Communication skills training for mental health professionals working with people with severe mental illness
Information
- DOI:
- https://doi.org/10.1002/14651858.CD010006.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 13 June 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Schizophrenia Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Alexia Papageorgiou: Protocol development, personal contact with author of unpublished studies, screening of studies, writing the report.
Yoon Loke : Protocol development, personal contact with author of unpublished studies, screening of studies, data analysis, writing the report.
Michelle Fromage :Protocol development, screening of studies, lay summary, writing the report.
Sources of support
Internal sources
-
George's University of London Medical School, University of Nicosia, Nicosia, Cyprus.
Employs lead review author Alexia Papageorgiou
-
Norwich Medical School, University of East Anglia, Norwich, UK.
Employs review author Yoon Loke and Michelle Fromage is a PhD student with this University.
External sources
-
None, Other.
Declarations of interest
None known.
Acknowledgements
The Cochrane Schizophrenia Group Editorial Base in Nottingham produces and maintains standard text for use in the Methods sections of their reviews. We have used this text as the basis of what appears here and adapted it as required. We also used the protocol by Kinoshita 2010 and the review by Lewin 2001 as guides for our protocol.
We thank Katherine Deane for her help with developing the protocol of this review.
The search terms have been developed by the Information Specialist of the Cochrane Schizophrenia Group, Samantha Roberts and the review authors.
We would like to acknowledge and thank Rose McCabe, Professor of Clinical Communication at the University of Exeter Medical School for her willingness to share the data from her unpublished study. Without her data this review would be incomplete. We would also like to thank Victoria Bird and Katie Tyrell for peer reviewing this version of the review.
Last but not least, we would like to express our special thanks to Claire Irving the Managing Editor of the Cochrane Schizophrenia Group for her continuous support and guidance throughout this process.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Jun 13 | Communication skills training for mental health professionals working with people with severe mental illness | Review | Alexia Papageorgiou, Yoon K Loke, Michelle Fromage | |
| 2012 Aug 15 | Communication skills training for mental health professionals working with people with severe mental illness | Protocol | Alexia Papageorgiou, Yoon Loke, Katherine HO Deane, Michelle Fromage | |
Differences between protocol and review
1. Change of authors
Catherine Deane is no longer an author of the review.
2. Selection of studies
The text in the protocol reads as follows: "Review authors AP and KD will independently inspect citations from the searches and identify relevant abstracts. A random 20% sample will be independently re‐inspected by YL to ensure reliability. Where disputes arise, we will acquire the full report for more detailed scrutiny. Full reports of the abstracts meeting the review criteria will be obtained and inspected by AP and KD. Again, a random 20% of reports will be re‐inspected by YL in order to ensure reliable selection. Where it is not possible to resolve disagreement by discussion, we will attempt to contact the authors of the study for clarification."
This now reads: "Due to the small amount of studies that were identified (four studies in total) by the Information Specialist of the Cochrane Schizophrenia Group, all three authors AP, YL, MF inspected all four studies and unanimously agreed that only one of studies should be included in the review. We obtained both abstracts and full study reports and thoroughly assessed all of them."
3. Change to 'Summary of findings' outcomes
Satisfaction with training programme was not reported in trials so we used the reported outcomes for satisfaction (with treatment and with 'therapeutic relationship').
Mental state was not a prestated outcome of interest in our protocol, however, as other data were not available, we included mental state data, reported in our included study, in the 'Summary of findings' table.
4. Assessment of risk of bias in included studies
The text in the protocol reads as follows: "Again, review authors AP and KD will work independently to assess risk of bias by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) to assess trial quality."
This now reads:
"Review authors AP, YL and MF aimed to work independently to assess risk of bias by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) to assess trial quality."
5. Data extraction and management
The text in the protocol reads as follows: "Review authors AP and YL will independently extract data from all included studies. Again, any disagreement will be discussed, decisions documented and, if necessary, we will contact the authors of studies for clarification. With remaining problems KD will help clarify issues and these final decisions will be documented. "
This now reads:
Review authors AP and YL independently extracted data from the included study. We discussed any disagreements and documented decisions.We contacted authors of the included study through an open‐ended request in order to obtain missing information or for clarification. If the study had been multi‐centre, where possible, we would have extracted data relevant to each component centre separately.
For cluster randomised trials, we extracted the adjusted difference in means (aMD) of the endpoint and a measure of variation (such as a confidence intervals or standard error).
6. References
Four more references were added to 'Additional references' (Dwamena 2012; Kay 1987; McGuire‐Snieckus 2007; Nguyen 1983).
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adult; Female; Humans; Male;
PICOs

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Communication skills training versus no specific training, Outcome 1 Patient satisfaction: 1. Satisfaction with treatment: average endpoint score (CSQ‐8, high = good, medium term).
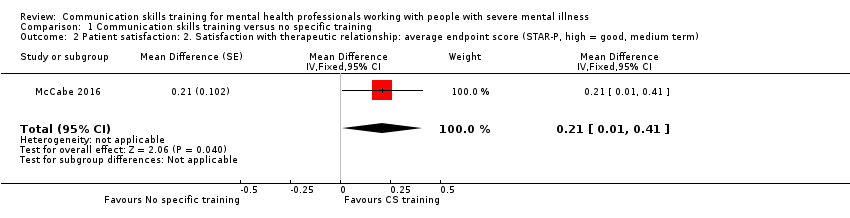
Comparison 1 Communication skills training versus no specific training, Outcome 2 Patient satisfaction: 2. Satisfaction with therapeutic relationship: average endpoint score (STAR‐P, high = good, medium term).

Comparison 1 Communication skills training versus no specific training, Outcome 3 Mental state: 1. General Symptom: Average endpoint score (PANSS General, high = poor, medium term).

Comparison 1 Communication skills training versus no specific training, Outcome 4 Mental state: 2. Positive Symptom; Average endpoint score (PANSS Positive, high = poor, medium term).
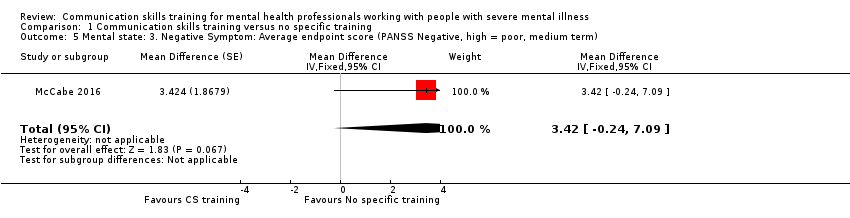
Comparison 1 Communication skills training versus no specific training, Outcome 5 Mental state: 3. Negative Symptom: Average endpoint score (PANSS Negative, high = poor, medium term).
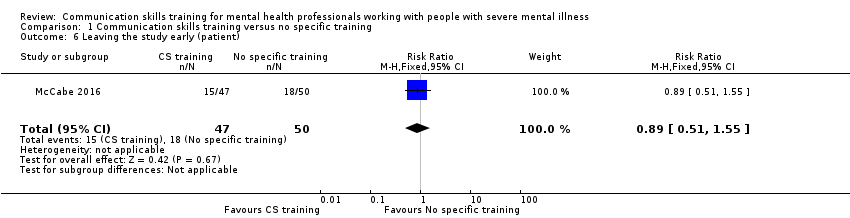
Comparison 1 Communication skills training versus no specific training, Outcome 6 Leaving the study early (patient).
| Method | Cluster‐randomised controlled study with the allocation clearly described Blinding: single‐blinded, described and tested Single‐blinding is a more realistic allocation for this type of study which should aim to blind trainees and patients to primary and secondary outcomes. Three‐, six‐ and 12‐month follow‐ups would be desirable in order to assess whether the impact of communication skills training is enduring. |
| Participants | Future studies target both trainee psychiatrists and more experienced psychiatrists. Patients diagnosed with specific mental health conditions (e.g. psychosis, bipolar, anxiety), but recruit inpatients or patients near discharge from hospital. In order to avoid loss to follow‐up and increase the power of the study a larger sample needs to be recruited with multiple psychiatric hospitals/trusts. |
| Intervention | The interventions could be expanded to include on‐line communication skills training, written feedback, a reflective written report and a control condition. Video‐taping of face‐to‐face consultations with patients could be done before the intervention starts in order to obtain baseline data and allow post‐intervention comparisons. Text messaging and access to computerised GP records could be employed to limit loss to follow‐up and improve data quality. |
| Outcomes | Primary outcomes With relation to the patients treated by the mental health professional. 1. Adherence to treatment 1.1 Taking of medication With relation to the mental health professional. 2.1 Satisfaction with the training programme 2.2 Integration of key communication skills into clinical practice post‐intervention 2.3 Reason for leaving the study early Secondary outcomes With relation to the patients treated by the mental health professional. 1. Global state 1.1 Clinically important improvement 2. Service Use 2.1 Number of hospital admissions 3. Mental state 3.1 Positive symptoms (delusions, hallucinations, disordered thinking) 4. Patient satisfaction 4.1 Average change or endpoint scores on satisfaction scales 5. Social functioning 5.1 Average change or endpoint scores on social functioning scales 6. Quality of life 6.1 Clinically important change in general quality of life 7. Reason for leaving the study early |
| Notes | A future study should be powered to be able to identify a difference of ˜10% between groups for primary outcomes with adequate degree of certainty |
| Communication skills training programme compared with no specific training programme for psychiatrists who treat patients with severe mental illness | ||||||
| Patient or population: psychiatrists and people with schizoaffective disorder or schizophrenia Settings: outpatient or community Intervention: communication skills training programme (CST) Comparison: no specific communication skills training programme (NST) | ||||||
| Outcomes | Illustrative comparative risks* (SD) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Experimental | |||||
| Adherence to Adherence to treatment: taking of medication, attending appointments | See comments | See comments | Not estimable | See comments | See comments | no data available |
| 1. Patient satisfaction: 1. Satisfaction with treatment: average endpoint score (CSQ‐8, high = good, medium term) | The mean patient satisfaction with treatment in NST group was 26.6 ± 4.6 | The mean patient satisfaction with treatment in the CST group was 28.3 ± 3.6 | Adjusted mean difference 1.77 (95% CI ‐ 0.13 to 3.68) | 1 RCT, n = 66/97 | ⊕⊕⊝⊝ | This was based on unpublished data obtained from the author. Intracluster correlation coefficient was 0.65. |
| Patient satisfaction: 2. Satisfaction with therapeutic relationship: average endpoint score (STAR‐P, high = good, medium term) | The mean therapeutic relationship (as judged by the patient) in the NST group was 2.6 ± 0.3 | The mean value for therapeutic relationship (as judged by the patient) in the CST group was 2.8 ± 0.4 | Adjusted mean difference 0.21 (95% CI 0.01 to 0.41, P = 0.043) | 1 RCT, n = 63/97) | ⊕⊕⊝⊝ | Patients in the intervention group judged the therapeutic relationship to be more favourable. There was a negative intracluster correlation coefficient. |
| Mental state: General, Positive and Negative Symptoms: Average endpoint score (PANSS General, Positive, Negative, high = poor, medium term) | In the NST group, the mean severity scores at follow‐up were: General symptoms 34.1 ± 7.9; Positive symptoms 14.5 ± 5.9 Negative symptoms 14.1 ± 5.5 | In the CST group, the mean severity scores at follow‐up were: General symptoms 34.3 ± 12.3 Positive symptoms 14.9 ± 6.9 Negative symptoms 16.3 ± 7.3 | Adjusted mean difference General 4.48 (95%CI ‐ 2.10 to 11.06) Positive ‐0.23 (95% CI ‐ 2.91 to 2.45) Negative 3.42 ( 95% CI ‐ 0.24 to 7.09) | 1 RCT, n = 59/97 | ⊕⊕⊝⊝ | No significant difference in endpoint disease severity scores between intervention and control. This was based on unpublished data obtained from the author. Intracluster correlation coefficient was zero. |
| Global State: clinically important improvement | See comments | See comments | Not estimable | See comments | See comments | no data available |
| Service Use: hospital admission, days in hospital | See comments | See comments | Not estimable | See comments | See comments | no data available |
| Quality of Life: clinically important improvement | See comments | See comments | Not estimable | See comments | See comments | no data available |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. Very serious: Downgraded by 2. The downgrading is because of the small pilot nature of the trial, imprecision and substantial losses to follow‐up amounting to >30%. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patient satisfaction: 1. Satisfaction with treatment: average endpoint score (CSQ‐8, high = good, medium term) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | 1.77 [‐0.13, 3.68] | |
| 2 Patient satisfaction: 2. Satisfaction with therapeutic relationship: average endpoint score (STAR‐P, high = good, medium term) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | 0.21 [0.01, 0.41] | |
| 3 Mental state: 1. General Symptom: Average endpoint score (PANSS General, high = poor, medium term) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | 4.48 [‐2.10, 11.06] | |
| 4 Mental state: 2. Positive Symptom; Average endpoint score (PANSS Positive, high = poor, medium term) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.23 [‐2.91, 2.45] | |
| 5 Mental state: 3. Negative Symptom: Average endpoint score (PANSS Negative, high = poor, medium term) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | 3.42 [‐0.24, 7.09] | |
| 6 Leaving the study early (patient) Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.51, 1.55] |


