口服抗血小板治療急性缺血性中風
Abstract
Background
In people with acute ischaemic stroke, platelets become activated and can cause blood clots to form and block an artery in the brain, resulting in damage to part of the brain. Such damage gives rise to the symptoms of stroke. Antiplatelet therapy might reduce the volume of brain damaged by ischaemia and also reduce the risk of early recurrent ischaemic stroke, thereby reducing the risk of early death and improving long‐term outcomes in survivors. However, antiplatelet therapy might also increase the risk of fatal or disabling intracranial haemorrhage.
Objectives
To assess the efficacy and safety of immediate oral antiplatelet therapy (that is started as soon as possible and no later than two weeks after stroke onset) in people with acute presumed ischaemic stroke.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched 16 October 2013), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library Issue 4, 2013), MEDLINE (June 1998 to May 2013), and EMBASE (June 1998 to May 2013). In 1998, for a previous version of this review, we searched the register of the Antiplatelet Trialists' Collaboration, MedStrategy and contacted relevant drug companies.
Selection criteria
Randomised trials comparing oral antiplatelet therapy (started within 14 days of the stroke) with control in people with definite or presumed ischaemic stroke.
Data collection and analysis
Two review authors independently applied the inclusion criteria and assessed trial quality. For the included trials, they extracted and cross‐checked the data.
Main results
We included eight trials involving 41,483 participants. No new trials have been added since the last update.Two trials testing aspirin 160 mg to 300 mg once daily, started within 48 hours of onset, contributed 98% of the data. The risk of bias was low. The maximum follow‐up was six months. With treatment, there was a significant decrease in death or dependency at the end of follow‐up (odds ratio (OR) 0.95, 95% confidence interval (CI) 0.91 to 0.99). For every 1000 people treated with aspirin, 13 people would avoid death or dependency (number needed to treat 79). Antiplatelet therapy was associated with a small but definite excess of symptomatic intracranial haemorrhages, but this small hazard was significantly outnumbered by the benefit, the reduction in recurrent ischaemic stroke and pulmonary embolus.
Authors' conclusions
Antiplatelet therapy with aspirin 160 mg to 300 mg daily, given orally (or by nasogastric tube or per rectum in people who cannot swallow) and started within 48 hours of onset of presumed ischaemic stroke, reduced the risk of early recurrent ischaemic stroke without a major risk of early haemorrhagic complications; long‐term outcomes were improved.
PICO
淺顯易懂的口語結論
口服抗血小板治療急性缺血性中風
問題
我們想比較口服抗血小板藥物治療與安慰劑或無治療對於急性缺血性中風病人的安全性和有效性,觀察口服抗血小板藥物是否可以減少死亡人數並改善生存者的長期預後。
研究背景
大多數的中風是由於血塊突然堵塞大腦中的動脈引起的 (稱為缺血性中風),立即使用抗血小板藥物(例如aspirin)治療可能會阻止新的血塊形成,從而提高中風後的恢復。但是,抗血小板藥物也可能導致大腦出血,這可能抵消任何益處。
研究特質
我們納入8項研究,檢索截止至2013年10月。這些研究總共包括41,483名受試者,其中兩項研究貢獻了98%的數據。四項研究測試aspirin,三項研究測試了ticlopidine,一項研究測試了aspirin加dipyridamole。該綜述的大多數受試者是老年人,其中很大一部分超過70歲。試驗中男女人數幾乎相等。在納入的試驗中,中風嚴重程度似乎有所不同。計劃的治療時間從五天到三個月不等,計劃的追綜時間從十天到六個月不等。
關鍵結果
在中風症狀發作48小時內開始服用每日160 mg至300 mg 的Aspirin,可挽救生命並降低兩週內發生中風的風險。如果在中風症狀發作48小時後但在14天內開始治療,本綜述提供的有限證據和其他外部資料表明,即使在這個較遲階段開始使用aspirin仍有好處。Aspirin還增加了存活和獨立生活的機會,並增加了中風後完全康復的可能性。嚴重出血的風險非常低。該綜述中幾乎所有的證據都來自aspirin 的試驗。在該綜述中,沒有關於其他口服抗血小板藥物(clopidogrel, ticlopidine, cilostazol, satigrel, sarpolgrelate, KBT 3022, iisbogrel)在治療急性中風方面的可靠證據。
證據品質
導致這些結果的證據品質普遍很好。
Authors' conclusions
Background
Description of the condition
Stroke is an enormous and serious public health problem. According to the World Health Organization, 15 million people suffer stroke worldwide each year. It is also a major cause of death and disability worldwide. Approximately 80% to 87% of all strokes are ischaemic (that is due to a blockage of an artery in the brain) in white populations (Jauch 2013; Warlow 2001) and about 67% in Asian populations (Tsai 2013).
Description of the intervention
Platelets become activated in people with acute ischaemic stroke. This review is focused on oral antiplatelet agents. Oral antiplatelet agents work via different mechanisms to inhibit platelet adhesion and aggregation. The types of drugs include cyclo‐oxygenase inhibitors (for example acetylsalicylic acid (ASA)), thienopyridine derivatives (for example ticlopidine, clopidogrel), phosphodiesterase inhibitors (for example dipyridamole, cilostazol) and thromboxane A2 antagonists (for example ozagrel).
How the intervention might work
Antiplatelet therapy is effective for long‐term secondary prevention of serious vascular events in people at high risk of vascular disease (ATC 1994a; ATC 2002; ATC 2009). In people with acute myocardial infarction, starting antiplatelet therapy immediately after the event, and continuing it for a month, avoids about 38 vascular events for every 1000 people treated (ATC 1994a; ATC 2002). In individuals with ischaemic stroke or transient ischaemic attack (TIA), being on long‐term antiplatelet therapy avoids about 36 serious vascular events for every 1000 people treated for three years (ATC 1994a; ATC 2002). Platelets are activated in the acute phase of ischaemic stroke, releasing neurotoxic and thrombogenic eicosanoids including thromboxane B2 (van Kooten 1994).
Antiplatelet therapy is, therefore, a logical treatment to evaluate in acute ischaemic stroke. It might reduce early deaths and improve outcomes in survivors by reducing the volume of brain damaged by ischaemia and reducing the risk of early recurrent ischaemic stroke and pulmonary embolism (ATC 1994a; ATC 1994b). However, antiplatelet therapy could also increase the risk of fatal or disabling intracranial haemorrhage, thus offsetting any benefits (ATC 1994a). The initial data were sufficiently promising that two large‐scale trials were undertaken, the International Stroke Trial (IST 1997) and the Chinese Acute Stroke Trial (CAST 1997), which together included over 40,000 participants. These trials provided reliable evidence of the net benefit from aspirin in this setting. As a result, evidence‐based guidelines in Europe, Canada and USA now recommend aspirin as the standard antithrombotic treatment for acute ischaemic stroke (CSS 2010; ESO 2008; Jauch 2013; RCP Guideline 2012).
The majority of the data relating to orally active antiplatelet agents is derived from trials of aspirin. Data regarding the utility of other single oral antiplatelet agents, including clopidogrel, dipyridamole or cilostazol, for the treatment of acute stroke are limited (CAIST 2011; Chairangsarit 2005; Suri 2008). Overall, the data do not provide solid evidence about the utility of these antiplatelet agents in the management of people with acute ischaemic stroke. There has been limited experience and no evidence to support the use of ozagrel in the setting of acute stroke (Zhang 2012). Recent trials have investigated the early use of multiple antiplatelet agents in addition to aspirin in the acute phase of stroke. Early initiation of aspirin plus extended‐release dipyridamole seem to be as safe and effective in preventing disability as later initiation after conventional aspirin monotherapy (EARLY 2010). Other trials have examined aspirin and clopidogrel combination therapy. The combination was found to be only significantly effective in the immediate high‐risk interval after stroke or TIA (CHANCE 2013; FASTER 2007;Hankey 2010). Ongoing trials continue to seek alternative regimes in dual or triple antiplatelet therapy (POINT; TARDIS).
Why it is important to do this review
This review is an update of a previously published review in the Cochrane Database of Systematic Reviews (2008, Issue 3) of 'Antiplatelet therapy for acute ischaemic stroke'. The previous version of this Cochrane review was published in 2008 and stated that antiplatelet therapy with aspirin is safe and effective when started within 48 hours after stroke. Since then more trials have been published. For this update we did not include parenterally administrated antiplatelet agents. Platelet glycoprotein (GP) IIb/IIIa receptor inhibitors are the subject of a separate review (Ciccone 2006). Therefore, we conducted this updated review to assess the efficacy and safety of oral antiplatelet therapy when administered to people with acute ischaemic stroke to provide more up‐to‐date evidence for clinical practice and to identify trials of newer agents.
Objectives
To assess the efficacy and safety of immediate oral antiplatelet therapy (that is started as soon as possible and no later than two weeks after stroke onset) in people with acute presumed ischaemic stroke.
We wished to test the hypotheses that oral antiplatelet therapy:
-
reduces the risk of a poor outcome (that is the risk of being dead or dependent on others for activities of daily living) several months after the stroke;
-
reduces the risk of death several months after ischaemic stroke;
-
reduces the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE) following ischaemic stroke;
-
reduces the risk of recurrent ischaemic stroke during the scheduled treatment period;
-
may increase the risk of bleeding, and that the incidence of both intracranial haemorrhage (ICH) and major extracranial haemorrhage may be increased during the scheduled treatment period.
Methods
Criteria for considering studies for this review
Types of studies
We sought to identify all randomised unconfounded trials of early treatment with oral antiplatelet therapy in which treatment allocation was adequately concealed from doctors entering people into the trials. We did not include trials that were not truly random (for example alternating or based on date of birth, day of the week, hospital number) or in which allocation to the treatment or control group was not adequately concealed (such as an open random number list) since foreknowledge of treatment allocation might lead to non‐random treatment allocation and consequent bias in the estimation of treatment effects (Odgaard‐Jensen 2011).
Types of participants
We included all trials that recruited people of any age or sex within two weeks of onset of presumed ischaemic stroke. We excluded trials of antiplatelet therapy after known primary intracerebral or subarachnoid haemorrhage, but included trials that did not adequately differentiate between ischaemic and haemorrhagic stroke by computed tomography (CT) or magnetic resonance (MR) scans prior to randomisation on the basis that 80% to 87% of strokes are ischaemic in predominantly white populations (Jauch 2013; Warlow 2001).
Types of interventions
We considered all unconfounded trials that compared either a single oral antiplatelet agent or a combination of oral antiplatelet agents with control (placebo or no treatment) as eligible. We excluded studies either involving 'head‐to‐head' direct comparisons of one agent versus another or comparison of one multiple agent regimen versus a different multi‐agent regimen (the latter is the subject of a separate review (Kamal 2012)). We broadly defined oral antiplatelet agents as any agents whose principal effects were to inhibit platelet adhesion and aggregation. These included:
-
cyclo‐oxygenase inhibitors (e.g. acetylsalicylic acid (ASA));
-
thienopyridine derivatives inhibiting adenosine diphosphate (ADP) receptors (e.g. ticlopidine, clopidogrel);
-
phosphodiesterase inhibitors (e.g. dipyridamole, cilostazol);
-
thromboxane A2 antagonists (e.g. ozagrel).
For this update we excluded parenterally administrated antiplatelet agents. GP IIb/IIIa receptor inhibitors are the focus of a separate review (Ciccone 2006), which is currently being updated.
We did not include agents with multiple modes of action including some antiplatelet activity (for example piracetam, prostacyclin, oxpentifylline), and some of these agents have been evaluated in other Cochrane systematic reviews (Bath 2004a; Bath 2004b; Ricci 2012).
Types of outcome measures
Primary outcomes
For each treatment group we sought the number of participants who were either dead or dependent on help from other people for their activities of daily living at least one month after their stroke. Many people regard this as the most important outcome since the aim of treatment should not only be to prevent death but also to prevent serious disability in survivors. The minimum interval of one month was used to allow time for recovery from the initial stroke.
Secondary outcomes
For each treatment group we sought the number of participants who:
-
died from any cause during the scheduled treatment period (generally shorter than the scheduled follow‐up period);
-
died from any cause during the scheduled follow‐up period (generally considered to be greater than one month after the stroke);
-
had objective evidence of deep vein thrombosis (DVT) detected by the systematic use of imaging techniques such as iodine 125 fibrinogen scanning (I‐125 scan), ultrasound of the leg, plethysmography, or X‐ray contrast venography in all participants during the scheduled treatment period (these methods detected both clinically suspected and silent DVTs, the outcome was therefore 'symptomatic or asymptomatic DVT'. Screening of participants by clinical observation alone was not considered adequate);
-
had at least one confirmed symptomatic pulmonary embolism (PE) diagnosed during life, or at autopsy (symptomatic or not) within the scheduled treatment period;
-
had a recurrent stroke during the treatment period that was either definitely ischaemic (haemorrhage excluded by CT or MR scan or autopsy) or of unknown type (no CT or MR scan or autopsy performed);
-
had a symptomatic intracranial (intracerebral and extracerebral) haemorrhage, including symptomatic haemorrhagic transformation of the cerebral infarct, during the scheduled treatment period (the haemorrhage must have been confirmed by CT (or MR) scanning after clinical deterioration, or by autopsy);
-
had any recurrent stroke (either of ischaemic or unknown type) or symptomatic intracranial haemorrhage during the treatment period;
-
had any major extracranial haemorrhage during the scheduled treatment period (the definition of major haemorrhage was usually taken from the original article but if none was given it was defined as any fatal bleed, or bleeding severe enough to require transfusion or operation);
-
made a complete recovery from their stroke.
Please note, the last outcome is a post hoc analysis for this outcome only, and we acknowledge that the addition of post hoc data is subject to selection bias. However, at the time we assessed the data for this review we realised that two trials (CAST 1997; IST 1997) reported data on the number of participants who had made a complete recovery from their stroke, an important functional outcome that was not a widely reported outcome in stroke trials when the protocol for the earlier version of this review was written. With the recently reported effects of thrombolysis on increasing the proportion of people who recover completely from their stroke (for example, the NINDS trial of tissue plasminogen activator (NINDS 1995)), it seems reasonable to include this outcome here with due allowance for its post hoc nature.
Search methods for identification of studies
See the 'Specialized register' section in the Cochrane Stroke Group module. We searched for trials in all languages and arranged translation of relevant papers published in languages other than English.
Electronic searches
We searched the Cochrane Stroke Group Trials Register, which was last searched by the Managing Editor in October 2013. In addition, we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2013, Issue 4) (searched May 2013) (Appendix 1), MEDLINE (Ovid) (June 1998 to May 2013) (Appendix 2), and EMBASE (Ovid) (June 1998 to May 2013) (Appendix 3).
We developed the search strategies for CENTRAL, MEDLINE and EMBASE with the help of the Cochrane Stroke Group Trials Search Co‐ordinator and we updated the search strategies to include any new vocabulary terms and drug names.
Searching other resources
In 1998, we searched the registers of the Antiplatelet Trialists' Collaboration (ATC 1994a; ATC 1994b) and MedStrategy (MedStrategy 1995). We contacted the following pharmaceutical companies who marketed antiplatelet agents for details of any trials, particularly unpublished ones: Roussel‐Uclaf (defibrotide), Syntex and Sanofi Winthrop (ticlopidine), Otsuka (cilostazol), Eisai (satigrel), Tokyo Tanebe Seiyaku (sarpolgrelate), Kanebo (KBT 3022), and Takeda Chemical Company (isbogrel). For this version of the review, we did not update the previous searches of the Antiplatelet Trialists' Collaboration register (no longer available), MedStrategy or make any further contact with pharmaceutical companies.
Data collection and analysis
Selection of studies
Two authors (for this update, PS and EC; for previous versions, PS and CC, PS and GG, PS and PF, PS and MT operating in pairs) read the titles, abstracts and keywords of all records identified from the searches of the electronic bibliographic databases and excluded studies that were clearly irrelevant. We obtained the full texts of the remaining studies and the same two authors selected trials for inclusion based on our defined criteria. The two review authors resolved any disagreements by discussion.
Data extraction and management
For each version of the review, two review authors independently extracted the data on methods, participants, interventions, outcomes and results, and recorded the information on a data extraction form. We sought data on the number of participants with each outcome event by allocated treatment group, irrespective of compliance and whether or not the participant was subsequently deemed ineligible or otherwise excluded from treatment or follow‐up, to allow an intention‐to‐treat analysis. We also sought data on whether CT or MR scanning was performed prior to randomisation. The same two review authors cross‐checked all extracted data and resolved any disagreements by discussion. If any of the above data were unavailable from the publications, we sought further information by contacting the study authors.
Assessment of risk of bias in included studies
The same review authors planned to assess the methodological quality of any new trials. We decided not to use a scoring system to assess quality but simply to record details of the following domains: random sequence generation; allocation concealment; blinding of participants, personnel and outcome assessment; incomplete outcome data; and selective outcome reporting. We planned to classify the risk of bias in any new trials as 'low risk', 'high risk' or 'unclear risk' according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion. However, since no new trials were identified we have retained the original assessment of risk of bias.
Measures of treatment effect
We calculated odds ratios (ORs), that is the ratio of the odds of an outcome among treatment‐allocated participants to the corresponding odds amongst controls) with 95% confidence intervals (CI), which we calculated using RevMan 5.2 (RevMan 2012).
Dealing with missing data
If any data were not available from the publications, we sought further information from the authors or the relevant pharmaceutical company. When data were missing and could not be derived, we used the published analysis.
Assessment of heterogeneity
We assessed the extent of heterogeneity between trial results by using the I2 statistic, which measures the percentage of the variability in effect estimates attributable to heterogeneity rather than sampling error (Higgins 2011). We considered a value greater than 50% as substantial heterogeneity.
Assessment of reporting biases
We planned to assess trials for selective outcome reporting and for the assessment of each new trial to be reported in the 'Risk of bias' tables. We sought evidence of publication bias in the assessment of the primary outcome and for death within the scheduled treatment period with funnel plots.
Data synthesis
We calculated ORs with 95% CIs, which were calculated using the Peto fixed‐effect method (ATC 1994a) using RevMan 5.2 (RevMan 2012). We also calculated the number needed to treat to benefit (NNTB) and the number of events avoided per 1000 people treated for each outcome if the result was statistically significant. We performed these calculations with the on‐line calculator provided by the Cochrane Stroke Group at http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp. The control event rate applied was based on the average of the relevant control event rates in CAST 1997 and IST 1997.
Subgroup analysis and investigation of heterogeneity
We pre‐specified the following subgroup analyses for the major outcomes of the review:
-
the type of oral antiplatelet agent used;
-
trials in which all participants had intracerebral haemorrhage excluded by CT or MR scanning prior to trial randomisation;
-
trials in which participants were recruited within 48 hours of their stroke.
We performed an additional post hoc subgroup analysis among participants with intracerebral haemorrhages inadvertently randomised in the trials. Two trials (CAST 1997; IST 1997) included a number of participants who did not have a CT scan until after randomisation. Data on those participants in whom the diagnosis of the initial event leading to randomisation was haemorrhagic stroke and who were dead or dependent at follow‐up were reported in the IST publication (IST 1997) and were kindly supplied on request from the CAST trial (CAST 1997).
We assessed heterogeneity by the I2 statistic.
Sensitivity analysis
We planned several pre‐specified sensitivity analyses limited to the major outcomes (for example death or dependency, death from all causes) of the review, including:
-
only trials with adequate concealment of randomisation;
-
only trials with blinding of participants, personnel and outcome assessment;
-
only trials at low risk of bias due to completeness of follow‐up.
In the sensitivity analysis, we compared two ORs by assessing whether the difference in the natural logarithms of the two ORs (lnOR) was significantly different from zero using a normal approximation. The variance of each lnOR was estimated as the reciprocal of the variance of the O‐E statistic given in RevMan 2012.
However, following an analysis of the available randomised evidence it became apparent that three of the pre‐specified analyses (trials in which participants were randomised within 48 hours, trials with adequate concealment of randomisation and trials with CT scans prior to randomisation) were inappropriate; this is explained in the Results section.
Results
Description of studies
Results of the search
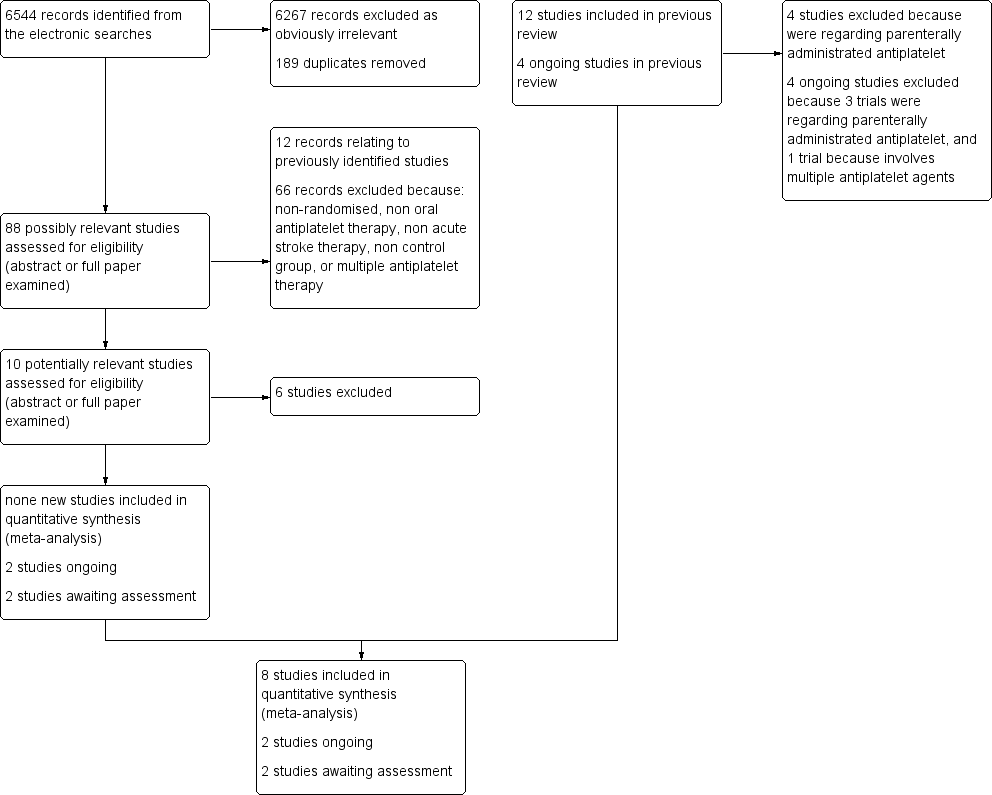
We identified a total of 6544 records from the electronic searches. After eliminating duplicates and non‐relevant studies from the titles and abstracts, we selected 88 possibly relevant studies. After examining the abstracts, or in some cases the full papers, we excluded 78 records: 12 records relating to previously identified studies and 66 records because they were non‐randomised, not of an oral antiplatelet therapy, not acute stroke therapy, had no control group or involved regimens with multiple antiplatelet agents (the latter are reviewed in a separate Cochrane review (Kamal 2012)). This process left 10 potentially relevant studies. Of these, six did not fulfil all the inclusion criteria of this review and are listed in the Characteristics of excluded studies table, two are ongoing (CAIST‐J 2006; CAPS 2009) and two are awaiting assessment (Fujimoto 2010; Wang 2000). Fujimoto 2010 has only been published in abstract form so far and further information is required, particularly regarding the method of randomisation; this study is therefore classified as awaiting classification. So, no new studies fulfilled all the inclusion criteria of this review. We excluded four studies included in the previous review because they assessed only parenterally administrated antiplatelet agents (Abciximab 2000; AbESTT 2005; AbESTT‐II (that contained three study cohorts: AbESTT‐II/P 2008, AbESTT‐II/C 2008, and AbESTT‐II/W 2008); Ohtomo 1991). A PRISMA flowchart of study selection is shown in Figure 1.
Flow diagram.
Included studies
We included eight studies involving a total of 41,483 participants (see Characteristics of included studies). Three of the included trials (162 participants) remain unpublished (Pince 1981; Turpie 1983; Utsumi 1988). The majority of participants in the review were elderly, with a significant proportion of participants over 70 years of age. For example, 61% of participants enrolled in the International Stroke Trial (IST 1997) were aged 70 years or older. Males and females were almost equally represented in the trials.
Antiplatelet regimens tested
Two of the studies (CAST 1997; IST 1997) contributed 98% of the data. IST 1997 was an open‐treatment, blinded outcome study with a factorial design; participants were allocated to 14 days of treatment with 300 mg aspirin, heparin, both, or neither; that is the trial tested the effects of aspirin in the presence and absence of heparin (and vice versa). CAST 1997 was a double‐blind randomised trial of one month's treatment with either aspirin 160 mg or matching placebo. In MAST‐I 1995 (a factorial trial of streptokinase and aspirin involving 309 participants) only those participants randomised to aspirin alone and the no treatment group were included in this review as there was a significant interaction between aspirin and streptokinase which invalidated the aspirin plus streptokinase versus streptokinase alone comparison. Other antiplatelet regimens that were compared with control were: aspirin (Rödén‐Jüllig 2003), ticlopidine (Ciufetti 1990; Turpie 1983; Utsumi 1988), and aspirin plus dipyridamole (Pince 1981).
Time window for inclusion
Trials included participants randomised within six hours (MAST‐I 1995), 12 hours (Ciufetti 1990), 48 hours (CAST 1997; IST 1997), 72 hours (Rödén‐Jüllig 2003) or six days (Pince 1981) of stroke onset. In two trials, the formal entry criterion was a stroke within the previous four weeks (Turpie 1983; Utsumi 1988) but as most participants were entered within two weeks they were included in this review. Data on only those participants entered within two weeks were not available from the authors or the pharmaceutical company.
Exclusion criteria
The two main trials in the review (CAST 1997; IST 1997) did not precisely specify exclusion criteria as they used the uncertainty principle, but suggested that these might include participants thought to be at high risk of adverse effects (for example clotting disorders, hepatic or renal failure) or those with a small likelihood of worthwhile benefit.
CT scanning
Three trials adequately excluded people with intracerebral haemorrhage by CT scanning all possible participants before entry into the trial (Ciufetti 1990; MAST‐I 1995; Rödén‐Jüllig 2003). Two trials (CAST 1997; IST 1997) performed a CT scan in almost all participants; in these trials clinicians had to have a low suspicion of intracranial haemorrhage prior to randomisation. In CAST 1997 87% had a CT prior to randomisation; by discharge this number had risen to 94%. In IST 1997 67% were scanned before randomisation and 29% after randomisation, so that overall 96% of participants were scanned. Two trials performed no CT scans (Pince 1981; Turpie 1983) and in Utsumi 1988 the use of CT scanning was uncertain. As a result of the variable use of pre‐randomisation CT scanning, some people with intracerebral haemorrhage were inadvertently entered in the trials and these were included in the main analyses of this review. This may have biased the results against antiplatelet agents although this is unlikely given the relatively small numbers of participants involved. Furthermore, the inclusion of these people may actually make the conclusions of the review more broadly applicable, since many hospitals admitting people with acute stroke do not have immediate access to CT scanning and so acute treatment may have to be started without definite knowledge of the pathological type of stroke.
Stroke severity at entry
There appeared to be some variation in stroke severity among the included trials. For example, in the control group of IST 1997 early death was recorded as 9%, but was only 4% in CAST 1997, even though CAST 1997 assessed participants at four weeks versus two weeks for IST 1997. Rödén‐Jüllig 2003 used a Scandinavian Stroke Supervision Scale score of one point or more as the inclusion criterion.
Scheduled duration of trial treatment
The scheduled duration of treatment varied from five days (Rödén‐Jüllig 2003) to three months (Utsumi 1988). The scheduled follow‐up period varied from 10 days (Pince 1981) to six months ( IST 1997; MAST‐I 1995).
Measures of outcome
Clinically important outcomes were poorly reported in the smaller trials. All trials evaluated death during the treatment period. Comparable definitions of dependence were used in most of the trials. They included: the modified Rankin disability scale (greater than or equal to three) (CAST 1997; MAST‐I 1995); and needing help from another person with daily activities (IST 1997). For Rödén‐Jüllig 2003 we used 'living in an institution' as equivalent to being dependent. Three trials (CAST 1997; IST 1997; MAST‐I 1995) used validated scales (Bamford 1989; Dennis 1997; Candelise 1994, respectively). In two trials the primary outcome was DVT (Pince 1981; Turpie 1983); these trials did not formally evaluate survival free of dependency for activities of daily living. Progression of stroke symptoms measured by the Scandinavian Stroke Supervision Scale was the primary outcome event of Rödén‐Jüllig 2003. Two trials (CAST 1997; IST 1997) recorded information on participants making a complete recovery from their stroke, and this information has been included in a post hoc analysis as discussed in the Types of outcome measures section of this review. No trials systematically assessed quality of life.
Excluded studies
We excluded 39 trials for a variety of reasons (see Characteristics of excluded studies). In the process of doing this update we excluded four studies that were included in the previous review because they assessed parenterally administrated antiplatelet agents (Abciximab 2000; AbESTT 2005; AbESTT‐II (that contained three study cohorts: AbESTT‐II/P 2008, AbESTT‐II/C 2008, AbESTT‐II/W 2008); Ohtomo 1991). We have now excluded four trials that were ongoing. Of these, we excluded three trials because they were assessing parenterally administrated antiplatelet agents (ARTIS 2012; Cheung 2000; SaTIS 2011), and one trial because it assessed multiple antiplatelet agents (Matsumoto 2005).
Risk of bias in included studies
Baseline characteristics
The large numbers of participants randomised in CAST 1997 and IST 1997 resulted in an equal distribution of baseline patient characteristics between the treatment and control groups. In two smaller trials (MAST‐I 1995; Utsumi 1988) there were significant imbalances between the treatment and control groups in potentially important baseline factors (level of consciousness in Utsumi 1988, and time to treatment in MAST‐I 1995) but these differences cannot bias the overall results due to the small numbers of participants involved.
Allocation
The method of randomisation provided adequate concealment of allocation in five trials (CAST 1997; IST 1997; MAST‐I 1995; Rödén‐Jüllig 2003; Turpie 1983). Sealed envelopes were used in Pince 1981 but it was unclear if the envelopes were opaque. In Ciufetti 1990 a random table was used but it was not clear if this was open to the investigators. The detail of the method of randomisation remains unknown in Utsumi 1988.
Blinding
Five trials used placebo as control (CAST 1997; Ciufetti 1990; Rödén‐Jüllig 2003; Pince 1981; Turpie 1983). Two trials did not use placebo but did use methods to obtain outcome data in a masked fashion (IST 1997; MAST‐I 1995). In IST 1997 the follow‐up data were collected by self‐completed questionnaires mailed to the participants six months after randomisation or by telephone interview by a person blinded to treatment allocation. An analysis of 207 participants from the UK who were enrolled in the IST pilot study showed that at the six month follow‐up the majority of participants could not remember what they had been treated with, and so these participants were effectively blinded (IST 1996). Utsumi 1988 did not appear to use any form of blinded outcome assessment.
Incomplete outcome data
Three trials (Pince 1981; Turpie 1983; Utsumi 1988) excluded a total of 14 participants (seven in the antiplatelet group, seven in the control group) after randomisation. In addition, two trials (CAST 1997; IST 1997) lost a total of 601 participants (300 antiplatelet group, 301 control group) to follow‐up (see Characteristics of included studies). An intention‐to‐treat analysis, which included the results on all participants randomised, was therefore only possible for three trials (Ciufetti 1990; MAST‐I 1995; Rödén‐Jüllig 2003). In the remaining trials we assumed that all participants who were randomised but excluded or lost from follow‐up did not have an outcome event of interest for the primary analyses. Given the very small numbers of participants lost or excluded (1.5% of all participants randomised), the results did not change if these participants were excluded from the denominators.
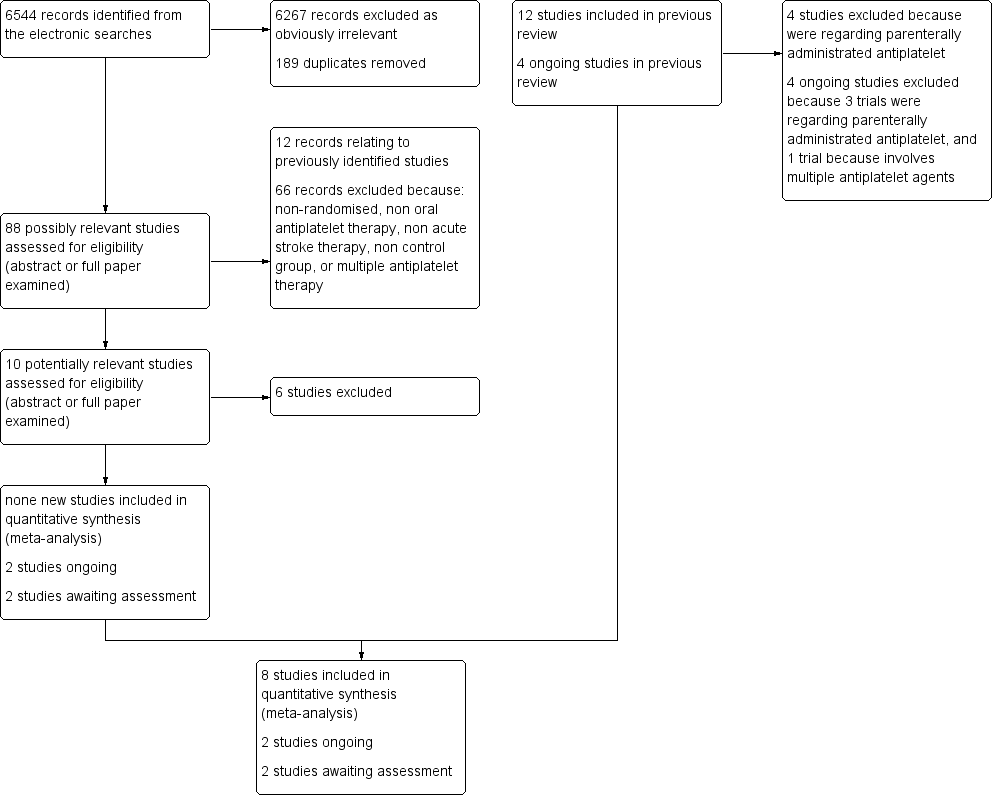
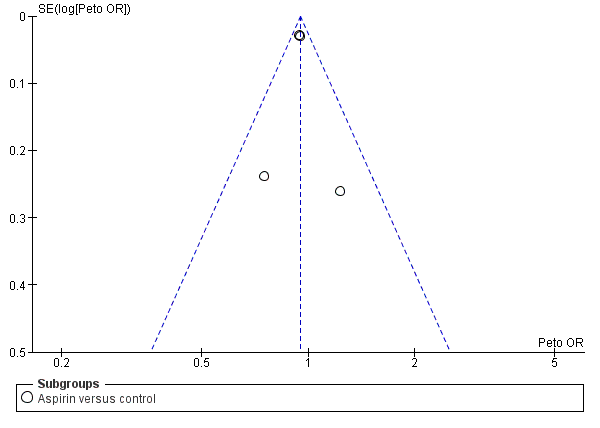
Selective reporting
Funnel plots did not suggest substantial publication bias in respect of the primary outcome (Figure 2) or death at the scheduled end of follow‐up (Figure 3).
Funnel plot of comparison: 1 Antiplatelet agent versus control in acute presumed ischaemic stroke, outcome: 1.1 Death or dependence at end of follow‐up.
Funnel plot of comparison: 1 Antiplatelet agent versus control in acute presumed ischaemic stroke, outcome: 1.2 Deaths from all causes during treatment period.
Effects of interventions
Comparison 1.1: death or dependence at end of follow‐up
Data from four trials with 41,291 participants were available. Antiplatelet therapy was associated with a significant reduction in the odds of being dead or dependent at final follow‐up (OR 0.95, 95% CI 0.91 to 0.99; P = 0.01) (Analysis 1.1). For aspirin, for every 1000 people treated 13 people would avoid death or dependency (NNTB 79) (Table 1). A pre‐specified sensitivity analysis (data not shown in forest plots) showed no statistically significant difference in the effect of treatment on death or dependence at final follow‐up between trials that were double‐blind (OR 0.95, 95% CI 0.90 to 1.01) or not (OR 0.94, 95% CI 0.89 to 1.00). A post hoc subgroup analysis (data not shown in forest plots) restricted to the subset of participants in whom the initial stroke was due to intracerebral haemorrhages and who had been inadvertently randomised in the trials (597 in IST 1997 and 174 in CAST 1997) showed that the odds of a poor outcome were significantly lower among those allocated to aspirin (OR 0.68, 95% CI 0.49 to 0.94), although the CIs were wide (Keir 2002). In CAST 1997 11 participants in the aspirin‐allocated group and five participants in the control group were not accounted for in this analysis. Assuming a worst‐case scenario (that is where all participants in the experimental group were assumed to be either dead or dependent, and all participants in the control group recovered fully), the trend toward a better outcome for the aspirin‐treated group continued but was no longer statistically significant (OR 0.74, 95% CI 0.53 to 1.03) (data not shown in forest plots). Thus, these data do not provide clear evidence of any harm to people with haemorrhagic stroke inadvertently treated with aspirin.
| Outcome | Control event rate | No of events avoided | NNTB or NNTH |
| Per 1000 people treated (95% CI) | Data are number needed to treat to benefit (NNTB) (95% CI) unless otherwise indicated. NNTH = number needed to treat to harm | ||
| Estimated from the average of the control event rate in the 2 largest trials (CAST 1997 and IST 1997) | Estimated by applying the odds ratio for the outcome for studies of aspirin. Calculator is available at: http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp | Estimated by applying the odds ratio for the outcome for studies of aspirin. Calculator is available at: http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp | |
| Death or dependence at end of follow‐up | 0.47 | 13 (3 to 23) | 79 (43 to 400) |
| Deaths from all causes during follow‐up | 0.13 | 9 (2 to 15) | 108 (66 to 436) |
| Pulmonary embolism during treatment period | 0.01 | 1 (0 to 2) | 693 (427 to 6700) |
| Recurrent ischaemic/unknown stroke during treatment period | 0.03 | 7 (4 to 10) | 140 (104 to 248) |
| Symptomatic intracranial haemorrhage during treatment period | 0.01 | ‐2 (i.e. 2 extra) (‐4 to 0) | NNTH 574 (254 to 126 010) |
| Any recurrent stroke/intracranial haemorrhage during treatment | 0.04 | 5 (1 to 8) | 200 (123 to 868) |
| Major extracranial haemorrhage during treatment period | 0.01 | ‐4 (i.e. 4 extra) (‐7 to ‐2) | NNTH 245 (153 to 481) |
| Complete recovery from stroke (post hoc) | 0.26 | 11 (2 to 21) | 89 (49 to 523) |
Comparison 1.2: deaths from all causes during treatment period
Data were available from eight trials with 41,483 participants. Antiplatelet therapy was associated with a nominally significant reduction in death at the end of the treatment period (OR 0.92, 95% CI 0.85 to 1.00; P = 0.05) (Analysis 1.2).
Comparison 1.3: deaths from all causes during follow‐up
Data were available for eight trials including 41,483 participants. Antiplatelet therapy was associated with a significant reduction in the odds of death at a final follow‐up of greater than one month (OR 0.92, 95% CI 0.87 to 0.98; P = 0.01) (Analysis 1.3). For aspirin, for every 1000 people treated nine people would avoid death (NNTB 108) (Table 1). A pre‐specified sensitivity analysis showed no statistically significant difference in the effect of treatment on death at final follow‐up between trials which were of a double‐blind design (OR 0.87, 95% CI 0.76 to 1.00) or not (OR 0.94, 95% CI 0.87 to 1.00).
Comparison 1.4: deep venous thrombosis (DVT) during treatment period
Two trials (Pince 1981; Turpie 1983) that included randomised data from 133 participants (less than 0.3% of participants included in the overall review) sought to systematically determine the effect of antiplatelet agents on the occurrence of 'symptomatic or asymptomatic DVT' at the end of the treatment period, as detected by I‐125 fibrinogen scanning. DVT was observed in 16/67 (23.9%) of those allocated to antiplatelet treatment and 19/66 (28.8%) of those allocated to control, a non‐significant result (OR 0.78, 95% CI 0.36 to 1.67; P = 0.52) (Analysis 1.4). There was substantial heterogeneity between these two trials (I2 = 82.9%), one of which involved ticlopidine and one a combination of aspirin and dipyridamole. This heterogeneity may have been due to chance or to the fact that the time between stroke onset and starting treatment varied in the two trials: less than six days in one (Pince 1981) and less than four weeks in the other (Turpie 1983). Sensitivity analyses were not possible for this outcome due to the limited amount of data.
Comparison 1.5: pulmonary embolism (PE) during treatment period
Data were available from seven trials, including data from 41,042 participants. Importantly, no trial systematically sought asymptomatic PE by performing ventilation‐perfusion scans in all participants at the end of the treatment period. Antiplatelet therapy was associated with a significant reduction in the odds of PE (OR 0.71, 95% CI 0.53 to 0.96; P = 0.03) (Analysis 1.5). For aspirin, for every 1000 people treated one person would avoid PE (NNTB 693) (Table 1). This may be an underestimate if antiplatelet treatment prevented both major and minor PE since minor PE was not sought systematically in any trial. Sensitivity analysis showed no statistically significant difference in this outcome between trials of a double‐blind design (OR 0.60, 95% CI 0.31 to 1.16) or not (OR 0.74, 95% CI 0.53 to 1.04).
Comparison 1.6: recurrent ischaemic or unknown stroke during treatment period
Data on recurrent stroke were available from seven trials with 41,042 participants, which systematically sought to record early recurrent strokes that were definitely ischaemic (CT scan excluded haemorrhage) or probably ischaemic, that is in which the cerebral pathology was unknown because brain imaging had not been performed. A total of 495 of the 551 reported recurrent ischaemic strokes took place in CAST 1997 and IST 1997. The use of antiplatelet agents (chiefly aspirin) was associated with a statistically significant reduction in recurrent ischaemic strokes (OR 0.77, 95% CI 0.69 to 0.87; P < 0.00001) (Analysis 1.6). For every 1000 people treated with aspirin, seven people would avoid recurrent ischaemic stroke (NNTB 140) (Table 1). Sensitivity analysis (data not shown in forest plots) showed no statistically significant difference in this outcome between trials of a double‐blind design (OR 0.85, 95% CI 0.71 to 1.02) or not (OR 0.72, 95% CI 0.62 to 0.85).
Comparison 1.7: symptomatic intracranial haemorrhage during treatment period
Data were available for seven trials including 41,042 participants. It remained unclear (even after correspondence) how haemorrhages were detected in three small trials (Pince 1981; Turpie 1983; Utsumi 1988). However, it was likely that participants who deteriorated neurologically were scanned using CT, or that haemorrhages were found at autopsy. In one trial (Pince 1981) four participants, two in each group, were excluded after randomisation because they were found to have intracerebral haemorrhage. These participants were included as having symptomatic intracranial haemorrhage in this analysis. In the trials where participants did not have a CT scan before randomisation, it was difficult to determine whether any intracranial haemorrhage first identified after treatment had been started was new or had been present before randomisation. For the purposes of this analysis, we assumed that all such haemorrhages were new. Antiplatelet therapy significantly increased the odds of symptomatic intracranial haemorrhage (OR 1.23, 95% CI 1.00 to 1.50; P = 0.04) (Analysis 1.7). For every 1000 people treated with aspirin, two people would have a symptomatic intracranial haemorrhage; the number needed to treat to harm (NNTH) was 574 (Table 1). There was the possibility of some bias within these data as there may have been a lower threshold for re‐scanning participants who had deteriorated clinically if they were known to be receiving antithrombotic treatment (for example in IST 1997, which was not blinded). However, this was not demonstrated in the sensitivity analysis (data not shown in forest plots), which found no statistically significant difference in the effect of treatment on symptomatic intracranial haemorrhage during the treatment period between trials which were of a double‐blind design (OR 1.24, 95% CI 0.95 to 1.63) or not (OR 1.21, 95% CI 0.89 to 1.64).
Comparison 1.8: any recurrent stroke or intracranial haemorrhage during treatment period
Immediate use of antiplatelet agents reduced the odds of ischaemic stroke but also appeared to increase the odds of symptomatic intracranial haemorrhage. An outcome which combines these two (without double counting, that is participant allowed only one of ischaemic stroke or intracranial haemorrhage with the first event being the one which was included) was useful for assessing the net short‐term effects of antiplatelet agents. However, symptomatic intracranial haemorrhages are more likely to cause death or disability than ischaemic recurrences, and so the severity of the recurrence also needed to be considered. No trial reported the severity of recurrences. Data were available from seven trials that included 41,042 participants. Antiplatelet therapy was associated with a net reduction in the odds of this outcome (OR 0.88, 95% CI 0.79 to 0.97; P = 0.01) (Analysis 1.8). For every 1000 people treated with aspirin, five people would avoid recurrent ischaemic stroke or symptomatic intracranial haemorrhage (NNTB 200) (Table 1). Sensitivity analysis showed that although the effect was somewhat smaller in trials of double‐blind design (OR 0.96, 95% CI 0.82 to 1.11) compared with non‐double blind trials (OR 0.81, 95% CI 0.71 to 0.93) the difference (test for interaction) was not significant.
Comparison 1.9: major extracranial haemorrhage during treatment period
Data were available for seven trials including 41,042 participants. Allocation to antiplatelet agents was associated with a significant increase in major extracranial haemorrhage (OR 1.69, 95% CI 1.35 to 2.11; P < 0.00001) (Analysis 1.9). For every 1000 people treated with aspirin, four people would have a symptomatic extracranial haemorrhage (NNTH 245) (Table 1). Sensitivity analysis (data not shown in forest plots) showed no statistically significant difference in this outcome between trials of a double‐blind design (OR 1.48, 95% CI 1.07 to 2.05) or not (OR 1.90, 95% CI 1.40 to 2.57).
Comparison 1.10: complete recovery from stroke (post hoc)
Two trials (CAST 1997; IST 1997) including randomised data on 40,541 participants (98% of participants included in the overall review) reported data on this outcome. Allocation to antiplatelet therapy significantly increased the odds of a complete recovery (OR 1.06, 95% CI 1.01 to 1.11; P = 0.02) (Analysis 1.10). For every 1000 people treated with aspirin, an extra 11 people would make a complete recovery (NNTB 89) (Table 1).
Re‐evaluation of the planned sensitivity and subgroup analyses in light of the available data
After an evaluation of the available evidence from the randomised trials, it became apparent that three of the planned sensitivity analyses were inappropriate. These were the analyses restricted to trials: (1) in which participants were randomised within 48 hours of the stroke; (2) with adequate concealment of randomisation; and (3) with 100% CT scans prior to randomisation. As the overwhelming majority of the data came from trials that randomised participants within 48 hours of stroke onset, the planned sensitivity analysis evaluating the effects of treatment beyond 48 hours was largely uninformative. Similarly, the analyses based on the concealment of treatment allocation were uninformative about trials with inadequate concealment as these trials contributed so few data. An analysis based on whether or not all participants had brain imaging prior to randomisation to rule out haemorrhage would exclude CAST 1997 and IST 1997, and would therefore disregard 98% of the data. An individual patient data analysis has examined the effect subdivided by whether participants had CT prior to randomisation or not; there was no clear heterogeneity of effect (Chen 2000).
Discussion
Strength of evidence of benefit on major outcomes
This systematic review has reliably established that antiplatelet therapy is safe and effective in the acute phase of ischaemic stroke. The conclusion is based on data from over 40,000 participants. Ninety‐eight per cent of the data came from two trials of medium dose aspirin, that is 160 mg to 300 mg daily (CAST 1997; IST 1997). Overall, antiplatelet therapy with aspirin started within 48 hours of onset of presumed ischaemic stroke was beneficial. Although associated with a small but definite risk of bleeding, this hazard was more than offset by the reduction in recurrent ischaemic stroke. The analysis of the effects of aspirin among participants who were first scanned after randomisation and who turned out to have had a haemorrhagic stroke was reassuring.
The benefits of a short course of antiplatelet therapy in acute ischaemic stroke compare very favourably with longer‐term antiplatelet therapy for secondary prevention in vascular disease. Two to four weeks of treatment in IST 1997 and CAST 1997 resulted in about eight fewer deaths per 1000 participants treated, whereas in long‐term secondary prevention a month of antiplatelet therapy typically avoids less than one death per 1000 (ATC 2002). Similarly, long‐term antiplatelet use prevents about one recurrent stroke per 1000 people per month (ATC 1994a; ATC 2002), whereas in the acute phase of ischaemic stroke one month of antiplatelet therapy prevents about four recurrent strokes per 1000 people (seven fewer ischaemic strokes and three extra haemorrhagic strokes).
The main conclusions of this review have not changed from the last update, despite the exclusion of the trials of intravenous antiplatelet agents.
Effects on venous thromboembolism
Aspirin reduced the odds of PE by 29%, but since the reported rate of pulmonary emboli was low the absolute benefit, one event prevented per 1000 participants treated, is very small. However, if there was a substantial under‐ascertainment of pulmonary emboli in the trials included in this systematic review, then the absolute benefits of aspirin may have been underestimated. Clinical series report a range of 0% to 3% for symptomatic PE (Davenport 1996). If the observed 29% reduction in the odds of PE was applied to a population with a 3% risk of pulmonary embolism the absolute reduction would increase to eight for every 1000 people treated. It seems reasonable to conclude that routine use of aspirin alone in people with acute ischaemic stroke will reduce the risk of DVT and PE somewhat yet not be associated with any substantial excess of intracerebral haemorrhages. It remains unclear whether aspirin alone is as good as heparin alone at preventing venous thromboembolism in acute ischaemic stroke, but data from IST 1997 suggest no statistically or clinically significant difference between aspirin and heparin in the prevention of PE.
Robustness of the findings
The sensitivity analyses have shown that the conclusions about the benefits of antiplatelet therapy are robust. A meta‐analysis based on individual patient data from CAST 1997 and IST 1997 confirmed this (Chen 2000). It showed no clear heterogeneity of treatment effect with delay in starting aspirin, age, gender, stroke type, infarct subtype, the presence of impaired consciousness or the presence or absence of atrial fibrillation. These results suggest that a wide variety of people with ischaemic stroke are likely to benefit from antiplatelet therapy with aspirin (Chen 2000). As a result of the strength of evidence, aspirin is now recommended as a standard therapy. Four major recent evidence‐based guidelines make strong recommendations for the routine use of aspirin for all people with acute ischaemic stroke (CSS 2010; ESO 2008; Jauch 2013; RCP Guideline 2012).
Public health impact
It can be argued that, although effective, the net benefits of aspirin are rather small when compared with the effects of stroke unit care (the OR of death or dependency was 0.79, 95% CI 0.68 to 0.90) (SUTC 2013), and thrombolysis with tissue plasminogen activator within three hours of stroke (the OR of death or dependency was 0.71, 95% CI 0.52 to 0.96) (Wardlaw 2009). However, aspirin is inexpensive, easy to administer and safe, which increases its potential public health impact worldwide and especially in developing countries. In a study published in 1997, the World Health Organization estimated that there were 4.6 million cerebrovascular deaths in the world in 1990 (Murray 1997). The global disease burden of stroke increased by 19% between 1990 and 2010 (Murray 2012) and current projections estimate the number of deaths worldwide will rise to 6.5 million in 2015 (Strong 2007). It is reasonable to estimate that about 80% of the deaths (5.2 million) are due to ischaemic stroke. If treatment with aspirin prevents seven deaths per 1000, then an additional 36,400 lives could be saved worldwide per year with substantial numbers of survivors avoiding long‐term disability.
Aspirin dose and route of administration
The benefits of aspirin in acute stroke are drawn from trials that tested a dose of aspirin between 160 mg and 330 mg daily. In acute myocardial infarction, 160 mg is the lowest dose that has been shown to be effective (ATC 1994a; ATC 2002; Dalen 2006; Patrono 1998). Lower doses of aspirin are effective for long‐term secondary stroke prevention but have not been evaluated in acute stroke. There is some (but not abundant) evidence that at least 120 mg of aspirin is needed to acetylate all circulating platelets within a short period of time (Patrono 1994; van Gijn 1992). There is also some experimental evidence that a dose of 160 mg to 300 mg of aspirin daily is required in the acute phase of an ischaemic cerebral or cardiac event in order to achieve rapid inhibition of thromboxane biosynthesis (Patrono 1998; van Kooten 1994; van Kooten 1997). For people who can swallow, aspirin can be given by mouth. However, as many people with stroke are unable to swallow another route may need to be used on occasions. In CAST 1997 aspirin was given via a nasogastric tube, and in IST 1997 as a rectal suppository or intravenously as 100 mg of the lysine salt of acetylsalicylic acid.
Other antiplatelet agents
The indirect comparisons of different agents in this review showed no evidence of significant heterogeneity of effect between the different agents tested, aspirin alone, ticlopidine alone, the combination of aspirin and dipyridamole. However, the data from the non‐aspirin regimens were extremely limited and such indirect comparisons are unreliable (ATC 1994a). The focus of current research is on comparing the effects of short‐term (30 days to three months) combination therapy with single agents, chiefly in people with TIA and minor stroke (CHANCE 2013; POINT; TARDIS); these regimes are the subject of a separate review (Kamal 2012).
Combination of aspirin with anticoagulants
Another question that remains unanswered is whether the addition of low‐dose subcutaneous heparin to aspirin could further reduce the risk of DVT and PE without unduly increasing the risk of intracranial and extracranial haemorrhage. A systematic review of the randomised trials of anticoagulants in acute myocardial infarction showed that the addition of intravenous or subcutaneous heparin did not add worthwhile extra benefit to the use of antiplatelet therapy alone (Collins 1996). However, the addition of low‐dose subcutaneous heparin to aspirin might be more effective in acute stroke. The only trial that provided a direct randomised comparison of aspirin with aspirin plus low‐dose heparin was IST 1997, yet the available data did not provide conclusive evidence that the combination was more effective than aspirin alone. The question of whether or not to add low‐dose heparin to aspirin can, therefore, only be answered reliably by a further, much larger trial that randomly allocates participants to aspirin or aspirin plus low‐dose subcutaneous heparin. Symptomatic PE (and intracranial haemorrhage) are infrequent in people with ischaemic stroke. Therefore, any proposed trial would need to include several 10s of 1000s of participants in order to provide reliable evidence on the size of any difference in the effects of these two antithrombotic regimens.
Time window for benefit from aspirin
There was clear evidence of net benefit when aspirin therapy was started within 48 hours of stroke onset. A more detailed meta‐analysis based on individual patient data from IST 1997 and CAST 1997 showed no clear evidence that the benefit declined with increasing time from stroke onset up to 48 hours (Chen 2000). The evidence on the effects of starting treatment at more that 48 hours and within 14 days of onset was extremely limited in this review. However, taken with the data from the Antithrombotic Trialists Collaboration the evidence is very strongly suggestive that starting after 48 hours but within 14 days of onset and continuing long‐term is highly likely to be of net benefit (ATC 2002).
Interaction with thrombolytic therapy
Thrombolytic therapy for acute ischaemic stroke within 4.5 hours of symptom onset has received regulatory approval (or is recommended in guidelines) in many places, and is the subject of ongoing research. Since antiplatelet and thrombolytic therapy can cause serious bleeding, it is important to assess the evidence for any interaction between the two agents. The subject is dealt with in some detail in the Cochrane systematic review of thrombolytic therapy (Wardlaw 2009). The interaction between thrombolytic drugs and antithrombotic drugs given simultaneously (or the latter very soon after the former) was only tested by random allocation in MAST‐I 1995, which therefore provides the only truly valid evidence. In MAST‐I 1995 there was a clinically important adverse interaction between aspirin and streptokinase when given simultaneously, resulting in a substantial increase in case fatality (early and late), which was not offset by a reduction in the number of dead or dependent participants at the end of follow‐up; 28% of those allocated to streptokinase alone versus 43% of those allocated to streptokinase plus aspirin were dead by the end of follow‐up (P < 0.001), and 62% and 63% were dead or dependent, respectively (versus 68% in the control group). The actual cause of the increase in early and total deaths with streptokinase and aspirin appeared largely to be due to neurological events. Aspirin with streptokinase significantly increased the number of deaths in hospital from all causes (OR 2.2, 95% CI 1.3 to 3.8), neurological causes (OR 2.0, 95% CI 1.1 to 3.7), and intracranial haemorrhage on CT scan or at autopsy (OR 2.2, 95% CI 1.0 to 5.0) when compared with the group who received streptokinase alone. There was no difference in deaths from neurological causes without intracranial haemorrhage, but note that more participants in the streptokinase plus aspirin group died of neurological causes without a CT scan or autopsy so they could also have had an intracranial haemorrhage. That is, the increase in intracranial haemorrhage with aspirin and streptokinase may be even greater. Information is also available on antithrombotic drug use in 12 other trials. There was a trend towards increased case fatality, which was more frequent the nearer to the administration of thrombolysis the concomitant antithrombotic drug use was (OR 1.95 when all participants received antithrombotic drugs within 24 hours of thrombolysis; 1.27 when some participants received antithrombotic drugs within 24 hours; 1.21 when no participants received antithrombotic drugs within 24 hours but some thereafter; and 0.89 for no antithrombotic drugs within the first 10 to 14 days). Although these data are based mainly on non‐randomised comparisons, they do support the evidence of a clinically significant adverse interaction between the concurrent use of thrombolysis and antithrombotic drugs as found in MAST‐I 1995. This is confirmed by the recent ARTIS 2012 trial comparing recombinant tissue plasminogen activator (rTPA) plus intravenous aspirin with rTPA alone.
New developments
The concept of acute stroke (and the differentiation of stroke from TIA) is changing as people with acute cerebral ischaemia are assessed and treated increasingly earlier and more aggressively. The boundary between acute treatment and very early initiation of secondary prevention is becoming blurred, as evidenced by the FASTER 2007, CHANCE 2013, TARDIS and POINT trials. There is clearly a place for further trials of more intensive antiplatelet regimens, started as soon after symptom onset as possible. However, since aspirin will remain the comparator treatment, such trials will need to be even larger than current trials if they are to produce reliable results.
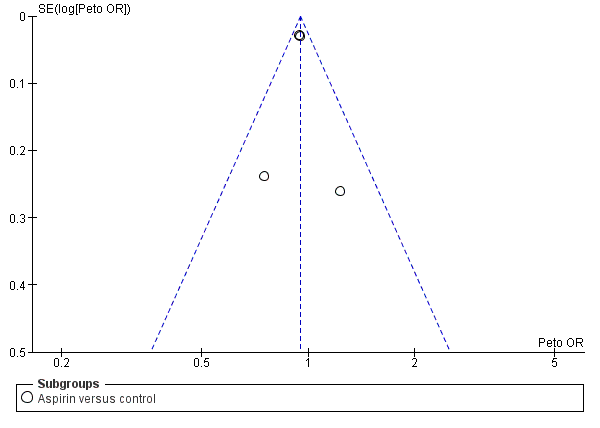
Funnel plot of comparison: 1 Antiplatelet agent versus control in acute presumed ischaemic stroke, outcome: 1.1 Death or dependence at end of follow‐up.

Funnel plot of comparison: 1 Antiplatelet agent versus control in acute presumed ischaemic stroke, outcome: 1.2 Deaths from all causes during treatment period.
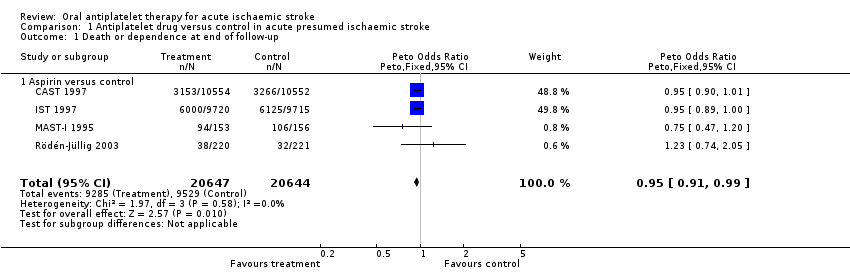
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 1 Death or dependence at end of follow‐up.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 2 Deaths from all causes during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 3 Deaths from all causes during follow‐up.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 4 Deep venous thrombosis during treatment period.
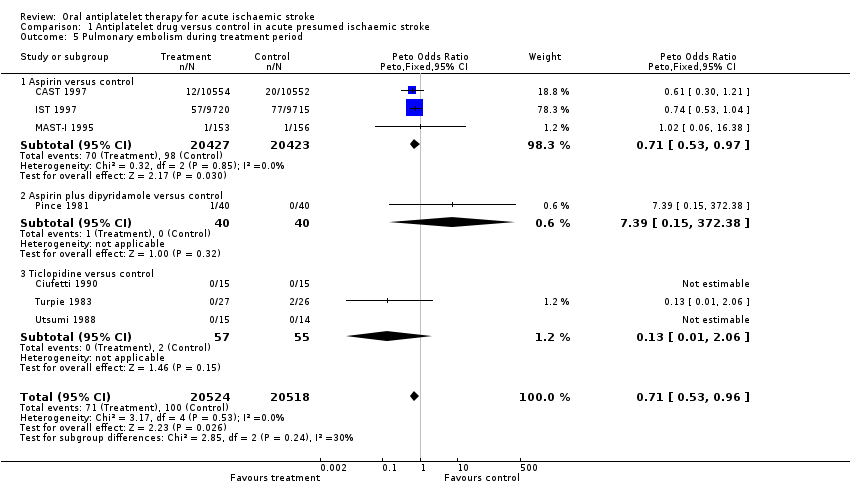
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 5 Pulmonary embolism during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 6 Recurrent ischaemic/unknown stroke during treatment period.
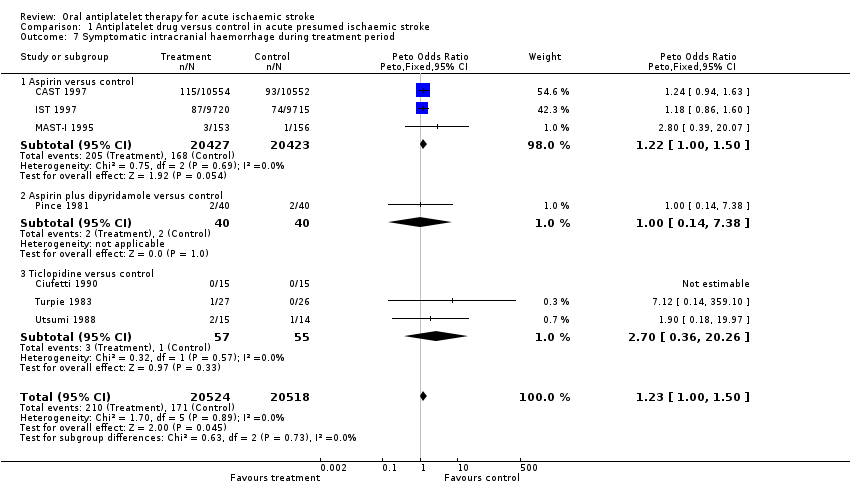
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 7 Symptomatic intracranial haemorrhage during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 8 Any recurrent stroke/intracranial haemorrhage during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 9 Major extracranial haemorrhage during treatment period.
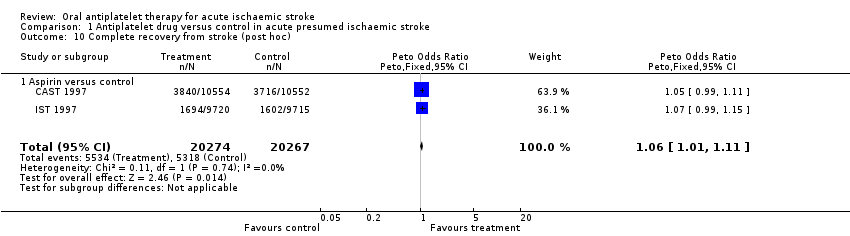
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 10 Complete recovery from stroke (post hoc).
| Outcome | Control event rate | No of events avoided | NNTB or NNTH |
| Per 1000 people treated (95% CI) | Data are number needed to treat to benefit (NNTB) (95% CI) unless otherwise indicated. NNTH = number needed to treat to harm | ||
| Estimated from the average of the control event rate in the 2 largest trials (CAST 1997 and IST 1997) | Estimated by applying the odds ratio for the outcome for studies of aspirin. Calculator is available at: http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp | Estimated by applying the odds ratio for the outcome for studies of aspirin. Calculator is available at: http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp | |
| Death or dependence at end of follow‐up | 0.47 | 13 (3 to 23) | 79 (43 to 400) |
| Deaths from all causes during follow‐up | 0.13 | 9 (2 to 15) | 108 (66 to 436) |
| Pulmonary embolism during treatment period | 0.01 | 1 (0 to 2) | 693 (427 to 6700) |
| Recurrent ischaemic/unknown stroke during treatment period | 0.03 | 7 (4 to 10) | 140 (104 to 248) |
| Symptomatic intracranial haemorrhage during treatment period | 0.01 | ‐2 (i.e. 2 extra) (‐4 to 0) | NNTH 574 (254 to 126 010) |
| Any recurrent stroke/intracranial haemorrhage during treatment | 0.04 | 5 (1 to 8) | 200 (123 to 868) |
| Major extracranial haemorrhage during treatment period | 0.01 | ‐4 (i.e. 4 extra) (‐7 to ‐2) | NNTH 245 (153 to 481) |
| Complete recovery from stroke (post hoc) | 0.26 | 11 (2 to 21) | 89 (49 to 523) |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependence at end of follow‐up Show forest plot | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.91, 0.99] |
| 1.1 Aspirin versus control | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.91, 0.99] |
| 2 Deaths from all causes during treatment period Show forest plot | 8 | 41483 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.85, 1.00] |
| 2.1 Aspirin versus control | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.85, 1.00] |
| 2.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.47 [0.43, 4.99] |
| 2.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.01, 1.20] |
| 3 Deaths from all causes during follow‐up Show forest plot | 8 | 41483 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.87, 0.98] |
| 3.1 Aspirin versus control | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.87, 0.98] |
| 3.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.47 [0.43, 4.99] |
| 3.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.02, 0.88] |
| 4 Deep venous thrombosis during treatment period Show forest plot | 2 | 133 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.36, 1.67] |
| 4.1 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.13, 0.95] |
| 4.2 Ticlopidine versus control | 1 | 53 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [0.72, 7.73] |
| 5 Pulmonary embolism during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.71 [0.53, 0.96] |
| 5.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.71 [0.53, 0.97] |
| 5.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.39 [0.15, 372.38] |
| 5.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.06] |
| 6 Recurrent ischaemic/unknown stroke during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.77 [0.69, 0.87] |
| 6.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.77 [0.69, 0.87] |
| 6.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Symptomatic intracranial haemorrhage during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.23 [1.00, 1.50] |
| 7.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.22 [1.00, 1.50] |
| 7.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.0 [0.14, 7.38] |
| 7.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.70 [0.36, 20.26] |
| 8 Any recurrent stroke/intracranial haemorrhage during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.88 [0.79, 0.97] |
| 8.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.79, 0.97] |
| 8.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.0 [0.14, 7.38] |
| 8.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.70 [0.36, 20.26] |
| 9 Major extracranial haemorrhage during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.69 [1.35, 2.11] |
| 9.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.69 [1.35, 2.11] |
| 9.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Complete recovery from stroke (post hoc) Show forest plot | 2 | 40541 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [1.01, 1.11] |
| 10.1 Aspirin versus control | 2 | 40541 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [1.01, 1.11] |