Epidural berbanding bukan epidural atau tanpa analgesia untuk pengurusan sakit semasa bersalin
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Computer‐generated list of random numbers were prepared by an uninvolved 3rd party. Randomisation was accomplished by selection of the next in a series of opaque, sealed envelopes. | |
| Participants | 100 women recruited (epidural N = 49, narcotics N = 51) | |
| Interventions | Epidural: preload given 500 ‐ 1000 mL sodium lactate 0.25% bupivacaine ± 50 ‐ 100 mg fentanyl until T10 sensory analgesia achieved, then continuous infusion 0.125% bupivacaine with 1.5 mg/mL fentanyl. Continued in 2nd stage | |
| Outcomes | Maternal: pain scores measured hourly, length of 1st and 2nd stage of labour, oxytocin in labour, malposition, amniotomy, nausea and vomiting, operative vaginal delivery, caesarean section, caesarean section for dystocia and fetal distress | |
| Notes | University of Mississippi, USA Dates: Trial carried out 1995 ‐ 1996 Funding: Supported by the Vicksburg Hospital Medical Foundation Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Selection of the next in a series of opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 2 women in the epidural group were delivered before obtaining regional analgesia and 12 women in the parenteral analgesia received "epidural rescue", but these participants remain in their group for all statistical considerations. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the Methods section have been reported on in the results. |
| Other bias | High risk | More white women in the narcotic group (P = 0.008) |
| Methods | All participants randomised according to a random number scheme with instructions contained in sequentially numbered, opaque envelopes | |
| Participants | 24 women were recruited (sufentanil intrathecal N = 9, epidural N = 8, IV N = 7). | |
| Interventions | Sufentanil 10 µg either intrathecally (N = 9), epidurally (N = 8) or intravenously (N = 7), using a CSE technique. The sufentanil was administered alone without concomitant local anaesthetics. Participants could request additional analgesia (bupivacaine 0.25% via the epidural catheter) if pain relief was unsatisfactory by 15 mins after injection of study drug. | |
| Outcomes |
| |
| Notes | Brigham and Women's Hospital, Harvard Medical School, USA Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised according to a random number scheme. |
| Allocation concealment (selection bias) | Low risk | All participants randomised in a double‐blind fashion according to a random number scheme with instructions contained in sequentially numbered, opaque envelopes. |
| Blinding of participants and personnel (performance bias) | Low risk | Presume so ‐ states "double‐blind" |
| Blinding of outcome assessment (detection bias) | Low risk | Probably ‐ "All injectates were prepared by an anaesthesiologist not involved in subsequent data collection" ‐ implies people collecting data would not have been aware of drug allocation. |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised appear to have been accounted for within the results, although only a small number of women were recruited because the study was stopped early. |
| Selective reporting (reporting bias) | High risk | They did not report the results for the following outcomes:
|
| Other bias | High risk | The study was stopped early because "it became clear that a large number of the subjects had clearly unsatisfactory analgesia" so the number of participants in the study was small. |
| Methods | RCT Parallel design Single centre Tongji Hospital, Wuhan, Hubei, China | |
| Participants | 200 women were randomly divided into 2 groups. Group 1 (N = 100) ‐ labour analgesia group ‐ ropivacaine 3.75 mg and fentanyl 20 µg injected into subarachnoid space while utero‐cervical was opened 2 ‐ 3 cm and then ropivacaine 0.1% plus fentanyl 2 µg/mL was used in epidural space. Group II (N = 100) ‐ natural delivery without analgesia Eligibility: ASA physical status I ‐ II parturients | |
| Interventions | Group 1 (N = 100) ‐ labour analgesia group ‐ ropivacaine 3.75 mg and fentanyl 20 µg injected into subarachnoid space while utero‐cervical was opened 2 ‐ 3 cm and then ropivacaine 0.1% plus fentanyl 2 µg/mL was used in epidural space. Group II ‐ natural delivery without analgesia | |
| Outcomes |
| |
| Notes | Abstract only ‐ so results limited Dates: Not stated Funding: Not stated Declarations of Interest: None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not reported |
| Methods | Reported to be single‐centre RCT with individual allocation but no information on methods | |
| Participants | 124 women anticipating vaginal delivery were recruited and divided into 2 groups: PCA epidural ropivacaine (N = 75), versus 'no pain relieving methods' (N = 49). Eligibility: women anticipating vaginal delivery (it was not clear whether any women subsequently had CS) Exclusion: pregnancy complications | |
| Interventions | Group 1 ‐ PCA epidural Ropivacaine ‐ 3 mL ropivacaine (0.125%) injected through an epidural catheter and another 12 mL 5 minutes later if there was no total spinal anaesthesia. The block level was controlled to be below the T10 level. Then 5 mL (0.104 mg/min) per hour until full dilatation. (N = 75). Group 2 ‐ control ‐ "no pain relieving measures” (N = 49) | |
| Outcomes | Prolactin levels at delivery and 2 hours later and time of the start of lactation Mean newborn weight reduction in the 1st day following delivery. No relevant outcomes reported | |
| Notes | Trial conducted in China, women attending a hospital in Bejing Dates of trial: January 2006 – June 2007 Funding: not stated Conflicts of Interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Translated notes state "controlled clinical trial" and that women were “randomly divided” into groups but no further information. |
| Allocation concealment (selection bias) | Unclear risk | Translated notes state "controlled clinical trial" and that women were “randomly divided” into groups but no further information. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding: women in the control group had no analgesia whereas the intervention group had epidural; staff would be aware of study group. |
| Blinding of outcome assessment (detection bias) | High risk | Not stated, although outcomes were measured immediately after delivery, so it is likely outcome assessors were aware of analgesia. |
| Incomplete outcome data (attrition bias) | Unclear risk | It was not stated whether or not there was any loss to follow‐up, translated notes report that numbers in tables report the same numbers as those randomised. Intention‐to‐treat analysis: not reported. It was not stated whether any women had CS or whether these women were excluded post‐randomisation. |
| Selective reporting (reporting bias) | High risk | We have no protocol and assessment is from stated notes. Although this was reported as an RCT there was considerable imbalance between groups (75 vs 49). There was no explanation for this. |
| Other bias | Unclear risk | Insufficient information to make a judgement. The control group were reported to receive no analgesia; it is not clear whether this was at the point of randomisation or whether women requesting pain relief were denied it. |
| Methods | Computer‐generated, random‐number tables, group assignments were placed in sealed, opaque, sequentially‐numbered envelopes. | |
| Participants | 318 women recruited (epidural N = 156, meperidine N = 162) | |
| Interventions | Epidural: IV fluid bolus of 1 litre normal saline solution following by placement of the epidural catheter through the L2 ‐ 3 or L3 ‐ 4 interspace. | |
| Outcomes | Maternal: oxytocin use, length of 1st and 2nd stages of labour, 2nd stage labour, mode of delivery, caesarean for dystocia, caesarean for fetal distress | |
| Notes | University of Louisville Hospital, Kentucky, USA Dates: Trial carried out 1995 ‐ 1996 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number tables |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque, sequentially‐numbered envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | Because of the large number of cross‐over participants (52%), the data were subsequently analysed with respect to those who were compliant with the assigned analgesic method. 78 of 162 (48.1%) received IV meperidine and 147 of 156 (94.2%) of the epidural group. |
| Selective reporting (reporting bias) | High risk | Additional outcomes reported in tables (Apgar scores, meconium) not specified in the Methods section. |
| Other bias | Low risk | 10 participants were excluded from the data analysis because of protocol violations. |
| Methods | Randomised controlled trial using individual randomisation | |
| Participants | 70 women randomised (combined spinal anaesthesia, n = 35; continuous support, n = 35). Women admitted to the antepartum unit of the Instituto de Medicina Integral Prof Fernando Figueira, Brazil Eligibility: pregnant women, singleton, full‐term fetus with cephalic presentation and cervical dilatation of 3 ‐ 6 cm Excluded: women with fever before or at the time of randomisation, those using antibiotics, those with high‐risk pregnancies (placenta previa, placental abruption, severe pre‐eclampsia/eclampsia, premature delivery, HIV‐positive), and those with an indication of immediate caesarean section | |
| Interventions | CSE anaesthesia: 2.5 mg of 0.5% heavy bupivacaine associated with 5 mg of sufentanil was injected into the subarachnoid space. Immediately afterwards, the epidural space was punctured using an 18 G Tuohy needle and a catheter was inserted into the same interspinous space used for subarachnoid puncture. Only 30 mins after subarachnoid puncture, administration of 5 mL of a solution containing 0.05% bupivacaine and sufentanil 0.2 mg mL–1 was initiated through the epidural catheter. This solution was administered intermittently every 30 mins until delivery of the infant. CSE was initiated only when requested by participants. 1 woman did not request epidural. Women in both groups received continuous support during delivery provided by a doula or trained lay person, and Swiss exercise balls, massage, and music therapy. | |
| Outcomes | Satisfaction Loss of control Mode of birth Oxytocin augmentation Fever | |
| Notes | Setting: hospital in Brazil Dates of trial: February – May 2010 Funding: unclear CoI: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A table of random numbers generated using the Random Allocation Software program |
| Allocation concealment (selection bias) | Low risk | Sealed open envelopes contained the allocation group to which each participant was to be assigned |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible ‐ women and staff would have been aware of intervention groups |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessor: insufficient information, labour outcome probably assessed by caregivers |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up occurred after randomisation. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes are reported. |
| Other bias | Low risk | Women in both the groups were balanced for all the baseline characteristics. |
| Methods | Randomly selected from block group of sealed, opaque envelopes. Primary analysis: intention‐to‐treat analysis. Secondary analysis of compliant participants only, randomisation stratification into spontaneous and induced labour. All women accounted for | |
| Participants | 992 women recruited (epidural N = 493, continuous midwifery support group N = 499) Eligibility: nulliparous women at term with singleton cephalic presentation in spontaneous labour (cervix < 5 cm dilated) and induced labour | |
| Interventions | CSE: needle‐through‐needle approach. Preload 500 ‐ 1000 mL crystalloids. Spinal block achieved with fentanyl 25 micrograms and bupivacaine 2 mg. Following onset of analgesia epidural catheter dosed with 0.125% bupivacaine ‐6 mL then participant‐controlled epidural analgesia until delivery with 0.1% bupivacaine and 2 micrograms of pethidine. 136 women did not receive epidural. | |
| Outcomes | Maternal: pain scores, caesarean section, duration of 1st and 2nd stages of labour. operative vaginal delivery, vomiting, catheterisation during labour, fever (> 37.5 ºC) and satisfaction with childbirth (median VAS); breastfeeding reported on compliant participants only Long‐term outcomes (Orlikowski 2006) ‐ back pain, headache, migraine, mod‐severe back pain, severe headache, severe migraine before pregnancy, during pregnancy, and at 2 (N = 576) and at 6 months (N = 521) postpartum | |
| Notes | King Edward Memorial Hospital for Women, Perth, Western Australia, between May 1997 and October 1999 Funding: supported by NH&MRC Grant 970076 Conflicts of interest: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Selection from a blocked group of 8 sealed opaque envelopes replenished from blocks of 12 |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Women were encouraged to manage their labour with the assistance of a midwife and with the intention of avoiding the use of epidural analgesia. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | The cross‐over rate from the EPI to the CMS group was 27.8% (N = 137) and cross‐over rate from CMS to EPI analgesia was 61.3% (N = 306). |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | High risk | As the compliance rate was approximately 40% in the CMS group and 75% in the EPI group, it would not be possible to distinguish between the caesarean section rates, as hypothesised, without 12,000 participants. As it was not feasible to recruit the number of women required to demonstrate such a difference, enrolment into the trial was stopped. |
| Methods | RCT with individual randomisation Participants randomly allocated to 2 intervention groups, control group recruited by observational cohort. Control group data not included in this review. | |
| Participants | 116 women recruited to 2 treatment groups but data reported only for 98 (epidural analgesia n = 49; intravenous remifentanil patient‐controlled analgesia n = 49). Eligibility: women who are classed as ASA class I or II parturients with a singleton pregnancy, between 37 and 42 weeks of gestation Excluded: BMI ≥ 40 kg/m2, insulin‐dependent diabetes, severe pre‐eclampsia (proteinuria ≥ 5 g/24 hr), use of antibiotics during delivery, initial maternal SpO2 < 98%, initial maternal temperature ≥ 38 oC, cervical dilation of > 7 cm and ruptured membranes for > 24 hrs at the time of inclusion. If delivery occurred within 1 hr of starting the study, women were excluded from analysis. | |
| Interventions | Epidural analgesia: EA (n = 49) A catheter was inserted at the L2 – 3 or L3 – 4 interspace using a 17‐gauge Tuohy needle. Parturients received a loading dose of ropivacaine 25 mg (0.2% ropivacaine 12.5 mL), followed by a continuous infusion of 0.1% ropivacaine and sufentanil 0.5 µg/mL at 10 mL/h. In case of inadequate analgesia, additional 10 mL boluses were given. In case of epidural catheter dislodgement, the catheter was replaced. rPCA (n = 49) Received a 40 µg bolus (lockout 2 mins, bolus duration 36 s) using a Graseby 3300 syringe pump. The maximum dose permitted was 1200 µg/h. No background infusion was added. Because of concerns about the potential for neonatal respiratory depression, the pump was stopped when the woman reached full cervical dilatation. When parturients were dissatisfied with analgesia, EA was offered as alternative. | |
| Outcomes | Mode of birth Side effects Apgar scores Umbilical cord gases Duration of labour Satisfaction scores | |
| Notes | Country and setting: Netherlands, Leiden University Medical Center Dates of trial: November 2008 – October 2010 Funding: Department of Anesthesiology, Leiden University Medical Centre Conflicts of interest: none Neonatal fever 2/49 EA; 2/49 rPCA Sepsis follow‐up 4/49 EA; 3/49 rPCA Positive blood culture 0/49 EA; 0/49 rPCA Overall satisfaction measured post‐delivery 8.4 (SD 1.2)/49 EA; 8.1 (SD 1.2)/49 rPCA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Randomisation list was kept in a numbered opaque sealed envelope that was opened upon the request for analgesia. |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible for these interventions |
| Blinding of outcome assessment (detection bias) | High risk | No information on who collected or analysed the outcome given, but probably collected by care provider in labour Satisfaction score was by self‐administered questionnaire |
| Incomplete outcome data (attrition bias) | High risk | 10 women were excluded from the analysis in EA group: 7 delivered < 1 hour of analgesia; 3 met exclusion criteria post‐randomisation but reasons not explicit. 8 women were excluded from the analysis in rPCA group: 6 delivered < 1 hr; 2 "met exclusion criteria". "Continuous saturation data were not always available and this information is reported for only 114 women." 1 women lost to follow‐up in labour in each group. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes are reported as per protocol. |
| Other bias | Unclear risk | Similar baseline characteristics. Some reporting of results is not clear. |
| Methods | RCT Parallel design Single centre Cairo, Egypt | |
| Participants | 30 nulliparous pre‐eclamptic parturient women were randomly divided into 2 equal groups. Epidural group: N = 15 Remifentanil group: N = 15 Eligibility: ≧ 32 weeks' gestation, normal cephalic presentation, < 5 cm cervical dilatation, clinical diagnosis of pre‐eclampsia | |
| Interventions | Epidural group (N = 15): received epidural analgesia according to a standardised protocol using bupivacaine plus fentanyl. Remifentanil group (N = 15): PCA was set up to deliver remifentanil 0.5 µg/kg as a loading bolus infused over 20 s, lockout time of 5 mins, PCA bolus of 0.25 µg/kg, continuous background infusion of 0.05 µg/kg/min, and maximum dose is 3 mg in 4 hrs. Women were advised to start the PCA bolus when they felt signs of a coming uterine contraction. | |
| Outcomes |
7. Maternal side effects:
8. Assisted vaginal delivery 9. Caesarean section 10. Normal delivery | |
| Notes | Cairo University, Egypt Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | All expected outcomes are reported. |
| Other bias | Low risk | Baseline characteristics of groups were similar. |
| Methods | RCT Parallel design Single centre Department of Obstetrics and Gynecology, The Edith Wolfson Medical Center, Israel | |
| Participants | 60 women recruited ‐ 4 excluded (epidural N = 29, iv meperidine N = 27) Eligibility: healthy, ASA physical status I and II primiparous women in spontaneous labour with singleton cephalic presentation at term | |
| Interventions | PCEA with 0.2 % ropivacaine (N = 29) Patient‐controlled IV analgesia (PCA) with meperidine (N = 27) | |
| Outcomes |
| |
| Notes | Department of Obstetrics and Gynecology, The Edith Wolfson Medical Center, Israel 4 exclusions (3 caesarean deliveries performed for non‐reassuring FHRs and 1 parturient in the meperidine group demanded epidural analgesia) Dates: Trial carried out February to September 2003 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was based on computer‐generated codes. |
| Allocation concealment (selection bias) | Low risk | Randomisation was based on computer‐generated codes, maintained in sequentially numbered opaque envelopes until just before use. |
| Blinding of participants and personnel (performance bias) | Low risk | Dummy IV saline and dummy epidural catheter were used. |
| Blinding of outcome assessment (detection bias) | High risk | Pathologist who examined placenta and umbilical cord was blinded to parturient's temperature. |
| Incomplete outcome data (attrition bias) | Low risk | 4 exclusions (3 caesarean deliveries performed for non‐reassuring FHRs and 1 parturient in the meperidine group demanded epidural analgesia) ‐ outcome data available for all remaining participants (N = 56). |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported within the Methods section are available within the Results. |
| Other bias | Low risk | Baseline characteristics similar between groups. |
| Methods | RCT Parallel design Single centre The Wolfson Medical Center, affiliated to Tel‐Aviv University, Israel | |
| Participants | 213 women recruited to the study, 201 completed it. The remaining 12 completed the delivery quickly and did not require any analgesia. All participants (N = 192) with at least 2 hrs of labour were included in the data analysis. Analgesia was randomly provided for 1 of 4 treatment groups:
Eligibility: healthy women with singleton cephalic presentation at term and presenting in spontaneous active labour. | |
| Interventions | Analgesia was randomly provided for 1 of 4 treatment groups:
| |
| Outcomes |
| |
| Notes | The Wolfson Medical Center, affiliated to Tel‐Aviv University, Israel The remaining 12 completed the delivery quickly and did not require any analgesia. All participants (N = 192) with at least 2 hrs of labour were included in the data analysis. Dates: Not stated Funding: "Supported by NIH Grant GM 061655 (Bethesda, MD), the Gheens Foundation (Louisville, KY), the Joseph Drown Foundation (Los Angeles, CA), and the Commonwealth of Kentucky Research Challenge Trust Fund (Louisville, KY). Mallinckrodt Anesthesiology Products, Inc. (St. Louis, MO) donated the thermocouples we used. Exergen, Inc. (Boston, MA) donated the infrared skin‐temperature thermometer." Declarations of Interest: "None of the authors has any personal financial interest in this research." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was based on computer‐generated codes. |
| Allocation concealment (selection bias) | Low risk | Randomisation was based on computer‐generated codes that were maintained in sequentially numbered opaque envelopes until just prior to use. The randomisation envelopes were opened and the designated treatment started when the visual analogue pain score (VAPS) reached 30 mm. |
| Blinding of participants and personnel (performance bias) | Low risk | The treatment regimen was blinded for the evaluator anaesthesiologists by using 2 patient‐controlled analgesia machine devices (PCIA and PCEA) for every participant. A "dummy" IV saline infusion (PCIA) was attached to parturients with PCEA and the other was a "dummy" epidural catheter attached superficially to the skin and connected to a PCEA syringe in the group with PCIA with remifentanil. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Pathologist was blinded to participant group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 213 women recruited to the study, 201 completed it. The remaining 12 completed the delivery quickly and did not require any analgesia. All patients (N = 192) with at least 2 hrs of labour were included in the data analysis. |
| Selective reporting (reporting bias) | High risk | Actual figures for Apgar scores, heart rate, blood pressure and oxygen saturation not given ‐ just mentioned in narrative, last paragraph page 108 before Discussion. |
| Other bias | Low risk | All groups appear to be similar according to baseline characteristics. |
| Methods | Multicentre randomised controlled trial with individual randomisation | |
| Participants | 1414 women randomised (remifentanil PCA n = 709; epidural n = 705) (data analysed for 3158 women). Dutch consortium for women’s health and reproductivity. Academic hospitals, and general hospital Eligibility: women in secondary and tertiary care (intermediate or high risk), i.e. they have illnesses in their medical history that can affect pregnancy or that are affected by pregnancy or if they have complications in this or previous pregnancies or deliveries. Women were eligible to participate if they were healthy or had a mild systemic disease, aged 18 or older, and were scheduled to deliver vaginally after 32 weeks. Excluded: contradictions for epidural analgesia or hypersensitivity to 1 of the drugs used | |
| Interventions | Epidural analgesia: women could request this when they requested pain relief, according to local protocol. If pain relief was judged inadequate, women could receive patient‐controlled remifentanil instead of epidural analgesia. Remifentanil: patient‐controlled device was programmed to deliver 30 μg remifentanil (solution 20 µg/mL) on request with a lockout time of 3 mins. The dose could be increased to 40 μg in case of insufficient pain relief or decreased to 20 μg in case of excessive side effects. If pain relief was inadequate, women could request epidural analgesia. They were advised to discontinue using the device during the 2nd stage of labour to minimise the risk of neonatal side effects. Women did not receive any advice about continuing epidural analgesia during 2nd stage of labour. "Of the 709 women randomised to patient controlled remifentanil, 447 (65%) actually received analgesia during labour, compared with 52% (347) in the epidural analgesia group (relative risk 1.32, 95% confidence interval 1.18 to 1.48)." For data analysis in this review we used the number randomised. We did not count the women removed for elective caesarean section. Denominators used: Epidural ‐ 676 women; remifentanil ‐ 687 Difficult to interpret as only 347/676 received epidural, and 447/687 received rPCA. | |
| Outcomes | Mode of birth Satisfaction scores Oxytocin augmentation Maternal hypotension Maternal respiratory depression Side effects Apgar scores Admission to neonatal special care | |
| Notes | Country and setting: Netherlands, secondary care Dates of trial: May 2011 – October 2012 Funding: grant from ZonMW (Dutch Organization for Health Care Research and Development) Conflict of interest declared. All authors completed the ICMJE uniform disclosure form: "no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Web‐based randomised programme, randomised in fixed blocks of 3, stratified for centre and parity |
| Allocation concealment (selection bias) | Unclear risk | Allocation code appears after a participant’s initials were entered in to the randomisation programme. Research nurses/midwives as well as attending medical staff performed randomisation. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding was not possible because of the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | There is no information on who assessed or analysed the outcomes. Labour outcomes likely to have been recorded by caregiver. |
| Incomplete outcome data (attrition bias) | High risk | Of 709 allocated to remifentanil, 22 were excluded from final analysis due to elective planned caesarean, while in the epidural group 29 were excluded due to elective planned caesarean. In the epidural group, 3 women were lost to follow‐up, while 2 withdrew informed consent after randomisation. Used multiple imputation to correct for missing primary outcome data, imputed missing AUC values for satisfaction with pain relief and pain intensity using 20 imputed datasets. Other missing values were not imputed. Some outcomes were only reported for the women who received the analgesia. Number randomised was used for this review. |
| Selective reporting (reporting bias) | Low risk | Protocol is available and all prespecified outcomes are reported in the main trial. |
| Other bias | Unclear risk | No baseline imbalance but denominators unclear following exclusions for CS. Not all women received analgesia allocated. |
| Methods | Computer‐generated, in groups of 100, allocation was secured in a numbered and sealed envelope. Intention‐to‐treat analysis used. All women accounted for. | |
| Participants | 1223 women recruited (epidural N = 616, meperidine = 607). Eligibility: nulliparous and parous women in spontaneous labour (regular contractions, at least 3 cm dilated), singleton, cephalic presentation, cervix < 5 cm dilated | |
| Interventions | CSE: preload with 500 mL sodium lactate. Catheter L2 ‐ 3 or L3 ‐ 4 interspace. Spinal block with 10 µg sufentanil in 2 mL normal saline. Needle‐through‐needle approach. Following dissipation of spinal analgesia, epidural analgesia achieved with 0.25% bupivacaine in 3 ‐ 5 mL increments to achieve T10 ‐ T8 sensory level. This was followed by epidural infusion 0.125% bupivacaine and 2 microgram per mL fentanyl at 8 mL/h. Rate of infusion halved during 2nd stage of labour. | |
| Outcomes | Maternal: intrapartum visual analogue pain score and postpartum overall satisfaction with labour analgesia, oxytocin, mode of delivery, hypotension, meconium, surgical amniotomy, motor block, fever, itch, operative vaginal delivery | |
| Notes | University of Texas, USA. Amniotomy routinely performed in active labour when fetal head is well applied to cervix. Intrauterine pressure catheter used to assess adequacy of contraction if progress < 1 cm/hr and oxytocin augmentation employed if uterine pressure < 200 montevideo units. Dates: Trial carried out 1994 ‐ 1995 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated in groups of 100 |
| Allocation concealment (selection bias) | Unclear risk | Numbered sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Cross‐over participants were analysed in their original groups. |
| Selective reporting (reporting bias) | High risk | Additional outcome (Apgar score) reported in tables not specified in the Methods section. |
| Other bias | Low risk | None evident |
| Methods | Reported to be a prospective randomised controlled study but methods not described. Women randomised into equal‐sized groups. | |
| Participants | 100 women randomised (epidural, N = 50; no epidural, N = 50) Eligibility: healthy, nulliparous women in active labour with 3 ‐ 5 cm cervical dilatation, 3 ‐ 5 contractions in 10 mins, healthy with singleton fetus at term (37 ‐ 41 weeks’ gestation), no evidence of cephalopelvic disproportion Exclusion: amniotic fluid deficiency or fetal heart rate non‐reactivity | |
| Interventions | Group 1: epidural. N = 50 2 cc test with 40 mg lidocaine; after 5 mins provided woman had no motor block and experienced pain relief, 4 cc of 0.5 bupivacaine and 50 mg of fentanyl were diluted in 0.9% saline and administered as a bolus injection. 5 ‐ 10 cc further administered as needed. Women were in bed in left lateral position. If they had fewer than 3 contractions in 10 mins labour was augmented with oxytocin. Group 2: not described. No epidural analgesia. N = 50 It was not clear whether women received other pharmacological analgesia or whether the same protocol was followed in case of any delay in labour. | |
| Outcomes | Mode of birth Side effects Duration of labour Hypotension | |
| Notes | Trial conducted at hospital in Izmir, Turkey. Dates of trial: July 2012 ‐ August 2014 Funding: not reported Conflicts of Interest: the authors reported no conflicts of interest. It was stated for women in the epidural group that if contractions were less than 3 in 10 mins oxytocin was administered. Not clear if the same protocol was used for the control group, so length of 1st stage may be meaningless (more in the ED group may have had oxytocin – this was not clear). Epidural mean 217.9 min (166.33); no epidural 258.87 (158.48) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described although there were equal‐sized groups |
| Blinding of participants and personnel (performance bias) | High risk | Participants and staff would be aware of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Most outcomes were recorded during labour by staff providing care, so susceptible to bias. |
| Incomplete outcome data (attrition bias) | Unclear risk | Women who had CS were excluded from the analysis. No other loss to follow‐up was reported. Not clear |
| Selective reporting (reporting bias) | Unclear risk | We have no protocol for this study. The intervention was not well described for the comparison group. There did not seem to be a power calculation. |
| Other bias | Unclear risk | The main outcome was duration of labour. There was a clear description of what happened for any delay for women in the intervention group (oxytocin augmentation). It was not clear that women in the non‐epidural group had the same treatment in case of delay. |
| Methods | Random allocation by drawing lots. All women accounted for | |
| Participants | 90 women recruited (epidural N = 30, phenoperidine N = 30, no analgesia N = 30) | |
| Interventions | Epidural: preload not mentioned. Epidural delivery of 12 mL of 1.5% lidocaine in 1:20,000 adrenaline. Followed by top‐ups of 6 mL lignocaine as needed | |
| Outcomes | Maternal: mode of delivery, blood gases and pH | |
| Notes | Toulouse, France Dates: Year trial carried out not stated Funding: Not stated in translation Declarations of Interest: Not stated in translation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Participants were drawn by lots, no further information given |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
| Methods | RCT Parallel design Multicentre Canada | |
| Participants | 242 parturients enrolled and assigned to the PCIA group (N = 118) and the PCEA group (N = 124) Eligibility: nulliparous women with healthy term (37 ‐ 42 weeks' gestation) pregnancies from 4 tertiary‐care Canadian centres. ASA I or II in spontaneous labour with singleton pregnancy in vertex presentation | |
| Interventions | Patient‐controlled epidural analgesia (PCEA) with 0.08% bupivacaine and fentanyl 1.6 µg/mL; N = 124 Patient‐controlled IV opioid analgesia (PCIA) with fentanyl; N = 118 | |
| Outcomes |
| |
| Notes | Multicentre ‐ 4 tertiary‐care centres, Canada 51 participants (43%) in the PCIA group received epidural analgesia: 39 (33%) because of inadequate pain relief and 12 (10%) to facilitate operative delivery. Dates: Trial carried out September 1997 ‐ December 1999 Funding: Supported by Physicians Services Incorporated Foundation, Toronto; Alberta Heritage Fund; Clinical Teaching and Research Grant, College of Medicine, University of Saskatchewan; Medical Services Incorporated of Alberta; Grace Maternity Research Foundation Grant; and Dalhousie University Department of Anaesthesia Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly assigned to one of two treatment allocations by using a computer‐generated random number system." |
| Allocation concealment (selection bias) | Low risk | "Each centre was randomised separately at a central location. Each centre received sealed, consecutively numbered opaque envelopes that were randomised in blocks of 20." |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | The data were analysed according to group assignment (intention‐to‐treat). |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported within the Methods section are available within the Results. |
| Other bias | High risk | According to sample size calculation ‐ 485 participants per group needed ‐ actually recruited 242 patients. "A priori we decided to inspect neonatal data after enrolling 200 patients to ensure neonatal safety. We also decided to stop the study after 2 yr of enrolment, regardless of the number of patients." All groups appear to be similar according to baseline characteristics. |
| Methods | Computer‐generated block randomisation, stratified according to gestational age (< 35 weeks versus ≥ 35 weeks). Numbered, sealed, opaque envelopes. Intention‐to‐treat analysis used. All women accounted for | |
| Participants | 116 women recruited (meperidine N = 60, epidural N = 56). | |
| Interventions | Epidural: preload 250 ‐ 500 mL sodium lactate over 20 mins. Epidural catheter placed in L3 ‐ L4 interspace. Test dose of 0.25% bupivacaine 3 mL, then incremental bolus doses of 3 ‐5 mL 0.25% bupivacaine to obtain T‐10 sensory level, maintained by continuous infusion of 0.125% bupivacaine with 2 microgram fentanyl at rate of 10 mL/hr. | |
| Outcomes | Maternal: intrapartum visual analogue pain score, mode of delivery, woman's satisfaction with pain relief, hypotension, headache, eclampsia, acute renal dysfunction | |
| Notes | Alabama, USA Dates: "42 month study period" Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated block randomisation schedule |
| Allocation concealment (selection bias) | Low risk | Consecutively‐numbered, sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | 10 women did not receive the assigned treatment, 3 in the epidural group and 7 in the opioid group. Rapid labour was the most common event that precluded the assigned treatment (epidural, n = 3 versus opioid, n = 5). 1 woman assigned to the opioid group received epidural analgesia at the discretion of the attending anaesthesiologist. Another woman who was assigned to opioids received epidural analgesia after experiencing severe nausea. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the Methods section have been reported on in the Results section. |
| Other bias | Low risk | None evident |
| Methods | "Randomized clinical trial." | |
| Participants | 105 women recruited (epidural N = 53, meperidine N = 52) | |
| Interventions | Epidural analgesia versus IV PCA with meperidine. No further information in abstract | |
| Outcomes | Maternal: caesarean section, pain score, satisfaction score, maternal ephedrine administration | |
| Notes | Birmingham, Alabama, USA Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | 10 participants did not received the assigned intervention. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
| Methods | Computer‐generated randomisation at the time of request for pain relief. Intention‐to‐treat analysis used. Outcome assessor for backache blinded. All women accounted for, with the exception of backache (17% loss to follow‐up at 26 months). | |
| Participants | 369 women recruited (epidural N = 184, non‐epidural N = 185). Eligibility: labouring nulliparous women at term with singleton pregnancy and cephalic presentation, with no contraindication to either form of analgesia. | |
| Interventions | Preload not stated. 10 mL of 0.25% bupivacaine. Followed by top‐ups of 0.25% 5 ‐ 10 mL as required. Pethidine: 50 ‐ 100 mg IM pethidine, repeated according to standard midwifery practice. Women in both groups allowed to use Entonox. | |
| Outcomes | Maternal: mode of delivery, length of labour, use of oxytocin, maternal satisfaction with pain relief, backache, postnatal depression, not feeling in control, drowsiness, concerns regarding pain relief, catheterisation postdelivery, postnatal haemoglobin, maternal blood loss at delivery | |
| Notes | North Staffordshire, UK Dates: Trial carried out 1992 ‐ 1997 Funding: "The study was funded by WellBeing, and Ms P. Upton was supported by a grant from the North Staffordshire Medical Institute. The clinical trials work of Mr Richard Johanson and Ms Linda Lucking is supported by a grant from the NHS(E) West Midlands Research and Development Programme." Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Allocation was displayed on the computer screen. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Women in the epidural and non‐epidural groups remain in the group to which they were initially allocated, regardless of the eventual method of pain relief given during labour. |
| Selective reporting (reporting bias) | High risk | Outcomes not all prespecified in Methods section. |
| Other bias | Low risk | None evident |
| Methods | 3‐armed RCT with individual randomisation 3 blocks of 380 participants. | |
| Participants | 1140 women recruited (epidural anaesthesia, N = 380; remifentanil group by patient‐controlled IV analgesia, N = 380; combined spinal‐epidural, N = 380). Eligibility: healthy nulliparous pregnant women (with term, singleton pregnancies), who spontaneously went into established labour (with at least 2 painful uterine contractions in 10 mins and the cervix is at least 80% effaced and up to 3 cm dilated) and requesting labour analgesia. Exclusion: (1) Allergy to opioids, a history of the use of centrally‐acting drugs of any sort, chronic pain, and psychiatric diseases records (2) Participants < 18 years or > 40 years (3) Those who were not willing to or could not finish the whole study (4) Alcohol‐ or opioid‐dependent women were excluded for their influence on the analgesic efficacy of the epidural analgesics (5) Women with a non‐vertex presentation or scheduled induction of labour (6) Women with diabetes mellitus and pregnancy‐induced hypertension (7) Twin gestation and breech presentation (8) Any contraindication to neuraxial or systemic opioid analgesia (9) Cervical dilation of 4 cm or more (10) Estimated fetal weight above 4000 g and abnormal fetal heart rate tracing on admission | |
| Interventions | Group 1: epidural anaesthesia (N = 380) All blocks were performed in the sitting position. The epidural space was located at the L3 – L4 interspace using loss of resistance to air (an 18‐gauge Tuohy needle was used). In both groups, a 3‐mL epidural test dose of 2% lidocaine was given through the epidural catheter. In the EA (Group I), after the test dose, an 8‐mL dose of 0.125 % levobupivacaine with 2 lg/mL fentanyl was administered through the epidural catheter. Then the catheter was connected to an electronic pump set to deliver a continuous infusion of 8 mL/hr of 0.125 % levobupivacaine and 2 lg/mL fentanyl. Further boluses of 5 – 10 mL of 0.125 % levobupivacaine were given by the attending anaesthesiologist upon request. Group 2: remifentanil group by patient‐controlled IV analgesia (N = 380) The PCIA device was set to deliver 0.1 ug/kg of Ultiva (remifentanil hydrochloride, Glaxo Operations UK Ltd, Barnard Castle, Durham, UK), diluted with saline and given as a solution of 25 ug/mL as a bolus infused during a period of 1 min, with a lockout time of 1 min, into an IV catheter attached to a 1‐way line providing continuous infusion of saline at approximately 100 mL/hr. During the study, the IV PCIA bolus was increased following a dose escalation scheme (0.1 – 0.2 – 0.3 – 0.5 – 0.7 – 0.9 ug/kg) after every 2nd contraction until the parturient answered ‘no’ to the question whether she would like to get more efficient pain relief or until a maximum dose of 0.9 ug/kg was achieved. Group 3: combined spinal–epidural (N = 380) A needle‐through‐needle technique was performed with 2 mg levobupivacaine and 15 lg fentanyl (total volume of 2 mL) injected intrathecally and the spinal needle removed. Then the epidural catheter was inserted and connected to an electronic pump set to deliver the same previously‐mentioned mixture. | |
| Outcomes | Pain score Mode of birth Oxytocin augmentation Side effects Duration of labour Satisfaction with pain relief Apgar scores Cord blood gases | |
| Notes | Motor block levels according to the Bromage scale (Groups I and III) and sedation levels according to the Ramsay scale (Group II) were observed. Decisions regarding obstetric management were made by the obstetricians. Artificial rupture of membranes was performed (if there was no ROM), and oxytocin infusions were titrated according to our hospital protocol. All participants had continuous external electronic fetal heart rate monitoring and tocodynamometry. Trial conducted at TAIBA Hospital in Kuwait. Dates of trial: September 2009 ‐ August 2011 Funding: not stated Conflicts of Interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The participants were randomised (in 3 blocks of 380 participants per block) through a computer‐generated, random‐number list to receive either EA (Group I), or patient‐controlled IV analgesia (PCIA) with remifentanil (Group II) or combined spinal–epidural (CSE) analgesia (Group III). The random‐number list was generated by means of the QuickCalcs (GraphPad Software Inc., La Jolla, CA, USA). |
| Allocation concealment (selection bias) | Low risk | The group assignment numbers were sealed in an envelope and kept by the study supervisor. |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible to blind participants or caregivers as mode of administration varied. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome data reported to be collected at time of delivery or the day after by assessors not involved in the woman’s care. However, labour outcomes would be recorded by staff providing care. ? e.g. VAS completed hourly during labour. |
| Incomplete outcome data (attrition bias) | Low risk | No post‐randomisation exclusions, no loss to follow‐up reported. 320 excluded prior to randomisation because they did not fit the inclusion criteria. Intention‐to‐treat analysis: no loss to follow‐up or protocol deviations reported (it was not clear how many women actually received the allocated analgesia). |
| Selective reporting (reporting bias) | Low risk | No, no protocol available but all outcomes reported from Methods text and all expected outcomes reported. |
| Other bias | Low risk | No baseline imbalance. Funding source not disclosed |
| Methods | Randomisation with Tippets random number table into 3 groups. Allocation was concealed using sealed, opaque envelopes (information obtained directly from trial authors). All women accounted for | |
| Participants | 126 women recruited (epidural N = 43, meperidine N = 39, tramadol N = 44) | |
| Interventions | Preload not mentioned. | |
| Outcomes | Maternal: mode of delivery, pain score, maternal satisfaction with pain relief, duration of 1st and 2nd stages of labour, hypotension, urinary retention, respiratory depression, desire to use same pain relief in future | |
| Notes | Chandigarh, India Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tippets random table |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed using sealed, opaque envelopes (information obtained directly from trial authors). |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 2 from group I delivered by caesarean section before analgesia could be given. |
| Selective reporting (reporting bias) | High risk | Outcomes documented in Methods section not reported ‐ PPH and neonatal sepsis |
| Other bias | Low risk | None evident |
| Methods | RCT. Unit of randomisation not clear, probably individual | |
| Participants | 36 women (Samanta), and 20 women (Jain) randomised (epidural N = ?, tramadol N = ?). Eligibility: pregnant women at term gestation with sonographic evidence of umbilical artery systolic‐diastolic ratio ≥ 3 (FGR) | |
| Interventions | Epidural parturients received an incremental bolus of 10 mL ropivacaine 0.1% with 2ì/mL fentanyl followed by 5 ‐ 15 mL/hr continuous infusion of the same drug. Tramadol parturients received intramuscular tramadol 1 mg/kg repeated every 4 hrs. | |
| Outcomes | Changes in doppler pulsality index Apgar scores Cord blood gases | |
| Notes | Authors contacted for more information Trial conducted in India but no further detail given. Dates of trial: not stated Funding: not stated Conflicts of Interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Infeasible to blind this intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome collection during labour so likely recorded by staff providing care that would be aware of allocation. |
| Incomplete outcome data (attrition bias) | High risk | Jain reports 20 women randomised – data only analysed for 14. Samanta reports 36 women randomised – data only analysed for 30. Not clear how many women were in this study or why 6 were excluded post‐randomisation. |
| Selective reporting (reporting bias) | Unclear risk | Unable to assess from abstract |
| Other bias | Unclear risk | Unable to assess from abstract |
| Methods | 3‐arm RCT with individual randomisation | |
| Participants | 90 women randomised (tramadol via epidural N = 30, tramadol IV N = 30, control N = 30) Eligibility: 37 ‐ 41 weeks of pregnancy, primipararous and multipararous women in established active stage of labour (uterine contraction 2 per 10 mins, lasting for 30 to 40 s and cervical dilation > 3 cm) with vertex presentation and willing for analgesia Exclusion: malpresentation, cephalopelvic disproportion, previous caesarean section, antepartum haemorrhage, any medical complications (diabetes, asthma, primary pulmonary hypertension, hypertensive disorders of pregnancy, etc.) | |
| Interventions | Tramadol via epidural: tramadol in doses of 1 mg/kg body weight along with 8 ‐ 10 mL of 0.25% bupivacaine was given by epidural route, N = 30 Tramadol IV: tramadol in doses of 1 mg/kg body weight IV bolus and 100 mg in 500 ml Ringer’s lactate drip at the rate of 8 ‐ 24 drops/min was given, N = 30 Control Group: control not described. No information whether women in the control group received any analgesia or whether they were denied analgesia (all of this group reported moderate to intolerable pain), N = 30 | |
| Outcomes | Pain intensity Satisfaction with pain relief Spontaneous birth | |
| Notes | No information whether women in the control group received any analgesia or whether they were denied analgesia (all of this group reported moderate to intolerable pain). Conducted in the Department of Obstetrics & Gynaecology, S.N.Medical College, Agra, India Dates of trial: not stated. Study accepted by journal 2010 Funding: not stated Conflicts of Interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | States “randomly divided”, although also says that the study group was subdivided into 2 groups. Not clear whether this was done randomly or not, or how many went into each group (although in tables results are reported for 30 women in each group). |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | High risk | Infeasible to blind women or staff |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned – probably high, as outcomes relate to labour and staff providing care would also have recorded outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Appears to report all, but numbers in each group not clearly stated. Not clear in tables whether all data are reported. Unclear if ITT |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not prespecified in Method text |
| Other bias | Unclear risk | Similar baseline characteristics. The methods were generally not clear |
| Methods | RCT with individual randomisation | |
| Participants | 192 women randomised (epidural n = 94; pethidine n = 98) Eligible: women in labour with ASA 1 ‐ 11, gravida 2 ‐ 5 with tested pelvis, spontaneous onset of labour, age between 18 ‐ 40 years old, singleton fetus with cephalic presentation, presenting OS 3 ‐ 5 cm, height more than 150 cm, and weight less than 100 kg Excluded: bad obstetric history, post‐date, history of allergy to local anaesthetic, patient refusal, failed epidural and those who had contraindications for epidural analgesia | |
| Interventions | Epidural (n = 94) Received IV fluid bolus of at least 500 mL of Ringer’s Lactate solution. Lumber epidural analgesia was achieved using an indwelling catheter inserted by 18‐gauge Tuohy needle at L2 ‐ L3 or L3 ‐ L4 interspaces. A 3‐mL test dose of 0.2% ropivacaine was given followed by a bolus dose making the total dose of 12 mL. This was followed by continuous epidural infusion of 0.2% ropivacaine with 2 ug/mL fentanyl at 7 ‐ 10 mL/hr. Pethidine IM (n = 98) 75 ‐ 100 mg IM pethidine with 25 mg promethazine hydrochloride at first request of pain relief. Additional 75 mg of pethidine were given by request to a maximum of 300 mg in 4 hrs. Both groups were able to self‐administer nitrous oxide. | |
| Outcomes | Mode of birth Oxytocin administration Apgar scores Pain score Satisfaction score Duration of labour | |
| Notes | Setting: hospital setting in Malaysia Dates of trial: 2005 ‐ 2006 Funding: Universiti Sains Malaysia short‐term grant no. 304/ppsp/613131 Conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “A trained staff nurse would choose an envelope to allocate the patient randomly (closed envelope technique).” |
| Allocation concealment (selection bias) | Unclear risk | “A trained staff nurse would choose an envelope to allocate the patient randomly (closed envelope technique).” It was not stated how the sequence was generated, whether the envelopes were sealed, in sequential order and all accounted for. |
| Blinding of participants and personnel (performance bias) | High risk | Authors say women were blinded to the expected effects of epidural but they cannot have been blind to intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Not clear who recorded outcomes, assuming it was care provider in labour |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up reported, data reported for each participant. It was not stated if there were any missing data for any outcomes. |
| Selective reporting (reporting bias) | Low risk | Outcomes prespecified in the Methods are all reported clearly. We did not have a study protocol. All expected outcomes reported. |
| Other bias | Unclear risk | Baseline characteristics similar in both groups. The clinical management of women in the 2 groups varied and this made it difficult to interpret some results. |
| Methods | RCT with individual randomisation | |
| Participants | 86 women randomised (epidural n = 42; inhaled nitrous oxide n = 44) Eligibility: nulliparous women, consent given for analgesia, no contraindication for vaginal delivery, single pregnancy, gestational age ≥ 37 weeks, cephalic presentation, active phase of labour (cervical dilatation 3 ‐ 5 cm with contractions occurring at least once every 3 mins), no contraindication for regional analgesia (coagulopathy disorder, infections in the site of catheter insertion, and haemodynamic instability) Excluded: labour arrest, maternal or fetal problems which need caesarean, previous caesarean | |
| Interventions | Epidural (n = 42) Epidural group were placed in sterile conditions, and after hydration by 500 mL ringer lactate, epidural was entered to epidural space from lumbar site L3 ‐ L4 or L4 ‐ L5 with Tuohy needle size 18, then it was entered 4 ‐ 6 cm into the space and then epidural needle was removed and catheter was fixed in the site using suture. The participant was controlled in the view of labour development and fetal heart monitoring. When dilatation was 5 cm, 1st dose including bupivacaine 0.125%, fentanyl 1 μg/mL in volume of 8 ‐ 10 mL was injected at the beginning. Then dilution solution was infused with speed of 8 ‐ 15 mL/h related to the participant’s need. If it was required, the concentration of bupivacaine was increased to 0.25%. Inhaled nitrous oxide (n = 44, data for 42) Inhaled nitrous oxide by a mask simultaneously with beginning of feeling contraction by mother. In pain intervals, mask was removed and room air was inhaled by mother. "2 mothers didn't continue the study due to giddiness and they were excluded from the study." | |
| Outcomes | Satifaction with pain relief Mode of birth | |
| Notes | Describe setting: hospital setting in Iran Dates of trial: 10 May 2010 – 10 May 2011 Funding: Women’s Health Research Center of Mashhad University of Medical Sciences Conflicts of interest: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly divided into 2 groups by means of random numbers of calculator |
| Allocation concealment (selection bias) | Unclear risk | Concealment not mentioned |
| Blinding of participants and personnel (performance bias) | High risk | Infeasible to blind |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned, assuming not blinded and caregiver collected information |
| Incomplete outcome data (attrition bias) | High risk | 2 women withdrew consent following randomisation – no reason given. Women who had a caesarean section for fetal distress were excluded, although unclear how many women this applied to. 2 women were excluded due to ‘giddiness’ in the Entonox group. Difficult to assess this domain due to poor reporting. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available and although outcomes are reported as prespecified in Methods section, outcome data are not reported clearly |
| Other bias | Unclear risk | Similar baseline characteristics but poor reporting |
| Methods | RCT Parallel design China | |
| Participants | 75 voluntary pregnancies were randomised: group A (N = 25), Group B (N = 25), Group C (N = 25). Eligibility: ASA I ‐ II, primiparous with completely normal pregnancy and labour stage of cervical os opening 2 ‐ 3 cm | |
| Interventions | Group A (N = 25) ‐ control ‐ no medicine to ease pain Group B (N = 25) ‐ epidural analgesia ‐ combination of ropivacaine and fentanyl firstly with a dose of 10 mL by way of cavitas epiduralis, then additional 5 mL was carried over with the assurance of uncavitas subarachnoidealis Group C (N = 25) ‐ CSE analgesia | |
| Outcomes |
| |
| Notes | Data limited as only abstract available. Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract only available |
| Allocation concealment (selection bias) | Unclear risk | Abstract only available |
| Blinding of participants and personnel (performance bias) | Unclear risk | Abstract only available. Insufficient information |
| Blinding of outcome assessment (detection bias) | Unclear risk | Abstract only available. Insufficient information |
| Incomplete outcome data (attrition bias) | Unclear risk | Abstract only available |
| Selective reporting (reporting bias) | Unclear risk | Abstract only available |
| Other bias | Unclear risk | Abstract only available |
| Methods | Reported to be randomised trial with individual women randomised. | |
| Participants | 120 women randomised (epidural PCEA, N = 30; PCIA ondansetron, N = 30; Acu‐stimulation, N = 30; no analgesia, N = 30) Eligibility: no previous poor obstetric outcome, no experience of Hans acupoint nerve stimulator and TENS, term pregnancy (> 37 weeks’ gestation), active stage of 1st stage with cervical dilatation 3 cm Exclusion: allergy to study drugs, maternal morbidity such as mental or neurological disease affecting evaluation of pain, pregnancy complications such as gestational hypertension, gestational diabetes, gestational thyroid disease, had already taken analgesia or had long‐term use of analgesic drugs, had already used sedative drugs in labour, had low or high BMI (< 18.5 or > 25 kg/m2) | |
| Interventions | 3 study groups: all treatments stopped at full dilatation. 30 women in each Group 1 ‐ epidural PCEA. Combined spinal 3 mg ropivacaine, epidural 100 mL 0.1% ropivacaine and 50 mcg of sufentanil; background infusion 5 mL, PCA dose 5 mL with 10 minute lockout Group 2 ‐ PCIA ondansetron 8 mg, 5 mins later 1.5 mg/kg tramadol, with 50 mL 0.7 tramadol and 8 mg ondansetron background and 2 mL PCA dose, with 10‐min lockout Group 3 ‐ Acu‐stimulation. Pulse stimulus at acupoints – Jiaji points (T 10 ‐ L3) and Ciliao (BL 32). 100 Hz with burst frequency 2 Hz, intensity 15 ‐ 30 mA, pulse duration 30 minutes Group 4 ‐ control. No analgesia | |
| Outcomes | Pain Duration of labour Mode of birth Oxytocin augmentation Maternal hypotension Side effects Neonatal asphyxia | |
| Notes | Trial conducted at hospital in Bejing, China. Dates of trial: August 2010 – November 2013 Funding: not stated Conflicts of Interest: not reported Data from groups 2, 3, and 4 combined to form overall comparison group. Maternal hypotension EA 1/30, Control 0/90 Neonatal asphyxia EA 1/30, Control 6/90 Pain after 1 hour EA 20 (6), Acu 65 (12), Opiate 45 (8), Control 97 (14) Duration of 1st stage EA 423.3 (181.2), Acu 430.1 (119.8), Opiate 425.2 (198.7), Control 439.6 (200.3) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reports using random‐number tables |
| Allocation concealment (selection bias) | Unclear risk | Not described, reports using random‐number tables but there were 4 equal‐sized study groups (30 women in each) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and caregivers would be aware of interventions. |
| Blinding of outcome assessment (detection bias) | High risk | Not reported although most outcomes were recorded in labour by staff providing care. |
| Incomplete outcome data (attrition bias) | Unclear risk | There were some discrepancies between tables, While the study flow diagram suggests there were 40 women in each group, the results tables report results for 120 women (30 in each group). There was no report of any missing data. The denominators for mean duration of labour appear to include all women (i.e. women having CS were not excluded). |
| Selective reporting (reporting bias) | Unclear risk | No protocol. There was no power calculation. |
| Other bias | Unclear risk | Groups appeared similar at baseline. The equal‐sized study groups, discrepancies between tables and lack of clarity regarding denominators make the results difficult to interpret. |
| Methods | Multicentre open‐label randomised trial with individual randomisation (described as randomised equivalence trial) in 18 midwifery practices in the Netherlands, positioned within the Dutch Obstetric Consortium for women’s health research | |
| Participants | 418 randomised before labour (IV remifentanil, n = 208; epidural, n = 210). Eligibility: low‐risk women beyond 32 weeks of gestation under the care of primary‐care midwives were eligible. Excluded: women < 18 years, women with a contraindication for epidural analgesia or a hypersensitivity to opioid and women in whom labour had already started were not eligible. | |
| Interventions | Intravenous remifentanil patient‐controlled analgesia (RPCA) (n = 208 – 203 analysed): Intravenous remifentanil 30‐lg boluses (solution 20 lg/mL) with a lockout time of 3 mins and without background infusion. A doctor or a midwife and a nurse were responsible for providing and monitoring the RPCA. The RPCA was administered by the parturient herself after instruction on how to use RPCA in the most beneficial way, which is to use the bolus dose just before the anticipated contraction. It was possible to increase the bolus dosage to 40 lg in case of insufficient pain relief, or to decrease the dose to 20 lg in case of excessive side effects. Epidural anaesthesia (n = 210 – 206 analysed): EA with a loading dose of 25 mg (12.5 mL ropivacaine 0.2%) and continuous infusion of ropivacaine 0.1% plus sufentanil 0.5 lg/mL was administered. Continuous infusion was used at a variable rate defined by the anaesthetist and the local protocol. Additional boluses were used for inadequate levels of analgesia. | |
| Outcomes | Pain intensity Satisfaction Mode of birth Maternal respiratory depression Headache Fever PPH Apgar scores Duration of 2nd stage | |
| Notes | Country and setting: Netherlands Dates of trial: November 2012 ‐ June 2013 Funding: no funding sources stated. “For this study we did not receive funding or supplies (such as financial supply or supply of drugs).” ZonMW (www.zonmw.nl) Conflicts of interest: stated on website – cannot find. Only 94/203 received RPCA, and 76/206 received EA ‐ authors contacted for more information. Data for pain intensity reported as "area under the curve" ‐ unusable data. Reports that "among women who actually received analgesia scores for satisfaction with pain relief were significantly lower in the rPCA group compared with the EA group." 23/94 women in Epidural group, and 35/76 women in rPCA reported satisfaction with analgesia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Performed using a web‐based randomisation programme stratified for midwifery practice and parity Randomisation was done before labour. |
| Allocation concealment (selection bias) | Unclear risk | "Both the woman and the midwife knew the randomisation allocation in case a request for pain relief should occur during labour." |
| Blinding of participants and personnel (performance bias) | High risk | Women and midwife knew the randomisation allocation. Not feasible to blind these interventions. |
| Blinding of outcome assessment (detection bias) | High risk | Not mentioned, assumed not blinded. |
| Incomplete outcome data (attrition bias) | High risk | 9 removed after randomisation for elective section (5 in RPCA group, 4 in EA group). “If analgesia with the randomly allocated pain method was insufficient according to the woman, a switch to the other trial arm was allowed.” Reported to be intention‐to‐treat with only ElCS women excluded from analysis, although side effects were only reported for those women receiving allocated intervention? There were missing data for some outcomes. Some outcomes were only reported for the women who received the analgesia. We used number randomised for this review. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported. The primary outcome was changed before analysis from satisfaction with pain relief at given time points to area under the curve. |
| Other bias | Unclear risk | Similar baseline characteristics 94/203 women in RPCA group received analgesia (105 requested pain relief). 76/206 women in epidural group received analgesia (101 requested pain relief). Results from this study were very difficult to interpret as fewer than half of the women received the allocated intervention. (Authors contacted for more information) |
| Methods | "Randomly divided into 3 groups." No further information. Intention‐to‐treat analysis used. All women accounted for | |
| Participants | 80 women recruited (CSE N = 30, tramadol N = 20, no analgesia N = 30). Eligibility: women at 37 ‐ 41 weeks' gestation in spontaneous, uncomplicated labour, aged between 23 and 32 years, ASA I ‐ II and expected to have vaginal delivery | |
| Interventions | Group 1 CSE: preload not mentioned, spinal administration of 2.5 mg ropivacaine with 5 micrograms of fentanyl. Epidural mixture of 0.1% ropivacaine and 1.5 micrograms of fentanyl PCEA infusing at 4 mL/h with PCEA dose of 4 mL and lockout time of 15 mins | |
| Outcomes | Maternal: pain scores, motor block assessed with modified Bromage score, duration of 1st and 2nd stages of labour, caesarean section, sedation, nausea and vomiting, urinary retention, post‐dural puncture headache | |
| Notes | Beijing, China Trial did not record side effect data for no‐analgesia group. Dates: Year trial carried out not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants randomly divided in to 3 groups. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Low risk | All outcomes in the Methods section have been reported on in the Results section. |
| Other bias | Unclear risk | Insufficient information |
| Methods | Computerised random‐number allocation, sealed, opaque envelopes. Intention‐to‐ treat analysis used; however, backache (at 6 months) analysed on data of women who responded to questionnaire only. Secondary analysis based on actual analgesia received. All women accounted for, with the exception of backache (17% loss to follow‐up at 6 months). | |
| Participants | 614 women recruited (epidural N = 304, pethidine N = 310). | |
| Interventions | Epidural: 0.25% bupivacaine 10 mL followed by infusion of 0.125% bupivacaine at 10 mL/hr until 2nd stage Lignocaine 2% was administered for instrumental or caesarean delivery | |
| Outcomes | Maternal: mode of delivery, long‐term backache, duration of 1st and 2nd stages of labour, oxytocin augmentation, pain scores | |
| Notes | Northwick Park, England Dates: Trial carried out 1992 ‐ 1995 Funding: National Health Service Executive, North Thames Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised number generation |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelope |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | All participants analysed in their original groups with no loss |
| Selective reporting (reporting bias) | Low risk | All outcomes in the Methods section have been reported on in the Results section. |
| Other bias | Low risk | No obvious signs of other bias |
| Methods | Computer‐generated numbers, in opaque, sealed envelopes | |
| Participants | 738 women randomised (epidural N = 372, meperidine PCIA N = 366) | |
| Interventions | Epidural: preload with 500 mL sodium lactate. Epidural analgesia achieved with boluses of 0.25% bupivacaine to T10 level of sensory analgesia, followed by continuous infusion of 0.125% bupivacaine with 2 mg/mL of fentanyl titrated to maintain analgesia | |
| Outcomes | Maternal: duration of 1st and 2nd stages of labour, hypotension, fever, oxytocin augmentation, mode of delivery, ephedrine use, pulmonary oedema, postpartum oliguria, postpartum weight loss | |
| Notes | Texas, USA Dates: Trial carried out 1996 ‐ 1998 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Low risk | Sealed, numbered opaque envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 77 women did not receive treatment as specified by the protocol, but analyses were reported as to intention‐to‐treat. |
| Selective reporting (reporting bias) | High risk | Outcomes documented in Methods section not reported ‐ serial laboratory values that included haematocrit level, platelet count, creatinine level, and liver enzymes. |
| Other bias | High risk | Nulliparous women, more of whom were assigned to the PCIA group (P = 0.005). |
| Methods | "Randomised into 2 groups", no further information given. Intention‐to‐treat analysis used | |
| Participants | 129 women recruited (epidural N = 69, no analgesia N = 63) | |
| Interventions | Epidural bupivacaine versus no analgesia. No further information in abstract | |
| Outcomes | Maternal: duration of 1st and 2nd stages of labour, pain scores | |
| Notes | Sinaloa, Mexico Dates: Trial carried out 1997 ‐ 1998 Funding: Not stated in translation Declarations of Interest: Not stated in translation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised into 2 groups |
| Allocation concealment (selection bias) | Unclear risk | Randomly divided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Low risk | All outcomes in the Methods section have been reported on in the Results section. |
| Other bias | Unclear risk | Insufficient information |
| Methods | RCT Double‐blind, randomised, cross‐over fashion Single centre University of Saskatchewan, Canada | |
| Participants | 100 labouring parturients assigned to IV fentanyl group (N = 50) or the epidural fentanyl group (N = 50) Eligibility: ASA I and II labouring parturients requesting epidural | |
| Interventions | IV fentanyl group (N = 50) ‐ 100 µg fentanyl IV and saline by an epidural catheter Epidural fentanyl group (N = 50) ‐ saline IV and 100 µg fentanyl by an epidural catheter | |
| Outcomes |
| |
| Notes | Single centre ‐ Canada Cross‐over ‐ at 2 hrs those participants who had not yet delivered were crossed over to the other study medication by the alternate route. Out of 100 labouring parturients, 41 crossed over to receive fentanyl by the alternate route ‐ does not specify how many from each group crossed over. Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Low risk | An anaesthetist initially prepared the syringes with either fentanyl or saline. These were then allocated by a separate study nurse: "These syringes together with labels enclosed in a randomisation envelope were given to an attending nurse who then re‐labelled the syringes, "epidural" or "intravenous", according to instructions within the envelope". |
| Blinding of participants and personnel (performance bias) | Unclear risk | Described as "double blind". |
| Blinding of outcome assessment (detection bias) | Unclear risk | "An anaesthetist blinded to the route of administration questioned each patient with regard to changes in analgesia, level of sedation, dizziness, or euphoria. He or she then guessed as to whether this patient had received intravenous fentanyl" within abstract. |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised appear to have been accounted for within the results ‐ although 41 crossed over and it does not specify from and to which group. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported within the Methods section are available within the Results. |
| Other bias | Low risk | Baseline characteristics of groups were similar ‐ "There were no differences between the groups at initial randomisation with regard to age, height, weight, parity, or racial origin (Table I)". |
| Methods | Women "prospectively randomised", no further information given | |
| Participants | 50 women recruited (epidural N = 28, meperidine N = 22) | |
| Interventions | Epidural method: preload not stated | |
| Outcomes | Maternal: pain scores, motor and sensory block, duration of labour, cervical dilation, use of oxytocin, mode of delivery, maternal satisfaction, temperature | |
| Notes | Canada Dates: Year trial carried out not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised |
| Allocation concealment (selection bias) | Unclear risk | Randomised |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | High risk | Outcome documented in Methods section not reported ‐ oxytocin use |
| Other bias | Unclear risk | Insufficient information |
| Methods | Participants randomly assigned to receive PCEA or PCIA. Computer‐generated random number system concealed in consecutively‐numbered sealed, opaque envelopes (further information was obtained directly from trial authors). | |
| Participants | 185 women recruited (epidural = 97, IV fentanyl = 88) | |
| Interventions | Epidural: 0.08% bupivacaine + 1.67 mcg/mL fentanyl ‐ loading dose of 10 ‐ 15 mL followed by 5 mL every 10 minutes as needed | |
| Outcomes | Maternal: pain scores, satisfaction with analgesia, need for further analgesia, duration of analgesia, caesarean section rate | |
| Notes | Canada. Multicentre trial. 18 (20%) women in the IV fentanyl group received an epidural also. Dates: Year trial carried out not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised |
| Allocation concealment (selection bias) | Low risk | Computer‐generated random‐number system concealed in consecutively‐numbered sealed, opaque envelopes (further information was obtained directly from trial authors). |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | High risk | Safety outcomes documented in Methods section not reported. |
| Other bias | Unclear risk | Insufficient information |
| Methods | "Randomised" method not specified | |
| Participants | 20 women recruited (epidural N = 10, fentanyl N = 10) | |
| Interventions | Epidural: preload unknown | |
| Outcomes | Maternal: VAS pain score, side effects, length of labour after analgesia, mode of delivery, heart rate, oxygen saturation | |
| Notes | Finland Dates: Not stated Funding: "supported by funds from Instrumentarium Research Foundation, Finland and funds from Turku University Hospital, Finland" Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised |
| Allocation concealment (selection bias) | Unclear risk | Randomised |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | 3 of 10 participants in fentanyl group received epidural because of unsatisfactory pain relief and 1 because fentanyl prolonged delivery. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the Methods section have been reported on in the Results. |
| Other bias | Low risk | |
| Methods | "Randomly assigned by random numbers, contained in sealed, consecutively opened envelopes." | |
| Participants | 112 women recruited (epidural N = 57, pethidine N = 55) | |
| Interventions | Epidural method: preload given. Bupivacaine 0.375% (1 mL per 10 kg) by intermittent top‐up. T10 ‐ L1 block. All women offered nitrous oxide/oxygen inhalation on demand, and pudendal block (20 mL mepivacaine) in 2nd stage | |
| Outcomes | Maternal: pain, hypotension, nausea and vomiting, urinary retention, sleepiness, motor blockade, length of 1st stage of labour, duration of 2nd stage of labour, position of fetal head at delivery, mode of delivery, maternal memory of labour | |
| Notes | Denmark Dates: Year trial carried out not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Sealed, consecutively opened envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No participant loss |
| Selective reporting (reporting bias) | High risk | Additional outcomes reported in tables not specified in the Methods section. |
| Other bias | High risk | 9 participants in the epidural group and 29 in the pethidine group used nitrous oxide. The participants' pain scores in stage 2 were found equal in the 2 groups, 86% in the pethidine versus 85% in the epidural group had a pudendal block. |
| Methods | RCT Parallel design Single centre Riyadh, Saudi Arabia | |
| Participants | 30 pregnant women were randomised to Group EP (N = 15) ‐ epidural or Group R ‐ (N = 15). Eligibility: ASA I or II with no obstetric complications or contraindication to remifentanil or epidural analgesia | |
| Interventions | Group EP (N = 15) ‐ epidural analgesia ‐ epidural infusion of bupivacaine 1% plus 2 µg/mL of fentanyl Group R (N = 15) ‐ PCA remifentanil ‐ with a bolus of 0.4 µg kg‐1 over 20 s and a lockout period of 1 min as an analgesia for labour | |
| Outcomes |
| |
| Notes | Abstract only, so data limited Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not reported |
| Methods | RCT Parallel design Single centre University of Texas Southwestern Medical Center, Dallas | |
| Participants | 1330 women with uncomplicated term pregnancies were randomised to be offered epidural (N = 664) or IV analgesia (N = 666) ‐ 65% of each randomisation group accepted the allocated treatment ‐ epidural group (N = 432), IV group (N = 437). Eligibility: women with normal pregnancies presenting in spontaneous labour | |
| Interventions | Epidural analgesia ‐ epidural bupivacaine‐fentanyl ‐ at participant's 1st request for pain relief, a 3 mL test dose of 0.25% bupivacaine was given, followed by further 3‐mL increments to achieve a bilateral T‐10‐ sensory level. This was followed by a continuous epidural infusion of 0.125% bupivacaine with 2 µg/mL fentanyl at 8 ‐ 10 mL/hr. The infusion was titrated to achieve a maximum T‐8 sensory level. Additional boluses of fentanyl or bupivacaine or both were injected to overcome inadequate analgesia. IV analgesia ‐ IV meperidine ‐ 50 mg with 25 mg of promethazine hydrochloride IV at 1st request for pain relief. Additional 50 mg doses of meperidine were given on request, to a maximum of 200 mg in 4 hrs. When pain relief was inadequate, epidural analgesia was administered on patient request. | |
| Outcomes |
| |
| Notes | Single centre, Dallas, USA 2680 offered participation, 1330 (51%) accepted. 1279 who did not consent to participate were demographically similar to those accepting of 1330 ‐ 664 randomised to epidural ‐ but 232 (35%) never received allocated treatment ‐ half had refused offer of epidural and the remainder progressed to delivery before epidural analgesia could be initiated. 666 women randomised to meperidine IV, but 229 (34%) were not treated ‐ 103 of this group requested epidural after finding meperidine to be inadequate. Dates: Trial carried out November 1 1993 ‐ April 30 1994 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomisation sequence was computer‐derived in blocks of 20." |
| Allocation concealment (selection bias) | Low risk | Women were randomly assigned using numbered, sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | There was a substantial loss of participants from both groups due to them not following the allocated protocol (35% loss in epidural group, 34% loss in the IV group). All but 1 set of results are therefore based on the available data ‐ operative delivery for dystocia was only outcome analysed on an intention‐to‐treat basis "when comparing the two groups on an intention‐to‐treat basis". However, they do say that a "multivariate analysis of the entire cohort was performed to control for confounding effects of other variables, particularly parity." The results of this cohort analysis are consistent with the labour outcome difference observed between the 2 allocation‐compliant treatment groups for the outcomes of caesarean section and operative delivery for dystocia. |
| Selective reporting (reporting bias) | High risk | Hypotension ‐ described as an outcome in Methods ‐ but not within the Results. All other prespecified outcomes reported within the Methods section are available within the Results. |
| Other bias | Low risk | None evident |
| Methods | Randomised controlled trial (prospective parallel single‐blind) with individual randomisation Set in hospital in Egypt. | |
| Participants | 60 women randomised to receive combined spinal epidural or epidural with bupivacaine or lidocaine (10 women received each method), or IV pethidine (20 women). Full‐term nulliparous women in active labour with cervical dilatation of 5 cm and cephalic‐presenting fetus. Exclusion criteria: women who had diabetes, neurological disease, pre‐eclampsia, or those who received parenteral analgesics or those with contraindication to epidural or spinal analgesia, or sensitivity to local anaesthetics or opioids were excluded | |
| Interventions | Group 1 (CSE1) – CSE, bupivacaine, (n = 10): CSE analgesia, 25 µg fentanyl were injected intrathecally and a bolus dose of 10 mL of 0.5% lidocaine injected epidurally. Top‐ups of 5 ‐ 10 mL of 0.5 ‐ 0.8% of lidocaine injected epidurally upon request Group 2 (CSE2) – CSE, lidocaine (n = 10): received CSE analgesia, 25 µg fentanyl were injected intrathecally and a bolus dose of 10 mL of 0.0625% bupivacaine injected epidurally. Top‐ups of 5 ‐ 10 mL of 0.0625 ‐ 0.8% of lidocaine injected epidurally upon request Group 3 (E1) – Epidural, bupivacaine (n = 10): received epidural analgesia, 50 µg fentanyl were injected epidurally together with a bolus dose of 10 mL of 0.5% lidocaine. Top‐ups of 5 ‐ 10 mL of 0.5 ‐ 0.8% of lidocaine injected epidurally upon request Group 4 (E2) – Epidural, lidocaine (n = 10): received epidural analgesia, 50 µg fentanyl were injected epidurally together with a bolus dose of 10 mL of 0.125 – 0.25% bupivacaine injected epidurally upon request Group 5 (IV) (n = 20): 50 mg of IV pethidine administered as a loading dose, followed by 0.5 mg/kg, with a maximum limit of 130 mg 4 epidural groups were combined in data and analysis, and compared with IV pethidine. | |
| Outcomes | SD for VAS pain score, number of top‐ups, degree of motor block | |
| Notes | Dates of trial: January 2008 – January 2009 Funding: self‐funded Conflicts of interest: none Maternal hypotension EA: 9/40; IV 0/20 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible |
| Blinding of outcome assessment (detection bias) | High risk | There is no information provided; probably labour outcomes would be collected by caregiver. |
| Incomplete outcome data (attrition bias) | Low risk | It appears that the data for all the women who were randomised are available. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes prespecified in protocol are reported except for modified Bromage scale and time from analgesia to birth. |
| Other bias | Low risk | Demographic variables were comparable between the groups, haemodynamic changes did not differ among the groups. |
| Methods | RCT Parallel design Single centre Northwestern University Medical School, Chicago, USA | |
| Participants | 100 healthy nulliparous women at term in spontaneous labour or with spontaneous rupture of membranes randomised to intrathecal opioid CSE (N = 49) or systemic opioid (N = 51) Eligibility: nulliparous, healthy at term in spontaneous labour or with spontaneous rupture of membranes requesting labour analgesia < 4 cm cervical dilatation | |
| Interventions | Intrathecal opioid ‐ as part of a combined spinal/epidural technique (fentanyl 25 µg followed by epidural test dose of 3 mL ‐ 1.5% lidocaine with epinephrine 15 µg) N = 49. Systemic opioid ‐ (hydromorphone 1 mg IV and 1 mg IM) N = 51 | |
| Outcomes |
| |
| Notes | Abstract only ‐ so limited data. Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | "A perinatologist blinded to patient group examined the heart rate and contraction pattern abnormalities." |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not reported |
| Methods | Randomised sequence was computer‐derived in blocks of 20, with numbered, opaque sealed envelopes. | |
| Participants | 715 women recruited (epidural N = 358, IV meperidine analgesia N = 357) | |
| Interventions | Epidural: preload given | |
| Outcomes | Maternal: visual analogue pain scores, length of labour, oxytocin augmentation, fever > 38º centigrade, mode of delivery | |
| Notes | Texas, USA Dates: Trial carried out 1995 ‐ 1996 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation sequence was computer‐derived in blocks of 20. |
| Allocation concealment (selection bias) | Low risk | Numbered and sealed opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | High risk | Of the 357 women who were allocated to receive epidural analgesia, 259 completed the study as allocated. Of the 98 women (28%) who did not comply with the patient controlled |
| Selective reporting (reporting bias) | High risk | Some outcomes reported in tables not specified in the Methods section |
| Other bias | Low risk | |
| Methods | Computer‐generated randomisation numbers in sealed envelopes | |
| Participants | 459 women recruited (epidural N = 226, meperidine N = 233) | |
| Interventions | Epidural: preload given 500 mL sodium lactate. Test dose of 3 mL of 1% lidocaine with epinephrine, then 0.25% bupivacaine in 3 mL increments till T‐10 sensory level analgesia. Then infusion of 0.0625% bupivacaine with 2 µg/mL fentanyl at 6 mL/h with 5 mL boluses every 15 min prn using PCA pump | |
| Outcomes | Maternal: fever, hypotension, oxytocin augmentation, instrumental delivery | |
| Notes | Texas, USA Dates: Trial carried out 1998 ‐ 2000 Funding: "Support was provided solely from institutional and/or departmental sources." Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐derived in blocks of 20 |
| Allocation concealment (selection bias) | Unclear risk | Numbered sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 14 who received IV meperidine as randomised crossed over to epidural analgesia because of inadequate pain relief, and 24 women refused their allocated analgesia and received other analgesia. All included in the intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | Outcomes not prespecified in Methods section, other than caesarean section |
| Other bias | Low risk | |
| Methods | RCT Parallel design Single centre Russia | |
| Participants | 90 healthy pregnant women ‐ randomised into 3 groups, 30 in each group Eligibility: healthy pregnant women Exclusion: women with a history of chronic back pain or neurological illnesses or symptoms and women who had already given birth before or with pregnancy and birth complications | |
| Interventions | Group 1 ‐ epidural analgesia (N = 30) ‐ 1% lidocaine Group 2 ‐ epidural analgesia (N = 30) ‐ 0.2% ropivacaine Group 3 ‐ control ‐ (N = 30) ‐ no epidural | |
| Outcomes | Caesarean section Transient neurological symptoms (2 days after labour) ‐ included symmetric pain and/or dysthaesia in the buttocks, lower lumbar region, and/or legs | |
| Notes | Faculty of Anaesthesiology, Russian University of Friendship Between Nations in Moscow. Paper in Russian ‐ sections translated Dates: Not stated in translation Funding: Not stated in translation Declarations of Interest: Not stated in translation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | "Two days after the EA, a blind observer asked patients questions using the BG Cramer table. The observer was not informed about the treatment received by the patients." |
| Incomplete outcome data (attrition bias) | Unclear risk | Total for control group for caesarean section rate is given as 50 in totals ? only 30 in original group (from translation ? so may be a typo). |
| Selective reporting (reporting bias) | Low risk | All expected outcomes are reported. |
| Other bias | Low risk | Not evident |
| Methods | Single‐centre, individually‐randomised non‐blinded controlled non‐inferiority design trial | |
| Participants | 40 women randomised (39 analysed) (remifentanil PCIA, N = 20; patient controlled epidural, N = 20) Eligibility: healthy, ASA physical status class I or II, age 18 ‐ 40 years, body weight < 110 kg, gestational age > 36 completed weeks, with singleton pregnancy and vertex presentation Excluded: contraindication to epidural analgesia, opioid administration in the previous 2 hours, previous uterine surgery, pre‐eclampsia, inability to understand the consent form, nasal obstruction for any reason and medical indication for epidural analgesia (e.g. cardiac disease, suspected difficult airway), or non‐reassuring fetal heart rate tracing | |
| Interventions | Group 1: Patient‐controlled remifentanil (N = 20 with 19 analysed) The bolus dose was titrated to effect from 20 mcg up to a maximum of 60 mcg as required; the lockout interval was initially set at 2 min, without a background infusion. The PCIA bolus/lockout interval was titrated to an end point of either participant comfort, or a maximal bolus dose of 60 mcg/minimal lockout interval of 1 min by the recruiting anaesthetist at any time during labour. The PCIA pump tubing was “piggybacked” into the distal‐most port of the mainline IV fluid tubing. The mainline tubing contained an antireflux valve designed to prevent remifentanil inadvertently backing up in the IV line during administration. The recruiting anaesthetist (a resident performing a mandatory research project) remained by the woman’s bedside until the end of treatment with remifentanil. Group 2: Patient‐controlled epidural (N = 20) For women randomised to receive epidural analgesia, a 17‐gauge Tuohy needle was inserted by the midline approach using loss of resistance to air at intervertebral space L3 ‐ 4 or L2 ‐ 3. An incremental initial loading dose of 15 mL of 0.1% bupivacaine with 50 mcg fentanyl was administered followed by patient‐controlled epidural analgesia infusion of 0.1% bupivacaine with 2 mcg/mL fentanyl: basal infusion of 5 mL/hr, patient‐controlled bolus 10 mL, and lockout interval 20 minutes. Additional epidural bolus doses (either 0.1% bupivacaine 10 mL during the 1st stage of labour or 1% lidocaine 8 mL during the 2nd stage of labour) were administered by the anaesthetist to treat breakthrough pain. If epidural analgesia failed, the epidural catheter was reinserted. After epidural analgesia administration, the recruiting anaesthetist remained by the woman’s bedside for the 1st hour and then remained in the labour ward, dedicated to her care, until delivery. | |
| Outcomes | Need for further analgesia Mode of birth Oxytocin augmentation Respiratory depression Side effects Apgar scores Neonatal resuscitation Pain change scores Duration of labour Satisfaction scores Cord blood gases | |
| Notes | Conducted in tertiary hospital in Jerusalem, Israel Dates of trial: February 2010 – August 2010 Funding: this study was supported by a research grant for Anesthesiologists from the Hadassah Hebrew University Medical Center, Jerusalem, Israel. Oridion® provided the capnography equipment, developed the dedicated software, and provided the mathematician who performed data extraction. Neither the funding body nor Oridion® had a role in study design, data interpretation, writing of the manuscript, or manuscript submission for publication. Conflicts of Interest: 2 authors received money from Oridion® for travel to conference to present paper. High level of women receiving oxytocin, so 1st stage of labour data not reported in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Shuffling cards. Group of 8 – 4 each of intervention and control |
| Allocation concealment (selection bias) | Low risk | Randomisation and group allocation were determined: cards were divided into groups of 8 cards. Each group contained 4 allocation cards for remifentanil and 4 allocation cards for epidural analgesia (ratio 1:1), and 8 opaque envelopes numbered in groups from 1 – 8, 9 – 16, etc. were assigned to each group of cards. The cards were placed face down, manually shuffled, randomly selected, and then inserted into the numbered, opaque envelopes by a person not involved in the study. These envelopes were then sealed. Treatment assignment was revealed by breaking the seal of an envelope in consecutive order from number. |
| Blinding of participants and personnel (performance bias) | High risk | Participants would be aware of allocation and were informed that they could cross over if analgesia not effective. Caregiver would be aware of allocation. |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded. Staff providing care would record labour outcomes. Outcome for infant respiratory rate observed by assessor blind to study hypothesis. |
| Incomplete outcome data (attrition bias) | Low risk | 58 declined to participate. 40 randomised. 1 in RPCA group was excluded by obstetrician request. 3 in Remifentanil group crossed over to epidural, 1 epidural crossed to remifentanil due to failure of allocated analgesia. These women are excluded for some analyses. Intention‐to‐treat analysis: yes |
| Selective reporting (reporting bias) | Low risk | Appear to all be reported. No protocol available but all expected outcomes reported. Power calculation for non‐inferiority design |
| Other bias | Low risk | Similar baseline characteristics and other bias not apparent |
| Methods | RCT Parallel design Single centre Chicago, Illinois, USA | |
| Participants | 180 healthy nulliparous women were randomised, to either systemic opioids (N = 70) or intrathecal opioids as part of a CSE technique (N = 80). Eligibility: term in spontaneous labour or with spontaneous rupture of membranes and requested labour analgesia prior to 4 cm of cervical dilatation. All received oxytocin to augment labour. | |
| Interventions | Group SYS ‐ systemic opioids ‐ hydromorphone 1 mg IV/1 mg IM (N = 70) Group IT ‐ intrathecal opioids as part of a combined spinal epidural technique ‐ intrathecal fentanyl 25 µg plus epidural test dose of lidocaine 45 mg with epinephrine 15 µg (N = 80) | |
| Outcomes | Oxytocin infusion rates ‐ recorded for 2‐hr period (1 hr prior to and 1 hr after the initiation of labour analgesia) | |
| Notes | Dept of Anesthesiology, Northwestern University Medical School, Chicago, Illinois, USA Abstracts only, so data limited. Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not reported |
| Methods | "Randomly allotted", using sealed envelopes drawn by a midwife | |
| Participants | 28 women recruited (epidural N = 14, meperidine N = 14) | |
| Interventions | Epidural method: preload given. Bupivacaine 0.25% with adrenaline 6 ‐ 8 mL by intermittent top‐up. Level of block not known | |
| Outcomes | Maternal: duration of 1st and 2nd stages of labour, oxytocin augmentation, acid/base values, mode of delivery | |
| Notes | Sweden Dates: Year trial carried out not stated Funding: "supported by a grant from the Swedish Medical Research Council" Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allotted to 2 groups |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | 4 participants were removed from the study: 2 from the control group and 2 from the epidural group, because of moderate to pronounced dysmaturity of the baby or clinical appearance of the baby indicated a gestational age of 36 weeks. |
| Selective reporting (reporting bias) | High risk | Outcomes not all prespecified in Methods section |
| Other bias | High risk | The tendency to increased duration of the 2nd stage after epidural block made the prophylactic use of vacuum extraction necessary to exclude the deleterious effect on the fetus of a 2nd stage exceeding 1 hr, but author continued to report on duration of the 2nd stage but not the instrumental delivery. |
| Methods | Randomisation to treatment by sealed envelopes. Randomisation sequence derived from a computer‐generated random number table | |
| Participants | 93 women recruited (epidural N = 48, control N = 45) | |
| Interventions | Epidural method. Preload not mentioned. Bupivacaine 0.25% bolus dose followed by 0.25% bupivacaine infusion. Block to T10 ‐ T12 | |
| Outcomes | Maternal: length of 1st and 2nd stages of labour, oxytocin augmentation, method of delivery, pain scores | |
| Notes | USA Dates: Trial took place 1990 ‐ 1992 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number tables |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | Described as unblinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Described as unblinded |
| Incomplete outcome data (attrition bias) | Low risk | No loss of the participants and crossed‐over participants analysed in their original groups |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported within the Methods section are available within the Results. |
| Other bias | High risk | Study was terminated early because after 93 participants entered in the trial statistically significant increase in the rate of caesarean sections seen in the epidural group. Initially 100 participants in each arm intended |
| Methods | Randomised controlled trial with individual randomisation | |
| Participants | 39 women randomised (epidural analgesia n = 20; IV remifentanil n = 19) Eligibility: ASA I or II with normal singleton pregnancies, regular uterine contractions, cervical dilatation > 2 cm, anticipated vaginal delivery, fetus without suspected abnormality, normal fetal cardiotocographic pattern, no complications during pregnancy and gestation age 37 ‐ 40 weeks Excluded: women were excluded if they requested EDA, had received pethidine < 8 hrs before the study period or if there were contraindications to remifentanil. | |
| Interventions | Remifentanil group: n = 19 Women received remifentanil hydrochloride diluted in "physiological saline to a concentration of 50 µg/mL, given as stepwise bolus doses with no background infusions. The starting bolus dose was 0.15 µg/kg, with increasing dose steps of 0.15 µg/kg and no maximum limit. The dose was allowed to be increased or decreased every 15th minute according to women’s request for dose adjustment. VAS pain score, and side effects. The lock‐out period was 2 mins." Remifentanil was administered using a PCA pump with a bolus infusion speed of 2 mL/min (100 µg/min). Epidural analgesia group: n = 20 Women had an epidural catheter inserted in the midline at L2 ‐ L3/L3 ‐ 4 by the investigator, received a continuous epidural infusion of ropivacaine 1 mg/mL and fentanyl 2 µg/ml (‘walking epidural’). An initial bolus dose of 10 mL, followed by a 5 mL top‐up after 5 min (total 15 mL) was given before the start of infusion (10 mL/hr). Midwife could adjust the infusion dose (5 ‐ 15 mL/hr) and give rescue doses (5 mL) if needed. EA group was managed in accordance with the local protocol. | |
| Outcomes | Satisfaction scores Oxytocin augmentation Side effects Duration of labour | |
| Notes | Country and setting: Norway Dates of trial: Not reported Funding: Sorlandet Hospital HF, Sorlandets Kompetansefond and Helse Sor‐Ost, Norway Conflicts of interest: none declared Duration of 1st stage not reported in review due to large number of women having oxytocin Sense of control in labour | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Randomisation codes were kept in a sealed envelopes until recruitment. |
| Blinding of participants and personnel (performance bias) | High risk | The study was not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | "after the study, two additional obstetricians, blinded to the analgesia method and neonatal outcome, independently evaluated fetal heart rate recordings." It was unclear for other outcomes; anaesthesiologist collected the pain scores. |
| Incomplete outcome data (attrition bias) | High risk | No loss to follow‐up 2 women in the remifentanil group discontinued intervention and received epidural. They were excluded from the analysis, although fig 1 reports that none were excluded. |
| Selective reporting (reporting bias) | Low risk | Protocol not seen but outcomes prespecified in Methods and appear to all be reported. |
| Other bias | Unclear risk | Underpowered because of finishing trial early due to technical faults. Baseline characteristics appear similar. |
| Methods | RCT Parallel design Single centre University of Oulo, Finland | |
| Participants | 52 women randomly allocated to remifentanil (N = 27) and to epidural analgesia (N = 25) Eligibility: healthy term parturients with uncomplicated singleton pregnancies, 1st stage of labour with normal cephalic presentation and no prior administration of opioid analgesia for at least 4 hrs or regional analgesia Exclusion: not reported | |
| Interventions | IV patient‐controlled analgesia (IV PCA) with remifentanil ‐ PCA dose given over 1 min with a lockout time of 1 min. Dose was increased starting from the bolus of 0.1 µg/kg and following a dose escalation scheme up until the individual‐effective dose was reached. Epidural analgesia with 20 mL Levobupivacaine 0.625 mg/mL and fentanyl 2 µg/mL in saline | |
| Outcomes |
| |
| Notes | 7 participants not included in the analysis: remifentanil group (N = 3) ‐ discontinued due to entering 2nd stage of labour; epidural group (N = 4) ‐ 3 discontinued due to entering 2nd stage of labour, 1 did not receive allocated intervention due to dural tap. Department of Anaesthesia & Intensive Care, University of Oulo, Finland Dates: Dates not stated. Accepted for publication 2007 Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list that was stratified according to parity |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes numbered according to computer‐generated list |
| Blinding of participants and personnel (performance bias) | Low risk | "Both the parturient and all the personnel present during the study were blinded as to which medication was used during the study." |
| Blinding of outcome assessment (detection bias) | Unclear risk | Fetal heart rate tracings were analysed by an obstetrician blinded to analgesia group and outcome of the newborn. |
| Incomplete outcome data (attrition bias) | Low risk | CONSORT flowchart outlining numbers allocated, followed‐up and analysed. Reasons for not including in the analysis clearly documented: remifentanil group (N = 3) ‐ discontinued due to entering 2nd stage of labour; epidural group (N = 4)‐ 3 discontinued due to entering 2nd stage of labour, 1 did not receive allocated intervention due to dural tap. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported within the Methods section are available within the Results. |
| Other bias | Low risk | Baseline characteristics similar, apart from more nausea before the study in the remifentanil group (N = 9) versus none in epidural group. |
| Methods | RCT Parallel design Single centre Chula‐longkorn University, Thailand | |
| Participants | 62 pre‐eclamptic women 16 ‐ 29 years (21 ± 4.23), primigravida, in labour at term randomised to study group (N = 31) continuous lumbar epidural analgesia, or control group (N = 31) pethidine or pentazocine intramuscularly | |
| Interventions | Continuous lumbar epidural analgesia ‐ standard precautions for epidural analgesia were taken throughout, bupivacaine (marcain) was intermittently given to provide painless labour (N = 31). Pethidine or pentazocine given intramuscularly (N = 31) | |
| Outcomes | Blood pressure | |
| Notes | Abstract only ‐ data limited. Dates: Not stated Funding: Not stated Declarations of Interest: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not reported |
| Methods | Reported to be RCT with individual randomisation | |
| Participants | 308 women randomised but data only for 285 (CSEA n = 143; control n = 142) Eligible: primiparous women who (1) were 22 – 30 years old; (2) were 155 – 165 cm tall; (3) were assigned a score of I or II on the ASA scale; and (4) gave birth by vaginal delivery to a live, single, mature fetus (38 ‐ 40 wks) in the vertex position with (5) a neonatal weight of 2900 – 3500 g Excluded: (1) history of chronic cough; (2) chronic constipation or pelvic organ resection; (3) family history of urinary incontinence; (4) pelvic organ prolapse; (5) any systemic disease before delivery; or (6) a history of surgery, trauma, tumour or deformity of lumbar vertebrae | |
| Interventions | Combined spinal‐epidural analgesia group (n = 143) Women in the CSEA group received CSEA during labour. An intravenous line was established when the cervical opening measured 1 – 2 cm. Then sufentanil (5 – 7 μg) was injected intrathecally. When the visual analogue pain score was 3 or higher, a mixture of ropivocaine (0.143%) and sufentanil (0.3 μg/mL) was continuously infused into the epidural space using an analgesia pump until the cervix was fully dilated. Load capacity was 5 mL. The analgesic plane was controlled under T10. Control group (n = 142) Women in the control group were not provided any analgesia during labour. | |
| Outcomes | Need for other analgesia Mode of birth Oxytocin administration Duration of labour Perineal injury | |
| Notes | Setting: Maternal and Child Health Hospital of Nanning, China Dates of trial: June 2013 and June 2014 Funding: this work was supported by the Scientific and Technological Key Project of Nanning City (no. 20133189). Conflicts of interest: the authors have declared that no competing interests exist. Duration of 1st and 2nd stage reported but not clear if it is median and IQR or range | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not described, although consecutive sampling is mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Staff and women knew allocation due to nature of intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Labour outcomes probably reported by caregiver in labour. Outcome assessor testing pelvic floor strength 6 ‐ 8 weeks post‐delivery was blinded but this outcome is not relevant to this review. |
| Incomplete outcome data (attrition bias) | Unclear risk | Following randomisation 2 women in each group were lost to follow up. “Another 12 women were excluded because they reported feeling vaginal fullness at an inflation volume <15 ml or >30 ml…. Three were delivered by caesarean and 4 fetal weight were outside the range of 2900–3500 g. These 7 women were also excluded.” 12/155 women in the CSEA group were excluded in total. 11/153 women in the control group were excluded. 5 women in the control group were given epidural on request but were analysed in the control group (ITT). Reasons given for exclusions, may have introduced attrition bias. |
| Selective reporting (reporting bias) | High risk | Duration of labour was added post hoc as the protocol was registered after the trial was completed. |
| Other bias | High risk | No baseline characteristic imbalances apparent. Methods not reported well (in the CONSORT checklist, authors have reported that they have provided information 8 – 10 on pages 4 and 5 in the report, but the information is missing). |
ASA: American Society of Anesthesiologist
AUC: area under the curve
BE: base excess
BMI: body mass index
CMS: continuous midwifery support
CS: Caesarean section
CSE: combined spinal‐epidural
CTG: cardiotocography
EPI: epidural
FGR: fetal growth restriction
FHR: fetal heart rate
hr: hour
IM: intramuscular
IV: intravenous
min: minutes
NACS: Neurological Adaptive Capacity Score
NICU: neonatal intensive care unit
NO: Nitric oxide
PCA: participant‐controlled analgesia
PCEA: participant‐controlled epidural analgesia
PCIA: participant‐controlled intravenous analgesia
PIH: pregnancy‐induced hypertension
PPH: postpartum haemorrhage
PRL: prolactin
RCT: randomised controlled trial
ROM: rupture of membrane
s: seconds
SD: standard deviation
TENS: transcutaneous electrical nerve stimulation
VAS: visual analogue scores
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This study was designed to assess the effect on beta‐endorphin levels, of momentarily withholding local anaesthetic after insertion of the catheter into the epidural space. | |
| This is not an RCT. Women were divided into 2 groups, 50 each "as per convenience". | |
| Excluded because the method of randomisation was not adequate (alternate allocation). Epidural bupivacaine (N = 10) compared with intramuscular pethidine (N = 10). Outcomes include corticosteroid levels and mode of delivery. | |
| Control group were not randomised, 2 epidural groups were randomised. Comparisons of interest therefore not randomised and study does not satisfy eligibility criteria. | |
| This is not an RCT. This was not a trial; it looked at 200 women, 100 chose EA and 100 other analgesia. It was looking at factors associated with choosing EA. | |
| Excluded because all women received epidural bupivacaine until pain free (N = 48), then randomised to IV fentanyl or epidural fentanyl (abstract of study published in full in 2003). | |
| Excluded because both groups received lumbar epidural analgesia with 20 ‐ 30 mL bupivacaine until pain‐free then randomised to IV fentanyl infusion and epidural fentanyl infusion. | |
| Excluded because both groups received epidural. This study was looking at paracetamol as an adjuvant therapy. | |
| Excluded because both experiment and control groups had regional procedure although saline was control. This study compared epidural bupivacaine (N = 14) with epidural saline (N = 14) for 60 minutes after insertion of the epidural catheter. The outcome of interest was fetal heart rate changes. | |
| Excluded because interventions do not meet review criteria. Denominators not clear, brief abstract. No relevant outcome data | |
| Excluded because the method of randomisation was not adequate (alternate allocation). Epidural bupivacaine (N = 14) compared with intramuscular pethidine (N = 14). Outcomes include duration of labour, growth hormone, insulin, fetal/infant outcomes and mode of delivery. | |
| Excluded because the method of randomisation was not adequate (alternate allocation). Epidural bupivacaine (N = 8) compared with intramuscular pethidine (N = 10). Outcomes include duration of labour, prolactin, fetal/infant outcomes and mode of delivery. | |
| Excluded because all participants were given epidural test dose followed by either intramuscular fentanyl or epidural fentanyl. Outcomes included duration of analgesia, hypotension, itching, bladder dysfunction and neonatal Apgar scores in correlation with plasma fentanyl concentration. | |
| Excluded because trial compared epidural with paracervical epidural. | |
| Quasi‐randomised | |
| Excluded because study compared epidural morphine (N = 13) with epidural saline (N = 12), with both groups receiving epidural bupivacaine at some stage in labour. | |
| Not RCT. All participants were offered epidural analgesia in labour and those who accepted formed the epidural group (N = 55), those who declined epidural analgesia were controls (N = 68). Outcomes included duration of labour, oxytocin augmentation and mode of delivery. | |
| All participants had epidural bupivacaine in labour prior to randomisation to continuous infusion of epidural bupivacaine and fentanyl (N = 7) or IV fentanyl (N = 6). Outcomes included fentanyl concentration in maternal and cord blood. | |
| Excluded because intervention is not relevant. | |
| Both groups received epidural analgesia. | |
| The study randomised participants to epidural analgesia or nalbuphine intravenously with the intention of providing all women with epidural analgesia later in labour. The outcome of interest was fetal heart rate changes in the 1st hour after randomisation. | |
| Excluded because this was not an RCT. | |
| Quasi‐randomised. Odd and even numbers used for allocation This study compared epidural (N = 197) with IV meperidine (N = 198). | |
| Quasi‐randomised (information from authors) N = 104 | |
| Excluded because the method of randomisation was not adequate (allocation by case record number). Epidural bupivacaine (N = 125) compared with intramuscular pethidine (N = 120). Outcomes include duration of labour, maternal hypotension, fetal/infant outcomes and mode of delivery. | |
| Excluded because both groups received epidural analgesia. | |
| Excluded because more than 28% of women excluded from analysis. Out of 386 randomised only 132 completed interviews in their allocated groups. Outcomes include pain scores, satisfaction with analgesia, and concerns of analgesic effects on the baby. | |
| Excluded because more than 30% of women excluded from analysis. Out of approximately 300 women initially randomised at antenatal visit into the 2 groups, only 93 completed the interviews having used only the analgesic allocated to them. The large proportion excluded compromises the reliability of the results. Epidural bupivacaine (N = 45) was compared with intramuscular pethidine (N = 48). Outcomes include duration of labour, mode of delivery and maternal pain/discomfort, nausea, sleepiness, backache, satisfaction and worry over baby. | |
| Intention‐to‐treat analysis not used. 153 participants randomly allocated to low extra‐dural analgesia with 0.125% bupivacaine with 50 µg fentanyl followed by 0.1% bupivacaine with 2 µg/mL fentanyl top‐ups (N = 89), and IM pethidine 100 mg (N = 64). | |
| Excluded because the method of randomisation was not adequate (alternate allocation). Epidural bupivacaine (N = 5) compared with intramuscular pethidine (N = 5). Outcomes include duration of labour, plasma leukocyte counts, fetal/infant outcomes. | |
| Not a randomised controlled trial | |
| Excluded because women chose intervention, therefore this was not a randomised trial. | |
| Quasi‐randomised (running order). 80 women. Epidural (N = 37), paracervical N = 16; control group (N = 27) (further data from authors). Outcomes include duration of 1st and 2nd stages of labour, oxytocin augmentation, Apgar scores, neonatal jaundice, neurological outcomes at 6/18 months. | |
| Not a randomised controlled trial. | |
| Excluded because this was not an RCT. | |
| Excluded because both groups received epidural analgesia: women randomly assigned to receive intrathecal fentanyl or systemic hydromorphone at the 1st request of analgesia ‐ but epidural analgesia was initiated in the intrathecal group at the 2nd request for analgesia and in the systemic group at a cervical dilatation of 4.0 cm or greater or at the 3rd request for analgesia. | |
| Excluded because both groups received epidural analgesia: participants were randomised to neuraxial (early) or systemic opioid (late) analgesia at the 1st analgesia request. Patient‐controlled epidural analgesia was initiated in the early group at the 2nd analgesia request and in the late group at cervical dilation of 4 cm or greater or at the 3rd analgesia request. | |
| Excluded because compared epidural morphine to IV morphine postoperative analgesia in women who had elective Caesarean delivery. All participants had received epidural lidocaine preoperatively, epidural morphine (N = 8) IV morphine (N = 8). Outcomes were plasma and urinary morphine concentration. |
h: hours
IM: intramuscular
IV: intravenous
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | It was not clear that this was a trial; women were "randomized to 3 groups ‐ one was "refused pain relief". |
| Participants | Women in the 1st stage of labour |
| Interventions | Group 1. Epidural Group 2. paravertebral block Group 3. "refused analgesia" |
| Outcomes | Duration of labour |
| Notes | Authors contacted ‐ awaiting response Unclear if this is an RCT. |
| Methods | Reports to be RCT |
| Participants | Women in labour at term |
| Interventions | Group 1. Epidural Group 2. No epidural |
| Outcomes | Duration of labour Mode of birth |
| Notes | Author contacted for more information on methods It was not clear that this was an RCT. |
| Methods | Reported to be trial |
| Participants | Women at term |
| Interventions | Group 1. Epidural Group 2. Entonox Group 3. no analgesia |
| Outcomes | No results ‐ trial registration |
| Notes |
| Methods | Reported to be RCT. Abstract only |
| Participants | Women in labour |
| Interventions | Epidural versus opiate analgesic (not specified) |
| Outcomes | Intra‐abdominal pressure, pain intensity |
| Notes | Unable to find author contact details |
| Methods | Methods not described, possibly RCT |
| Participants | Women in labour |
| Interventions | Epidural versus IV nalbuphine, or pethidine |
| Outcomes | Pain and Apgar score |
| Notes | Unable to find email address to contact authors |
| Methods | Randomised, parallel‐assignment, open‐label controlled trial |
| Participants | Target number: 60 randomised Inclusion criteria: not clear Exclusion criteria: all parturients with cardiac disease, neurological disease, endocrine disease, diabetes, hypertension or any parturients being treated with medications that might effect the cardiovascular autonomic system |
| Interventions | Epidural versus IV Meperidine |
| Outcomes | Not stated |
| Notes | Predicted start and finish: March ‐ December 2006 Contacted study hospital for further information 15 June 2017 ‐ awaiting response |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score in labour Show forest plot | 5 | 1133 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐4.56, ‐0.73] |
| Analysis 1.1  Comparison 1 Epidural versus opioids, Outcome 1 Pain score in labour. | ||||
| 2 Pain intensity severe or intolerable Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.2  Comparison 1 Epidural versus opioids, Outcome 2 Pain intensity severe or intolerable. | ||||
| 3 Woman's perception of pain relief in labour Show forest plot | 3 | 1166 | Mean Difference (IV, Random, 95% CI) | ‐3.36 [‐5.41, ‐1.31] |
| Analysis 1.3  Comparison 1 Epidural versus opioids, Outcome 3 Woman's perception of pain relief in labour. | ||||
| 4 Woman's perception of pain relief during first stage of labour Show forest plot | 3 | 194 | Mean Difference (IV, Random, 95% CI) | ‐12.05 [‐19.35, ‐4.75] |
| Analysis 1.4  Comparison 1 Epidural versus opioids, Outcome 4 Woman's perception of pain relief during first stage of labour. | ||||
| 5 Woman's perception of pain relief during the second stage of labour Show forest plot | 2 | 164 | Mean Difference (IV, Fixed, 95% CI) | ‐20.75 [‐22.50, ‐19.01] |
| Analysis 1.5  Comparison 1 Epidural versus opioids, Outcome 5 Woman's perception of pain relief during the second stage of labour. | ||||
| 6 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 7 | 1911 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [1.03, 2.08] |
| Analysis 1.6  Comparison 1 Epidural versus opioids, Outcome 6 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good. | ||||
| 7 Satisfaction with pain relief in labour ‐ continuous data Show forest plot | 7 | 3171 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.10, 0.91] |
| Analysis 1.7  Comparison 1 Epidural versus opioids, Outcome 7 Satisfaction with pain relief in labour ‐ continuous data. | ||||
| 8 Time of administration of pain relief to time pain relief was satisfactory (minutes) Show forest plot | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐6.70 [‐8.02, ‐5.38] |
| Analysis 1.8 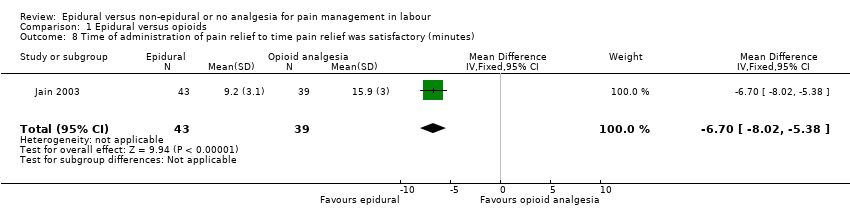 Comparison 1 Epidural versus opioids, Outcome 8 Time of administration of pain relief to time pain relief was satisfactory (minutes). | ||||
| 9 Perceived feeling of poor control in labour Show forest plot | 1 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.62, 2.21] |
| Analysis 1.9  Comparison 1 Epidural versus opioids, Outcome 9 Perceived feeling of poor control in labour. | ||||
| 10 Satisfaction with childbirth experience ‐ proportion rating satisfied to very satisfied Show forest plot | 1 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.87, 1.03] |
| Analysis 1.10 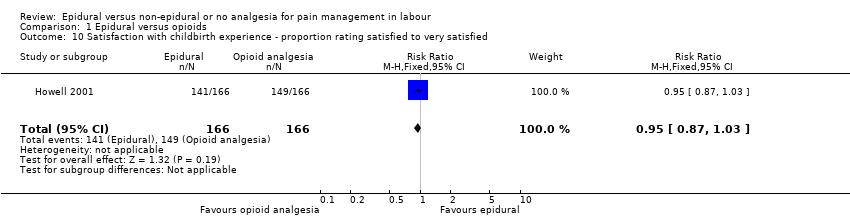 Comparison 1 Epidural versus opioids, Outcome 10 Satisfaction with childbirth experience ‐ proportion rating satisfied to very satisfied. | ||||
| 11 Need for additional means of pain relief Show forest plot | 16 | 5099 | Risk Ratio (M‐H, Random, 95% CI) | 0.10 [0.04, 0.25] |
| Analysis 1.11 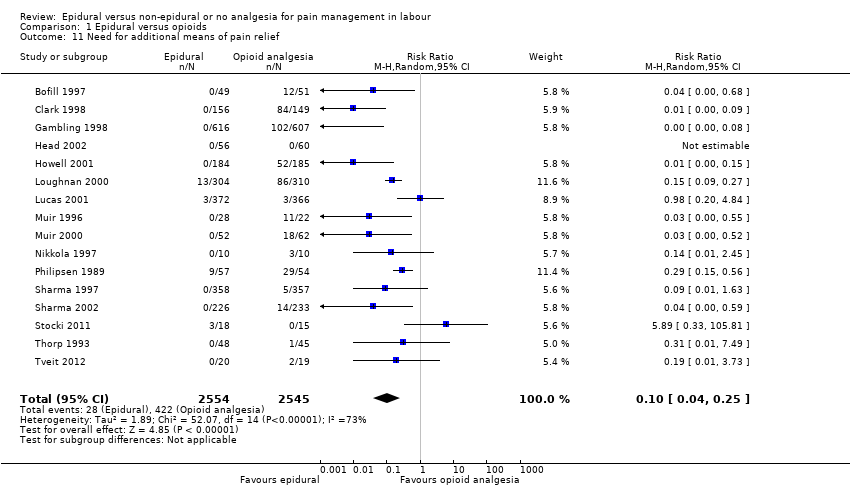 Comparison 1 Epidural versus opioids, Outcome 11 Need for additional means of pain relief. | ||||
| 12 Assisted vaginal birth Show forest plot | 30 | 9948 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.29, 1.60] |
| Analysis 1.12  Comparison 1 Epidural versus opioids, Outcome 12 Assisted vaginal birth. | ||||
| 13 Caesarean section Show forest plot | 33 | 10350 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.18] |
| Analysis 1.13  Comparison 1 Epidural versus opioids, Outcome 13 Caesarean section. | ||||
| 14 Long‐term backache Show forest plot | 2 | 814 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.89, 1.12] |
| Analysis 1.14  Comparison 1 Epidural versus opioids, Outcome 14 Long‐term backache. | ||||
| 15 Hypotension as defined by trial authors Show forest plot | 10 | 4212 | Risk Ratio (M‐H, Random, 95% CI) | 11.34 [1.89, 67.95] |
| Analysis 1.15 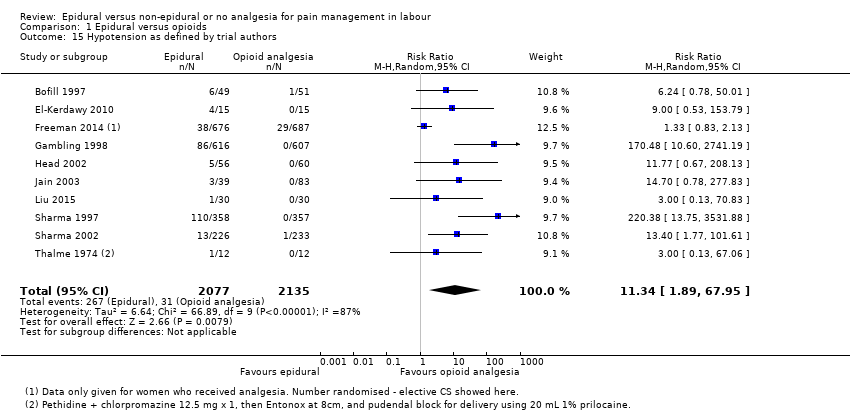 Comparison 1 Epidural versus opioids, Outcome 15 Hypotension as defined by trial authors. | ||||
| 16 Postnatal depression (authors definition, on medication, or self‐reported) Show forest plot | 1 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.38, 1.05] |
| Analysis 1.16  Comparison 1 Epidural versus opioids, Outcome 16 Postnatal depression (authors definition, on medication, or self‐reported). | ||||
| 17 Motor blockade Show forest plot | 3 | 322 | Risk Ratio (M‐H, Fixed, 95% CI) | 31.71 [4.16, 241.99] |
| Analysis 1.17 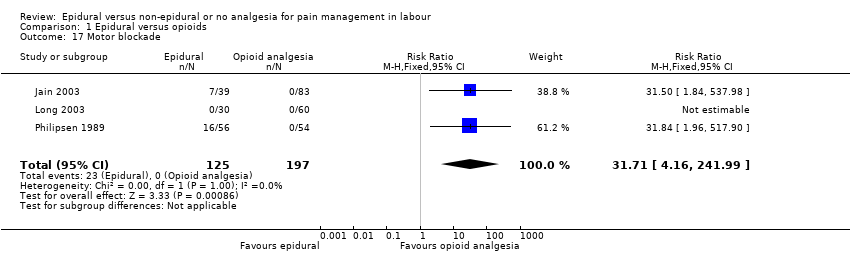 Comparison 1 Epidural versus opioids, Outcome 17 Motor blockade. | ||||
| 18 Respiratory depression requiring oxygen administration Show forest plot | 5 | 2031 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.05, 0.97] |
| Analysis 1.18  Comparison 1 Epidural versus opioids, Outcome 18 Respiratory depression requiring oxygen administration. | ||||
| 19 Headache Show forest plot | 4 | 1938 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.74, 1.54] |
| Analysis 1.19  Comparison 1 Epidural versus opioids, Outcome 19 Headache. | ||||
| 20 Perineal trauma requiring suturing Show forest plot | 1 | 369 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.93, 1.18] |
| Analysis 1.20 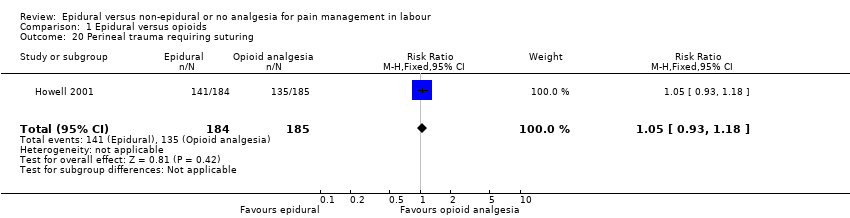 Comparison 1 Epidural versus opioids, Outcome 20 Perineal trauma requiring suturing. | ||||
| 21 Nausea and vomiting Show forest plot | 15 | 4440 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.45, 0.87] |
| Analysis 1.21  Comparison 1 Epidural versus opioids, Outcome 21 Nausea and vomiting. | ||||
| 22 Itch Show forest plot | 8 | 2900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.81, 1.77] |
| Analysis 1.22  Comparison 1 Epidural versus opioids, Outcome 22 Itch. | ||||
| 23 Fever > 38 º C Show forest plot | 9 | 4276 | Risk Ratio (M‐H, Random, 95% CI) | 2.51 [1.67, 3.77] |
| Analysis 1.23  Comparison 1 Epidural versus opioids, Outcome 23 Fever > 38 º C. | ||||
| 24 Shivering Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.27, 92.62] |
| Analysis 1.24 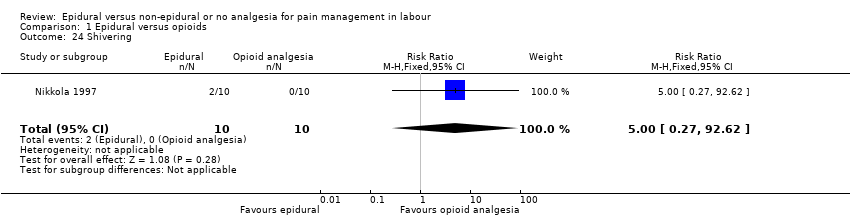 Comparison 1 Epidural versus opioids, Outcome 24 Shivering. | ||||
| 25 Drowsiness Show forest plot | 6 | 740 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.17, 1.33] |
| Analysis 1.25 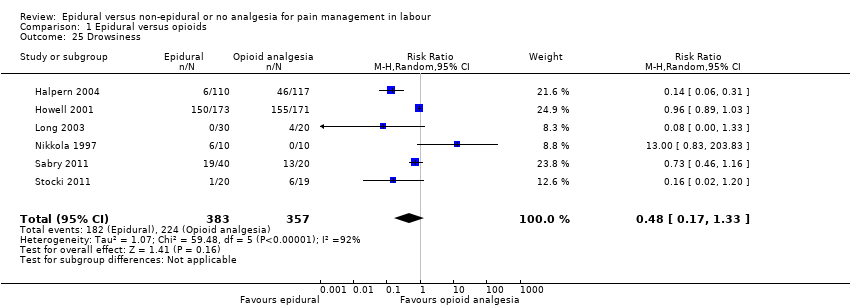 Comparison 1 Epidural versus opioids, Outcome 25 Drowsiness. | ||||
| 26 Urinary retention Show forest plot | 4 | 343 | Risk Ratio (M‐H, Fixed, 95% CI) | 14.18 [4.52, 44.45] |
| Analysis 1.26 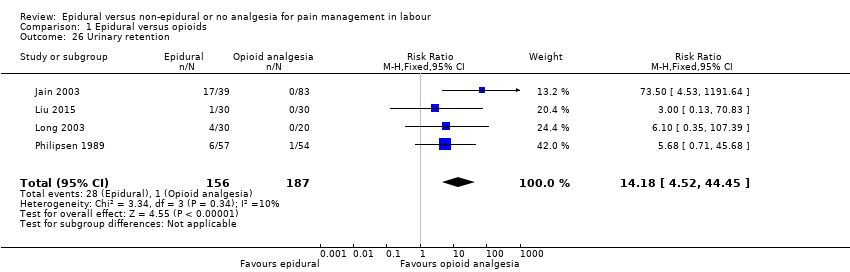 Comparison 1 Epidural versus opioids, Outcome 26 Urinary retention. | ||||
| 27 Catheterisation during labour Show forest plot | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 5.68 [0.71, 45.68] |
| Analysis 1.27  Comparison 1 Epidural versus opioids, Outcome 27 Catheterisation during labour. | ||||
| 28 Malposition Show forest plot | 4 | 673 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.98, 1.99] |
| Analysis 1.28  Comparison 1 Epidural versus opioids, Outcome 28 Malposition. | ||||
| 29 Surgical amniotomy Show forest plot | 2 | 211 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.74, 1.43] |
| Analysis 1.29  Comparison 1 Epidural versus opioids, Outcome 29 Surgical amniotomy. | ||||
| 30 Acidosis defined by cord arterial pH < 7.2 at delivery Show forest plot | 8 | 4783 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.69, 0.94] |
| Analysis 1.30  Comparison 1 Epidural versus opioids, Outcome 30 Acidosis defined by cord arterial pH < 7.2 at delivery. | ||||
| 31 Acidosis defined by cord arterial pH < 7.15 Show forest plot | 3 | 480 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.64, 2.14] |
| Analysis 1.31 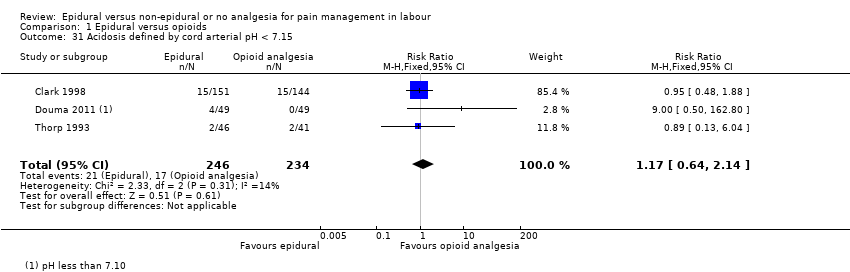 Comparison 1 Epidural versus opioids, Outcome 31 Acidosis defined by cord arterial pH < 7.15. | ||||
| 32 Naloxone administration Show forest plot | 10 | 2645 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.10, 0.23] |
| Analysis 1.32  Comparison 1 Epidural versus opioids, Outcome 32 Naloxone administration. | ||||
| 33 Meconium staining of liquor Show forest plot | 5 | 2295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.84, 1.21] |
| Analysis 1.33  Comparison 1 Epidural versus opioids, Outcome 33 Meconium staining of liquor. | ||||
| 34 Neonatal intensive care unit admission Show forest plot | 8 | 4488 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.12] |
| Analysis 1.34 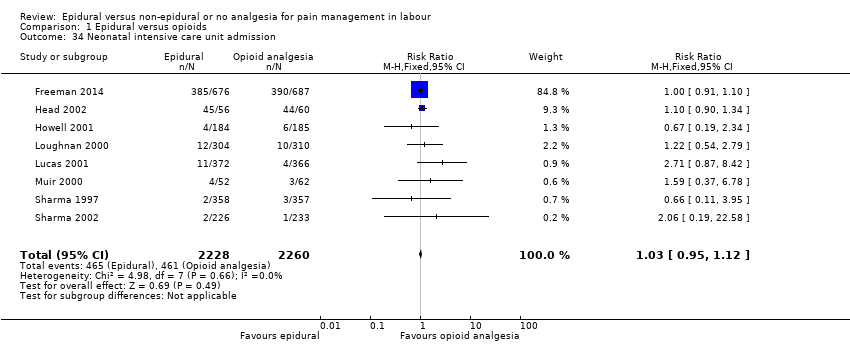 Comparison 1 Epidural versus opioids, Outcome 34 Neonatal intensive care unit admission. | ||||
| 35 Apgar score less than 7 at 5 minutes Show forest plot | 22 | 8752 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.52, 1.02] |
| Analysis 1.35  Comparison 1 Epidural versus opioids, Outcome 35 Apgar score less than 7 at 5 minutes. | ||||
| 36 Length of first stage of labour (minutes) Show forest plot | 9 | 2259 | Mean Difference (IV, Fixed, 95% CI) | 32.28 [18.34, 46.22] |
| Analysis 1.36 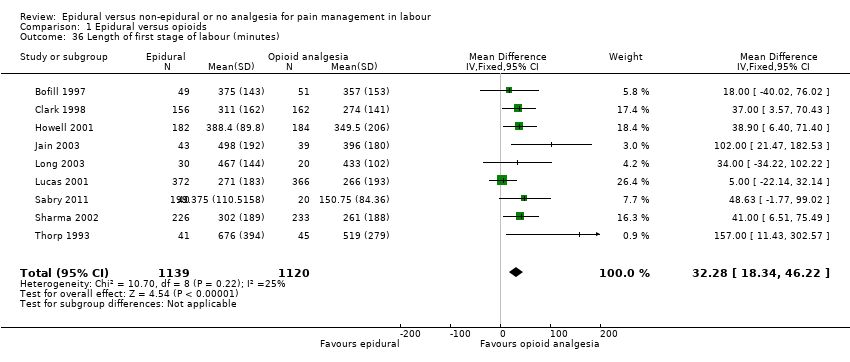 Comparison 1 Epidural versus opioids, Outcome 36 Length of first stage of labour (minutes). | ||||
| 37 Length of second stage of labour (minutes) Show forest plot | 16 | 4979 | Mean Difference (IV, Random, 95% CI) | 15.38 [8.97, 21.79] |
| Analysis 1.37  Comparison 1 Epidural versus opioids, Outcome 37 Length of second stage of labour (minutes). | ||||
| 38 Oxytocin augmentation Show forest plot | 19 | 8351 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [1.00, 1.26] |
| Analysis 1.38  Comparison 1 Epidural versus opioids, Outcome 38 Oxytocin augmentation. | ||||
| 39 Caesarean section for fetal distress Show forest plot | 12 | 5753 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.97, 1.79] |
| Analysis 1.39  Comparison 1 Epidural versus opioids, Outcome 39 Caesarean section for fetal distress. | ||||
| 40 Caesarean section for dystocia Show forest plot | 13 | 5938 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.79, 1.11] |
| Analysis 1.40  Comparison 1 Epidural versus opioids, Outcome 40 Caesarean section for dystocia. | ||||
| 41 Sensitivity analysis ‐ allocation concealment: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 4 | 1372 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.70, 2.92] |
| Analysis 1.41 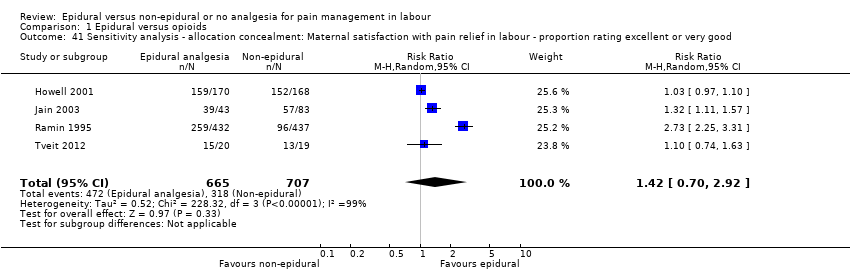 Comparison 1 Epidural versus opioids, Outcome 41 Sensitivity analysis ‐ allocation concealment: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good. | ||||
| 42 Sensitivity analysis ‐ incomplete outcome data: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 3 | 923 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.97, 1.55] |
| Analysis 1.42 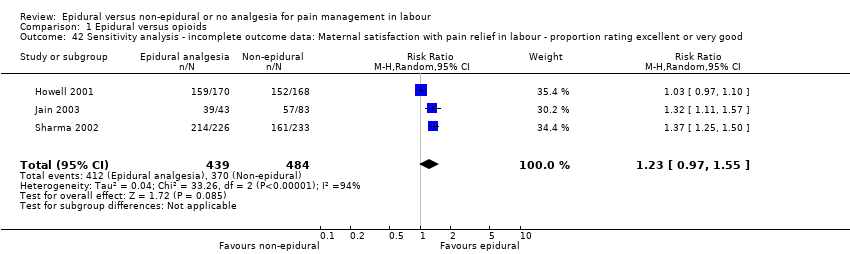 Comparison 1 Epidural versus opioids, Outcome 42 Sensitivity analysis ‐ incomplete outcome data: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good. | ||||
| 43 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief Show forest plot | 9 | 3043 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.03, 0.53] |
| Analysis 1.43 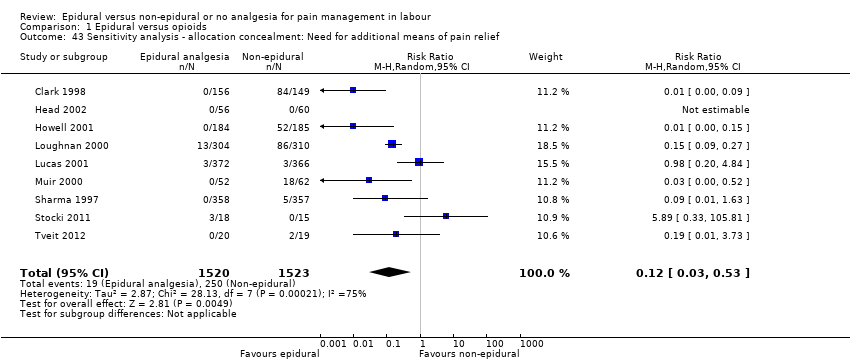 Comparison 1 Epidural versus opioids, Outcome 43 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief. | ||||
| 44 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief Show forest plot | 9 | 3740 | Risk Ratio (M‐H, Random, 95% CI) | 0.15 [0.05, 0.45] |
| Analysis 1.44  Comparison 1 Epidural versus opioids, Outcome 44 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score in labour Show forest plot | 2 | 120 | Std. Mean Difference (IV, Random, 95% CI) | ‐9.55 [‐12.91, ‐6.19] |
| Analysis 2.1  Comparison 2 Epidural versus placebo/no treatment, Outcome 1 Pain score in labour. | ||||
| 2 Woman's perception of pain relief during first stage of labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐55.90 [‐61.09, ‐50.71] |
| Analysis 2.2 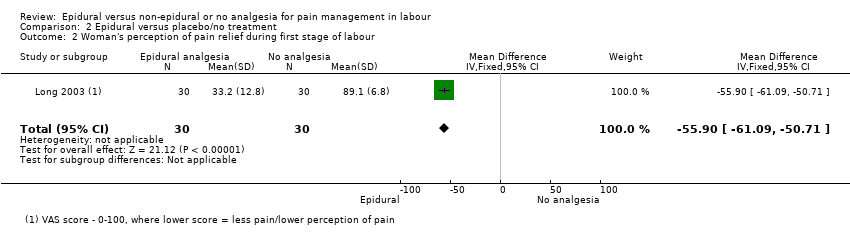 Comparison 2 Epidural versus placebo/no treatment, Outcome 2 Woman's perception of pain relief during first stage of labour. | ||||
| 3 Woman's perception of pain relief during the second stage of labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐55.70 [‐63.54, ‐47.86] |
| Analysis 2.3  Comparison 2 Epidural versus placebo/no treatment, Outcome 3 Woman's perception of pain relief during the second stage of labour. | ||||
| 4 Pain intensity Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.41] |
| Analysis 2.4 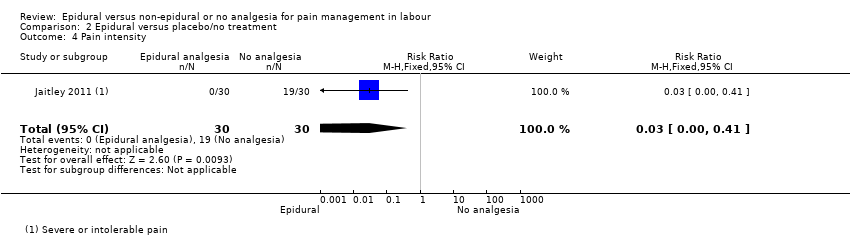 Comparison 2 Epidural versus placebo/no treatment, Outcome 4 Pain intensity. | ||||
| 5 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [1.05, 1.65] |
| Analysis 2.5  Comparison 2 Epidural versus placebo/no treatment, Outcome 5 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good. | ||||
| 6 Perceived feeling of poor control in labour Show forest plot | 2 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.52, 1.50] |
| Analysis 2.6  Comparison 2 Epidural versus placebo/no treatment, Outcome 6 Perceived feeling of poor control in labour. | ||||
| 7 Need for additional means of pain relief Show forest plot | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.14] |
| Analysis 2.7 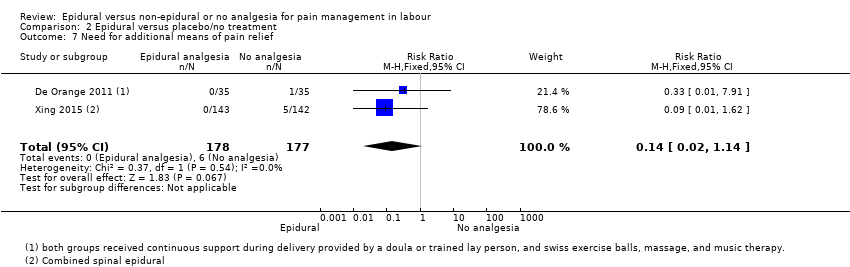 Comparison 2 Epidural versus placebo/no treatment, Outcome 7 Need for additional means of pain relief. | ||||
| 8 Instrumental delivery Show forest plot | 4 | 515 | Risk Ratio (M‐H, Random, 95% CI) | 3.41 [0.62, 18.80] |
| Analysis 2.8 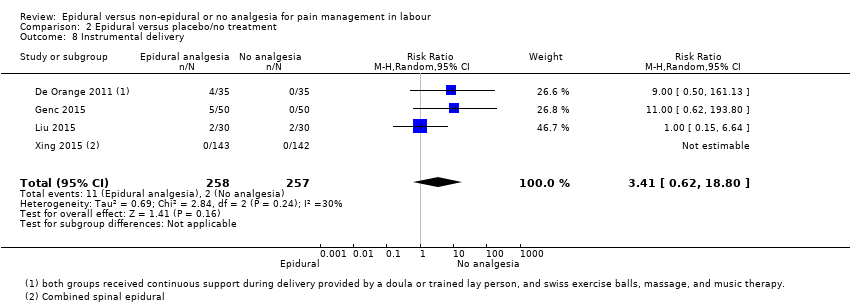 Comparison 2 Epidural versus placebo/no treatment, Outcome 8 Instrumental delivery. | ||||
| 9 Caesarean section Show forest plot | 5 | 578 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.23, 0.90] |
| Analysis 2.9 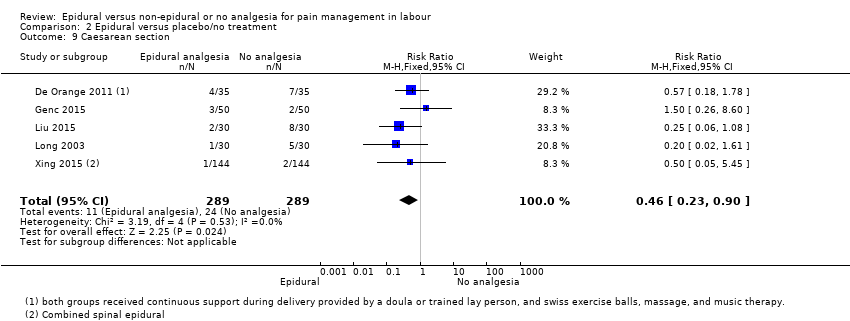 Comparison 2 Epidural versus placebo/no treatment, Outcome 9 Caesarean section. | ||||
| 10 Motor blockade Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 2.10  Comparison 2 Epidural versus placebo/no treatment, Outcome 10 Motor blockade. | ||||
| 11 Headache Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 2.11  Comparison 2 Epidural versus placebo/no treatment, Outcome 11 Headache. | ||||
| 12 Perineal trauma requiring suturing Show forest plot | 1 | 285 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.50] |
| Analysis 2.12 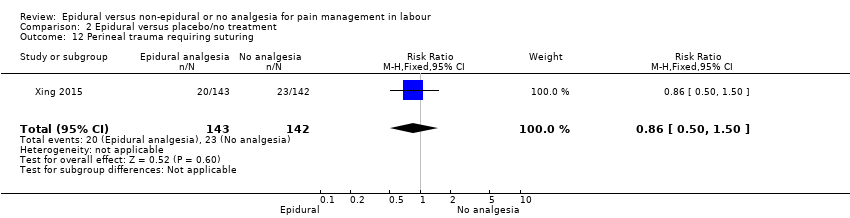 Comparison 2 Epidural versus placebo/no treatment, Outcome 12 Perineal trauma requiring suturing. | ||||
| 13 Nausea and vomiting Show forest plot | 2 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 11.00 [0.62, 193.80] |
| Analysis 2.13  Comparison 2 Epidural versus placebo/no treatment, Outcome 13 Nausea and vomiting. | ||||
| 14 Itch Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| Analysis 2.14  Comparison 2 Epidural versus placebo/no treatment, Outcome 14 Itch. | ||||
| 15 Fever > 38 º C Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.0 [0.63, 191.69] |
| Analysis 2.15  Comparison 2 Epidural versus placebo/no treatment, Outcome 15 Fever > 38 º C. | ||||
| 16 Shivering Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.0 [1.04, 61.62] |
| Analysis 2.16 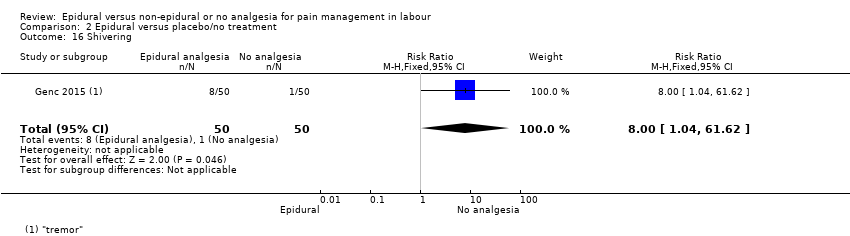 Comparison 2 Epidural versus placebo/no treatment, Outcome 16 Shivering. | ||||
| 17 Drowsiness Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 7.0 [0.37, 132.10] |
| Analysis 2.17  Comparison 2 Epidural versus placebo/no treatment, Outcome 17 Drowsiness. | ||||
| 18 Urinary retention Show forest plot | 2 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.32, 28.21] |
| Analysis 2.18 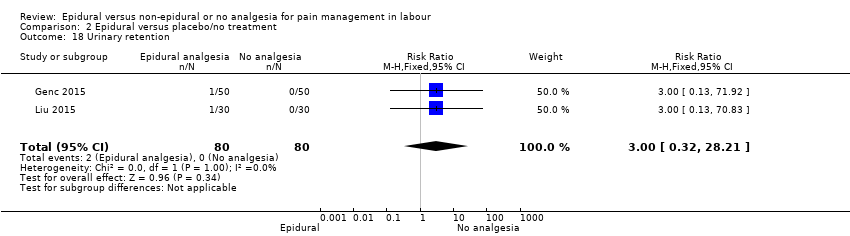 Comparison 2 Epidural versus placebo/no treatment, Outcome 18 Urinary retention. | ||||
| 19 Apgar score less than 7 at 5 minutes Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 2.19  Comparison 2 Epidural versus placebo/no treatment, Outcome 19 Apgar score less than 7 at 5 minutes. | ||||
| 20 Length of first stage of labour (minutes) Show forest plot | 2 | 189 | Mean Difference (IV, Random, 95% CI) | ‐55.09 [‐186.26, 76.09] |
| Analysis 2.20 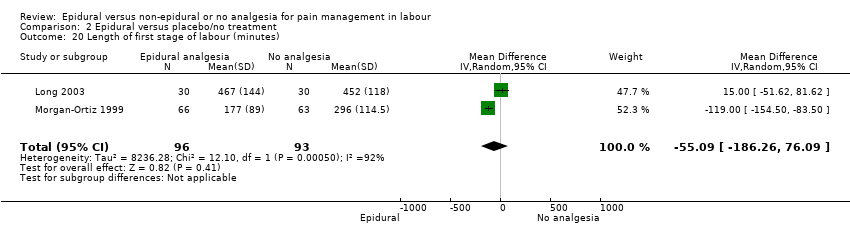 Comparison 2 Epidural versus placebo/no treatment, Outcome 20 Length of first stage of labour (minutes). | ||||
| 21 Length of second stage of labour (minutes) Show forest plot | 4 | 344 | Mean Difference (IV, Random, 95% CI) | 7.66 [‐6.12, 21.45] |
| Analysis 2.21 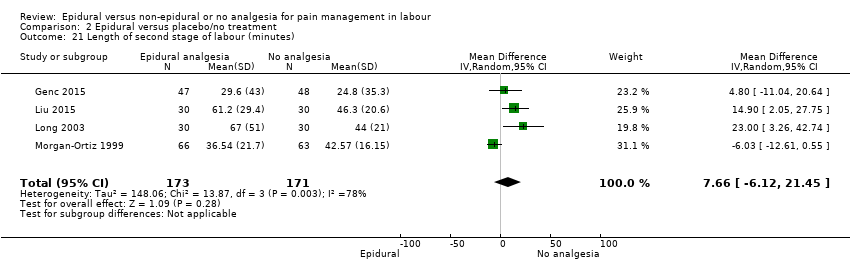 Comparison 2 Epidural versus placebo/no treatment, Outcome 21 Length of second stage of labour (minutes). | ||||
| 22 Oxytocin augmentation Show forest plot | 3 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.63, 1.24] |
| Analysis 2.22  Comparison 2 Epidural versus placebo/no treatment, Outcome 22 Oxytocin augmentation. | ||||
| 23 Caesarean section for fetal distress Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 15.55] |
| Analysis 2.23  Comparison 2 Epidural versus placebo/no treatment, Outcome 23 Caesarean section for fetal distress. | ||||
| 24 Caesarean section for dystocia Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.36] |
| Analysis 2.24 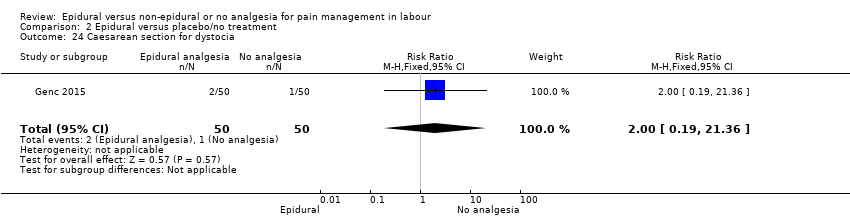 Comparison 2 Epidural versus placebo/no treatment, Outcome 24 Caesarean section for dystocia. | ||||
| 25 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| Analysis 2.25 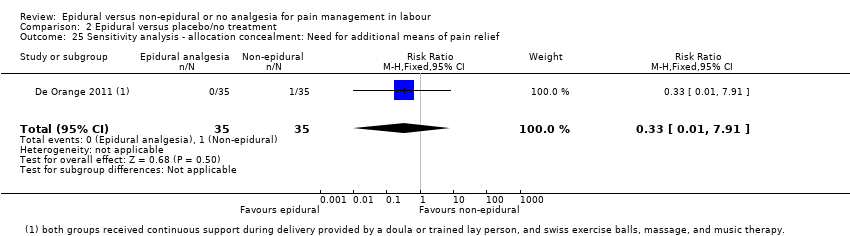 Comparison 2 Epidural versus placebo/no treatment, Outcome 25 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief. | ||||
| 26 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| Analysis 2.26  Comparison 2 Epidural versus placebo/no treatment, Outcome 26 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maternal pain score in labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐53.00 [‐57.98, ‐48.02] |
| Analysis 3.1  Comparison 3 Epidural versus TENS, Outcome 1 Maternal pain score in labour. | ||||
| 2 Instrumental delivery Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.64] |
| Analysis 3.2  Comparison 3 Epidural versus TENS, Outcome 2 Instrumental delivery. | ||||
| 3 Caesarean section Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 20.90] |
| Analysis 3.3  Comparison 3 Epidural versus TENS, Outcome 3 Caesarean section. | ||||
| 4 Hypotension as defined by trial authors Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| Analysis 3.4  Comparison 3 Epidural versus TENS, Outcome 4 Hypotension as defined by trial authors. | ||||
| 5 Urinary retention Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| Analysis 3.5  Comparison 3 Epidural versus TENS, Outcome 5 Urinary retention. | ||||
| 6 Nausea and vomiting Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 3.6  Comparison 3 Epidural versus TENS, Outcome 6 Nausea and vomiting. | ||||
| 7 Length of second stage of labour (minutes) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 17.90 [5.66, 30.14] |
| Analysis 3.7 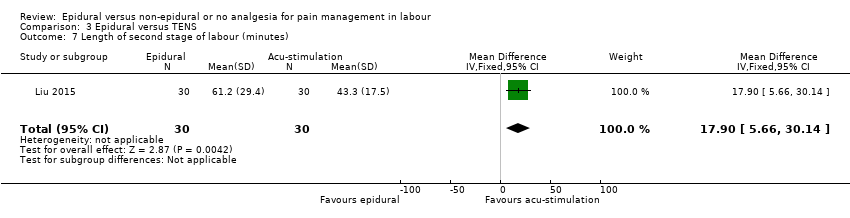 Comparison 3 Epidural versus TENS, Outcome 7 Length of second stage of labour (minutes). | ||||
| 8 Oxytocin augmentation Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.59, 1.97] |
| Analysis 3.8  Comparison 3 Epidural versus TENS, Outcome 8 Oxytocin augmentation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [1.31, 3.62] |
| Analysis 4.1 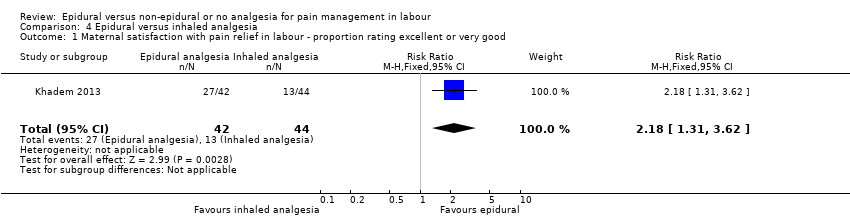 Comparison 4 Epidural versus inhaled analgesia, Outcome 1 Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good. | ||||
| 2 Caesarean section Show forest plot | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.16, 2.47] |
| Analysis 4.2  Comparison 4 Epidural versus inhaled analgesia, Outcome 2 Caesarean section. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [1.00, 1.02] |
| Analysis 5.1  Comparison 5 Epidural versus continuous support, Outcome 1 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good. | ||||
| 2 Need for additional means of pain relief Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.00 [0.00, 0.03] |
| Analysis 5.2  Comparison 5 Epidural versus continuous support, Outcome 2 Need for additional means of pain relief. | ||||
| 3 Instrumental delivery Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.96, 1.39] |
| Analysis 5.3  Comparison 5 Epidural versus continuous support, Outcome 3 Instrumental delivery. | ||||
| 4 Caesarean section Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.91, 1.62] |
| Analysis 5.4  Comparison 5 Epidural versus continuous support, Outcome 4 Caesarean section. | ||||
| 5 Long‐term backache Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.69, 1.11] |
| Analysis 5.5  Comparison 5 Epidural versus continuous support, Outcome 5 Long‐term backache. | ||||
| 6 Headache Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.79, 1.17] |
| Analysis 5.6  Comparison 5 Epidural versus continuous support, Outcome 6 Headache. | ||||
| 7 Nausea and vomiting Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.80, 1.57] |
| Analysis 5.7  Comparison 5 Epidural versus continuous support, Outcome 7 Nausea and vomiting. | ||||
| 8 Cathetherisation during labour Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.04, 1.29] |
| Analysis 5.8 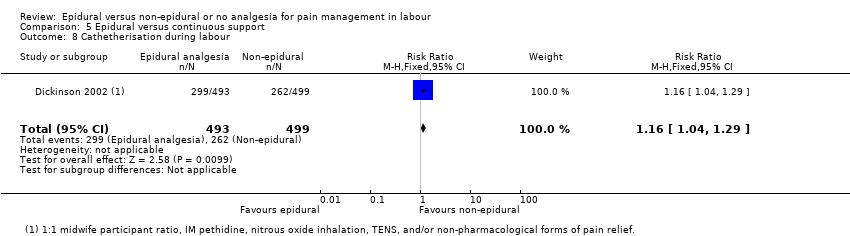 Comparison 5 Epidural versus continuous support, Outcome 8 Cathetherisation during labour. | ||||
| 9 Apgar score less than 7 at 5 minutes Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.61, 6.68] |
| Analysis 5.9 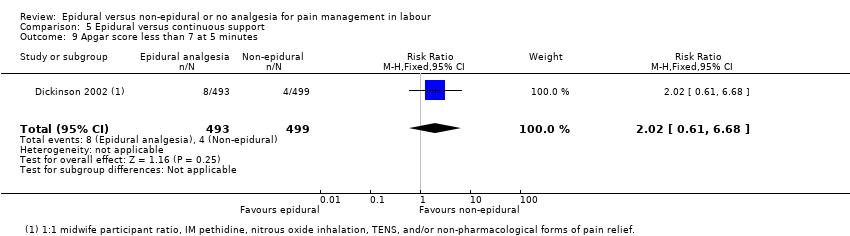 Comparison 5 Epidural versus continuous support, Outcome 9 Apgar score less than 7 at 5 minutes. | ||||

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot of comparison: 1 Epidural versus opioids, outcome: 1.12 Assisted vaginal birth.

Funnel plot of comparison: 1 Epidural versus opioids, outcome: 1.13 Caesarean section.

Funnel plot of comparison: 1 Epidural versus opioids, outcome: 1.35 Apgar score less than 7 at 5 minutes.

Comparison 1 Epidural versus opioids, Outcome 1 Pain score in labour.

Comparison 1 Epidural versus opioids, Outcome 2 Pain intensity severe or intolerable.

Comparison 1 Epidural versus opioids, Outcome 3 Woman's perception of pain relief in labour.

Comparison 1 Epidural versus opioids, Outcome 4 Woman's perception of pain relief during first stage of labour.

Comparison 1 Epidural versus opioids, Outcome 5 Woman's perception of pain relief during the second stage of labour.

Comparison 1 Epidural versus opioids, Outcome 6 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good.

Comparison 1 Epidural versus opioids, Outcome 7 Satisfaction with pain relief in labour ‐ continuous data.

Comparison 1 Epidural versus opioids, Outcome 8 Time of administration of pain relief to time pain relief was satisfactory (minutes).
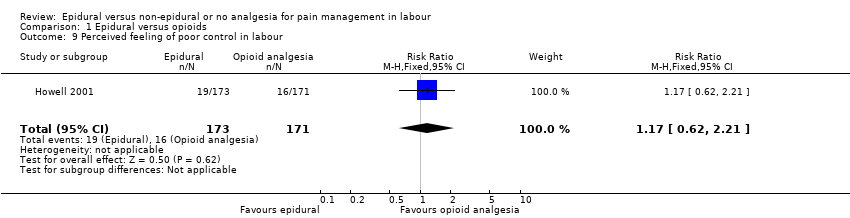
Comparison 1 Epidural versus opioids, Outcome 9 Perceived feeling of poor control in labour.

Comparison 1 Epidural versus opioids, Outcome 10 Satisfaction with childbirth experience ‐ proportion rating satisfied to very satisfied.

Comparison 1 Epidural versus opioids, Outcome 11 Need for additional means of pain relief.

Comparison 1 Epidural versus opioids, Outcome 12 Assisted vaginal birth.

Comparison 1 Epidural versus opioids, Outcome 13 Caesarean section.

Comparison 1 Epidural versus opioids, Outcome 14 Long‐term backache.

Comparison 1 Epidural versus opioids, Outcome 15 Hypotension as defined by trial authors.

Comparison 1 Epidural versus opioids, Outcome 16 Postnatal depression (authors definition, on medication, or self‐reported).

Comparison 1 Epidural versus opioids, Outcome 17 Motor blockade.

Comparison 1 Epidural versus opioids, Outcome 18 Respiratory depression requiring oxygen administration.

Comparison 1 Epidural versus opioids, Outcome 19 Headache.

Comparison 1 Epidural versus opioids, Outcome 20 Perineal trauma requiring suturing.

Comparison 1 Epidural versus opioids, Outcome 21 Nausea and vomiting.

Comparison 1 Epidural versus opioids, Outcome 22 Itch.

Comparison 1 Epidural versus opioids, Outcome 23 Fever > 38 º C.

Comparison 1 Epidural versus opioids, Outcome 24 Shivering.

Comparison 1 Epidural versus opioids, Outcome 25 Drowsiness.

Comparison 1 Epidural versus opioids, Outcome 26 Urinary retention.

Comparison 1 Epidural versus opioids, Outcome 27 Catheterisation during labour.

Comparison 1 Epidural versus opioids, Outcome 28 Malposition.

Comparison 1 Epidural versus opioids, Outcome 29 Surgical amniotomy.

Comparison 1 Epidural versus opioids, Outcome 30 Acidosis defined by cord arterial pH < 7.2 at delivery.

Comparison 1 Epidural versus opioids, Outcome 31 Acidosis defined by cord arterial pH < 7.15.

Comparison 1 Epidural versus opioids, Outcome 32 Naloxone administration.

Comparison 1 Epidural versus opioids, Outcome 33 Meconium staining of liquor.

Comparison 1 Epidural versus opioids, Outcome 34 Neonatal intensive care unit admission.

Comparison 1 Epidural versus opioids, Outcome 35 Apgar score less than 7 at 5 minutes.

Comparison 1 Epidural versus opioids, Outcome 36 Length of first stage of labour (minutes).

Comparison 1 Epidural versus opioids, Outcome 37 Length of second stage of labour (minutes).

Comparison 1 Epidural versus opioids, Outcome 38 Oxytocin augmentation.

Comparison 1 Epidural versus opioids, Outcome 39 Caesarean section for fetal distress.

Comparison 1 Epidural versus opioids, Outcome 40 Caesarean section for dystocia.

Comparison 1 Epidural versus opioids, Outcome 41 Sensitivity analysis ‐ allocation concealment: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good.

Comparison 1 Epidural versus opioids, Outcome 42 Sensitivity analysis ‐ incomplete outcome data: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good.

Comparison 1 Epidural versus opioids, Outcome 43 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief.

Comparison 1 Epidural versus opioids, Outcome 44 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief.

Comparison 2 Epidural versus placebo/no treatment, Outcome 1 Pain score in labour.

Comparison 2 Epidural versus placebo/no treatment, Outcome 2 Woman's perception of pain relief during first stage of labour.

Comparison 2 Epidural versus placebo/no treatment, Outcome 3 Woman's perception of pain relief during the second stage of labour.
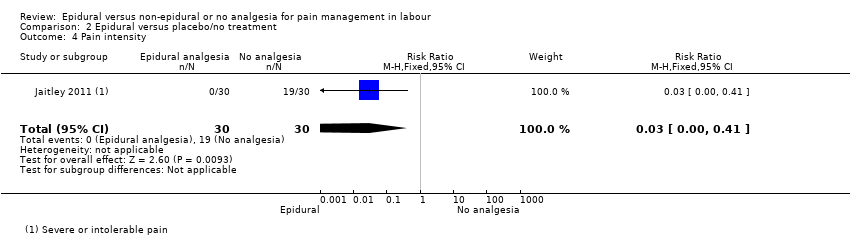
Comparison 2 Epidural versus placebo/no treatment, Outcome 4 Pain intensity.

Comparison 2 Epidural versus placebo/no treatment, Outcome 5 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good.

Comparison 2 Epidural versus placebo/no treatment, Outcome 6 Perceived feeling of poor control in labour.

Comparison 2 Epidural versus placebo/no treatment, Outcome 7 Need for additional means of pain relief.

Comparison 2 Epidural versus placebo/no treatment, Outcome 8 Instrumental delivery.

Comparison 2 Epidural versus placebo/no treatment, Outcome 9 Caesarean section.

Comparison 2 Epidural versus placebo/no treatment, Outcome 10 Motor blockade.

Comparison 2 Epidural versus placebo/no treatment, Outcome 11 Headache.

Comparison 2 Epidural versus placebo/no treatment, Outcome 12 Perineal trauma requiring suturing.

Comparison 2 Epidural versus placebo/no treatment, Outcome 13 Nausea and vomiting.

Comparison 2 Epidural versus placebo/no treatment, Outcome 14 Itch.

Comparison 2 Epidural versus placebo/no treatment, Outcome 15 Fever > 38 º C.

Comparison 2 Epidural versus placebo/no treatment, Outcome 16 Shivering.

Comparison 2 Epidural versus placebo/no treatment, Outcome 17 Drowsiness.

Comparison 2 Epidural versus placebo/no treatment, Outcome 18 Urinary retention.

Comparison 2 Epidural versus placebo/no treatment, Outcome 19 Apgar score less than 7 at 5 minutes.

Comparison 2 Epidural versus placebo/no treatment, Outcome 20 Length of first stage of labour (minutes).

Comparison 2 Epidural versus placebo/no treatment, Outcome 21 Length of second stage of labour (minutes).

Comparison 2 Epidural versus placebo/no treatment, Outcome 22 Oxytocin augmentation.

Comparison 2 Epidural versus placebo/no treatment, Outcome 23 Caesarean section for fetal distress.

Comparison 2 Epidural versus placebo/no treatment, Outcome 24 Caesarean section for dystocia.

Comparison 2 Epidural versus placebo/no treatment, Outcome 25 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief.
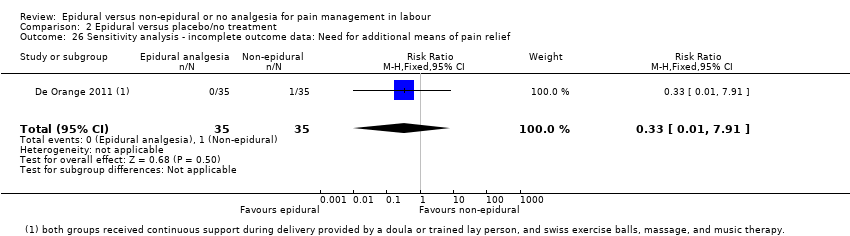
Comparison 2 Epidural versus placebo/no treatment, Outcome 26 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief.

Comparison 3 Epidural versus TENS, Outcome 1 Maternal pain score in labour.

Comparison 3 Epidural versus TENS, Outcome 2 Instrumental delivery.

Comparison 3 Epidural versus TENS, Outcome 3 Caesarean section.

Comparison 3 Epidural versus TENS, Outcome 4 Hypotension as defined by trial authors.

Comparison 3 Epidural versus TENS, Outcome 5 Urinary retention.

Comparison 3 Epidural versus TENS, Outcome 6 Nausea and vomiting.

Comparison 3 Epidural versus TENS, Outcome 7 Length of second stage of labour (minutes).

Comparison 3 Epidural versus TENS, Outcome 8 Oxytocin augmentation.

Comparison 4 Epidural versus inhaled analgesia, Outcome 1 Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good.

Comparison 4 Epidural versus inhaled analgesia, Outcome 2 Caesarean section.

Comparison 5 Epidural versus continuous support, Outcome 1 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good.

Comparison 5 Epidural versus continuous support, Outcome 2 Need for additional means of pain relief.

Comparison 5 Epidural versus continuous support, Outcome 3 Instrumental delivery.

Comparison 5 Epidural versus continuous support, Outcome 4 Caesarean section.

Comparison 5 Epidural versus continuous support, Outcome 5 Long‐term backache.

Comparison 5 Epidural versus continuous support, Outcome 6 Headache.

Comparison 5 Epidural versus continuous support, Outcome 7 Nausea and vomiting.
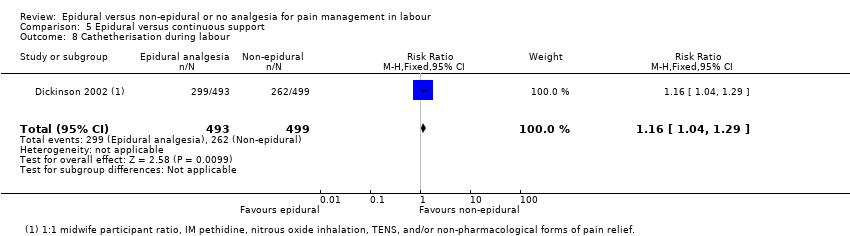
Comparison 5 Epidural versus continuous support, Outcome 8 Cathetherisation during labour.

Comparison 5 Epidural versus continuous support, Outcome 9 Apgar score less than 7 at 5 minutes.
| Epidural compared to opioids in labour (maternal outcomes) | ||||||
| Patient or population: women in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with opioids | Risk with epidural | |||||
| Pain intensity measured using pain score in labour (lower scores = less pain) | SMD 2.64 lower | ‐ | 1133 | ⊕⊕⊝⊝ | ‐ | |
| Satisfaction with pain relief ‐ proportion rating excellent or very good | Study population | Average RR 1.47 | 1911 | ⊕⊕⊝⊝ | ‐ | |
| 500 per 1000 | 735 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.44 | 9948 | ⊕⊕⊝⊝ | ‐ | |
| 99 per 1000 | 142 per 1000 | |||||
| Caesarean section | Study population | RR 1.07 | 10,350 | ⊕⊕⊕⊝ | ‐ | |
| 114 per 1000 | 122 per 1000 | |||||
| Side effects (maternal) ‐ long‐term backache | Study population | RR 1.00 | 814 | ⊕⊕⊕⊝ | ‐ | |
| 585 per 1000 | 585 per 1000 | |||||
| Admission to special care baby unit/neonatal intensive care unit (as defined by trialists) | Study population | RR 1.03 | 4488 | ⊕⊕⊕⊝ | ‐ | |
| 204 per 1000 | 210 per 1000 (194 to 228) | |||||
| Apgar score less than 7 at 5 minutes | Study population | RR 0.73 | 8752 | ⊕⊕⊝⊝ | ‐ | |
| 17 per 1000 | 12 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded due to limitation of study design (‐1). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score in labour Show forest plot | 5 | 1133 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐4.56, ‐0.73] |
| 2 Pain intensity severe or intolerable Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Woman's perception of pain relief in labour Show forest plot | 3 | 1166 | Mean Difference (IV, Random, 95% CI) | ‐3.36 [‐5.41, ‐1.31] |
| 4 Woman's perception of pain relief during first stage of labour Show forest plot | 3 | 194 | Mean Difference (IV, Random, 95% CI) | ‐12.05 [‐19.35, ‐4.75] |
| 5 Woman's perception of pain relief during the second stage of labour Show forest plot | 2 | 164 | Mean Difference (IV, Fixed, 95% CI) | ‐20.75 [‐22.50, ‐19.01] |
| 6 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 7 | 1911 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [1.03, 2.08] |
| 7 Satisfaction with pain relief in labour ‐ continuous data Show forest plot | 7 | 3171 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.10, 0.91] |
| 8 Time of administration of pain relief to time pain relief was satisfactory (minutes) Show forest plot | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐6.70 [‐8.02, ‐5.38] |
| 9 Perceived feeling of poor control in labour Show forest plot | 1 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.62, 2.21] |
| 10 Satisfaction with childbirth experience ‐ proportion rating satisfied to very satisfied Show forest plot | 1 | 332 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.87, 1.03] |
| 11 Need for additional means of pain relief Show forest plot | 16 | 5099 | Risk Ratio (M‐H, Random, 95% CI) | 0.10 [0.04, 0.25] |
| 12 Assisted vaginal birth Show forest plot | 30 | 9948 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.29, 1.60] |
| 13 Caesarean section Show forest plot | 33 | 10350 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.18] |
| 14 Long‐term backache Show forest plot | 2 | 814 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.89, 1.12] |
| 15 Hypotension as defined by trial authors Show forest plot | 10 | 4212 | Risk Ratio (M‐H, Random, 95% CI) | 11.34 [1.89, 67.95] |
| 16 Postnatal depression (authors definition, on medication, or self‐reported) Show forest plot | 1 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.38, 1.05] |
| 17 Motor blockade Show forest plot | 3 | 322 | Risk Ratio (M‐H, Fixed, 95% CI) | 31.71 [4.16, 241.99] |
| 18 Respiratory depression requiring oxygen administration Show forest plot | 5 | 2031 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.05, 0.97] |
| 19 Headache Show forest plot | 4 | 1938 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.74, 1.54] |
| 20 Perineal trauma requiring suturing Show forest plot | 1 | 369 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.93, 1.18] |
| 21 Nausea and vomiting Show forest plot | 15 | 4440 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.45, 0.87] |
| 22 Itch Show forest plot | 8 | 2900 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.81, 1.77] |
| 23 Fever > 38 º C Show forest plot | 9 | 4276 | Risk Ratio (M‐H, Random, 95% CI) | 2.51 [1.67, 3.77] |
| 24 Shivering Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.27, 92.62] |
| 25 Drowsiness Show forest plot | 6 | 740 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.17, 1.33] |
| 26 Urinary retention Show forest plot | 4 | 343 | Risk Ratio (M‐H, Fixed, 95% CI) | 14.18 [4.52, 44.45] |
| 27 Catheterisation during labour Show forest plot | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 5.68 [0.71, 45.68] |
| 28 Malposition Show forest plot | 4 | 673 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.98, 1.99] |
| 29 Surgical amniotomy Show forest plot | 2 | 211 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.74, 1.43] |
| 30 Acidosis defined by cord arterial pH < 7.2 at delivery Show forest plot | 8 | 4783 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.69, 0.94] |
| 31 Acidosis defined by cord arterial pH < 7.15 Show forest plot | 3 | 480 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.64, 2.14] |
| 32 Naloxone administration Show forest plot | 10 | 2645 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.10, 0.23] |
| 33 Meconium staining of liquor Show forest plot | 5 | 2295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.84, 1.21] |
| 34 Neonatal intensive care unit admission Show forest plot | 8 | 4488 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.12] |
| 35 Apgar score less than 7 at 5 minutes Show forest plot | 22 | 8752 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.52, 1.02] |
| 36 Length of first stage of labour (minutes) Show forest plot | 9 | 2259 | Mean Difference (IV, Fixed, 95% CI) | 32.28 [18.34, 46.22] |
| 37 Length of second stage of labour (minutes) Show forest plot | 16 | 4979 | Mean Difference (IV, Random, 95% CI) | 15.38 [8.97, 21.79] |
| 38 Oxytocin augmentation Show forest plot | 19 | 8351 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [1.00, 1.26] |
| 39 Caesarean section for fetal distress Show forest plot | 12 | 5753 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.97, 1.79] |
| 40 Caesarean section for dystocia Show forest plot | 13 | 5938 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.79, 1.11] |
| 41 Sensitivity analysis ‐ allocation concealment: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 4 | 1372 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.70, 2.92] |
| 42 Sensitivity analysis ‐ incomplete outcome data: Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 3 | 923 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.97, 1.55] |
| 43 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief Show forest plot | 9 | 3043 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.03, 0.53] |
| 44 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief Show forest plot | 9 | 3740 | Risk Ratio (M‐H, Random, 95% CI) | 0.15 [0.05, 0.45] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score in labour Show forest plot | 2 | 120 | Std. Mean Difference (IV, Random, 95% CI) | ‐9.55 [‐12.91, ‐6.19] |
| 2 Woman's perception of pain relief during first stage of labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐55.90 [‐61.09, ‐50.71] |
| 3 Woman's perception of pain relief during the second stage of labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐55.70 [‐63.54, ‐47.86] |
| 4 Pain intensity Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.41] |
| 5 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [1.05, 1.65] |
| 6 Perceived feeling of poor control in labour Show forest plot | 2 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.52, 1.50] |
| 7 Need for additional means of pain relief Show forest plot | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.14] |
| 8 Instrumental delivery Show forest plot | 4 | 515 | Risk Ratio (M‐H, Random, 95% CI) | 3.41 [0.62, 18.80] |
| 9 Caesarean section Show forest plot | 5 | 578 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.23, 0.90] |
| 10 Motor blockade Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Headache Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Perineal trauma requiring suturing Show forest plot | 1 | 285 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.50] |
| 13 Nausea and vomiting Show forest plot | 2 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 11.00 [0.62, 193.80] |
| 14 Itch Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| 15 Fever > 38 º C Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.0 [0.63, 191.69] |
| 16 Shivering Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.0 [1.04, 61.62] |
| 17 Drowsiness Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 7.0 [0.37, 132.10] |
| 18 Urinary retention Show forest plot | 2 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.32, 28.21] |
| 19 Apgar score less than 7 at 5 minutes Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Length of first stage of labour (minutes) Show forest plot | 2 | 189 | Mean Difference (IV, Random, 95% CI) | ‐55.09 [‐186.26, 76.09] |
| 21 Length of second stage of labour (minutes) Show forest plot | 4 | 344 | Mean Difference (IV, Random, 95% CI) | 7.66 [‐6.12, 21.45] |
| 22 Oxytocin augmentation Show forest plot | 3 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.63, 1.24] |
| 23 Caesarean section for fetal distress Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 15.55] |
| 24 Caesarean section for dystocia Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.36] |
| 25 Sensitivity analysis ‐ allocation concealment: Need for additional means of pain relief Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 26 Sensitivity analysis ‐ incomplete outcome data: Need for additional means of pain relief Show forest plot | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maternal pain score in labour Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐53.00 [‐57.98, ‐48.02] |
| 2 Instrumental delivery Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.64] |
| 3 Caesarean section Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 20.90] |
| 4 Hypotension as defined by trial authors Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| 5 Urinary retention Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| 6 Nausea and vomiting Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Length of second stage of labour (minutes) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 17.90 [5.66, 30.14] |
| 8 Oxytocin augmentation Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.59, 1.97] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maternal satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.18 [1.31, 3.62] |
| 2 Caesarean section Show forest plot | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.16, 2.47] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Satisfaction with pain relief in labour ‐ proportion rating excellent or very good Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [1.00, 1.02] |
| 2 Need for additional means of pain relief Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.00 [0.00, 0.03] |
| 3 Instrumental delivery Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.96, 1.39] |
| 4 Caesarean section Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.91, 1.62] |
| 5 Long‐term backache Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.69, 1.11] |
| 6 Headache Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.79, 1.17] |
| 7 Nausea and vomiting Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.80, 1.57] |
| 8 Cathetherisation during labour Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.04, 1.29] |
| 9 Apgar score less than 7 at 5 minutes Show forest plot | 1 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.61, 6.68] |

