Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community‐dwelling populations
Abstract
Background
Excessive alcohol use contributes significantly to physical and psychological illness, injury and death, and a wide array of social harm in all age groups. A proven strategy for reducing excessive alcohol consumption levels is to offer a brief conversation‐based intervention in primary care settings, but more recent technological innovations have enabled people to interact directly via computer, mobile device or smartphone with digital interventions designed to address problem alcohol consumption.
Objectives
To assess the effectiveness and cost‐effectiveness of digital interventions for reducing hazardous and harmful alcohol consumption, alcohol‐related problems, or both, in people living in the community, specifically: (i) Are digital interventions more effective and cost‐effective than no intervention (or minimal input) controls? (ii) Are digital interventions at least equally effective as face‐to‐face brief alcohol interventions? (iii) What are the effective component behaviour change techniques (BCTs) of such interventions and their mechanisms of action? (iv) What theories or models have been used in the development and/or evaluation of the intervention? Secondary objectives were (i) to assess whether outcomes differ between trials where the digital intervention targets participants attending health, social care, education or other community‐based settings and those where it is offered remotely via the internet or mobile phone platforms; (ii) to specify interventions according to their mode of delivery (e.g. functionality features) and assess the impact of mode of delivery on outcomes.
Search methods
We searched CENTRAL, MEDLINE, PsycINFO, CINAHL, ERIC, HTA and Web of Knowledge databases; ClinicalTrials.com and WHO ICTRP trials registers and relevant websites to April 2017. We also checked the reference lists of included trials and relevant systematic reviews.
Selection criteria
We included randomised controlled trials (RCTs) that evaluated the effectiveness of digital interventions compared with no intervention or with face‐to‐face interventions for reducing hazardous or harmful alcohol consumption in people living in the community and reported a measure of alcohol consumption.
Data collection and analysis
We used standard methodological procedures expected by The Cochrane Collaboration.
Main results
We included 57 studies which randomised a total of 34,390 participants. The main sources of bias were from attrition and participant blinding (36% and 21% of studies respectively, high risk of bias). Forty one studies (42 comparisons, 19,241 participants) provided data for the primary meta‐analysis, which demonstrated that participants using a digital intervention drank approximately 23 g alcohol weekly (95% CI 15 to 30) (about 3 UK units) less than participants who received no or minimal interventions at end of follow up (moderate‐quality evidence).
Fifteen studies (16 comparisons, 10,862 participants) demonstrated that participants who engaged with digital interventions had less than one drinking day per month fewer than no intervention controls (moderate‐quality evidence), 15 studies (3587 participants) showed about one binge drinking session less per month in the intervention group compared to no intervention controls (moderate‐quality evidence), and in 15 studies (9791 participants) intervention participants drank one unit per occasion less than no intervention control participants (moderate‐quality evidence).
Only five small studies (390 participants) compared digital and face‐to‐face interventions. There was no difference in alcohol consumption at end of follow up (MD 0.52 g/week, 95% CI ‐24.59 to 25.63; low‐quality evidence). Thus, digital alcohol interventions produced broadly similar outcomes in these studies. No studies reported whether any adverse effects resulted from the interventions.
A median of nine BCTs were used in experimental arms (range = 1 to 22). 'B' is an estimate of effect (MD in quantity of drinking, expressed in g/week) per unit increase in the BCT, and is a way to report whether individual BCTs are linked to the effect of the intervention. The BCTs of goal setting (B ‐43.94, 95% CI ‐78.59 to ‐9.30), problem solving (B ‐48.03, 95% CI ‐77.79 to ‐18.27), information about antecedents (B ‐74.20, 95% CI ‐117.72 to ‐30.68), behaviour substitution (B ‐123.71, 95% CI ‐184.63 to ‐62.80) and credible source (B ‐39.89, 95% CI ‐72.66 to ‐7.11) were significantly associated with reduced alcohol consumption in unadjusted models. In a multivariable model that included BCTs with B > 23 in the unadjusted model, the BCTs of behaviour substitution (B ‐95.12, 95% CI ‐162.90 to ‐27.34), problem solving (B ‐45.92, 95% CI ‐90.97 to ‐0.87), and credible source (B ‐32.09, 95% CI ‐60.64 to ‐3.55) were associated with reduced alcohol consumption.
The most frequently mentioned theories or models in the included studies were Motivational Interviewing Theory (7/20), Transtheoretical Model (6/20) and Social Norms Theory (6/20). Over half of the interventions (n = 21, 51%) made no mention of theory. Only two studies used theory to select participants or tailor the intervention. There was no evidence of an association between reporting theory use and intervention effectiveness.
Authors' conclusions
There is moderate‐quality evidence that digital interventions may lower alcohol consumption, with an average reduction of up to three (UK) standard drinks per week compared to control participants. Substantial heterogeneity and risk of performance and publication bias may mean the reduction was lower. Low‐quality evidence from fewer studies suggested there may be little or no difference in impact on alcohol consumption between digital and face‐to‐face interventions.
The BCTs of behaviour substitution, problem solving and credible source were associated with the effectiveness of digital interventions to reduce alcohol consumption and warrant further investigation in an experimental context.
Reporting of theory use was very limited and often unclear when present. Over half of the interventions made no reference to any theories. Limited reporting of theory use was unrelated to heterogeneity in intervention effectiveness.
PICOs
Plain language summary
Does personalised advice via computer or mobile devices reduce heavy drinking?
Review question
We aimed to find out if personalised advice to reduce heavy drinking provided using a computer or mobile device is better than nothing or printed information. We also compared advice provided using a computer or mobile device to advice given in a face‐to‐face conversation. The main outcome was how much alcohol people drank.
Background
Heavy drinking causes over 60 diseases, as well as many accidents, injuries and early deaths each year. Brief advice or counselling, delivered by doctors or nurses, can help people reduce their drinking by around 4 to 5 units a week. In the UK, this is around two pints (1.13 L) of beer or half a bottle of wine (375 mL) each week. However, people may be embarrassed by talking about alcohol.
Search date
Current to March 2017.
Study characteristics
The studies included people in workplaces, colleges or health clinics and internet users. Everyone typed information about their drinking into a computer or mobile device ‐ which then gave half the people advice about how much they drank and the effect this has on health. This group also received suggestions about how to cut down on drinking. The other group could sometimes read general health information. Between one month and one year later, everyone was asked to confirm how much they were drinking. Drinking levels in both groups were compared to each other at these time points.
Study funding sources
Many (56%) studies were funded by government or research foundation funds. Some (11%) were funded by personal awards such as PhD fellowships. The rest did not report sources of funding.
Key results
We included 57 studies comparing the drinking of people getting advice about alcohol from computers or mobile devices with those who did not after one to 12 months. Of these, 41 studies (42 comparisons, 19,241 participants) focused on the actual amounts that people reported drinking each week. Most people reported drinking less if they received advice about alcohol from a computer or mobile device compared to people who did not get this advice.
Evidence shows that the amount of alcohol people cut down may be about 1.5 pints (800 mL) of beer or a third of a bottle of wine (250 mL) each week. Other measures supported the effectiveness of digital alcohol interventions, although the size of the effect tended to be smaller than for overall alcohol consumption. Positive differences in measures of drinking were seen at 1, 6 and 12 months after the advice.
There was not enough information to help us decide if advice was better from computers, telephones or the internet to reduce risky drinking. We do not know which pieces of advice were the most important to help people reduce problem drinking. However, advice from trusted people such as doctors seemed helpful, as did recommendations that people think about specific ways they could overcome problems that might prevent them from drinking less and suggestions about things to do instead of drinking. We included five studies which compared the drinking of people who got advice from computers or mobile devices with advice from face‐to‐face conversations with doctors or nurses; there may be little or no difference between these to reduce heavy drinking.
No studies reported whether any harm came from the interventions.
Personalised advice using computers or mobile devices may help people reduce heavy drinking better than doing nothing or providing only general health information. Personalised advice through computers or mobile devices may make little or no difference to reduce drinking compared to face‐to‐face conversation.
Quality of the evidence
Evidence was moderate‐to‐low quality.
Authors' conclusions
Summary of findings
| Digital intervention compared to no or minimal intervention for reducing hazardous and harmful alcohol consumption in community‐dwelling populations | ||||||
| Patient or population: People living in the community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no or minimal intervention | Risk with digital intervention | |||||
| Quantity of drinking (g/week), based on longest follow‐up (quantity) | The mean quantity of drinking (g/week), based on longest follow‐up was 176 g/week | MD 23 g/week lower | ‐ | 19,241 | ⊕⊕⊕⊝ | Heterogeneity was substantial (78%) but not unexplained; interventions differed in content and delivery. The direction of effect favoured the intervention in 88% of the studies. |
| Frequency of drinking (number of days drinking/week), based on longest follow‐up (frequency) | The mean frequency of drinking (number of days drinking/week), based on longest follow‐up was 2.5 drinking days/week | MD 0.16 drinking days/week lower | ‐ | 10,862 | ⊕⊕⊕⊝ | |
| Frequency of binge drinking (number of binges/week), based on longest follow‐up | The mean frequency of binge drinking (number of binges/week), based on longest follow‐up was 1.2 binges/week | MD 0.24 binges/week lower | ‐ | 3587 | ⊕⊕⊕⊝ | Heterogeneity was moderate (53%) but not unexplained; interventions differed in content and delivery. The direction of effect favoured the intervention in 93% of the studies. |
| Intensity of drinking (g/drinking day), based on longest follow‐up (intensity) | The mean intensity of drinking (g/drinking day), based on longest follow‐up was 56 g/drinking day | MD 5 g/drinking day lower | ‐ | 9791 | ⊕⊕⊕⊝ | Heterogeneity was substantial (78%) but not unexplained; interventions differed in content and delivery. The direction of effect favoured the intervention in 73% of the studies. |
| Adverse events | Not reported | Not reported | ‐ | ‐ | ‐ | No studies assessed this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded due to high risk of attrition or performance bias or both in many studies. A sensitivity analysis based on the primary meta‐analysis, which omitted studies at high risk of performance bias and contained 11 studies, suggested that the intervention led to a reduction of at least 11 g alcohol (7 to 14 g) or 1.5 UK units (Analysis 1.7). | ||||||
| Digital intervention compared to face‐to‐face intervention for reducing hazardous and harmful alcohol consumption in community‐dwelling populations | ||||||
| Patient or population: People living in the community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with face‐to‐face intervention | Risk with digital intervention | |||||
| Quantity of drinking (g/week), based on longest follow‐up (quantity) follow up: range 1 month to 12 months | The mean quantity of drinking (g/week), based on longest follow‐up was 180 g/week | MD 0.52 g/week higher | ‐ | 390 | ⊕⊕⊝⊝ | |
| Frequency of drinking (number of days drinking/week), based on longest follow‐up (frequency) follow up: range 1 months to 12 months | The mean frequency of drinking (no. of days drinking/week), based on longest follow‐up was 1.85 drinking days/week | MD 0.05 drinking days/week higher | ‐ | 58 | ⊕⊕⊝⊝ | |
| Frequency of binge drinking (number of binges/week), based on longest follow‐up | The mean frequency of binge drinking (no. of binges/week), based on longest follow‐up was 0.7 binges/week | MD 0.04 binges/week higher | ‐ | 206 | ⊕⊕⊝⊝ | |
| Intensity of drinking (g/drinking day) | Not reported | Not reported | ‐ | ‐ | ‐ | No studies assessed this outcome. |
| Adverse events | Not reported | Not reported | ‐ | ‐ | ‐ | No studies assessed this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias (high risk of attrition or performance bias or both). 2 Downgraded one level due to serious imprecision (fewer than 400 participants). | ||||||
Background
Description of the condition
Excessive drinking contributes significantly to physical and psychological illness, injury and death, and a wide array of social harm in all age groups (WHO 2014). Of all deaths worldwide, nearly 6% are attributable to alcohol consumption, and alcohol contributes to over 60 diseases as well as many accidents and injuries. Approximately 5% of the global burden of disease and injury is attributable to alcohol, as measured in disability‐adjusted life years (DALYs).
Alcohol contributes to 20% of deaths due to road traffic accidents, 30% of deaths caused by oesophageal and liver cancers, epilepsy and homicide, and 50% of all deaths caused by liver cirrhosis (WHO 2009). Although drinking limited amounts of alcohol has been reported to decrease the incidence of a small number of diseases and can have a positive social effect, the net effect of alcohol consumption is detrimental to health. The economic cost – including both health and social harms, such as property damage and domestic violence relating to alcohol consumption – tends to amount to more than 1% of gross domestic product in high‐ and middle‐income countries (Rehm 2009).
Excessive drinking can include hazardous, harmful and high‐intensity consumption. People drinking hazardously display a repeated pattern of drinking above recommended limits and are at risk of (but not yet experiencing) physical or psychological harm, whilst those drinking harmfully are drinking above recommended limits and currently experiencing harms (WHO 1992). Hazardous or harmful patterns of alcohol consumption can involve either regular exceeding of consumption guidelines, or high volume consumption which can be regular or infrequent and which is known by a number of terms such as single episode high‐intensity drinking, heavy episodic drinking or often as 'binge' drinking (Herring 2008). There are more people who exhibit hazardous, harmful or high‐intensity drinking than those with alcohol dependence (e.g. McManus 2009 in the UK). At a population level, the greatest impact on alcohol‐related problems can be made by addressing interventions for people who exhibit hazardous, harmful or high‐intensity drinking (McGovern 2013).
Description of the intervention
An evidence‐based strategy for reducing excessive alcohol consumption levels is to offer a brief intervention in primary care settings provided by general practitioners, nurses or other generalist health professionals; this strategy is backed up by findings from 24 systematic reviews and meta‐analyses, encompassing 56 unique trials (O'Donnell 2013). A Cochrane Review incorporating a meta‐analysis of 22 randomised controlled trials (RCTs) found that face‐to‐face brief interventions in primary care settings were consistently effective at reducing excessive drinking, producing an average reduction of 38 g (4 to 5 UK standard drink units) per week (Kaner 2007). These interventions typically comprise a conversation of anywhere between 5 and 45 minutes, include an initial screening process to identify people who are experiencing alcohol‐related risk or harm, provide personalised feedback on alcohol use and harms, identify high‐risk situations for drinking and coping strategies, suggest strategies to increase motivation for positive behaviour change, and develop a personal plan to reduce drinking. This intervention is effective when delivered by a range of health practitioners (Sullivan 2011) and a cost‐effective alcohol risk reduction strategy (Purshouse 2013). Despite clear benefits of face‐to‐face brief alcohol interventions, some heavy drinkers are reluctant to seek help or unable to attend health services, and there are various barriers to delivery from the perspective of health professionals, which results in comparatively low rates of intervention (Brown 2016). Recent technological innovations have enabled people to interact directly via computers, mobile devices or smartphones with digital interventions designed to address problem alcohol consumption using some of the same intervention content (Khadjesari 2011).
How the intervention might work
Digital interventions for alcohol consumption include some of the same features as face‐to‐face interventions to motivate the person to reduce alcohol consumption over time; for example personalised feedback, engaging the person in creating coping strategies and goal‐based plans.
Face‐to‐face brief interventions have generally been found to be effective (Kaner 2007), but various differences should be considered when translating these interventions to a digital medium:
-
Setting: most of the cited evidence on face‐to‐face studies of brief interventions (Kaner 2007) took place in general practice or emergency care‐based primary care, although there is a growing literature on other health settings, such as general hospital wards (McQueen 2011). However, screening for hazardous and harmful alcohol consumption may not occur or be implemented consistently or reliably in busy healthcare settings and may miss people with problems. Barriers to implementation of alcohol interventions (McAvoy 2001) include excessive drinkers not attending primary care settings, and practitioners being too busy to engage in this work (Wilson 2011). Digital interventions have been proposed as a means of accessing hard to reach groups outside health settings, and also to provide a cheaper alternative to interventions delivered by health professionals within health settings (Kaner 2011).
-
Modality: digital interventions differ considerably in their modality or delivery mechanism, which may present advantages and disadvantages. Some people may find disclosing excessive alcohol consumption easier if they feel anonymous, but others may feel that their data confidentiality may be at risk if entered and stored electronically. It is possible that face‐to‐face intervention outcomes may be due, at least in part, to therapist effects; greater outcome effects have been reported for delivery by physicians compared to other practitioners (Sullivan 2011). It is also plausible that a smartphone app which can be used anywhere and at any time at the user’s discretion may produce a different effect to a specific computer sited in a primary care practice, despite the actual content being very similar.
-
Timing: published evidence suggests that alcohol intervention effects may decay over time for face‐to‐face brief interventions (Moyer 2002), which may also apply to digital interventions. Nevertheless, the scope for repeated intervention may potentiate initial effects. Whereas a face‐to‐face intervention is often delivered as a one‐off event (although there can be several sessions), digital interventions may be used as a one‐off or more frequently and regularly over an extended time period.
-
Population: differences in effectiveness may arise for different population groups due to variations in enthusiasm for (e.g. technophilia versus technophobia) or access to technology; for example by age, gender, ethnicity, or socio‐economic status.
Most brief interventions are typically structured according to a FRAMES approach which includes: giving Feedback on the person's intake, impressing the Responsibility for change onto them, offering Advice, listing a Menu of options, having an Empathic approach, and building Self‐efficacy (Miller 1994). However, intervention components are more complex in that they are usually made up of several behaviour change techniques (BCTs) and may incorporate several stages. A BCT is “an observable, replicable, and irreducible component of an intervention designed to alter or redirect causal processes that regulate behaviour" (Michie 2013; Michie 2015).
To identify the ‘active ingredients’ within interventions, it is important to document the component BCTs using a reliable method. For example, an analysis of brief interventions, based on the trials in the Cochrane Review by Kaner 2007 and using a reliable taxonomy of BCTs, identified self‐monitoring as an effective component of these health promoting approaches (Michie 2012).
Economic modelling based on published studies to date has suggested that a programme of face‐to‐face brief interventions rolled out in primary care would be cost‐effective compared to no programme; providing additional health benefits at reduced health service cost (Angus 2014; Purshouse 2013). Little has yet been published on the cost‐effectiveness of digital alcohol interventions, although one study (Blankers 2012) suggested that internet‐based therapy (including a therapist) is more cost‐effective than internet self‐help. A question remains on the relative cost‐effectiveness of digital versus face‐to‐face interventions.
Why it is important to do this review
An overview of reviews (Kaner 2012) identified a large and relatively well‐designed research literature with around 35 published trials in this field around the beginning of the current decade (e.g. Carey 2009a; Khadjesari 2011; Rooke 2010; White 2010). Since this point, the number of trials has increased significantly, and a number of systematic reviews of this evidence base have reported findings often in specific population subgroups. This body of work included the use of technology to deliver alcohol interventions in educational contexts, health and social care settings, and other community‐based settings as well as via the internet or mobile phone applications. In this review we advanced upon previous reviews by taking a public health (secondary) prevention perspective and focusing on people living in the community who were not seeking formal treatment for alcohol‐related problems but nonetheless were drinking at a level which could cause them risk or harm. Participants had to have undergone a screening process to assess drinking behaviour, and risky or harmful drinkers had to engage with any digitally delivered intervention designed to help reduce alcohol consumption. We did not restrict our focus by type of digital intervention so as to capture all interventions targeting this population, and include interventions which take place on multiple platforms (e.g. text prompts to use smartphone apps). We also compared the effect of digital alcohol interventions to face‐to‐face brief alcohol interventions often delivered by health professionals. Health professionals are an established part of public health policy (e.g. UK Government 2012), but practitioners report limited time to screen and deliver alcohol intervention to patients. In addition, some people may be reluctant to disclose heavy alcohol consumption to doctors, nurses or other practitioners. Finally, the digital intervention field is a fast‐moving and rapidly evolving field, so it is crucial to keep the evidence base up to date.
Objectives
The main objective of this review was to assess the effectiveness and cost‐effectiveness of digital interventions for reducing hazardous and harmful alcohol consumption,alcohol‐related problems, or both in people living and recruited from the community. Specifically, we addressed the following questions:
-
Are digital interventions more effective and cost‐effective than no intervention (or minimal input) controls?
-
Are digital interventions at least equally as effective as face‐to‐face brief alcohol interventions?
-
What are the effective component behaviour change techniques (BCTs) of such interventions and their mechanisms of action?
-
What theories or models have been used in the development and/or evaluation of the intervention?
Secondary objectives were as follows:
-
To assess whether outcomes differ between trials where the digital intervention targets participants attending health, social care, education or other community‐based settings and those where it is offered remotely via the internet or mobile phone platforms.
-
To specify interventions according to their mode of delivery (e.g. functionality features) and assess the impact of mode of delivery on outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with individual, cluster, or stepped wedge designs. We did not restrict inclusion by language or publication status.
Types of participants
Participants were people living in the community whose alcohol consumption had been screened as hazardous or harmful (WHO 1992) and who were directed toward any digital intervention including web‐based, mobile phone text messaging, smartphone apps, social networking, or stand alone computer‐based technologies (including CD‐ROMs). Recruitment was via a range of settings, including primary healthcare (including emergency departments and community midwifery services), social care, educational, workplaces or the internet. No restriction was applied to where participants interacted with the intervention, since it could be delivered through mobile devices. We did not restrict to a particular age group because we aimed to assess the effectiveness of digital alcohol interventions for all current drinkers who were likely to experience risk or harm due to alcohol consumption. Although some countries restrict the age at which people can legally purchase alcohol, this does not necessarily mean it is illegal to drink alcohol (except in very young children). As an example, in the UK it is not legally permissible for people under the age of 18 years to purchase alcohol. However, it is legal for these people to drink alcohol provided by family members in their homes; the current UK lower legal age at which alcohol can be consumed under supervision is five years of age (UK Government 2017).
Studies were excluded if:
-
interventions were directed mainly toward people who were seeking specialist health or social care treatment for their alcohol consumption, or who were in treatment for, or recovery from, alcohol dependence (e.g. 12‐step programmes);
-
interventions were directed mainly at primary prevention, i.e. preventing or delaying the onset of alcohol consumption;
-
interventions were delivered in a secondary or tertiary care setting;
-
interventions were delivered to people who were not living freely in the community (e.g. prisoners);
-
interventions were targeted at someone other than the drinker (e.g. at a significant other or someone serving alcohol);
-
participants were under obligation to complete the intervention, or had extra motivation to reduce their drinking, e.g. mandated college students (where low consumption satisfies the mandate) or interventions associated with drink driving. The effect of the mandate to complete the intervention or to reduce consumption would give participants extra motivation compared to those using the intervention freely, which might confound the results; or
-
participants were screened according to their alcohol consumption but it did not have to be hazardous, e.g. participants reported consuming alcohol in the last month.
Types of interventions
Interventions were digital, defined as being delivered primarily through a programmable computer or mobile device (laptop, phone or tablet), and were responsive to user input to generate personalised content which aimed to change the participants’ alcohol‐related behaviours. Interventions were not restricted to those accessible online.
Interventions targeting multiple behaviours (e.g. other substance abuse) or conditions (e.g. depression) were included if all participants were screened into the trial as risky drinkers and alcohol consumption data were reported separately.
For primary objectives 1 and 3 the control condition was no intervention (screening or screening and assessment only), printed or onscreen health or alcohol‐related information, or in a health setting the care the patient would have received anyway for their presenting complaint. For primary objective 2, the control condition was a face‐to‐face brief intervention to reduce alcohol consumption or harm.
Studies were excluded if:
-
the intervention was limited to replicating a real‐time talk‐based intervention (e.g. a conversation by mobile phone). Trials of real‐time interventions which were not talk‐based (e.g. instant messaging), or talk‐based interventions which were not in real time (e.g. on video/DVD/YouTube where replay was available) were included;
-
digital technology was used to screen participants into the study but the advice or behaviour change element was solely face‐to‐face;
-
two digital interventions were compared to each other with no control arm; or
-
the intervention did not generate feedback or other output based on the personal characteristics of the user (e.g. generic educational interventions).
Types of outcome measures
Studies were included if they measured alcohol consumption in grams of alcohol per week (and converted from other measures where possible). We included quantity (g/day), frequency (drinking days/week) and intensity (drinks/drinking day) of consumption in 'Summary of findings' tables. We assessed outcomes on the basis of the behaviour change techniques (BCTs) incorporated in the interventions, their theoretical underpinning, and mechanisms of action as reported elsewhere (Webb 2010).
Primary outcomes
Many types of outcome measures are available in the alcohol literature. Our primary outcome was quantity of alcohol consumed, which we converted into grams of alcohol per week using either definitions in the trial report where available, or from governmental definitions (listed in Kalinowski 2016). We considered trials reporting outcomes at one month or longer post‐intervention, but separated trials according to follow‐up time, as well as by longest follow‐up time.
Secondary outcomes
-
Other measures of consumption (e.g. number of binge episodes, frequency of drinking occasions, number of participants exceeding limits as defined by study authors).
-
Indices of alcohol‐related harm or social problems to the drinkers or affected others.
-
Cost‐effectiveness.
-
Any reported adverse effects.
Search methods for identification of studies
The following sources of information were used to capture studies for the review. The search was not limited by publication status, language or date (some digital interventions, such as CD‐ROMs, were available in the 1980s).
Electronic searches
We used thesaurus headings (such as MeSH headings in MEDLINE), title and abstract terms, and the Cochrane Highly Sensitive Search Strategy for randomised trials: sensitivity‐maximising version (2008 revision) (Lefebvre 2011). The search strategy was designed in MEDLINE on OVID (Appendix 1) and translated as appropriate to other databases searched.
-
MEDLINE (OVID) 1946 to March week 1 2017, searched 15 March 2017 (Appendix 1).
-
PubMed (www.ncbi.nlm.nih.gov/pubmed), searched 29 January 2016.
-
Cochrane Database of Systematic Reviews (CDSR) (Wiley) issue 3 2017, searched 18 March 2017 (Appendix 2).
-
Cochrane Central Register of Controlled Trials (CENTRAL) (Wiley) issue 2 2017, searched 18 March 2017.
-
Database of Abstract of Reviews of Effects (DARE) (Wiley) issue 2 2015, searched 18 March 2017.
-
Health Technology Assessment (HTA) (Wiley) issue 1 2017, searched 18 March 2017.
-
PsycINFO (OVID) 1967 to March week 1 2017, searched 15 March 2017 (Appendix 3).
-
CINAHL (EBSCO) 1981 to March 2017, searched 18 March 2017 (Appendix 4).
-
ERIC (EBSCO) 1966 to March 2017, searched 23 March 2017 (Appendix 5).
-
SCI Science Citation Index (Web of Knowledge) 1970 to March 2017, searched 23 March 2017 (Appendix 6).
-
CPCI‐S Conference Proceeding (Web of Knowledge) 1990 to March 2017, searched 23 March 2017 (Appendix 6).
-
International Alcohol Information Database (ICAP) www.drinksresearch.org, searched 16 January 2015 (unavailable when running update March 2017).
-
Index to Theses www.theses.com searched 15 April 2014.
-
British Library EThOS ethos.bl.uk searched 25 March 2017.
-
Clinicaltrials.gov searched 25 March 2017.
-
WHO International Clinical Trials Registry Platform (ICTRP) www.who.int/ictrp/en searched 25 March 2017.
-
Google Scholar searched 25 March 2017.
We searched the following websites for evaluations of digital interventions:
-
Beacon 2.0 beacon.anu.edu.au
-
Substance Abuse and Mental Health Services Administration (SAMHSA) NREPP (National Registry of Evidence‐based Programs and Practices) nrepp.samhsa.gov/Index.aspx
-
Drug and Alcohol Findings findings.org.uk.
Searching other resources
We checked the reference lists of all included studies and relevant reviews.
Data collection and analysis
Selection of studies
Two review authors independently screened all titles and abstracts identified from the search, using EndNote version X7 (Endnote 2014) to ensure consistency in screening approach. The full text of any studies identified as being potentially eligible for inclusion were assessed by two review authors independently. Any discrepancies were resolved by consulting a third review author.
Data extraction and management
Separate data extraction forms were developed and piloted in MS Excel for outcome extraction, BCT coding and theory coding. These were used by two independent review authors to extract data from all included studies (8 review authors extracted outcomes data and 2 review authors extracted theory and BCT data). Any discrepancies were resolved by consulting a third review author.
Outcome data
Outcome data were extracted as follows: details of the intervention (e.g. setting, duration, mode of delivery and costs), participants (size and characteristics of sample), trial design (to enable critical appraisal), and baseline and follow‐up consumption data (all reported follow‐up points).
Behaviour change techniques (BCT) data
All studies were coded for BCTs using a taxonomy of 93 distinct BCTs (BCTTv1) developed by consensus methods with input from a large group of international behaviour change experts (Michie 2015; Michie 2013). Intervention descriptions were read line‐by‐line, text that may indicate the presence of a BCT was highlighted, and highlighted text was compared to the definition for the BCT given in the taxonomy (Michie 2013). A BCT was coded as included only when it was explicitly present.
The reliability of the method was developed and assessed in iterative rounds of coding. Two review authors independently coded a sample of five studies. Coding differences were resolved through discussion and the coding manual was reviewed and updated in the light of these discussions. If agreement could not be reached, the views of a behaviour change expert were sought. Inter‐rater reliability (IRR) was assessed with both the Kappa and prevalence‐adjusted bias‐adjusted Kappa (PABAK) statistics. Cohen’s Kappa accounts for coders agreeing on the presence of codes (Landis 1977). PABAK is an adjusted Kappa statistic that accounts for coders agreeing on the presence and the absence of codes (Byrt 1993). Whilst it is important to measure levels of agreement about the absence of BCTs, using PABAK alone could result in the reporting of exaggerated levels of agreement when coding against a taxonomy of 93 BCTs, most of which were unlikely to be used in any one intervention (Direito 2014; Dombrowski 2012). Therefore, IRR was assessed with both statistics. The first round of joint coding lead to an IRR of Kappa = 0.73, PABAK = 0.95, which reflects a substantial level of agreement (Landis 1977). As this exceeded the pre‐determined threshold of Kappa = 0.70, remaining studies were coded by one review author, with the second coding 22% (8/36) of the same studies to ensure against rater drift. The IRR for all included studies that were also joint coded was Kappa = 0.73, PABAK = 0.96, n = 13 (for all joint‐coded studies prior to exclusion: Kappa = 0.70, PABAK = 0.95, n = 38/90).
Theory data
The extent to which a theory or model of behaviour was used in the development or evaluation of the intervention was investigated with the 19‐item Theory Coding Scheme (Michie 2010). Two review authors independently coded a sample of five studies and differences were resolved through discussion. The coding guidelines were amended in accordance with these discussions. If agreement was not reached, the views of a behaviour change expert were sought. IRR was assessed with the PABAK statistic as described previously (Byrt 1993). Further rounds of testing were performed until the IRR reached a substantial level of agreement (≥ 0.70; Landis 1977). After this level of agreement was achieved, the remaining studies were coded by one review author. The PABAK statistic across the five rounds of IRR checking was 0.84 which reflects a substantial level of agreement. The Theory Coding Scheme has 19 items; two of these items (quality of measures and randomisation of participants to condition) were not evaluated in this Cochrane Review because they relate to methodological issues rather than informing whether or how theory was used in an intervention. Of the 17 items coded, three had sub‐items (12a, 12b, 14a, 14b, 14c, 14d, 17a, 17b). If a theory or model of behaviour was mentioned (item 1), then the relevant name was documented. Each of the 22 items and sub‐items were dummy coded as present (1) or absent (0). If a protocol or other paper was referenced as describing the intervention, then that paper was also coded for use of theory, although only for items 1 to 11 which relate to the development of the intervention rather than the evaluation.
The Theory Coding Scheme specifies theory use in six categories (Michie 2010); reference to underpinning theory (items 1 to 3); whether any relevant theoretical constructs are targeted by the intervention (items 2, 5, and 7 to 11); whether theory was used to select recipients or tailor interventions (items 4 and 6); measurement of constructs (items 12a and 12b); whether mediation effects were tested (items 12a and 12b, 13, 14a to 14d, 15, 16); whether the results of the study were used to refine theory (items 17a and 17b). Composite scores were calculated for these six areas of theory use. A total use of theory score (sum of all items) was also calculated. These composite scores were used as a crude estimate of the extent of theory use in specific areas, or in total, as a basis of assessing the relationship between that and the effect size of the intervention.
There were two pairs of items (items 7 and 8; items 10 and 11) in the Theory Coding Scheme that refer to “all” and “at least one”, respectively. For the composite scores of theory use, if the all items (7 and 10) were coded as 1 then the at least one item was also coded as 1 (as in Webb 2010). This was to ensure that the composite scores of theory use were representative of the studies and that studies credited with linking all theoretical constructs (for example) are also credited as linking some. Otherwise, linking one theoretical construct would give the same contribution toward the use of theory score as would linking all the constructs.
Assessment of risk of bias in included studies
Risk of bias was assessed independently by two review authors using the criteria recommended in the Cochrane Handbook (Higgins 2011). The recommended approach for assessing risk of bias in studies included in Cochrane Reviews is a two‐part tool, addressing seven specific domains: sequence generation and allocation concealment (selection bias), blinding of participants and providers (performance bias), blinding of outcome assessor (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other sources of bias. The first part of the tool involves describing what was reported to have happened in the study. The second part of the tool involves assigning a judgement relating to the risk of bias for that entry, in terms of low, high or unclear risk. To make these judgments we used the criteria indicated by the Handbook adapted to the addiction field (see Appendix 7 for details).
'Risk of bias' assessments were used to carry out sensitivity analyses (see Sensitivity analysis).
Measures of treatment effect
Consumption outcomes
For continuous variable outcomes (e.g. quantity of alcohol consumed) we examined mean differences (MD) with the uncertainty in each result being expressed with a 95% confidence interval (CI), and for dichotomous outcomes (e.g. participants classified as binge drinker, or drinking over set limits) we examined proportions using relative risks (RR) with 95% CI. Where outcomes had been assessed at more than one time, data for each time point were extracted. The primary analyses focused on the longest follow‐up time.
Unit of analysis issues
It had been planned that for trials with more than one – and very similar – control arms, the results for these arms would be combined in the meta‐analysis. However, this was not required since, as described in the Results section, there was only one relevant control arm for each trial included in the meta‐analysis. The same approach was planned for very similar intervention arms. However, it was not used, since for trials with more than one relevant intervention arm, the results for each arm were analysed separately because the interventions were substantively different from each other so it was not appropriate to combine them (Collins 2014 (DBF); Collins 2014 (PNF)).
Cluster randomised trials were eligible for inclusion in the meta‐analysis. If the analysis in a trial reported a standard error for the intervention effect that accounted for the cluster design, then, so data could be presented and analysed in the same manner as for non‐cluster trials, we assigned imputed standard deviations to the intervention and control groups such that the standard error of the intervention effect calculated by the weighted mean difference method in Review Manager 2014 was the same as the reported standard error. If the analysis in a trial report did not account for the cluster design, we had planned to add an external estimate of the intra‐cluster coefficient (ICC) to estimate a design effect, thus inflating the variance of the effect estimate. However, this situation did not occur in the trials included in the meta‐analysis.
Dealing with missing data
We contacted study authors to obtain missing data and seek clarification where appropriate. Where this was impossible, we estimated primary outcome measures using secondary outcome measures; for example, we estimated quantity of alcohol consumed using frequency and intensity of consumption, although it was not possible to estimate the associated standard deviation. Trials with missing standard deviations or for which the number of participants in each arm was not reported were excluded from the main analysis for the associated continuous measure, but were included in a sensitivity analysis, using imputed values for the standard deviations or the number of participants in each arm.
Assessment of heterogeneity
The magnitude of heterogeneity was assessed using the I² statistic, and the statistical significance of the heterogeneity was assessed using P values derived from Chi² tests (Deeks 2001). The cut‐off points were I² value of more than 50% and a P value for the Chi² test of less than 0.1. Heterogeneity was explored both narratively and using subgroup and sensitivity analyses. The trials were heterogeneous, due not only to the variation in delivery methods (e.g. web, app, CD‐ROM) but also to aspects of content (e.g. focus on feedback versus behaviour change, duration of exposure).
Assessment of reporting biases
We assessed whether studies appeared to have incomplete reporting bias by noting in the risk of bias assessments whether the reported outcomes matched methods sections or any published protocols. We made every effort to minimise publication bias by searching a wide range of databases and sources of grey literature and not restricting by language or publication status, but we used funnel plots to assess the potential for bias related to the size of the trials when there were at least 10 studies included in the meta‐analysis. Funnel plots and associated approximate (pseudo) 95% confidence limits were calculated using the meta‐funnel option in Stata version 14 (Stata 2015).
Data synthesis
We pooled data for each outcome using a random‐effects model in a meta‐analysis that compared intervention and control arms using Review Manager 2014. For continuous measurements, the weighted mean difference was calculated to estimate pooled effect sizes and 95% CIs. If means or standard deviations at follow‐up were not available, change scores were used instead on the proviso that their standard deviations were available. If the median and inter‐quartile range were reported in place of the mean and standard deviation, then the mean and standard deviation were estimated from the inter‐quartile range. If only the mean difference and its 95% CI were reported (e.g. as in Hansen 2012), then data were entered into Review Manager 2014 so that the reported values for the mean difference and CI were included in the meta‐analysis. For dichotomous outcomes, relative risks and 95% CIs were calculated and pooled in a meta‐analysis using Mantel‐Haenzel weighting.
Where possible, we had planned to consider key population groups such as men versus women, older versus younger participants, and different socio‐economic groups. However, the opportunity for analyses of these types was limited by the availability of relevant data.
We planned to estimate long‐term cost‐effectiveness of strategies for the use of internet, mobile phone text messaging, smart phone app interventions or computer‐based technologies by adapting the current Sheffield Alcohol Policy Model (SAPM) analysis of screening and brief interventions, but we found insufficient data. Instead, we included a summary review of the available studies with economic findings.
Behaviour change technique (BCT) analysis
The revised metareg command in Stata version 14 (Stata 2015) was used to conduct a series of random‐effects unadjusted meta‐regression models to assess the associations between individual BCTs and effect size. The regression coefficients (B) represented an estimate of effect (mean difference (MD) in quantity of drinking, expressed in grams per week) per unit increase in the covariate (dummy‐coded as 1 = used the BCT or 0 = did not use the BCT). Only BCTs uniquely present in experimental arms, i.e. not present in both experimental and control arms, were included in analyses. A negative coefficient for a BCT indicated that studies using that BCT produced a larger pooled effect than studies that did not. The approach used in a previous meta‐regression study of the BCTs contained within physical activity and healthy eating interventions was adopted (Michie 2009); to be included in analysis, each BCT needed to be used in at least four separate studies.
To assess the independent association after mutual adjustment, we created a multivariable meta‐regression model including all BCTs that had a meaningful association with effect in the unadjusted models. A meaningful association was defined a priori as B < ‐23, which in absolute terms was the lower confidence interval of the effect size reported in a meta‐analysis of the effect of brief advice on alcohol consumption (Kaner 2007). The lower confidence interval of the previous Cochrane Review by Kaner 2007 was chosen to enable comparisons between the effectiveness of face‐to‐face and digital interventions. The size and significance of the associations in the multivariable model were regarded as providing the primary indication of association between BCTs and effect.
To assess the association between the total number of BCTs included in experimental arms and effect size we created a random‐effects unadjusted meta‐regression model. Lastly, we assessed the overall fit of a model, in terms of adjusted R², containing only a theoretically derived cluster of Control Theory congruent BCTs. These BCTs were grouped into four categories: Goals (goal setting (behaviour), goal setting (outcome), review behaviour goal(s), review outcome goal(s), discrepancy between current behaviour and goal)); self‐monitoring (self‐monitoring of behaviour, self‐monitoring of outcome(s) of behaviour, monitoring of emotional consequences); feedback (feedback on behaviour, feedback on outcome(s) of behaviour, biofeedback) and action plans (action planning). Trials were dummy‐coded as 1 = used BCTs from three or four of these groupings; or 0 = used BCTs from two or less of these groupings.
Theory analysis
Frequency counts and descriptive statistics were used to describe the theoretical basis for digital interventions of alcohol reduction. The range and frequency of theories used were tabulated.
A series of random‐effects unadjusted meta‐regression analyses were conducted to examine the association between the Theory Coding Scheme covariates (individual theory items, required to be included by at least 10% of studies; categories of theory use; and total theory use), with intervention effectiveness and the percentage of the between‐study heterogeneity (adjusted R²) explained by each predictor.
The meta‐regression analyses were conducted in Stata version 14 (Stata 2015) using the metareg command. Effect sizes were based on a random‐effects model because the intervention effects were likely to have residual heterogeneity not modelled by the covariates. The effectiveness of the intervention was measured using the primary outcome measure of difference in quantity of alcohol consumption (g of ethanol) per week between the digital intervention and control arms at the longest follow‐up time point. The weighted mean difference was calculated to estimate pooled effect sizes and 95% CIs.
In these analyses, the regression coefficient (B) represented an estimate of effect (mean difference in quantity of alcohol consumption, g/week) per unit increase in the covariate. A negative coefficient for a covariate indicated that studies reporting that theory item, or with higher scores on the categories of theory use and total theory use, were associated with a larger reduction in consumption than studies that did not. The P value indicated whether the B weight was statistically significantly different from zero, based on a two‐sided test. The adjusted R² value indicates the proportion of between‐study variance explained by each predictor.
To investigate the independent associations, an adjusted meta‐regression analysis was conducted, including all of the variables that had a meaningful association with effect in the unadjusted models. As before, a meaningful association was defined as B < ‐23 as for the BCT models.
Subgroup analysis and investigation of heterogeneity
Subgroup analyses were carried out based on:
-
Timing of outcomes: to investigate possible decay over time, based on a pragmatic grouping of trials according to the follow‐up time points reported.
-
Component BCTs (Michie 2013) as a comparison for face‐to‐face brief interventions.
-
Theoretical basis of the interventions.
-
Key population subgroups: by age (adolescents and young adults) and gender.
We also planned to carry out a subgroup analysis based on socio‐economic status but insufficient information was reported in the included trials.
We planned to undertake a subgroup analysis according to mode of delivery of interventions (e.g. web sites versus smartphone app), but most were delivered via web sites and there were insufficient trials of interventions delivered via other mechanisms.
Funnel plots split by subgroups and meta‐regressions on longest period of follow‐up and on year of publication were constructed using Stata version 14 (Stata 2015).
Sensitivity analysis
We conducted sensitivity analyses by investigating the effect of omitting studies with either a high risk of attrition bias or a high risk of performance bias (due to lack of participant blinding). We also investigated the sensitivity of the analysis based on the primary outcome measure to including studies with unknown standard deviations (by inputting the median SD from studies that did report this) or unknown numbers of participants per arm (by assuming approximately equal numbers in each arm, based on the total number of participants at the time in question).
'Summary of findings' tables
We used the GRADE approach to assess the quality of the evidence.
The GRADE Working Group developed a system for grading the quality of evidence (GRADE 2004; Guyatt 2008; Guyatt 2011), which takes into account issues not only related to internal validity but also to external validity, such as directness of results. The 'Summary of findings' tables present the main findings of a review in a transparent and simple tabular format. In particular, they provide key information concerning the quality of evidence, the magnitude of effect of the interventions examined and the sum of available data on the main outcomes.
The GRADE system uses the following criteria for assigning grades of evidence:
-
High: We are very confident that the true effect lies close to that of the estimate of the effect.
-
Moderate: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different .
-
Low: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
-
Very low: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
GRADEpro GDT 2015 was used to import data from Review Manager 2014 for the main outcomes of quantity of drinking (g/week), frequency of drinking in terms of days/week and binges/week, and intensity of drinking (drinks/drinking day) for each of the comparisons (digital intervention versus control or minimal intervention, digital intervention versus face‐to‐face intervention). The tables were then imported back into the review (summary of findings Table for the main comparison; summary of findings Table 2).
Results
Description of studies
Results of the search
The search retrieved 3506 records after deduplication (Figure 1), which were screened by title and abstract in EndNote by two independent review authors. We excluded 3363 abstracts at this stage and retrieved the full text of 135 papers for further detailed evaluation, from which we selected 55 papers (reporting 57 studies) for inclusion in the review (Figure 1).
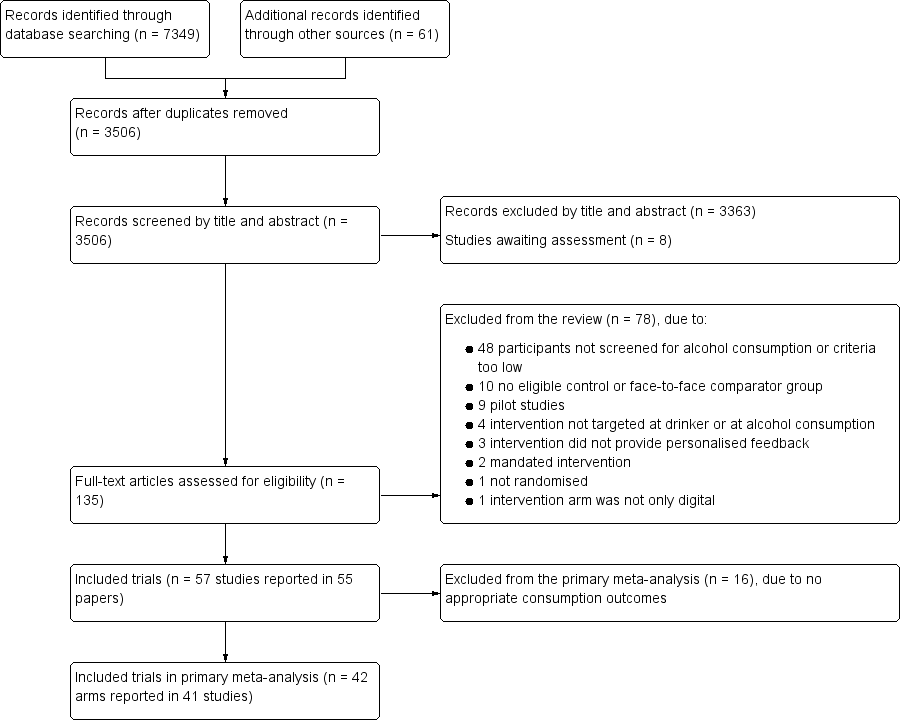
Study flow diagram
Included studies
Full details of the included studies are listed in the Characteristics of included studies section. We included 57 studies (reported in 55 papers) which randomised a total of 34,390 participants.
Of these, 33 studies were conducted in North America, 16 in mainland Europe, two in the UK, one in Japan, and five in Australasia.
One study recruited only women or girls (Delrahim‐Howlett 2011), three studies recruited only men or boys (Araki 2006; Bertholet 2015; Boon 2011), whilst another four studies recruited both but reported gender‐specific results (Chiauzzi 2005; Hansen 2012; Khadjesari 2014; Lewis 2007a). One study reported results by ethnicity (African American versus Caucasian students, Murphy 2010 (Study 1)).
Thirty‐seven studies considered teenagers, younger adults or students or both; the remaining 20 studies were specific to adults.
Thirty‐seven studies were based on interventions delivered completely online, and in 20 studies, the intervention was location specific.
Follow‐up times ranged from 1 to 24 months (median = 3 months). Fifty‐five trials compared a digital intervention to a no intervention or minimal intervention group, of which 41 reported appropriate information to be included in the primary meta‐analysis (one trial contained two substantially different intervention arms which were treated separately, so that there are 42 comparisons in the primary meta‐analysis). Seven trials included a comparison of a digital intervention versus a face‐to‐face intervention (Araki 2006; Blankers 2011; Butler 2009; Murphy 2010 (Study 1); Murphy 2010 (Study 2); Wagener 2012; Walters 2009), of which five (Butler 2009; Murphy 2010 (Study 1); Murphy 2010 (Study 2); Wagener 2012; Walters 2009) reported appropriate information to be included in the meta‐analysis. Six trials had a digital, face‐to‐face, and a no intervention control arm (Araki 2006; Blankers 2011; Butler 2009; Murphy 2010 (Study 2); Wagener 2012; Walters 2009).
A wide range of consumption outcomes was reported in the included trials, the most common were:
-
quantity of consumption in terms of mean or median units, drinks or grams per day, week, fortnight or month;
-
frequency of consumption in terms of percentage of drinking days over time or mean number of heavy drinking days;
-
intensity of consumption in terms of mean or median or peak drinks per drinking day or on the last or heaviest occasion;
-
screening tool results such as mean or median AUDIT or AUDIT‐C or FAST score, or percentage of participants over a certain score;
-
binge drinking percentage; and
-
blood alcohol concentration (BAC). BAC was reported as an estimate based on participants' self‐reported consumption rather than a direct measure so we did not use in the meta‐analysis because it was not adding to other self‐reported consumption measures.
We contacted one author because an outcome was reported differently in the tables than the text.
Study funding sources
Many (56%) studies were funded by government or research foundation funds. Some (11%) were funded by personal awards such as PhD fellowships. The rest of the studies did not report sources of funding.
Excluded studies
After checking the full text of studies we excluded 78 paper of 135 obtained (see Characteristics of excluded studies table). The most common reason for exclusion (n = 48) was that participants were not screened as hazardous or harmful drinkers ‐ including studies where participants only had to have consumed "any alcohol" or "one or two drinks" in the previous six months, and studies which aimed at primary prevention. Four studies were excluded because the target of the intervention was not the drinker themselves, or it was targeting other substances alongside alcohol and alcohol consumption could not be separated. The intervention was ineligible in six studies, including two where it was mandated (e.g. for university students who had to demonstrate reduced consumption to continue their courses). Other interventions were generic rather than personalised, or were not solely digital, or the feedback was not related to alcohol consumption. We excluded 10 studies because the comparator was either another digital intervention or the control group was not comparable to other studies. One study was excluded because it was not randomised, and nine because they were either pilot studies for which we had the full trial or aimed to test feasibility. See Characteristics of excluded studies.
Studies awaiting classification
Eight studies await classification (Characteristics of studies awaiting classification). Four studies tested digital interventions in college students (Balestrieri 2016; Bock 2016; Leeman 2016; Gajecki 2017). Balestrieri 2016 replicated the Australian College Drinkers Check‐up intervention (Hester 2012 (exp 1); Hester 2012 (exp 2)) in the USA, and reported a reduction in consumption and alcohol‐related consequences in intervention participants compared to control. Leeman 2016 reported that a multi‐component web‐based intervention called THRIVE also reduced consumption, and Gajecki 2017 found no difference between an intervention group receiving access to a skills training smartphone app and control. Bock 2016 reported that an SMS‐based intervention (TMAP) reduced heavy drinking and alcohol‐related consequences. Another USA study (Muench 2017) tested different types of SMS messages in a population recruited online, and reported that an automated daily message can reduce drinking more than weekly self‐tracking, and that a tailored adaptive text produced the greatest effect sizes. Two studies reported no difference in consumption between a computer‐assisted brief intervention and control: one delivered to patients in a French emergency department (Duroy 2016), and the other to American post‐partum women (Ondersma 2016). Finally, Acosta 2017 reported a reduction in consumption in veterans with posttraumatic stress disorder (PTSD) receiving a cognitive behavioural therapy (CBT) web‐based intervention.
Ongoing studies
Three of the ongoing studies are evaluating the use of smartphone apps for reducing hazardous or harmful alcohol consumption. Two are taking place in the UK: the SIPS Jr trial (ISRCTN45300218) is recruiting adolescents (aged 14‐18 yrs) in emergency departments, and a second trial (ISRCTN40104069) is testing the Drink Less app in a UK population of hazardous and/or harmful alcohol users. Three apps (Promillekoll, PartyPlanner and TeleCoach) are being evaluated in a further trial recruiting Swedish university students (NCT02064998). Finally, ISRCTN10323951 is a trial of a web‐based self‐help intervention for hazardous drinkers with mild to moderate depression.
Risk of bias in included studies
All reported outcomes in this review relate to self‐reported consumption of alcohol by participants, and so we have summarised the risk of bias at the study rather than the outcome level (Figure 2). Risk of bias assessments for each study are presented in Characteristics of included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Random sequence generation
None of the included studies were assigned high risk of bias due to the method of randomisation. Fifteen studies were judged to have an unclear risk of bias due to randomisation because it was not clear whether the process was automated and the sequence generation process was not clearly reported. Forty‐one studies (72%) were considered to be at low risk of bias either because sequence generation took place as part of a completely automated assessment and intervention process, or because authors described using a computer‐generated sequence generation process.
Allocation concealment
It was clear from the description of the process in 29 studies that allocation was completely automated. These studies were judged to be at low risk of bias, along with an additional five studies that described allocation being conducted by someone independent of the trial, giving a total of 34 studies (60%) at low risk of bias due to allocation concealment. Two studies (4%) were judged to be at high risk of bias due to allocation concealment: Boon 2011 reported that the condition to which participants were assigned was revealed to research assistants once recruitment was complete; and in Hester 1997, a researcher was reported to log both intervention and control participants' data into the computer.
Blinding
Performance bias
Trials were judged by default to be at high risk of performance bias due to participant blinding because participants always knew that they were receiving alcohol‐related advice. However, if trials reported that there was an attempt to blind participants (e.g. by 'camouflaging' alcohol advice among other health‐related information) then the trial was assigned as low risk of bias in this respect ‐ 13 trials (23%) received this rating.
Detection bias
We judged 29 trials (51%) to be at low risk of detection bias. Eight trials (14%) (Bendtsen 2015; Blankers 2011; Boon 2011; Butler 2003; Chiauzzi 2005; Hester 1997; Khadjesari 2014; Postel 2010) were judged to be at high risk of bias because outcome assessment was not automated and researchers carrying out the assessments could have been aware of participant allocation. Outcome assessment for both intervention and control groups tended to occur by the same mechanism within individual trials, so we did not consider there was any difference in the risk of detection bias between intervention and control participants in the same trial.
Incomplete outcome data
The main source of bias in the included studies was due to attrition; follow‐up was challenging because there was often little face‐to‐face contact between trialists and participants. Trials were judged to be at high risk of attrition bias if loss to follow‐up was > 30% or if it was different between arms with no explanation to account for this; 17 trials (30%) were considered to be at high risk of attrition bias and 23 (40%) were judged to be at low risk.
Selective reporting
Selective reporting was not a major source of bias in the included studies. Most trials reported data for the same outcomes as they had specified in the protocol (where available) or methods section of the paper. Two trials (Butler 2003; Weaver 2014) were judged to be at unclear risk of bias because outcome values were not reported consistently.
Effects of interventions
See: Summary of findings for the main comparison Digital intervention compared to no or minimal intervention for reducing hazardous and harmful alcohol consumption in community‐dwelling populations; Summary of findings 2 Digital intervention compared to face‐to‐face intervention for reducing hazardous and harmful alcohol consumption in community‐dwelling populations
1. Digital intervention versus no intervention or minimal intervention
1.1 Quantity of alcohol consumed per week: primary meta‐analysis, based on longest period of follow‐up
This analysis comprised data from 41 trials (42 comparisons; 1 trial comprised 2 digital intervention arms that were analysed separately). The remaining 16 trials could not be included in the primary meta‐analysis because they did not report consumption data. There was a total of 19,241 participants in these 41 trials (9631 randomised to a digital intervention, 9610 randomised to a control group). The longest period of follow‐up in these 41 trials varied from 1 to 12 months. Overall, participants who received a digital intervention drank 22.8 g (95% CI 15.4 to 30.3) of alcohol per week less than control group participants at the longest reported follow‐up point (see Analysis 1.1, summary of findings Table for the main comparison). There was considerable heterogeneity in the estimate of the effect size among trials (I² = 78%), although the quantity of drinking was greater in the digital intervention arm than in the control arm in only four studies. The associated funnel plot (Figure 3) indicates some evidence of asymmetry, suggesting the possibility of under‐reporting of results with little or no evidence of an intervention effect. Meta‐regression showed that the effect size varied according to year of publication of the trial; specifically, for every year going forwards in time the mean difference in consumption between digital intervention and no or minimal intervention arms decreased by 6.3 g/week (95% CI 2.0 to 10.6). In other words, there was a smaller difference in consumption between intervention and comparison groups in more recent trials.

Funnel plot of comparison 1: Digital intervention vs. control, outcome 1.1: Quantity of drinking (g/week), based on longest follow‐up
The trials that could not be included in the primary meta‐analysis tended to be smaller, but did not tend to be at higher risk of bias compared to those included.
1.2 Quantity of alcohol consumed per week: subgroup analyses
Intervention modality
Trials included insufficient different types of modalities (web sites, apps, etc.) to carry out a subgroup analysis.
Timing of outcomes (using follow‐up times reported in the trials)
The follow‐up periods in the 41 trials in the primary meta‐analysis ranged from 1 to 12 months. Twenty‐six trials reported alcohol consumption at one time point only; and 15 trials reported these data at two or more time points. For the purpose of Analysis 1.2, follow‐up times were grouped as one month (17 comparisons, 7187 participants); more than 1 month and up to 2 months (6 studies, 2846 participants); more than two months and up to three months (13 studies, 3000 participants); more than three months and up to six months (19 comparisons, 12,822 participants); and 12 months (7 comparisons, 3372 participants). At each of these follow‐up time points, the estimated difference in consumption between digital intervention and no or minimal intervention arms was less than zero, ranging from ‐43.3 g/week (range = ‐73.2 to ‐13.4) at two to three months, to ‐11.5 g/week (range = ‐16.3 to ‐6.7) at three to six months (Analysis 1.2). At all follow‐up times other than 12 months, the difference in alcohol consumption between trial arms was significantly less than zero (test for subgroup differences Chi² = 6.36, df = 4, P = 0.17); they were not significantly different from each other.
A meta‐regression analysis of effect size on length of follow‐up could not be conducted based on data in Analysis 1.2 because some of the trials contributed to more than one follow‐up period. However, when trials were classified on the basis of their longest follow‐up using data in Analysis 1.1, the change per month of follow‐up in the difference in alcohol consumption between digital intervention and control arms was only 2.8 g/week (95% CI ‐1.0 to 6.6).
Age: trials restricted to younger people versus trials in adults
Of the 41 trials in the main meta‐analysis, 27 trials (providing 28 comparisons; one had two digital intervention arms) with 13,477 participants who were solely adolescents, young adults or college students. The age limits varied but the maximum specified age in this subgroup of trials was 29 years. Analysis 1.3 shows the results from the meta‐analysis based on the longest period of follow‐up, separately for trials restricted to younger people and those trials in adults (i.e. aged > 18 years). For adolescents or young adults, the difference between the digital intervention and no or minimal intervention arms in the quantity of alcohol consumed was smaller in magnitude than in the main analysis (‐13.4 g/week, 95% CI ‐19.3 to ‐7.6). Furthermore, this value differed significantly from the corresponding value based on 14 trials in 5764 adults (aged > 18 years) (‐56.1 g/week, 95% CI ‐82.1 to ‐30.0). The degree of heterogeneity in the effect size differed markedly between these two sets of trials: 52% for trials in adolescents and young adults and 89% for the trials in adults (aged > 18 years) (test for subgroup differences Chi² = 9.8, df = 1, P = 0.002). The associated funnel plot (Figure 4) indicated that much of the heterogeneity was associated with trials of adults (aged > 18 years).
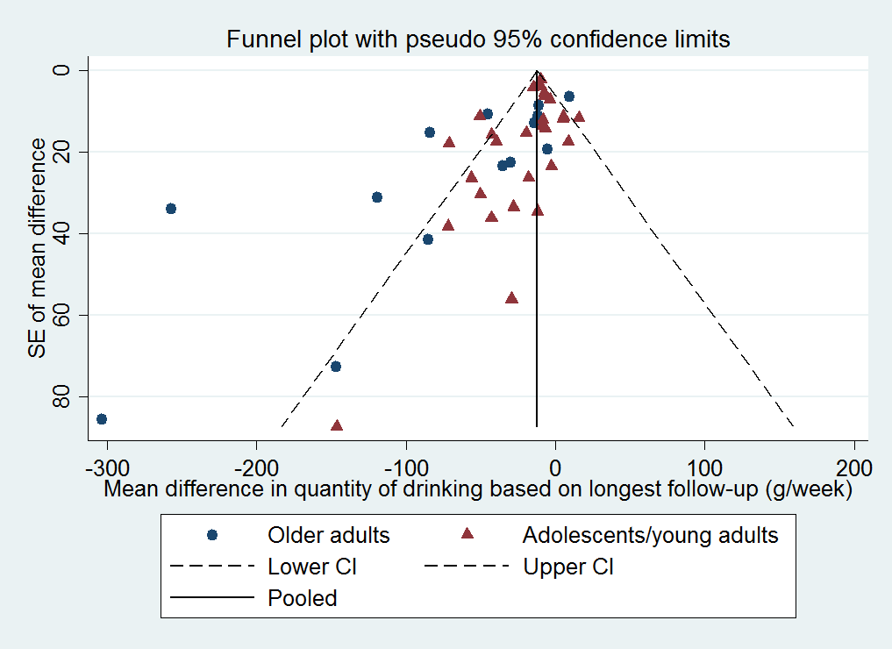
Funnel plot of comparison 1: Digital intervention vs. control, outcome 1.6: Quantity of drinking (g/week), based on longest follow‐up and categorised on whether restricted to adolescents or young adults
Age: trials restricted to younger people versus trials in adults, categorised by length of follow‐up
For follow‐up times of one month and three to six months, most participants in the main analysis were adolescents, young adults or college students. Estimates of the difference in alcohol consumption at these follow‐up times were similar in Analysis 1.2 and Analysis 1.4. For most follow‐up times, the difference in alcohol consumption between the digital intervention and no or minimal intervention arms was significantly less than zero, except at one to two months when this difference was ‐7.6 g/week (95% CI ‐19.0 to 3.8) and at 12 months when this difference was ‐2.4 g/week (95% CI ‐23.6 to 18.9).
Trials restricted by gender
Only five included trials (Bertholet 2015; Chiauzzi 2005; Delrahim‐Howlett 2011; Khadjesari 2014; Lewis 2007a; 2566 participants) provided appropriate information on alcohol consumption by gender for meta‐analysis. There was no evidence from these trials that the difference in alcohol consumption between trial arms was modified by gender. Male intervention group participants drank 8.9 g/week less (95% CI ‐32.0 to 14.3) and females drank 9.8 g/week less (95% CI ‐21.9 to 2.2) (test for subgroup differences Chi² = 0.01, df = 1, P = 0.94; Analysis 1.5). However, the data available were limited, particularly for females. A further 11 trials mentioned secondary analyses by gender but did not present corresponding data; most stated they found no evidence of a differential impact of the intervention by gender.
1.3 Quantity of alcohol consumed per week: sensitivity analyses
The sensitivity analyses demonstrated that the primary meta‐analysis is robust to the impact of potential biases and missing data. Imputing values for missing standard deviations and numbers of participants had very little impact on the effect estimate. Omitting trials at high risk of attrition and performance bias (in separate analyses) resulted in a smaller estimate of effect in each case.
Omitting trials at high risk of attrition bias
Of the 41 trials in the main meta‐analysis, 14 were judged to be at high risk of bias due to incomplete data, either through high losses to follow‐up overall or differences between trial arms in the level of follow‐up, or both. After omitting these 14 trials, the difference between the digital intervention and control arms in the quantity of alcohol consumed was slightly smaller than before, although there was still strong evidence for a reduction in consumption (difference of ‐16.2 g/week, 95% CI ‐23.4 to ‐9.1; Analysis 1.6).
Omitting trials at high risk of performance bias
Of the 41 trials in the primary meta‐analysis, 30 were judged to be at high risk of performance bias linked to a lack of participant blinding. In an analysis based on the remaining 11 trials (10,272 participants), the difference between the digital intervention and control arms in the quantity of alcohol consumed was smaller than in the primary meta‐analysis, although there was still evidence for a reduction in consumption (difference of ‐10.5 g/week, 95% CI ‐13.7 to ‐7.4; Analysis 1.7). Note that two included studies in Figure 2 depicted as assessment at low risk of performance bias could not be included in the primary meta‐analysis, the other 11 trials appear in this sensitivity analysis.
Imputation of missing standard deviations or unknown numbers of participants per arm
Six trials (Araki 2006; Cucciare 2013; Hedman 2008; Kypri 2008; Neighbors 2010; Ridout 2014) had unknown standard deviations for the quantity of alcohol consumed. The number of participants per arm was not reported for Neighbors 2004. Analysis 1.8 shows the results based on including these seven trials with imputed values for the unknown SDs or numbers of participants per arm (Araki 2006; Cucciare 2013; Hedman 2008; Kypri 2008; Neighbors 2004; Neighbors 2010; Ridout 2014). These results were very similar to those based on excluding these trials (Analysis 1.1). Specifically, the estimated difference in consumption between the digital intervention and control arms was ‐22.2 g/week (range = ‐29.2 to ‐15.2 g/week).
Imputation of missing standard deviations or unknown numbers of participants per arm, categorised by length of follow‐up
Analysis 1.9 shows the results by length of follow‐up, based on including the six trials with imputed values for unknown SDs or unknown numbers of participants per arm. These results are broadly similar to those based on excluding these trials (Analysis 1.2). Only one trial (Neighbors 2010) provided information for follow‐up periods over 12 months, and did not provide evidence for an effectiveness of interventions at 18 months (22.4 g/week; range = ‐5.56 to 50.36 g/week) or 24 months (1.4 g/week; range = ‐20.28 to 23.08 g/week).
1.4 Frequency of drinking per week: meta‐analysis, based on longest follow‐up
This analysis was based on data from 15 trials (10,862 participants; 16 comparisons; 1 trial comprised two digital intervention arms that were analysed separately). The estimated difference between the digital intervention and no or minimal intervention arms was ‐0.16 days drinking per week (95% CI ‐0.24 to ‐0.09), which equates to less than one day fewer drinking per month linked to a digital intervention (see Analysis 1.10, summary of findings Table for the main comparison). There was no evidence from a meta‐regression analysis of an association between frequency of drinking and length of longest follow‐up; specifically, the change per month of longest follow‐up in the difference between digital intervention and no or minimal intervention arms in the number of days drinking per week was 0.09 (95% CI ‐0.17 to 0.36). However, another meta‐regression analysis showed that the difference between arms was significantly smaller in magnitude for more recent trials; specifically, for every year going forwards in time the mean difference in number of days drinking per week between digital intervention and no or minimal intervention arms decreased by 0.036 days per week (95% CI 0.05 to 0.068).
1.5 Frequency of binges per week: meta‐analysis, based on longest follow‐up
This analysis was based on data from 15 trials (3587 participants). The definition of binge drinking varied among studies, but was most commonly at least four (for women) or five (for men) drinks in a single session. The estimated difference between the digital intervention and no or minimal intervention arms in the number of binges per week was ‐0.24 (95% CI ‐0.35 to ‐0.13), which equates to about one binge fewer per month linked to a digital intervention (see Analysis 1.11, summary of findings Table for the main comparison). Meta‐regressions showed no associations with either length of longest follow‐up or year of publication.
1.6 Intensity of drinking: meta‐analysis, based on longest follow‐up
This analysis was based on data from 15 trials (9791 participants). The estimated difference between the digital intervention and no or minimal intervention arms in the intensity of drinking was ‐4.63 g/alcohol per drinking day (95% CI ‐8.02 to ‐1.23), which equates to less than one unit fewer per drinking day (see Analysis 1.12, summary of findings Table for the main comparison). Meta‐regressions showed no associations with either length of longest follow‐up or year of publication.
1.7 Binge drinkers: meta‐analysis, based on longest follow‐up
Nine trials (9417 participants) reported data on the numbers of binge drinkers per arm at follow‐up. The risk ratio of being a binge drinker at the time of longest follow‐up among those randomised to a digital intervention relative to those randomised to a control or minimal intervention condition was 0.98 (95% CI 0.97 to 1.00; Analysis 1.13). Meta‐regressions showed no associations with either length of longest follow‐up or year of publication.
1.8 Alcohol problems and consequences
Thirteen studies reported some measure of alcohol problems or consequences, but on many different scales, so it was difficult to compare across studies. Some studies in students reported a trend toward reduction in alcohol‐related problems.
2. Digital intervention versus face‐to‐face intervention
2.1 Quantity of alcohol consumed per week: meta‐analysis, based on longest period of follow‐up
Only five trials (390 participants) reported alcohol consumption in both digital and face‐to‐face intervention arms. There was no evidence of a difference in alcohol consumption between these arms: 0.5 g/week (95% CI ‐24.6 to 25.6; Analysis 2.1, summary of findings Table 2). However, the numbers of participants in this analysis were small (< 200 in each arm).
2.2 Quantity of alcohol consumed per week: meta‐analysis, subdivided by length of follow‐up
The period of follow‐up of trials that included both digital and face‐to‐face intervention arms ranged from one month to six months. There was no indication that the difference in alcohol consumption between these arms varied according to period of follow‐up, although data were sparse (Analysis 2.2).
2.3 Frequency of drinking per week: meta‐analysis, based on longest period of follow‐up
Only one trial with 58 participants (Butler 2009) reported frequency of drinking at follow‐up by trial arm. There was no indication of difference in frequency between the digital and face‐to‐face intervention arms: 0.05 days drinking per week (95% CI ‐0.33 to 0.43; Analysis 2.3, summary of findings Table 2), but the number of participants in this trial was small.
2.4 Frequency of binges per week: meta‐analysis, based on longest period of follow‐up
Only three trials with 206 participants (Butler 2009; Murphy 2010 (Study 1); Murphy 2010 (Study 2)) reported frequency of binges at follow‐up by trial arm. There was no indication of difference in frequency between the digital and face‐to‐face intervention arms ‐ 0.04 binges per week (95% CI ‐0.15 to 0.22; Analysis 2.4, summary of findings Table 2), but the numbers of participants in this analysis were small (about 100 in each arm).
Six studies were eligible for inclusion but provided no data for any meta‐analyses, because they did not report consumption outcomes that could be converted to g/week (Boon 2011; Butler 2003; Cunningham 2012b; Palfai 2011; Sinadinovic 2014; Spijkerman 2010). Only one of these studies (Boon 2011) reported a decrease in consumption in intervention participants compared to control; the others reported either that all arms of the trial had reduced their consumption, or that only a subgroup of participants (e.g. binge drinkers) had done so.
None of the studies reported whether any harms resulted from the interventions.
3. Behaviour change techniques
Prevalence of behaviour change techniques (BCTs)
The BCT content of 42 comparisons analysed on the basis of quanity of drinking (g/week) based on longest follow‐up (Analysis 1.1) was assessed. Of the BCTs uniquely present in experimental arms, i.e. not present in both experimental and control arms, the five most frequently used were: feedback on behaviour (85.7%, n = 36), social comparison (81.0%, n = 34), information about social and environmental consequences (71.4%, n = 30) feedback on outcomes of behaviour (69.0%, n = 29) and social support (unspecified) (64.3%, n = 27) (Table 1). Of the 93 possible BCTs that could have been used, 15 were used in more than 20% of trials, 44 were used at least once and 49 were never used. The mean number of BCTs used in experimental arms was 9.1 (SD = 5.3), the median was nine and the range was 1 to 21.
| Behaviour change technique | % age (N) |
| 2.2. Feedback on behaviour | 85.7% (36) |
| 6.2. Social comparison | 81.0% (34) |
| 5.3. Information about social and environmental consequences | 71.4% (30) |
| 2.7. Feedback on outcome(s) of behaviour | 69.0% (29) |
| 3.1. Social support (unspecified) | 64.3% (27) |
| 4.1. Instruction on how to perform the behaviour | 52.4% (22) |
| 2.6. Biofeedback | 50.0% (21) |
| 5.2. Salience of consequences | 50.0% (21) |
| 9.2. Pros and cons | 35.7% (15) |
| 1.2. Problem solving | 33.3% (14) |
| 5.1. Information about health consequences | 33.3% (14) |
| 1.4. Action planning | 31.0% (13) |
| 9.1. Credible source | 31.0% (13) |
| 1.1. Goal setting (behaviour) | 28.6% (12) |
| 2.3. Self‐monitoring of behaviour | 26.2% (11) |
| 3.2. Social support (practical) | 16.7% (7) |
| 2.4. Self‐monitoring of outcome(s) of behaviour | 14.3% (6) |
| 4.2. Information about antecedents | 14.3% (6) |
| 1.3. Goal setting (outcome) | 11.9% (5) |
| 1.6. Discrepancy between current behaviour and goal | 11.9% (5) |
| 8.2. Behaviour substitution | 9.5% (4) |
| 12.2. Restructuring the social environment | 9.5% (4) |
| 15.4. Self‐talk | 9.5% (4) |
| 5.6. Information about emotional consequences | 7.1% (3) |
| 7.1. Prompts/cues | 7.1% (3) |
| 11.2. Reduce negative emotions | 7.1% (3) |
| 12.3. Avoidance/reducing exposure to cues for the behaviour | 7.1% (3) |
| 1.5. Review behaviour goal(s) | 4.8% (2) |
| 5.4. Monitoring of emotional consequences | 4.8% (2) |
| 10.3. Non‐specific reward | 4.8% (2) |
| 10.9. Self‐reward | 4.8% (2) |
| 1.7. Review outcome goal(s) | 2.4% (1) |
| 1.8. Behavioural contract | 2.4% (1) |
| 3.3. Social support (emotional) | 2.4% (1) |
| 4.4. Behavioural experiments | 2.4% (1) |
| 8.1. Behavioural practice/rehearsal | 2.4% (1) |
| 8.7. Graded tasks | 2.4% (1) |
| 10.4. Social reward | 2.4% (1) |
| 10.6. Non‐specific incentive | 2.4% (1) |
| 13.2. Framing/reframing | 2.4% (1) |
| 14.2. Punishment | 2.4% (1) |
| 15.1. Verbal persuasion about capability | 2.4% (1) |
| 15.3. Focus on past success | 2.4% (1) |
The following behaviour change techniques were not used in any digital intervention: 1.9. Commitment, 2.1. Monitoring of behaviour by others without feedback, 2.5. Monitoring of outcome(s) of behaviour without feedback, 4.3. Re‐attribution, 5.5. Anticipated regret, 6.1. Demonstration of the behaviour, 6.3. Information about others’ approval, 7.2. Cue signalling reward, 7.3. Reduce prompts/cues, 7.4. Remove access to the reward, 7.5. Remove aversive stimulus, 7.6. Satiation, 7.7. Exposure, 7.8. Associative learning, 8.3. Habit formation, 8.5. Overcorrection, 8.6. Generalisation of target behaviour, 9.3. Comparative imagining of future outcomes, 10.1. Material incentive (behaviour), 10.2. Material reward (behaviour), 10.5. Social incentive, 10.7. Self‐incentive, 10.8. Incentive (outcome), 10.10. Reward (outcome), 10.11. Future punishment, 11.1. Pharmacological support, 11.3. Conserving mental resources, 11.4. Paradoxical instructions, 12.1. Restructuring the physical environment, 12.4. Distraction, 12.5. Adding objects to the environment, 12.6. Body changes, 13.1. Identification of self as role model, 13.3. Incompatible beliefs, 13.4. Valued self‐identify, 13.5. Identity associated with changed behaviour, 14.1. Behaviour cost, 14.3. Remove reward, 14.4. Reward approximation, 14.5. Rewarding completion, 14.6. Situation‐specific reward, 14.7. Reward incompatible behaviour, 14.8. Reward alternative behaviour, 14.9. Reduce reward frequency, 14.10. Remove punishment, 15.2. Mental rehearsal of successful performance, 16.1. Imaginary punishment, 16.2. Imaginary reward, 16.3. Vicarious consequences.
Unadjusted associations between behaviour change techniques (BCTs) and intervention effectiveness
The BCTs of goal setting (B ‐43.94, SE 17.14, 95% CI ‐78.59 to ‐9.30, P = 0.01, R²adj 6.64%), problem solving (B ‐48.03, SE 14.72, 95% CI ‐77.79 to ‐18.27, P < 0.01, R²adj 25.01%), information about antecedents (B ‐74.20, SE 21.53, 95% CI ‐117.72 to ‐30.68, P < 0.01, R²adj 32.15%), behaviour substitution (B ‐123.71, SE 30.14, 95% CI ‐184.63 to ‐62.80, P < 0.001, R²adj 48.53%) and credible source (B ‐39.89, SE 16.22, 95% CI ‐72.66 to ‐7.11, P = 0.02, R²adj 15.60%) were associated with reduced alcohol consumption in unadjusted models (Table 2).
| Behaviour change technique | B (SE) | P | 95% CI | I² | Adj R² | |
| 1.1 | Goal setting (behaviour) | ‐43.94 (17.14) | 0.01 | ‐78.59 to ‐9.30 | 78.05% | 6.64% |
| 1.2 | Problem solving | ‐48.03 (14.72) | < 0.01 | ‐77.79 to ‐18.27 | 74.64% | 25.01% |
| 1.3 | Goal setting (outcome) | ‐14.43 (23.46) | 0.54 | ‐61.85 to 32.99 | 77.71% | ‐2.95% |
| 1.4 | Action planning | ‐26.21 (16.58) | 0.12 | ‐59.73 to 7.30 | 77.57% | 5.45% |
| 1.6 | Discrepancy between current behaviour and goal | ‐33.88 (24.97) | 0.18 | ‐84.35 to 16.58 | 78.24% | 0.15% |
| 2.2 | Feedback on behaviour | 12.97 (21.30) | 0.55 | ‐30.08 to 56.02 | 78.31% | ‐7.13% |
| 2.3 | Self‐monitoring of behaviour | ‐30.39 (17.14) | 0.08 | ‐65.03 to 4.26 | 78.36% | 2.07% |
| 2.4 | Self‐monitoring of outcome(s) of behaviour | ‐8.60 (22.37) | 0.70 | ‐53.81 to 36.61 | 78.52% | ‐4.67% |
| 2.6 | Biofeedback | 10.81 (15.24) | 0.48 | ‐19.99 to 41.62 | 77.85% | 1.55% |
| 2.7 | Feedback on outcome(s) of behaviour | ‐4.62 (16.45) | 0.78 | ‐37.87 to 28.63 | 78.48% | ‐5.63% |
| 3.1 | Social support (unspecified) | ‐19.55 (15.39) | 0.21 | ‐50.65 to 11.55 | 78.53% | ‐0.41% |
| 3.2 | Social support (practical) | ‐26.35 (22.59) | 0.25 | ‐72.01 to 19.31 | 77.18% | 0.29% |
| 4.1 | Instruction on how to perform the behaviour | 4.46 (15.51) | 0.78 | ‐26.89 to 35.80 | 78.55% | ‐5.77% |
| 4.2 | Information about antecedents | ‐74.20 (21.53) | <0.01 | ‐117.72 to ‐30.68 | 74.91% | 32.15% |
| 5.1 | Information about health consequences | 16.75 (15.70) | 0.29 | ‐14.99 to 48.49 | 78.42% | 0.06% |
| 5.2 | Salience of consequences | 21.99 (14.86) | 0.15 | ‐8.05 to 52.02 | 78.17% | 4.92% |
| 5.3 | Information about social and environmental consequences | 28.88 (16.56) | 0.09 | ‐4.59 to 62.34 | 77.59% | 1.01% |
| 6.2 | Social comparison | 24.25 (18.95) | 0.21 | ‐14.06 to 62.56 | 78.53% | ‐4.98% |
| 8.2 | Behaviour substitution | ‐123.71 (30.14) | < 0.001 | ‐184.63 to ‐62.80 | 72.92% | 48.53% |
| 9.1 | Credible source | ‐39.89 (16.22) | 0.02 | ‐72.66 to ‐7.11 | 75.84% | 15.60% |
| 9.2 | Pros and cons | ‐30.10 (15.77) | 0.06 | ‐61.97 to 1.78 | 77.57% | 10.15% |
| 12.2 | Restructuring the social environment | ‐22.91 (31.52) | 0.47 | ‐86.62 to 40.79 | 78.56% | ‐7.66% |
| 15.4 | Self‐talk | ‐41.53 (26.37) | 0.12 | ‐94.84 to 11.77 | 77.93% | 6.04% |
Abbreviation: B = regression coefficient
Rows in italics denote BCTs demonstrating a significant association with effect size in the unadjusted analysis
Adjusted associations between behaviour change techniques (BCTs) and intervention effectiveness
In an adjusted model that included BCTs with B > 23 in the unadjusted model, the BCTs of behaviour substitution (B ‐95.12, SE 33.09, 95% CI ‐162.90 to ‐27.34, P = 0.01), problem solving (B ‐45.92, SE 21.99, 95% CI ‐90.97 to ‐0.87, P = 0.05), and credible source (B ‐32.09, SE 13.94, 95% CI ‐60.64 to ‐3.55, P = 0.03) were significantly associated with reduced alcohol consumption (Table 3). The adjusted meta‐regression model produced relatively good indices of fit and substantially reduced heterogeneity (I² 67.24%, R²adj 59.51%, P < 0.01) compared to the I² heterogeneity of 78.0% from the main outcomes.
| Behaviour change technique | B (SE) | P | 95% CI | |
| 1.1 | Goal setting (behaviour) | 0.75 (19.60) | 0.97 | ‐39.40 to 40.89 |
| 1.2 | Problem solving | ‐45.92 (21.99) | 0.05 | ‐90.97 to ‐0.87 |
| 1.4 | Action planning | 30.75 (19.50) | 0.13 | ‐9.19 to 70.68 |
| 1.6 | Discrepancy between current behaviour and goal | ‐29.86 (23.97) | 0.22 | ‐78.97 to 19.25 |
| 2.3 | Self‐monitoring of behaviour | ‐6.34 (18.35) | 0.73 | ‐43.91 to 31.24 |
| 3.2 | Social support (practical) | 33.73 (21.85) | 0.13 | ‐11.03 to 78.49 |
| 4.2 | Information about antecedents | ‐43.38 (23.93) | 0.08 | ‐92.39 to 5.63 |
| 5.2 | Salience of consequences | 13.20 (14.96) | 0.39 | ‐17.55 to 43.95 |
| 5.3 | Information about social and environmental consequences | 24.64 (12.17) | 0.05 | ‐0.30 to 49.57 |
| 8.2 | Behaviour substitution | ‐95.12 (33.09) | 0.01 | ‐162.90 to ‐27.34 |
| 9.1 | Credible source | ‐32.09 (13.94) | 0.03 | ‐60.64 to ‐3.55 |
| 9.2 | Pros and cons | 6.68 (13.68) | 0.63 | ‐21.33 to 34.69 |
| 15.4 | Self‐talk | ‐8.41 (26.69) | 0.76 | ‐63.09 to 46.27 |
Abbreviation: B = regression coefficient
Rows in italics denote BCTs demonstrating a significant association with effect size in the adjusted analysis
Neither the model containing the total number of BCTs, nor the model containing BCTs in the control BCTs group produced significant findings.
Most of the 30 most prevalent BCTs were common to both studies included in the primary meta‐analysis and studies that were ineligible for meta‐analysis. However, the order differs (e.g. 2.3 is the 7th most prevalent BCT in the former group and the 7th most prevalent in the latter group) and there are a number of highly prevalent BCTs found in one group but not the other (e.g. 1.9 is in the top 30 BCTs of excluded studies but not in the top 30 BCTs of included studies). In total, of the 30 most prevalent BCTs in each group, there are 8 unique to the excluded group and a different 8 unique to the included group.
Most of the 30 prevalent BCTs were common to both studies included in the primary meta‐analysis and studies that were ineligible for meta‐analysis.
4. Theory use and impact
Prevalence of use of theory items and areas, and individual theories
The use of theory was assessed in interventions in the 42 comparisons that were focus of Analysis 1.1 (quality of drtinking g/week, based on longest follow‐up). The most frequently reported aspects of theory were: a theory or model mentioned (n = 21, 50%), targeted constructs mentioned as a predictor of behaviour (n = 17, 40%), and theory or theoretical predictors used to select or develop intervention techniques (n = 16, 38%) (Table 4). There was no mention of theory for 21 interventions (50%), including any reference to the use of theory in either the design or evaluation of the intervention. Only three studies used theory to tailor the intervention to recipients. No intervention used a theory or predictors to select recipients for the intervention, or to refine the theory, either by adding or removing theoretical constructs or by specifying that the inter‐relationships between theoretical constructs should be changed (Table 4).
| Theory Coding Scheme item description (item number) | N (%) of studies where item = 1 |
| Theory/model of behaviour mentioned (I1) | 21 (50%) |
| Targeted construct mentioned as predictor of behaviour (I2) | 17 (40%) |
| Intervention based on single theory (I3) | 9 (21%) |
| Theory/predictors used to select recipients for the intervention (I4) | 0 (0%) |
| Theory/predictors used to select/develop intervention techniques (I5) | 16 (38%) |
| Theory/predictors used to tailor intervention techniques to recipients (I6) | 3 (7%) |
| All intervention techniques are explicitly linked to at least one theory‐relevant construct/predictor (I7) | 6 (14%) |
| At least one, but not all, of the intervention techniques are explicitly linked to at least one theory‐relevant construct/predictor (I8) | 11 (26%) |
| Group of techniques are linked to a group of constructs/predictors (I9) | 2 (5%) |
| All theory‐relevant constructs/predictors are explicitly linked to at least one intervention technique (I10) | 7 (17%) |
| At least one, but not all, of the theory‐relevant constructs/predictors are explicitly linked to at least one intervention technique (I11) | 10 (24%) |
| Theory‐relevant constructs are measured: post‐intervention (I12a) | 12 (29%) |
| Theory‐relevant constructs are measured: post‐ and pre‐intervention (I12b) | 10 (24%) |
| Changes in measured theory‐relevant constructs/predictor (I13) | 8 (19%) |
| Mediational analysis of constructs/ predictors: mediator predicts the dependent variable (I14a) | 6 (14%) |
| Mediational analysis of constructs/ predictors: mediator predicts dependent variable, controlling for the independent variable (I14b) | 3 (7%) |
| Mediational analysis of constructs/ predictors: intervention does not predict the dependent variable when controlling the independent variable (I14c) | 4 (10%) |
| Mediational analysis of constructs/ predictors: mediated effect is statistically significant (I14d) | 6 (14%) |
| Results discussed in relation to theory (I15) | 12 (29%) |
| Appropriate support for theory (I16) | 7 (17%) |
| Results used to refine theory: adding/ removing constructs to the theory (I17a) | 0 (0%) |
| Results used to refine theory: specifying that the interrelationships between the theoretical constructs should be changed (I17b) | 0 (0%) |
The most frequently mentioned theories or models were Motivational Interviewing Theory (8/21), Transtheoretical Model (6/21) and Social Norms Theory (6/21) (Table 5). There were 18 different theories or models mentioned. The mean total use of theory score was 4.4 out of a possible 22 which indicates that most studies did not use, report, or both use or report theory in intervention development and evaluation (Table 6).
| Study ID | Theories (n) | Total theory use score | TM | SRT | SCT | SLT | DMT | MIT | SNT | TPB | SIT | SCompT | SImpT | SDT | ICM | HBM | TSI | ET | CBT | PBT |
| 3 | 6 | X | X | X | ||||||||||||||||
| 3 | 6 | X | X | X | ||||||||||||||||
| 1 | 6 | X | ||||||||||||||||||
| 1 | 15 | X | ||||||||||||||||||
| 1 | 7 | X | ||||||||||||||||||
| 1 | 8 | X | ||||||||||||||||||
| 1 | 8 | X | ||||||||||||||||||
| 1 | 1 | X | ||||||||||||||||||
| 3 | 12 | X | X | X | ||||||||||||||||
| 4 | 16 | X | X | X | X | |||||||||||||||
| 3 | 14 | X | X | X | ||||||||||||||||
| 2 | 15 | X | X | |||||||||||||||||
| 1 | 12 | X | ||||||||||||||||||
| 1 | 16 | X | ||||||||||||||||||
| 2 | 4 | X | X | |||||||||||||||||
| 5 | 9 | X | X | X | X | X | ||||||||||||||
| 3 | 6 | X | X | X | ||||||||||||||||
| 3 | 5 | X | X | X | ||||||||||||||||
| 5 | 8 | X | X | X | X | X | ||||||||||||||
| 2 | 7 | X | X | |||||||||||||||||
| 2 | 2 | X | X | |||||||||||||||||
| Number of studies: | 6 | 2 | 2 | 2 | 1 | 7 | 6 | 3 | 2 | 3 | 3 | 1 | 3 | 1 | 2 | 1 | 1 | 1 | ||
Abbreviations: CBT = cognitive‐behavioural theory; DMT = decision‐making theory; ET = expectancy theory; HBM = health belief model; ICM = I‐change model; MIT = motivational interviewing theory; PBT = problem behaviour theory; SCT = social cognitive theory; SCompT = social comparison theory; SDT = social determination theory; SImpT = social impact theory; SIT = social identity theory; SLT = social learning theory; SNT = social norms theory; SRT = self‐regulation theory; TM = transtheoretical model; TPB = theory of planned behaviour; TSI = theory of social influence
| Theory Coding Scheme Categories (category number) | Items included | Maximum score | Mean (SD) | Number of studies scoring ≥ 1 |
| Reference to underpinning theory (C1) | 1, 2, 3 | 3 | 1.1 (1.23) | 20 |
| Targeting of relevant theoretical constructs (C2) | 2, 5, 6, 7, 8, 9, 10, 11 | 8 | 2.0 (2.43) | 17 |
| Using theory to select recipients or tailor interventions (C3) | 4, 6 | 2 | 0.1 (0.26) | 2 |
| Measurement of constructs (C4) | 12a, 12b | 2 | 0.5 (0.86) | 11 |
| Testing of theory: mediation effects (C5) | 12a, 12b, 13, 14a, 14b, 14c, 14d, 15, 16 | 9 | 1.6 (2.83) | 14 |
| Refining theory (C6) | 17a, 17b | 2 | ‐ | ‐ |
| Total use of theory | All items | 22 | 4.4 (5.43) | 20 |
Unadjusted associations between use of theory and intervention effectiveness
The relationship between reported theory use and intervention effectiveness is reported in Table 7 for the unadjusted meta‐regression analyses. Items 4, 6, 9, 14b, 17a and 17b were not included because the item was not present in more than 10% of the included trials.
| Theory Coding Scheme covariates (item/category number) | B (SE) | P | 95% CI | Adj. R² | I² | |
| Lower bound | Upper bound | |||||
| Theory/model of behaviour mentioned (I1) | 9.73 (14.63) | 0.510 | ‐19.84 | 39.31 | ‐4.90% | 78.09% |
| Targeted construct mentioned as predictor of behaviour (I2) | 24.17 (14.09) | 0.094 | ‐4.30 | 52.64 | 2.27% | 78.13% |
| Intervention based on single theory (I3) | 12.92 (17.60) | 0.467 | ‐22.64 | 48.49 | ‐4.44% | 78.08% |
| Theory/predictors used to select recipients | Not present in > 10% of studies | |||||
| Theory/predictors used to select/develop | 18.25 (14.57) | 0.218 | ‐11.20 | 47.69 | ‐3.43% | 78.15% |
| Theory/predictors used to tailor intervention techniques | Not present in > 10% of studies | |||||
| All intervention techniques are explicitly linked to at least | ‐3.73 (19.91) | 0.852 | ‐43.98 | 36.51 | ‐4.86% | 76.50% |
| At least one, but not all, of the intervention techniques are | 26.39 (15.34) | 0.093 | ‐4.60 | 57.39 | 10.54% | 77.49% |
| Group of techniques are linked to a group of | Not present in > 10% of studies | |||||
| All theory‐relevant constructs/predictors are explicitly | 8.53 (19.81) | 0.673 | ‐31.60 | 48.46 | ‐5.82% | 78.14% |
| At least one, but not all, of the theory‐relevant | 18.79 (15.99) | 0.247 | ‐13.54 | 51.11 | ‐3.45% | 78.15% |
| Theory‐relevant constructs are measured: | ‐14.67 (15.81) | 0.359 | ‐46.62 | 17.28 | 1.42% | 76.37% |
| Theory‐relevant constructs are measured: | ‐13.78 (16.88) | 0.419 | ‐47.90 | 20.33 | ‐1.67% | 76.94% |
| Changes in measured theory‐relevant | ‐33.04 (17.48) | 0.066 | ‐68.37 | 2.28 | 16.92% | 74.82% |
| Mediational analysis of constructs/ predictors: | ‐7.77 (20.24) | 0.703 | ‐48.68 | 33.15 | ‐3.13% | 76.43% |
| Mediational analysis of constructs/ predictors: | Not present in > 10% of studies | |||||
| Mediational analysis of constructs/ predictors: | ‐21.88 (24.11) | 0.370 | ‐70.61 | 26.86 | 4.48% | 75.41% |
| Mediational analysis of constructs/ predictors: | ‐7.77 (20.24) | 0.703 | ‐48.68 | 33.14 | ‐3.13% | 76.43% |
| Results discussed in relation to theory (I15) | 1.59 (16.08) | 0.922 | ‐30.91 | 34.08 | ‐6.81% | 77.35% |
| Appropriate support for theory (I16) | ‐8.73 (19.43) | 0.656 | ‐48.01 | 30.55 | ‐2.11% | 76.33% |
| Results used to refine theory: | Not present in > 10% of studies | |||||
| Results used to refine theory: | Not present in > 10% of studies | |||||
| Reference to underpinning theory (C1) | 7.19 (5.89) | 0.230 | ‐4.72 | 19.10 | ‐1.55% | 78.08% |
| Targeting of relevant theoretical constructs (C2) | 3.94 (2.97) | 0.192 | ‐2.06 | 9.93 | ‐4.08% | 78.12% |
| Using theory to select recipients or tailor interventions (C3) | 13.30 (27.27) | 0.628 | ‐41.81 | 68.42 | ‐7.21% | 77.67% |
| Measurement of constructs (C4) | ‐7.58 (8.41) | 0.373 | ‐24.58 | 9.42 | 0.19% | 76.61% |
| Testing of theory: mediation effects (C5) | ‐2.09 (2.53) | 0.413 | ‐7.20 | 3.02 | 2.29% | 75.71% |
| Refining theory (C6) | No score > 0 for any studies | |||||
| Total use of theory | 0.39 (1.37) | 0.778 | ‐2.38 | 3.15 | ‐7.46% | 77.58% |
The results indicated that the Theory Coding Scheme items, categories of theory use and total use of theory score explained little of the heterogeneity observed. No significant associations were detected between the Theory Coding Scheme covariates and intervention effectiveness (P > 0.076). It should be noted that the items refer to theory use as reported in publications.
The following Theory Coding Scheme items explained the greatest amount of heterogeneity: changes in measured theory‐relevant constructs/predictor (item 13; 16.92%), at least one of the intervention techniques are explicitly linked to at least one theory‐relevant construct (item 8; 10.54%), total use of theory score (‐7.46%), using theory to select recipients or tailor interventions (category 3; ‐7.21%), and results discussed in relation to theory (item 15; ‐6.81%).
Multivariable associations between use of theory and intervention effectiveness
A multivariable model was constructed using the covariates (item 2, item 8 and item 13) that had a modest association with effect size (B > 23) in the unadjusted models. Relationships between reported theory use and intervention effectiveness are reported in Table 8 (I² = 74.3%; adjusted R² = 32.9%). Two significant independent associations were detected between intervention effectiveness and Theory Coding Scheme items; targeted construct mentioned as predictor of behaviour (item 2, B = 50.82, P = 0.020) and changes in measured theory‐relevant constructs/predictor (item 13, B = ‐61.41, P = 0.003) (Table 8). However, these are difficult to interpret in the absence of any significant associations in the unadjusted models and the pattern of results is not robust to standardised effect sizes or slight changes to studies included.
| Theory Coding Scheme covariates (item number) | B (SE) | P | 95% CI | |
| Lower bound | Upper bound | |||
| Targeted construct mentioned as predictor of behaviour (I2) | 50.82 (21.00) | 0.020 | 8.31 | 93.34 |
| At least one, but not all, of the intervention techniques are | ‐12.19 (20.71) | 0.560 | ‐54.12 | 29.74 |
| Changes in measured theory‐relevant constructs/predictor (I13) | ‐61.41 (19.42) | 0.003 | ‐100.71 | ‐22.10 |
There was no apparent difference among studies within and without the primary meta‐analysis in terms of prevalence of theory items.
Summary of economic studies
A narrative synthesis of economic assessment is provided because there were only few economic evaluations and significant heterogeneity in these studies.
Seven studies reporting economic data met the inclusion criteria. These fall into three categories: four studies were economic evaluations alongside clinical trials (Blankers 2012; Khadjesari 2014; Kruger 2014; Schulz 2014a), one stand‐alone modelling evaluation (Smit 2011), and two studies measured costs and benefits (Essex 2014; Hester 2006).
All seven studies took place in developed Western countries (3 in the UK, 3 in the Netherlands, and 1 discussed tools developed in the USA). The Drummond Checklist was used to assess study quality (Drummond 2005). There was some variation in study quality; with four rated at high quality, two at moderate quality, and one weak quality study. The main criticisms were insufficient economic analysis or description of an intervention.
There was significant variation in the types of intervention and control groups utilised in the studies. The four studies reporting economic evaluations alongside a clinical trial compared internet‐based therapy to internet‐based self‐help (Blankers 2012); receiving immediate personalised feedback related to alcohol consumption with opportunity for a more extended intervention to delayed feedback of three months (Khadjesari 2014); an online tool to help students in the month before they started university to access resources and information about a healthy lifestyle compared to doing nothing (Kruger 2014); and receiving personalised advice online on two health related behaviours to receiving generic advice (Schulz 2014a). The modelling study (Smit 2011) compared usual care with three different e‐health interventions related to alcohol: two self‐help and one internet‐based therapy. The study exploring the feasibility of EQ‐5D‐3L as an outcome measure (Essex 2014) compared an online tool offering enhanced psychological advice to one offering standard information related to alcohol consumption only. The EQ‐5D‐3L is a generic health‐related quality of life measure that asks individuals about five dimensions of their health: mobility, self‐care, pain/discomfort, usual activities, and anxiety. In the three level questionnaire the options are none/some/a lot. Index based values or utilities are a major feature of the EQ‐5D‐3L instrument which can be used for the calculation of quality adjusted life years (QALYs) which is used to inform economic evaluations of healthcare interventions (Devlin 2010). The study looking at costs of interventions was purely descriptive (Hester 2006). Hester 2006 listed the costs of different software programmes for delivering digital alcohol interventions and other costs such as staff training, software maintenance, and incorporating into practice that are associated with implementing this intervention. Other studies (such as Blankers 2012; Kruger 2014; Schulz 2014a; Smit 2011) used EQ‐5D as a benefit measure in an analysis of an internet‐based brief alcohol intervention and identified a meaningful change in QALYs leading to reports that the interventions had significant effects.
There was some variation in the length of the study period; one study had a three month follow‐up period (Khadjesari 2014), two studies with six months follow‐up (Blankers 2012; Kruger 2014), two studies with 12 months follow‐up (Essex 2014; Smit 2011), and one study with 24 months follow‐up (Schulz 2014a).
Of the five studies exploring cost‐effectiveness (Blankers 2012; Khadjesari 2014; Kruger 2014; Schulz 2014a; Smit 2011), all except Khadjesari 2014 found the intervention cost‐effective compared to the control group. Three studies (Blankers 2012; Kruger 2014; Schulz 2014a) performed cost‐effectiveness analyses where cost‐effectiveness was measured by incremental cost‐effectiveness ratios (ICERs) and the benefit measure was QALYs estimated from the EQ‐5D. Smit 2011 estimated cost‐effectiveness using ICERs but the benefit measure used in this study was disability‐adjusted life years. Khadjesari 2014 performed a cost‐analysis focusing only on costs of healthcare utilisation and costs to the employer, and not on benefits to the individual, which may be why this study did not find the intervention to be cost‐effective. Two studies (Schulz 2014a; Smit 2011) found that the point estimates were sensitive to how the parameters were defined in the model, although the intervention dominated in all model specifications. Essex 2014, which explored the value of EQ‐5D‐3L as an outcome measure, found it may not be an appropriate primary outcome measure for clinical and cost‐effectiveness in trials of harmful and hazardous drinking because it was only weakly correlated with the amount of alcohol consumed.
There was no evidence to suggest that the length of the intervention impacted on cost‐effectiveness. There was no evidence to suggest that the specific type of internet‐based or digital intervention impacted on cost‐effectiveness. However, the sample sizes may be too small to draw any definitive conclusions on the cost‐effectiveness by type of digital interventions.
Discussion
Summary of main results
We found moderate‐quality evidence that digital interventions may be superior to either no intervention or minimal input controls, and that digital interventions typically led to a reduction in alcohol consumption of approximately 23 g (3 UK standard drink units) per week (summary of findings Table for the main comparison). There was considerable heterogeneity in these findings, although heterogeneity was lower among trials of adolescents, young adults or college students. Sensitivity analyses which removed studies at high risk of bias suggested that the reduction in consumption may be closer to 11 g (1.5 UK standard drinks) per week. We found little or no evidence of a difference in effectiveness between digital and face‐to‐face interventions (low‐quality evidence, summary of findings Table 2). Limited economic evidence suggested that digital interventions may be cost‐effective compared to no intervention. No evidence was found to suggest this was dependent on duration or type of intervention, but the evidence base was too small to draw definitive conclusions.
The behaviour change techniques (BCTs) of behaviour substitution, problem solving and credible source were associated with the effectiveness of digital interventions to reduce alcohol consumption and warrant further investigation in experimental research. Behaviour substitution, defined as "prompt substitution of the unwanted behaviour with a wanted or neutral behaviour” and problem solving, defined as “analyse, or prompt the person to analyse, factors influencing the behaviour and generate or select strategies that include overcoming barriers and/or increasing facilitators” (Michie 2013), are recommended by guidance documents and treatment manuals for use in alcohol reduction (Michie 2012) and have been widely used in a variety of health behaviour change interventions (Abood 2003; Araújo‐Soares 2009; Fitzgibbon 2008; Gardner 2016; Webster 2015). These BCTs may be effective in digital alcohol interventions because they help people who are otherwise engaged in self‐directed behaviour change generate practical and specific ways of meeting their drinking reduction goals.
Credible source, defined as “present verbal or visual communication from a credible source in favour of or against the behaviour” (Michie 2013), generally consisted of advice about national guidelines for consumption, or advice about drinking provided by a member of the study. Evidence from this review and from a review of the BCTs in alcohol‐reduction apps (Crane 2015) suggests that people may value guidance from a credible source about the maximum amount of alcohol they should consume. Further investigation of the effectiveness of providing such information in digital interventions is warranted. The small number of interventions available for analysis and the infrequent use of many BCTs (70 of the 93 were used fewer than 4 times), meant that the effects of most BCTs could not be evaluated. Other BCTs were used so frequently (feedback on behaviour and social comparison were both present in more than 80% of trials) as to reduce the ability to evaluate their effectiveness.
The reporting of theory use in the development or evaluation of digital alcohol interventions was very limited and often unclear when present. Half of all interventions made no reference to any theories of behaviour and only a third used theories to develop the intervention. This limited reporting of theory use was unrelated to heterogeneity in intervention effectiveness. This meta‐regression analysis had limited power, which means the current literature is insensitive to addressing the more general question of whether good quality use of theory in designing digital alcohol interventions may be associated with more effective interventions.
The meta‐analysis of quantity of alcohol consumed was based on means, rather than (for example) medians, which might be more appropriate if the data were very heavily skewed. Whilst the distribution of alcohol consumption was skewed toward lower values, the skewness was not extreme owing to the exclusion of participants screened as abstinent or dependent drinkers.
The meta‐analysis was restricted to analyses of separate outcome measures, rather than combining results for each outcome measure. This was because it was unclear a priori whether the intervention would influence all of the outcome measures considered, nor whether ‐ as is implicit in analyses of standardised mean differences ‐ the difference in the mean outcome measure between intervention and control groups would be related to the standard deviation of the outcome measure.
Overall completeness and applicability of evidence
Findings of this review suggest that digital interventions are better than no intervention (or minimal input controls) at reducing weekly alcohol consumption in unselected or student populations who are drinking at hazardous or harmful levels. These results are not applicable to lighter or low‐risk drinkers or to treatment‐seeking populations, since the trials did not include these people. Dependent or addicted drinkers were not the focus of these trials, although in some cases, they comprised a proportion of participants due to a lack of upper consumption cut‐offs in eligibility criteria. Most included trials tested web‐based interventions, so the effectiveness of other types of interventions such as smartphone apps or SMS messages is less clear. None of the trials took place in developing countries; and although many of the trials recruited participants online, there was no evidence from study baseline characteristics that many resided in developing countries.
The primary meta‐analysis was based on the longest reported follow‐up time point of the trials, which ranged from one month to one year. When subgroup analyses based on the actual length of follow‐up were conducted, we found that the positive effect of digital interventions at reducing alcohol consumption persisted to six months but not to one year. There were fewer trials with longer term follow‐up points and so this analysis may not have had the statistical power to detect smaller effect sizes. However, it is likely that intervention effects will decay, or reduce over time. Thus repeated engagement with digital programmes may need to occur if positive effects of the intervention programmes are to be maintained over time. There was limited information reported in this literature about the extent to which participants engaged with the digital programmes or whether they returned to re‐engage after initial use.
Few trials have been carried out comparing digital interventions to face‐to‐face interventions, but those conducted to date suggest little difference in terms of their impact on consumption. More research is required to provide a more definitive conclusion; however, a non‐inferiority trial is currently underway (Struzzo 2013). Nevertheless, an ongoing qualitative systematic review investigating factors affecting whether and how people engage with digital interventions suggests that user perceptions about the usefulness and relevance of intervention content, as well as participants' preferences regarding how interventions are delivered, may influence the outcome of digital alcohol interventions (Beyer 2015). It is plausible that the overall lack of evidence of difference in effectiveness between face‐to‐face and digital interventions may mask differences between subgroups within populations ‐ some of whom tend to engage and have better outcomes when interacting with another person, and others who prefer the privacy or convenience of, and respond better to, interventions via digital devices. Face‐to‐face interventions did not feature in any of the economic studies in this review. However, it is reasonable to assume that digital interventions may be more cost‐effective than directly delivered interventions if they have a similar impact on consumption. After their initial development and set‐up are accounted for, digital interventions are likely to be cheaper to deliver at scale, more consistent in terms of content delivery, and accessible multiple times compared to a face‐to‐face intervention. Conversely, it may be challenging to ensure that users access only high‐quality digital programmes available via web‐based programmes or smartphone apps. Furthermore, it is not possible to ensure that users engage with all aspects of a remotely delivered intervention programme.
We looked for evidence that digital interventions could help to address socio‐economic inequalities in access to help for alcohol information, advice, or online counselling. We specifically looked for data relating to trial participants that directly measured or could be used as a proxy for socio‐economic status; these were income, ethnicity, employment or educational attainment. Although many trials reported one or more of these characteristics at baseline, very few reported outcomes on the basis of these characteristics at follow‐up. Thus there were insufficient data to enable subgroup analysis by socio‐economic status. Most trials (n = 29) involved university or college student participants and so were likely to reflect data for people from higher economic status backgrounds. Although ethnicity was better reported at baseline in these trials, most trial participants were categorised as white.
Quality of the evidence
The direction of evidence was broadly consistent: most (88%) of the 41 included trials in the primary meta‐analysis reported that participants using a digital intervention reduced their consumption compared to no or minimal intervention groups.
A positive feature of these digital intervention trials is that most procedures are fully automated and so there was typically a low risk of bias regarding randomisation procedures, allocation to different conditions and intervention delivery. It is impossible to blind participants to these types of behaviour change interventions, and although some trialists made attempts to counter the impact of this aspect, performance bias is an inescapable issue in trials of this kind. Although it has been argued that small effect sizes may be caused entirely by exaggerated self‐report of outcome measures by unblinded participants (Hróbjartsson 2014), the sensitivity analysis conducted in this review of studies at low risk of performance bias (Analysis 1.7) suggested that the intervention caused a real effect. Most included trials relied on self‐reported measures of alcohol use at enrolment and follow‐up, so this literature could be subject to recall bias or socially desirable responding. However, most of the trials used well validated screening tools to determine levels of alcohol consumed, typically the Alcohol Use Disorders Identification Test (AUDIT) or one of its shorter variants. These tools have been shown to have good sensitivity and specificity when measured against a range of diagnostic gold standard measures (Reinert 2007). Moreover, AUDIT has been shown to have higher sensitivity, specificity, and positive predictive value than biochemical markers in primary care (Coulton 2006). Finally, any potential bias due to self‐reported consumption will affect both intervention and control groups (particularly where control groups received alcohol‐related information) and so were unlikely to account for differential intervention effects. Blinding of providers was not an issue in most trials because outcome data collection was automated. However, this same automated procedure made it very difficult to ensure good follow‐up, and attrition is another source of bias in this group of trials (only 44% of trials were judged to be at low risk of bias for this domain). It seems likely that participants who were lost to follow‐up stopped using the intervention, but it is impossible to gauge whether these people would have been more or less likely to benefit than completers had they continued in the trial. There could be a potential risk of detection bias in the trials due to participants self‐reporting their alcohol consumption, but this was likely to have been similar between intervention and control participants in the same trial and so unlikely to differentially affect study findings. In trials which included a face‐to‐face arm, there was a higher risk of detection bias because the intervention was provided by a researcher or clinician.
We downgraded the evidence from high‐quality to moderate‐quality due to high levels of risk of performance and attrition bias. Both performance and attrition bias are very difficult to mitigate in this type of intervention because participants cannot easily be blinded to receiving this type of intervention and follow‐up is more difficult when the intervention is received remotely without any interaction with trial personnel. However, given that the direction of effect was broadly consistent (at least 88% of trials reported a decrease in consumption in the intervention compared to the control arm for quantity and frequency; 73% for intensity), and all the sensitivity analyses accounting for risk of bias suggested that the effect was real, if potentially smaller than in the primary meta‐analysis, the addition of further trials seems unlikely to alter the direction of effect. With a large body of evidence mostly pointing in the same direction, we judged the most appropriate GRADE assignment to be moderate‐quality evidence.
There were high levels of heterogeneity in the analyses for quantity and intensity of drinking, but this was explained. In large part this heterogeneity was likely due to differences in the content and delivery of the interventions ‐ some early trials included digital devices that have since become almost obsolete (e.g. CD‐ROMS) and new technologies have evolved rapidly over the last decade. Also, subgroup analysis suggested that much of this heterogeneity was associated with trials involving older adults (Analysis 1.3; Figure 4).
The trials comparing digital with face‐to‐face interventions were all very small and for each of the outcomes totaled fewer than 400 participants, so we downgraded the quality of evidence for imprecision (low‐quality evidence).
Potential biases in the review process
We made every effort to minimise the publication bias that can arise because studies reporting positive effects are more likely to be published than those with negative or equivocal results. We searched a range of bibliographic databases alongside sources of unpublished literature, but it is possible that the search strategy missed studies. We also assessed the potential bias from selective reporting by inspecting the difference between the outcomes which were stated in study protocols (where available) or methods sections, and those in the final study report; these judgements are in the Risk of Bias tables. The funnel plot suggests that smaller studies showing little or no evidence of effect may have been missed, although inspection of funnel plots may not to be a robust indication of publication bias when there is significant heterogeneity (as in the current review) (Mavridis 2014; Terrin 2005). We contacted study authors where possible to obtain missing data, and we carried out sensitivity analyses in which missing values were imputed where required. These analyses suggested that the effect of digital interventions is robust, albeit small.
Study authors were also contacted for further detail for the BCT and theory coding assessment. However, recognised issues with the incomplete reporting of intervention content (Abraham 2008) may have resulted in BCTs being incorrectly coded as present or absent. This may produce noise and undermine the power to test associations. Simply recording a BCT as present or absent does not take into account the frequency, intensity or the quality in which it was delivered. For example, it is unclear to what extent individuals may need to self‐monitor their consumption of alcohol. The quality of implementation may be particularly critical in digital interventions where different language, graphic design or usability of the BCT implementation could have a considerable effect on the degree of user engagement (Garrett 2010). To assess BCT effectiveness it may be necessary to develop methods to measure its ‘dose’ (Lorencatto 2015; Voils 2014).
Although there is no evidence that reporting of theory use is associated with substantial heterogeneity among interventions, the current literature is insensitive to addressing the more general question of whether good quality use of theory in designing digital alcohol interventions may be associated with more effective interventions. Previous simulation studies have found that more than 200 studies are required for 80% power (Hempel 2013). We cannot draw a conclusion about whether an association does not exist or whether there was insufficient power to detect one.
Funding for included studies was obtained mostly from government grants or research foundations, where reported. One third of studies did not report their source of funding.
Agreements and disagreements with other studies or reviews
Digital alcohol interventions
During the conduct of our current review we identified 19 published systematic reviews focused on digital alcohol interventions (Balhara 2014; Bewick 2008a; Bhochhibhoya 2015; Black 2016; Carey 2009a; Carey 2012; Dedert 2015; Donoghue 2014; Dotson 2015; Elliott 2008; Khadjesari 2011; Nair 2015; Newman 2011; Riper 2011; Riper 2014; Rooke 2010; Vernon 2010; White 2010; Zisserson 2007), although the precise target groups or types of technology varied among reviews. Five of these systematic reviews were published in the last two years (Bhochhibhoya 2015; Black 2016; Dedert 2015; Dotson 2015; Nair 2015). The most recent systematic review included 94 computer‐delivered interventions (Black 2016). Enrolled participants had a median age of 20 years and the median proportion of women was 55%; it was not clear how many participants were included in the analysis (Black 2016). Black 2016 reported small, significant effects across five outcomes (total consumption or quantity, e.g. drinks/week; average consumption or intensity, e.g. drinks/drinking per day; peak consumption e.g. maximum consumption/occasion; frequency of heavy episodic (binge) drinking; or frequency of drinking any amount, d + = 0.07 to 0.15) in an analysis considering all time points.
The current review differed from the most recent review (Black 2016) with respect to inclusion criteria (e.g. we excluded trials where interventions were mandated or participants were not screened as hazardous or harmful drinkers), and there are only 27 trials common to both reviews. Our primary meta‐analysis included 41 trials with 19,241 participants, whose median age was 20 years (IQR 19 to 31 years) across 28 studies that reported participants' age, and our median proportion of females was 51% across 34 studies that reported participants' gender. We found a reduction of 22.8 g (95% CI 15.4 to 30.3) of alcohol per week (approximately 2 USA or 3 UK standard drink units) less than controls. The standardised effect size calculated for this consumption change, based on longest follow‐up, was 0.20 (95% CI 0.14 to 0.27; I² = 74%). Thus, our finding of modest weekly reduction in the amount of alcohol consumed which equated to a small effect size is in line with other recent reports in terms of changes in consumption.
Black 2016 also assessed BCTs of included interventions and found that, in contrast to our review, the BCTs of commitment, social comparison, feedback and review of goals were associated with better outcomes. The more recent and extensive 93‐item taxonomy (Michie 2013; Michie 2015) used in our meta‐analysis differs in a number of ways from the 42‐item, alcohol‐specific, taxonomy (Michie 2012) used by Black 2016. The 93‐item taxonomy is more fine grained and includes a BCT of credible source (in contrast to the 42‐item taxonomy). It has three feedback BCTs, two review goal BCTs and three BCTs that provide information on negative consequences of performing a behaviour, whereas the 42‐item taxonomy only has one BCT for each of these techniques.
Our findings relating to theory also differ from Black 2016, which found that the Social Norms approach was associated with improved outcomes although no association between the extent of theory use and effectiveness was found. Black 2016 and the current review differed in terms of the criteria used for including covariates in the adjusted meta‐regression model. Black 2016 used the criterion of significant P values, which could be altered by using an unadjusted or adjusted model. The criterion we used of size of B value is more stable during adjustment and therefore a more reliable method.
All of the systematic reviews cited above which were published since 2011 reported that digital interventions can be successful in reducing hazardous alcohol consumption compared to assessment only, and two (Dotson 2015; Riper 2014) suggested that although the effect is small, large‐scale implementation may be cost‐effective from a public health perspective. Many of these reviews focused on students, but had different inclusion criteria to each other and to this review with respect to participant consumption levels, included interventions, and whether the students were mandated to 'complete' the intervention. Reviews published before 2011 were more tentative in their conclusions (presumably due to having fewer trials available), but all of them reported 'some' evidence of effectiveness or that interventions 'may' reduce alcohol consumption, except for one (Bewick 2008a) which reported inconsistent results.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Funnel plot of comparison 1: Digital intervention vs. control, outcome 1.1: Quantity of drinking (g/week), based on longest follow‐up
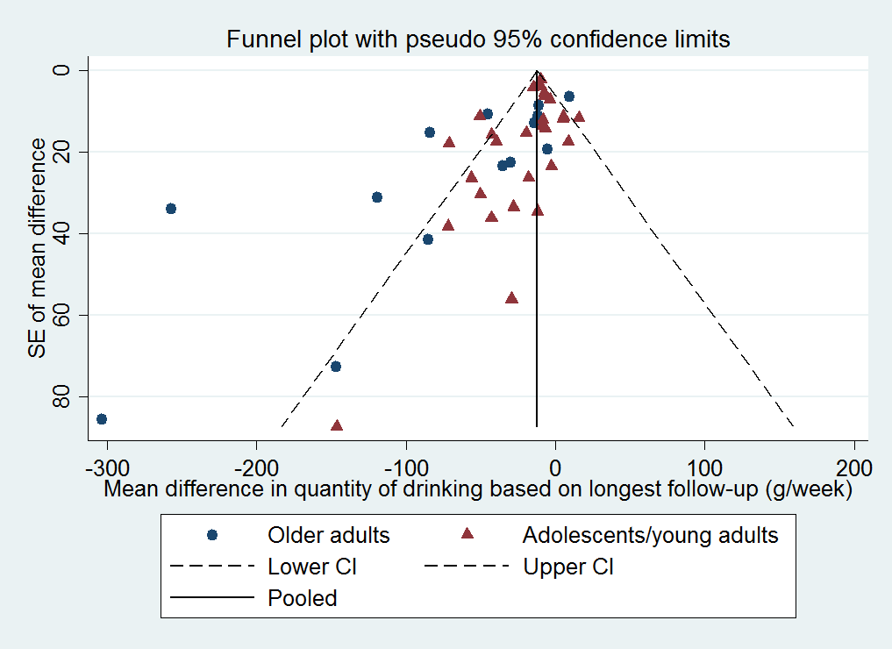
Funnel plot of comparison 1: Digital intervention vs. control, outcome 1.6: Quantity of drinking (g/week), based on longest follow‐up and categorised on whether restricted to adolescents or young adults

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 1 Quantity of drinking (g/week), based on longest follow‐up.
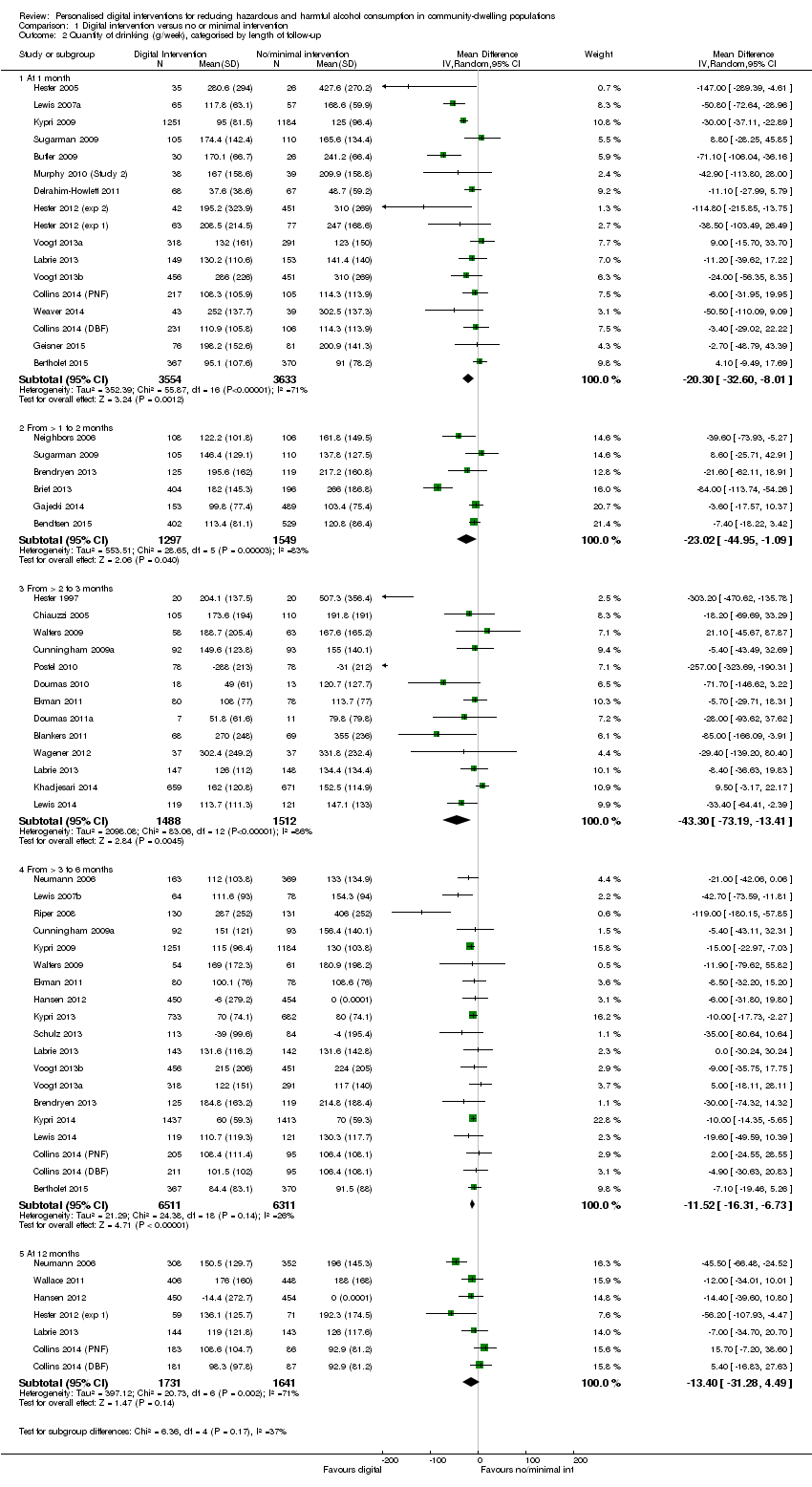
Comparison 1 Digital intervention versus no or minimal intervention, Outcome 2 Quantity of drinking (g/week), categorised by length of follow‐up.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 3 Quantity of drinking (g/week), based on longest follow‐up and categorised on whether restricted to adolescents or young adults.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 4 Quantity of drinking (g/week), categorised by length of follow‐up and restricted to trials of adolescents/young adults.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 5 Quantity of drinking (g/week), based on longest follow‐up and categorised by gender.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 6 Quantity of drinking (g/week), based on longest follow‐up and omitting trials at high risk of bias owing to incomplete data.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 7 Quantity of drinking (g/week), based on longest follow‐up and omitting trials at high risk of performance bias.
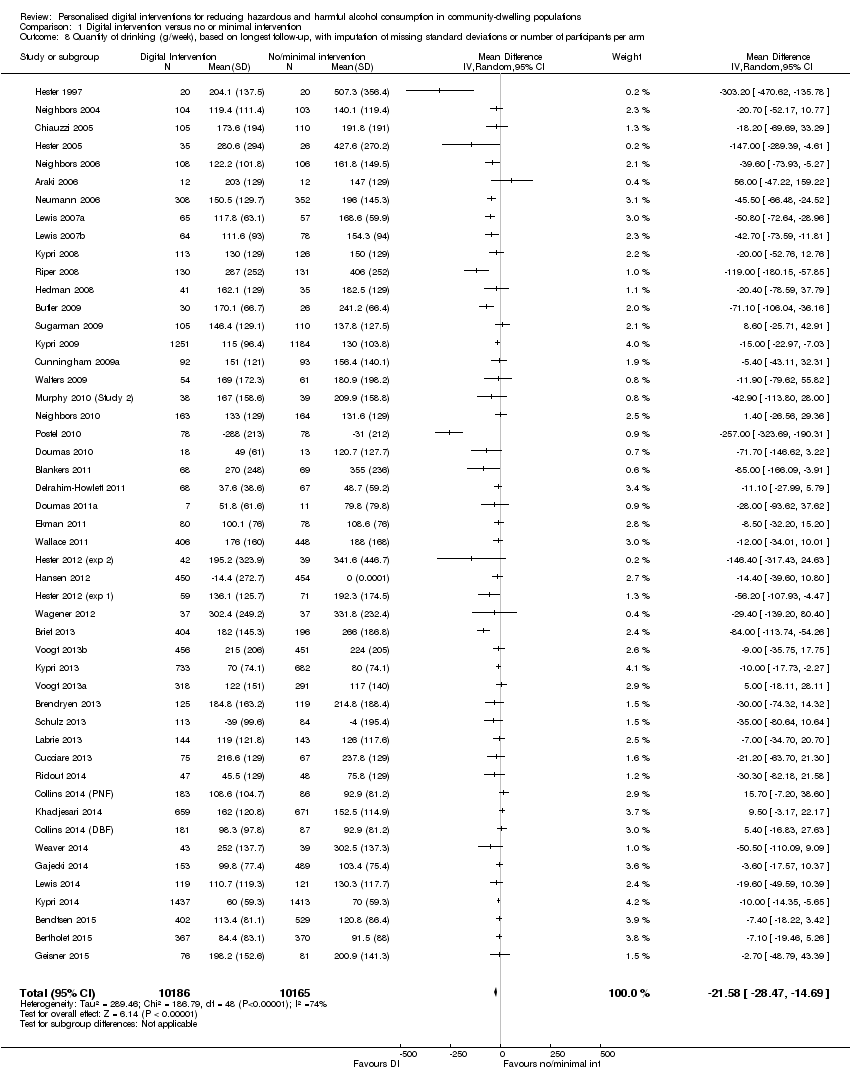
Comparison 1 Digital intervention versus no or minimal intervention, Outcome 8 Quantity of drinking (g/week), based on longest follow‐up, with imputation of missing standard deviations or number of participants per arm.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 9 Quantity of drinking (g/week), categorised by length of follow‐up, with imputation of missing standard deviations or number of participants per arm.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 10 Frequency of drinking (no. of days drinking/week), based on longest follow‐up.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 11 Frequency of binge drinking (no. of binges/week), based on longest follow‐up.
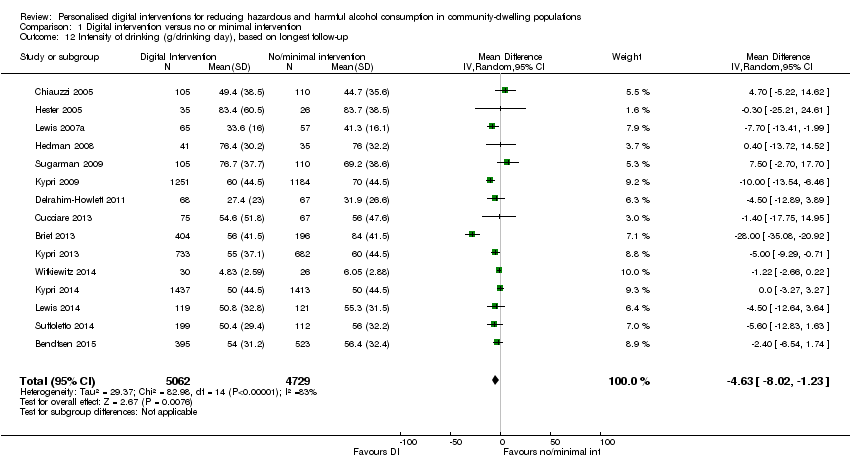
Comparison 1 Digital intervention versus no or minimal intervention, Outcome 12 Intensity of drinking (g/drinking day), based on longest follow‐up.

Comparison 1 Digital intervention versus no or minimal intervention, Outcome 13 Binge drinkers, based on longest period of follow‐up.

Comparison 2 Digital intervention versus face‐to‐face intervention, Outcome 1 Quantity of drinking (g/week), based on longest follow‐up.

Comparison 2 Digital intervention versus face‐to‐face intervention, Outcome 2 Quantity of drinking (g/week), categorised by length of follow‐up.

Comparison 2 Digital intervention versus face‐to‐face intervention, Outcome 3 Frequency of drinking (no. of days drinking/week), based on longest follow‐up.

Comparison 2 Digital intervention versus face‐to‐face intervention, Outcome 4 Frequency of binge drinking (no. of binges/week), based on longest follow‐up.
| Digital intervention compared to no or minimal intervention for reducing hazardous and harmful alcohol consumption in community‐dwelling populations | ||||||
| Patient or population: People living in the community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no or minimal intervention | Risk with digital intervention | |||||
| Quantity of drinking (g/week), based on longest follow‐up (quantity) | The mean quantity of drinking (g/week), based on longest follow‐up was 176 g/week | MD 23 g/week lower | ‐ | 19,241 | ⊕⊕⊕⊝ | Heterogeneity was substantial (78%) but not unexplained; interventions differed in content and delivery. The direction of effect favoured the intervention in 88% of the studies. |
| Frequency of drinking (number of days drinking/week), based on longest follow‐up (frequency) | The mean frequency of drinking (number of days drinking/week), based on longest follow‐up was 2.5 drinking days/week | MD 0.16 drinking days/week lower | ‐ | 10,862 | ⊕⊕⊕⊝ | |
| Frequency of binge drinking (number of binges/week), based on longest follow‐up | The mean frequency of binge drinking (number of binges/week), based on longest follow‐up was 1.2 binges/week | MD 0.24 binges/week lower | ‐ | 3587 | ⊕⊕⊕⊝ | Heterogeneity was moderate (53%) but not unexplained; interventions differed in content and delivery. The direction of effect favoured the intervention in 93% of the studies. |
| Intensity of drinking (g/drinking day), based on longest follow‐up (intensity) | The mean intensity of drinking (g/drinking day), based on longest follow‐up was 56 g/drinking day | MD 5 g/drinking day lower | ‐ | 9791 | ⊕⊕⊕⊝ | Heterogeneity was substantial (78%) but not unexplained; interventions differed in content and delivery. The direction of effect favoured the intervention in 73% of the studies. |
| Adverse events | Not reported | Not reported | ‐ | ‐ | ‐ | No studies assessed this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded due to high risk of attrition or performance bias or both in many studies. A sensitivity analysis based on the primary meta‐analysis, which omitted studies at high risk of performance bias and contained 11 studies, suggested that the intervention led to a reduction of at least 11 g alcohol (7 to 14 g) or 1.5 UK units (Analysis 1.7). | ||||||
| Digital intervention compared to face‐to‐face intervention for reducing hazardous and harmful alcohol consumption in community‐dwelling populations | ||||||
| Patient or population: People living in the community | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with face‐to‐face intervention | Risk with digital intervention | |||||
| Quantity of drinking (g/week), based on longest follow‐up (quantity) follow up: range 1 month to 12 months | The mean quantity of drinking (g/week), based on longest follow‐up was 180 g/week | MD 0.52 g/week higher | ‐ | 390 | ⊕⊕⊝⊝ | |
| Frequency of drinking (number of days drinking/week), based on longest follow‐up (frequency) follow up: range 1 months to 12 months | The mean frequency of drinking (no. of days drinking/week), based on longest follow‐up was 1.85 drinking days/week | MD 0.05 drinking days/week higher | ‐ | 58 | ⊕⊕⊝⊝ | |
| Frequency of binge drinking (number of binges/week), based on longest follow‐up | The mean frequency of binge drinking (no. of binges/week), based on longest follow‐up was 0.7 binges/week | MD 0.04 binges/week higher | ‐ | 206 | ⊕⊕⊝⊝ | |
| Intensity of drinking (g/drinking day) | Not reported | Not reported | ‐ | ‐ | ‐ | No studies assessed this outcome. |
| Adverse events | Not reported | Not reported | ‐ | ‐ | ‐ | No studies assessed this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias (high risk of attrition or performance bias or both). 2 Downgraded one level due to serious imprecision (fewer than 400 participants). | ||||||
| Behaviour change technique | % age (N) |
| 2.2. Feedback on behaviour | 85.7% (36) |
| 6.2. Social comparison | 81.0% (34) |
| 5.3. Information about social and environmental consequences | 71.4% (30) |
| 2.7. Feedback on outcome(s) of behaviour | 69.0% (29) |
| 3.1. Social support (unspecified) | 64.3% (27) |
| 4.1. Instruction on how to perform the behaviour | 52.4% (22) |
| 2.6. Biofeedback | 50.0% (21) |
| 5.2. Salience of consequences | 50.0% (21) |
| 9.2. Pros and cons | 35.7% (15) |
| 1.2. Problem solving | 33.3% (14) |
| 5.1. Information about health consequences | 33.3% (14) |
| 1.4. Action planning | 31.0% (13) |
| 9.1. Credible source | 31.0% (13) |
| 1.1. Goal setting (behaviour) | 28.6% (12) |
| 2.3. Self‐monitoring of behaviour | 26.2% (11) |
| 3.2. Social support (practical) | 16.7% (7) |
| 2.4. Self‐monitoring of outcome(s) of behaviour | 14.3% (6) |
| 4.2. Information about antecedents | 14.3% (6) |
| 1.3. Goal setting (outcome) | 11.9% (5) |
| 1.6. Discrepancy between current behaviour and goal | 11.9% (5) |
| 8.2. Behaviour substitution | 9.5% (4) |
| 12.2. Restructuring the social environment | 9.5% (4) |
| 15.4. Self‐talk | 9.5% (4) |
| 5.6. Information about emotional consequences | 7.1% (3) |
| 7.1. Prompts/cues | 7.1% (3) |
| 11.2. Reduce negative emotions | 7.1% (3) |
| 12.3. Avoidance/reducing exposure to cues for the behaviour | 7.1% (3) |
| 1.5. Review behaviour goal(s) | 4.8% (2) |
| 5.4. Monitoring of emotional consequences | 4.8% (2) |
| 10.3. Non‐specific reward | 4.8% (2) |
| 10.9. Self‐reward | 4.8% (2) |
| 1.7. Review outcome goal(s) | 2.4% (1) |
| 1.8. Behavioural contract | 2.4% (1) |
| 3.3. Social support (emotional) | 2.4% (1) |
| 4.4. Behavioural experiments | 2.4% (1) |
| 8.1. Behavioural practice/rehearsal | 2.4% (1) |
| 8.7. Graded tasks | 2.4% (1) |
| 10.4. Social reward | 2.4% (1) |
| 10.6. Non‐specific incentive | 2.4% (1) |
| 13.2. Framing/reframing | 2.4% (1) |
| 14.2. Punishment | 2.4% (1) |
| 15.1. Verbal persuasion about capability | 2.4% (1) |
| 15.3. Focus on past success | 2.4% (1) |
| The following behaviour change techniques were not used in any digital intervention: 1.9. Commitment, 2.1. Monitoring of behaviour by others without feedback, 2.5. Monitoring of outcome(s) of behaviour without feedback, 4.3. Re‐attribution, 5.5. Anticipated regret, 6.1. Demonstration of the behaviour, 6.3. Information about others’ approval, 7.2. Cue signalling reward, 7.3. Reduce prompts/cues, 7.4. Remove access to the reward, 7.5. Remove aversive stimulus, 7.6. Satiation, 7.7. Exposure, 7.8. Associative learning, 8.3. Habit formation, 8.5. Overcorrection, 8.6. Generalisation of target behaviour, 9.3. Comparative imagining of future outcomes, 10.1. Material incentive (behaviour), 10.2. Material reward (behaviour), 10.5. Social incentive, 10.7. Self‐incentive, 10.8. Incentive (outcome), 10.10. Reward (outcome), 10.11. Future punishment, 11.1. Pharmacological support, 11.3. Conserving mental resources, 11.4. Paradoxical instructions, 12.1. Restructuring the physical environment, 12.4. Distraction, 12.5. Adding objects to the environment, 12.6. Body changes, 13.1. Identification of self as role model, 13.3. Incompatible beliefs, 13.4. Valued self‐identify, 13.5. Identity associated with changed behaviour, 14.1. Behaviour cost, 14.3. Remove reward, 14.4. Reward approximation, 14.5. Rewarding completion, 14.6. Situation‐specific reward, 14.7. Reward incompatible behaviour, 14.8. Reward alternative behaviour, 14.9. Reduce reward frequency, 14.10. Remove punishment, 15.2. Mental rehearsal of successful performance, 16.1. Imaginary punishment, 16.2. Imaginary reward, 16.3. Vicarious consequences. | |
| Behaviour change technique | B (SE) | P | 95% CI | I² | Adj R² | |
| 1.1 | Goal setting (behaviour) | ‐43.94 (17.14) | 0.01 | ‐78.59 to ‐9.30 | 78.05% | 6.64% |
| 1.2 | Problem solving | ‐48.03 (14.72) | < 0.01 | ‐77.79 to ‐18.27 | 74.64% | 25.01% |
| 1.3 | Goal setting (outcome) | ‐14.43 (23.46) | 0.54 | ‐61.85 to 32.99 | 77.71% | ‐2.95% |
| 1.4 | Action planning | ‐26.21 (16.58) | 0.12 | ‐59.73 to 7.30 | 77.57% | 5.45% |
| 1.6 | Discrepancy between current behaviour and goal | ‐33.88 (24.97) | 0.18 | ‐84.35 to 16.58 | 78.24% | 0.15% |
| 2.2 | Feedback on behaviour | 12.97 (21.30) | 0.55 | ‐30.08 to 56.02 | 78.31% | ‐7.13% |
| 2.3 | Self‐monitoring of behaviour | ‐30.39 (17.14) | 0.08 | ‐65.03 to 4.26 | 78.36% | 2.07% |
| 2.4 | Self‐monitoring of outcome(s) of behaviour | ‐8.60 (22.37) | 0.70 | ‐53.81 to 36.61 | 78.52% | ‐4.67% |
| 2.6 | Biofeedback | 10.81 (15.24) | 0.48 | ‐19.99 to 41.62 | 77.85% | 1.55% |
| 2.7 | Feedback on outcome(s) of behaviour | ‐4.62 (16.45) | 0.78 | ‐37.87 to 28.63 | 78.48% | ‐5.63% |
| 3.1 | Social support (unspecified) | ‐19.55 (15.39) | 0.21 | ‐50.65 to 11.55 | 78.53% | ‐0.41% |
| 3.2 | Social support (practical) | ‐26.35 (22.59) | 0.25 | ‐72.01 to 19.31 | 77.18% | 0.29% |
| 4.1 | Instruction on how to perform the behaviour | 4.46 (15.51) | 0.78 | ‐26.89 to 35.80 | 78.55% | ‐5.77% |
| 4.2 | Information about antecedents | ‐74.20 (21.53) | <0.01 | ‐117.72 to ‐30.68 | 74.91% | 32.15% |
| 5.1 | Information about health consequences | 16.75 (15.70) | 0.29 | ‐14.99 to 48.49 | 78.42% | 0.06% |
| 5.2 | Salience of consequences | 21.99 (14.86) | 0.15 | ‐8.05 to 52.02 | 78.17% | 4.92% |
| 5.3 | Information about social and environmental consequences | 28.88 (16.56) | 0.09 | ‐4.59 to 62.34 | 77.59% | 1.01% |
| 6.2 | Social comparison | 24.25 (18.95) | 0.21 | ‐14.06 to 62.56 | 78.53% | ‐4.98% |
| 8.2 | Behaviour substitution | ‐123.71 (30.14) | < 0.001 | ‐184.63 to ‐62.80 | 72.92% | 48.53% |
| 9.1 | Credible source | ‐39.89 (16.22) | 0.02 | ‐72.66 to ‐7.11 | 75.84% | 15.60% |
| 9.2 | Pros and cons | ‐30.10 (15.77) | 0.06 | ‐61.97 to 1.78 | 77.57% | 10.15% |
| 12.2 | Restructuring the social environment | ‐22.91 (31.52) | 0.47 | ‐86.62 to 40.79 | 78.56% | ‐7.66% |
| 15.4 | Self‐talk | ‐41.53 (26.37) | 0.12 | ‐94.84 to 11.77 | 77.93% | 6.04% |
| Abbreviation: B = regression coefficient Rows in italics denote BCTs demonstrating a significant association with effect size in the unadjusted analysis | ||||||
| Behaviour change technique | B (SE) | P | 95% CI | |
| 1.1 | Goal setting (behaviour) | 0.75 (19.60) | 0.97 | ‐39.40 to 40.89 |
| 1.2 | Problem solving | ‐45.92 (21.99) | 0.05 | ‐90.97 to ‐0.87 |
| 1.4 | Action planning | 30.75 (19.50) | 0.13 | ‐9.19 to 70.68 |
| 1.6 | Discrepancy between current behaviour and goal | ‐29.86 (23.97) | 0.22 | ‐78.97 to 19.25 |
| 2.3 | Self‐monitoring of behaviour | ‐6.34 (18.35) | 0.73 | ‐43.91 to 31.24 |
| 3.2 | Social support (practical) | 33.73 (21.85) | 0.13 | ‐11.03 to 78.49 |
| 4.2 | Information about antecedents | ‐43.38 (23.93) | 0.08 | ‐92.39 to 5.63 |
| 5.2 | Salience of consequences | 13.20 (14.96) | 0.39 | ‐17.55 to 43.95 |
| 5.3 | Information about social and environmental consequences | 24.64 (12.17) | 0.05 | ‐0.30 to 49.57 |
| 8.2 | Behaviour substitution | ‐95.12 (33.09) | 0.01 | ‐162.90 to ‐27.34 |
| 9.1 | Credible source | ‐32.09 (13.94) | 0.03 | ‐60.64 to ‐3.55 |
| 9.2 | Pros and cons | 6.68 (13.68) | 0.63 | ‐21.33 to 34.69 |
| 15.4 | Self‐talk | ‐8.41 (26.69) | 0.76 | ‐63.09 to 46.27 |
| Abbreviation: B = regression coefficient Rows in italics denote BCTs demonstrating a significant association with effect size in the adjusted analysis | ||||
| Theory Coding Scheme item description (item number) | N (%) of studies where item = 1 |
| Theory/model of behaviour mentioned (I1) | 21 (50%) |
| Targeted construct mentioned as predictor of behaviour (I2) | 17 (40%) |
| Intervention based on single theory (I3) | 9 (21%) |
| Theory/predictors used to select recipients for the intervention (I4) | 0 (0%) |
| Theory/predictors used to select/develop intervention techniques (I5) | 16 (38%) |
| Theory/predictors used to tailor intervention techniques to recipients (I6) | 3 (7%) |
| All intervention techniques are explicitly linked to at least one theory‐relevant construct/predictor (I7) | 6 (14%) |
| At least one, but not all, of the intervention techniques are explicitly linked to at least one theory‐relevant construct/predictor (I8) | 11 (26%) |
| Group of techniques are linked to a group of constructs/predictors (I9) | 2 (5%) |
| All theory‐relevant constructs/predictors are explicitly linked to at least one intervention technique (I10) | 7 (17%) |
| At least one, but not all, of the theory‐relevant constructs/predictors are explicitly linked to at least one intervention technique (I11) | 10 (24%) |
| Theory‐relevant constructs are measured: post‐intervention (I12a) | 12 (29%) |
| Theory‐relevant constructs are measured: post‐ and pre‐intervention (I12b) | 10 (24%) |
| Changes in measured theory‐relevant constructs/predictor (I13) | 8 (19%) |
| Mediational analysis of constructs/ predictors: mediator predicts the dependent variable (I14a) | 6 (14%) |
| Mediational analysis of constructs/ predictors: mediator predicts dependent variable, controlling for the independent variable (I14b) | 3 (7%) |
| Mediational analysis of constructs/ predictors: intervention does not predict the dependent variable when controlling the independent variable (I14c) | 4 (10%) |
| Mediational analysis of constructs/ predictors: mediated effect is statistically significant (I14d) | 6 (14%) |
| Results discussed in relation to theory (I15) | 12 (29%) |
| Appropriate support for theory (I16) | 7 (17%) |
| Results used to refine theory: adding/ removing constructs to the theory (I17a) | 0 (0%) |
| Results used to refine theory: specifying that the interrelationships between the theoretical constructs should be changed (I17b) | 0 (0%) |
| Study ID | Theories (n) | Total theory use score | TM | SRT | SCT | SLT | DMT | MIT | SNT | TPB | SIT | SCompT | SImpT | SDT | ICM | HBM | TSI | ET | CBT | PBT |
| 3 | 6 | X | X | X | ||||||||||||||||
| 3 | 6 | X | X | X | ||||||||||||||||
| 1 | 6 | X | ||||||||||||||||||
| 1 | 15 | X | ||||||||||||||||||
| 1 | 7 | X | ||||||||||||||||||
| 1 | 8 | X | ||||||||||||||||||
| 1 | 8 | X | ||||||||||||||||||
| 1 | 1 | X | ||||||||||||||||||
| 3 | 12 | X | X | X | ||||||||||||||||
| 4 | 16 | X | X | X | X | |||||||||||||||
| 3 | 14 | X | X | X | ||||||||||||||||
| 2 | 15 | X | X | |||||||||||||||||
| 1 | 12 | X | ||||||||||||||||||
| 1 | 16 | X | ||||||||||||||||||
| 2 | 4 | X | X | |||||||||||||||||
| 5 | 9 | X | X | X | X | X | ||||||||||||||
| 3 | 6 | X | X | X | ||||||||||||||||
| 3 | 5 | X | X | X | ||||||||||||||||
| 5 | 8 | X | X | X | X | X | ||||||||||||||
| 2 | 7 | X | X | |||||||||||||||||
| 2 | 2 | X | X | |||||||||||||||||
| Number of studies: | 6 | 2 | 2 | 2 | 1 | 7 | 6 | 3 | 2 | 3 | 3 | 1 | 3 | 1 | 2 | 1 | 1 | 1 | ||
| Abbreviations: CBT = cognitive‐behavioural theory; DMT = decision‐making theory; ET = expectancy theory; HBM = health belief model; ICM = I‐change model; MIT = motivational interviewing theory; PBT = problem behaviour theory; SCT = social cognitive theory; SCompT = social comparison theory; SDT = social determination theory; SImpT = social impact theory; SIT = social identity theory; SLT = social learning theory; SNT = social norms theory; SRT = self‐regulation theory; TM = transtheoretical model; TPB = theory of planned behaviour; TSI = theory of social influence | ||||||||||||||||||||
| Theory Coding Scheme Categories (category number) | Items included | Maximum score | Mean (SD) | Number of studies scoring ≥ 1 |
| Reference to underpinning theory (C1) | 1, 2, 3 | 3 | 1.1 (1.23) | 20 |
| Targeting of relevant theoretical constructs (C2) | 2, 5, 6, 7, 8, 9, 10, 11 | 8 | 2.0 (2.43) | 17 |
| Using theory to select recipients or tailor interventions (C3) | 4, 6 | 2 | 0.1 (0.26) | 2 |
| Measurement of constructs (C4) | 12a, 12b | 2 | 0.5 (0.86) | 11 |
| Testing of theory: mediation effects (C5) | 12a, 12b, 13, 14a, 14b, 14c, 14d, 15, 16 | 9 | 1.6 (2.83) | 14 |
| Refining theory (C6) | 17a, 17b | 2 | ‐ | ‐ |
| Total use of theory | All items | 22 | 4.4 (5.43) | 20 |
| Theory Coding Scheme covariates (item/category number) | B (SE) | P | 95% CI | Adj. R² | I² | |
| Lower bound | Upper bound | |||||
| Theory/model of behaviour mentioned (I1) | 9.73 (14.63) | 0.510 | ‐19.84 | 39.31 | ‐4.90% | 78.09% |
| Targeted construct mentioned as predictor of behaviour (I2) | 24.17 (14.09) | 0.094 | ‐4.30 | 52.64 | 2.27% | 78.13% |
| Intervention based on single theory (I3) | 12.92 (17.60) | 0.467 | ‐22.64 | 48.49 | ‐4.44% | 78.08% |
| Theory/predictors used to select recipients | Not present in > 10% of studies | |||||
| Theory/predictors used to select/develop | 18.25 (14.57) | 0.218 | ‐11.20 | 47.69 | ‐3.43% | 78.15% |
| Theory/predictors used to tailor intervention techniques | Not present in > 10% of studies | |||||
| All intervention techniques are explicitly linked to at least | ‐3.73 (19.91) | 0.852 | ‐43.98 | 36.51 | ‐4.86% | 76.50% |
| At least one, but not all, of the intervention techniques are | 26.39 (15.34) | 0.093 | ‐4.60 | 57.39 | 10.54% | 77.49% |
| Group of techniques are linked to a group of | Not present in > 10% of studies | |||||
| All theory‐relevant constructs/predictors are explicitly | 8.53 (19.81) | 0.673 | ‐31.60 | 48.46 | ‐5.82% | 78.14% |
| At least one, but not all, of the theory‐relevant | 18.79 (15.99) | 0.247 | ‐13.54 | 51.11 | ‐3.45% | 78.15% |
| Theory‐relevant constructs are measured: | ‐14.67 (15.81) | 0.359 | ‐46.62 | 17.28 | 1.42% | 76.37% |
| Theory‐relevant constructs are measured: | ‐13.78 (16.88) | 0.419 | ‐47.90 | 20.33 | ‐1.67% | 76.94% |
| Changes in measured theory‐relevant | ‐33.04 (17.48) | 0.066 | ‐68.37 | 2.28 | 16.92% | 74.82% |
| Mediational analysis of constructs/ predictors: | ‐7.77 (20.24) | 0.703 | ‐48.68 | 33.15 | ‐3.13% | 76.43% |
| Mediational analysis of constructs/ predictors: | Not present in > 10% of studies | |||||
| Mediational analysis of constructs/ predictors: | ‐21.88 (24.11) | 0.370 | ‐70.61 | 26.86 | 4.48% | 75.41% |
| Mediational analysis of constructs/ predictors: | ‐7.77 (20.24) | 0.703 | ‐48.68 | 33.14 | ‐3.13% | 76.43% |
| Results discussed in relation to theory (I15) | 1.59 (16.08) | 0.922 | ‐30.91 | 34.08 | ‐6.81% | 77.35% |
| Appropriate support for theory (I16) | ‐8.73 (19.43) | 0.656 | ‐48.01 | 30.55 | ‐2.11% | 76.33% |
| Results used to refine theory: | Not present in > 10% of studies | |||||
| Results used to refine theory: | Not present in > 10% of studies | |||||
| Reference to underpinning theory (C1) | 7.19 (5.89) | 0.230 | ‐4.72 | 19.10 | ‐1.55% | 78.08% |
| Targeting of relevant theoretical constructs (C2) | 3.94 (2.97) | 0.192 | ‐2.06 | 9.93 | ‐4.08% | 78.12% |
| Using theory to select recipients or tailor interventions (C3) | 13.30 (27.27) | 0.628 | ‐41.81 | 68.42 | ‐7.21% | 77.67% |
| Measurement of constructs (C4) | ‐7.58 (8.41) | 0.373 | ‐24.58 | 9.42 | 0.19% | 76.61% |
| Testing of theory: mediation effects (C5) | ‐2.09 (2.53) | 0.413 | ‐7.20 | 3.02 | 2.29% | 75.71% |
| Refining theory (C6) | No score > 0 for any studies | |||||
| Total use of theory | 0.39 (1.37) | 0.778 | ‐2.38 | 3.15 | ‐7.46% | 77.58% |
| Theory Coding Scheme covariates (item number) | B (SE) | P | 95% CI | |
| Lower bound | Upper bound | |||
| Targeted construct mentioned as predictor of behaviour (I2) | 50.82 (21.00) | 0.020 | 8.31 | 93.34 |
| At least one, but not all, of the intervention techniques are | ‐12.19 (20.71) | 0.560 | ‐54.12 | 29.74 |
| Changes in measured theory‐relevant constructs/predictor (I13) | ‐61.41 (19.42) | 0.003 | ‐100.71 | ‐22.10 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quantity of drinking (g/week), based on longest follow‐up Show forest plot | 42 | 19241 | Mean Difference (IV, Random, 95% CI) | ‐22.84 [‐30.31, ‐15.36] |
| 2 Quantity of drinking (g/week), categorised by length of follow‐up Show forest plot | 42 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At 1 month | 17 | 7187 | Mean Difference (IV, Random, 95% CI) | ‐20.30 [‐32.60, ‐8.01] |
| 2.2 From > 1 to 2 months | 6 | 2846 | Mean Difference (IV, Random, 95% CI) | ‐23.02 [‐44.95, ‐1.09] |
| 2.3 From > 2 to 3 months | 13 | 3000 | Mean Difference (IV, Random, 95% CI) | ‐43.30 [‐73.19, ‐13.41] |
| 2.4 From > 3 to 6 months | 19 | 12822 | Mean Difference (IV, Random, 95% CI) | ‐11.52 [‐16.31, ‐6.73] |
| 2.5 At 12 months | 7 | 3372 | Mean Difference (IV, Random, 95% CI) | ‐13.40 [‐31.28, 4.49] |
| 3 Quantity of drinking (g/week), based on longest follow‐up and categorised on whether restricted to adolescents or young adults Show forest plot | 42 | 19241 | Mean Difference (IV, Random, 95% CI) | ‐22.84 [‐30.31, ‐15.36] |
| 3.1 Trials of adolescents/young adults | 28 | 13477 | Mean Difference (IV, Random, 95% CI) | ‐13.44 [‐19.27, ‐7.61] |
| 3.2 Trials of adults | 14 | 5764 | Mean Difference (IV, Random, 95% CI) | ‐56.05 [‐82.08, ‐30.02] |
| 4 Quantity of drinking (g/week), categorised by length of follow‐up and restricted to trials of adolescents/young adults Show forest plot | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 At 1 month | 15 | 6579 | Mean Difference (IV, Random, 95% CI) | ‐19.67 [‐32.96, ‐6.37] |
| 4.2 From > 1 to 2 months | 4 | 2002 | Mean Difference (IV, Random, 95% CI) | ‐7.60 [‐18.98, 3.77] |
| 4.3 From > 2 to 3 months | 8 | 1152 | Mean Difference (IV, Random, 95% CI) | ‐15.42 [‐29.39, ‐1.45] |
| 4.4 From > 3 to 6 months | 13 | 10499 | Mean Difference (IV, Random, 95% CI) | ‐10.36 [‐13.47, ‐7.25] |
| 4.5 At 12 months | 4 | 954 | Mean Difference (IV, Random, 95% CI) | ‐2.35 [‐23.57, 18.88] |
| 5 Quantity of drinking (g/week), based on longest follow‐up and categorised by gender Show forest plot | 5 | 2566 | Mean Difference (IV, Random, 95% CI) | ‐9.58 [‐22.24, 3.07] |
| 5.1 Males | 4 | 1923 | Mean Difference (IV, Random, 95% CI) | ‐8.86 [‐31.99, 14.27] |
| 5.2 Females | 4 | 643 | Mean Difference (IV, Random, 95% CI) | ‐9.81 [‐21.87, 2.24] |
| 6 Quantity of drinking (g/week), based on longest follow‐up and omitting trials at high risk of bias owing to incomplete data Show forest plot | 28 | 13559 | Mean Difference (IV, Random, 95% CI) | ‐16.24 [‐23.43, ‐9.05] |
| 7 Quantity of drinking (g/week), based on longest follow‐up and omitting trials at high risk of performance bias Show forest plot | 11 | 10272 | Mean Difference (IV, Random, 95% CI) | ‐10.53 [‐13.70, ‐7.36] |
| 8 Quantity of drinking (g/week), based on longest follow‐up, with imputation of missing standard deviations or number of participants per arm Show forest plot | 49 | 20351 | Mean Difference (IV, Random, 95% CI) | ‐21.58 [‐28.47, ‐14.69] |
| 9 Quantity of drinking (g/week), categorised by length of follow‐up, with imputation of missing standard deviations or number of participants per arm Show forest plot | 49 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 At 1 month | 18 | 6870 | Mean Difference (IV, Random, 95% CI) | ‐20.07 [‐31.94, ‐8.20] |
| 9.2 From > 1 to 2 months | 8 | 2946 | Mean Difference (IV, Random, 95% CI) | ‐20.18 [‐40.45, 0.09] |
| 9.3 From > 2 to 3 months | 16 | 3443 | Mean Difference (IV, Random, 95% CI) | ‐33.24 [‐57.32, ‐9.16] |
| 9.4 From > 3 to 6 months | 23 | 13736 | Mean Difference (IV, Random, 95% CI) | ‐11.89 [‐16.48, ‐7.30] |
| 9.5 At 12 months | 9 | 3938 | Mean Difference (IV, Random, 95% CI) | ‐11.62 [‐26.42, 3.17] |
| 9.6 At 18 months | 1 | 327 | Mean Difference (IV, Random, 95% CI) | 22.40 [‐5.56, 50.36] |
| 9.7 At 24 months | 1 | 327 | Mean Difference (IV, Random, 95% CI) | 1.40 [‐20.28, 23.08] |
| 10 Frequency of drinking (no. of days drinking/week), based on longest follow‐up Show forest plot | 16 | 10862 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.24, ‐0.09] |
| 11 Frequency of binge drinking (no. of binges/week), based on longest follow‐up Show forest plot | 15 | 3587 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.35, ‐0.13] |
| 12 Intensity of drinking (g/drinking day), based on longest follow‐up Show forest plot | 15 | 9791 | Mean Difference (IV, Random, 95% CI) | ‐4.63 [‐8.02, ‐1.23] |
| 13 Binge drinkers, based on longest period of follow‐up Show forest plot | 9 | 9417 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.97, 1.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quantity of drinking (g/week), based on longest follow‐up Show forest plot | 5 | 390 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐24.59, 25.63] |
| 2 Quantity of drinking (g/week), categorised by length of follow‐up Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 At 1 month | 3 | 206 | Mean Difference (IV, Random, 95% CI) | 4.03 [‐36.90, 44.96] |
| 2.2 From > 1 to 2 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 From > 2 to 3 months | 2 | 188 | Mean Difference (IV, Random, 95% CI) | 17.16 [‐42.07, 76.39] |
| 2.4 From > 3 to 6 months | 1 | 113 | Mean Difference (IV, Random, 95% CI) | 6.70 [‐50.53, 63.93] |
| 2.5 At 12 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Frequency of drinking (no. of days drinking/week), based on longest follow‐up Show forest plot | 1 | 58 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.33, 0.43] |
| 4 Frequency of binge drinking (no. of binges/week), based on longest follow‐up Show forest plot | 3 | 206 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.15, 0.22] |

