Recombinant human growth hormone for treating burns and donor sites
Abstract
Background
Recombinant human growth hormone (rhGH) increases protein synthesis, therefore it is used in burns with a total body surface area (TBSA) greater than 40%, where there is frequently an increase in protein breakdown and a decrease in protein synthesis. This change in protein metabolism correlates with poor wound healing of the burn and donor sites.
Objectives
To determine the effects of rhGH on the healing rate of burn wounds and donor sites in people with burns.
Search methods
For this first update we searched the Cochrane Wounds Group Specialised Register (searched 04 September 2014); The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 8); Database of Abstracts of Reviews of Effects (DARE) (The Cochrane Library 2014, Issue 3); Ovid MEDLINE (1950 to September Week 4 2014); Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations September 8, 2014); Ovid EMBASE (1980 to 2014 Week 35); and EBSCO CINAHL (1982 to 8 September 2014).
Selection criteria
Randomised controlled trials (RCTs) comparing rhGH with any comparator intervention, e.g. oxandrolone or placebo, in adults or children with burns.
Data collection and analysis
Two review authors independently selected studies, assessed trial quality and extracted data. The primary outcomes were the healing of the burn wound and donor sites and the occurrence of wound infections. The secondary outcomes were mortality rate, length of hospital stay, scar assessment, and adverse events: hyperglycaemia and septicaemia.
Main results
We included 13 RCTs (701 people). Six of the RCTs included only children aged 1 to 18 years and seven involved only adults (from 18 to 65 years of age). The mean TBSA of the included participants was greater than 49%. Twelve studies compared rhGH with placebo and one study compared rhGH with oxandrolone. Two trials found that compared with placebo, burn wounds in adults treated with rhGH healed more quickly (by 9.07 days; 95% confidence interval (CI) 4.39 to 13.76, I² = 0%). The donor site healing time was significantly shorter in rhGH‐treated adults compared with placebo‐treated participants (by 3.15 days; 95% CI 1.54 to 4.75, I² = 0%). Two studies in children with the outcome of donor site healing time could be pooled and the donor site healing time was shorter in the rhGH‐treated children (by 1.70 days; 95% CI 0.87 to 2.53, I² = 0%). No studies reporting the outcome of wound infection were found. The incidence of hyperglycaemia was higher in adults during rhGH treatment compared with placebo (risk ratio (RR) 2.43; 95% CI 1.54 to 3.85), but not in children. Pooling the studies of adults and children yielded a significantly higher incidence of hyperglycaemia in the rhGH‐treated participants (RR 2.65; 95% CI 1.68 to 4.16).
Authors' conclusions
There is some evidence that using rhGH in people with large burns (more than 40% of the total body surface area) could result in more rapid healing of the burn wound and donor sites in adults and children, and in reduced length of hospital stay, without increased mortality or scarring, but with an increased risk of hyperglycaemia. This evidence is based on studies with small sample sizes and risk of bias and requires confirmation in higher quality, adequately powered trials.
PICOs
Plain language summary
Human growth hormone for treating burns and skin graft donor sites
Growth hormone is produced by the pituitary gland. For decades, it could only be obtained by extraction from pituitary glands but more recently it has been produced through genetic engineering and made available for therapy as recombinant human growth hormone (rhGH). The aim of this review was to determine the effects of rhGH when used to treat burns and skin graft donor sites and to determine its safety compared with other treatments.
A burn that affects more than 40% of total body surface area affects the entire body. In people with such large burns, metabolism increases, as represented by a higher heart rate. This state of increased metabolism is called hypermetabolism. Hypermetabolism consumes high levels of energy Part of this energy is obtained through the breakdown of the patient’s own muscles, which leads to wasting. This breaking down of tissues into smaller molecules to release energy is called catabolism. However, such catabolism does not provide sufficient energy for the hypermetabolic state. This shortage of energy and building molecules leads to prolonged burn wound and donor site healing. In children, this shortage also leads to growth retardation. This catabolic state can be treated with anabolic agents that reverse the protein breakdown. One of the anabolic agents recommended for such a treatment approach is recombinant growth hormone.
We found 13 eligible randomised controlled trials (RCTs) involving 701 people for inclusion in this review. There is some evidence that recombinant growth hormone therapy in people with burns covering more than 40% of the total body surface area helps burn wounds and donor sites heal more rapidly and reduce the length of hospital stay, without increased mortality or increased scarring. We found it difficult to assess the quality of these studies due to poor reporting therefore we cannot be completely confident in their results.
Authors' conclusions
Summary of findings
| Recombinant human growth hormone compared with placebo for treating burns and donor sites | ||||||
| Patient or population: | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Recombinant human growth hormone | ||||||
| Healing time of burn wounds in days for adults | The mean healing time of burn wounds in days for adults in the intervention groups was 9.07 lower (4.39 to 13.76 lower) | 36 | ⊕⊕⊝⊝ | |||
| Donor site healing time in days for adults | The mean donor site healing time in days for adults in the intervention groups was | 36 | ⊕⊕⊝⊝ | |||
| Donor site healing time in days for children | The mean donor site healing time in days for children in the intervention groups was | 73 (2 studies) | ⊕⊕⊝⊝ | |||
| Mortality in adults and children | Study population5 | RR 0.53 | 324 | ⊕⊕⊝⊝ | ||
| 7 per 100 | 4 per 100 (2 to 9) | |||||
| Low5 | ||||||
| 5 per 100 | 3 per 100 (1 to 6) | |||||
| High5 | ||||||
| 13 per 100 | 7 per 100 (3 to 17) | |||||
| Septicaemia in adults | Study population8 | RR 0.61 | 267 | ⊕⊕⊝⊝ | ||
| 13 per 100 | 8 per 100 (4 to 16) | |||||
| Low8 | ||||||
| 4 per 100 | 2 per 100 (1 to 5) | |||||
| High8 | ||||||
| 13 per 100 | 8 per 100 (4 to 16) | |||||
| Hyperglycaemia in adults and children | Study population10 | RR 2.65 | 340 | ⊕⊕⊝⊝ | ||
| 11 per 100 | 30 per 100 (19 to 48) | |||||
| Low10 | ||||||
| 0 per 100 | 0 per 100 (0 to 0) | |||||
| High10 | ||||||
| 19 per 100 | 50 per 100 (32 to 79) | |||||
| Length of hospital stay in days for adults | The mean length of hospital stay in days for adults in the intervention groups was | 99 | ⊕⊕⊝⊝ | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Method of randomisation, allocation concealment and blinding not reported. | ||||||
Background
Description of the condition
Fire‐related burns (not including scalds or electric or chemical burns) were responsible for an estimated 322,000 deaths globally in 2002 (Mock 2008). Mortality rates due to these burns vary greatly among different regions of the world, ranging from 11.6 deaths per 100,000 people per year in Southeast Asia to 1.0 deaths per 100,000 people in high‐income countries (Mock 2008).
People with a major thermal injury experience a hypermetabolic response (an increase in metabolic activity). This hypermetabolic response is characterised by a hyperdynamic circulatory response, with increased body temperature; increased oxygen and glucose consumption; increased carbon dioxide production; hyperglycaemia (raised blood sugar levels); peripheral insulin resistance; glycogenolysis, proteolysis and lipolysis (i.e., the breakdown of glycogen, protein and lipids, respectively); the loss of lean body mass; and muscle and bone wasting. These symptoms can last for one to two years after the burn injury (Herndon 2004; Przkora 2005; Przkora 2006; Jeschke 2008; Branski 2009). The intensity of this response depends on the percentage of the total body surface area (TBSA) involved. The response is most frequently observed in burns with a TBSA greater than 40%. The hypermetabolic response is associated with sympathetic nervous system stimulation, increased levels of stress hormones (catecholamines, glucagon and glucocorticoids) and the release of inflammatory mediators (e.g., tumour necrosis factor, interleukin). In the severely burned patient, hypermetabolism correlates with protein catabolism (breakdown), which appears as muscle wasting and weakness, the loss of lean body mass, poor wound healing of the burn site and/or donor sites and immune system depression. Protein catabolism is an imbalance between protein synthesis and breakdown. The breakdown of muscles yields free amino acids for building proteins in the burn wound (Demling 2000; Pereira 2005).
Burn wounds can be treated with autologous skin transplantations using skin taken from another part of the burn victim's body. The donor sites of these transplants can be harvested more than once. Shortening the healing time of the donor sites can accelerate the person's recovery. The healing time of the donor sites is influenced by the person's nutritional state and is prolonged during severe hypermetabolism (Hart 2000).
Description of the intervention
Growth hormone is produced by the pituitary gland. For decades, growth hormone could only be obtained by extraction from the pituitary glands of corpses; however since 1985 it has been genetically engineered and is currently available for therapy as recombinant human growth hormone (rhGH). This hormone can be administered once or twice daily through subcutaneous or intramuscular injection. The usual dose for metabolic indications is 0.1 to 0.2 mg/kg/day, and it can be administered for a time period ranging from days to one year (Van Loon 1998). The price for 5 mg/mL is approximately USD 300; and treatment for a person with a body weight of 50 kg is USD 300 to 600 per day. New depot forms of rhGH, which enable the injections to be given once or twice a month, are becoming available. The drug is administered at bedtime to mimic the physiological pattern of growth hormone secretion. There are various rhGH formulations available on the market, including Genotropin®, Humatrope®, Nutropin®, Nutropin AQ®, Protropin®, Serostim® and Zorbitive®. The rhGH indications approved by the Food and Drug Administration (FDA) and the European Medicines Agency (EMEA) for giving rhGH are growth disturbance in children and growth hormone deficiency in adults.
How the intervention might work
Due to its potent anabolic (growth‐stimulating) properties, rhGH can be used to limit the catabolism of burned tissue (Demling 2000; Pereira 2005). Its anabolic effects increase the cellular uptake of amino acids, nitrogen retention and protein synthesis and the release of insulin‐like growth factor (IGF). It can have a direct effect on the skin due to the presence of growth hormone receptors on epidermal cells. The hypermetabolic response after burn injuries persists, despite improvements in surgical and nursing care. The modulation of hormonal imbalances after burn injuries was introduced in the 1990s, and investigated in animal studies and clinical trials (Herndon 1990; Klein 1998; Ramirez 1998; Singh 1998; Jeschke 1999a; Jeschke 1999b; Aili 2001; Hart 2001; Przkora 2006a; Branski 2009). Herndon 1990 showed reduced donor site healing times and a reduced length of hospital stay in children with burns who were treated with rhGH. Human growth hormone administration is associated with side effects, including hyperglycaemia and reactions at the injection site (e.g., nodules, erythema, pain and swelling). Long‐term treatment at doses of 0.1 mg/kg/day has been considered safe and well tolerated (Van Loon 1998).
Why it is important to do this review
The precise role of recombinant human growth hormone (rhGH) in the treatment of burns and skin donor sites is uncertain. Treatment with rhGH has been used with success to stimulate growth in children with growth retardation, including those with growth hormone deficiency, Turner and Nooan syndromes (Bryant 2007), small size for gestational age, Prader‐Willi syndrome, idiopathic short stature (Bryant 2007) and cystic fibrosis (Krysiak 2007). In adults, growth hormone therapy is indicated in people with growth hormone deficiency, and it has positive effects on the lipid profile, muscle strength, cardiac function and quality of life. In another study with thermally injured rats, rhGH attenuated the decrease in IGF‐1 after burns (Jeschke 1999b). Although randomised controlled trials (RCTs) are available there are no published systematic reviews or evidence‐based guidelines to direct clinical decision‐making in the costly use of rhGH to treat burn wounds.
Objectives
To determine the safety and effects of recombinant human growth hormone on the healing rate of burn wounds and donor sites in people with burns.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomised controlled trials (RCTs).
Types of participants
We included trials that included people of any age who had a burn wound covering more than 20% TBSA with more than 10% full‐thickness (i.e., a third‐degree burn). Trials involving any type of burn injury were eligible (e.g., chemical, scald or flame burns). We included trials with donor sites only when the donor sites were used to treat burn wounds.
Types of interventions
We considered studies for inclusion if recombinant human growth hormone (rhGH, any regimen) was compared with any comparable intervention, for example, testosterone analogues (e.g., oxandrolone), β‐blockade (propranolol) or placebo.
Types of outcome measures
Primary outcomes
-
Burn wound healing. Objective measures of the healing of transplanted and non‐operated burn wounds included the time to complete wound healing or the proportion of the burn wound that healed completely (epithelialised) within a specific time period.
-
Donor site healing. Objective measures of donor site healing included the healing time (in days) for the first and successive donor sites or the number of wounds that healed completely during the trial period.
-
Wound infection (as defined by the trial authors).
-
Mortality rate.
Secondary outcomes
-
Length of hospital stay
-
Any objective measurement of scar formation. The most frequently used measure of scar evaluation is the Vancouver Scar Scale (Sullivan 1990; Baryza 1995). This is a clinical scale that has been tested for reliability and validity (Nedelec 2000). Another reliable and valid scar scale is the Patient and Observer Scar Assessment Scale (POSAS) (Draaijers 2004; Vercelli 2009). The Seattle Scar Scale (Yeong 1997) and Hamilton Scale (Crowe 1998) are used to assess scars using photographs of burn wounds.
-
Adverse events (e.g., hyperglycaemia, septicaemia).
-
Quality of life measures, such as the Burns Specific Health Scale (BSHS) questionnaire (Blades 1982).
Search methods for identification of studies
The search methods for the original review can be found in Appendix 1
Electronic searches
For this first update we searched the following electronic databases to find reports of relevant RCTs:
-
Cochrane Wounds Group Specialised Register (searched 4 September 2014);
-
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 8);
-
Database of Abstracts of Reviews of Effects (DARE) (The Cochrane Library 2014, Issue 3);
-
Ovid MEDLINE (1950 to September Week 4 2014);
-
Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations September 8, 2014);
-
Ovid EMBASE (1980 to 2014 Week 35);
-
EBSCO CINAHL (1982 to 8 September 2014);
-
PEDro, the Physiotherapy Evidence database (1980 to 8 September 2014);
-
National Research Register (NRR) Archive (https://portal.nihr.ac.uk/Pages/NRRArchive.aspx);
-
OAIster (http://oaister.umdl.umich.edu/o/oaister/) international institutional digital repository search engine;
-
Web of Science (1975 to 8 September 2014);
-
Dissertation abstracts (www.dissonline.de; www.theses.com; www.proquest.co.uk/products.pq/descriptions/pqdt.shtml), searched 8 September 2014;
-
U.S. Food and Drug Administration (www.fda.gov), searched 8 September 2014;
-
European Medicines Agency (www.ema.europa.eu), searched 8 September 2014.
We used the following strategy to search The Cochrane Central Register of Controlled Trials (CENTRAL):
#1 MeSH descriptor: [Burns] explode all trees 1195
#2 (burn or burns or burned or scald*):ti,ab,kw 3823
#3 (thermal* NEXT injur*):ti,ab,kw 154
#4 #1 OR #2 OR #3 4024
#5 MeSH descriptor: [Growth Hormone] explode all trees 3004
#6 (growth NEXT hormone*):ti,ab,kw 4425
#7 rhGH:ti,ab,kw 382
#8 somatotropin:ti,ab,kw 113
#9 #5 OR #6 OR #7 OR #8 4455
#10 #4 AND #9 65
Additional search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 2.
We did not restrict studies with respect to language, date of publication or study setting. We considered and included abstracts and letters if we were able to obtain complete manuscripts from the study author(s).
Searching other resources
Manual searches
We searched the following journals manually:
-
Annals of Burns and Fire Disasters (1987 to September 2014);
-
(http://www.journalofburnsandwounds.com). Since 2008, this journal has been called ePlasty (http://www.eplasty.com) (2004 to 2014).
We searched scientific conference proceedings for the following associations (1995 to 2014) manually:
-
Asia‐Pacific Burns Association;
-
European Burns Association (EBA);
-
American Burn Association (ABA);
-
Australian and New Zealand Burns Association (ANZBA);
-
Mediterranean Council for Burns and Fire Disasters (MBC);
-
European Paediatric Burn Club (ECPB);
-
South African Burns Society;
-
International Society for Burn Injury (ISBI).
We performed manual searches of conference proceedings to identify papers, authors and grey literature related primarily to managing the hypermetabolic stress response. When only abstracts were available, we contacted the authors to request further information and full publications.
Grey literature and unpublished studies
We contacted authors and recognised experts in the field of acute burn management. We made formal requests for unpublished manuscripts by email to corresponding authors from the short list of identified publications.
We reviewed the following grey literature Internet web sites for appropriate studies and we contacted the authors as described above:
-
National Library of Medicine (http://www.nlm.nih.gov/nichsr/ehta/chapter10.html);
-
New York Academy of Medicine (http://www.nyam.org/library/grey.shtml);
-
GrayLIT Network (http://www.osti.gov/graylit/).
We reviewed the Trials Central and Current Controlled Trials databases for relevant studies registered since 2000. We searched the reference lists of retrieved articles and other systematic reviews and meta‐analyses identified using the above methods.
Data collection and analysis
Selection of studies
Two review authors independently screened the titles and abstracts of all records retrieved by the searches against the inclusion criteria to exclude obviously irrelevant studies. We retrieved as full text all citations that appeared to be relevant, and two review authors independently assessed these records against the inclusion criteria. In all instances, we resolved differences of opinion by discussion among the review authors.
Data extraction and management
Two review authors independently extracted data from the studies using paper data collection forms developed for this purpose. The standardised forms allowed the extraction of specific data, such as:
-
country of origin;
-
depth of the burn wound, size of the burn wound, burn type;
-
care setting;
-
number of participants randomised to each trial arm;
-
eligibility criteria and key baseline participant data;
-
details of the intervention (e.g., dosage, duration, type) that each group received;
-
details of any co‐interventions;
-
primary and secondary outcome(s) (with definitions);
-
outcomes data for primary and secondary outcomes (by group);
-
duration of follow‐up;
-
number of withdrawals (by group);
-
adverse events;
-
funding sources.
We resolved all differences by discussion among the review authors. Each review author checked the data independently for accuracy and one review author (WET) entered the data into Review Manager 5 (RevMan 2011). The second review author verified the data entered (RSB).
Assessment of risk of bias in included studies
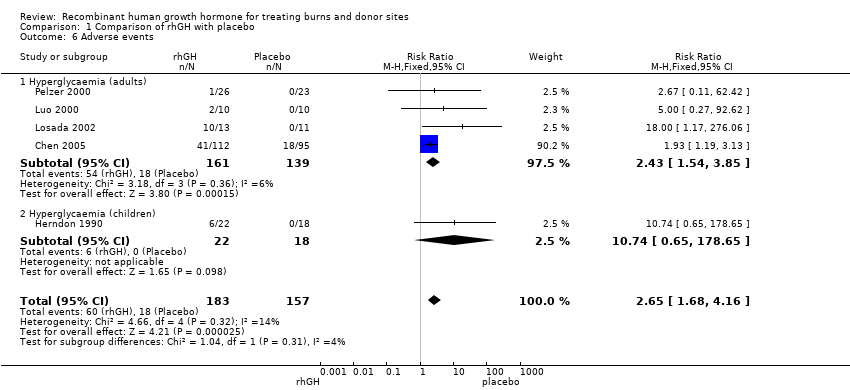
Two review authors independently assessed each included study using the Cochrane Collaboration tool for assessing the risk of bias (Higgins 2011a). This tool addresses six specific domains, namely: sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other issues (e.g., extreme baseline imbalance) (Appendix 3). We assessed blinding and the completeness of outcome data for each outcome separately. We completed a 'Risk of bias' table for each eligible study and discussed any disagreements amongst all review authors to achieve a consensus. We present the assessment of the risk of bias using a 'Risk of bias' summary figure, which presents all of the judgements in a study‐by‐entry cross‐tabulation (Figure 1). This display of internal validity indicates the weight the reader may give to each study's results.
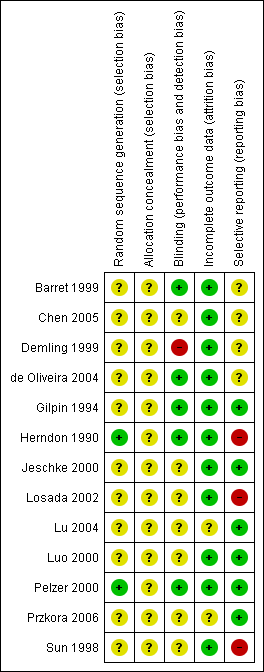
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
For data analysis, we followed the guidelines outlined in Section 9 of the Cochrane Handbook for Systematic Reviews of Interventions 5.0.1 (Deeks 2011).
We reported dichotomous outcomes (e.g., mortality) as risk ratios (RRs) with 95% confidence intervals (CIs). For continuous data, we presented results as the mean differences (MD) with 95% Cls. We used the standardised mean difference (SMD) when the studies assessed the same outcome, but used different scales (e.g., Vancouver Scar Scale and POSAS for scar assessment). The time to complete wound healing is time‐to‐event data and the most appropriate way of summarising this type of data is to use survival analysis methods and express the intervention effect as a hazard ratio. It is not appropriate to analyse time‐to‐event data using methods for continuous outcomes (e.g., using mean times‐to‐event) because the relevant times are only known for the subset of participants who had the event. When time is analysed as a continuous variable and not all participants experience the event (i.e., they are censored) they are excluded from the analysis which almost certainly introduces bias. When all of the participants in a study had completely healed wounds (the event), the mean wound‐healing time could be used.
We used Review Manager Version 5 software to generate the figures and statistical analyses (RevMan 2011).
Unit of analysis issues
The analysis of the included studies took into account the level at which randomisation occurred.
Dealing with missing data
We analysed data according to the intention‐to‐treat principle, i.e., all people included in the study at the point of randomisation were analysed according to their assigned treatment group, regardless of whether treatment was completed. Whenever possible, we contacted the original investigators to request missing data. We did not impute data if the missing data were not provided after several attempts to contact the study author. The potential impact of missing data on the review findings is addressed in the Discussion section.
Assessment of heterogeneity
The study synthesis methods depended on study quality, design and heterogeneity. We explored both clinical and statistical heterogeneity. In statistical heterogeneity the reported effect size is not consistent across studies. Clinical heterogeneity is characterised by a difference in study design; for instance, in the mixes of participants and in the implementation of interventions. We assessed heterogeneity between study results statistically using the I² statistic (Higgins 2003). This approach examines the percentage of the total variation across studies that is due to heterogeneity rather than chance. If the heterogeneity was more than 50% we used a random‐effects model instead of a fixed‐effect model when pooling was appropriate.
Assessment of reporting biases
We planned to assess reporting bias graphically using a funnel plot. We planned to report separately for each primary outcome; however, it must be recognised that if the number of eligible studies is small, the results are likely to be inconclusive (Egger 1997). The number of studies that could be pooled was very small (two to five studies), therefore this portion of the analysis was not undertaken.
Data synthesis
We examined clinical and methodological heterogeneity with reference to the study population (gender, age and TBSA percentage), intervention and outcome. In the absence of clinical and statistical heterogeneity, we used a fixed‐effect model to pool data. We investigated the cause of heterogeneity. In the presence of statistical heterogeneity (as estimated by an I² greater than 50%), we either applied a random‐effects model to pool the data or did not pool the data but undertook a narrative overview.
Subgroup analysis and investigation of heterogeneity
When we identified studies that included both adults and children, we presented the main effects for children and adults separately, data permitting.
Sensitivity analysis
We considered studies to have a high risk of bias if randomisation sequence generation, allocation concealment and outcome assessment blinding methods were inadequate or unclear. We performed a sensitivity analysis that omitted studies with a high risk of bias.
Results
Description of studies
Results of the search
The searches retrieved a total of 78 records (Figure 2). Independent scrutiny of the titles and abstracts identified 27 potentially relevant articles. We assessed these in full‐text and subsequently excluded 14 studies. The remaining 13 studies were eligible for inclusion in the review. Six studies included only children and seven included only adults. Five studies (Barret 1999; Demling 1999; Jeschke 2000; de Oliveira 2004; Przkora 2006) could not be included in a quantitative synthesis (meta‐analysis). New searches for the first update of the review in September 2014 did not yield any further studies.

Study flow diagram.
Included studies
See: Characteristics of included studies.
Thirteen studies with 701 participants met the inclusion criteria. Six RCTs included 289 children (Herndon 1990; Gilpin 1994; Barret 1999; Jeschke 2000; de Oliveira 2004; Przkora 2006); seven RCTs included 412 adults (Sun 1998; Demling 1999; Luo 2000; Pelzer 2000; Losada 2002; Lu 2004; Chen 2005).
Design
Twelve RCTs were two‐armed trials with two independent groups, 11 trials compared rhGH injections with placebo injections (Herndon 1990; Gilpin 1994; Sun 1998; Barret 1999; Demling 1999; Jeschke 2000; Luo 2000; Pelzer 2000; Losada 2002; de Oliveira 2004; Chen 2005; Przkora 2006) one trial compared rhGH injections with oral oxandrolone (Demling 1999). One trial was a three‐arm trial comparing oral glycine, oral glutamine and oral glutamine with rhGH injections (Lu 2004); however only the last two arms were included in this review.
Sample size
The sample sizes ranged from 16 (Sun 1998) to 207 (Chen 2005) people. The child study sample sizes ranged from 27 (Herndon 1990) to 94 (Barret 1999) participants, with a mean of 47; the adult study sample sizes ranged from 16 (Sun 1998) to 207 (Chen 2005), with a mean of 48.
Setting
All 13 trials took place in hospitals (burn centres), but two trials also continued after patient discharge (de Oliveira 2004; Przkora 2006). Seven studies were performed in the United States (Herndon 1990; Gilpin 1994; Barret 1999; Demling 1999; Jeschke 2000; de Oliveira 2004; Przkora 2006), four in China (Sun 1998; Luo 2000; Lu 2004; Chen 2005), one in Germany (Pelzer 2000) and one in Spain (Losada 2002). Six trials took place in the same institution (Herndon 1990; Gilpin 1994; Barret 1999; Jeschke 2000; de Oliveira 2004; Przkora 2006). The following five studies described explicitly obtaining informed consent for the study from the patient or relatives: Pelzer 2000; Losada 2002; de Oliveira 2004; Chen 2005; Przkora 2006.
Participants
Six RCTs included 289 children (Herndon 1990; Gilpin 1994; Barret 1999; Jeschke 2000; de Oliveira 2004; Przkora 2006) and the other seven RCTs included 412 adults (Sun 1998; Demling 1999; Luo 2000; Pelzer 2000; Losada 2002; Lu 2004; Chen 2005). Ages ranged from one to 65 years. The mean TBSA of the included participants was greater than 40% and the mean full‐thickness (third‐degree) TBSA was greater than 20%. Nine studies reported the male‐to‐female ratio (Gilpin 1994; Barret 1999; Jeschke 2000; Luo 2000; Pelzer 2000; Losada 2002; de Oliveira 2004; Chen 2005; Przkora 2006). The percentage of males ranged from 60% (de Oliveira 2004) to 90% (Pelzer 2000), with a mean of 72%.
Interventions
Eleven trials compared rhGH with placebo (Herndon 1990; Gilpin 1994; Sun 1998; Barret 1999; Jeschke 2000; Luo 2000; Pelzer 2000; Losada 2002; de Oliveira 2004; Chen 2005; Przkora 2006). One trial compared rhGH with oxandrolone (Demling 1999) and one trial compared oral glutamine with oral glutamine combined with rhGH injections (Lu 2004). The doses of rhGH used were 0.05 mg/kg/day in two trials (de Oliveira 2004; Przkora 2006), 0.1 mg/kg/day in one trial (Demling 1999), 0.15 mg/kg/day in one trial (Losada 2002), 0.2 mg/kg/day in four trials (Herndon 1990; Gilpin 1994; Barret 1999; Jeschke 2000), 0.19 IU/kg/day in one trial (Chen 2005), 0.2 IU/kg/day in one trial (Lu 2004), 0.3 IU/kg/day in one trial (Sun 1998) and 0.5 IU/kg/day in two trials (Luo 2000; Pelzer 2000). The oxandrolone dose was 20 mg given orally (Demling 1999). In six of the 12 rhGH trials, the control injections contained saline (Herndon 1990; Sun 1998; Barret 1999; Jeschke 2000; Luo 2000; Chen 2005); in one study, the control injections contained water with cresol (a neutral carrier substance) (Pelzer 2000), and in four studies the control substance was not reported (Gilpin 1994; Losada 2002; de Oliveira 2004; Przkora 2006). In one study, 0.5 g/kg/day of glutamine was given orally to both the control group and to the rhGH group, but the control group received no placebo injections (Lu 2004).
Outcomes
Not all trials reported on all outcome measures. The following outcomes were reported: burn wound healing time in days (Sun 1998; Luo 2000), burn wound healing rate (on the 30th postburn day Sun 1998; Lu 2004), donor site healing time in adults (Sun 1998; Demling 1999; Luo 2000; Losada 2002), donor site healing time in children (Herndon 1990; Gilpin 1994), mortality (Sun 1998; Jeschke 2000; Pelzer 2000; Losada 2002; Chen 2005; of which one study described the mortality in children: Jeschke 2000), length of hospital stay in adults (Sun 1998; Demling 1999; Luo 2000; Losada 2002; Lu 2004) and in children (Herndon 1990; Jeschke 2000), percentage of children requiring reconstruction (Barret 1999), number of reconstructive procedures in children (Przkora 2006), scar scales in children (de Oliveira 2004), septicaemia (Sun 1998; Luo 2000; Losada 2002; Chen 2005) and hyperglycaemia (in adults: Demling 1999; Luo 2000; Pelzer 2000; Losada 2002; Chen 2005 and in children: Herndon 1990).
Excluded studies
See: Characteristics of excluded studies.
In total 14 studies were excluded from the review. Twelve of the excluded studies addressed none of the pre‐specified outcome measures, reporting metabolic outcome measures, growth, weight, cardiac and pulmonary function (Aarsland 1996; Klein 1998; Chrysopoulo 1999; Low 1999; Chai 2002a; Chai 2002b; Hart 2002; Suman 2003; Suman 2004; Mlcak 2005; Jeschke 2008; Branski 2009). In addition, one study was excluded because it was a controlled clinical trial and not a RCT (Herndon 1995) and one study was excluded because it had zero events of hyperglycaemia in the rhGH and placebo groups (Hart 2001).
Risk of bias in included studies
Details of the risk of bias assessment are provided in the table Characteristics of included studies. Additionally, a descriptive analysis of the studies is provided below. In general, study quality was assessed as having a low or unclear risk of bias. A summary of the risk of bias is provided in Figure 1.
Allocation
Adequate sequence generation
The method of randomisation was described in only two of the 13 studies (Herndon 1990; Pelzer 2000). In the other articles, no information was reported about the random component of the sequence generation process.
Allocation concealment
Allocation concealment was not clearly reported in any of the 13 studies.
Blinding
Four studies stated that the injection vials contents (saline or rhGH) were blinded for participants, nurses and physicians (Herndon 1990; Gilpin 1994; Barret 1999; Pelzer 2000). In one study, the drugs (oxandrolone) could not be blinded because one was provided parenterally and the other was given orally (Demling 1999). And in a second study blinding was not performed, because the control group received no injections but glutamine orally (Lu 2004). Only two studies reported using blinded outcome observers for scar assessment (Barret 1999; de Oliveira 2004).
Incomplete outcome data
All studies either had no incomplete data for the pre‐specified outcomes (Herndon 1990; Gilpin 1994; Sun 1998; Demling 1999; Jeschke 2000; Luo 2000; de Oliveira 2004) or the missing data were balanced in numbers across intervention groups (Barret 1999; Pelzer 2000; Losada 2002; Chen 2005 ; Przkora 2006). In Pelzer 2000, five of the 23 placebo group participants and seven of the 26 rhGH group participants dropped out, representing a 24% dropout rate for the entire group of participants. However, seven of the dropouts in this study were caused by mortality, which was an outcome measure. In Przkora 2006, which had a one‐year follow‐up, seven of the 19 placebo group participants and five of the 25 rhGH group participants dropped out, representing a 27% dropout rate for all participants.
Selective reporting
None of the studies provided a study protocol. The studies by Gilpin 1994; Jeschke 2000; Luo 2000; Pelzer 2000; Lu 2004 and Przkora 2006 were at low risk of bias for this domain as they reported the pre‐specified outcomes in the study. The studies by Barret 1999; Demling 1999; de Oliveira 2004 and Chen 2005 provided insufficient information about the criteria used to judge selective outcome reporting and are at unclear risk of bias. The outcome measures incorporated into this meta‐analysis from the studies by Herndon 1990; Sun 1998 and Losada 2002 were not pre‐specified in the methods of the articles and this represents a high risk of reporting bias for this domain.
Effects of interventions
We analysed trials involving adults and children separately, except for the outcomes mortality and hyperglycaemia for which we analysed the trials in adults and children both separately and together.
Comparison of rhGH with placebo
Primary outcomes
Healing rate of burn wounds (adults)
For the primary outcome of the healing rate of burn wounds in adults, four studies compared recombinant human growth hormone (rhGH) and placebo and measured the outcome in three different ways (Sun 1998; Luo 2000; Pelzer 2000; Lu 2004).
Two studies reported mean wound healing time in days and we pooled them. The time to complete wound healing is time‐to‐event data but because all participants were followed until complete wound healing, the data can be analysed as if time is a continuous variable since no participants were censored. The mean wound healing time was statistically significantly shorter with rhGH treatment compared with placebo (Analysis 1.1: mean difference (MD) ‐9.07 days; 95% confidence interval (CI) ‐13.76 to ‐4.39; I² = 0%; Sun 1998; Luo 2000). We did not pool two studies that estimated the wound healing rate on the 30th post‐burn day (Lu 2004; Sun 1998) because of considerable heterogeneity (I² = 88%) and the compared treatments were different between the studies. Wound healing rate on the 30th post‐burn day could mean how many wounds have completely healed at day 30 or how much on average (percentage) is healed by day 30 and the definition of wound healing rate at day 30 was unclear in both Sun 1998 and Lu 2004. The wound healing rate on the 30th post‐burn day was significantly higher after rhGH treatment in both studies (Sun 1998 MD 20.10%; 95% CI 12.46 to 27.74; Lu 2004 MD 8.00%; 95% CI 4.58 to 11.42). The heterogeneity of these studies could be explained by a larger mean total % total body surface area (TBSA) and a larger mean % full‐thickness burn in the study by Sun 1998. In Lu 2004 the control group did not receive injections, as in the study by Sun 1998; instead controls received oral glutamine, which accelerated the wound healing rate in comparison with a third patient group that received oral glycine. Therefore, the wound healing rate difference in this study could be reduced by the glutamine effect. Pelzer 2000 did not report standard deviations of the wound closure index. The trial report states that the wound closure index was not significantly higher after 0.5 IU/kg/day of rhGH for 28 days, starting on second post‐burn day (P < 0.2); however, this could not be confirmed due to missing data.
Donor site healing
Adults
Three studies involving adults reported this outcome (Sun 1998; Luo 2000; Losada 2002). Although time to complete wound healing is a type of time‐to‐event data and was not analysed in these studies using survival methods, all participants were followed until complete wound healing therefore the mean time to wound healing can be presented. We pooled two studies (Sun 1998; Luo 2000;) because pooling three studies caused considerable heterogeneity (I² = 81%). Donor site healing was statistically significantly shorter in the rhGH group compared with the other groups (Analysis 1.2: MD ‐3.15 days; 95% CI ‐4.75 to ‐1.54). The mean wound healing time was not significantly different between placebo and rhGH group in Losada 2002 (MD ‐0.28 days; 95% CI ‐0.94 to 0.38). The standard deviations of the donor site healing time were smaller in the Losada 2002 study than in the Sun 1998 and Luo 2000 studies. In Sun 1998 and Luo 2000 the method used to assess healing time was not reported; and in Losada 2002 the donor site was defined as being healed when it was adequate for harvesting as a new autograft donor site. This could have introduced a difference in the healing time variability in the studies.
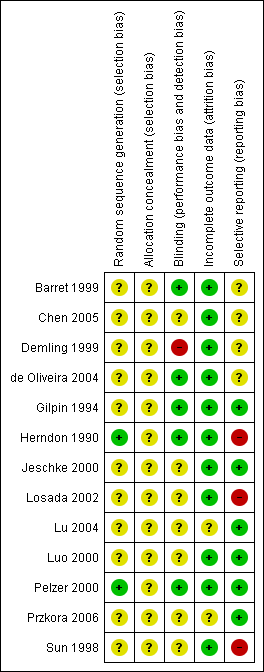
Children
We pooled two studies involving children (Herndon 1990; Gilpin 1994). The donor site healed significantly more quickly after rhGH treatment compared with placebo injections (Analysis 1.3: MD ‐1.70; 95% CI ‐2.53 to ‐0.87; I² = 0%)
Wound infections
No studies reported this outcome.
Mortality
We pooled data from the four studies involving adults (Sun 1998; Pelzer 2000; Losada 2002; Chen 2005). Overall there were 15 deaths; 5 in the rhGH groups and 10 in the placebo groups however this difference was not statistically significant, possibly due to lack of statistical power (Analysis 1.5.1: risk ratio (RR) 0.48; 95% CI 0.19 to 1.25; P = 0.13; I² = 0%). One study involving children (Jeschke 2000) found no statistically significant difference in mortality between rhGH and placebo (Analysis 1.5.2: RR 1.15; 95% CI 0.08 to 16.67). Combining the five studies in both adults and children resulted in no statistically significant difference in mortality between the rhGH and placebo groups (Analysis 1.5: RR = 0.53; 95% CI 0.22 to 1.29) however this comparison is underpowered with only 17 deaths in total therefore an effect on mortality cannot be ruled out.
Secondary outcomes
Length of hospital stay
We pooled four studies involving adults (Sun 1998; Luo 2000; Losada 2002; Lu 2004). Hospital stay was significantly shorter in the rhGH group compared with the placebo group (Analysis 1.4.1: MD ‐12.55 days; 95% CI ‐17.09 to ‐8.00; I² = 0%).
A study in children found no statistically significant difference in the length of hospital stay between the groups (Analysis 1.4.2: MD ‐7.00 days; 95% CI ‐29.94 to 15.94).
Burn scar formation
Three of the studies involving children reported this outcome (Barret 1999; de Oliveira 2004; Przkora 2006), but these studies could not be pooled because they used different methods to measure the outcome.
de Oliveira 2004 scored the Seattle, Hamilton and Vancouver scar scales at discharge and 6, 12 and 18 to 24 months after the burn. Photographs of the scars were evaluated using the Seattle and Hamilton Scar Scale. Clinically the most hypertrophic scars were assessed using the Vancouver Scar Scale. A higher score on these scar assessment scales indicates a worse outcome. The Seattle Scar Scale score was not significantly different in the rhGH group compared with the placebo group at discharge (MD ‐0.25; 95% CI ‐1.50 to 1.00), at six months (MD ‐0.05; 95% CI ‐1.55 to 01.45), nine months (MD ‐0.93; 95% CI ‐2.31 to 0.45), 12 months (MD ‐0.24; 95% CI ‐1.93 to 1.45) or 18 to 24 months after the burn (MD ‐0.78; 95% CI ‐2.91 to 1.35). The Hamilton Scar Scale was not significantly different in the rhGH group compared to the placebo group at discharge (MD ‐0.40; 95% CI ‐1.51 to 0.71) or at six months (MD ‐0.24; 95% CI ‐1.20 to 0.72), nine months (MD ‐0.50; 95% CI ‐2.05 to 1.05), 12 months (MD ‐0.50; 95% CI ‐2.09 to 1.09) or 18 to 24 months after burn (MD ‐0.83; 95% CI ‐2.51 to 0.85). The Vancouver Scar Scale was not significantly different in the rhGH group compared to the placebo group at discharge (MD ‐1.86; 95% CI ‐4.07 to 0.35), at six months (MD ‐1.51; 95% CI ‐4.04 to 1.02), at nine months (MD ‐1.60; 95% CI ‐5.56 to 2.36) or at 18 to 24 months after burn (MD ‐0.50; 95% CI ‐2.66 to 1.66); the Vancouver Scar Scale was significantly lower in the rhGH group compared with the placebo group at 12 months (MD ‐1.90; 95% CI ‐3.31 to ‐0.49).
One study, which provided no data, reported no significant difference in the Vancouver Scar Scale scores in the rhGH group compared with placebo after discharge or up to 24 months after the burn (Przkora 2006). Barret 1999 reported no difference between the burn scar rating scale scores of children who received a placebo and those who received rhGH during the acute phase of the hospital stay. These data could not be pooled because ranges should not be used to calculate standard deviations (Higgins 2011b).
Adverse events
Hyperglycaemia
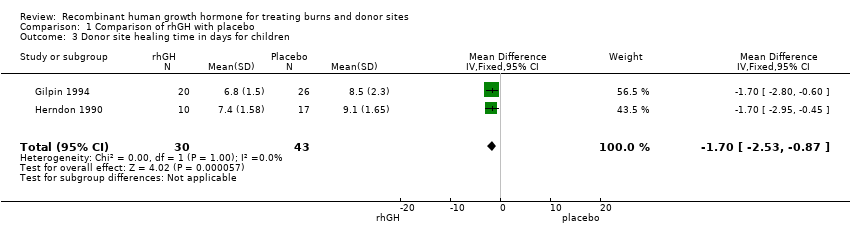
Four adult studies (Luo 2000; Pelzer 2000; Losada 2002; Chen 2005; 300 participants, 72 events) and one child study (Herndon 1990; 40 participants, six events) reported the incidence of hyperglycaemia. In adults, the incidence was significantly higher in the rhGH group than in the placebo group (Analysis 1.6.1: RR 2.43; 95% CI 1.54 to 3.85; I² = 6%). In children whilst there was a difference in the incidence of hyperglycaemia (6 cases in the rHGH group and none in the placebo group) this difference was not statistically significant, probably due to lack of statistical power (Analysis 1.6.2: RR 10.74; 95% CI 0.65 to 178.65). Combining data for the adults and children yielded an incidence that was significantly higher in the rhGH group than in the placebo group (Analysis 1.6: RR 2.65; 95% CI 1.68 to 4.16; I² = 14%).
Septicaemia
Four studies reported septicaemia data in adults and we pooled them (Sun 1998; Luo 2000; Losada 2002; Chen 2005). There was no statistically significant difference in the proportion of participants with septicaemia between rhGH and placebo (Analysis 1.7: RR 0.61; 95% CI 0.31 to 1.22; I² = 0%).
Quality of life
No studies reported this outcome.
Comparison of rhGH with oxandrolone
One study compared rhGH with oxandrolone in adults (Demling 1999). There was no significant difference in the donor site healing time between the two treatment groups (Analysis 2.1: MD 0.00; 95% CI ‐1.64 to 1.64). All participants were followed until complete wound healing, therefore the time‐to‐event data are presented correctly. No participants were censored; therefore, the mean wound healing time is presented. The incidence of hyperglycaemia was significantly higher in the rhGH group than in the oxandrolone group (36 participants, 28 events; Analysis 2.2: RR 1.95; 95% CI 1.21 to 3.16).
Discussion
This systematic review summarises the best available evidence about the effects of recombinant human growth hormone (rhGH) for treating burns and donor sites. Thirteen randomised controlled trials met the inclusion criteria for this review. The mean total body surface area (TBSA) of the included participants was greater than 40%, and the mean full‐thickness (third‐degree) TBSA was greater than 20%. Therefore, all of the participants had serious burn injuries.
Our results indicate some preliminary evidence that burn wounds and donor sites in children and adults heal more rapidly when rhGH is administered and that length of hospital stay in adults is also shorter with rhGH compared to placebo. The statistically significant differences between rhGH and placebo administration are clinically meaningful and include a nine‐day reduction in the wound healing time in adults (Analysis 1.1) and a three‐day reduction in the donor site healing time in adults (Analysis 1.2) and a nearly two‐day reduction in the donor site healing time in children (Analysis 1.3). No evidence of a shorter hospital stay was reported when rhGH was administered to children. Whilst the differences in mortality between rhGH and placebo‐treated groups in adults and children were not statistically significant, mortality is a rare outcome and the number of included participants was small; therefore even after pooling there may not have been sufficient statistical power to detect a real difference in mortality as statistically significant. There was no evidence of a difference in septicaemia when rhGH and placebo groups in adults were compared. Three scar assessment scales showed no difference between children who received rhGH for a year after discharge and those who received placebo (de Oliveira 2004). Our results indicate that hyperglycaemia, as an adverse event, was more frequent after rhGH treatment than after placebo or oxandrolone therapy. Hyperglycaemia itself is associated with the hyper metabolic stress response and is related to increased mortality in severe burns (Gore 2001). The hyperglycaemia induced by rhGH is associated with insulin resistance (Gore 1991). However the effect of rhGH‐induced hyperglycaemia on hypermetabolism is unknown. There is evidence from one study (Demling 1999) that no difference exists in donor site healing, length of hospital stay or weight loss in groups of participants treated with rhGH or oxandrolone.
The summary of finding table, which was prepared with the software GRADEprofiler (GRADEpro), indicates clearly the low quality of the evidence for all the outcomes. No large effects were found in the studies. The risk of bias caused by imprecision was serious, because the studies included few participants and few events. This low quality of the evidence reduces the ability to make firm statements about what the evidence tells exactly about the treatment effects.
These results must therefore be interpreted with caution. The included studies often could not be pooled because they used different methods to measure outcomes. For instance, various studies measured wound healing time in adults in days, as a healing rate or with a wound closure index. Many of the studies included a small number of participants. No studies with wound healing time data in children could be found. We found no studies with wound infections as a primary outcome and no studies comparing rhGH and propranolol using the pre‐specified outcomes.
In general, the study quality was limited by failures to report randomisation techniques, allocation concealment and blinding. Eleven of the 13 studies included in this review did not mention the randomisation method, which may imply that several of these studies are not randomised controlled trials (RCTs), but controlled clinical trials. Blinding at outcome assessment is very important for outcome measures, such as the healing of burn wounds or donor sites, because it is difficult to determine when wound epithelisation is complete. Data, especially standard deviations, were sometimes missing, or outcomes were only presented in figures. The authors of the included studies could not (Barret 1999; Przkora 2006) or were not willing to (Pelzer 2000) provide missing data upon our request. The authors of this review cannot rule out selection bias and language bias when searching the Chinese literature. Due to the uncertainty about the amount of missing data, its impact on the findings of this review could not be estimated.
The costs of rhGH treatment are USD 300 to 600 per day, which could be counterbalanced by a reduction in hospital stay. However, no economic analyses to prove this were retrieved, and these costs are only a part of the overall expense of burn injury treatment. The high cost of this long‐term treatment could be a great disadvantage and hindrance to its wide application, especially in developing nations.
A review of metabolic support for burn injury that used some of the same literature included in this review came to the same conclusions about rhGH administration: it is associated with reduced wound healing time, reduced length of hospital stay and no increase in scarring, and increased hyperglycaemia as an adverse effect (Herndon 2004). A study by Ramirez 1998 analysed the records of 130 children who received rhGH in RCTs. These children were compared with 133 controls. No difference in mortality (2%) was found. Concern about the mortality related to rhGH administration arose after the publication of two RCTs that showed increased morbidity and mortality in non‐burned critically ill adults who were treated with rhGH (Takala 1999). The studies included in this review were not primarily designed to study the effect of rhGH on mortality and their sample sizes were small, therefore no definite conclusion can be drawn about the differences in mortality between rhGH‐ and placebo‐treated participants.
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Comparison of rhGH with placebo, Outcome 1 Healing time of burn wounds in days for adults.

Comparison 1 Comparison of rhGH with placebo, Outcome 2 Donor site healing time in days for adults.
Comparison 1 Comparison of rhGH with placebo, Outcome 3 Donor site healing time in days for children.

Comparison 1 Comparison of rhGH with placebo, Outcome 4 Length of hospital stay.

Comparison 1 Comparison of rhGH with placebo, Outcome 5 Mortality.
Comparison 1 Comparison of rhGH with placebo, Outcome 6 Adverse events.
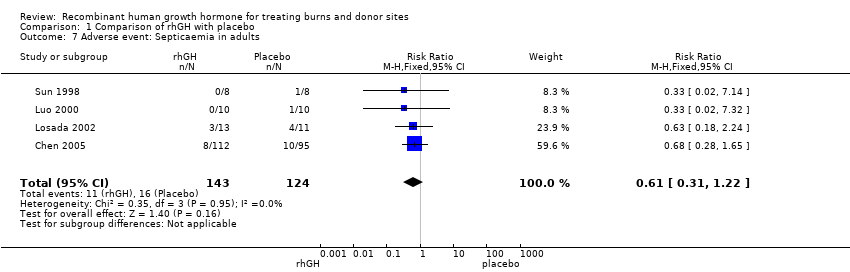
Comparison 1 Comparison of rhGH with placebo, Outcome 7 Adverse event: Septicaemia in adults.

Comparison 2 Comparison of rhGH with oxandrolone, Outcome 1 Donor site healing in days.

Comparison 2 Comparison of rhGH with oxandrolone, Outcome 2 Hyperglycaemia (blood glucose > 225 mg/dl).
| Recombinant human growth hormone compared with placebo for treating burns and donor sites | ||||||
| Patient or population: | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Recombinant human growth hormone | ||||||
| Healing time of burn wounds in days for adults | The mean healing time of burn wounds in days for adults in the intervention groups was 9.07 lower (4.39 to 13.76 lower) | 36 | ⊕⊕⊝⊝ | |||
| Donor site healing time in days for adults | The mean donor site healing time in days for adults in the intervention groups was | 36 | ⊕⊕⊝⊝ | |||
| Donor site healing time in days for children | The mean donor site healing time in days for children in the intervention groups was | 73 (2 studies) | ⊕⊕⊝⊝ | |||
| Mortality in adults and children | Study population5 | RR 0.53 | 324 | ⊕⊕⊝⊝ | ||
| 7 per 100 | 4 per 100 (2 to 9) | |||||
| Low5 | ||||||
| 5 per 100 | 3 per 100 (1 to 6) | |||||
| High5 | ||||||
| 13 per 100 | 7 per 100 (3 to 17) | |||||
| Septicaemia in adults | Study population8 | RR 0.61 | 267 | ⊕⊕⊝⊝ | ||
| 13 per 100 | 8 per 100 (4 to 16) | |||||
| Low8 | ||||||
| 4 per 100 | 2 per 100 (1 to 5) | |||||
| High8 | ||||||
| 13 per 100 | 8 per 100 (4 to 16) | |||||
| Hyperglycaemia in adults and children | Study population10 | RR 2.65 | 340 | ⊕⊕⊝⊝ | ||
| 11 per 100 | 30 per 100 (19 to 48) | |||||
| Low10 | ||||||
| 0 per 100 | 0 per 100 (0 to 0) | |||||
| High10 | ||||||
| 19 per 100 | 50 per 100 (32 to 79) | |||||
| Length of hospital stay in days for adults | The mean length of hospital stay in days for adults in the intervention groups was | 99 | ⊕⊕⊝⊝ | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Method of randomisation, allocation concealment and blinding not reported. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Healing time of burn wounds in days for adults Show forest plot | 2 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐9.07 [‐13.76, ‐4.39] |
| 2 Donor site healing time in days for adults Show forest plot | 2 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐3.15 [‐4.75, ‐1.54] |
| 3 Donor site healing time in days for children Show forest plot | 2 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.53, ‐0.87] |
| 4 Length of hospital stay Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Adults | 4 | 99 | Mean Difference (IV, Fixed, 95% CI) | ‐12.55 [‐17.09, ‐8.00] |
| 4.2 Children | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | ‐7.0 [‐29.94, 15.94] |
| 5 Mortality Show forest plot | 5 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.22, 1.29] |
| 5.1 Adults | 4 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.19, 1.25] |
| 5.2 Children | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.08, 16.67] |
| 6 Adverse events Show forest plot | 5 | 340 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.65 [1.68, 4.16] |
| 6.1 Hyperglycaemia (adults) | 4 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.43 [1.54, 3.85] |
| 6.2 Hyperglycaemia (children) | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 10.74 [0.65, 178.65] |
| 7 Adverse event: Septicaemia in adults Show forest plot | 4 | 267 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.31, 1.22] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Donor site healing in days Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Hyperglycaemia (blood glucose > 225 mg/dl) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

