L'acide tranexamique dans l'hémorragie digestive haute
Résumé scientifique
Contexte
L'acide tranexamique réduit l'hémorragie grâce à ses effets antifibrinolytiques. Dans une version précédente de la présente revue, nous avons constaté que l'acide tranexamique pouvait réduire la mortalité. Cette revue inclut des recherches mises à jour et de nouveaux essais.
Objectifs
Évaluer les effets de l'acide tranexamique par rapport à l'absence d'intervention, un placebo ou d'autres médicaments anti‐ulcéreux dans l'hémorragie digestive haute.
Stratégie de recherche documentaire
Nous avons mis à jour la revue en effectuant des recherches dans des bases de données électroniques (registre Cochrane des essais contrôlés (CENTRAL), MEDLINE, EMBASE, Science Citation Index) ainsi que des recherches manuelles en juillet 2014.
Critères de sélection
Essais contrôlés randomisés, indépendamment de la langue ou du statut de publication.
Recueil et analyse des données
Nous avons utilisé les procédures méthodologiques standard de la Collaboration Cochrane. La mortalité toutes causes, l'hémorragie et les événements indésirables étaient les principales mesures de résultats. Nous avons effectué des méta‐analyses à l'aide des modèles à effets fixes et aléatoires et présenté les résultats sous forme de risques relatifs (RR) avec des intervalles de confiance (IC) à 95 %, et avons utilisé l'I² comme une mesure de l'hétérogénéité entre les essais. Nous avons analysé séparément l'acide tranexamique par rapport à un placebo ou l'absence d'intervention, et l'acide tranexamique par rapport à des médicaments anti‐ulcéreux. Pour analyser les sources d'hétérogénéité et la robustesse des résultats globaux, nous avons effectué des analyses en sous‐groupes, de sensibilité et séquentielles.
Résultats principaux
Nous avons inclus huit essais contrôlés randomisés sur l'acide tranexamique dans l'hémorragie digestive haute. En outre, nous avons identifié un grand essai contrôlé randomisé pragmatique en cours, dont les données ne sont pas encore disponibles. Les groupes témoins ont été assignés au hasard à un placebo (sept essais) ou à l'absence d'intervention (un essai). Deux essais incluaient aussi un groupe de contrôle assigné au hasard à des médicaments anti‐ulcéreux (lansoprazole ou cimétidine). Les études incluses ont été publiés entre 1973 et 2011. Le nombre de participants assignés au hasard variait de 47 à 216 (médiane 204). Tous les essais rendaient compte de la mortalité. Au total, 42 des 851 participants assignés au hasard à l'acide tranexamique et 71 des 850 participants dans le groupe témoin sont décédés (RR 0,60, IC à 95 % de 0,42 à 0,87 ; P = 0,007 ; I² = 0 %). L'analyse n'a pas été confirmée lorsque tous les participants dans le groupe d'intervention avec des données de résultats manquants ont été inclus à titre d'échecs de traitement, ou quand l'analyse a été limitée aux essais avec un faible risque de biais d'attrition. Une récidive hémorragique a été diagnostiquée chez 117 des 826 participants dans le groupe sous acide tranexamique et chez 146 des 825 participants dans le groupe de contrôle (RR 0,80, IC à 95 % de 0,64 à 1,00 ; P = 0,07 ; I² = 49 %). Nous n'avons pu évaluer le risque d'événements indésirables graves que sur la base de quatre essais. Nos analyses n'ont montré « aucune preuve d'une différence entre l'acide tranexamique et les interventions de contrôle concernant le risque d'événements thromboemboliques ». Dans la méta‐analyse à effets fixes, l'acide tranexamique semblait réduire le risque de chirurgie (RR 0,73, IC à 95 % de 0,56 à 0,95), mais ce résultat n'était plus statistiquement significatif dans la méta‐analyse à effets aléatoires (RR 0,61, IC à 95 % de 0,35 à 1,04 ; P = 0,07). Aucune différence n'a été observée entre l'acide tranexamique et le placebo dans l'évaluation de la transfusion (RR 1,02, IC à 95 % de 0,94 à 1,11 ; I² = 0 %), et les méta‐analyses comparant l'acide tranexamique aux médicaments anti‐ulcéreux n'ont pas permis d'identifier des effets bénéfiques ou néfastes de l'acide tranexamique pour aucun des critères évalués.
Conclusions des auteurs
Cette revue a constaté que l'acide tranexamique semblait avoir un effet bénéfique sur la mortalité, mais en raison d'un taux élevé d'abandon dans certains essais, nous ne pouvons pas en être certains jusqu'à ce que les résultats de recherches supplémentaires soient publiés. Au moment de cette mise à jour en 2014, une grande étude (8 000 participants) est en cours, de sorte que cette revue sera beaucoup plus instructive dans quelques années. Un examen plus approfondi de l'acide tranexamique nécessiterait l'inclusion d'essais contrôlés randomisés de haute qualité. Le moment de randomisation est essentiel pour éviter le biais d'attrition et limiter le nombre d'abandons. Les futurs essais peuvent utiliser une conception pragmatique et devraient inclure tous les participants chez qui une hémorragie est soupçonnée ou vérifiée par endoscopie, ainsi qu'un bras de placebo tranexamique et une co‐administration d'inhibiteurs de la pompe et d'un traitement endoscopique. L'évaluation des mesures de résultats dans ces études devrait être clairement définie. Un examen endoscopique avec un contrôle approprié des hémorragies graves doit être effectué, ainsi qu'une vérification endoscopique de récidives hémorragiques cliniquement significatives. En outre, des mesures cliniques de la récidive hémorragique doivent être incluses. D'autres mesures de résultats importants comprennent la mortalité (sur 30 jours ou à l'hôpital), le recours à la chirurgie d'urgence ou à une transfusion sanguine et les événements indésirables (majeurs ou mineurs).
PICOs
Résumé simplifié
L'acide tranexamique (un agent favorisant la coagulation du sang) dans les saignements graves ou incontrôlés des voies digestives supérieures
Contexte
Le saignement gastro‐intestinal supérieur est un motif fréquent d'admission aux urgences. Le pronostic est grave. Certains patients peuvent mourir suite à un saignement incontrôlé.
Problématique de la revue
L'acide tranexamique est un antifibrinolytique. Ce médicament réduit la dégradation de la fibrine, qui constitue la charpente pour la formation d'un caillot de sang, nécessaire pour arrêter le saignement. Les essais cliniques suggèrent que l'acide tranexamique pourrait réduire la mortalité des saignements gastro‐intestinaux supérieurs.
Caractéristiques des études
Cette revue inclut des données issues de huit essais randomisés sur l'acide tranexamique. Deux essais ont également évalué des médicaments anti‐ulcéreux. Un seul essai avait utilisé un traitement endoscopique supplémentaire, étant donné que les autres essais avaient été réalisés avant que cette intervention ne soit introduite dans la pratique clinique.
Principaux résultats
Ces essais ont constaté que l'acide tranexamique semblait avoir un effet bénéfique sur la mortalité, mais en raison d'un taux élevé d'abandon dans certains essais, nous ne pouvons pas être certains de ces résultats jusqu'à ce que des recherches supplémentaires soient publiées. L'acide tranexamique n'a pas réduit la mortalité dans les essais qui incluaient des médicaments anti‐ulcéreux ou un traitement endoscopique. D'autres essais contrôlés randomisés sont nécessaires avant que nous puissions déterminer si l'acide tranexamique a un effet bénéfique sur le saignement gastro‐intestinal supérieur grave ou incontrôlé.
Qualité des preuves
Beaucoup de patients assignés au hasard ont ensuite été exclus de l'évaluation. La principale source de biais est donc l'attrition. La qualité globale des preuves était modérée à faible.
Authors' conclusions
Summary of findings
| Tranexamic acid vs placebo for upper gastrointestinal bleeding | ||||||
| Patient or population: patients with upper gastrointestinal bleeding | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Tranexamic acid vs placebo | |||||
| Mortality | Study population | RR 0.6 | 1701 | ⊕⊕⊕⊝ | ||
| 84 per 1000 | 50 per 1000 | |||||
| Moderate | ||||||
| 83 per 1000 | 50 per 1000 | |||||
| Rebleeding | Study population | RR 0.72 | 1651 | ⊕⊕⊝⊝ | ||
| 177 per 1000 | 142 per 1000 | |||||
| Moderate | ||||||
| 196 per 1000 | 157 per 1000 | |||||
| Any thromboembolic event | Study population | RR 1.86 | 1095 | ⊕⊕⊕⊝ | ||
| 11 per 1000 | 20 per 1000 | |||||
| Moderate | ||||||
| 10 per 1000 | 19 per 1000 | |||||
| Surgery | Study population | RR 0.61 | 1551 | ⊕⊕⊕⊝ | ||
| 142 per 1000 | 103 per 1000 | |||||
| Moderate | ||||||
| 154 per 1000 | 112 per 1000 | |||||
| Transfusion | Study population | RR 1.02 | 931 | ⊕⊝⊝⊝ | ||
| 564 per 1000 | 558 per 1000 | |||||
| Moderate | ||||||
| 583 per 1000 | 577 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aMost trials had high risk of attrition bias. | ||||||
| Tranexamic acid vs cimetidine or lansoprazole for upper gastrointestinal bleeding | ||||||
| Patient or population: patients with upper gastrointestinal bleeding | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Tranexamic acid vs cimetidine or lansoprazole | |||||
| Mortality | Study population | RR 0.91 | 720 | ⊕⊕⊕⊝ | ||
| 61 per 1000 | 56 per 1000 | |||||
| Moderate | ||||||
| 48 per 1000 | 44 per 1000 | |||||
| Rebleeding | Study population | RR 0.87 | 720 | ⊕⊕⊕⊝ | ||
| 188 per 1000 | 166 per 1000 | |||||
| Moderate | ||||||
| 161 per 1000 | 142 per 1000 | |||||
| Surgery | Study population | RR 0.83 | 720 | ⊕⊕⊕⊝ | ||
| 139 per 1000 | 115 per 1000 | |||||
| Moderate | ||||||
| 105 per 1000 | 87 per 1000 | |||||
| Transfusion | Study population | RR 0.97 | 720 | ⊕⊕⊝⊝ | ||
| 573 per 1000 | 579 per 1000 | |||||
| Moderate | ||||||
| 599 per 1000 | 605 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aHigh risk of bias based on assessment of attrition. | ||||||
Background
Description of the condition
Upper gastrointestinal bleeding is a common reason for emergency hospital admission and a common complication in hospitalised patients (Rockall 1995; Blatchford 1997). A systematic review of general, population‐based epidemiological studies found that the incidence of upper gastrointestinal bleeding among patients treated with non‐steroidal anti‐inflammatory drugs was 0.8 per 1000 (Hernandez 2002). The risk of upper gastrointestinal bleeding has been found to increase significantly with age, co‐morbidity and use of non‐steroidal anti‐inflammatory drugs (Yavorski 1995; Paspatis 2000; Ng 2006). About 80% of patients with upper gastrointestinal bleeding will spontaneously stop bleeding, without recurrence (Laine 1994). The highest mortality and morbidity rates are seen in the remaining 20%, who experience recurrent or continued bleeding. Among patients referred to endoscopy for suspected upper gastrointestinal bleeding, 30‐day mortality is 10% to 14% (van Leerdam 2003; Barkun 2004; Barkun 2010).
Description of the intervention
Several endoscopic therapies have been found to be effective in clinical trials (Kahi 2005). However, some hospital departments may not have access to acute endoscopy. In other cases, patients may refuse to undergo endoscopy. Identification of drugs that may achieve haemostasis, stabilising patients until endoscopy can be performed, is therefore essential.
How the intervention might work
Tranexamic acid reduces fibrinolysis by slowing down the conversion of plasminogen to plasmin. The resulting reduction in fibrinolysis prevents the breakdown of blood clots, which may result in haemostasis but increased risk of thromboembolic complications. This drug was introduced for menorrhagia in 1968 (Vermylen 1968) and is used to reduce blood loss during surgery (Laupacis 1997; Cid 2005). A large multi‐centre trial found that tranexamic acid reduces mortality in individuals with bleeding trauma by 9% and results in no apparent increase in thromboembolic events (CRASH‐2). It is possible that a similar effect can be achieved in cases of upper gastrointestinal bleeding.
Why it is important to do this review
Endoscopic therapy and proton pump inhibitors serve as the cornerstone in the treatment of bleeding from peptic ulcers (Lau 2013). These treatments are highlighted in recent evidence‐based guidelines (Dworzynski 2012), which do not recommend tranexamic acid for the management of upper gastrointestinal bleeding. Randomised trials have assessed the effects of tranexamic acid among patients with suspected or verified upper gastrointestinal bleeding (Cormack 1973; Biggs 1976; Engquist 1979; Bergqvist 1980; Barer 1983; Holstein 1987; Hawkey 2001). A meta‐analysis of these trials revealed that tranexamic acid reduces the risks of rebleeding and mortality (Henry 1989). However, results of individual trials varied considerably. Furthermore, the overall result has been characterised as disproportionately skewed by inclusion of a trial in which mortality in the control group was surprisingly high (Barer 1983; Palmer 2002). We have previously published a systematic review on tranexamic acid versus placebo (Gluud 2008). A randomised trial on tranexamic acid for upper gastrointestinal bleeding was published after our previous meta‐analysis had been completed (Bagnenko 2011). This trial was included in a recent review, which determined that we still have insufficient evidence for definitive conclusions (Manno 2014). We performed this updated systematic review on tranexamic acid versus placebo, cimetidine or lansoprazole for upper gastrointestinal bleeding.
Objectives
To assess the effects of tranexamic acid versus no intervention, placebo or other antiulcer drugs for upper gastrointestinal bleeding.
Methods
Criteria for considering studies for this review
Types of studies
Randomised trials, irrespective of language, blinding, length of follow‐up or publication status.
Types of participants
Individuals with suspected or endoscopically verified upper gastrointestinal bleeding, irrespective of the bleeding source.
Types of interventions
Primary analyses included trials on tranexamic acid versus placebo or no intervention. Secondary analyses compared tranexamic acid versus any other antiulcer drug.
Types of outcome measures
Primary outcomes
-
Mortality.
-
Adverse events. We defined serious adverse events as all adverse events considered serious by study participants or investigators.
Secondary outcomes
-
Rebleeding.
-
Surgery.
Search methods for identification of studies
Electronic searches
Electronic searches of the following were performed July 2014.
-
Cochrane Central Register of Controlled Trials (CENTRAL) (Appendix 1).
-
MEDLINE via Ovid SP (Appendix 2).
-
EMBASE via Ovid SP (Appendix 3).
-
Science Citation Index Expanded (Appendix 4).
Searching other resources
We scanned conference proceedings and reference lists from relevant trials, wrote to authors of included trials and searched the International Clinical Trials Registry Platform (ICTRP) to identify trials on tranexamic acid (Appendix 5).
Data collection and analysis
Selection of studies
Three review authors (LLG, SLK and CB) screened search results for potentially eligible trials and identified trials that were eligible for inclusion. Excluded trials were listed together with the reasons for exclusion. At each stage of the selection process, at least two review authors independently reviewed search results and selected trials for inclusion. Three review authors (LLG, SLK and CB) agreed on the final list.
Data extraction and management
Two review authors (LLG and SLK) independently extracted data using data collection forms designed to capture information specific to this review. CB verified the extracted data at this update. Disagreements were resolved through discussion before analyses were performed. Data on baseline participant characteristics (inclusion criteria, mean age, proportion of men and source of bleeding), dose and duration of treatment, country of origin, publication status, funding, duration of follow‐up and risk of bias were gathered from the included trials and from correspondence with study authors. For trials published in Russian, two review authors (LLG and CB) extracted data obtained by machine translation (Google translate). Dimitrinka Nikolova from the Cochrane Hepato‐Biliary Group read the original Russian language publication and verified the extracted data.
Assessment of risk of bias in included studies
At least two review authors (LLG and SLK or CB) independently assessed risk of bias in the included studies by using the risk of bias assessment tool provided in Chapter 8 of theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We compared these evaluations and discussed and resolved inconsistencies.
We rated the following domains separately for each of the included studies as 'low risk of bias,' 'high risk of bias' or 'unclear risk of bias' if the risk of bias was uncertain or unknown. These assessments are reported in the 'Risk of bias' table for each individual study included in the Characteristics of included studies section of the review.
-
Allocation sequence was adequately generated ('sequence generation').
-
Allocation was adequately concealed ('allocation concealment').
-
Knowledge of allocated interventions was adequately prevented during the study ('blinding') (whether the trial was described as double‐blind or single‐blind, and whether blinding involved healthcare providers, outcome assessors or those performing data extraction or data analysis).
-
Incomplete outcome data were adequately addressed.
-
Reports of the study were free of suggestions of selective outcome reporting (whether clinically relevant outcome measures were defined and reported).
-
The study was apparently free of other sources of bias that could put it at high risk of bias (e.g. potential conflicts of interest, pharmaceutical funding/support, or both).
-
Other biases (sample size calculations and registration in clinical trial databases).
We categorised and reported the overall risk of bias of each of the included studies according to the following.
-
Low risk of bias (plausible bias unlikely to seriously alter the results) if all criteria were met.
-
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more criteria were assessed as unclear.
-
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more criteria were not met.
We reported these assessments in the Risk of bias in included studies section of this review.
Measures of treatment effect
The effect measure consisted of risk ratios (RRs) with 95% confidence intervals (CIs).
Unit of analysis issues
As the primary outcome measure was mortality, only trials using a parallel‐group design were included. Data on all intervention groups were analysed separately for all trials, including those with more than two parallel arms. Risk of selection bias was noted in the allocation of participants to intervention or control groups and in the administration of collateral interventions; therefore we did not include cluster‐randomised trials.
Multi‐armed trials
For trials with multiple intervention groups, we partitioned participants into individual allocation arms to perform pair‐wise comparisons. For example, a three‐arm trial with 30 participants (10 in each arm) allocated to tranexamic acid versus placebo versus antiulcer drugs would allow two pair‐wise comparisons of tranexamic acid versus placebo (10 vs 10 participants) and tranexamic acid versus antiulcer drugs (10 vs 10 participants).
Dealing with missing data
We contacted study investigators to request data on all randomly assigned participants to perform intention‐to‐treat analyses. We used simple imputation to evaluate the potential influence of missing data: imputing failures, imputing successes and worst‐ and best‐case scenarios (Higgins 2008).
Assessment of heterogeneity
We assessed clinical heterogeneity by examining trial conditions on the basis of characteristics of included trials, participants and interventions. We assessed statistical heterogeneity by using I2 statistical values and reported heterogeneity as important when the I² statistic was > 60% (Higgins 2011).
Assessment of reporting biases
We attempted to obtain trial protocols to compare reported outcome measures in the protocol versus those in the published trial. For analyses with at least 10 trials, we planned to assess reporting biases and other dissemination biases by using funnel plots (Higgins 2011) and to perform regression analyses by using Harbord's modified test (Harbord 2006). Our analyses included only eight trials; therefore we did not carry out a statistical analysis of reporting bias.
Data synthesis
We performed analyses in RevMan 2014 (The Nordic Cochrane Centre, Copenhagen, Denmark), STATA version 13 (Stata Corp., Texas, USA) and Trial Sequential Analysis (The Cochrane Hepato‐Biliary Group, Copenhagen, Denmark). We performed all meta‐analyses using both random‐effects and fixed‐effect models. Fixed‐effect model meta‐analyses are reported only when the results of the two models differ (e.g. one model shows no difference between interventions and the other shows an intervention effect).
We report the results of analyses with the total number of participants. When it was possible to calculate an effect size, we report this with 95% confidence intervals. When the calculated effect size was statistically significant (defined as P value < 0.05), we state whether the result favoured the intervention or control condition.
Subgroup analysis and investigation of heterogeneity
We performed separate analyses of trials on tranexamic acid versus placebo or no intervention and trials on tranexamic acid versus antiulcer drugs, as well as subgroup analyses of trials with low risk of bias based on assessment of the separate domains. We also analysed subgroups of trials that used endoscopic therapy and trials published in English or Russian.
Sensitivity analysis
We performed two further analyses to determine the effects of missing outcome data and a per‐protocol analysis to evaluate the influence of missing data. In the first scenario, all participants in the intervention arm with missing outcome data were included as treatment failures and participants in the control group with missing outcome data were considered as treatment successes. In the per‐protocol analyses, we excluded participants with missing outcome data. We performed a post hoc analysis that excluded a trial with a very high event rate in the control group (Barer 1983).
Trial sequential analysis
We performed a post hoc trial sequential analysis to determine the risk of bias associated with cumulative testing and to evaluate futility in the assessment of mortality and bleeding (Higgins 2008; Wetterslev 2008). We performed the analysis with power set to 80%, alpha to 5% and model‐based diversity and with relative risk reduction (RRR) to 30%. We set the control incidence to 10% for the analysis of mortality and to 30% for the analysis of bleeding.
'Summary of findings' tables
We prepared a 'Summary of findings' table (Guyatt 2008) using GRADEpro software (Gradepro 3.6) and we included information on the results of our primary outcomes in relation to risk of heterogeneity, duration of follow‐up and quality of the evidence.
Results
Description of studies
Results of the search
The original electronic searches identified 84 hits, and the updated search 37 hits (Appendix 6). The manual search identified one additional record. After reading the titles and abstracts, we retrieved 15 records for further assessment. One record referred to an ongoing trial (ISRCTN11225767) on tranexamic acid for gastrointestinal bleeding (Characteristics of ongoing studies). We will include this trial in future updates if the results become available (Figure 1). We excluded four records that did not assess tranexamic acid for upper gastrointestinal bleeding. In total, we included eight randomised controlled trials in our analyses (Cormack 1973; Biggs 1976; Engquist 1979; Bergqvist 1980; Barer 1983; Holstein 1987; Hawkey 2001; Bagnenko 2011). We received additional information about study design and outcomes from the primary investigators of one of the included trials (Hawkey 2001). For the remaining trials, we had access only to published data. The included trials were published as full paper articles, from 1973 to 2011. One trial was published in Russian (Bagnenko 2011), and the remaining in English.
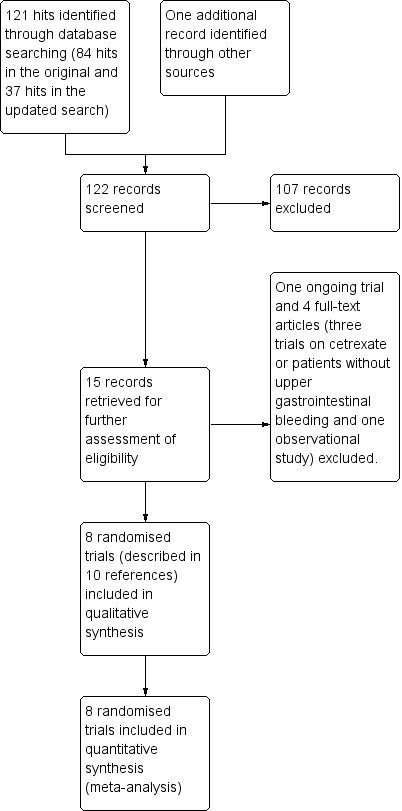
Study flow diagram.
Included studies
Design
All trials were randomised, parallel arm. One trial was open (Bagnenko 2011), and the remaining trials were double blind with a placebo control.
Sample sizes
The numbers of participants randomly assigned ranged from 47 to 216 (median 204).
Setting
All trials were performed at hospitals.
Participants
The trials included participants admitted with suspected upper gastrointestinal bleeding confirmed by endoscopy or clinically through gastric lavage, hematemesis or melena. Participants with previous or ongoing thromboembolic disease or renal disease and pregnant women were excluded from the trials. Three trials included only participants with severe bleeding (Engquist 1979; Bergqvist 1980; Bagnenko 2011). In the remaining trials, proportions of participants with circulatory involvement ranged from 1% to 21%. Mean participant age ranged from 56 to 62 years in the tranexamic acid groups and from 56 to 65 years in the control groups. Five trials reported that a proportion of participants had oesophageal varices (mean proportion 8%, range 5% to 16%). In four trials (Barer 1983; Holstein 1987; Hawkey 2001; Bagnenko 2011), participants underwent endoscopy within 24 hours after admission. One trial reported that 12% of included participants did not undergo the planned endoscopy. Two trials evaluated participants with endoscopy but did not specify the time frame (Engquist 1979; Bergqvist 1980). The remaining two trials did not include an endoscopic evaluation (Cormack 1973) or had access to endoscopy only during a portion of the trial (Biggs 1976).
Interventions
Tranexamic acid was administered intravenously in one trial (Barer 1983) and orally in three trials (Cormack 1973; Bergqvist 1980; Hawkey 2001). The remaining trials used intravenous followed by oral administration. The total daily dose of tranexamic acid ranged from 4 to 8 g. Duration of therapy ranged from two to seven days.
Comparisons
One trial included a no intervention control group (Bagnenko 2011), and the remaining trials included a placebo control. Two trials were multi‐armed and included control groups randomly assigned to the histamine receptor (H2) agonist cimetidine (Barer 1983) or the proton pump inhibitor lansoprazole alone or with tranexamic acid (Hawkey 2001). One trial allowed co‐intervention with the histamine receptor agonist famotidine (Bagnenko 2011). In five trials, a variety of co‐interventions, including novaluzide and cimetidine or ranitidine, were administered to participants in both treatment arms (Cormack 1973; Biggs 1976; Engquist 1979; Bergqvist 1980; Holstein 1987). Two trials used endoscopic therapy to control bleeding (Hawkey 2001; Bagnenko 2011).
Outcomes
One trial reported endoscopically verified rebleeding (Bagnenko 2011). Another trial reported rebleeding as assessed by hematemesis, melena or hypotension plus a drop in haemoglobin or rebleeding seen at endoscopy (Hawkey 2001). Two trials defined rebleeding on the basis of a drop in haemoglobin (Holstein 1987) or a drop in haemoglobin, hematemesis or melena (Barer 1983). The remaining trials did not define rebleeding.
Excluded studies
We excluded four trials that were published as full paper articles (Hollanders 1982; Tam 1989; Adachi 2001; Sabovic 2003). These trials were excluded because they were observational, assessed certrexate or did not include participants with upper gastrointestinal bleeding (Excluded studies).
Risk of bias in included studies
Allocation
One trial (Bagnenko 2011) reported an adequate method for allocation sequence generation (Figure 2). The remaining trials did not describe how the allocation sequence was generated. One trial did not describe how allocation was concealed (Bagnenko 2011). In the remaining trials, allocation was adequately concealed through double‐blind administration of the intervention or placebo.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Blinding
One trial was open (Bagnenko 2011). The remaining trials were double blind with a placebo control.
Incomplete outcome data
Attrition was one of the main sources of bias. Five trials reported losses to follow‐up (Engquist 1979; Bergqvist 1980; Barer 1983; Holstein 1987; Hawkey 2001). Three trials gave the impression that no dropouts or withdrawals had occurred, although this was not specifically reported (Cormack 1973; Biggs 1976; Bagnenko 2011). One in five participants (20%) were withdrawn or excluded after randomisation. Reasons for exclusion included lack of verified bleeding, malignant disease and terminal illness, or the treatment was administered too late.
Selective reporting
One trial did not report bleeding and was classed as having high risk of reporting bias (Bergqvist 1980).
Other potential sources of bias
None of the trials had other potential sources of bias.
Effects of interventions
See: Summary of findings for the main comparison Tranexamic acid vs placebo for upper gastrointestinal bleeding; Summary of findings 2 Tranexamic acid vs cimetidine or lansoprazole for upper gastrointestinal bleeding
Comparison 1. Tranexamic acid versus placebo
Primary outcomes
Mortality
All trials reported mortality (Analysis 1.1). Forty‐two of 851 participants randomly assigned to tranexamic acid and 71 of 850 in the control group died. The fixed‐effect meta‐analysis showed that tranexamic acid reduced mortality (RR 0.60, 95% CI 0.42 to 0.87; P value 0.007). No statistical heterogeneity was noted between trials (I² = 0%).
Sensitivity analyses and trial sequential analysis
The analysis was not confirmed in a scenario analysis in which all participants with missing outcome data were included as treatment failures (Analysis 1.2), but it was confirmed in a per‐protocol analysis (data not shown).
Analyses of studies with low risk of bias confirmed that attrition was the main source of bias (Analysis 1.3). The single remaining trial with low risk of attrition bias (Hawkey 2001) found no effects of the intervention. A similar result was seen when trials that used endoscopic therapy to control bleeding were analysed (Analysis 1.4). No difference (test for subgroup differences P value 0.67) was noted between trials published in English and those translated from Russian (Analysis 1.5).
One of the trials has been criticised for reporting a high control group event rate (Barer 1983; Palmer 2002). This trial included 516 participants and reported a large weight in the analysis (49%). In a post hoc analysis that excluded this trial, tranexamic acid was seen to have no effect on mortality (RR 0.73, 95% CI 0.45 to 1.19; analysis not shown). In our post hoc trial sequential analysis (Figure 3), the required information size was not met, suggesting that the meta‐analysis is inconclusive.

Trial sequential analysis of eight trials on tranexamic acid versus placebo or no intervention. Outcome measure is mortality. Analysis was performed with alpha 5% and power 80%. Model‐based heterogeneity correction was 0%, relative risk reduction 30% and control group incidence 10%. Graph shows the Z‐curve, which is the cumulative result of analysis with trials added according to year of publication. Horizontal line represents 'traditional' 5% level of significance, and inward sloping red line shows trial sequential monitoring boundary. Vertical line represents required information size. Analysis shows that the Z‐curve crosses the trial sequential monitoring boundary, suggesting that the result of the meta‐analysis is confirmed when analysis is adjusted for cumulative testing. Total number of included participants (N = 1701) is only 62% of required information size (N=2714). The meta‐analysis therefore remains inconclusive.
Bleeding
Seven trials reported rebleeding (Analysis 1.6). In total, rebleeding was diagnosed for 117 of 826 participants in the tranexamic acid group and for 146 of 825 participants in the control group.
Sensitivity analyses and trial sequential analysis
The difference was not statistically significant (RR 0.72, 95% CI 0.50 to 1.03; P value 0.07). A similar conclusion was reached in worst‐case scenario analysis (Analysis 1.7) and per‐protocol analysis (data not shown). Analyses of trials with low risk of bias found no effects of tranexamic acid on bleeding (Analysis 1.8), and no differences were noted between trials stratified according to use of endoscopic therapy (Analysis 1.9) or language (Analysis 1.10). In the trial sequential analysis (Figure 4), 95% of the required information size was reached. This analysis suggested that the meta‐analysis was inconclusive.

Trial sequential analysis of seven trials on tranexamic acid versus placebo or no intervention. Outcome measure is bleeding. Analysis was performed with alpha 5% and power 80%. Model‐based heterogeneity correction was 53%, relative risk reduction 30% and control group incidence 10%. Graph shows the Z‐curve, which is the cumulative result of analysis with trials added according to year of publication. Horizontal line represents 'traditional' 5% level of significance, and inward sloping red line shows trial sequential monitoring boundary. Vertical line represents required information size. Analysis shows that the Z‐curve does not cross the trial sequential monitoring boundary, and the total number of participants (N = 1651) is 95% of required information size (N = 1734). The meta‐analysis therefore remains inconclusive.
Adverse events
Several participants randomly assigned to tranexamic acid experienced abdominal pain, nausea, vomiting and thrombophlebitis at the injection site (Table 1). We were unable to perform meta‐analyses on these adverse events because data were not provided for both treatment and control groups.
| Trial | Serious adverse events | Non‐serious adverse events | Non‐serious adverse events | ||
| Tranexamic acid | Control group | Intervention group not specified | Tranexamic acid | Control group | |
| Fatal stroke (n = 1) | Confusion | Pulmonary embolism (n = 5). Myocardial infarction (n = 8) | None described | Confusion (n = 1) | |
| None described | None described | None described | Thrombophlebitis at injection site (n = 3). Nausea or headache (n = 4) | Thrombophlebitis at injection site (n = 2). Nausea or headache (n = 5). Fever (n = 2) | |
| Pulmonary embolism (n = 2). Myocardial infarction (n = 2) | Cerebral infarction | None described | None described | None described | |
| None described | None described | Several participants experienced thromboembolic complications. The numbers were described as not significantly different in treatment and control groups, but no specific data are provided | None described | None described | |
| None described | Cerebral infarction | Five additional participants were excluded as the result of thromboembolic disease, but whether these participants were randomly assigned to tranexamic acid or placebo is not reported | Nausea and vomiting, tachycardia (n = 3). Hypotension (n = 3). Thrombophlebitis at injection site (n = 2). Deep venous thrombosis (n = 1) | None described | |
Three trials (Analysis 1.13) on 1048 participants reported thromboembolic events (Engquist 1979; Barer 1983; Holstein 1987). Among participants randomly assigned to tranexamic acid, two cases of myocardial infarction, two cases of pulmonary embolism and one case of cerebral infarction occurred. In the placebo group, two cases of myocardial infarction and two cases of cerebral infarction were recorded. When data on these serious thromboembolic events were combined, the difference was not statistically significant (RR 1.37, 95% CI 0.36 to 5.28; Analysis 1.11). Six cases of deep venous thrombosis occurred among participants randomly assigned to tranexamic acid compared with two cases in the placebo group (RR 2.32, 95% CI 0.60 to 8.89; Analysis 1.12). The numbers of participants with any thrombotic event were not significantly different between treatment and control groups (RR 1.86, 95% CI 0.66 to 5.24; Analysis 1.13).
Secondary outcomes
Surgery
Seven studies with 1551 participants reported the numbers of participants who required surgery (Analysis 1.14). Between‐trial heterogeneity was important (I² = 63%). Tranexamic acid appeared to reduce the risk of surgery in a fixed‐effect meta‐analysis (RR 0.73, 95% CI 0.56 to 0.95), but this result was no longer statistically significant at the 5% level, when a random‐effects meta‐analysis was used (RR 0.61, 95% CI 0.35 to 1.04; Analysis 1.14).
Transfusions
We planned to analyse the transfusion requirements of included participants, but we did not identify the necessary data. We therefore performed a post hoc analysis of the total numbers of participants who needed at least one blood transfusion (Analysis 1.15) and found no apparent differences between tranexamic acid and placebo (RR 1.02, 95% CI 0.94 to 1.11 in 931 participants; five studies; I² = 0%).
Comparison 2. Tranexamic acid versus antiulcer drugs (cimetidine or lansoprazole)
Primary outcomes
Mortality and rebleeding
Two trials compared tranexamic acid with cimetidine (Barer 1983) or lansoprazole (Hawkey 2001). These trials found no significant effects of tranexamic acid on mortality (RR 0.91, 95% CI 0.50 to 1.64; 720 participants; I² = 0%; Analysis 2.1) or bleeding (RR 0.87, 95% CI 0.64 to 1.20; I² = 0%; Analysis 2.2).
Adverse events
We were unable to perform meta‐analyses on adverse events (Table 1). Barer 1983 reported one case of fatal stroke in the tranexamic acid group and two cases of confusion in the control group. Hawkey 2001 reported no adverse events in the tranexamic acid or control groups.
Surgery and transfusions
Trials comparing tranexamic acid versus cimetidine or lansoprazole (Barer 1983; Hawkey 2001) found no differences between allocation groups regarding the need for surgery (RR 0.83, 95% CI 0.54 to 1.26; 720 participants; two studies; I² = 3%; Analysis 2.3) or blood transfusion (RR 0.97, 95% CI 0.78 to 1.22; 720 participants; two studies; I² = 64%; Analysis 2.4).
'Summary of findings' tables
As shown in the 'Summary of findings' tables on tranexamic acid versus placebo (summary of findings Table for the main comparison) or cimetidine or lansoprazole (summary of findings Table 2), the quality of the evidence was downgraded to moderate or low because of risk of bias.
Discussion
Summary of main results
This review includes eight randomised controlled trials and a total of 1701 participants with acute upper gastrointestinal bleeding. The meta‐analyses found that tranexamic acid appears to have a beneficial effect on mortality, but a high dropout rate in some trials means that we cannot be sure of this until additional research is published. Reduced mortality did not clearly reflect reduced bleeding or surgery. The result of the primary meta‐analysis was not stable in analyses that adjusted for risk of attrition bias or in trial sequential analyses. When trials with high risk of attrition bias were removed, only one trial was left (Hawkey 2001) in the analysis, so although we may need to be cautious about the potential effects of dropouts, the evidence is still fairly strong in favour of tranexamic acid. Likewise, only two of the included trials used endoscopic therapy (Hawkey 2001; Bagnenko 2011). These trials found no clear effects of tranexamic acid on bleeding was noted and that attrition bias may affect the assessment of mortality, therefore the combined evidence does not allow any recommendations to be made. Additional randomised controlled trials are needed to determine the effects of tranexamic acid. A large randomised double‐blind trial on tranexamic acid for gastrointestinal bleeding is ongoing (ISRCTN11225767). This trial has started to randomly assign the first participants. Results of this trial are expected to finally confirm or refute the effects of tranexamic acid for individuals with upper gastrointestinal bleeding.
Overall completeness and applicability of evidence
During recent years, standard care and assessment of outcomes have changed considerably (Dworzynski 2012). Previously, patients were not offered full diagnostic endoscopy or endoscopic interventions that are used as standard care today. It is noteworthy that the trial that is the most favourable towards tranexamic acid was published in 1983 (Barer 1983). The clinical question today is not whether tranexamic acid is better than placebo, but whether tranexamic acid is better than or may be used in combination with current treatments. One of the included trials found no significant difference between tranexamic acid and lansoprazole when used alone, or when the two treatments were combined (Hawkey 2001). This trial was not designed to assess clinical outcomes, and its statistical power may well have been too small to detect clinically relevant effects. On the other hand, this trial does suggest that additional research is necessary.
Several reasons may explain why we found that tranexamic acid reduces mortality but not bleeding. One possible explanation is that tranexamic acid may be effective in subgroups of patients with a serious prognosis. One of the included trials assessed the influence of the severity of bleeding on the intervention effect (Hawkey 2001). This trial included 414 participants with suspected upper gastrointestinal bleeding and asked admitting investigators to classify participant risk as high or low on the basis of their presentation. No specific criteria were used. Overall, high‐risk participants were more likely to die or need surgery. The effect of tranexamic acid was not related to risk stratification.
Quality of the evidence
In clinical guidelines on the management of upper gastrointestinal non‐variceal bleeding, tranexamic acid may be considered, but it is not recommended as routine therapy (Palmer 2002; Barkun 2003). This treatment generally is not recommended for variceal bleeding, and in several trials, participants with varices were excluded after randomisation. However, meta‐analyses in the present review include participants with upper gastrointestinal bleeding due to oesophageal varices. No significant association was found between treatment effect and the proportion of participants with varices. These analyses are only hypothesis generating but suggest that the effects of tranexamic acid on mortality may also be seen in this patient group. Likewise, we found no significant differences between trials in which participants received tranexamic acid in a daily dose of 12 g for two days and those in which the dose was 4 g for seven days. It may be interesting to determine whether dose or treatment duration is related to the risk of thromboembolic events, but we did not have sufficient data to analyse this question.
Vested interests were reported in some of the included trials. We were unable to identify specific design features that introduced bias due to vested interests and the fact that we included only eight trials limited the possibility of further analyses. Nevertheless, we cannot exclude that this factor can lead to bias. On the other hand, the trial that received full funding (Hawkey 2001) found no effect of tranexamic acid on any of the outcomes assessed.The largest trials received tranexamic acid and placebo from pharmaceutical companies (Barer 1983; Hawkey 2001). The trial with the most positive assessment of tranexamic acid received only medications (Barer 1983).
Mortality is an outcome measure that is relatively stable in relation to performance and ascertainment bias, but not to attrition bias. We found that attrition was the main source of bias. Included trials randomly assigned participants early, and many excluded participants after the source of bleeding had been identified by endoscopy. Exclusion of participants appeared to be done before blinding was broken, although this is not specifically stated. As the result of risk of bias and clinical heterogeneity between trials, which is inevitable given that trials were conducted over several decades, the overall quality of the evidence was deemed moderate or low (summary of findings Table for the main comparison; summary of findings Table 2).
Potential biases in the review process
Potential biases in the review process are limited. In particular, we attempted to avoid bias in identification and selection of trials, but one possible limitation is that despite exhaustive searching, it is possible that other trials have been conducted, and although we searched extensively, we did not identify unpublished trials or trials published in abstract form. We included only one paper that was published in Russian (Bagnenko 2011). Remaining trials were published in English. Because the number of identified trials was limited, we were not able to analyse the risk of publication bias. In theory, meta‐analyses are observational, which may lead to biases. A written protocol is necessary to determine biases in the review process and in general, the original protocol must be followed. However, we made methodological changes to our protocol that were based on recent evidence and guidelines (Guyatt 2008; Higgins 2008; Higgins 2011). These changes were mainly related to assessment of risk of bias. We also performed post hoc sequential analyses to improve assessment of biases.
Agreements and disagreements with other studies or reviews
Although our review methods did include assessment of all reported adverse events, we did not carry out a separate search for adverse effects; therefore one of the most important limitations of the present review is the fact that information about adverse events was limited. The recent debate on the use of antifibrinolytic drugs highlights the need for valid safety data. In 2006, an observational study of patients undergoing revascularisation was reported (Mangano 2006). This study included 1295 participants who received aprotinin and 822 who received tranexamic acid. Multi‐variable analyses found that aprotinin, but not tranexamic acid, significantly increased the risk of renal failure and cardiovascular or cerebral adverse events. Although results support the safety of tranexamic acid, the participant cohort was considerably different from that included in the present review. In particular, the trials included in the present review excluded participants with previous thromboembolic or renal disease. Therefore, it may be argued that one of the most important limitations of the present review is that limited information about adverse events was available. Although we found no significant association between tranexamic acid and risk of thromboembolic events, our analyses did not have sufficient statistical power to allow clear inferences. Theoretically, tranexamic acid increases the risk of thrombosis due to unopposed fibrin generation. Case reports have associated tranexamic acid with thromboembolic events, which may be fatal (Rydin 1976; Agnelli 1982; Endo 1988; Woo 1989; Taparia 2002). The trials in the present review excluded participants with previous thromboembolic events, although this is not generally accepted as a contraindication in clinical practice. Likewise these trials excluded participants with renal disease. One observational study has assessed the effects of tranexamic acid on patients undergoing dialysis. Tranexamic acid seems relatively safe to use in this patient group. However, the study included only 20 participants, so additional evidence is needed (Sabovic 2003).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Trial sequential analysis of eight trials on tranexamic acid versus placebo or no intervention. Outcome measure is mortality. Analysis was performed with alpha 5% and power 80%. Model‐based heterogeneity correction was 0%, relative risk reduction 30% and control group incidence 10%. Graph shows the Z‐curve, which is the cumulative result of analysis with trials added according to year of publication. Horizontal line represents 'traditional' 5% level of significance, and inward sloping red line shows trial sequential monitoring boundary. Vertical line represents required information size. Analysis shows that the Z‐curve crosses the trial sequential monitoring boundary, suggesting that the result of the meta‐analysis is confirmed when analysis is adjusted for cumulative testing. Total number of included participants (N = 1701) is only 62% of required information size (N=2714). The meta‐analysis therefore remains inconclusive.

Trial sequential analysis of seven trials on tranexamic acid versus placebo or no intervention. Outcome measure is bleeding. Analysis was performed with alpha 5% and power 80%. Model‐based heterogeneity correction was 53%, relative risk reduction 30% and control group incidence 10%. Graph shows the Z‐curve, which is the cumulative result of analysis with trials added according to year of publication. Horizontal line represents 'traditional' 5% level of significance, and inward sloping red line shows trial sequential monitoring boundary. Vertical line represents required information size. Analysis shows that the Z‐curve does not cross the trial sequential monitoring boundary, and the total number of participants (N = 1651) is 95% of required information size (N = 1734). The meta‐analysis therefore remains inconclusive.
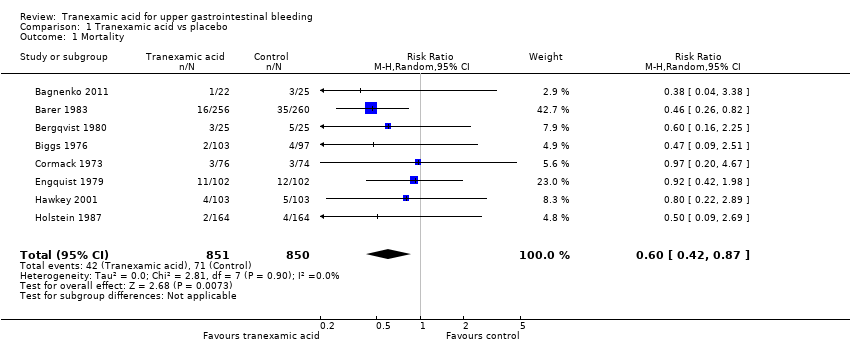
Comparison 1 Tranexamic acid vs placebo, Outcome 1 Mortality.
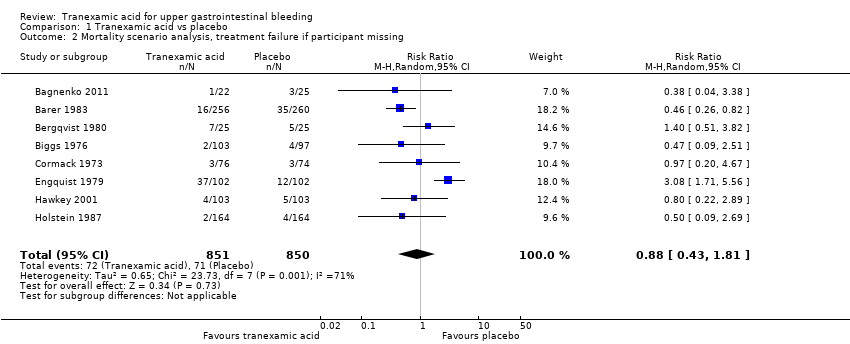
Comparison 1 Tranexamic acid vs placebo, Outcome 2 Mortality scenario analysis, treatment failure if participant missing.
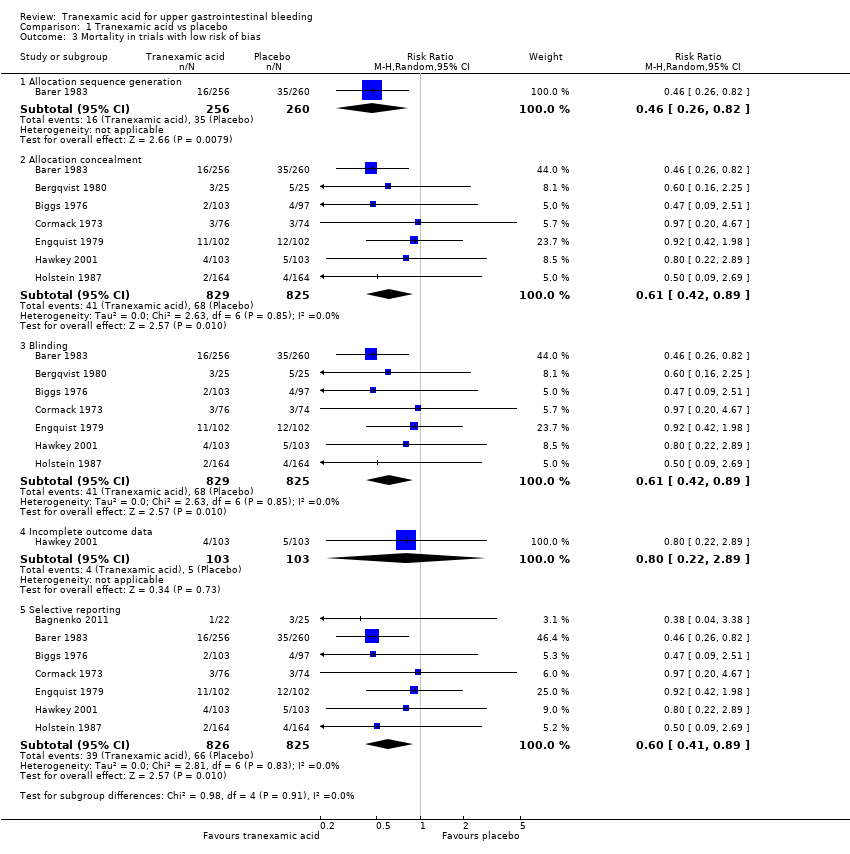
Comparison 1 Tranexamic acid vs placebo, Outcome 3 Mortality in trials with low risk of bias.

Comparison 1 Tranexamic acid vs placebo, Outcome 4 Mortality in relation to endoscopic therapy.

Comparison 1 Tranexamic acid vs placebo, Outcome 5 Mortality in relation to language of publication.

Comparison 1 Tranexamic acid vs placebo, Outcome 6 Rebleeding.

Comparison 1 Tranexamic acid vs placebo, Outcome 7 Rebleeding scenario analysis, treatment failure if participant missing.

Comparison 1 Tranexamic acid vs placebo, Outcome 8 Rebleeding in trials with low risk of bias.

Comparison 1 Tranexamic acid vs placebo, Outcome 9 Rebleeding in relation to endoscopic therapy.

Comparison 1 Tranexamic acid vs placebo, Outcome 10 Rebleeding in relation to language of publication.

Comparison 1 Tranexamic acid vs placebo, Outcome 11 Myocardial infarction, pulmonary embolism and cerebral infarction.
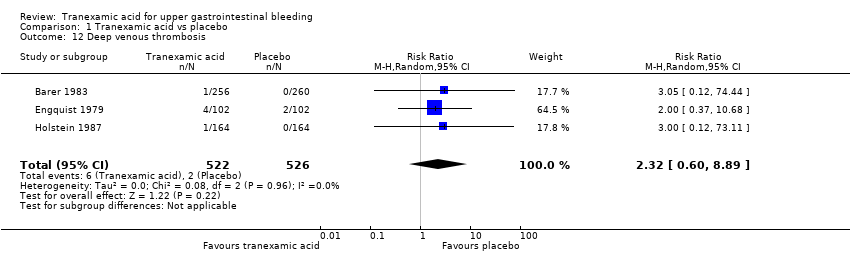
Comparison 1 Tranexamic acid vs placebo, Outcome 12 Deep venous thrombosis.

Comparison 1 Tranexamic acid vs placebo, Outcome 13 Any thromboembolic event.

Comparison 1 Tranexamic acid vs placebo, Outcome 14 Surgery.

Comparison 1 Tranexamic acid vs placebo, Outcome 15 Transfusion required.
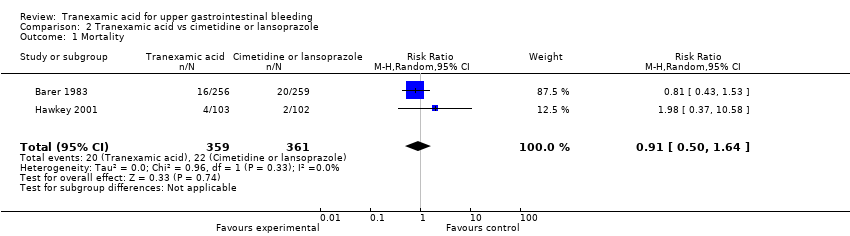
Comparison 2 Tranexamic acid vs cimetidine or lansoprazole, Outcome 1 Mortality.
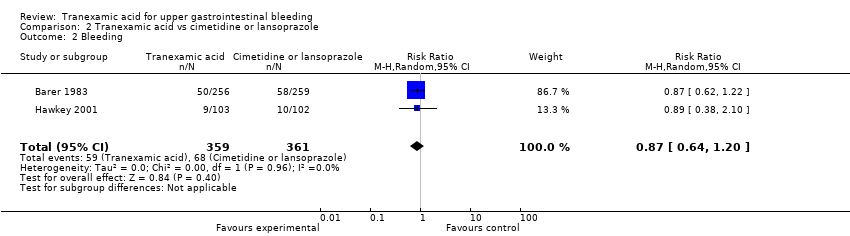
Comparison 2 Tranexamic acid vs cimetidine or lansoprazole, Outcome 2 Bleeding.

Comparison 2 Tranexamic acid vs cimetidine or lansoprazole, Outcome 3 Surgery.

Comparison 2 Tranexamic acid vs cimetidine or lansoprazole, Outcome 4 Transfusion.
| Tranexamic acid vs placebo for upper gastrointestinal bleeding | ||||||
| Patient or population: patients with upper gastrointestinal bleeding | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Tranexamic acid vs placebo | |||||
| Mortality | Study population | RR 0.6 | 1701 | ⊕⊕⊕⊝ | ||
| 84 per 1000 | 50 per 1000 | |||||
| Moderate | ||||||
| 83 per 1000 | 50 per 1000 | |||||
| Rebleeding | Study population | RR 0.72 | 1651 | ⊕⊕⊝⊝ | ||
| 177 per 1000 | 142 per 1000 | |||||
| Moderate | ||||||
| 196 per 1000 | 157 per 1000 | |||||
| Any thromboembolic event | Study population | RR 1.86 | 1095 | ⊕⊕⊕⊝ | ||
| 11 per 1000 | 20 per 1000 | |||||
| Moderate | ||||||
| 10 per 1000 | 19 per 1000 | |||||
| Surgery | Study population | RR 0.61 | 1551 | ⊕⊕⊕⊝ | ||
| 142 per 1000 | 103 per 1000 | |||||
| Moderate | ||||||
| 154 per 1000 | 112 per 1000 | |||||
| Transfusion | Study population | RR 1.02 | 931 | ⊕⊝⊝⊝ | ||
| 564 per 1000 | 558 per 1000 | |||||
| Moderate | ||||||
| 583 per 1000 | 577 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aMost trials had high risk of attrition bias. | ||||||
| Tranexamic acid vs cimetidine or lansoprazole for upper gastrointestinal bleeding | ||||||
| Patient or population: patients with upper gastrointestinal bleeding | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Tranexamic acid vs cimetidine or lansoprazole | |||||
| Mortality | Study population | RR 0.91 | 720 | ⊕⊕⊕⊝ | ||
| 61 per 1000 | 56 per 1000 | |||||
| Moderate | ||||||
| 48 per 1000 | 44 per 1000 | |||||
| Rebleeding | Study population | RR 0.87 | 720 | ⊕⊕⊕⊝ | ||
| 188 per 1000 | 166 per 1000 | |||||
| Moderate | ||||||
| 161 per 1000 | 142 per 1000 | |||||
| Surgery | Study population | RR 0.83 | 720 | ⊕⊕⊕⊝ | ||
| 139 per 1000 | 115 per 1000 | |||||
| Moderate | ||||||
| 105 per 1000 | 87 per 1000 | |||||
| Transfusion | Study population | RR 0.97 | 720 | ⊕⊕⊝⊝ | ||
| 573 per 1000 | 579 per 1000 | |||||
| Moderate | ||||||
| 599 per 1000 | 605 per 1000 | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aHigh risk of bias based on assessment of attrition. | ||||||
| Trial | Serious adverse events | Non‐serious adverse events | Non‐serious adverse events | ||
| Tranexamic acid | Control group | Intervention group not specified | Tranexamic acid | Control group | |
| Fatal stroke (n = 1) | Confusion | Pulmonary embolism (n = 5). Myocardial infarction (n = 8) | None described | Confusion (n = 1) | |
| None described | None described | None described | Thrombophlebitis at injection site (n = 3). Nausea or headache (n = 4) | Thrombophlebitis at injection site (n = 2). Nausea or headache (n = 5). Fever (n = 2) | |
| Pulmonary embolism (n = 2). Myocardial infarction (n = 2) | Cerebral infarction | None described | None described | None described | |
| None described | None described | Several participants experienced thromboembolic complications. The numbers were described as not significantly different in treatment and control groups, but no specific data are provided | None described | None described | |
| None described | Cerebral infarction | Five additional participants were excluded as the result of thromboembolic disease, but whether these participants were randomly assigned to tranexamic acid or placebo is not reported | Nausea and vomiting, tachycardia (n = 3). Hypotension (n = 3). Thrombophlebitis at injection site (n = 2). Deep venous thrombosis (n = 1) | None described | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 8 | 1701 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.42, 0.87] |
| 2 Mortality scenario analysis, treatment failure if participant missing Show forest plot | 8 | 1701 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.43, 1.81] |
| 3 Mortality in trials with low risk of bias Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Allocation sequence generation | 1 | 516 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.26, 0.82] |
| 3.2 Allocation concealment | 7 | 1654 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.42, 0.89] |
| 3.3 Blinding | 7 | 1654 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.42, 0.89] |
| 3.4 Incomplete outcome data | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 0.8 [0.22, 2.89] |
| 3.5 Selective reporting | 7 | 1651 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.41, 0.89] |
| 4 Mortality in relation to endoscopic therapy Show forest plot | 8 | 1701 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.42, 0.87] |
| 4.1 Endoscopic therapy not used | 6 | 1448 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.40, 0.88] |
| 4.2 Endoscopic therapy used to control bleeding | 2 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 2.00] |
| 5 Mortality in relation to language of publication Show forest plot | 8 | 1701 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.42, 0.87] |
| 5.1 Trials published in English | 7 | 1654 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.42, 0.89] |
| 5.2 Trials translated from Russian | 1 | 47 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.04, 3.38] |
| 6 Rebleeding Show forest plot | 7 | 1651 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.50, 1.03] |
| 7 Rebleeding scenario analysis, treatment failure if participant missing Show forest plot | 7 | 1651 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.51, 1.27] |
| 8 Rebleeding in trials with low risk of bias Show forest plot | 7 | 5581 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.65, 0.93] |
| 8.1 Allocation sequence generation | 1 | 516 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.83, 1.61] |
| 8.2 Allocation concealment | 6 | 1604 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.07] |
| 8.3 Blinding | 6 | 1604 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.07] |
| 8.4 Incomplete outcome data | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 0.9 [0.38, 2.12] |
| 8.5 Selective reporting | 7 | 1651 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.50, 1.03] |
| 9 Rebleeding in relation to endoscopic therapy Show forest plot | 7 | 1651 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.50, 1.03] |
| 9.1 Endoscopic therapy not used | 5 | 1398 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.45, 1.08] |
| 9.2 Endoscopic therapy used to control bleeding | 2 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.36, 1.62] |
| 10 Rebleeding in relation to language of publication Show forest plot | 7 | 1651 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.50, 1.03] |
| 10.1 Trials published in English | 6 | 1604 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.07] |
| 10.2 Trials translated from Russian | 1 | 47 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.10, 2.11] |
| 11 Myocardial infarction, pulmonary embolism and cerebral infarction Show forest plot | 3 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.36, 5.28] |
| 12 Deep venous thrombosis Show forest plot | 3 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 2.32 [0.60, 8.89] |
| 13 Any thromboembolic event Show forest plot | 4 | 1095 | Risk Ratio (M‐H, Random, 95% CI) | 1.86 [0.66, 5.24] |
| 14 Surgery Show forest plot | 7 | 1551 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.35, 1.04] |
| 15 Transfusion required Show forest plot | 5 | 931 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.94, 1.11] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.50, 1.64] |
| 2 Bleeding Show forest plot | 2 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.64, 1.20] |
| 3 Surgery Show forest plot | 2 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.54, 1.26] |
| 4 Transfusion Show forest plot | 2 | 720 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.78, 1.22] |

