Multi‐disciplinary rehabilitation for acquired brain injury in adults of working age
Information
- DOI:
- https://doi.org/10.1002/14651858.CD004170.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 22 December 2015see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Injuries Group
- Copyright:
-
- Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
LTS: planned the review protocol and methods, with input from DTW and PD; also co‐ordinated the search with support from the Cochrane Injuries Group and led selection and evaluation of trials.
AN, AP and LTS: independently handsearched article abstracts and agreed on the short list of trials for inclusion; when opinions differed, DTW arbitrated.
AN, LTS, AP and DTW: performed independent quality assessments and then agreed on final quality scores for articles included in the analysis.
PBD: in addition to his role the original conceptual design, has read and commented on drafts of this update and approved the final submission.
LTS: played the role of lead author; however, all review authors contributed to the final write‐up and discussion.
Sources of support
Internal sources
-
King's College London, UK.
-
London North West Hospitals Trust, UK.
External sources
-
Luff Foundation, UK.
-
Department of Health Research and Development Programme, UK.
-
Dunhill Medical Trust, UK.
Declarations of interest
All review authors are clinicians engaged in the field of brain injury rehabilitation who naturally wish to provide an effective and efficient service for their patients. No review authors have personal or financial interests in the findings of this review.
DW: As a part of my work I see people with spasticity to advise on management. My employer is paid for each patient I see. I also teach, but neither I nor my employer get paid for this. I give evidence, legally and in advising NHS bodies etc about rehabilitation and the need for multidisciplinary teams, and I write about such teams but rarely get paid for this.
LTS: None known.
AP: None known.
AN: None known.
PBD: None known.
Acknowledgements
This study was funded by grants from the Department of Health Research and Development Programme and from the Luff Foundation. The review authors would like to acknowledge Fiona Renton, Karen Blackhall and Deirdre Beecher of the Cochrane Injuries Group for help with literature searching; Emma Sydenham for assistance with the risk of bias tables and general editing; Kanchana Jeganathan and staff from the John Squire Library, Northwick Park Hospital, for assistance in gathering the references; and Dr Beatrice Zhang for kind assistance with interpretation of various papers published in the Chinese literature.
Imad Sedki contributed to the 2009 and 2010 versions of the review.
This project was supported by the UK National Institute for Health Research, through Cochrane Infrastructure funding to the Cochrane Injuries Group. The views and opinions expressed are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Dec 22 | Multi‐disciplinary rehabilitation for acquired brain injury in adults of working age | Review | Lynne Turner‐Stokes, Anton Pick, Ajoy Nair, Peter B Disler, Derick T Wade | |
| 2005 Jul 20 | Multi‐disciplinary rehabilitation for acquired brain injury in adults of working age | Review | Lynne Turner‐Stokes, Ajoy Nair, Imad Sedki, Peter B Disler, Derick T Wade | |
| 2003 Apr 22 | Multi‐disciplinary rehabilitation for acquired brain injury in adults of working age | Protocol | Lynne Turner‐Stokes, Peter B Disler, Ajoy Nair, Derick T Wade | |
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adolescent; Adult; Aged; Humans; Middle Aged;
PICOs

Study flow diagram. The numbers for identification, screening and eligibility are from updated searches in 2013, 2014 and 2015.
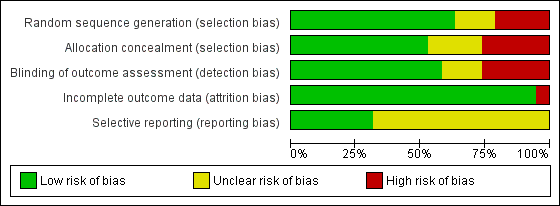
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Nineteen studies are included in this review.
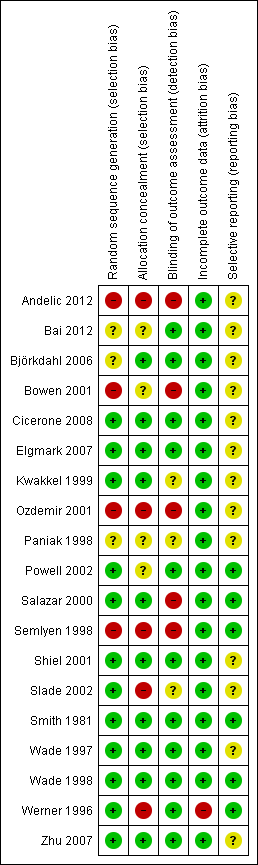
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Criterion | Score positive if: |
| Eligibility criteria specified | A list of inclusion/exclusion criteria was explicitly stated. |
| Method of randomisation | A random (unpredictable) assignment sequence was used. |
| Treatment allocation concealment | Assignment was concealed from investigators. Assignment was generated by an independent person not responsible for determining the eligibility of patients. This person has no information about individuals included in the trial and has no influence on the assignment sequence nor on the decision about eligibility of patients. |
| Similarity of baseline characteristics | Study groups were comparable at baseline for important prognostic parameters. To receive a 'yes', groups had to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms and value of main outcome measure(s). |
| Treatment and control interventions specifically described | Details are given of the programme, including disciplines involved and treatment duration. |
| Care provider blinded to the intervention | Treating team is blinded regarding the intervention (NB: rarely possible in this context). |
| Co‐interventions avoided or equal | Co‐interventions should be avoided in the trial design or similar between index and control. |
| Compliance | Compliance was measured and satisfactory in all study groups. |
| Participant blinded to the intervention | Participant was blinded regarding the intervention (NB: rarely possible in this context if consent procedures are properly applied). |
| Outcome assessor blinded to the intervention | Outcome assessor was blinded regarding treatment allocation, and standardised assessment measures were used to structure the interviews. Scored negative if only self reported (questionnaire) outcomes were used and no observer outcomes were provided. |
| Outcome measures relevant | Outcome measures reflected disability (activity) or participation as relevant to the intervention. |
| Adverse effects described | Any adverse effects of the intervention are described. |
| Withdrawal rate described and acceptable | Number of participants included in the study who did not complete the observation period or were not included in the analysis must be described and reasons given. If percentage of withdrawals and dropouts does not exceed 20% for immediate‐ and short‐term follow‐up or 30% for intermediate‐ and long‐term follow‐up, and does not lead to substantial bias, 'yes' is scored. |
| Short‐term outcome measurement | Outcomes were measured at the end of treatment (e.g. admission to discharge) or within 6 months of the end of treatment. |
| Long‐term outcome measurement | Outcomes were measured at 1 year or longer. |
| Timing of outcome assessment in both groups comparable | Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments. |
| Sample size described for each group | Number of participants was stated for each group. |
| Intention‐to‐treat analysis | All randomly assigned participants were included in the analysis (minus missing values), irrespective of non‐compliance and co‐interventions. If loss to follow‐up was substantial (≥ 20%), an intention‐to‐treat analysis as well as an alternative analysis that accounts for missing values (e.g. a worst‐case analysis) should have been performed. |
| Point estimates and measures of variability | A mean or median figure was given for each important outcome parameter, together with a measure of variability such as standard deviation, standard error of the mean or 95% confidence intervals. |
| Category of evidence | Criteria |
| Strong evidence | Consistent statistically significant findings in outcome measures in ≥ 2 high‐quality RCTs. |
| Moderate evidence | Consistent statistically significant findings in outcome measures in ≥ 1 high‐quality RCT and ≥ 1 controlled study. |
| Limited evidence | Consistent statistically significant findings in outcome measures in ≥ 1 high‐quality RCT, or |
| Indicative findings | Consistent statistically significant findings in process or outcome measures in ≥ 1 controlled studies. |
| No evidence | Conflicting results between trials or in cases of insufficient data. |
| Study ID | Internal validity | Descriptive criteria | Statistical criteria | Total score | Positive criteria |
| Kwakkel 1999 | 8 | 5 | 2 | 15 | a,bi,bii,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Wade 1997 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mi,n,o,q. |
| Wade 1998 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mi,n,o,q. |
| Powell 2002 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mii,n,o,q. |
| Cicerone 2008 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,g,i,j,l,mi,n,o,p,q |
| Smith 1982 | 7 | 5 | 2 | 14 | a,bi,c,d,f,g,i,j,l,mi,mii,n,o. |
| Salazar 2000 | 7 | 5 | 2 | 14 | a,bi,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Paniak 1998 | 6 | 5 | 2 | 13 | a,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Slade 2002 | 7 | 3 | 2 | 12 | a,bi,bii,c,d,f,g,j,l,mi,o,p,q |
| Shiel 2001 | 7 | 3 | 2 | 12 | a,bi,d,g,h,i,j,l,mi,o,q. |
| Zhu 2007 | 6 | 4 | 2 | 12 | a.bi,bii,c,d,i,j,l,mi,mii,n,o,p,q |
| Elgmark 2007 | 6 | 4 | 2 | 12 | a,bi,bii,c,d,i,j,l,mii,n,o,p,q |
| Bowen 2001 | 4 | 4 | 2 | 10 | a,c,d,f,j,l,mi,n,o,p,q. |
| Bjorkdahl 2006 | 5 | 3 | 2 | 10 | d,i,j,l,mi,mii,n,o,p,q |
| Bai 2012 | 5 | 3 | 1 | 9 | a,c,g,i,j,l,mi,n,o |
| Werner 1996 | 4 | 4 | 1 | 9 | a,bi,d,i,j,mi,mii,n,o. |
| Semlyen 1998 | 4 | 4 | 1 | 9 | a,d,f,g,j,l,mi,mii,n,o. |
| Andelic 2012 | 4 | 4 | 1 | 9 | a,c,d,g,j,l,mii,n,o |
| Ozdemir 2001 | 3 | 4 | 2 | 9 | a,c,d,f,g,j,mi,o,q. |
| Paniak 1998 and 2000 | Participant and group comparisons | Patients with TBI admitted to hospital (all severities); mean age 33 y Intervention: ‘treatment as needed’ (TAN) (n = 58) Control: single session (SS) of education and advice (n = 53) | |||
| Primary outcomes | Impairment: Problem Checklist (PCL) Participation: Community Integration Questionnaire (CIQ) Health status: Short‐Form 36 (SF‐36) Work status: socio‐economic status (SES) | ||||
| Assessment points | 3 to 4 months (n = 111) and 1 year (n = 105) | ||||
| Summary of results | Participation (CIQ) did not change significantly for either group Impairment (PCL) and health status (SF‐36): Repeated measures MANOVA showed significant effects for time in both groups, which were maintained at 1 year Results showed no significant group interaction or time by group for any of the primary outcomes at either time point | ||||
| Vocational status (SES) | Intervention Mean (SD) | Control Mean (SD) | Difference in mean | P value (MANOVA) | |
| Pre‐injury | 37.2 (18.7) | 34.3 (18.5) | 2.9 | N/S | |
| Baseline | 26.9 (20.7) | 23.2 (19.9) | 0.8 | N/S | |
| 3 to 4 mo | 32.5 (20.2) | 32.8 (19.7) | 0.3 | N/S | |
| 1 y | 34.8 (19.7) | 36.7 (21.0) | 1.9 | N/S | |
| Authors' conclusions |
Interventions appear to be equally effective | ||||
| Salazar 2000 | Participant and group comparisons | Active duty military personnel with moderate to severe TBI; mean age 25 y Intervention: 8‐week intensive in‐patient cognitive‐behavioural programme (n = 67) Control: limited home programme of weekly telephone support from psychiatric nurse (educational material, counselling and suggested home exercises) (n = 53) | |||
| Primary outcomes | Work status: return to work return to fitness for military duty | ||||
| Assessment points | 1 year | ||||
| Summary of results | No overall differences in outcomes between groups Post hoc analysis demonstrated significant group interaction (in favour of the intervention group) for ‘fitness for military duty’ at 1 year for the more severe subgroup, who were unconscious for > 1 h | ||||
| Vocational status at 1 y | Intervention % achieved | Control % achieved | Difference | P value (Fisher's exact) | |
| Return to work | 90% | 94% | 4% (‐5.14) | N/S | |
| Fit for military duty | 73% | 66% | 7% (‐10.24) | N/S | |
| Post hoc analysis of subgroup unconscious for > 1 h (n = 75) | |||||
|
| (n = 35) | (n = 40) | Difference | P value | |
| Fit for military duty | 80% | 58% | 22% | 0.05 | |
| Authors' conclusions | Overall benefit of in‐patient cognitive rehabilitation programme similar to that of limited home rehabilitation, although institutional therapy may be beneficial for selected patients with severe TBI | ||||
| Wade 1997 | Participant and group comparisons | All patients presenting to Accident and Emergency following TBI; age 16 to 65 y Intervention: telephone follow‐up at 7 to 10 days with advice and referral as required (n = 252) Control: no specific intervention (standard services only) (n = 226) (NB: Despite major efforts to trace and contact patients, follow‐up interview at 6 months could be achieved in only 478 of 1156 (41%) participants randomly assigned) | |||
| Primary outcomes | Social disability: Rivermead Head Injury Follow‐Up Questionnaire (RFUQ) Symptoms: Rivermead Post‐concussion Symptoms Questionnaire (RPQ) | ||||
| Assessment points | 6 months | ||||
| Summary of results | No overall differences between intervention and control groups Post hoc analysis revealed significant group interaction (in favour of the active intervention group) with respect to social disability in a subgroup of individuals with more severe injury (>1 h PTA) | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | P value (Mann‐Whitney) | ||
| RFUQ | 3.6 (6.0) | 3.3 (6.3) | N/S | ||
| RPQ | 7.7 (10.9) | 6.8 (10.0) | N/S | ||
| Post hoc analysis of subgroup with PTA > 1 h (n = 121) | |||||
| (n = 71) | (n = 53) | ||||
| RFUQ | 0.85 (0.89) | 1.17 (1.07) | 0.003 | ||
| RPQ | 2.03 (0.85) | 2.21 (0.89) | N/S | ||
| Authors' conclusions | Routine follow‐up does not appear to be necessary for all patients presenting with head injury, but a subgroup of patients with more severe TBI may benefit from such intervention | ||||
| Wade 1998 | Participant and group comparisons | All patients admitted to hospital following TBI (i.e. a more severe group than the total group reported in Wade 1997); age 16 to 65 y Intervention: telephone follow‐up at 7 to 10 days with advice and referral as required (n = 132) Control: no specific intervention (standard services only) (n = 86) (NB: follow‐up data obtained in 218 (69%) of 314 participants randomly assigned) | |||
| Primary outcomes | Social disability: Rivermead Head Injury Follow‐Up Questionnaire (RFUQ) Symptoms: Rivermead Post‐concussion Symptoms Questionnaire (RPQ) | ||||
| Assessment points | 6 months | ||||
| Summary of results | Significant group interaction (in favour of the active intervention group) with respect to social disability and post‐concussion symptoms. Subgroup analysis demonstrated that the main benefit appeared in the group with PTA < 7 days | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | P value (Mann‐Whitney U test) | ||
| RFUQ | 5.36 (7.81) | 8.23 (8.75) | 0.01 | ||
| RPQ | 9.8 (11.7) | 13.9 (13.6) | 0.02 | ||
| Authors’ conclusions | Early intervention by a specialist service significantly reduced social morbidity and severity of post‐concussion symptoms 6 months after head injury, in the group of patients who required admission to hospital. Possibly most beneficial for the moderate to severe group, some of whom may not present without pro‐active intervention | ||||
| Elgmark 2007 | Participant and group comparisons | All patients aged 16 to 60 with mild traumatic brain injury according to American Congress of Rehabilitation medicine criteria Intervention: follow‐up at 2 to 8 weeks by telephone or letter with advice and referral as required (n = 264 ‐ 96 received intervention; 150 declined); 18 lost to follow‐up Control: no specific intervention (regular care) (n = 131); 22 lost to follow‐up 246 treatment and 109 control included in intention‐to‐treat analysis | |||
| Primary outcomes | Symptoms: change in post‐concussion symptoms ‐ Swedish Post‐concussion Symptoms Questionnaire (PCSQ) Social disability: Community Integration Questionnaire (CIQ), Life Satisfaction Questionnaire, Short‐Form Health Survey (SF‐36) | ||||
| Assessment points | 1 y post injury | ||||
| Summary of results | No statistically significant differences were found between intervention and control groups. Participants who experienced few PCS 2 to 8 weeks post injury declined rehabilitation and returned to work. Those who suffered several PCS and accepted rehabilitation did not recover after 1 y | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | Significance
| ||
| Total PCSQ | 5.2 (5.3) | 4.4 (5.3) | N/S | ||
| CIQ | 20.3 (4.0) | 19.8 (4.0) | 0.02 | ||
| Authors’ conclusions | In this particular study of MTBI, active rehabilitation did not change outcomes to a significant degree. Additional studies should focus on patients who remain symptomatic during the first 1 to 3 months and should test various types of interventions | ||||
| PTA = post‐traumatic amnesia; TBI = traumatic brain injury. | |||||
| Smith 1981 | Participant and group comparisons | Patients suitable for out‐patient rehabilitation following discharge from hospital after acute stroke (n = 133); mean age 63 y Intervention: out‐patient physiotherapy and occupational therapy for 6 months at 2 levels of intensity:
Control: no routine rehabilitation, health visitor encourages home exercises as learned in hospital (n = 44) | |||
| Primary outcomes | Dependency for ADL: Northwick Park ADL score | ||||
| Assessment points | 3 and 12 months | ||||
| Summary of results | Significantly greater decrease in ADL scores in intNervention groups compared with controls at 3 months. Difference is sustained at 1 y follow‐up with greater number of control group participants (NB: trend towards better results from intensive rehabilitation than from conventional regimen not tested statistically) | ||||
| Decrease in ADL score | Intensive rehabilitation | Conventional rehabilitation | Control | P value | |
| Mean change 0 to 3 m | 3.54 (n = 41) | 2.87 (n = 40) | 1.50 (n = 42) | 1 vs 3: P value < 0.01 1/2 vs 3: P value < 0.01 | |
| Mean change 0 to 12 m | 3.50 (n = 36) | 2.89 (n = 36) | 0.60 (n = 35) | 1 vs 3: P value < 0.05 | |
| Authors’ conclusions | Out‐patient rehabilitation following stroke appears to be effective. Decreasing intensity of rehabilitation was associated with an increase in both the proportion of participants who deteriorated and the extent to which they deteriorated | ||||
| Werner 1996 | Participant and group comparisons | Patients discharged from in‐patient rehabilitation and ≥ 1 y (mean 2.9 y) after stroke (n = 49); mean age 63 y Intervention: out‐patient physiotherapy and occupational therapy (2 hours, 4 times per week, for 3 months) (n = 33) Control: no specific intervention (n = 16) (NB: 28% (5/33 intervention group and 9/16 control group) did not complete follow‐up: 5 non‐randomised controls were subsequently recruited to make control numbers up to 12) | |||
| Primary outcomes | Activity: Functional Independence Measure ‐ Motor (FIM‐MM) Limitation of participation: Sickness Impact Profile (SIP) Depression: Beck Depression Inventory (BDI) | ||||
| Assessment points | 3 and 9 months | ||||
| Summary of results | Significant changes in FIM and SIP at 3 months maintained at 9 months. Trend towards improved mood did not reach significance | ||||
| Mean change in score | Intervention (n = 28) | Control (n = 12) | Difference in mean | P value (t‐tests) | |
| FIM‐MM (0 to 3 mo) | 6.6 | 1.5 | 5.1 | 0.03 | |
| FIM‐MM (3 to 9 mo) | 0.7 | ‐1.0 | 1.7 | N/S | |
| SIP (0 to 3 mo) | ‐5.2 | 2.6 | 7.8 | 0.04 | |
| BDI (0 to 3 mo) | ‐2.6 | 0.2 | 2.8 | N/S | |
| BDI (3 to 9 mo) | 0.7 | 0.5 | 0.2 | N/S | |
| Authors’ conclusions | Significant gains can still be attained in the post‐acute stroke survivor, despite prior in‐patient rehabilitation services | ||||
| ADLs = activities of daily living. | |||||
| Powell 2002 | Participant and group comparisons | Patients (16 to 65 y) with severe traumatic brain injury 3 mo to 20 y previously (n = 110 allocated: 94 (85%) completed follow‐up) Intervention: inter‐disciplinary team interventions: 2 sessions per week for mean 27.3 (SD 19.1) weeks in community settings (home, work or day centres) (n = 48) Control: written information only (n = 46) | |||
| Primary outcomes | Activity: Barthel Index (BI) Participation: Brain Injury Community Rehabilitation Outcome (BICRO‐39) | ||||
| Assessment points | Approximately 2 y (median 23 mo) (IQR 18 to 40) | ||||
| Summary of results | Intervention group made significantly greater gains on both BI and BICRO scales. Median changes were small, reflecting the diversity of the population, but 40% of intervention group and only 20% of controls made a clinically significant improvement of 2+ points on ≥ 1 BICRO subscale | ||||
| Change scores from baseline | Intervention | Control | P value | ||
| BI: % improving Median (IQR) change | 35.4% 0 (‐5, 5) | 19.6% 0 (‐5, 4) | < 0.05 | ||
| BICRO‐39: % Median (IQR) change | 80% 2.5 (‐1.7, 6.2) | 70% 0.9 (‐4.1, 6.8) | < 0.05 | ||
| Authors’ conclusions | Multi‐disciplinary community rehabilitation, even years after injury, can make clinically significant gains which outlive the active treatment period. | ||||
| Bowen 2001 | Participant and group comparisons | Carers of young adult (16 to 65 y) TBI survivors with hospital stay ≥ 3 days (n = 96) Intervention: active intervention from Head Injury Neurorehabilitation Team (HINT)
Control: no specific intervention ‐ existing services only (n = 27) (NB: 20/96 (21%) received service other than that allocated ‐ only 56% allocated to early intervention actually received it) | |||
| Primary outcomes | Information received: carer perceptions of how well informed they are ‐ 7 questions Emotional state: Wimbledon Self‐report Scale (WSS) | ||||
| Assessment points | 6 mo post injury | ||||
| Summary of results | Analyses adjusted for potential confounding factors confirmed a clinically plausible superior outcome for both treatment groups compared with controls, but none of the results reached significance (set at P value < 0.01) | ||||
| Mean change from baseline | Early (n = 41) | Late (n = 28) | Control (n = 27) | P value (t‐tests) | |
| % poorly informed | 46%‐64% | 46%‐81% | 63%‐89% | N/S | |
| WSS, median (IQR) | 3 (0‐9) | 2 (0‐6) | 8 (1‐15) | N/S | |
| Authors' conclusions | Hypothesis not confirmed, but absence of effect cannot be proven with these data, which may reflect type II error in view of mixing of groups. Longer‐term follow‐up data also required | ||||
| Bjorkdahl 2006 | Participant and group comparisons | Stroke patients (mean age 53 y) discharged from an in‐patient rehabilitation programme
| |||
| Primary outcomes | Functional assessment: Motor and Process Skills (AMPS); secondary measures: mobility (30 m walking test); FIM, instrumental activity measure Impairment: NIH scale | ||||
| Assessment points | End of intervention (3 wk post discharge), 3 and 12 mo | ||||
| Summary of results | Both groups improved significantly from discharge to 1‐y follow‐up. No significant differences between groups for any of the 4 assessments, at any time point, although trends show earlier gains in the home‐rehabilitation group. Only the day clinic group changed ‘significantly’ on the FIM, but degree of change was small (5 FIM points over 1 y). Costs of home rehabilitation programme were less than half those of the day clinic | ||||
| Rasch transformed AMPS data (logits) | Home (n = 30) Mean (SD) | Day clinic (n = 39) Mean (SD) | |||
| Motor | Process | Motor | Process | ||
| Discharge 3 wk 3 mo 1 y | 1.45 1.71 2.02 2.18 | 1.00 1.26 1.23 1.55 | 1.42 1.52 1.88 2.28 | 1.18 1.37 1.54 1.59 | |
| Authors’ conclusions | Both rehabilitation programmes could be recommended, but additional studies are required to define patients who may benefit specifically from home rehabilitation. Costs should be taken into consideration | ||||
| Semlyen 1998 | Participant and group comparisons | Consecutive patients in‐hospital with severe TBI and referred for in‐patient rehabilitation within 4 weeks of injury; age 16 to 62 y Intervention: multi‐disciplinary specialist rehabilitation service ‐ Hunter’s Moor (HM) (n = 33) Control: ‘Other rehabilitation’ (OR) in local non‐specialist services in district hospitals (n = 18) | ||
| Primary outcomes | Activity and independence: Barthel Index, FIM and Newcastle Independence Assessment Form (NIAF) Care‐givers' Health: GHQ‐28 | |||
| Assessment points | 1, 2, 3, 6, 12 and 24 mo after injury | |||
| Summary of results | Only Z values (BI) and t‐values (FIM and NIAF) are given HM intervention group was significantly more disabled at outset (as indicated by FIM up to 3 mo, BI up to 6 mo and NIAF up to 12 mo). By 12 mo, therefore, the HM group had caught up with the OR group in level of activity OR group made significant gains only up to 12 wk on NIAF and FIM cognitive scales, but none on the FIM motor or BI (already at ceiling). By contrast, HM continued to make significant gains up to 24 mo, as assessed by NIAF and BI Significant improvements in carer distress for the HM group were sustained at 2 y, whereas the OR group showed evidence of deterioration between 6 and 12 mo No differences in length of stay between groups | |||
| Authors’ conclusions | Results support the efficiency of specialist rehabilitation services in achieving lasting gains for patients with more severe disability over similar lengths of stay | |||
| Ozedemir 2001 | Participant and group comparisons | Stroke patients referred for rehabilitation after medical stabilisation (n = 60); mean age 59.1 y (SD 5.9) Group 1: in‐patient rehabilitation (n = 30) ‐ ≥ 2 h/d of formal therapy, 5 d/wk Group 2: home‐based rehabilitation (n = 30) ‐ team visited home for 2 h/wk and instructed family in home exercises ‐ family provided therapy ≥ 2 h/d, 7 d/wk Mean duration of rehabilitation 64 d in both groups | ||
| Primary outcomes | Impairment: Brunnstrom score, Ashworth (spasticity) Activity: FIM, Mini‐Mental State Examination (MMSE) | |||
| Assessment points | Before and after rehabilitation | |||
| Summary of results | Significant group differences in favour of in‐patient group for change in Brunnstrom, FIM and MMSE scores, but no differences in spasticity | |||
| Change scores | Group 1 Mean (SD) | Group 2 Mean (SD) | P value (t‐tests) | |
| Ashworth UE | 0.5 (1.2) | 0.2 (0.5) | N/S | |
| Ashworth LE | 0.2 (1.2) | 0.1 (0.3) | N/S | |
| Brunnstrom (UE) | 2.0 (1.2) | 0.3 (0.6) | < 0.001 | |
| Brunnstrom (LE) | 2.4 (1.2) | 0.8 (0.6) | < 0.001 | |
| FIM | 59.6 (14.2) | 12.3 (13.4) | < 0.001 | |
| MMSE | 4.8 (5.0) | 2.0 (2.1) | < 0.001 | |
| Authors' conclusions | Intensive in‐patient rehabilitation provided significantly more favourable functional and cognitive outcomes than home‐based rehabilitation programme | |||
| Kwakkel 1999 | Participant and | Stroke patients within 2 wk of onset (n = 101) All groups received 15 min arm training plus 15 min leg training daily, plus 1.5 h ADL training per wk In addition, for 30 min 5 d/wk, groups received: Group 1: intensive arm training (n = 33) Group 2: intensive leg training (n = 31) Group 3 (control): inflatable splint (n = 37) | |||
| Primary outcomes | ADL ability: Barthel Index (BI) Walking ability: functional ambulation categories (FAC) Dexterity: Action Research Arm Test (AR Arm Test) | ||||
| Assessment points | 0, 6, 12, 20, 26, 38, 52 wk | ||||
| Median (IQR) at 20 wk | Arm training | Leg training | Control | P value (K‐W test) | |
| BI | 17 (14‐20) | 19 (16‐20) | 16 (10‐19) | < 0.05 | |
| FAC | 4 (3‐5) | 4 (3‐5) | 3 (1‐4) | < 0.05 | |
| AR Arm Test | 9 (0‐39) | 2 (0‐56) | 0 (0‐2) | < 0.01 | |
| Authors’ conclusions | Greater intensity of leg training improves early functional recovery; whereas greater intensity of arm training improves only dexterity, providing further evidence that therapy primarily induces effects on abilities at which training is specifically aimed. Functional gains maintained up to 1 y | ||||
| Zhu 2001
| Participant and | Patients aged 12 to 65 y with moderate to severe TBI up to 6 mo post injury (n = 68) Interventions: multi‐disciplinary rehabilitation at 2 intensities:
| |||
| Primary outcomes | Global outcome: Glasgow Outcome Scale (GOS) Activity (disability): FIM, Neurobehavioural Cognitive Status Examination (NCSE) | ||||
| Assessment points | 0, 1, 2, 3, 4, 5, 8, 10 and 12 mo | ||||
| Summary of results | No statistically significant differences in FIM or NSCE between groups. However, significantly greater number of participants achieved maximal FIM and GOS scores within 3 mo, although no differences were noted at later time points and up to 1 year | ||||
| Outcome | Intensive (n = 36) | Conventional (n = 32) | P value (Chi2) | ||
| % good GOS 3 mo | 38
| 14
| Chi2 3.9, df 1, P value = 0.044 P value = 0.483 | ||
| % full FIM 3 mo | 47
| 19
| Chi2 5.8, df 1, P value = 0.015 P value = 0.242 | ||
| Authors’ conclusions | Early intensive rehabilitation can improve functional outcomes of patients with TBI in the early months post injury, and hence may increase the chance of their early return to work Intensive rehabilitation in this study speeded up recovery rather than changing final outcomes | ||||
| Shiel 2001
| Participant and | Patients with moderate to severe TBI (age 16 to 70 y) admitted for rehabilitation (n = 51); stratified and randomly assigned on age and GCS Intervention groups
(NB: study conducted across 2 centres, which had very different structures and processes, 1 offering significantly more routine therapy than the other. Participants at each centre were randomly assigned to received standard and enhanced therapy according to their practice | |||
| Primary outcomes | Activity (disability): FIM+FAM | ||||
| Assessment points | Admission and discharge | ||||
| Summary of results | Despite procedural differences between centres, no significant differences in FIM+FAM change scores were reported between centres. Significant differences were observed between intensive and routine intervention groups and were greatest in the domains of self care, continence, locomotion and psychosocial function. No significant difference in length of stay overall, but possibly skewed by very prolonged LOS for intervention group at 1 centre | ||||
| Change scores during admission | Enhanced intensity Median (IQR)
| Routine Median (IQR) | P (Mann‐Whitney) | ||
| FIM+FAM Motor | 74 (47‐95)
| 21 (2‐48) | < 0.01 | ||
| FIM+FAM Cognitive | 40 (14‐45)
| 12 (5‐22) | < 0.01 | ||
| Authors’ conclusions | Increased intensity of rehabilitation is associated with enhanced function recovery | ||||
| Slade 2001
| Participant and | Patients with acquired brain injury (stroke, TBI or MS) aged 16 to 65 y admitted for rehabilitation (n = 131) Interventions: multi‐disciplinary rehabilitation at 2 intensities:
(NB: Although in theory the intensive group should have received 67% more therapy than controls, in reality, they received only 30% more) | |||
| Primary outcomes | Length of stay (LOS) ADL ability: Modified Barthel Index | ||||
| Assessment points | Admission and discharge | ||||
| Summary of results | No significant differences in discharge Barthel scores were reported (data not given), but this is expected, as patients are discharged at the point at which they are sufficiently independent to manage in the community. This question is then whether more intensive therapy reaches that point earlier Mean LOS for all participants was 84.6 d. Straightforward comparison showed no significant group interactions However, a multiple regression model was applied to take account of confounders of experimental design that could not be controlled for (impairment mix, community delays, missed treatment, etc.); this demonstrated a 14‐d reduction for the intensive group | ||||
| Authors’ conclusions | Intensive rehabilitation has the potential to reduce length of stay, but concurrently, LOS in both groups was increased by 16 d as the result of external delays in discharge | ||||
| Andelic 2012 | Participant and group comparisons | Patients with severe TBI; mean age 29.4 y Intervention:continuous chain of rehabilitation from specialist on ITU directly into specialist subacute rehabilitation post discharge from ITU (n = 33). | ||
| Primary outcomes | Disability: Glasgow Outcome Scale Extended (GOSE) | |||
| Secondary outcomes | Disability: Disability Rating Score (DRS) Employment status: return to work Living situation: at home with or without care, or in a nursing home | |||
| Assessment points | 12 months post injury (n = 61) | |||
| Summary of results | Disability (GOSE) at 12 mo significantly less in the early rehabilitation group than in the control group Significantly higher percentage of participants in the early rehabilitation group were living at home when compared with controls Non‐significant trend towards higher rate of return to work in the early rehabilitation group than in the control group Non‐significant trend towards shorter overall length of stay (acute hospital and rehabilitation unit) in the early rehabilitation group | |||
| Outcomes | Intervention | Control | P value | |
| Favourable GOSE (6‐8) | 71% | 37% | 0.007 | |
| % living at home | 81 | 53 | 0.06 | |
| Authors' conclusions | Early comprehensive rehabilitation in a continuous chain leads to better functional outcomes at 12 months post injury among patients with severe TBI | |||
| Bai 2012 | Participant and group comparisons | Patients with moderate to severe intracerebral haemorrhage; mean age 61 y Intervention: early rehabilitation commencing in the Emergency Department and continuing for 6 mo (n = 181) Controls: standard medical care (n = 183) | ||
| Primary outcomes | Impairment: Fugl‐Meyer Assessment (FMA) Disability: Modified Barthel Index (MBI) | |||
| Assessment points | Outcome measures administered at 1, 3 and 6 mo | |||
| Summary of results | At baseline, post hoc testing showed no significant differences between FMA and MBI scores in the 2 groups At 1, 3 and 6 mo, intervention group had significantly higher FMA and MBI scores | |||
| Authors' conclusions | Early rehabilitation can significantly improve ADLs and motor recovery in patients with intracranial haemorrhage | |||
| Cicerone 2008 | Participant and group comparisons | Mixed severity traumatic brain injury; mean age 36.6 y Intervention: intensive cognitive rehabilitation provided in a therapeutic environment (n = 34) with a focus on group work Control: standard neurorehabilitation; mostly individual, discipline‐specific therapy (n = 34) | |||
| Primary outcomes | Community integration: Community Integration Questionnaire (CIQ) Life satisfaction: Perceived Quality of Life Scale (PQOL) | ||||
| Secondary outcomes | Neuropsychological functioning Perceived self‐efficacy Vocational outcome: Vocational Integration Scale (VIS) | ||||
| Assessment points | 2 wk before treatment, 2 wk post treatment and 6 mo follow‐up | ||||
| Summary of results | Treatment arm showed significantly improved community integration and quality of life scores ‐ not seen in control arm Self efficacy was significantly improved in the treatment arm – another improvement not seen in the control arm Additionally, treatment group had a significantly higher rate of employment compared with control group | ||||
| Standard neurorehabilitation | |||||
| Outcome measures | Pre‐Tx | Post‐Tx | Follow‐up | P value | |
| CIQ | 12.1 | 11.7 | 12.9 | > 0.05 | |
| PQOL | 61.2 | 62.2 | 59.6 | > 0.05 | |
| Authors' conclusions | This trial demonstrates that an intensive cognitive rehabilitation programme can produce significantly better outcomes when compared with standard neurorehabilitation | ||||
| Salazar 2000 | Participant and group comparisons | Active duty military personnel with moderate to severe TBI; mean age 25 y Intervention: 8‐week intensive in‐patient cognitive‐behavioural programme (n = 67) Control: limited home programme of weekly telephone support from psychiatric nurse (educational material, counselling and suggested home exercises) (n = 53) | |||
| Primary outcomes | Work status: return to work return to fitness for military duty | ||||
| Assessment points | 1 y | ||||
| Summary of results | No overall differences in outcomes between groups Post hoc analysis demonstrated significant group interaction (in favour of the intervention group) for ‘fitness for military duty’ at 1 y for members of the more severe subgroup, who were unconscious for >1 h | ||||
| Vocational status at 1 y | Intervention % achieved | Control % achieved | Difference | P value (Fisher's exact) | |
| Return to work | 90% | 94% | 4% (‐5,14) | N/S | |
| Fit for military duty | 73% | 66% | 7% (‐10.24) | N/S | |
| Post hoc analysis of subgroup unconscious for > 1 h (n = 75) | |||||
| (n = 35) | (n = 40) | Difference | P value | ||
| Fit for military duty | 80% | 58% | 22% | 0.05 | |
| Authors' conclusions | Overall benefit of in‐patient cognitive rehabilitation programme similar to that of limited home rehabilitation, although institutional therapy may be beneficial for selected patients with more severe TBI | ||||

