Добавление витамина А для предотвращения смертности, краткосрочной и долгосрочной заболеваемости у младенцев с очень низкой массой тела при рождении
Abstract
Background
Vitamin A is necessary for normal lung growth and the integrity of respiratory tract epithelial cells. Preterm infants have low vitamin A status at birth and this has been associated with an increased risk of developing chronic lung disease.
Objectives
To evaluate supplementation with vitamin A on the incidence of death or neonatal chronic lung disease and long‐term neurodevelopmental disability in very low birth weight (VLBW) infants compared with a control (placebo or no supplementation), and to consider the effect of the supplementation route, dose, and timing.
Search methods
For the original review and subsequent updates, we searched the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library), MEDLINE, Science Citation Index, and the Oxford Database of Perinatal Trials. The reference lists of relevant trials, paediatric and nutrition journals, and conference abstracts and proceedings were handsearched up to 2010.
For the 2016 update, we used the standard search strategy of the Cochrane Neonatal Review group to search the Cochrane Central Register of Controlled Trials (CENTRAL 2016, Issue 4), MEDLINE via PubMed (1 May 2016), EMBASE (1 May 2016), and CINAHL (1 May 2016). We also searched clinical trials' databases, conference proceedings, and the reference lists of retrieved articles for randomised controlled trials and quasi‐randomised trials.
Selection criteria
Randomised controlled trials comparing vitamin A supplementation with a control (placebo or no supplementation) or other dosage regimens in VLBW infants (birth weight ≤ 1500 grams or less than 32 weeks' gestation).
Data collection and analysis
Two review authors screened the search results, extracted data, and assessed the trials for risk of bias. Results were reported as risk ratios (RR), risk differences (RD), and number needed to treat to benefit (NNTB), all with 95% confidence intervals (CI). Trialists were contacted for additional data.
Main results
Eleven trials met the inclusion criteria. Ten trials (1460 infants) compared vitamin A supplementation with a control and one (120 infants) compared different regimens of vitamin A supplementation. Compared to the control group, vitamin A appeared to have a small benefit in reducing the risk of death or oxygen requirement at one month of age (typical RR 0.93, 95% CI 0.88 to 0.99; typical RD −0.05, 95% CI −0.10 to −0.01; NNTB 20, 95% CI 10 to 100; 6 studies, 1165 infants) and the risk of chronic lung disease (oxygen requirement) at 36 weeks' postmenstrual age (typical RR 0.87, 95% CI 0.77 to 0.99; typical RD −0.07, 95% CI −0.13 to −0.01; NNTB 11, 95% CI 6 to 100; 5 studies, 986 infants) (moderate‐quality evidence). There was a marginal reduction of the combined outcome of death or chronic lung disease (typical RR 0.92, 95% CI 0.84 to 1.01; typical RD −0.05, 95% CI −0.11 to 0.01; 4 studies, 1089 infants). Neurodevelopmental assessment of 88% of the surviving infants in the largest trial showed no difference between the groups at 18 to 22 months of age, corrected for prematurity (low‐quality evidence). There is no evidence to support different vitamin A dosing regimens. No adverse effects of vitamin A supplementation were reported, but it was noted that intramuscular injections of vitamin A were painful.
Authors' conclusions
Whether clinicians decide to utilise repeat intramuscular doses of vitamin A to prevent chronic lung disease may depend upon the local incidence of this outcome and the value attached to achieving a modest reduction in the outcome balanced against the lack of other proven benefits and the acceptability of the treatment. Information on long‐term neurodevelopmental status suggests no evidence of either benefit or harm from the intervention.
PICO
Резюме на простом языке
Добавление витамина А для предотвращения смертельных случаев, краткосрочных и долгосрочных болезней у младенцев с очень низкой массой тела при рождении
Вопрос обзора Могут ли добавки с витаминами А предотвратить смерть, хроническое поражение легких и развитие инвалидности, связанной с психомоторным развитием, в отдаленные сроки у младенцев с очень низкой массой тела по сравнению с контролем (плацебо или отсутствие добавок)?
Актуальность Витамин А представляет собой группу жирорастворимых соединений, используемых организмом для регуляции и стимуляции роста и дифференциации многих клеток, включая клетки сетчатки глаза и клетки, выстилающие дыхательные пути в легких. У недоношенных детей отмечается низкий уровень витамина А при рождении. Это может способствовать повышенному риску развития хронического заболевания легких и, следовательно, потребности в кислороде. Возможно, что дополнительное введение витамина А может уменьшить частоту осложнений, связанных с недоношенностью, включая аномалии развития сетчатки (ретинопатия), кровотечение в головном мозге (внутрижелудочковое кровоизлияние), а также воспалительное поражение кишечника (некротизирующий энтероколит), в том числе снижение частоты респираторных инфекций. Слишком большое количество витамина А в организме считается потенциально вредным, поскольку может повысить внутричерепное давление, а также вызвать изменения кожи, слизистых (травмы или повреждения) и рвоту.
Характеристика исследований В этот обзор были включены одиннадцать испытаний, в десяти сравнивали витамин А с контролем (плацебо или отсутствие добавок), и в одном испытании сравнивали различные схемы приема витамина А. Поиск подходящих испытаний был обновлен в мае 2016 года.
Результаты: По сравнению с контрольной группой, добавление витамина А младенцам с очень низким весом при рождении, по‐видимому, имеет небольшое преимущество в снижении риска смерти или потребности в кислороде в возрасте одного месяца, и риска хронического заболевания легких (потребность в кислороде) в постменструальном (постконцептуальном) возрасте 36 недель (доказательства умеренного качества). Наблюдалось незначительное уменьшение комбинированного исхода смерти или хронического заболевания легких (доказательства умеренного качества). Несмотря на статистически значимое уменьшение частоты развития хронического заболевания легких, эти данные согласуются как с значимым воздействием на хроническое заболевание легких, так и незначительным влиянием. Одно испытание, в котором исследовали психомоторный статус с 18 до 22 месяцев скорректированного возраста с учетом недоношенности, не было обнаружено доказательств пользы или вреда, связанного с добавлением витамина А по сравнению с контролем (доказательства низкого качества). Не сообщалось о побочных эффектах добавления витамина А, но было отмечено, что внутримышечные инъекции витамина А были болезненными.
Вывод Решают ли врачи применять повторные внутримышечные дозы витамина А для профилактики развития хронического заболевания легких может зависеть от локальной распространенности этого исхода и ценности для достижения умеренного снижения частоты исхода, сбалансированного от отсутствия других доказанных преимуществ и приемлемости лечения. Данные о психомоторном статусе в отдаленные сроки не свидетельствует о наличии каких‐либо преимуществ или вреда от вмешательства.
Authors' conclusions
Summary of findings
| Supplemental vitamin A compared to no supplementation in very low birth weight infants | ||||||
| Patient or population: very low birth weight infants | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| no supplementation | Supplemental vitamin A | |||||
| Neonatal death | 168 per 1000 | 144 per 1000 | RR 0.86 | 1165 | ⊕⊕⊕⊝ | Imprecision: 95% CI are wide and imprecise |
| Chronic lung disease (oxygen use at 28 days in survivors) | 725 per 1000 | 674 per 1000 | RR 0.93 | 1070 | ⊕⊕⊕⊕ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Death or chronic lung disease (oxygen use at 28 days) | 798 per 1000 | 742 per 1000 | RR 0.93 | 1165 | ⊕⊕⊕⊕ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Death before 36 weeks' postmenstrual age | 168 per 1000 | 168 per 1000 | RR 1.00 | 1089 | ⊕⊕⊕⊝ | Imprecision: 95% CI are wide and imprecise |
| Chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors) | 546 per 1000 | 486 per 1000 | RR 0.87 | 986 | ⊕⊕⊕⊝ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Death or chronic lung disease (oxygen use at 36 weeks' postmenstrual age) | 622 per 1000 | 573 per 1000 | RR 0.92 | 1089 | ⊕⊕⊕⊝ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Neurodevelopmental impairment at 18 to 22 months | 481 per 1000 | 428 per 1000 | RR 0.89 | 538 | ⊕⊕⊝⊝ | Concerning imprecision: does not met the optimal information size criteria |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Imprecision: 95% CI are wide and imprecise 2 Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect 3 Concerning imprecision; does not met the optimal information size criteria | ||||||
Background
Description of the condition
Vitamin A is the generic name for a group of fat‐soluble compounds which have the biological activity of the primary alcohol retinol. Vitamin A is involved in the regulation and promotion of growth and differentiation of many cells and in maintaining the integrity of the epithelial cells of the respiratory tract. Vitamin A is also necessary for formation of the photosensitive visual pigment in the retina, reproductive functions, and immunocompetence. Carotenoids, dietary precursors of vitamin A, have antioxidant properties.
The foetus accumulates vitamin A in the third trimester. The transport mechanism of vitamin A across the placenta and its regulation are not fully established. Premature infants have reduced hepatic stores of retinyl ester. In the plasma, vitamin A is bound to a specific carrier protein, retinol‐binding protein (RBP), and the resulting complex is further complexed with transthyretin (formerly pre‐albumin) (Mactier 2005). Premature infants have lower concentrations of plasma RBP than term infants, and most preterm infants have low plasma vitamin A concentrations and low plasma retinol/RBP molar ratios, suggesting they are vitamin A deficient (Shenai 1993). Inadequate provision and delivery of vitamin A postnatally may exacerbate the problem.
Description of the intervention
Preterm infants who are unable to tolerate oral feeds are routinely fed parenterally with both an amino acid and dextrose mixture and a lipid emulsion. Multivitamin preparations containing retinol or an equivalent are commonly added to the amino acid and dextrose mixture and infused over 24 to 48 hours, but significant losses in delivered vitamin A have been shown to result from light degradation and from adsorption to the tubing. Alternatively, the multivitamins may be added to the lipid infusate (Greene 1987). Kennedy 1997 demonstrated improved serum retinol concentrations following intramuscular injections given three days per week. This route of administration has been adopted in several recent studies. In preterm infants who are able to tolerate enteral feeds, the absorption of enteral vitamin A by the immature gut may be poor.
An 'adequate' concentration of plasma vitamin A in very low birth weight (VLBW) infants is not known. Concentrations below 200 μg/L (0.70 μmol/L) have been considered deficient in premature infants, and concentrations below 100 μg/L (0.35 μmol/L) indicate severe deficiency and depleted liver stores. Both the plasma RBP response (Shenai 1990) and the relative rise in serum retinal concentration (Zachman 1996) following intramuscular vitamin A administration have been described as useful tests to assess functional vitamin A status. However, in a recent review Mactier 2005 concluded that the relationship between measures of vitamin A concentration and functional vitamin A status is not clear in preterm infants.
Vitamin A deficiency in laboratory animals produces a sequence of histopathological changes in the respiratory tract epithelium including necrotising tracheobronchiolitis and squamous metaplasia. These changes can be reversed by restoration of an adequate vitamin A status. Similar changes are observed in ventilated infants with chronic neonatal lung injury, leading to the suggestion that vitamin A deficiency may contribute to such injury and supplementation with vitamin A may facilitate healing and recovery (Chytil 1992; Shenai 1993). Two earlier studies reported that VLBW infants who developed chronic lung disease had lower concentrations of vitamin A than similar infants without chronic lung disease (Hustead 1984; Shenai 1985), although other studies from an era when all infants received more adequate supplementation have given conflicting results (Chabra 1994; Spears 2004).
How the intervention might work
In the 1920s, vitamin A was considered to be an anti‐infective agent. There is increasing evidence that vitamin A does have a role in immune function (Bates 1995). Several studies in areas of the world where there is generally poor nutritional status have suggested vitamin A supplementation in infancy may be associated with decreased mortality and morbidity. In infants in Indonesia, Humphrey 1996 reported that a single dose of 52 μmol (50,000 IU) given orally to term infants at birth reduced infant mortality and the prevalence of severe respiratory infections compared with placebo. A Cochrane review concluded that two oral doses of 200,000 IU in children under two years of age with measles was associated with a reduced risk of overall mortality and of pneumonia‐specific mortality (Huiming 2005).
Vitamin A has a role early in gestation in the development of the cardiovascular system (Mactier 2005). Animal models suggest higher vitamin A concentrations may accelerate postnatal constriction of the ductus arteriosus. The possibility that vitamin A supplementation may ameliorate other complications of prematurity, including retinopathy, intraventricular haemorrhage, and necrotising enterocolitis, has been suggested by a number of authors, although the basis for any effect is not clearly established.
Vitamin A is potentially toxic and raised intracranial pressure and vomiting have been described in infants receiving large doses. In children and adults, chronic hypervitaminosis A may include bone and joint pain, mucocutaneous lesions, and hepatic dysfunction, but the syndrome has not been recognised in preterm infants.
Why it is important to do this review
Although a role for vitamin A in neonatal chronic lung disease is not in doubt, uncertainty exists regarding the efficacy of supplementation and whether additional benefit may be obtained by achieving concentrations beyond sufficiency.
This is an update of previous versions of this Cochrane Review (Darlow 1998; Darlow 2000; Darlow 2002; Darlow 2007; Darlow 2011).
Objectives
To evaluate supplementation with vitamin A on the incidence of death or neonatal chronic lung disease and long‐term neurodevelopmental disability in very low birth weight (VLBW) infants compared with a control (placebo or no supplementation), and to consider the effect of the supplementation route, dose, and timing.
Methods
Criteria for considering studies for this review
Types of studies
Randomised and quasi‐randomised controlled trials.
Types of participants
Very low birth weight (VLBW) infants (defined as birth weight ≤ 1500 grams or less than 32 weeks' gestation).
Types of interventions
-
Vitamin A supplementation compared with control (placebo or no supplementation)
-
Different vitamin A supplementation dosage regimens
Types of outcome measures
Primary outcomes
-
Death (at 28 days and at hospital discharge)
-
Chronic lung disease (defined as oxygen use at 28 days or at 36 weeks' postmenstrual age)
-
Death or chronic lung disease (defined as oxygen use at 28 days or at 36 weeks' postmenstrual age)
Secondary outcomes
-
Vitamin A concentration (for studies comparing vitamin A dosage)
-
Nosocomial infection
-
Patent ductus arteriosus*
-
Necrotising enterocolitis*
-
Intraventricular haemorrhage (any intraventricular haemorrhage or severe intraventricular haemorrhage grades 3 and 4) (Papile 1978)*
-
Periventricular leukomalacia*
-
Retinopathy of prematurity (any, or requiring laser therapy)**
-
Neurodevelopment at 18 to 24 months
-
Death at 18 to 24 months**
-
Death or neurodevelopmental impairment at 18 to 24 months**
-
Adverse effects, including manifestations of hypervitaminosis A, particularly raised intracranial pressure and mucocutaneous lesions
*Additional secondary outcomes added in the 2010 update
** Additional secondary outcomes added in the 2016 update
Search methods for identification of studies
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal Group search strategy for specialized register).
Electronic searches
We conducted a comprehensive search including: the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library, Issue 4, 2016; MEDLINE via PubMed (1966 to 1 May 2016); EMBASE (1980 to 1 May 2016); CINAHL (1982 to 1 May 2016). We used the following search terms: (vitamin A or retinol), plus database‐specific limiters for RCTs and neonates (see Appendix 1 for the full search strategies for each database).
We applied no language restrictions. We searched the reference lists of any articles selected for inclusion in this review in order to identify additional relevant articles.
Searching other resources
We handsearched issues of paediatric and nutritional journals and abstracts from the Pediatric Academic Societies' Annual Meeting from 2002 to 2010. We also searched for conference abstracts from Pediatric Academic Societies (PAS) and the European Society for Paediatric Research (ESPR). Searches were carried out in Abstracts to View (2000 to 2014) and Pediatric Reseach.
We searched clinical trials registries for ongoing or recently completed trials (clinicaltrials.gov; the World Health Organization’s International Trials Registry and Platform www.whoint/ictrp/search/en/; and the ISRCTN Registry) without date limits up to May 2016.
Data collection and analysis
Selection of studies
We included all trials fulfilling the review's selection criteria. We cited all identified articles and made the decision regarding inclusion or exclusion of the studies by consensus. In the event of disagreements, we sought the opinion of a third party (Figure 1).

Study flow diagram: review update
Data extraction and management
For each included study, we collected information regarding the method of randomisation, blinding, drug intervention, stratification, trial location, and whether the trial was conducted at a single centre or multiple centres. We also collected information regarding inclusion criteria, including gestational age and postnatal age at the time of treatment. The list of data extraction fields for the trial interventions and outcomes are shown in Appendix 2.
We completed data collection sheets before comparing them and resolving any discrepancies by referring to the original sources. For each study, one review author entered the final and agreed data into Review Manager 5 and a second review author checked the data. We referred to a third party to resolve any disagreements.
Assessment of risk of bias in included studies
For the 2010 and 2016 updates, one author assessed the risk of bias in the included studies according to the methods in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This built on the previous version's assessment of the methodological quality of the included studies. Any uncertainties were resolved through discussion with a second author.
We assessed the following factors and judged them as having a high, low, or unclear risk of bias using the criteria in Higgins 2011:
-
Sequence generation (checking for possible selection bias)
-
Allocation concealment (checking for possible selection bias)
-
Blinding (checking for possible performance bias and detection bias)
-
Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
-
Selective outcome reporting (whether all of the study’s pre‐specified outcomes were reported (by checking the trial protocol if available) or whether the study failed to include results of a key outcome that would have been expected to have been reported)
-
Other biases (including source of funding and sample size calculation)
For each item, and where possible, we have provided a supporting quotation from the trial article.
Measures of treatment effect
We conducted separate analyses for each of the following outcomes: neonatal death; chronic lung disease; retinopathy of prematurity; sepsis (one or more defined episodes); and neurodevelopmental disability. Since there were only a small numbers of deaths, we conducted analyses using the composite endpoints of neonatal chronic lung disease or death, and neurodevelopmental disability or death. All analyses were conducted on an intention‐to‐treat basis. We stratified the analyses by route of vitamin A administration.
For dichotomous outcomes, we analysed the effect of vitamin A supplementation via both the risk ratio (RR) and the risk difference (RD) with 95% confidence intervals (CI). From 1/RD we calculated the number need to treat to benefit (NNTB) or the number needed to treat for an additional harmful outcome (NNTH). For vitamin A concentrations the intention was to focus the analysis on the mean difference between the supplemented and control groups. We combined continuous data using the standardised mean difference (SMD) and 95% CI.
Assessment of heterogeneity
We assessed between‐study heterogeneity using the standard Chi² test and the I² statistic.
Data synthesis
We performed the meta‐analysis using Review Manager 5. We used the Mantel‐Haenszel method for estimates of the pooled RR and RD. For measured quantities we used the inverse variance method. We used the fixed‐effect model for all meta‐analyses.
Pooled estimates of the effects and corresponding 95% confidence interval of the outcomes of neonatal death, chronic lung disease (oxygen use at 28 days in survivors), death or chronic lung disease (oxygen use at 28 days), death before 36 weeks' postmenstrual age, chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors) and neurodevelopmental disability at 18 to 22 months are included in the 'Summary of findings' tables in which the summary of the assessment of the evidence found for each outcome is presented.
Quality of evidence
For the 2016 update, we used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the quality of evidence for the following (clinically relevant) outcomes: neonatal death; chronic lung disease at 28 days and 36 weeks' postmenstrual age; death or chronic lung disease at 28 days and 36 weeks' postmenstrual age; and neurodevelopmental impairment at 18 to 22 months.
Two authors independently assessed the quality of the evidence for each of the outcomes above. We considered evidence from randomised controlled trials as high quality but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias); consistency across studies; directness of the evidence; precision of estimates; and presence of publication bias. We used the GRADEpro‐GDT 2013 Guideline Development Tool to create a ‘Summary of findings’ table to report the quality of the evidence.
The GRADE approach results in an assessment of the quality of a body of evidence in one of four grades:
-
High: We are very confident that the true effect lies close to that of the estimate of the effect.
-
Moderate: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
-
Low: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
-
Very low: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Subgroup analysis and investigation of heterogeneity
If data were available, we planned subgroup analyses to address the effect of the route, dose, and timing of supplementation.
Sensitivity analysis
Where appropriate, we planned sensitivity analyses to explore the impact of the risk of bias assessments.
Results
Description of studies
Results of the search
We identified 21 potentially relevant trials of which 11 met the eligibility criteria (Shenai 1987; Papagaroufalis 1988; Pearson 1992; Bental 1994; Werkman 1994; Tyson 1999; Wardle 2001; Ambalavanan 2003; Ravishankar 2003; Mactier 2012; Kiatchoosakun 2014). Ten trials compared vitamin A with a control, while one trial compared three different vitamin A dosing regimens and had a primary outcome of serum retinol concentrations at 28 days (Ambalavanan 2003); see trial details in the 'Characteristics of included studies' table.
We excluded ten trials from the review (Aranda 1992; Landman 1992; Koo 1993; Robbins 1993; Rush 1994; Coutsoudis 1996; Coutsoudis 2000; Aurvag 2007; Longardt 2014; Schmiedchen 2016) (see 'Characteristics of excluded studies'). Robbins 1993 was not a randomised controlled trial. Coutsoudis 1996 and Coutsoudis 2000 enrolled low birth weight infants of less than 36 weeks' gestation and the primary outcome was the incidence of respiratory infections in the first year of life. Aurvag 2007 compared vitamin A supplementation using human milk fortifier with historical controls and did not report clinical outcomes. Four studies were studies of pharmacodynamics that reported vitamin A concentrations but not clinical outcomes (Aranda 1992; Landman 1992; Koo 1993; Rush 1994). The unpublished study by Aranda 1992 did not state the route of vitamin A supplementation and the reported vitamin A levels appeared to contain a decimal point error. Landman 1992 and Rush 1994 compared equivalent doses of vitamin A administered either enterally or intramuscularly. The data in Rush 1994 were only reported graphically. Koo 1993 compared three doses of vitamin A added to preterm formula, which were given for an unstated period of time.
Longardt 2014 was not a randomised controlled trial and reported on serum retinol, retinyl palmitate, total retinol‐binding protein 4 (RBP4), retinol‐unbound RBP4 (apo‐RBP4) and transthyretin concentrations. Clinically relevant outcomes were not reported.
Schmiedchen 2016 studied the impact of urinary retinol excretion on the serum retinol concentration of 63 VLBW infants treated with vitamin A (5000 IU intramuscular, 3 times/week for 4 weeks) compared to 38 untreated infants classified as control group. The groups were not randomised. See trial details in the Characteristics of excluded studies table.
Calisici 2014 is published only as an abstract and is awaiting further assessment. See trial details in the Characteristics of studies awaiting classification table.
Trial location and size
Most trials were conducted in the USA (Shenai 1987; Pearson 1992; Werkman 1994; Tyson 1999; Ambalavanan 2003; Ravishankar 2003). Three trials were conducted in Europe: in Greece (Papagaroufalis 1988); and the UK (Wardle 2001; Mactier 2012). One trial was conducted in South Africa (Bental 1994); and one trial was conducted in Thailand (Kiatchoosakun 2014).
Most trials included fewer than 100 infants (Shenai 1987; Papagaroufalis 1988; Pearson 1992; Bental 1994; Werkman 1994; Ravishankar 2003; Mactier 2012; Kiatchoosakun 2014). Two included between 100 and 200 participants (Wardle 2001; Ambalavanan 2003); and one trial included 807 infants (Tyson 1999).
Participants
Vitamin A versus control
The ten trials comparing vitamin A with a control reported outcomes for 1460 infants, 735 treated with vitamin A and 725 control infants.
Shenai 1987: Single centre randomised controlled trial. Enrolled 40 infants, birth weight 700 to 1300 grams and gestational age 26 to 30 weeks, requiring supplemental oxygen and mechanical ventilation for at least 72 hours in the first week; Caucasian infants only; birth weight appropriate for gestational age; no congenital abnormalities.
Papagaroufalis 1988: Single centre randomised controlled trial. Enrolled 55 infants with birth weight ≤ 1300 grams; gestation < 29 weeks; requirement for > 40% oxygen and mechanical ventilation for > 72 hours in first week.
Pearson 1992: Multicentre randomised controlled trial. Enrolled 49 infants with birth weight 700 to 1100 grams requiring supplemental oxygen and mechanical ventilation between 72 and 96 hours of age with previous cumulative duration of ventilation and oxygen > 48 hours. Infants with growth restriction (undefined), congenital or chromosomal abnormalities, hydrops fetalis, congenital infection, neonatal hepatitis or 'do not resuscitate' order were excluded.
Bental 1994: Single centre randomised controlled trial. Enrolled 60 infants with birth weight between 1000 and 1500 grams; gestational age of ≤ 34 weeks; infants were receiving supplemental oxygen and mechanical ventilation for at least 72 hours during the first week; no congenital anomalies or infection; black South African infants.
Werkman 1994: Single centre randomised controlled trial. Enrolled 86 infants with birth weight 725 to 1300 grams, age < 96 hours; no intraventricular or periventricular haemorrhage, history of maternal substance abuse, or sexually transmitted disease; no congenital anomalies.
Tyson 1999: Multicentre randomised controlled trial. Enrolled 807 infants with birth weight 401 to 1000 grams requiring supplemental oxygen or mechanical ventilation at 24 hours of age; and no major congenital anomalies, non‐bacterial infection, or terminal illness.
Wardle 2001: Multicentre randomised controlled trial. Enrolled 154 infants with birth weight < 1000 grams; no life‐threatening congenital abnormalities; consent before 24 hours of age.
Ravishankar 2003: Single centre randomised controlled trial. Enrolled 40 infants with birth weight 500 to 1500 grams; gestation < 32 weeks; having indwelling umbilical line; no major congenital malformations or chromosomal anomalies; and < 24 hours of age.
Mactier 2012: Double‐blind, randomised controlled trial conducted at three neonatal centres in Glasgow. Enrolled 89 infants (42 supplemented and 47 controls) < 32 weeks' gestation or < 1501 grams birth weight, or both.
Supplemented infants received additional intramuscular vitamin A 10,000 IU 3 times weekly from day 2 for a minimum of 2 weeks or until establishment of oral feeding.
Kiatchoosakun 2014: Randomised controlled trial to assess the effect of vitamin A supplementation for prevention of bronchopulmonary dysplasia in VLBW premature infants. Eighty premature infants weighing < 1500 grams who received mechanical ventilation or oxygen supplementation at 24 hours of age and admitted to Neonatal units of Srinagarind Hospital, Khon Kaen University, Khon Kaen, Thailand.
Vitamin A dosing regimens
Ambalavanan 2003: Single centre randomised controlled trial evaluating vitamin A dosage. Enrolled 120 infants, birth weight between 401 and 1000 grams; requiring mechanical ventilation or supplemental oxygen at 24 hours of age; and no major congenital anomalies, non‐bacterial infection, or terminal illness. Ambalavanan 2003 used the same entry criteria as Tyson 1999.
Interventions
Vitamin A versus control
Ten trials compared vitamin A with a control. All but Werkman 1994 and Wardle 2001 gave supplemental vitamin A (water‐soluble retinyl palmitate) by intramuscular injection soon after birth, usually day four, and over the next 28 days. The trials varied in the vitamin A dose and regimen.
Shenai 1987: Vitamin A (water‐soluble retinyl palmitate) versus control
Supplemental 2000 IU vitamin A by intramuscular injection alternate days from day 4 for a total of 14 injections (n = 20) compared to normal saline placebo (n = 20)
Other: both control and study infants received vitamin A 400 IU/dL in parenteral nutrition and 240 to 550 IU/dL from milk plus 1500 IU supplements when fed orally
Papagaroufalis 1988: Vitamin A (water‐soluble retinyl palmitate) versus control
Supplemental 4000 IU vitamin A intramuscular injection from day 4 to 6 on alternate days until extubated (n = 27) compared to normal saline placebo (n = 28).
Pearson 1992: Vitamin A (water‐soluble retinyl palmitate) versus control
Supplemental 2000 IU vitamin A by intramuscular injection alternate days from day 4 for 14 doses (n = 27) compared to normal saline placebo or mock injection (n = 22)
Other: both control and study infants received 1200 to 1500 IU/d vitamin A in protein‐dextrose solution when on parenteral nutrition; when fed orally all infants received vitamin A 250 to 1030 IU/100 mL milk; antenatal steroids received by 26% infants in the vitamin A group and 41% in the control group; > 90% received an artificial surfactant
Bental 1994: Vitamin A (water‐soluble retinyl palmitate) versus control
Supplemental 4000 IU vitamin A intramuscular injection 3 times a week from day 4 for a total of 12 injections (n = 31); no supplementation (n = 29)
Other: some control and study infants received vitamin A 1500 to 3000 IU after 1 week of age when fed orally
Werkman 1994: Vitamin A (retinyl palmitate) versus control
Supplemental vitamin A 80,000 RE/L (giving about 1300 to 3300 IU/kg/d) in intravenous lipid infused over 16 h from randomisation (48 to 96 hours) and while receiving parenteral nutrition (n = 44) compared to no supplementation (n = 42)
Other: both control and study infants received vitamin A as multivitamin preparation added to protein‐dextrose solution (birth weight < 1000 grams 1.5 mL/d, 210 RE/d; > 1000 grams 3.4 mL/d, 476 RE/d) and oral supplements when fed orally
Tyson 1999: Vitamin A (water‐soluble retinyl palmitate) versus control
Supplemental 5000 IU vitamin A intramuscular injection 3 times a week for 4 weeks (n = 405) compared to sham injection (n = 402)
Other: control and study infants received similar intakes of vitamin A from non‐study enteral and parenteral sources but amounts not stated; antenatal steroids received by 76% of infants in the vitamin A group and 74% in the control group; > 80% received a natural surfactant
Wardle 2001: Vitamin A (form not stated) versus control
Supplemental 5000 IU vitamin A orally daily until day 28 (n = 77) compared to same volume look‐alike placebo liquid (n = 77)
Other: control and study infants received 23 IU/kg/d vitamin A (stated amount but probably 233 IU) in intralipid when on parenteral nutrition; when on full enteral feeds and more than 14 days of age all infants received 5000 IU/kg/d vitamin A orally; antenatal steroids received by 77% in the vitamin A group and 82% in the control group; all but 1 infant in the control group received an artificial surfactant
Ravishankar 2003: Vitamin A (water‐miscible preparation of vitamin A (Aquasol A)) versus control
Supplemental 1500 to 3000 IU vitamin A (based on weight) by intramuscular injection on days 1, 3 and 7 (n = 22) compared to sham injection (n = 18)
Other: most infants received parenteral nutrition including 466 IU/dL vitamin A and an additional 1000 IU supplement when fed orally; antenatal steroids received by 86% of infants in the vitamin A group and 72% in the control group
Mactier 2012: Supplemented infants received additional intramuscular vitamin A 10,000 IU 3 times weekly from day 2 for a minimum of 2 weeks or until establishment of oral feeding.
Kiatchoosakun 2014: Infants were assigned to receive either intramuscular vitamin A 5000 IU 3 times/week (treatment group) or sham procedure (control group) for four weeks.
Study and control infants were also administered standard vitamin A. However, the amount of vitamin A in standard therapy, and hence received by the control groups, varied between studies. When on parenteral nutrition infants in Shenai 1987 received vitamin A 400 IU/100 mL of protein‐dextrose infusion and usually less than 700 IU/kg/d from all sources. Infants in Pearson 1992 received 1200 to 1500 IU/d of vitamin A in the protein‐dextrose solution. In Bental 1994, infants on parenteral nutrition received no vitamin A but some received 1500 to 3000 IU/d after one week when fed orally. In Papagaroufalis 1988, the amount of standard vitamin A was not stated. In Werkman 1994, standard vitamin A was added to the protein‐dextrose solution, with infants less than 1000 grams receiving 700 IU/d and infants more than 1000 grams receiving 1580 IU/d. In Tyson 1999, infants received approximately 700 IU/kg/d in the first week, principally in protein‐dextrose solution, and closer to 1000 IU/kg/d in weeks two to four from all sources (data estimated from a graph). Infants in Wardle 2001 were stated to receive 23 IU/kg/d added to intralipid when on parenteral nutrition (however, the standard UK dose at that time was 233 IU/kg/d and it was probable that infants in this study received this dose) and 5000 IU/kg/day orally when on full enteral feeds from the 14th postnatal day. In Ravishankar 2003, most infants on parenteral nutrition received 466 IU vitamin A added to 100 mL of the protein‐dextrose solution, and 1500 IU/d orally when fully enterally fed. In Mactier 2012, infants on parenteral nutrition received routine fat soluble vitamins as part of their lipid infusion (Vitlipid N). Lipid infusion was stopped once the infants had achieved 75% of their expected enteral intake and all infants received oral supplementation of vitamin A on day 14 of life if tolerating enteral feeds.
Vitamin A dosing regimens
Ambalavanan 2003: Infants were randomised to receive a standard vitamin A supplement by 5000 IU intramuscular injection of vitamin A on three days per week for four weeks (considered as the control group) (n=40), a higher dose of 10,000 IU on three days per week for four weeks (n = 40), or a once‐per‐week dose of 15,000 IU for four weeks (n = 40).
Outcomes
We contacted several trial authors for further details about the trial outcomes and data. Bental 1994 gave complete data, published in an earlier abstract from 1990, and we sought and obtained further clarification from the trial authors concerning two outcomes: oxygen use at one month in survivors; and death or oxygen use at one month. We were able to update the data of Papagaroufalis 1988 with information provided by the trial author to Dr K Kennedy at the time of an earlier review (Kennedy 1997). We obtained information on the age of infants at death from the corresponding author of Ravishankar 2003. Further information on the numbers examined for retinopathy of prematurity and numbers with any retinopathy in Wardle 2001 were provided by the trial author. We also received further information on the timing of death, numbers of infants having serum retinol estimations at 28 days, and any retinopathy of prematurity from the author of Ambalavanan 2003.
Vitamin A versus control
Shenai 1987: Death before 31 days, bronchopulmonary dysplasia (oxygen requirement or ventilation at 31 days plus characteristic chest x‐ray), total days' oxygen, episodes of sepsis, retinopathy of prematurity, and vitamin A levels.
Papagaroufalis 1988: Death before 31 days, bronchopulmonary dysplasia (oxygen requirement and characteristic chest x‐ray on day 31) and vitamin A levels. Unpublished data of Papagaroufalis 1988 were available for 28, 29, 30 and 31 days.
Pearson 1992: Death before 31 days, bronchopulmonary dysplasia (oxygen requirement at 31 days and characteristic chest x‐ray), oxygen requirement at 34 weeks' post‐conceptual age, retinopathy of prematurity, plasma vitamin A levels and retinyl binding protein at various times.
Bental 1994: Death before 31 days, bronchopulmonary dysplasia (oxygen or ventilation on day 31 and characteristic chest x‐ray; full data obtained from trial authors), culture‐proven sepsis, vitamin A levels at various times.
Werkman 1994: Bronchopulmonary dysplasia (oxygen beyond 28 days and characteristic chest x‐ray, total days' oxygen requirement, vitamin A and retinol‐binding protein levels at various times.
Tyson 1999: Oxygen requirement at, or death before, 36 weeks' postmenstrual age; oxygen requirement at, or death before, 28 days of age; culture‐proven sepsis; grade 3 or 4 intracranial haemorrhage; periventricular leukomalacia; vitamin A on study day 28 in subset of infants and relative dose‐response to 2000 IU vitamin A intramuscular. Examination for potential toxicity weekly. Assessment of neurodevelopmental status at 18 to 22 months' corrected age is available in Ambalavanan 2005 (companion paper for Tyson 1999). Additional subgroup analysis of 'small for gestational age' infants.
Wardle 2001: Oxygen requirement at 28 days, death pre‐discharge, oxygen requirement at 36 weeks' postmenstrual age, retinopathy of prematurity requiring treatment. Wardle 2001 also reported on a patent ductus arteriosus requiring treatment with indomethacin or surgical closure, but the timing of this was uncertain as to whether some infants had died before this outcome; hence we did not include these data.
Ravishankar 2003: Failure of patent ductus arteriosus closure, defined as patent ductus arteriosus larger than trivial on day 14, indomethacin treatment, or surgical ligation. Ravishankar 2003 also reported deaths (and further information on the timing of these was obtained from the trial authors) and oxygen requirement at 36 weeks' postmenstrual age.
Mactier 2012: Hepatic stores were assessed by relative dose response (RDR). The primary outcome measure was cone‐corrected dark‐adapted retinal rod sensitivity measured by electroretinogram at 36 weeks' postmenstrual age (PMA). Complications of prematurity were reported including use of respiratory support, intraventricular haemorrhage, retinopathy of prematurity, supplemental oxygen at 36 weeks' postmenstrual age, and death
Kiatchoosakun 2014: The investigators reported on serum vitamin A levels, and complications of prematurity including supplemental oxygen at 36 weeks postmenstrual age, duration of intubation, days on oxygen therapy, and length of hospital stay.
Vitamin A dosing regimens
The primary outcome measure for the trial by Ambalavanan 2003 was serum retinol concentrations in μg/L at 28 days. Ambalavanan 2003 also reported on death before 36 weeks' postmenstrual age, oxygen requirement at or death before 36 weeks' postmenstrual age, and threshold retinopathy of prematurity. We obtained further information on timing of death, numbers of infants having serum retinol estimations, and any retinopathy of prematurity from the trial authors.
Risk of bias in included studies
Full details of the 'Risk of bias' assessment are available by trial in the 'Assessment of risk of bias in included studies' tables and are summarised in Figure 2.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Of the 11 included trials, eight used adequate methods to generate the allocation sequence and seven used adequate methods to conceal allocation (low risk of bias). Papagaroufalis 1988 and Werkman 1994 did not provide details to allow this risk of bias component to be assessed, and Bental 1994 provided details only for the sequence generation method (computer‐generated random numbers).
Ambalavanan 2003 used shuffled blocks of sealed opaque envelopes for randomisation and stratified randomisation by birth weight. The randomisation and allocation for Pearson 1992, Ravishankar 2003, Shenai 1987, Mactier 2012, Kiatchoosakun 2014 and Wardle 2001 were conducted by someone outside of the trial team and used sealed envelopes.
Blinding
Six trials blinded participants to the intervention and outcome assessors (Shenai 1987; Pearson 1992; Tyson 1999; Wardle 2001; Mactier 2012; Kiatchoosakun 2014). Pearson 1992, for example, used opaque tape to conceal the contents of the syringes and reported that the “staff responsible for patient care had no knowledge of group designation”.
Incomplete outcome data
All but Werkman 1994 and Papagaroufalis 1988 had complete follow‐up of participants. Werkman 1994 did not report outcomes on all infants entered into the study as they excluded 10 who transferred to another centre for surgery and two who died, for whom group assignment was not stated. For Papagaroufalis 1988, no information was available in the study abstract.
Selective reporting
Most trials were free of selective reporting in that it was clear that all of the trial’s pre‐specified outcome measures and all expected outcome measures of interest to the review were reported. This was unclear for Papagaroufalis 1988 because only a study abstract (from a conference proceedings) was available, while Werkman 1994 did not report all outcome measures of interest.
Other potential sources of bias
This item was evaluated in relation to information about trial funding (such as industry funding) and sample size calculation. Tyson 1999 appeared to be free of these sources of bias because the study protocol was described in detail, including the sample size calculation, and the trial was free of industry funding. Mactier 2012 was funded by the Chief Scientific Office, Scotland, and appeared to be free of other potential sources of bias. Papagaroufalis 1988 and Pearson 1992 were assessed as having a high risk of bias for this component: Papagaroufalis 1988 because little information was available in the abstract; and Pearson 1992 because few of the eligible infants were enrolled in the trial. Information about this item for the 'Risk of bias' assessment was unclear in the other studies.
Effects of interventions
Comparison 1: Supplemental vitamin A versus no supplementation
Neonatal death (Outcome 1.1)
Six trials reported on neonatal death (Shenai 1987; Papagaroufalis 1988; Pearson 1992; Bental 1994; Tyson 1999; Wardle 2001); none showed a significant difference between the vitamin A and control groups. The meta‐analysis does not support a reduction of the risk of neonatal death associated with receiving vitamin A (typical RR 0.86, 95% CI 0.66 to 1.11; typical RD −0.02, 95% CI −0.06 to 0.02; 1165 infants) (Analysis 1.1; Figure 3).The quality of evidence for this outcome is moderate because of imprecision of estimates of effect (summary of findings Table for the main comparison).

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.1 Death (before 1 month).
Chronic lung disease (oxygen use at 28 days in survivors) (Outcome 1.2)
Seven trials (the six trials above plus Werkman 1994) reported on chronic lung disease at 28 days. Only one study (Shenai 1987) reported a statistically significant difference between intervention groups. The largest trial showed an important trend to no differences between treatment arms (RR 0.97, 95% CI 0.89 to 1.06; 718 infants) (Tyson 1999). The meta‐analysis of these seven studies showed a trend towards a reduced risk of chronic lung disease between treatment arms (typical RR 0.93, 95% CI 0.86 to 1.01; typical RD −0.05, 95% CI −0.10 to 0.00; 1070 infants) (Analysis 1.2; Figure 4). The overall quality of the evidence for this outcome was judged as moderate; we downgraded the quality of evidence based upon imprecision because although the 95% CI for the typical RR is narrow the result is consistent with minimal clnical effect.

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.2 Chronic lung disease (oxygen use at 28 days in survivors).
Death or chronic lung disease (oxygen use at 28 days) (Outcome 1.3)
Data for the combined outcome of death or chronic lung disease at 28 days were available in six trials (Shenai 1987; Papagaroufalis 1988; Pearson 1992; Bental 1994; Tyson 1999; Wardle 2001). Only one study reported a statistically significant difference in this outcome (Shenai 1987). When the meta‐analysis was confined to the five trials reporting on supplementation via intramuscular injection (excluding Wardle 2001) there was a trend towards a reduction in death or oxygen use at one month that was of borderline statistical significance (typical RR 0.93, 95% CI 0.86 to 1.00; typical RD −0.06, 95% CI −0.11 to −0.00; NNTB 17, 95% CI 9 to 1000+; 1011 infants) (Analysis 1.3). When Wardle 2001 (in which oral vitamin A supplementation was given to treated infants) was included in the meta‐analysis the pooled data showed a significant reduction in this outcome (typical RR 0.93, 95% CI 0.88 to 0.99; typical RD −0.05, 95% CI −0.10 to −0.01; NNTB 20, 95% CI 10 to 100; 1165 infants, I² = 37%) (Analysis 1.3; Figure 5). The overall quality of the evidence for this outcome was judged as moderate; we downgraded the quality of evidence based upon imprecision because although the 95% CI for the typical RR is narrow the result is consistent with minimal clnical effect.

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.3 Death or chronic lung disease (oxygen use at 28 days).
Death (before 36 weeks' postmenstrual age) (Outcome 1.4)
Four trials reported on this outcome (Tyson 1999; Wardle 2001; Ravishankar 2003; Mactier 2012). Kiatchoosakun 2014 reported "death before discharge" (but not at 36 weeks' PMA) and therefore is not included in this analysis. The polled estimate of the effect showed no significant differences between the vitamin A and control groups (typical RR 1.00, 95% CI 0.77 to 1.29; 1089 infants) (Analysis 1.4; Figure 6). The overall quality of the evidence for this outcome is moderate because of imprecision in estimates.
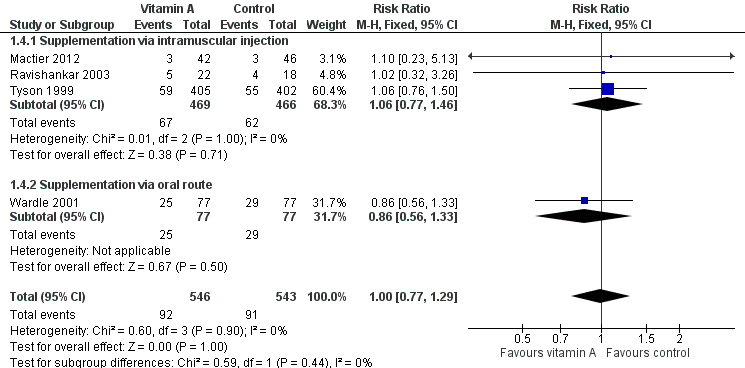
Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.4 Death before 36 weeks' postmenstrual age.
Chronic lung disease (oxygen use at 36 weeks' postmenstrual age) (Outcome 1.5)
Five trials reported on this outcome (Tyson 1999; Wardle 2001; Ravishankar 2003; Mactier 2012; Kiatchoosakun 2014). Tyson 1999 reported a marginal reduction in oxygen use at 36 weeks postmenstrual age in the vitamin A group (RR 0.85, 95% CI 0.73 to 0.98; RD −0.09, 95% CI −0.16 to −0.01; NNTB 11, 95% CI 6 to 100; 693 infants).
Similar results are seen in the pooled analysis, with a small beneficial effect of vitamin A on the risk of chronic lung disease at 36 weeks' postmenstrual age (typical RR 0.87, 95% CI 0.77 to 0.99; typical RD −0.07, 95% CI −0.13 to −0.01; NNTB 14, 95% CI 8 to 100; 986 infants) (Analysis 1.5; Figure 7). The overall quality of the evidence for this outcome was judged as moderate; we downgraded the quality of evidence based upon imprecision because although the 95% CI for the typical RR is narrow the result is consistent with minimal clnical effect.

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.5 Chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors).
Death or chronic lung disease (Oxygen use at 36 weeks' postmenstrual age) (Outcome 1.6)
Four trials reported on this outcome (Tyson 1999; Wardle 2001; Ravishankar 2003; Mactier 2012). Tyson 1999 showed a trend towards reduction in death or chronic lung disease in the vitamin A group that was of borderline statistical significance (RR 0.89, 95% CI 0.79 to 1.00; RD −0.07, 95% CI −0.14 to 0.00). Pooling the data from the four trials did not meaningfully alter this finding (typical RR 0.92, 95% CI 0.84 to 1.01; typical RD −0.05, 95% CI −0.11 to 0.01; 1089 infants) (Analysis 1.6). Including the outcome data at 34 weeks' postmenstrual age from Pearson 1992 in this analysis, there was essentially no difference to these results. The overall quality of the evidence for this outcome was judged as moderate; we downgraded the quality of evidence based upon imprecision because although the 95% CI for the typical RR is narrow the result is consistent with minimal clnical effect.
Death (at 18 to 24 months) (Outcome 1.7)
Tyson 1999 reported on this outcome and found no significant difference between the vitamin A and control groups (RR 0.95, 95% CI 0.71 to 1.27; RD −0.01, 95% CI −0.06 to 0.04; 807 infants (Analysis 1.7).
Neurodevelopmental impairment at 18 to 24 months (Outcome 1.8)
Ambalavanan 2005 followed up 88% of the surviving infants who participated in the Tyson 1999 trial at 18 to 22 months corrected age. Forty‐one infants could not be assessed, leaving 290 infants in the intervention group and 289 in the control group (15% lost to follow‐up in both groups). There was no difference between the groups in either neurodevelopment impairment, defined as one or more of: Bayley II Mental Index less than 70, Psychomotor Index less than 70, any cerebral palsy, blind in both eyes, or bilateral hearing aids (RR 0.89, 95% CI 0.74 to 1.08; RD −0.05, 95% CI −0.04 to 0.03; 1538 infants) (Analysis 1.8). The overall quality of the evidence for this outcome is moderate because of imprecision in estimates.
Death or neurodevelopmental impairment at 18 to 24 months (Outcome 1.9)
Tyson 1999 reported on this outcome and found no significant differences between the vitamin A and control groups (RR 0.92, 95% CI 0.81 to 1.05; RD −0.05, 95% CI −0.12 to 0.03; 687 infants) (Analysis 1.9).
Patent ductus arteriosus (Outcome 1.10)
Ravishankar 2003 found no significant difference in the failure of ductal closure or treatment by day 14 between the vitamin A and control groups (RR 0.98, 95% CI 0.56 to 1.72; RD −0.01, 95% CI −0.32 to 0.30; 40 infants) (Analysis 1.10).
Kiatchoosakun 2014 reported on any evidence of PDA diagnosed by echocardiography but did not report rates of treatment between the two groups.
Sepsis (Outcome 1.11)
Three trials reported on one or more episodes of culture‐proven nosocomial sepsis (Bental 1994; Tyson 1999; Kiatchoosakun 2014). The pooled data showed a non‐significant trend towards a reduction in sepsis in the vitamin A group (typical RR 0.89, 95% CI 0.76 to 1.04; typical RD −0.05, 95% CI −0.11 to 0.01; 947 infants) (Analysis 1.11).
Necrotising enterocolitis (Outcome 1.12)
Four trials reported on necrotising enterocolitis (Bental 1994; Tyson 1999; Wardle 2001; Kiatchoosakun 2014); and the pooled data showed no significant difference between the vitamin A and control groups (typical RR 0.92, 95% CI 0.67 to 1.27; typical RD −0.01, 95% CI −0.05 to 0.03; 1101 infants) (Analysis 1.12).
Intraventricular haemorrhage (Outcome 1.13)
Three trials reported on any intraventricular haemorrhage (Bental 1994; Tyson 1999; Ravishankar 2003). The pooled data found no significant difference between the vitamin A and control groups (typical RR 0.95, 95% CI 0.82 to 1.10; typical RD −0.02, 95% CI −0.09 to 0.04; 907 infants) (Analysis 1.13).
Four of the trials also reported on severe intraventricular haemorrhage (Bental 1994; Tyson 1999; Mactier 2012; Kiatchoosakun 2014). There was no significant difference between the vitamin A and control groups (typical RR 0.95, 95% CI 0.72 to 1.25; typical RD −0.01, 95% CI −0.05 to 0.04; 1035 infants) (Analysis 1.13).
Periventricular leukomalacia (Outcome 1.14)
Tyson 1999 reported on this outcome and found no significant differences in periventricular leukomalacia between the vitamin A and control groups (RR 0.74, 95% CI 0.44 to 1.25; RD −0.01, 95% CI −0.05 to 0.03; 646 infants) (Analysis 1.14).
Retinopathy of prematurity (Outcome 1.15)
Three trials reported on this outcome (Shenai 1987; Pearson 1992; Kiatchoosakun 2014). Additional data was obtained from the trial author of Wardle 2001. Shenai 1987 and Kiatchoosakun 2014 noted a trend to reduced incidence of retinopathy of prematurity in the vitamin A group; this was reflected in the pooled trial data (typical RR 0.81, 95% CI 0.65 to 1.01; typical RD −0.10, 95% CI −0.20 to 0.00; 255 infants)(Analysis 1.15).
Retinopathy of prematurity requiring laser therapy (Outcome 1.16)
Two trials reported on retinopathy of prematurity requiring laser therapy (Wardle 2001; Mactier 2012). No difference was seen in the risk of retinopathy of prematurity requiring laser therapy (typical RR 1.27, 95% CI 0.55, 2.94; 236 infants).
Adverse effects
The studies by Bental 1994, Papagaroufalis 1988, and Ravishankar 2003 make no comment on monitoring for adverse effects. Shenai 1987 noted that clinical monitoring for toxicity included periodic anterior fontanelle pressure assessment to detect raised intracranial pressure and reported no clinical or biochemical evidence of toxicity. Pearson 1992 reported that intramuscular injections of vitamin A were painful, and both this trial and Werkman 1994 found no evidence of biochemical toxicity. Wardle 2001 noted that the incidence of potential adverse effects, seizures, and persistent vomiting did not differ between the groups. Infants in Tyson 1999 were independently assessed for signs of toxicity on a weekly basis; a suspected or definite increase in fontanelle tension was slightly more frequent in control than supplemented infants (18% versus 15%, P = 0.26), and potential toxicity unexplained by other factors occurred in 0.8% controls and 1.0% supplemented infants.
Vitamin A dosing regimens
Comparison 2: Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 × week for 4 weeks
Comparison 3: Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks
Ambalavanan 2003 compared a 'standard' intramuscular regimen of supplemental vitamin A (5000 IU 3 × per week for 4 weeks) as used in Tyson 1999, with a higher dose (10,000 IU 3 × per week for 4 weeks) and with a once‐per‐week dose (15,000 IU weekly for 4 weeks). The vitamin A was given intramuscularly, and the trial's primary outcome was the serum retinol concentration at 28 days
Death before 36 weeks' postmenstrual age (Outcomes 2.1 and 3.1)
There was no significant difference for this outcome between the higher‐ and standard‐dose groups (80 infants) (Analysis 2.1), or between the once‐a‐week and standard regimens (80 infants) (Analysis 3.1).
Oxygen use at 36 weeks' postmenstrual age in survivors (Outcomes 2.2 and 3.2)
There was no significant difference for this outcome between the higher‐ and standard‐dose groups (61 infants) (Analysis 2.2), or between the once‐a‐week and standard regimens (61 infants, Analysis 3.2).
Death or oxygen use at 36 weeks' postmenstrual age (Outcomes 2.3 and 3.3)
There was no significant difference for this outcome between the higher‐ and standard‐dose groups (80 infants) (Analysis 2.3), or between the once‐a‐week and standard regimens (80 infants, Analysis 3.3).
Vitamin A concentration (retinol) (Outcomes 2.4, 2.5, 3.4 and 3.5)
There was no significant difference between the standard dose and higher dose for this outcome when measured as retinol (μg/L) on study day 28 (55 infants) (Analysis 2.4) or as retinol (< 200 μg/L) on day 28 (%) (55 infants) (Analysis 2.5).
The once‐per‐week regimen resulted in significantly lower concentrations than the standard regimen on study day 28 (SMD −0.97, 95% CI ‐1.56 to −0.38; 50 infants (Analysis 3.4). The once‐per‐week dose regimen also resulted in a higher proportion of infants with 28‐day retinol concentrations below 200 μg/L (RR 2.52, 95% CI 1.24 to 5.09; 50 infants) (Analysis 3.5)
Necrotising enterocolitis (Outcome 2.6 and 3.6)
There were no significant differences for this outcome between the higher‐ and standard‐dose groups (80 infants) (Analysis 2.6) or between the once‐a‐week and standard regimens (80 infants) (Analysis 3.6).
Retinopathy of prematurity (Outcomes 2.7, 2.8, 3.7 and 3.8)
There was a trend to fewer infants with retinopathy of prematurity in the higher‐dose group compared to the standard‐dose group, for both any grade (63 infants)(Analysis 2.7) and threshold disease (63 infants)(Analysis 2.8).
When we compared the once‐a‐week regimen with the standard regimen there was a trend to fewer infants with retinopathy of prematurity for any grade (64 infants) (Analysis 3.7) but there was no significant difference between the groups when measured as threshold disease (64 infants) (Analysis 3.8).
For both analyses, only small numbers of infants were involved and the trial lacked power to assess this outcome.
Sepsis (Outcomes 2.9 and 3.9)
There were no significant differences in the number of episodes of sepsis between the higher‐ and standard‐dose groups (80 infants) (Analysis 2.9) or between the once‐a‐week and standard regimens (80 infants) (Analysis 3.9).
Vitamin A concentration
The data did not allow a quantitative analysis of vitamin A concentrations among survivors.
Adverse effects
Ambalavanan 2003 monitored for potential adverse effects. One infant in the higher‐dose group was noted to have transient fullness of the anterior fontanelle without other causes and which resolved in 48 hours.
Discussion
This Cochrane review includes 11 randomised controlled trials, ten comparing vitamin A with placebo and one comparing different vitamin A regimens. Tyson 1999 is the largest trial included in the review with a sample size (807 infants) more than five times that of the next largest trial (154 infants, Wardle 2001).
The first version of this review reported a significant reduction in death or oxygen use at one month of age in vitamin A‐treated infants (RR 0.75, 95% CI 0.62 to 0.91) (Darlow 1998). The addition of Tyson 1999, which found no difference in outcome at one month, to the pooled data resulted in the meta‐analysis showing only a trend of borderline significance towards reduction in death or oxygen use at this time (RR 0.93, 95% CI 0.86 to 1.00) (Darlow 2000). Wardle 2001, the only trial to give supplemental vitamin A via the enteral route, had a moderate sample size (154) and found no significant benefit of supplementation; however, the further addition of data from this trial resulted in the meta‐analysis showing a small but statistically significant reduction in this outcome (RR 0.93, 95% CI 0.88 to 0.99; RD −0.05, 95% CI −0.10 to −0.01; NNTB 20, 95% CI 10 to 100).
Four trials which gave intramuscular vitamin A to supplemented infants reported outcomes at 36 weeks' postmenstrual age (Tyson 1999; Wardle 2001; Ravishankar 2003; Mactier 2012). The meta‐analysis of these trials supports a marginal reduction in oxygen use in vitamin A‐treated infants at 36 weeks' postmenstrual age (typical RR 0.89, 95% CI 0.78 to 1.00; typical RD −0.06, 95% CI −0.13 to 0.00; NNTB 16, 95% CI 8 to 1000+; 906 infants) as well as a marginal reduction in death or oxygen use at 36 weeks' postmenstrual age (typical RR 0.92, 95% CI 0.84 to 1.01; typical RD −0.05, 95% CI −0.11 to 0.01; 1089 infants). From the meta‐analysis of the combined data, the NNTB with regard to oxygen requirement at 36 weeks is 13 with wide 95% confidence intervals, ranging from 7 to more than 1000. It is also noteworthy that there was no difference in other outcomes, including days of ventilation and length of stay, and between vitamin A‐supplemented and control infants in Tyson 1999.
Some differences between the trials may be explained by the differences in patient populations (birth weight and ethnicity), the differences in both the route of vitamin A supplementation (intramuscular, intravenous in lipid emulsion, or enteral), and the dose given. Tyson 1999 and Wardle 2001 included somewhat lower birth weight infants (401 to 1000 grams and < 1000 grams respectively) than most other trials whereas other trials used various lower weight limits (500 grams for Ravishankar 2003; 700 grams for Pearson 1992 and Shenai 1987; 725 grams for Werkman 1994; and 1000 grams for Bental 1994). The incidence of supplemental oxygen requirement at one month of age in vitamin A‐supplemented infants was higher at 73% in Tyson 1999 and 83% in Wardle 2001, compared with a range of 34% to 67% in the other trials; this is consistent with their lower birth weight and gestational age. For the smallest infants the outcome at 36 weeks' postmenstrual age may be more clinically relevant.
In all the included trials there were higher vitamin A or retinol concentrations in the infants in the vitamin A group compared with the control group at most of the time periods studied. Kennedy 1997 reported that an intramuscular dose of 5000 IU vitamin A three times per week was required to achieve serum concentrations greater than 250 μg/L in most very low birth weight infants. This was the dose used by Tyson 1999 and was generally greater than the dose used in earlier studies; for example, Bental 1994 used 4000 IU three times weekly, Papagaroufalis 1988 used 4000 IU on alternate days while the infants were ventilated, Pearson 1992 and Shenai 1987 used 2000 IU on alternate days, and Ravishankar 2003 used between 1500 IU and 3000 IU for three doses only. Nevertheless, in Tyson 1999 25% of infants who received supplemental vitamin A and 54% of controls (data from the first 300 enrolled infants) had vitamin A concentrations below 200 μg/L on day 28. Similar percentages, 22% of those who received supplemental vitamin A and 45% of controls, had a relative dose response (change in the serum retinol concentration divided by the pre‐injection concentration) of more than 10% following an intramuscular dose of 2000 IU. Taken together, these data suggest that an even higher dose of vitamin A given intramuscularly may be required to achieve vitamin A sufficiency in very premature infants.
In Wardle 2001, infants received a much higher cumulative dose of supplemental vitamin A than in other studies (140,000 IU in 28 days compared with 60,000 IU in Tyson 1999) but by the enteral route. Vitamin A concentrations were only measured in the first 84 infants enrolled and the median concentration 24 hours after the first dose was significantly higher in supplemented infants (230 μg/L versus 150 μg/L). At 7 and 28 days of age, however, there were no significant differences in vitamin A concentrations between the groups and the median concentration in both groups was less than 200 μg/L at these times. Vitamin A absorption is less efficient using the enteral route. Rush 1994 compared the same dose of vitamin A (2000 IU/kg on alternate days) given by intramuscular injection or orally and reported that the former route gave higher plasma vitamin A concentrations after one week. Landman 1992 reported that enteral supplementation with 5000 IU vitamin A daily resulted in similar plasma concentrations at 32 days of age to those resulting from 2000 IU vitamin A on alternate days by the intramuscular route.
There were also quite marked differences in the vitamin A dose received by the control groups. This has previously been suggested to account for differences in outcome between the early studies (Lorch 1994). Infants in the control group in Pearson 1992 received higher doses of vitamin A and had mean vitamin A concentrations at weeks three and four of greater than 200 μg/L. This is higher than in infants in the control group in Shenai 1987 in which mean vitamin A concentrations were less than 150 μg/L at these times. One interpretation is that Shenai 1987 demonstrated a benefit of supplemental vitamin A in a population with vitamin deficiency, while Pearson 1992 showed a minimal benefit of additional supplementation in a population with more adequate vitamin status. However, Georgieff 1989 reported that postnatal steroids led to a near doubling of plasma vitamin A concentrations, and this finding was confirmed in Tyson 1999. Certainly variability in exposure to postnatal steroids complicates the interpretation of these data. Two trials included in this review reported the incidence of treatment with postnatal steroids (Pearson 1992, 46% in vitamin A group and 44% in controls; Wardle 2001, 39% and 34% respectively), while two others noted that steroids were used in some infants (Bental 1994; Tyson 1999).
Further information on the optimal dosage of intramuscular vitamin A for infants with birth weights 401 to 1000 grams is available from the Ambalavanan 2003 trial. Ambalavanan 2003 compared the dose regimen used by Tyson 1999 (5000 IU three times weekly for four weeks) with both a higher dose (10,000 IU three times weekly for four weeks) and a once‐a‐week dose (15,000 IU weekly for four weeks) in 120 infants. Only two infants received postnatal steroids between study days 21 and 28. Compared with the standard regimen, the higher dose regimen was not associated with a significantly higher mean retinol concentration at 28 days and there were no differences between the groups in the proportion of infants having concentrations of less than 200 μg/L at this time (26% versus 21%). The once‐a‐day regimen, however, was associated with significantly lower mean concentrations at 28 days and increased the risk of infants having concentrations of less than 200 μg/L at this time by a factor of 2.5 (26% versus 65%).
Many other variables will also affect the rate of chronic lung disease, which is known to vary considerably between centres. These factors include use of antenatal steroids (stated in four trials: Pearson 1992 where they were received by 26% of study infants and 41% controls; Tyson 1999 where the rates were 76% and 74%; Wardle 2001 where the rates were 77% and 82%; and Ravishankar 2003 where the rates were 86% and 72%); exogenous surfactant (stated in three trials: Pearson 1992 where > 90% received an artificial surfactant; Tyson 1999 where > 80% received a natural surfactant; and Wardle 2001 where all but one infant in the control group received an artificial surfactant); mode of ventilation including early nasal continuous positive airway pressure; postnatal steroids; and criteria for prescribing supplemental oxygen.
Despite the variations among trials discussed above, the quality assessment of the body of evidence found in this review for the critical neonatal outcomes was judged to be of moderate quality. The effect of vitamin A on 28‐day outcomes (chronic lung disease or death, or both), death before 36 weeks' postmenstrual age, and chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors) is of moderate quality; therefore the possibility exists that the true effect is different than that estimated here and further research could change the estimates of the effects on these last outcomes.
Less is known regarding follow‐up at 18 to 24 months. Ambalavanan 2003 assessed 85% of infants who participated in the study of Tyson 1999. Results regarding the long‐term effects that vitamin A could have on either neurodevelopment impairment (RR 0.89, 95% CI 0.74 to 1.08) or the combined outcome of death or neurodevelopmental impairment (RR 0.92, 95% CI 0.81 to 1.05) were inconclusive. The low quality of evidence for the neurodevelopment impairment makes evident the need for further research to define the long‐term effects of the supplementation of vitamin A in preterms. This trial was not powered appropriately to assess long‐term outcomes, and the benefit or harm from repeated intramuscular vitamin A following birth remains uncertain.
The studies did not generally report the frequency or severity of adverse events, although Pearson 1992 noted that repeat intramuscular injections may have been painful.
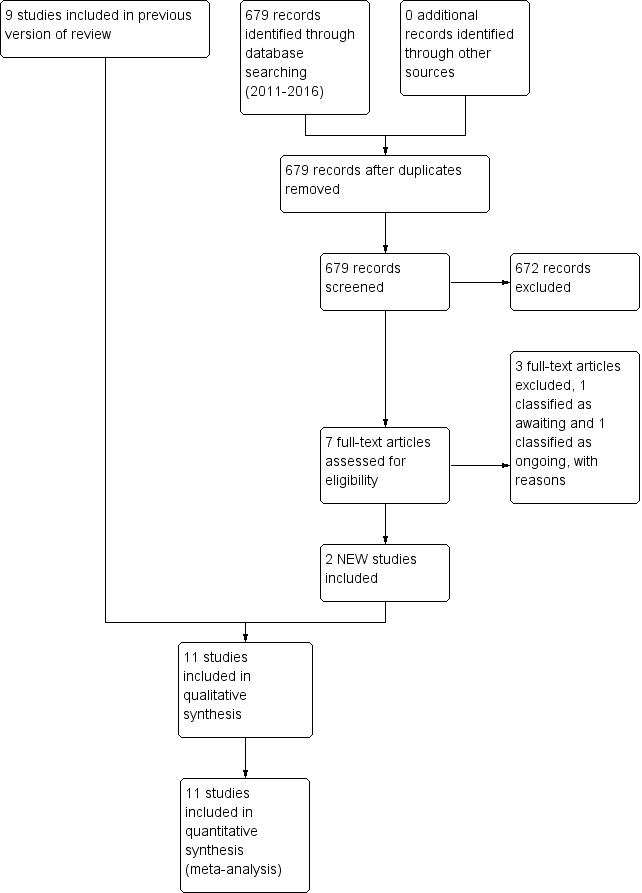
Study flow diagram: review update

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
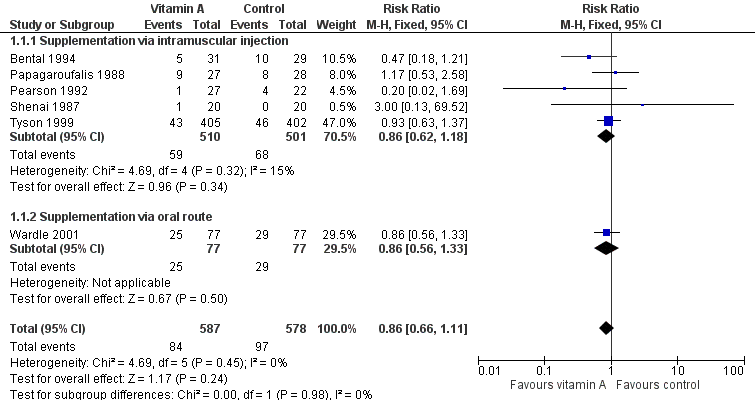
Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.1 Death (before 1 month).

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.2 Chronic lung disease (oxygen use at 28 days in survivors).
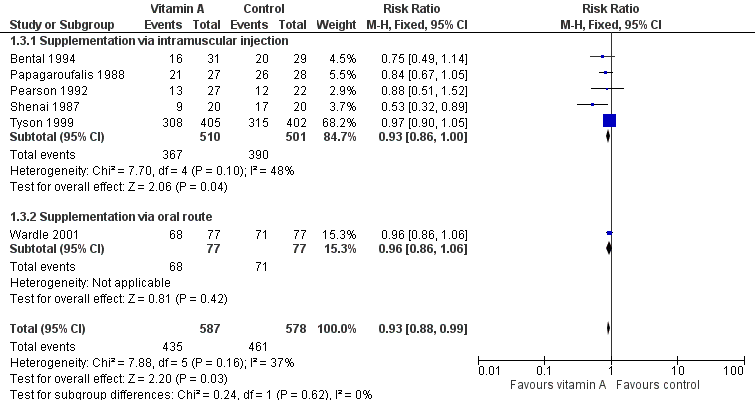
Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.3 Death or chronic lung disease (oxygen use at 28 days).

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.4 Death before 36 weeks' postmenstrual age.

Forest plot of comparison: 1 Supplemental vitamin A versus no supplementation, outcome: 1.5 Chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors).
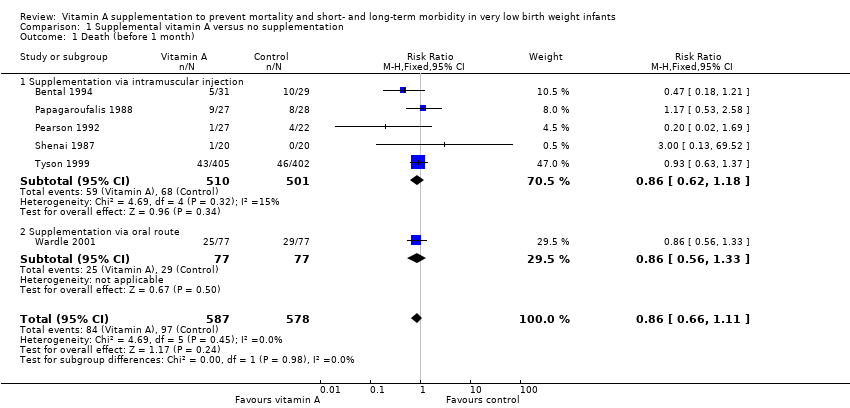
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 1 Death (before 1 month).
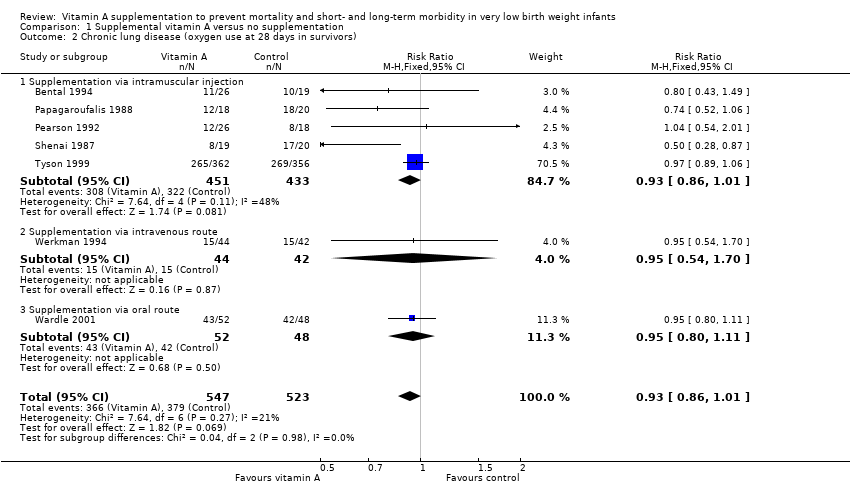
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 2 Chronic lung disease (oxygen use at 28 days in survivors).

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 3 Death or chronic lung disease (oxygen use at 28 days).

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 4 Death before 36 weeks' postmenstrual age.

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 5 Chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors).
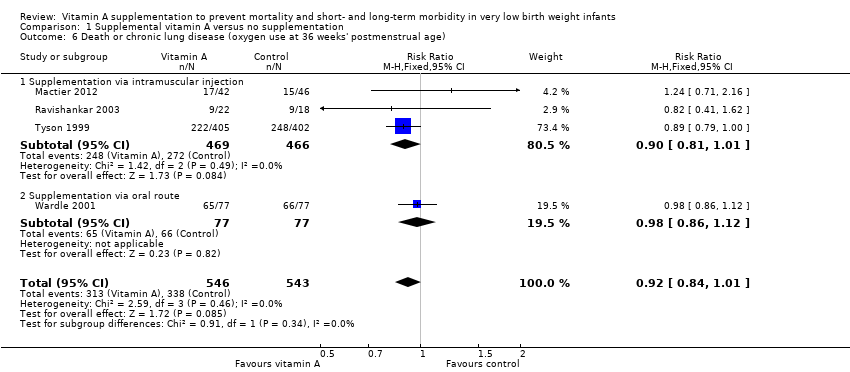
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 6 Death or chronic lung disease (oxygen use at 36 weeks' postmenstrual age).
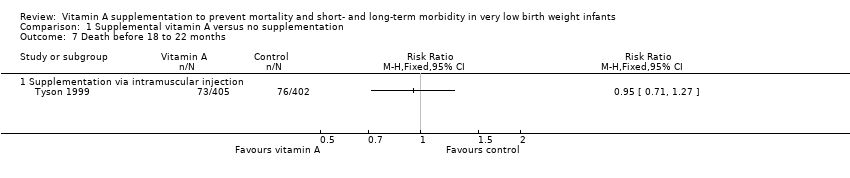
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 7 Death before 18 to 22 months.

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 8 Neurodevelopmental impairment at 18 to 22 months.

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 9 Death or neurodevelopmental impairment at 18 to 22 months.
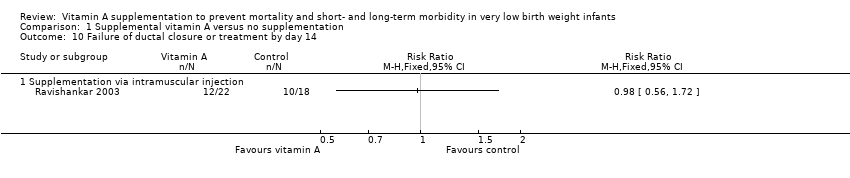
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 10 Failure of ductal closure or treatment by day 14.
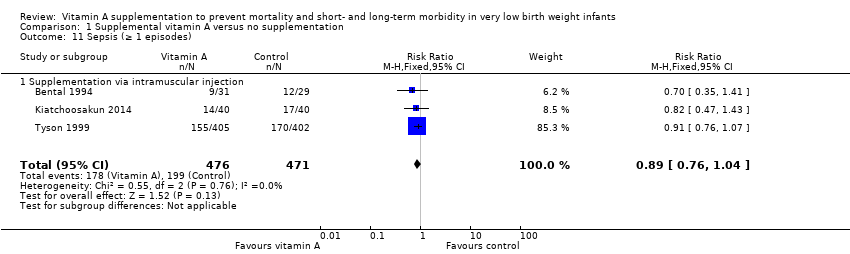
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 11 Sepsis (≥ 1 episodes).

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 12 Necrotising enterocolitis.

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 13 Intraventricular haemorrhage.

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 14 Periventricular leukomalacia.

Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 15 Retinopathy of prematurity (any grade).
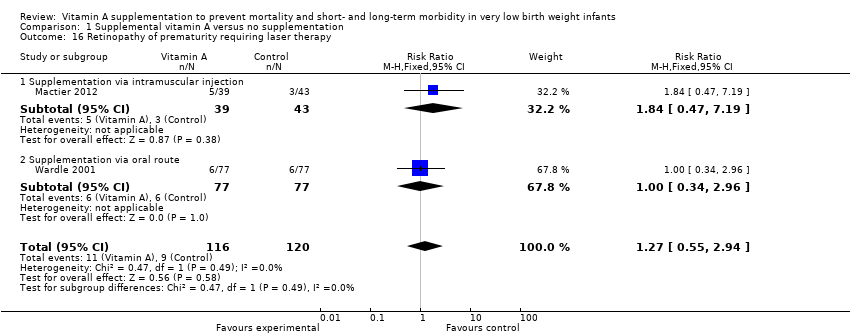
Comparison 1 Supplemental vitamin A versus no supplementation, Outcome 16 Retinopathy of prematurity requiring laser therapy.
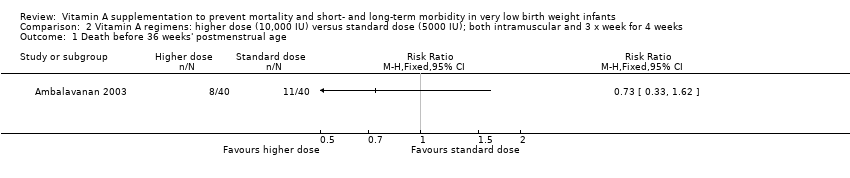
Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 1 Death before 36 weeks' postmenstrual age.
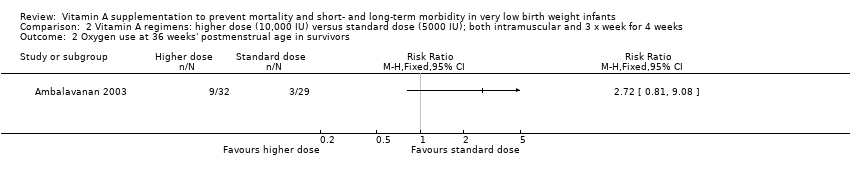
Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 2 Oxygen use at 36 weeks' postmenstrual age in survivors.

Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 3 Death or oxygen use at 36 weeks' postmenstrual age.
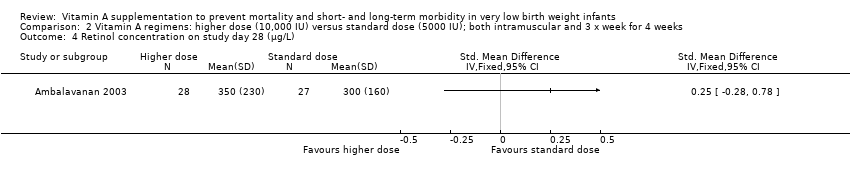
Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 4 Retinol concentration on study day 28 (μg/L).

Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 5 Retinol < 200 μg/L on day 28 (%).
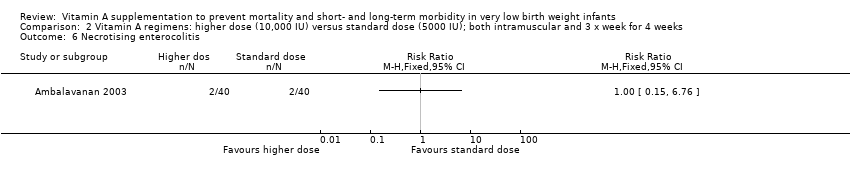
Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 6 Necrotising enterocolitis.

Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 7 Retinopathy of prematurity (any grade).
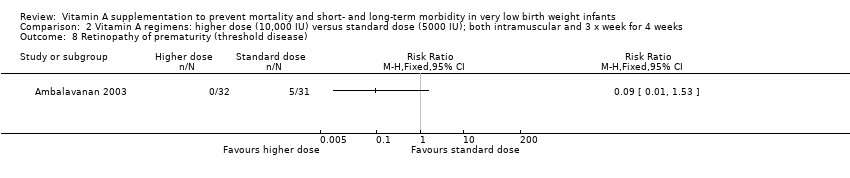
Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 8 Retinopathy of prematurity (threshold disease).
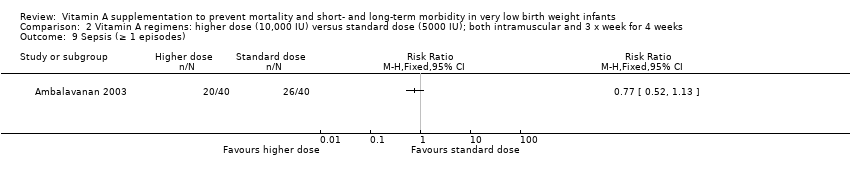
Comparison 2 Vitamin A regimens: higher dose (10,000 IU) versus standard dose (5000 IU); both intramuscular and 3 x week for 4 weeks, Outcome 9 Sepsis (≥ 1 episodes).

Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 1 Death before 36 weeks' postmenstrual age.
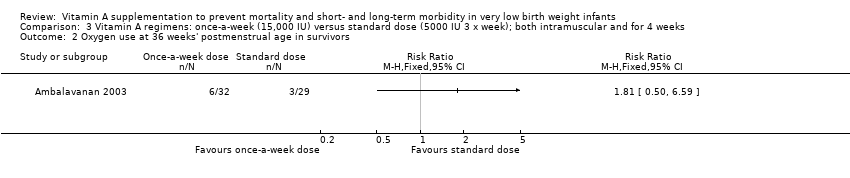
Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 2 Oxygen use at 36 weeks' postmenstrual age in survivors.

Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 3 Death or oxygen use at 36 weeks' postmenstrual age.
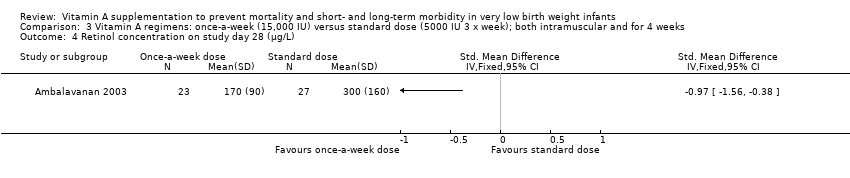
Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 4 Retinol concentration on study day 28 (μg/L).

Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 5 Retinol < 200 μg/L on day 28 (%).

Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 6 Necrotising enterocolitis.
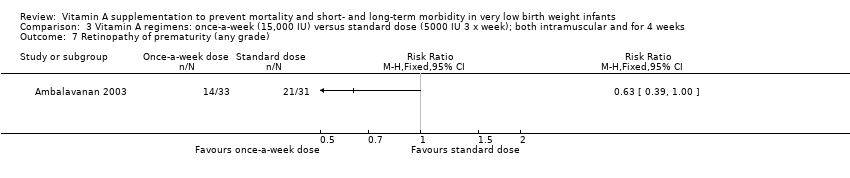
Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 7 Retinopathy of prematurity (any grade).

Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 8 Retinopathy of prematurity (threshold disease).

Comparison 3 Vitamin A regimens: once‐a‐week (15,000 IU) versus standard dose (5000 IU 3 x week); both intramuscular and for 4 weeks, Outcome 9 One or more episodes of sepsis.
| Supplemental vitamin A compared to no supplementation in very low birth weight infants | ||||||
| Patient or population: very low birth weight infants | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| no supplementation | Supplemental vitamin A | |||||
| Neonatal death | 168 per 1000 | 144 per 1000 | RR 0.86 | 1165 | ⊕⊕⊕⊝ | Imprecision: 95% CI are wide and imprecise |
| Chronic lung disease (oxygen use at 28 days in survivors) | 725 per 1000 | 674 per 1000 | RR 0.93 | 1070 | ⊕⊕⊕⊕ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Death or chronic lung disease (oxygen use at 28 days) | 798 per 1000 | 742 per 1000 | RR 0.93 | 1165 | ⊕⊕⊕⊕ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Death before 36 weeks' postmenstrual age | 168 per 1000 | 168 per 1000 | RR 1.00 | 1089 | ⊕⊕⊕⊝ | Imprecision: 95% CI are wide and imprecise |
| Chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors) | 546 per 1000 | 486 per 1000 | RR 0.87 | 986 | ⊕⊕⊕⊝ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Death or chronic lung disease (oxygen use at 36 weeks' postmenstrual age) | 622 per 1000 | 573 per 1000 | RR 0.92 | 1089 | ⊕⊕⊕⊝ | Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect |
| Neurodevelopmental impairment at 18 to 22 months | 481 per 1000 | 428 per 1000 | RR 0.89 | 538 | ⊕⊕⊝⊝ | Concerning imprecision: does not met the optimal information size criteria |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Imprecision: 95% CI are wide and imprecise 2 Imprecision: although the 95% CI is narrow, the result is consistent with minimal clnical effect 3 Concerning imprecision; does not met the optimal information size criteria | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death (before 1 month) Show forest plot | 6 | 1165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.66, 1.11] |
| 1.1 Supplementation via intramuscular injection | 5 | 1011 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.62, 1.18] |
| 1.2 Supplementation via oral route | 1 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.56, 1.33] |
| 2 Chronic lung disease (oxygen use at 28 days in survivors) Show forest plot | 7 | 1070 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.86, 1.01] |
| 2.1 Supplementation via intramuscular injection | 5 | 884 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.86, 1.01] |
| 2.2 Supplementation via intravenous route | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.54, 1.70] |
| 2.3 Supplementation via oral route | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.80, 1.11] |
| 3 Death or chronic lung disease (oxygen use at 28 days) Show forest plot | 6 | 1165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.88, 0.99] |
| 3.1 Supplementation via intramuscular injection | 5 | 1011 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.86, 1.00] |
| 3.2 Supplementation via oral route | 1 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.86, 1.06] |
| 4 Death before 36 weeks' postmenstrual age Show forest plot | 4 | 1089 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.77, 1.29] |
| 4.1 Supplementation via intramuscular injection | 3 | 935 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.77, 1.46] |
| 4.2 Supplementation via oral route | 1 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.56, 1.33] |
| 5 Chronic lung disease (oxygen use at 36 weeks' postmenstrual age in survivors) Show forest plot | 5 | 986 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.77, 0.99] |
| 5.1 Supplementation via intramuscular injection | 4 | 886 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.74, 0.98] |
| 5.2 Supplementation via oral route | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.81, 1.24] |
| 6 Death or chronic lung disease (oxygen use at 36 weeks' postmenstrual age) Show forest plot | 4 | 1089 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.84, 1.01] |
| 6.1 Supplementation via intramuscular injection | 3 | 935 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.81, 1.01] |
| 6.2 Supplementation via oral route | 1 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.12] |
| 7 Death before 18 to 22 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Supplementation via intramuscular injection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Neurodevelopmental impairment at 18 to 22 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Supplementation via intramuscular injection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Death or neurodevelopmental impairment at 18 to 22 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Supplementation via intramuscular injection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Failure of ductal closure or treatment by day 14 Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.1 Supplementation via intramuscular injection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Sepsis (≥ 1 episodes) Show forest plot | 3 | 947 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.04] |
| 11.1 Supplementation via intramuscular injection | 3 | 947 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.04] |
| 12 Necrotising enterocolitis Show forest plot | 4 | 1101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.67, 1.27] |
| 13 Intraventricular haemorrhage Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Any intraventricular haemorrhage | 3 | 907 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.82, 1.10] |
| 13.2 Severe intraventricular haemorrhage (Grade 3 or 4) | 4 | 1035 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.72, 1.25] |
| 14 Periventricular leukomalacia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15 Retinopathy of prematurity (any grade) Show forest plot | 4 | 255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.65, 1.01] |
| 15.1 Supplementation via intramuscular injection | 3 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.42, 0.99] |
| 15.2 Supplementation via oral route | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.75, 1.20] |
| 16 Retinopathy of prematurity requiring laser therapy Show forest plot | 2 | 236 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.55, 2.94] |
| 16.1 Supplementation via intramuscular injection | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.84 [0.47, 7.19] |
| 16.2 Supplementation via oral route | 1 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.34, 2.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death before 36 weeks' postmenstrual age Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Oxygen use at 36 weeks' postmenstrual age in survivors Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Death or oxygen use at 36 weeks' postmenstrual age Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Retinol concentration on study day 28 (μg/L) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Retinol < 200 μg/L on day 28 (%) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Necrotising enterocolitis Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Retinopathy of prematurity (any grade) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Retinopathy of prematurity (threshold disease) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9 Sepsis (≥ 1 episodes) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death before 36 weeks' postmenstrual age Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Oxygen use at 36 weeks' postmenstrual age in survivors Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Death or oxygen use at 36 weeks' postmenstrual age Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Retinol concentration on study day 28 (μg/L) Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Retinol < 200 μg/L on day 28 (%) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Necrotising enterocolitis Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Retinopathy of prematurity (any grade) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Retinopathy of prematurity (threshold disease) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9 One or more episodes of sepsis Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

