Provision of respiratory support compared to no respiratory support before cord clamping for preterm infants
Information
- DOI:
- https://doi.org/10.1002/14651858.CD012491.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 08 March 2018see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Neonatal Group
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
All authors contributed to the study design and protocol (Meyer 2017).
MM extracted the data and MW checked the entries.
MM and MW evaluated the quality of evidence according to GRADE, and evaluated the risk of bias.
MM wrote the primary draft of the review and all authors approved the content.
Declarations of interest
Two of the review authors (MM and EN) are investigators for the ABC study (see Characteristics of ongoing studies table).
MW: has no conflict of interest to report.
Acknowledgements
We wish to thank Colleen Ovelman for her help with the search terms and literature search.
We are grateful to the study authors for providing us with unpublished data (Katheria 2016).
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Mar 08 | Provision of respiratory support compared to no respiratory support before cord clamping for preterm infants | Review | Michael P Meyer, Elizabeth Nevill, Maisie M Wong | |
| 2017 Jan 10 | Provision of respiratory support compared to no respiratory support before cord clamping for preterm infants | Protocol | Michael P Meyer, Elizabeth Nevill, Maisie M Wong | |
Differences between protocol and review
The included study presented results for caesarean and vaginal births separately. It was not our intention to have mode of birth as a separate subgroup. Summary results for categorical outcomes could be generated from the original article. Results for continuous variables (e.g. haematocrit and days of phototherapy) were generated from unpublished data made available by the authors.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Umbilical Cord;
- Blood Transfusion [statistics & numerical data];
- Cerebral Intraventricular Hemorrhage [epidemiology];
- Constriction;
- Continuous Positive Airway Pressure [methods, mortality];
- Hematocrit;
- Hospital Mortality;
- Hyperbilirubinemia [therapy];
- Hypotension [therapy];
- Infant, Premature;
- Phototherapy [statistics & numerical data];
- Positive‐Pressure Respiration [*methods, mortality];
Medical Subject Headings Check Words
Humans; Infant, Newborn;
PICOs

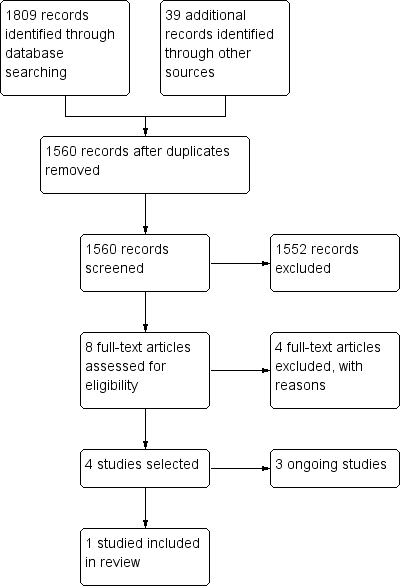
Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.1 Mortality during neonatal admission.

Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.2 Need for intubation in delivery room.

Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.3 Inotropic support for hypotension.
![Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.4 Peak haematocrit in first 24 hours [%].](/cdsr/doi/10.1002/14651858.CD012491.pub2/media/CDSR/CD012491/image_n/nCD012491-AFig-FIG05.png)
Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.4 Peak haematocrit in first 24 hours [%].

Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.5 Blood transfusion during neonatal admission.
![Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.6 Phototherapy for hyperbilirubinaemia [days].](/cdsr/doi/10.1002/14651858.CD012491.pub2/media/CDSR/CD012491/image_n/nCD012491-AFig-FIG07.png)
Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.6 Phototherapy for hyperbilirubinaemia [days].
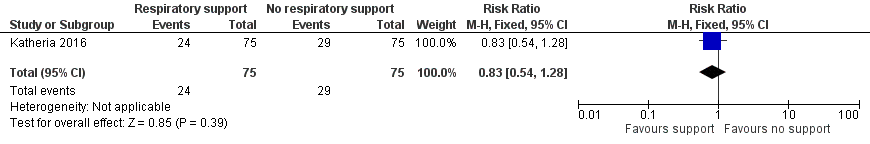
Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.7 Use of surfactant in the first 48 hours of life.
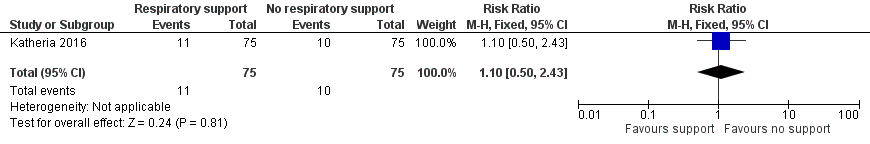
Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.8 Bronchopulmonary dysplasia.
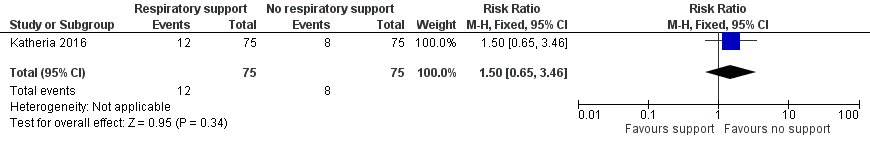
Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.9 Intraventricular haemorrhage (of any grade).

Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.10 Severe intraventricular haemorrhage grade 3 or 4.
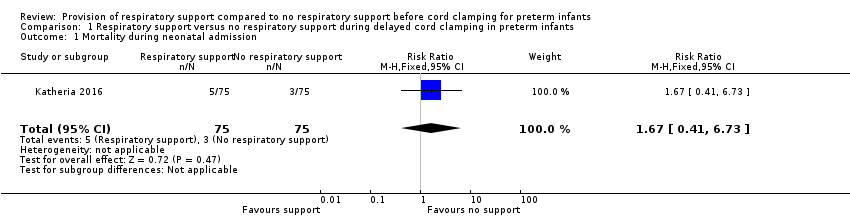
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 1 Mortality during neonatal admission.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 2 Need for intubation in delivery room.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 3 Inotropic support for hypotension.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 4 Peak haematocrit in first 24 hours.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 5 Blood transfusion during neonatal admission.
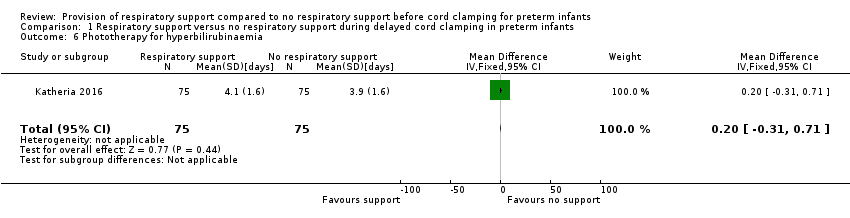
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 6 Phototherapy for hyperbilirubinaemia.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 7 Use of surfactant in the first 48 hours of life.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 8 Bronchopulmonary dysplasia.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 9 Intraventricular haemorrhage (of any grade).

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 10 Severe intraventricular haemorrhage grade 3 or 4.
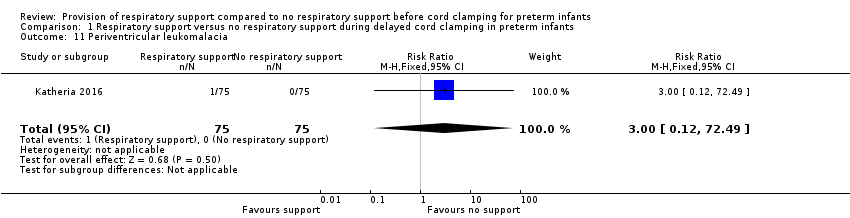
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 11 Periventricular leukomalacia.

Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 12 Necrotizing enterocolitis ≥ Bell's stage 2.
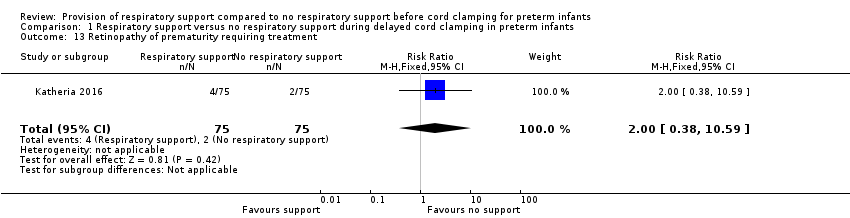
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 13 Retinopathy of prematurity requiring treatment.
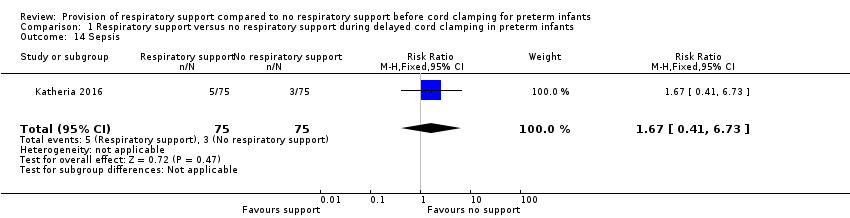
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 14 Sepsis.
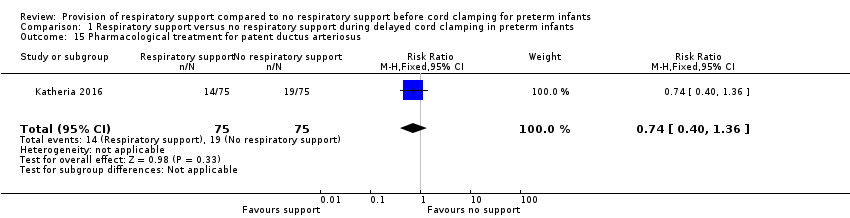
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 15 Pharmacological treatment for patent ductus arteriosus.
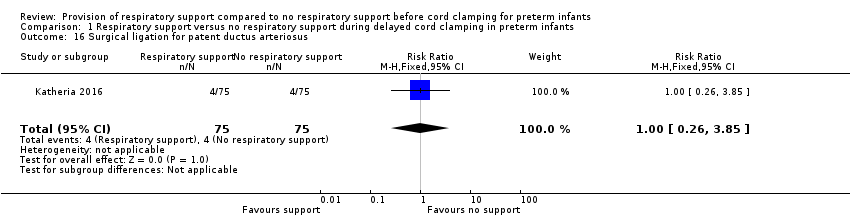
Comparison 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, Outcome 16 Surgical ligation for patent ductus arteriosus.
| Respiratory support compared with no respiratory support before cord clamping in preterm infants | ||||
| Patient or population: preterm infants Settings: undergoing delayed cord clamping Intervention: respiratory support Comparison: no respiratory support | ||||
| Outcomes | Relative effect | No of participants | Quality of the evidence | Comments |
| Mortality ≤2 years after hospital discharge | RR 1.67 (0.41 to 6.73) | 150 | ⊕⊕⊝⊝ | Secondary study outcome. |
| Inotropic support for hypotension | RR 1.25 (0.63 to 2.49) | 150 | ⊕⊕⊝⊝ | ‐ |
| Peak haematocrit | MD 0.20 (‐1.85 to 2.25) | 150 | ⊕⊕⊕⊝ | Primary outcome. |
| Blood transfusion during neonatal admission | RR 1.03 (0.70 to 1.54) | 150 | ⊕⊕⊕⊝ | 40% with this outcome |
| Phototherapy for hyperbilirubinaemia | MD 0.20 (‐0.31 to 0.71) | 150 | ⊕⊕⊕⊝ | From unpublished data |
| Intraventricular haemorrhage (of any grade) | RR 1.50 (0.65 to 3.46) | 150 | ⊕⊕⊝⊝ | Secondary outcome. |
| Severe intraventricular haemorrhage grade 3 or 4 | RR 1.33 (0.31 to 5.75) | 150 | ⊕⊝⊝⊝ | Uncommon secondary outcome. |
| CI: confidence interval; MD: mean difference; RR: risk ratio. | ||||
| GRADE Working Group grades of evidence | ||||
| In the published report, results were presented according to method of delivery. For categorical variables (e.g. mortality), the RR was calculated for the delayed cord clamping with ventilation support (intervention) and delayed cord clamping (control) groups as a whole. For continuous variables (e.g. haematocrit), the authors provided unpublished data that enabled whole group statistics to be determined. 1Downgraded one level due to lack of precision with wide confidence intervals. 2Downgraded two levels due to lack of precision (confidence intervals included both important benefit and harm). The optimal information size for a 30% risk reduction with 80% power and 95% confidence intervals was 3280 infants per group. 3Unpublished data. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality during neonatal admission Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.73] |
| 2 Need for intubation in delivery room Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.55, 1.21] |
| 3 Inotropic support for hypotension Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.63, 2.49] |
| 4 Peak haematocrit in first 24 hours Show forest plot | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐1.85, 2.25] |
| 5 Blood transfusion during neonatal admission Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.70, 1.54] |
| 6 Phototherapy for hyperbilirubinaemia Show forest plot | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.31, 0.71] |
| 7 Use of surfactant in the first 48 hours of life Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.54, 1.28] |
| 8 Bronchopulmonary dysplasia Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.1 [0.50, 2.43] |
| 9 Intraventricular haemorrhage (of any grade) Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.65, 3.46] |
| 10 Severe intraventricular haemorrhage grade 3 or 4 Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.31, 5.75] |
| 11 Periventricular leukomalacia Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.12, 72.49] |
| 12 Necrotizing enterocolitis ≥ Bell's stage 2 Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.59] |
| 13 Retinopathy of prematurity requiring treatment Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.38, 10.59] |
| 14 Sepsis Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.73] |
| 15 Pharmacological treatment for patent ductus arteriosus Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.40, 1.36] |
| 16 Surgical ligation for patent ductus arteriosus Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.26, 3.85] |