Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea
Information
- DOI:
- https://doi.org/10.1002/14651858.CD007736.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 08 January 2014see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Airways Group
- Copyright:
-
- Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
DRW: Study assessment (2013); data extraction, data entry and analysis (2013); write‐up (2013).
TJL: Study assessment (2009); data extraction, data entry and analysis (2009); write‐up (2013).
IS: Study assessment; data extraction and analysis, write‐up (2009 and 2013).
Previous author(s) no longer contributing to this version of the review:
Vidya Nadig (2009): study assessment; data extraction; write‐up.
Sources of support
Internal sources
-
St George's, University of London, UK.
-
Papworh NHS Trust, UK.
External sources
-
No sources of support supplied
Declarations of interest
None known.
Acknowledgements
We are very grateful to the members of the Cochrane Airways Group editorial base, who provided support with searching for and retrieving studies for inclusion in the review, and to Prof John Wright for constructive comments on the protocol and the review. We are very grateful for assistance given to us by study authors who responded to our requests for additional data and information: Mark Aloia (Aloia 2001; Aloia 2012a; Aloia 2012b); Keir Lewis (Lewis 2006); Carol Smith (Schiefelbein 2005, Smith 2006); Carl Stepnowsky (Stepnowsky 2007); Delwyn Bartlett (Bartlett 2010); Domagoj Damjanovic (Damjanovic 2009); Ozen K Basoglu (Basoglu 2011); George Zaldivar (Shaikh 2009); Sairam Parthasarathy (Parthasarathy 2012); and Simon Smith (Olsen 2012). We acknowledge the contribution of Vidya Nadig to the previous version of this review.
John White was the Editor for this review and commented critically on the review.
Version history
| Published | Title | Stage | Authors | Version |
| 2020 Apr 07 | Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea | Review | Kathleen Askland, Lauren Wright, Dariusz R Wozniak, Talia Emmanuel, Jessica Caston, Ian Smith | |
| 2014 Jan 08 | Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea | Review | Dariusz R Wozniak, Toby J Lasserson, Ian Smith | |
| 2009 Apr 15 | Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea | Review | Ian Smith, Vidya Nadig, Toby J Lasserson | |
Differences between protocol and review
This review incorporates a risk of bias table for eligible studies, and we performed post hoc subgroup analysis based on awareness of machine monitoring and average compliance with CPAP in the control arm using four hours/night as the cutoff.
We have incorporated summary of findings tables for the three comparisons in this review.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Patient Compliance;
- Cognitive Behavioral Therapy [*methods];
- Continuous Positive Airway Pressure [instrumentation, *statistics & numerical data];
- Motivation;
- Patient Education as Topic [*methods];
- Randomized Controlled Trials as Topic;
- Reinforcement, Psychology;
- Sleep Apnea, Obstructive [psychology, *therapy];
Medical Subject Headings Check Words
Adult; Humans;
PICOs

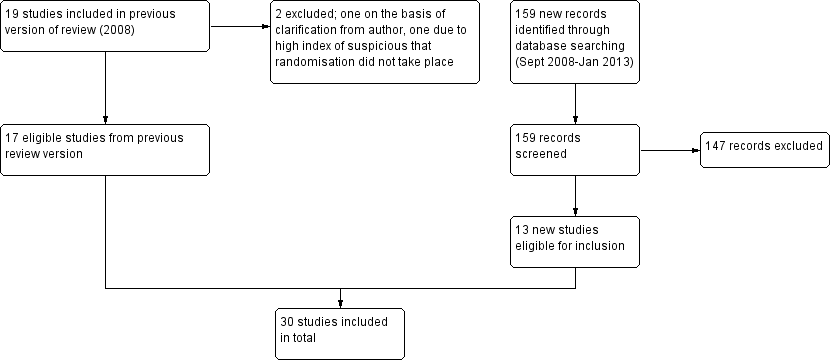
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

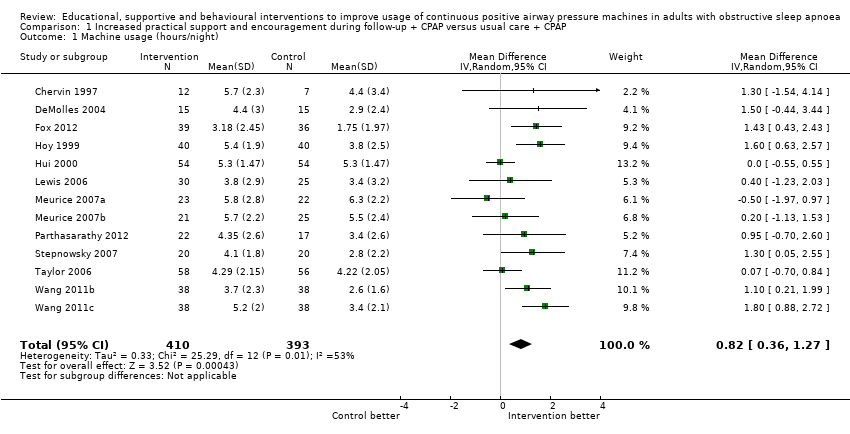
Forest plot of comparison: 1 Increased psychological and/or practical support during follow‐up + CPAP versus usual care + CPAP, outcome: 1.1 Machine usage (hours/night)—first arm/parallel studies.
Forest plot of comparison: 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, outcome: 1.3 Machine usage, sensitivity analysis: adherence in control group =< four hours/night.

Funnel plot of comparison: 1 Increased practical support and encouragement + CPAP versus usual care + CPAP, outcome: 1.1 Machine usage (hours/night).

Forest plot of comparison: 2 Educational interventions + CPAP versus usual care + CPAP, outcome: 2.1 Machine usage (hours/night).

Forest plot of comparison: 4 Behavioural therapy + CPAP versus control + CPAP, outcome: 4.1 Machine usage.
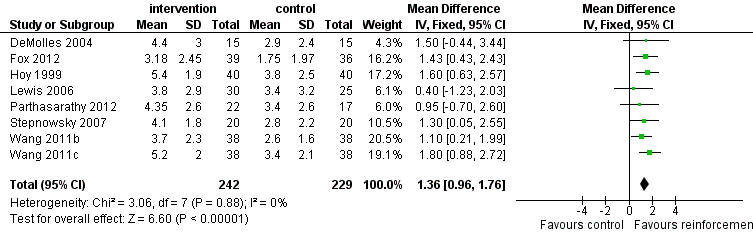
Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 1 Machine usage (hours/night).
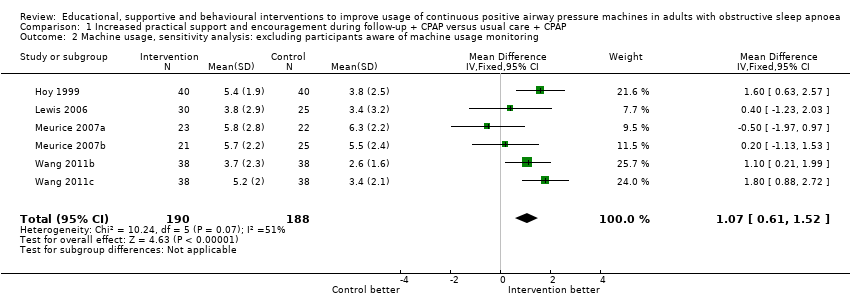
Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 2 Machine usage, sensitivity analysis: excluding participants aware of machine usage monitoring.

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 3 Machine usage, sensitivity analysis: adherence in control group < four hours/night.

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 4 N deemed adherent (≥ four hours/night).

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 5 Epworth Sleepiness Scale scores.

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 6 Quality of life: Functional Outcomes of Sleep Questionnaire.

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 7 Quality of life: Sleep Apnoea Quality of Life Index (SAQLI).

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 8 Mood.
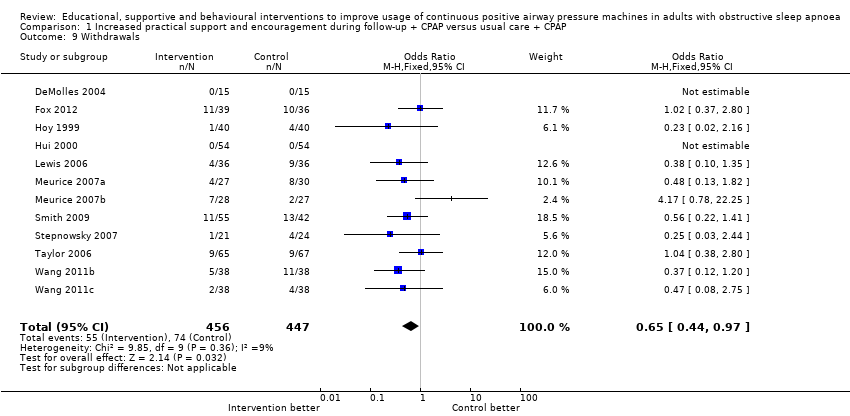
Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 9 Withdrawals.
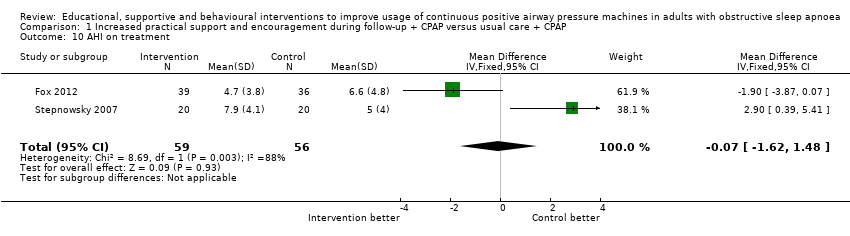
Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 10 AHI on treatment.

Comparison 1 Increased practical support and encouragement during follow‐up + CPAP versus usual care + CPAP, Outcome 11 Maintenance of Wakefulness Test (MWT).
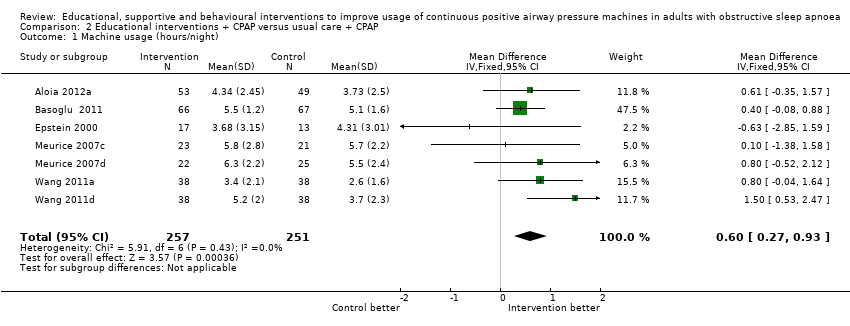
Comparison 2 Educational interventions + CPAP versus usual care + CPAP, Outcome 1 Machine usage (hours/night).

Comparison 2 Educational interventions + CPAP versus usual care + CPAP, Outcome 2 N deemed adherent (≥ four hours/night).

Comparison 2 Educational interventions + CPAP versus usual care + CPAP, Outcome 3 Epworth Sleepiness Scale scores.

Comparison 2 Educational interventions + CPAP versus usual care + CPAP, Outcome 4 Quality of life: Sleep Apnoea Quality of Life Index (SAQLI).
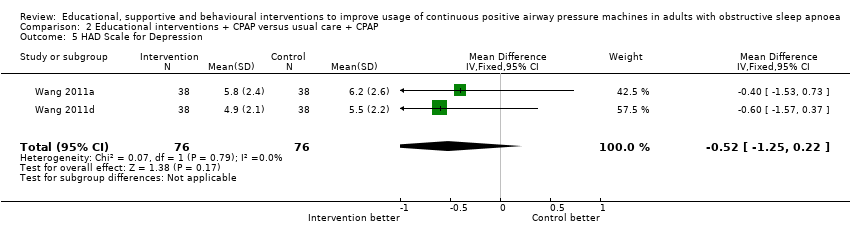
Comparison 2 Educational interventions + CPAP versus usual care + CPAP, Outcome 5 HAD Scale for Depression.

Comparison 2 Educational interventions + CPAP versus usual care + CPAP, Outcome 6 Withdrawal.

Comparison 3 Behavioural therapy + CPAP versus control + CPAP, Outcome 1 Machine usage (hours/night).
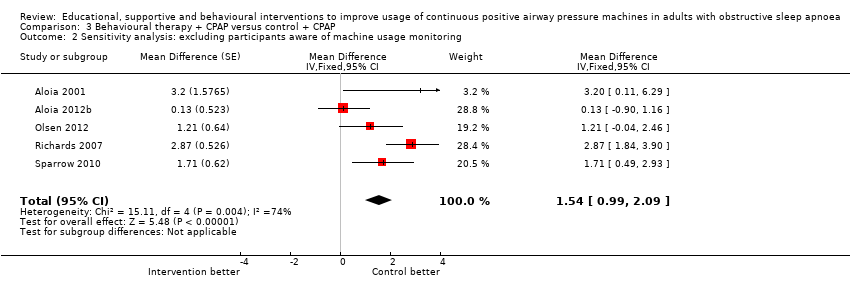
Comparison 3 Behavioural therapy + CPAP versus control + CPAP, Outcome 2 Sensitivity analysis: excluding participants aware of machine usage monitoring.

Comparison 3 Behavioural therapy + CPAP versus control + CPAP, Outcome 3 N deemed adherent (≥ four hours/night).

Comparison 3 Behavioural therapy + CPAP versus control + CPAP, Outcome 4 Epworth Sleepiness Scale score.
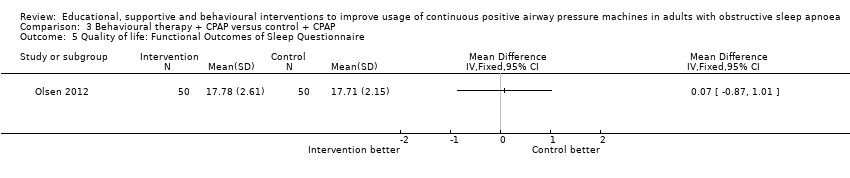
Comparison 3 Behavioural therapy + CPAP versus control + CPAP, Outcome 5 Quality of life: Functional Outcomes of Sleep Questionnaire.

Comparison 3 Behavioural therapy + CPAP versus control + CPAP, Outcome 6 Withdrawal.
| Increased practical support and encouragement for adults with sleep apnoea | ||||||
| Patient or population: adults with sleep apnoea Comparison: CPAP Settings: community | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Increased practical support and encouragement | |||||
| Machine usage | Average CPAP machine usage ranged across control groups from | Mean machine usage in the intervention groups was | 803 | ⊕⊕⊝⊝ | ||
| N deemed adherent (≥ four hours/night) | 59 per 100 | 75 per 100 | OR 2.06 | 268 | ⊕⊕⊝⊝ | |
| Symptoms of sleepiness | Average Epworth symptom scores in control groups ranged from 4.5 to 13 | Mean symptoms of sleepiness in the intervention groups was | 501 | ⊕⊝⊝⊝ | ||
| Quality of life | Mean quality of life in the intervention groups was | 70 | ⊕⊕⊝⊝ | |||
| Quality of life | See comment | See comment | 108 | ⊕⊕⊝⊝ | Single study estimate | |
| Withdrawals | 17 per 100 | 11 per 100 | OR 0.65 | 903 | ⊕⊕⊕⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| 1Risk of bias (‐1): In the absence of blinding across studies, the study effect estimates are at risk of performance bias. | ||||||
| Educational interventions for adults with sleep apnoea | ||||||
| Patient or population: adults with sleep apnoea Comparison: CPAP Settings: community | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Educational interventions | |||||
| Machine usage | Average CPAP machine usage ranged across control groups from 2.6 to 5.7 hours per night | Mean machine usage in the intervention groups was | 508 | ⊕⊕⊕⊝ | ||
| N deemed adherent (≥4 hours/night) | 57 per 100 | 71 per 100 | OR 1.8 | 285 | ⊕⊕⊝⊝ | |
| Symptoms of sleepiness | Mean Epworth Sleepiness Scale scores across control groups ranged from 5.4 to 10.8 | Mean Epworth Sleepiness Scale scores in the intervention groups was | 336 | ⊕⊕⊕⊝ | ||
| Quality of life: Sleep Apnoea Quality of Life Index (SAQLI) | See comment | See comment | Not estimable | 89 | ⊕⊝⊝⊝ | Single study estimate |
| Withdrawal | 24 per 100 | 18 per 100 | OR 0.67 | 683 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| 1Risk of bias (‐1): In the absence of blinding across studies, effect estimates may be biased because of performance bias. | ||||||
| Behavioural therapy for adults with sleep apnoea who are using CPAP | ||||||
| Patient or population: adults with sleep apnoea Comparison: CPAP Settings: community | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Behavioural therapy | |||||
| Machine usage | See comment | Average machine usage in the intervention groups was | 584 | ⊕⊕⊝⊝ | Data analysed as generic inverse variance | |
| N deemed adherent (≥4 hours/night) | 28 per 100 | 47 per 100 | OR 2.23 | 358 | ⊕⊝⊝⊝ | |
| Symptoms | See comment | See comment | 100 | ⊕⊕⊝⊝ | Single study estimate | |
| Quality of life | See comment | See comment | 100 | ⊕⊕⊝⊝ | Single study estimate | |
| Withdrawal | 23 per 100 | 20 per 100 | OR 0.85 | 609 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| 1Risk of bias (‐1): In the absence of blinding across studies, effect estimates may be biased because of performance bias. | ||||||
| Study | N Screened | Entered | Completed | % Screened | % Entered |
| NA | 12 | 12 | NA | 100 | |
| 339 | 227 | 149 | 44 | 66 | |
| 246 | 133 | 133 | 54 | 100 | |
| NA (75% of those approached agreed to participate) | 40 | 33 | NA | 82.5 | |
| NA | 30 | 30 | NA | 100 | |
| NA | 50 | 43 | NA | 86 | |
| NA | 75 | 54 | NA | 72 | |
| NA | 80 | 75 | NA | 94 | |
| NA | 108 | 108 | NA | 100 | |
| 74 | 72 | 55 | 74 | 76 | |
| 133 | 112 | 91 | 68 | 81 | |
| 132 | 100 | 73 | 55 | 73 | |
| 49 | 39 | 37 | 76 | 95 | |
| 109 | 100 | 79 | 72 | 79 | |
| NA | 30 | 28 | NA | 93 | |
| NA | 51 | 51 | NA | 100 | |
| NA | 19 | 19 | NA | 100 | |
| NA | 97 | 73 | NA | 75 | |
| 423 | 250 | 115 | 27 | 46 | |
| 91 | 45 | 40 | 44 | 88 | |
| 160 | 132 | 114 | 71 | 86 | |
| NA | 152 | 130 | NA | 86 | |
| NA | 93 | 56 | NA | 60 |
| Intervention group | Study | Intervention | Control | Study duration (weeks) | ||
| Increased support and reinforcement components | Increased educational components | Behavioural therapy | ||||
| Increased support and reinforcement | Weekly telephone calls to monitor progress and troubleshoot | Written information on OSA and CPAP | Usual care | Eight | ||
| Computer‐based telecommunication system allowing for monitoring and reinforcing compliance | Education provided by the computer‐based telecommunication system | Usual care | Eight | |||
| Telecomunication system allowing for daily monitoring of CPAP usage, timely detection and troubleshooting of problems | Usual care | 12 | ||||
| 2 additional titration nights in hospital, 4 additional visits at home by sleep nurses | Initial education at home with partner | Usual care | 24 | |||
| 2 additional early reviews by sleep physician and frequent telephone calls by sleep nurses | Videotape and additional education session | Usual care | 12 | |||
| 1 additional early review by sleep physician and 1 early telephone interview with sleep nurse | Educational video | Usual care | 52 | |||
| 4 additional home visits in the first 3 months by sleep practitioner for problem solving | Written information and detailed explanation by the prescriber, additional education during home visits | Written information and detailed explanation by the prescriber + usual care | 52 | |||
| 4 additional home visits in the first 3 months by sleep practitioner for problem solving | Additional education during home visits | Usual care | 52 | |||
| 2 individual sessions and 8 telephone conversations with trained peer CPAP users providing support and sharing their positive experience with CPAP | Peers shared their knowledge on CPAP and OSA | Interventions delivered by peer contained elements of promoting self‐efficacy, risk perception, participant activation and motivation | Usual care | 12 | ||
| Internet‐based application aimed at encouraging CPAP use and problem solving | Internet‐based application similar in format to intervention but directed activities in neutral health topics (vitamin intake) | 16 | ||||
| Home video‐link sessions delivered by nurse, who guided correct CPAP use and provided problem solving | Nurse provided education on CPAP and OSA | Home video‐link sessions similar in form to intervention but directed activities in neutral health topics (vitamin intake) | 12 | |||
| Audiotaped music along with softly spoken directions on relaxation techniques and habit‐promoting instructions for using CPAP, user reminder placard | Handouts on benefits of CPAP adherence and health consequences of poor compliance | Audiotaped music along with spoken information about vitamins. Information packet similar in format to intervention, but content was on vitamins | 24 | |||
| Wireless telemonitoring of compliance and treatment efficacy on daily basis and acting on the data via prespecified clinical pathways | Usual care | Eight | ||||
| Internet‐based application aimed at monitoring self‐reported compliance, acting on the information in timely fashion | Usual care | Four | ||||
| Progressive muscle relaxation | Usual care | 12 | ||||
| Progressive muscle relaxation + 2 additional nights of CPAP titration | 4hour group education session, written information, video CD | Two additional nights of CPAP titration + four‐hour group education session, written information, video CD + usual care | 12 | |||
| Increased education | Two 45‐minute individual didactic sessions and one booster phone call by sleep nurse | Usual care | 52 | |||
| 10‐Minute educational video session on OSA and CPAP | Usual care | 24 | ||||
| Educational and desensitisation course | Usual care | 24 | ||||
| 4 additional home visits in the first 3 months by sleep practitioner for problem solving | Written information and detailed explanation by the prescriber, additional education during home visits | Four additional home visits in the first three months by sleep practitioner for problem solving and additional education + usual care | 52 | |||
| Written information and detailed explanation by the prescriber | Usual care | 52 | ||||
| 2 additional nights of CPAP titration | Four‐hour group education session, written information, video CD | Usual care | 12 | |||
| Progressive muscle relaxation + 2 additional nights of CPAP titration | Four‐hour group education session, written information, video CD | Progressive muscle relaxation + usual care | 12 | |||
| 15‐Minute educational video addressing misconception about OSA and barriers to effective CPAP treatment | Usual care | Four | ||||
| Behavioural therapy | Elements of education on consequences of OSA and efficacy of CPAP | Two 45‐minute sessions of cognitive‐behavioural therapy interventions | Two 45‐minute sessions involving discussion on sleep architecture and sleep clinic | 12 | ||
| Two 45‐minute sessions of Motivational Enhancement Therapy, one booster phone call | Usual care | 52 | ||||
| 45‐Minute individual education session | Three 30‐minute sessions of Motivational Interviewing Therapy | 45‐Minute educational session + usual care | 52 | |||
| Slide presentation and written information on OSA and CPAP | Two one‐hour group sessions of cognitive‐behavioural therapy | Usual care | Four | |||
| Written personalised feedback report framed according to Motivational Enhancement Theory | Written information from the American Academy of Sleep Medicine | 12 | ||||
| Side effects management module incorporated in the automated telephone‐linked communication system | Information exchange on OSA and CPAP incorporated in the automated telephone‐linked communication system | Automated telephone‐linked communication system designed around the concept of Motivational Interviewing, which allowed one to assess and enhance CPAP compliance | General education on unrelated health topics via automated telephone‐linked communication system | 52 | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Machine usage (hours/night) Show forest plot | 13 | 803 | Mean Difference (IV, Random, 95% CI) | 0.82 [0.36, 1.27] |
| 2 Machine usage, sensitivity analysis: excluding participants aware of machine usage monitoring Show forest plot | 6 | 378 | Mean Difference (IV, Fixed, 95% CI) | 1.07 [0.61, 1.52] |
| 3 Machine usage, sensitivity analysis: adherence in control group < four hours/night Show forest plot | 8 | 471 | Mean Difference (IV, Fixed, 95% CI) | 1.36 [0.96, 1.76] |
| 4 N deemed adherent (≥ four hours/night) Show forest plot | 4 | 268 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.06 [1.22, 3.47] |
| 5 Epworth Sleepiness Scale scores Show forest plot | 8 | 501 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.81, 0.62] |
| 6 Quality of life: Functional Outcomes of Sleep Questionnaire Show forest plot | 2 | 70 | Mean Difference (IV, Fixed, 95% CI) | 0.98 [‐0.84, 2.79] |
| 7 Quality of life: Sleep Apnoea Quality of Life Index (SAQLI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Mood Show forest plot | 3 | 312 | Mean Difference (IV, Fixed, 95% CI) | ‐0.94 [‐1.55, ‐0.33] |
| 8.1 HAD Scale for Anxiety | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐2.95, 0.75] |
| 8.2 HAD Scale for Depression | 3 | 232 | Mean Difference (IV, Fixed, 95% CI) | ‐0.93 [‐1.57, ‐0.28] |
| 9 Withdrawals Show forest plot | 12 | 903 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.44, 0.97] |
| 10 AHI on treatment Show forest plot | 2 | 115 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐1.62, 1.48] |
| 11 Maintenance of Wakefulness Test (MWT) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Machine usage (hours/night) Show forest plot | 7 | 508 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.27, 0.93] |
| 2 N deemed adherent (≥ four hours/night) Show forest plot | 3 | 285 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.80 [1.09, 2.95] |
| 3 Epworth Sleepiness Scale scores Show forest plot | 5 | 336 | Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐2.07, ‐0.26] |
| 4 Quality of life: Sleep Apnoea Quality of Life Index (SAQLI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 HAD Scale for Depression Show forest plot | 2 | 152 | Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.22] |
| 6 Withdrawal Show forest plot | 8 | 683 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.45, 0.98] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Machine usage (hours/night) Show forest plot | 6 | 584 | Mean Difference (Random, 95% CI) | 1.44 [0.43, 2.45] |
| 2 Sensitivity analysis: excluding participants aware of machine usage monitoring Show forest plot | 5 | Mean Difference (Fixed, 95% CI) | 1.54 [0.99, 2.09] | |
| 3 N deemed adherent (≥ four hours/night) Show forest plot | 3 | 358 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.23 [1.45, 3.45] |
| 4 Epworth Sleepiness Scale score Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Quality of life: Functional Outcomes of Sleep Questionnaire Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Withdrawal Show forest plot | 5 | 609 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.57, 1.25] |