Повторные люмбальные или вентрикулярные пункции у новорожденных с внутрижелудочковым кровоизлиянием
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Open randomised clinical trial | |
| Participants | Preterm infants with grade 3 or 4 intraventricular haemorrhage (IVH) on ultrasound scan | |
| Interventions | Daily lumbar puncture starting at 7 to 10 days. Cerebrospinal fluid (CSF) was drained until flow stopped. Lumbar punctures were continued until the ventricular size decreased, remained unchanged for 2 consecutive weeks, or if the infant developed hydrocephalus requiring a ventricular drain or shunt. | |
| Outcomes |
| |
| Notes | This trial used a random number table for treatment allocation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial used a random number table to allocate participants to treatment. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not give any information regarding allocation concealment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial authors reported that the ultrasonographers were blinded to study classification. However, the trial defined hydrocephalus as an outcome by ultrasound and clinical signs of raised ICP. The trial authors did not give any information as to whether the assessors of the clinical signs of raised ICP were blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | The trial included almost all participants to the end of the trial. |
| Selective reporting (reporting bias) | Low risk | The trial authors reported on the main outcomes of hydrocephalus, death, and shunt placement. The trial did not test the neurodevelopmental outcome. |
| Other bias | Low risk | No other sources of bias identified |
| Methods | Open randomised clinical trial using random number tables | |
| Participants | Neonates with asymptomatic severe posthaemorrhagic hydrocephalus (PHH) | |
| Interventions | Daily lumbar punctures, taking enough CSF to lower the CSF pressure by half. Volumes ranged from 2 to 21 mL. Duration 1 to 3 weeks. | |
| Outcomes |
| |
| Notes | The trial authors did not state whether the paediatric neurologists and the psychologist were blind to early treatment allocation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial used a random number table to allocate participants to treatment. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not give any information regarding allocation concealment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial authors did not give any information regarding whether or not the observers of outcomes (neurologists and psychologist) were blinded to treatment group. |
| Incomplete outcome data (attrition bias) | Low risk | The trial included all children for the outcome of hydrocephalus management failure. Regarding neurodevelopmental follow‐up, 1/15 children in the close observation group were lost to follow‐up at 1 to 2 years. None of the 16 children in the LP group were lost to follow‐up. At 3 to 6 years, 1/15 children in the close observation group and 1/16 children in the LP group were lost to follow‐up. This small proportion of missing data is unlikely to have a significant bias to the outcome. |
| Selective reporting (reporting bias) | Low risk | The trial reported the main outcomes of death, hydrocephalus, shunt placement, and disability. |
| Other bias | Low risk | No other sources of bias identified |
| Methods | Open clinical trial with alternation of treatment | |
| Participants | Infants weighing less than 2000 g with grade 2 or 3 IVH on computed tomography (CT) scan | |
| Interventions | Daily lumbar punctures starting 24 hours after diagnosis of IVH. 3 to 5 mL CSF was removed daily. Lumbar punctures were continued until the CSF was clear and protein concentration was < 180 mg/dL. | |
| Outcomes |
| |
| Notes | Not true randomisation. The trial authors did not state whether or not the observers of outcomes were blinded to early treatment allocation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The trial used an alternation method to assign participants to treatment. |
| Allocation concealment (selection bias) | High risk | Alternation method, allocation method not concealed to researchers. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial authors did not state whether or not the outcome observers were blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | The trial authors analysed almost all participants recruited to the trial. |
| Selective reporting (reporting bias) | Low risk | The trial authors commented on the main outcomes of hydrocephalus, shunt placement, and death. The trial did not test neurodevelopmental outcomes. |
| Other bias | Low risk | No other sources of bias identified |
| Methods | Open randomised multicentre clinical trial at 15 neonatal intensive care units in England, Ireland, and Switzerland. Randomisation by telephoning and registering the infant before hearing the allocation. | |
| Participants | Neonates with IVH, with progressive increase in ventricular size and whose ventricular width had increased to 4 mm over the 97th centile. | |
| Interventions | Repeated lumbar puncture taking as much CSF as possible, maximum 2% body weight, carried out daily or less frequently to prevent further increases in ventricular size. If not more than 2 mL of CSF could be obtained, ventricular tapping was carried out in the same way and often enough to hold the ventricular width constant. | |
| Outcomes |
| |
| Notes | The developmental paediatrician that assessed the survivors at 12 and 30 months was blinded to early treatment allocation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial used a telephone method to allocate participants to treatment. |
| Allocation concealment (selection bias) | Low risk | The trial used a telephone method to allocate participants to treatment. |
| Blinding (performance bias and detection bias) | Low risk | The developmental paediatrician that assessed survivors was blinded to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | At 12 months follow‐up, 3/79 children in the early tapping group and 3/78 children in the conservative group were lost to follow‐up. By 30 months, a further 3 in the early tapping group and 4 in the conservative management group were lost to follow‐up. This small proportion of missing data is unlikely to have significantly biased the outcome. |
| Selective reporting (reporting bias) | Low risk | The trial authors reported the main outcomes of interest: death, hydrocephalus, shunt placement, and disability. |
| Other bias | Low risk | No other sources of bias identified |
Abbreviations: CT: computed tomography; ICP: intracranial pressure; IVH: intraventricular haemorrhage; PHH: posthaemorrhagic hydrocephalus; RCT: randomised controlled trial; VPS: ventriculoperitoneal shunt.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a randomised controlled trial (RCT). | |
| Not a RCT. | |
| Not a RCT. |
Abbreviations: RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A multicentre randomised controlled trial of low versus high threshold treatment in preterm infants with progressive posthaemorrhagic ventricular dilatation (PHVD) |
| Methods | The infants are randomly allocated to the low threshold group or the high threshold group. Those in the low threshold group are treated when the ventricles reach a lower size threshold compared with the high threshold group. Treatment consists of lumbar punctures, where a needle is inserted into the lower part of the spine to drain fluid. If lumbar punctures are still needed over 28 days after the first one, a shunt is inserted into the brain to drain fluid. The two groups are compared with regard to how many infants need a shunt and their brain development at two years of age. |
| Participants | Premature infants with: |
| Interventions | Comparison: low threshold versus high threshold intervention. Intervention: Lumbar punctures (LP; 10 ml/kg) on 2 days. Cranial ultrasound is repeated daily. If on the third day a LP is still required, a subcutaneous reservoir will be inserted. Daily 10 cc/kg will be drained in 2 taps a day. Punctures from the reservoir will be continued over the next days or weeks. The amount of CSF drained will be increased or decreased in order to reach and keep the ventricular index according to Levene <P97 and diagonal anterior horn width <6 mm. If punctures are still necessary exceeding 28 days after the first LP, a ventriculoperitoneal shunt is inserted. If the bodyweight of the infant is less than 2.5 kg, the insertion of the shunt will be postponed until the bodyweight is over 2.5 kg, if CSF drainage is still needed then. |
| Outcomes | Primary: Need for ventriculoperitoneal shunt Secondary: 1. Neurodevelopmental outcome on the Bayley Scales of Infant Development at 24 months corrected age, assessed by a ‘blinded’ developmental psychologist |
| Starting date | January 27, 2006 |
| Contact information | LS de Vries MD, PhD, [email protected] |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Placement of a hydrocephalus shunt Show forest plot | 3 | 233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.73, 1.26] |
| Analysis 1.1  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 1 Placement of a hydrocephalus shunt. | ||||
| 2 Death prior to 12‐month follow‐up Show forest plot | 4 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.44] |
| Analysis 1.2  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 2 Death prior to 12‐month follow‐up. | ||||
| 3 Major disability in survivors Show forest plot | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.81, 1.18] |
| Analysis 1.3  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 3 Major disability in survivors. | ||||
| 4 Multiple disability in survivors Show forest plot | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.66, 1.24] |
| Analysis 1.4  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 4 Multiple disability in survivors. | ||||
| 5 Death or disability Show forest plot | 2 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| Analysis 1.5  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 5 Death or disability. | ||||
| 6 Death or shunt Show forest plot | 3 | 233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.75, 1.11] |
| Analysis 1.6  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 6 Death or shunt. | ||||
| 7 Infection of CSF presurgery Show forest plot | 2 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.73 [0.53, 5.67] |
| Analysis 1.7  Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 7 Infection of CSF presurgery. | ||||

Study flow diagram: review update
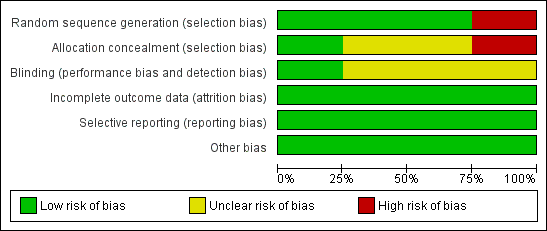
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study

Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 1 Placement of a hydrocephalus shunt.

Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 2 Death prior to 12‐month follow‐up.

Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 3 Major disability in survivors.

Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 4 Multiple disability in survivors.

Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 5 Death or disability.
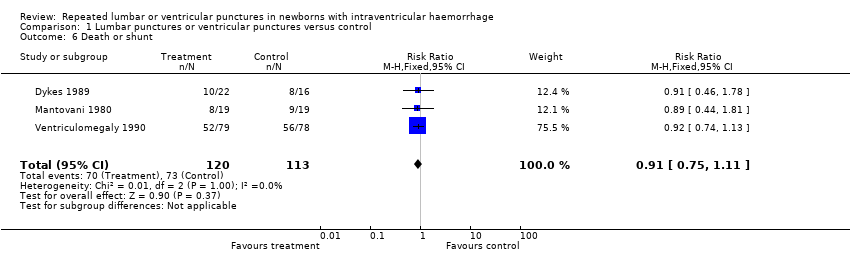
Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 6 Death or shunt.

Comparison 1 Lumbar punctures or ventricular punctures versus control, Outcome 7 Infection of CSF presurgery.
| Repeated lumbar or ventricular punctures compared to conservative management for infants with intraventricular haemorrhage (IVH) | |||||
| Population: preterm infants less than three months of age with either: a) IVH demonstrated by ultrasound or computed tomography (CT) scan; or b) infants with IVH followed by progressive ventricular dilatation. Settings: neonatal intensive care units. Intervention: serial lumbar puncture, ventricular puncture, or tapping from a subcutaneous reservoir. Comparison: conservative management. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants | Quality of the evidence | |
| Risk with conservative treatment | Risk with serial lumbar or ventricular punctures | ||||
| Hydrocephalus shunt | Study population | RR 0.96 | 233 | ⊕⊕⊕⊝ | |
| 469 per 1000 | 450 per 1000 | ||||
| Death | Study population | RR 0.88 | 280 | ⊕⊕⊝⊝ | |
| 199 per 1000 | 175 per 1000 | ||||
| Major disability in survivors | Study population | RR 0.98 | 141 | ⊕⊕⊕⊕ | |
| 761 per 1000 | 746 per 1000 | ||||
| Multiple disability in survivors | Study population | RR 0.90 | 141 | ⊕⊕⊕⊕ | |
| 537 per 1000 | 484 per 1000 | ||||
| Death or disability | Study population | RR 0.99 | 180 | ⊕⊕⊕⊕ | |
| 814 per 1000 | 806 per 1000 | ||||
| Death or shunt | Study population | RR 0.91 | 233 | ⊕⊕⊕⊝ | |
| 646 per 1000 | 588 per 1000 | ||||
| Infection of CSF presurgery | Study population | RR 1.73 | 195 | ⊕⊕⊝⊝ | |
| 43 per 1000 | 74 per 1000 | ||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Downgraded by 1 as Mantovani 1980 used an alternation method for random sequence generation. | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Placement of a hydrocephalus shunt Show forest plot | 3 | 233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.73, 1.26] |
| 2 Death prior to 12‐month follow‐up Show forest plot | 4 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.44] |
| 3 Major disability in survivors Show forest plot | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.81, 1.18] |
| 4 Multiple disability in survivors Show forest plot | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.66, 1.24] |
| 5 Death or disability Show forest plot | 2 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| 6 Death or shunt Show forest plot | 3 | 233 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.75, 1.11] |
| 7 Infection of CSF presurgery Show forest plot | 2 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.73 [0.53, 5.67] |

