Corticosteroids for tuberculous pleurisy
Information
- DOI:
- https://doi.org/10.1002/14651858.CD001876.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 14 March 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Infectious Diseases Group
- Classified:
-
- Up to date
All studies incorporated from most recent search
All eligible published studies found in the last search (18 Nov, 2016) were included and two ongoing studies have been identified (see 'Characteristics of ongoing studies' section)Assessed: 11 April 2019
- Up to date
- Copyright:
-
- Copyright © 2017 The Authors. Cochrane Database of Systematic Reviews published by John Wiley & Sons, Ltd. on behalf of The Cochrane Collaboration.
- This is an open access article under the terms of the Creative Commons Attribution‐Non‐Commercial Licence, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
HR and PD refreshed the protocol and performed the selection of studies. HR, PD, and YJ extracted data and performed 'Risk of bias' assessments for the included trials. HR revised the Background, Methods, Results, and Discussion sections, with input from PD and YJ.
Sources of support
Internal sources
-
South African Medical Research Council, South Africa.
-
University of Cape Town, South Africa.
-
Liverpool School of Tropical Medicine, UK.
External sources
-
Department for International Development, UK.
Declarations of interest
HR was employed by the Cochrane Infectious Diseases Group, which is funded by a grant from the UK Government DFID.
PD is employed by the National Institute for Research in Tuberculosis, Chennai, a permanent institute under the Indian Council of Medical Research, which is funded by the Government of India through the Ministry of Health and Family Welfare.
HR and PD conducted the preliminary work that contributed to the conception and design of this Cochrane Review as part of the evidence review process for the Indian Extra‐Pulmonary TB (INDEX‐TB) Guidelines, a guideline for extrapulmonary TB commissioned by the Ministry of Health and Family Welfare, Government of India. Global Health Advocates funded this guideline, and the All India Institute of Medical Sciences, New Delhi convened it.
Acknowledgements
We thank Vittoria Lutje, Information Specialist of the Cochrane Infectious Diseases Group (CIDG), for kindly conducting searches for us. Thanks also to Paul Garner and David Sinclair, Co‐ordinating Editors of the CIDG, for their help and support with this review.
HR and the editorial base of the Cochrane Infectious Diseases Group is supported by the Effective Health Care Research Consortium. This Consortium is funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this review do not necessarily reflect UK government policy.
We are grateful to Professor SK Sharma and other members of the core committee, as well as Dr D Behera and other members of the pleural TB specialty subcommittee of the INDEX‐TB Guidelines 2016, whose insights elucidated and enhanced this review update.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Mar 14 | Corticosteroids for tuberculous pleurisy | Review | Hannah Ryan, Jinho Yoo, Padmapriya Darsini | |
| 2007 Oct 17 | Corticosteroids for tuberculous pleurisy | Review | Mark E Engel, Patrice T Matchaba, Jimmy Volmink | |
| 2000 Jan 24 | Steroids for treating tuberculous pleurisy | Review | Patrice Tinaye Matchaba, Jimmy Volmink | |
Differences between protocol and review
We updated this review with the aim of adding any new evidence that may have been published since the previous search in 2007. For this version, we revised the protocol, and in particular altered the outcomes of interest. This was informed by discussions with expert clinicians which took place during the development of a new guideline on extrapulmonary TB in India, the INDEX‐TB guidelines (INDEX‐TB 2016).
Notes
There is a discrepancy between the number of participants across all the trials in this update and the previous version (Engel 2007). This is because the data extraction was done again using a different data extraction tool.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Adrenal Cortex Hormones [adverse effects, *therapeutic use];
- Antitubercular Agents [therapeutic use];
- HIV Seronegativity;
- HIV Seropositivity [mortality];
- Pleura [drug effects];
- Randomized Controlled Trials as Topic;
- Tuberculosis, Pleural [*drug therapy, mortality];
- Tuberculosis, Pulmonary [drug therapy];
Medical Subject Headings Check Words
Humans;
PICOs
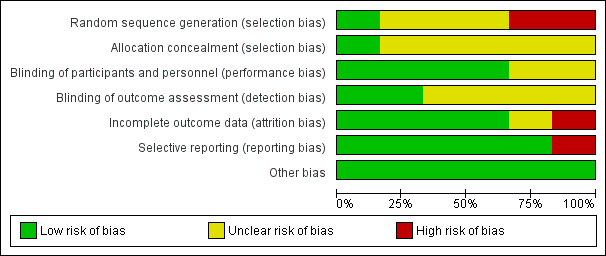
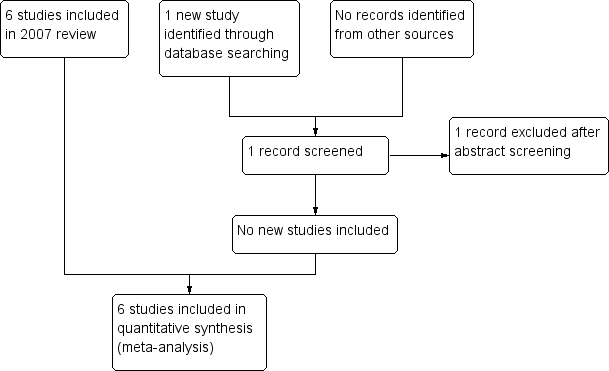
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included trials.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included trial.
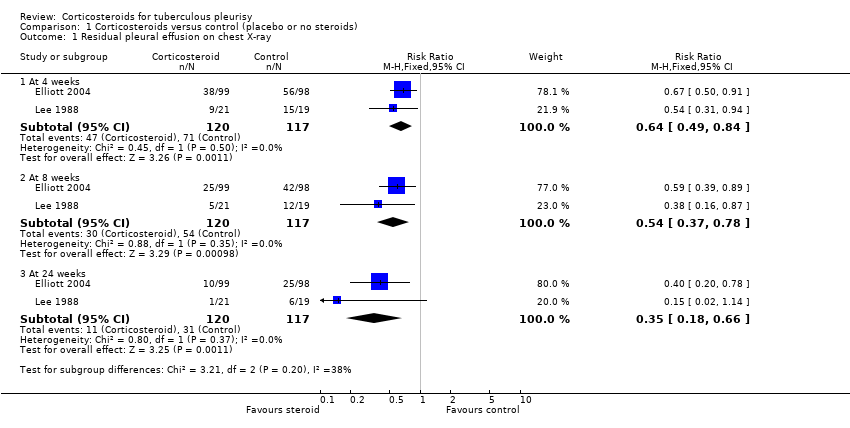
Comparison 1 Corticosteroids versus control (placebo or no steroids), Outcome 1 Residual pleural effusion on chest X‐ray.
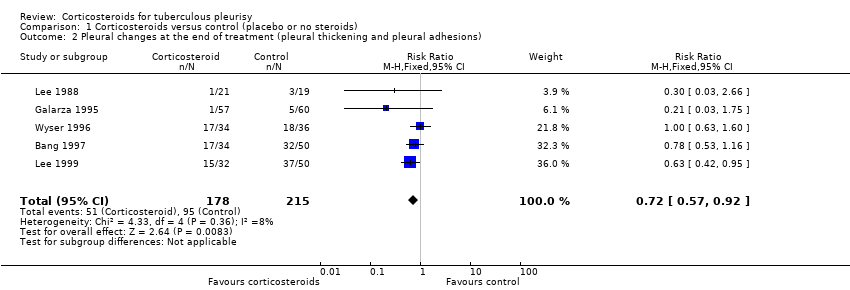
Comparison 1 Corticosteroids versus control (placebo or no steroids), Outcome 2 Pleural changes at the end of treatment (pleural thickening and pleural adhesions).
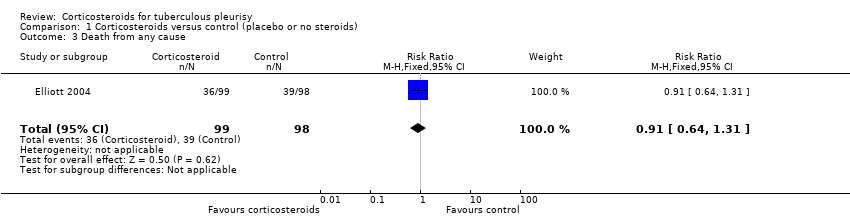
Comparison 1 Corticosteroids versus control (placebo or no steroids), Outcome 3 Death from any cause.

Comparison 1 Corticosteroids versus control (placebo or no steroids), Outcome 4 Adverse events leading to study drug discontinuation.

Comparison 1 Corticosteroids versus control (placebo or no steroids), Outcome 5 HIV‐associated adverse events.

Comparison 2 Effect of study quality on the outcome residual pleural fluid on chest X‐ray, Outcome 1 Residual pleural fluid on chest X‐ray ‐ studies at high risk of selection bias excluded.

Comparison 2 Effect of study quality on the outcome residual pleural fluid on chest X‐ray, Outcome 2 Residual pleural fluid on chest X‐ray ‐ studies at high risk of selection bias included.
| Steroids compared with placebo for pleural TB | |||||
| Patient or population: adults and adolescents with pleural TB Settings: hospital care and community follow‐up Intervention: corticosteroids Comparison: placebo | |||||
| Outcomes | Illustrative comparative risks¹ (95% CI) | Relative effect | Number of participants | Certainty of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Control | Corticosteroids | ||||
| Residual pleural fluid on chest X‐ray at 8 weeks | 62 per 100 | 33 per 100 (23 to 48) | RR 0.54 (0.37 to 0.78) | 237 (2 trials) | ⊕⊕⊝⊝1,2,3,4 |
| Residual pleural fluid on chest X‐ray at 24 weeks | 29 per 100 | 10 per 100 (5 to 19) | RR 0.35 (0.18 to 0.66) | 237 (2 trials) | ⊕⊕⊝⊝1,2,3,4 low |
| Pleural changes at the end of follow‐up (pleural adhesions or pleural thickening on chest X‐ray; follow‐up 6 to 24 months) | 50 per 100 | 36 per 100 (29 to 46) | RR 0.72 (0.57 to 0.92) | 393 (5 trials) | ⊕⊕⊝⊝5,6,7 |
| Long‐term functional respiratory impairment (> 6 months) | — | — | Average percentage predicted FVC similar in corticosteroid and control groups. | 187 (2 trials) | ⊕⊝⊝⊝8 |
| Adverse events leading to treatment discontinuation (follow‐up 6 to 24 months) | 1 per 100 | 3 per 100 | RR 2.78 (1.11 to 6.94) | 590 | ⊕⊕⊝⊝9,10 |
| HIV‐related infections (cryptococcal meningitis) | 5 per 100 | 3 per 100 (1 to 12) | RR 0.59 (0.15 to 2.42) | 103 (1 trial) | ⊕⊝⊝⊝11,12 |
| HIV‐related cancer (Kaposi's sarcoma) | 14 per 100013 | 180 per 1000 (1 to 316) | RR 12.87 (0.73 to 225.40) | 103 (1 trial) | ⊕⊝⊝⊝14,15 |
| ¹The basis for the assumed risk (for example, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Downgraded by one for risk of bias: of the four trials that reported this outcome, we excluded two trials from the final analysis due to high risk of selection bias, after a subgroup analysis suggested the pooled estimate including these studies could be misleading (Bang 1997; Lee 1999). We judged this to be our best estimate of effect. However because we excluded trials from this analysis this generates uncertainty, so we have downgraded the quality of the evidence. | |||||
| Clinical Feature | Isolated pleural TB | Pleuro‐pulmonary TB |
| Sputum microscopy/culture | Negative | Some positive |
| Pleural fluid | Usually demonstrates exudative effusion Usually negative for M. tuberculosis on smear and culture | Usually demonstrates exudative effusion Usually negative for M. tuberculosis on smear and culture |
| Chest X‐ray | Discrete pleural effusion, or pleural thickening, or both | Pleural effusion with other changes such as consolidation, cavities, atelectasis, or hilar enlargement |
| Chest computed tomography (CT) | May demonstrate underlying lung infection | Demonstrates underlying lung infection |
| Pathogenesis | Predominantly driven by delayed type hypersensitivity reaction | Predominantly driven by TB infection of the lung |
| Prognosis | Most people will improve with no antituberculous treatment (ATT), but may experience a relapse of TB infection | People may deteriorate and die without ATT |
| Trial | Country | Year | Participants | Adults or children | HIV status | ATT regimen | Therapeutic thoracocentesis performed | |
| Steroid group | Control group | |||||||
| South Korea | 1991 to 1994 | 34 | 50 | Adults | Not reported | 2RHZE/7RHE | No | |
| Uganda | 1998 to 2002 | 99 | 98 | Adults | Positive | 2RHZE/4RH | No | |
| Spain | 1985 to 1992 | 57 | 60 | Both | Negative | 6RH | Yes | |
| Taiwan | 1983 to 1987 | 21 | 19 | Adults | Not reported | 3RHE/6‐9RH | No | |
| South Korea | 1990 to 1997 | 50 | 32 | Adults | Not reported | 6RHZE or 2RHZS/4RHZ | No | |
| South Africa | 1994 to 1995 | 34 | 36 | Adults | Negative | 6RHZ | Yes | |
| Abbreviations: ATT: antituberculous treatment; E: ethambutol; H: isoniazid; R: rifampicin; S: streptomycin; Z: pyrazinamide. | ||||||||
| Trial | Diagnostic criteria for pleural TB | Other diagnostic tests |
| Microscopy positive for AFB or culture positive from sputum, pleural fluid, or pleural biopsy. |
| |
| Positive culture from pleural biopsy, pleural fluid, or sputum, or histopathologic analysis of pleural biopsy consistent with tuberculous pleurisy |
| |
| At least one of the following
|
| |
| Pleural biopsy reported as pleural TB or chronic granulomatous inflammation |
| |
| TB on pleural biopsy, or pleural effusion plus AFB stain positive or culture positive from sputum, pleural fluid, or pleural biopsy |
| |
| Pleural biopsy with caseating granulomata with or without AFB on histological examination, or positive culture. |
| |
| Abbreviations: ADA: adenosine deaminase activity; AFB: acid‐fast bacilli; CT: computed tomography; ELISA: enzyme‐linked immunosorbent assay; FEV1: forced expiratory volume at one second; FVC: forced vital capacity; HIV: human immunodeficiency virus; PPD: purified protein derivative; PPD‐S: purified protein derivative‐standard; TB: tuberculosis | ||
| Trial | Steroid | Regimen |
| Prednisolone | 1 mg/kg twice daily, tapered by 10 mg each week until cessation | |
| Prednisolone | 50 mg daily for 2 weeks, 40 mg daily for 2 weeks, then 25 mg daily for 2 weeks, then 15 mg daily for 2 weeks, then stopped | |
| Prednisone | 1 mg/kg/day for 15 days, tapering over the next 15 days | |
| Prednisolone | 0.75 mg/kg/day, tapered by 5 mg per week until discontinued once radiological improvement was seen | |
| Prednisolone | 30 mg four times daily for 1 month and tapered over the following month | |
| Prednisone | 0.75 mg/kg/day for 2 to 4 weeks; dose tapered by 5 mg/day over 2 weeks after clinical and radiological improvement | |
| Abbreviations: mg: milligrams | ||
| Trial | Indicator | Units | Corticosteroids | Control | |
| Mean values | “Fever, pleuritic pain, malaise and breathlessness” | Mean days to resolution | 3.8 (N = 34) | 7.41 (N = 50) | |
| “Fever duration” | Mean days | 3.32 (N = 57) | 4.15 (N = 60) | ||
| “Fever, pleuritic pain, malaise and breathlessness” | Mean days to resolution | 2.4 (N = 21) | 5.6 (N = 19) | ||
| Cut‐offs (categorical) | “Anorexia” | Number of participants with anorexia at 4 weeks | 3/99 (3%) | 18/98 (18.4%) | |
| “Cough” | Number of participants with cough at 4 weeks | 35/99 (35.4%) | 57/98 (58.2%) | ||
| “Weight” | Mean weight in kg at 4 weeks | 57 | 52.5 | ||
| Symptoms resolved in all patients (VAS score) | Weeks | 12 | 16 | ||
| Abbreviations: kg: kilograms; VAS: visual analogue scale | |||||
| Trial | Units | Corticosteroids | Control | |
| Mean values | Mean days to resolution | 88 (N=34) | 100 (N=50) | |
| Mean days to resolution | 54.5 (N=21) | 123.2 (N=19) | ||
| Reabsorption index1 at 4 weeks | 93% | 89%2 | ||
| Categorical values | Number of participants with residual effusion at 4 weeks | 26/34 (76.5%) | 39/50 (78%) | |
| Number of participants with residual effusion at 8 weeks | 19/34 (55.9%) | 30/50 (60%) | ||
| Number of participants with residual effusion at 24 weeks | 2/34 (5.9%) | 3/50 (6%) | ||
| Number of participants with residual effusion at 4 weeks | 38/99 (38.4%) | 56/98 (57.1%) | ||
| Number of participants with residual effusion at 8 weeks | 25/99 (30.3%) | 42/98 (56.1%) | ||
| Number of participants with residual effusion at 24 weeks | 10/99 (10.1%) | 25/98 (25.5%)3 | ||
| Number of participants with residual effusion at 4 weeks | 9/21 (42.9%) | 15/19 (78.9%) | ||
| Number of participants with residual effusion at 8 weeks | 5/21 (23.8%) | 12/19 (63.2%) | ||
| Number of participants with residual effusion at 24 weeks | 1/21 (4.8%) | 6/19 (31.6%) | ||
| Number of participants with residual effusion at 8 weeks | 29/32 (90.6%) | 49/50 (98%) | ||
| Number of participants with residual effusion at 24 weeks | 20/32 (62.5%) | 44/50 (88%) | ||
| Abbreviations: N: number of participants | ||||
| Trial | Indicator | Units | Corticosteroids | Control |
| Percentage predicted FVC | Mean percentage predicted FVC | 95% (N = 57) | 95% (N = 60)1 | |
| Percentage predicted FVC | Mean percentage predicted FVC | 85% (N = 34) | 80% (N = 36)2 | |
| Lung function impairment | Number of participants with restrictive PFT results | 11/34 (33.3%) | 14/36 (39.4%)3 | |
| Abbreviations: FVC: forced vital capacity; N: number of participants; PFT: pulmonary function tests | ||||
| Trial | Corticosteroid | Control |
| 1/34 (2.9%)1 | 0/50 | |
| 9/99 (9.1%)2 | 2/98 (2.0%) | |
| 0/57 | NR | |
| 1/21 (4.8%)3 | NR | |
| NR | NR | |
| 4/34 (11.8%) | 3/36 (8.3%)4 | |
| Abbreviations: NR: not reported 1Aggravation of epigastric pain in one patient, steroids stopped, and patient withdrawn from the trial. | ||
| Trial | Indicator | Control (N/98) | Corticosteroid (N/99) |
| Kaposi’s sarcoma | 0 | 6 (6.1%) | |
| Cryptococcal meningitis | 5 (5.1%) | 3 (3.0%) | |
| Oesophageal candidiasis | 23 (23.5%) | 35 (35.4%) | |
| Oral candidiasis | 31 (32.6%) | 31 (31.3%) | |
| Herpes zoster | 19 (19.4%) | 22 (22.2%) | |
| Oral or genital herpes simplex | 20 (20.4%) | 22 (22.2%) | |
| Gastroenteritis | 28 (28.6%) | 34 (34.3%) | |
| Abbreviations: N: number of participants | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Residual pleural effusion on chest X‐ray Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 4 weeks | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.49, 0.84] |
| 1.2 At 8 weeks | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.37, 0.78] |
| 1.3 At 24 weeks | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.18, 0.66] |
| 2 Pleural changes at the end of treatment (pleural thickening and pleural adhesions) Show forest plot | 5 | 393 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.57, 0.92] |
| 3 Death from any cause Show forest plot | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.64, 1.31] |
| 4 Adverse events leading to study drug discontinuation Show forest plot | 6 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.78 [1.11, 6.94] |
| 5 HIV‐associated adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Cryptococcal meningitis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Oesophageal candidiasis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Oral candidiasis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Gastroenteritis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.5 Herpes simplex | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.6 Herpes zoster | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.7 Kaposi sarcoma | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Residual pleural fluid on chest X‐ray ‐ studies at high risk of selection bias excluded Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 4 weeks | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.49, 0.84] |
| 1.2 At 8 weeks | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.37, 0.78] |
| 1.3 At 24 weeks | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.18, 0.66] |
| 2 Residual pleural fluid on chest X‐ray ‐ studies at high risk of selection bias included Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 At 4 weeks | 3 | 321 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.52, 1.07] |
| 2.2 At 8 weeks | 4 | 403 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.47, 1.12] |
| 2.3 At 24 weeks | 4 | 403 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.30, 0.98] |