Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities
Information
- DOI:
- https://doi.org/10.1002/14651858.CD009461.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 21 February 2015see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Gynaecology and Fertility Group
- Copyright:
-
- Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
JB co‐ordinated the writing of the protocol and review and its update.
JK co‐authored the protocol for the background section and searched the literature.
FB and TD independently assessed the retrieved published reports for inclusion of potentially eligible studies.
SW independently extracted study data.
BWM gave advice on review methodology and content and critically appraised the Cochrane review.
Sources of support
Internal sources
-
CEBAM, Belgium.
Research grant was obtained through CEBAM, the Centre for Evidence‐based Medicine, Belgian Branch of the Cochrane Collaboration
External sources
-
No sources of support supplied
Declarations of interest
FB and JK (principal investigator) and BWM (co‐investigator) are at present involved in the 'inSIGHT trial' (SIGnificance of Routine Hysteroscopy Prior to a First 'in Vitro Fertilization' Treatment Cycle: NCT 01242852), which is financially supported by ZonMw, a Dutch government operated consortium responsible for granting funds in the field of clinical practice research. This study is still in the recruitment phase.
The first published version of the present Cochrane review has been part of a PhD thesis entitled "Studies on the effectiveness of endoscopic surgery in reproductive medicine" (http://dare.uva.nl/record/497164), which has been successfully defended at the faculty of Medicine of the University of Amsterdam, the Netherlands on 2 September 2014 by the first author (JB).
Acknowledgements
Cochrane Menstrual Disorders and Subfertility Group (MDSG): we wish to thank Prof. Cindy Farquhar, MDSG Editor in Chief; Ms. Jane Clarke, former MDSG Managing Editor; Ms. Helen Nagels, MDSG Managing Editor and Ms. Jane Marjoribanks, MDSG Assistant Managing Editor for their advice and support. Ms. Marian Showell, MDSG Trials Search Co‐ordinator assisted in searching the MDSG Specialised Register and gave advice on the handsearch.
Biomedical Library Gasthuisberg, Catholic University, Leuven, Belgium. Many thanks to Mr. Jens De Groot for skilful assistance in developing the literature search strategy.
Prof. Tirso Pérez‐Medina, head of the department of Gynaecology at the University Hospital Puerta de Hierro, Madrid, Spain, has answered all the queries concerning the randomised controlled trial on the effectiveness of hysteroscopic polypectomy prior to IUI.
The Board of the European Society of Gynaecological Endoscopy (ESGE). Prof. Hans Brolmann (ESGE President) and Dr. Rudi Campo (ESGE Secretary) have been very helpful in contacting a group of experts in hysteroscopy in the field of Reproductive Medicine. Dr. Rudi Campo (ZOL Genk, Belgium), Dr. Dick Schoot (Catharina Hospital, Eindhoven, the Netherlands), Prof. Attilio Di Spiezio Sardo (University of Naples 'Frederico II', Naples, Italy), Prof. Hervé Fernandez (Hôpital Bicêtre, Le Kremin‐Bicêtre, France) have provided data on published or ongoing randomised trials relevant to the research questions.
Dr. Ben Cohlen (Fertility Centre Isala, Zwolle, the Netherlands), Prof. Willem Ombelet (ZOL, Genk, Belgium) and Prof. Carl Spiessens (Leuven University Fertility Centre, Leuven, Belgium) have provided useful data on the clinical pregnancy rates after gonadotropin stimulation and IUI. Dr. Mariette Goddijn (AMC Amsterdam, the Netherlands) has given valuable feedback on the risk of bias assessment for one of the included trials at the occasion of the oral opposition and defence of the PhD thesis of the first author.
Ms.Elizabeth Bosselaers (Managing Secretary CEBAM, the Belgian Branch of the Dutch Cochrane Centre) has given valuable remarks for improving the Plain language summary.
We acknowledge comments sent by Professor Hossam Eldin Shawki Abdalla MD of the Obstetrics & Gynecology Department, Faculty of Medicine, El ‐Minia University, Egypt. Our formal response was published in October 2014 and the points made were taken into account in this update.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Dec 05 | Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities | Review | Jan Bosteels, Steffi van Wessel, Steven Weyers, Frank J Broekmans, Thomas M D'Hooghe, M Y Bongers, Ben Willem J Mol | |
| 2015 Feb 21 | Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities | Review | Jan Bosteels, Jenneke Kasius, Steven Weyers, Frank J Broekmans, Ben Willem J Mol, Thomas M D'Hooghe | |
| 2013 Jan 31 | Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities | Review | Jan Bosteels, Jenneke Kasius, Steven Weyers, Frank J Broekmans, Ben Willem J Mol, Thomas M D'Hooghe | |
| 2011 Nov 09 | Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. | Protocol | Jan Bosteels, Jenneke Kasius, Steven Weyers, Frank J Broekmans, Ben Willem J Mol, Thomas M D'Hooghe | |
Differences between protocol and review
-
As a result of further peer review, the objectives of the review have been rephrased. The descriptions in the Types of interventions and Data synthesis sections were modified accordingly. For both comparisons we made a stratification according to the types of uterine pathology; for the second comparison we made a clear distinction between IUI, IVF or ICSI.
-
A 'Summary of findings' table using the GRADE approach has been added.
-
In the Assessment of risk of bias in included studies section of the review, the items 'blinding of participants and personnel' and 'blinding of outcome assessors' were reinserted as requested by the editorial reviewers. We assessed all six items including blinding of participants, personnel and outcome assessors in the final review as opposed to the protocol.
-
In the Assessment of heterogeneity section of the review we have added the Q‐statistic.
-
In the Subgroup analysis and investigation of heterogeneity section of the review we planned to conduct a further subgroup analysis based on the women's age.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Coitus;
- Endometrium;
- Fertilization in Vitro;
- *Hysteroscopy [adverse effects];
- Infertility [etiology, *surgery];
- Insemination, Artificial [methods];
- Leiomyoma [*surgery];
- Live Birth;
- Polyps [*surgery];
- Randomized Controlled Trials as Topic;
- Tissue Adhesions [surgery];
- Uterine Diseases [*surgery];
- Uterus [abnormalities];
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICOs
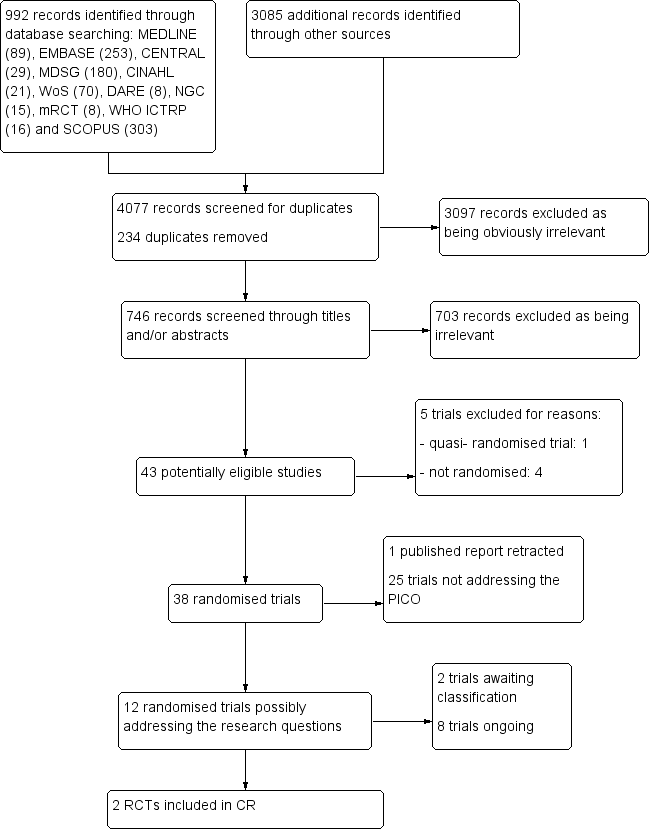
PRISMA study flow diagram.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
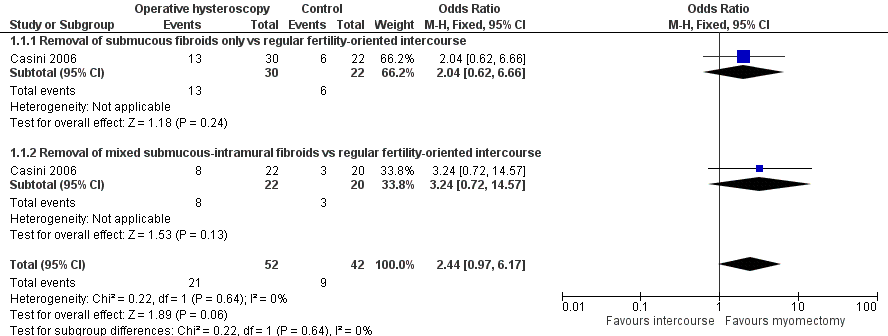
Forest plot of comparison: 1 Hysteroscopic myomectomy vs regular fertility‐oriented intercourse in women with unexplained subfertility and submucous fibroids.Outcome: 1.1 Clinical pregnancy per woman randomised.

Forest plot of comparison: 1 Hysteroscopic myomectomy vs regular fertility‐oriented intercourse in women with unexplained subfertility and submucous fibroids. Outcome: 1.2 Miscarriage per clinical pregnancy.

Forest plot of comparison: 2 Hysteroscopic removal of polyps vs diagnostic hysteroscopy and biopsy only prior to IUI. Outcome: 2.1 Clinical pregnancy per woman randomised.
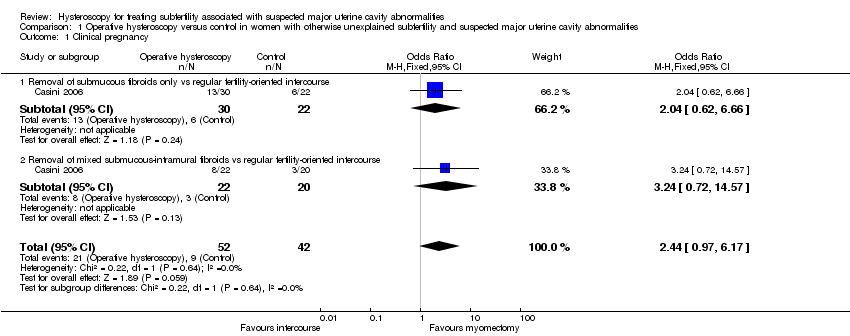
Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.

Comparison 1 Operative hysteroscopy versus control in women with otherwise unexplained subfertility and suspected major uterine cavity abnormalities, Outcome 2 Miscarriage.

Comparison 2 Operative hysteroscopy versus control in women undergoing MAR with suspected major uterine cavity abnormalities, Outcome 1 Clinical pregnancy.
| Operative hysteroscopy compared with control for unexplained subfertility associated with suspected major uterine cavity abnormalities | ||||||
| Patient or population: women with submucous fibroids and otherwise unexplained subfertility Settings: infertility centre in Rome, Italy Intervention: hysteroscopic removal of one submucous fibroid ≤ 40 mm Comparison: regular fertility‐oriented intercourse | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Myomectomy | |||||
| Live birth | No data were reported for this primary outcome. | |||||
| Hysteroscopy complications | No data were reported for this primary outcome. | |||||
| Clinical pregnancy ultrasound1 12 months | Medium‐risk population | OR 2.44 (0.97 to 6.17) | 94 | ⊕⊝⊝⊝ | ||
| 214 per 1000 | 399 per 1000 | |||||
| Miscarriage ultrasound5 12 months | Medium‐risk population | OR 0.58 (0.12 to 2.8) | 30 pregnancies in 94 women | ⊕⊝⊝⊝ | ||
| 556 per 1000 | 421 per 1000 | |||||
| *The basis for the assumed risk is the control group risk of the single included study (Casini 2006). The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. 2 Unclear allocation concealment. 3 Wide confidence intervals. 4 High risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics. 5 Miscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Operative hysteroscopy compared with control for suspected major uterine cavity abnormalities prior to medically assisted reproduction | ||||||
| Patient or population: subfertile women with endometrial polyps diagnosed by ultrasonography prior to treatment with gonadotropin and intrauterine insemination Settings: infertility unit of a university tertiary hospital in the Spanish capital Madrid Intervention: hysteroscopic polypectomy using a 5.5 mm continuous flow office hysteroscope with a 1.5 mm scissors and forceps Comparison: diagnostic hysteroscopy using a 5.5 mm continuous flow office hysteroscope and polyp biopsy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Polypectomy | |||||
| Live birth | No data were reported for this primary outcome. | |||||
| Hysteroscopy complications | No data were reported for this primary outcome. | |||||
| Clinical pregnancy ultrasound1 4 IUI cycles | Low‐risk population2 | OR 4.41 (2.45 to 7.96) | 204 | ⊕⊕⊕⊝ | ||
| 250 per 1000 | 595 per 1000 | |||||
| Medium‐risk population3 | ||||||
| 366 per 1000 | 718 per 1000 | |||||
| High‐risk population4 | ||||||
| 528 per 1000 | 831 per 1000 | |||||
| Miscarriage | No data were reported for this secondary outcome. | |||||
| *The basis for the assumed risk in the low‐, medium‐ or high‐risk populations is the control group risk of three studies provided in the footnotes below. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Clinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. 2 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for male factor subfertility based on data from Bensdorp 2007. 3 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for unexplained subfertility based on data from Veltman‐Verhulst 2012. 4 Based on the clinical pregnancy rate per woman after 4 cycles gonadotropins and IUI for female factor subfertility based on data from Spiessens 2003. 5 There was high risk for selective outcome reporting. | ||||||
| Polyp size | Clinical pregnancy1 | Clinical pregnancy rate (95% CI)2 |
| < 5 mm | 19/25 | 76% (from 72% to 80%) |
| 5 to 10 mm | 18/32 | 56% (from 53% to 59%) |
| 11 to 20 mm | 16/26 | 61% (from 58% to 65%) |
| > 20 mm | 11/18 | 61% (from 58% to 64%) |
| 1 Clinical pregnancy is defined by a pregnancy diagnosed by ultrasound visualisation of at least one gestational sac per woman randomised. 2 No significant difference was found for the clinical pregnancy rates between the 4 subgroups (P = 0.32). | ||
| Quality assessment Submucous fibroids and unexplained subfertility | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 1 year; ultrasound1) | ||||||
| 1 | RCT | Serious2 | No serious inconsistency | No serious indirectness | Serious3 | Reporting bias4 |
| Miscarriage (follow‐up 1 year; ultrasound5) | ||||||
| 1 | RCT | Serious2 | No serious inconsistency | No serious indirectness | Serious3 | Reporting bias4 |
| 1 A clinical pregnancy was defined by the visualisation of an embryo with cardiac activity at six to seven weeks' gestational age. 2 Unclear allocation concealment. 3 Wide confidence intervals. 4 High risk of selective outcome reporting and unclear whether there is other bias caused by imbalance in the baseline characteristics. 5 Miscarriage was defined by the clinical loss of an intrauterine pregnancy between the 7th and 12th weeks of gestation. | ||||||
| Quality assessment Endometrial polyps prior to gonadotropin and IUI treatment | ||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations |
| Clinical pregnancy (follow‐up 4 IUI cycles; ultrasound1) | ||||||
| 1 | RCT | No serious limitations | No serious inconsistency | No serious indirectness | No serious imprecision | Selective outcome reporting2 |
| 1 Clinical pregnancy was defined by the presence of at least one gestational sac on ultrasound. 2 There was high risk for selective outcome reporting bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.44 [0.97, 6.17] |
| 1.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.62, 6.66] |
| 1.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [0.72, 14.57] |
| 2 Miscarriage Show forest plot | 1 | 30 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.12, 2.85] |
| 2.1 Removal of submucous fibroids only vs regular fertility‐oriented intercourse | 1 | 19 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.09, 4.40] |
| 2.2 Removal of mixed submucous‐intramural fibroids vs regular fertility‐oriented intercourse | 1 | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.03, 7.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical pregnancy Show forest plot | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |
| 1.1 Hysteroscopic polypectomy vs diagnostic hysteroscopy and biopsy only prior to IUI | 1 | 204 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.41 [2.45, 7.96] |

