | 7 | 1708 | Hazard Ratio (Fixed, 95% CI) | 0.86 [0.76, 0.97] |
| 13.1 Focal | 7 | 1454 | Hazard Ratio (Fixed, 95% CI) | 0.87 [0.77, 1.00] |
| 13.2 Generalised | 5 | 254 | Hazard Ratio (Fixed, 95% CI) | 0.78 [0.55, 1.11] |
| 14 Seizure freedom at 6 months Show forest plot | 14 | 3760 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.89, 1.03] |
| 15 Time to 12‐month remission Show forest plot | 2 | 988 | Hazard Ratio (Fixed, 95% CI) | 0.91 [0.77, 1.07] |
| 16 Time to 12‐month remission by seizure type Show forest plot | 2 | 988 | Hazard Ratio (Fixed, 95% CI) | 0.90 [0.76, 1.07] |
| 16.1 Focal | 2 | 894 | Hazard Ratio (Fixed, 95% CI) | 0.91 [0.77, 1.09] |
| 16.2 Uncertain | 1 | 94 | Hazard Ratio (Fixed, 95% CI) | 0.81 [0.47, 1.37] |
| 17 Time to 24‐month remission Show forest plot | 1 | 755 | Hazard Ratio (Fixed, 95% CI) | 1.00 [0.80, 1.25] |
| 18 Time to 24‐month remission by seizure type Show forest plot | 1 | 755 | Hazard Ratio (Fixed, 95% CI) | 1.03 [0.82, 1.30] |
| 18.1 Focal | 1 | 661 | Hazard Ratio (Fixed, 95% CI) | 1.06 [0.83, 1.35] |
| 18.2 Uncertain | 1 | 94 | Hazard Ratio (Fixed, 95% CI) | 0.86 [0.44, 1.67] |

