Reparación extraabdominal versus intraabdominal de la incisión uterina en la operación cesárea
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial. Randomisation by a table of random numbers, and allocations kept secure in sealed envelopes. Not stated whether or not these were opaque. Analysis by "intention to treat" principle. | |
| Participants | 194 women included. Exclusion of those with placenta previa, placental abruption, chorioamnionitis. | |
| Interventions | 2 groups ‐ uterine exteriorisation = 100 women. In situ repair = 94 women. All received prophylactic antibiotics. Pain relief by patient controlled analgesia ‐ morphine for the first 24‐36 hours, then rectal diclofenac/codeine‐ paracetamol combination PRN. | |
| Outcomes | 1. Hosp. stay. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | "all...were randomly assigned". No details of method of randomisation were given. | |
| Participants | 386 consecutive caesarean sections, in a county hospital. 78 (20%) excluded, as they required extensive surgical manipulations. | |
| Interventions | 2 groups ‐ | |
| Outcomes | 1. Febrile days (excluding first 24 hours, when a temperature of 100.4 F or greater was recorded). 2. Postoperative infection. 3. Postoperative days in hospital. 4. Drop in haematocrit (patients with third trimester bleeding excluded from analysis). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomised prospective study. Four groups of cards prepared from a random number table. | |
| Participants | 100 women having a caesarean section. Women with a bleeding diathesis, abnormal placentation, or prior postpartum haemorrhage were excluded. | |
| Interventions | 4 groups formed: | |
| Outcomes | 1. Blood loss (measured in suction apparatus, drapes, sponges and pads). | |
| Notes | Women recruited to the Magann studies were doubly randomised in trials with factorial design. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Random group assignment by card selection, from sealed opaque envelopes. Group appointment from random number table. | |
| Participants | 120 women undergoing caesarean section. Exclusion of women with chorioamnionitis, those who refused, those who received antenatal steroid/insulin therapy. | |
| Interventions | 4 groups formed: | |
| Outcomes | 1. Infectious morbidity (as gauged by: maternal temp > 38 C on 2 occasions, 6 hours apart, excluding the first 24 hours: uterine tenderness: foul smelling lochia: blood and urine cultures. 2. Duration of operation. | |
| Notes | Women recruited to the Magann studies were doubly randomised in trials with factorial design. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | Computer generated random sequence, sealed in opaque envelopes. | |
| Participants | 284 women undergoing caesarean section. Exclusion of women who refused, chorioamnionitis, history of previous caesarean section without labour. | |
| Interventions | Participants divided into 4 equal groups (71). | |
| Outcomes | 1. Operative blood loss (measured in suction apparatus, surgical drapes and sponges). | |
| Notes | Women recruited to the Magann studies were doubly randomised in trials with factorial design. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomised prospective study. Four groups of cards prepared from a random number table. | |
| Participants | 100 women having a caesarean section. Women with a bleeding diathesis, abnormal placentation, or prior postpartum haemorrhage were excluded. | |
| Interventions | 4 groups formed: | |
| Outcomes | 1. Blood loss (measured in suction apparatus, drapes, sponges and pads). | |
| Notes | Women recruited to the Magann studies were doubly randomised in trials with factorial design. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Random group assignment by card selection, from sealed opaque envelopes. Group appointment from random number table. | |
| Participants | 120 women undergoing caesarean section. Exclusion of women with chorioamnionitis, those who refused, those who received antenatal steroid/insulin therapy. | |
| Interventions | 4 groups formed: | |
| Outcomes | 1. Infectious morbidity (as gauged by: maternal temp > 38 C on 2 occasions, 6 hours apart, excluding the first 24 hours: uterine tenderness: foul smelling lochia: blood and urine cultures. 2. Duration of operation. | |
| Notes | Women recruited to the Magann studies were doubly randomised in trials with factorial design. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Computer generated random sequence, sealed in opaque envelopes. | |
| Participants | 284 women undergoing caesarean section. Exclusion of women who refused, chorioamnionitis, history of previous caesarean section without labour. | |
| Interventions | Participants divided into 4 equal groups (71). | |
| Outcomes | 1. Operative blood loss (measured in suction apparatus, surgical drapes and sponges). | |
| Notes | Women recruited to the Magann studies were doubly randomised in trials with factorial design. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Randomised controlled trial. Randomisation by closed, numbered envelope technique, after anaesthetic technique established. Also, independent randomisation for 3 anaesthetic techniques used. Surgeons and anaesthetists blinded. Analysis by "intention to treat" principle. | |
| Participants | 316 women randomised, although only 288 included in analysis. (? 112 in pilot study, included in interim analysis.) Exclusion: Pre‐/postoperative blood specimens not taken, technical problems with anaesthetic, any change in standard operative procedure. | |
| Interventions | 1. Group 1 (139) Uterine exteriorisation. 2. Group 2 (149) | |
| Outcomes | 1. Peri‐operative drop in Hb. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Hosp: hospital
hr: hour
HVS: high vaginal swab
IV: intravenous
temp: temperature
UTI: urinary tract infection
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| We felt that the methods of uterine repair in this study compared extra‐peritoneal closure, rather than exteriorisation of the uterus, with intra‐peritoneal closure. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative blood loss (ml) Show forest plot | 6 | 504 | Mean Difference (IV, Fixed, 95% CI) | 17.11 [‐23.15, 57.37] |
| Analysis 1.1  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 1 Operative blood loss (ml). | ||||
| 1.1 with manual removal of placenta | 3 | 252 | Mean Difference (IV, Fixed, 95% CI) | 26.75 [‐34.54, 88.05] |
| 1.2 with spontaneous separation of placenta | 3 | 252 | Mean Difference (IV, Fixed, 95% CI) | 9.79 [‐43.59, 63.18] |
| 1.3 placental management not stated | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Postoperative drop in haematocrit Show forest plot | 3 | 324 | Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐1.48, 0.54] |
| Analysis 1.2  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 2 Postoperative drop in haematocrit. | ||||
| 2.1 with manual removal of placenta | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐3.52, 0.52] |
| 2.2 with spontaneous separation of placenta | 1 | 50 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.47, 1.47] |
| 2.3 placental management not stated | 1 | 224 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐0.90, ‐0.70] |
| 3 Postoperative drop in haemoglobin levels (g/dl) Show forest plot | 2 | 482 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.62, 0.65] |
| Analysis 1.3  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 3 Postoperative drop in haemoglobin levels (g/dl). | ||||
| 4 Febrile morbidity for more than 3 days Show forest plot | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.17, 0.97] |
| Analysis 1.4  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 4 Febrile morbidity for more than 3 days. | ||||
| 5 Endometritis Show forest plot | 3 | 592 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.64, 2.60] |
| Analysis 1.5  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 5 Endometritis. | ||||
| 6 Wound complications (infection, haematoma, breakdown) Show forest plot | 3 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.46] |
| Analysis 1.6  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 6 Wound complications (infection, haematoma, breakdown). | ||||
| 7 Nausea/vomiting (intra‐operative) Show forest plot | 3 | 667 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.78, 1.80] |
| Analysis 1.7  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 7 Nausea/vomiting (intra‐operative). | ||||
| 8 Postoperative sepsis Show forest plot | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.19, 4.57] |
| Analysis 1.8  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 8 Postoperative sepsis. | ||||
| 9 Duration of operation Show forest plot | 9 | 1281 | Mean Difference (IV, Random, 95% CI) | 0.82 [‐2.31, 3.95] |
| Analysis 1.9  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 9 Duration of operation. | ||||
| 10 Satisfaction with operation Show forest plot | 1 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.82, 1.04] |
| Analysis 1.10  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 10 Satisfaction with operation. | ||||
| 11 Length of hospital stay (postoperative) Show forest plot | 4 | 766 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.08, 0.39] |
| Analysis 1.11  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 11 Length of hospital stay (postoperative). | ||||
| 12 Pain (intra‐operative) Show forest plot | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.79, 2.27] |
| Analysis 1.12  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 12 Pain (intra‐operative). | ||||
| 13 Failure of procedure Show forest plot | 2 | 405 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.16, 1.28] |
| Analysis 1.13  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 13 Failure of procedure. | ||||
| 14 Patients requiring blood transfusion Show forest plot | 2 | 482 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.43, 3.19] |
| Analysis 1.14  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 14 Patients requiring blood transfusion. | ||||
| 15 Deep vein thrombosis Show forest plot | 1 | 194 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.82 [0.12, 68.42] |
| Analysis 1.15  Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 15 Deep vein thrombosis. | ||||
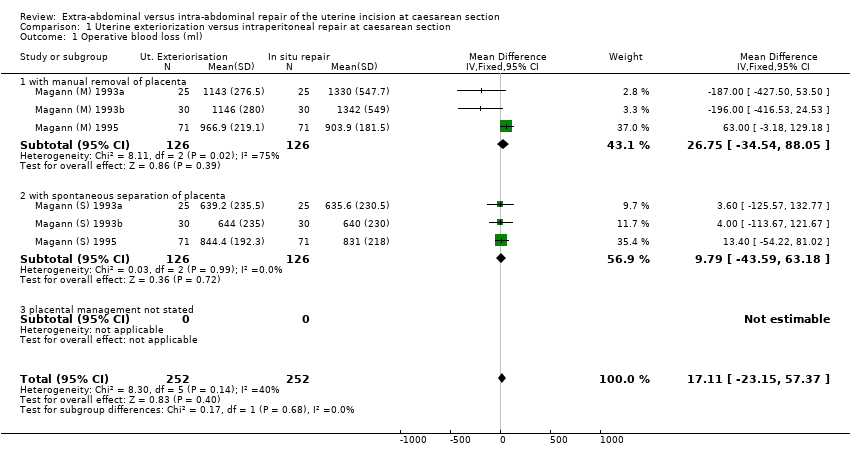
Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 1 Operative blood loss (ml).

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 2 Postoperative drop in haematocrit.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 3 Postoperative drop in haemoglobin levels (g/dl).

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 4 Febrile morbidity for more than 3 days.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 5 Endometritis.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 6 Wound complications (infection, haematoma, breakdown).

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 7 Nausea/vomiting (intra‐operative).

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 8 Postoperative sepsis.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 9 Duration of operation.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 10 Satisfaction with operation.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 11 Length of hospital stay (postoperative).

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 12 Pain (intra‐operative).
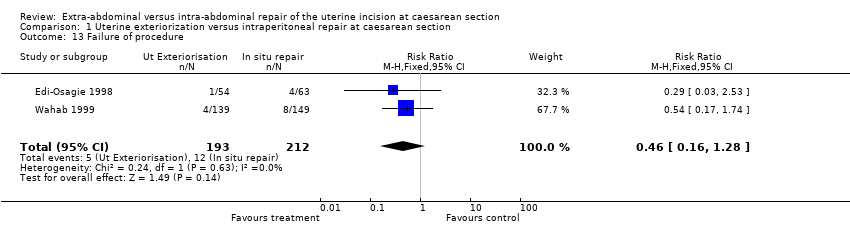
Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 13 Failure of procedure.

Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 14 Patients requiring blood transfusion.
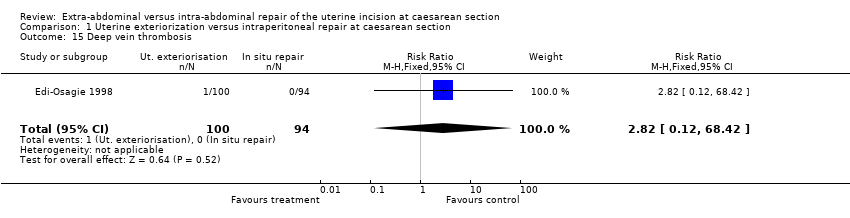
Comparison 1 Uterine exteriorization versus intraperitoneal repair at caesarean section, Outcome 15 Deep vein thrombosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative blood loss (ml) Show forest plot | 6 | 504 | Mean Difference (IV, Fixed, 95% CI) | 17.11 [‐23.15, 57.37] |
| 1.1 with manual removal of placenta | 3 | 252 | Mean Difference (IV, Fixed, 95% CI) | 26.75 [‐34.54, 88.05] |
| 1.2 with spontaneous separation of placenta | 3 | 252 | Mean Difference (IV, Fixed, 95% CI) | 9.79 [‐43.59, 63.18] |
| 1.3 placental management not stated | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Postoperative drop in haematocrit Show forest plot | 3 | 324 | Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐1.48, 0.54] |
| 2.1 with manual removal of placenta | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐3.52, 0.52] |
| 2.2 with spontaneous separation of placenta | 1 | 50 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.47, 1.47] |
| 2.3 placental management not stated | 1 | 224 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐0.90, ‐0.70] |
| 3 Postoperative drop in haemoglobin levels (g/dl) Show forest plot | 2 | 482 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.62, 0.65] |
| 4 Febrile morbidity for more than 3 days Show forest plot | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.17, 0.97] |
| 5 Endometritis Show forest plot | 3 | 592 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.64, 2.60] |
| 6 Wound complications (infection, haematoma, breakdown) Show forest plot | 3 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.46] |
| 7 Nausea/vomiting (intra‐operative) Show forest plot | 3 | 667 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.78, 1.80] |
| 8 Postoperative sepsis Show forest plot | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.19, 4.57] |
| 9 Duration of operation Show forest plot | 9 | 1281 | Mean Difference (IV, Random, 95% CI) | 0.82 [‐2.31, 3.95] |
| 10 Satisfaction with operation Show forest plot | 1 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.82, 1.04] |
| 11 Length of hospital stay (postoperative) Show forest plot | 4 | 766 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.08, 0.39] |
| 12 Pain (intra‐operative) Show forest plot | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.79, 2.27] |
| 13 Failure of procedure Show forest plot | 2 | 405 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.16, 1.28] |
| 14 Patients requiring blood transfusion Show forest plot | 2 | 482 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.43, 3.19] |
| 15 Deep vein thrombosis Show forest plot | 1 | 194 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.82 [0.12, 68.42] |

