Related content
Related reviews and protocols
Mylene Lagarde, Natasha Palmer | 13 April 2011
Willem A Odendaal, Kim Ward, Jesse Uneke, Henry Uro‐Chukwu, Dereck Chitama, Yusentha Balakrishna, Tamara Kredo | 3 April 2018
Tamara Kredo, Nathan Ford, Folasade B Adeniyi, Paul Garner | 27 June 2013
Sami Pande, Janet E Hiller, Nancy Nkansah, Lisa Bero | 28 February 2013
Tracey Perez Koehlmoos, Rukhsana Gazi, Shahed Hossain, K Zaman | 21 January 2009
Mylene Lagarde, Andy Haines, Natasha Palmer | 7 October 2009
Angela Oyo-Ita, Olabisi Oduwole, Dachi Arikpo, Emmanuel E Effa, Ekpereonne B Esu, Yusentha Balakrishna, Moriam T Chibuzor, Chioma M Oringanje, Chukwuemeka E Nwachukwu, Charles S Wiysonge, Martin M Meremikwu | 6 December 2023
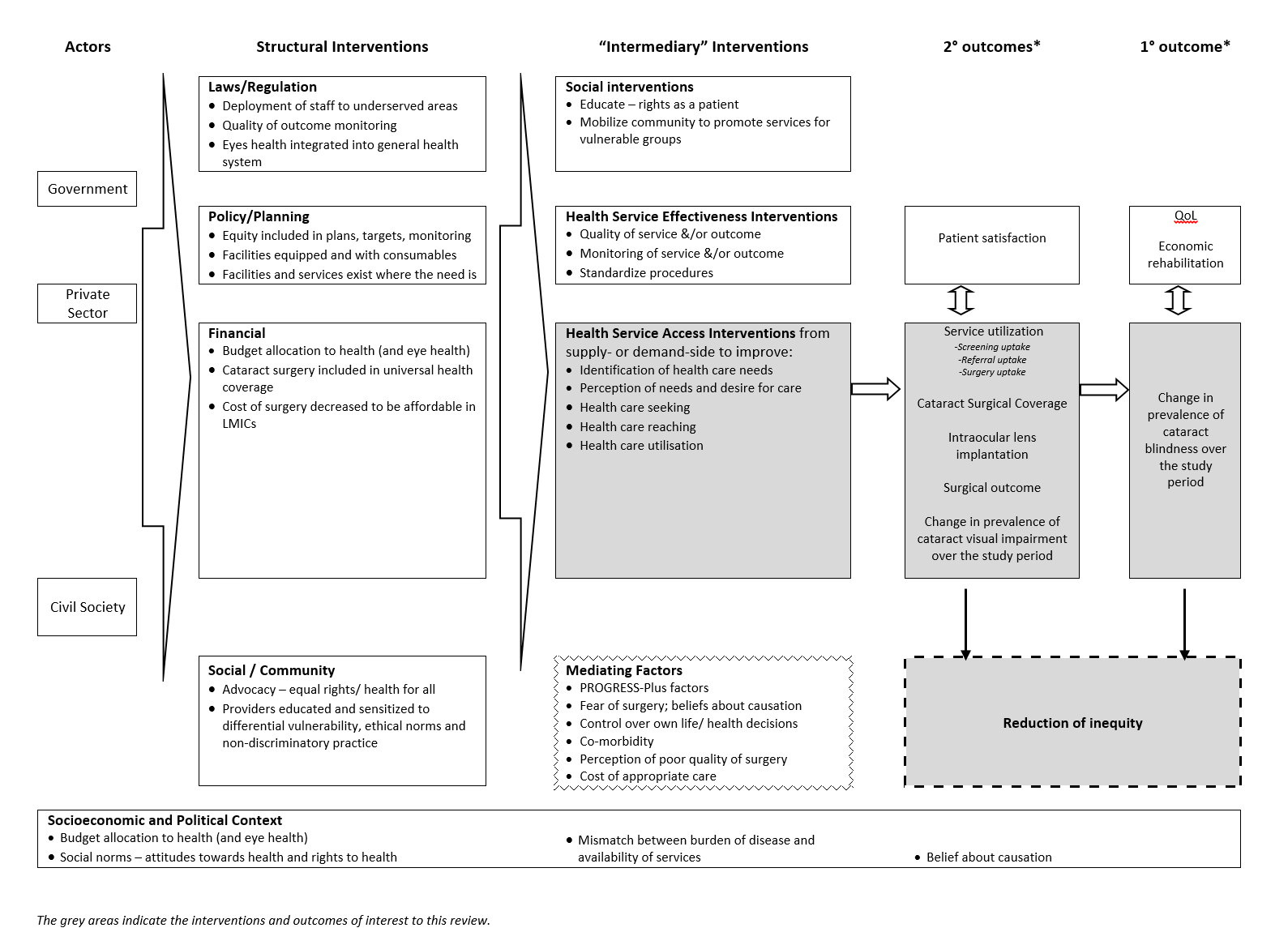
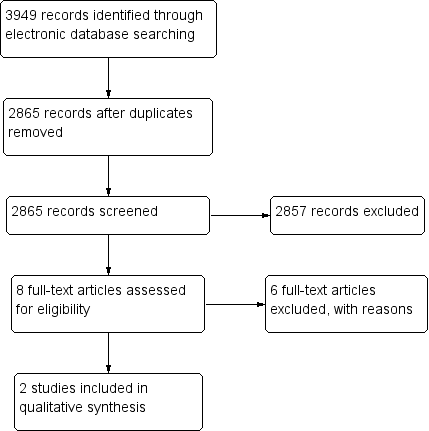
Jennifer R Evans, Priya Morjaria, Christine Powell | 15 February 2018
Zohra S Lassi, Sophie GE Kedzior, Zulfiqar A Bhutta | 5 November 2019
Blanca Peñaloza, Tomas Pantoja, Gabriel Bastías, Cristian A Herrera, Gabriel Rada | 7 September 2011