Fibrinolytic agents for peripheral arterial occlusion
Information
- DOI:
- https://doi.org/10.1002/14651858.CD001099.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 19 December 2013see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Vascular Group
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Iain Robertson selected the trials, wrote the text of the review, interpreted and extracted trial data, and worked on the review manuscript.
David C Berridge selected trials, interpreted and extracted trial data, and reviewed the manuscript.
David Kessel interpreted study data and reviewed the manuscript.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK.
The PVD Group editorial base is supported by the Chief Scientist Office.
Declarations of interest
David Berridge is an author of the Berridge 1991 study which is included in the review.
Acknowledgements
We would like to thank the Cochrane Peripheral Vascular Disease Group for their assistance with this review and the Cochrane Consumer Network for providing a plain language summary.
Version history
| Published | Title | Stage | Authors | Version |
| 2013 Dec 19 | Fibrinolytic agents for peripheral arterial occlusion | Review | Iain Robertson, David O Kessel, David C Berridge | |
| 2010 Mar 17 | Fibrinolytic agents for peripheral arterial occlusion | Review | Iain Robertson, David O Kessel, David C Berridge | |
| 1998 Apr 27 | Fibrinolytic agents for acute arterial occlusion | Protocol | David C Berridge, David O Kessel, Iain Robertson | |
Notes
This is the third of three reviews concerning surgical techniques for thrombolysis.
The first review is 'Surgery versus thrombolysis for initial management of acute limb ischaemia' (Berridge 2013). The second review is 'Infusion techniques for peripheral arterial thrombolysis' (Kessel 2004).
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Arterial Occlusive Diseases [*drug therapy];
- Fibrinolytic Agents [adverse effects, *therapeutic use];
- Peripheral Vascular Diseases [*drug therapy];
- Randomized Controlled Trials as Topic;
- Recombinant Proteins [adverse effects, therapeutic use];
- Streptokinase [adverse effects, therapeutic use];
- Thrombolytic Therapy [adverse effects, *methods];
- Thrombosis [*drug therapy];
- Tissue Plasminogen Activator [adverse effects, therapeutic use];
- Urokinase‐Type Plasminogen Activator [adverse effects, therapeutic use];
Medical Subject Headings Check Words
Humans;
PICOs

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
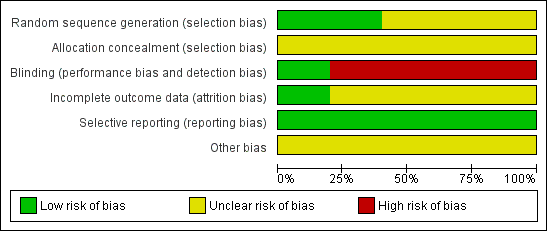
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Comparison 1 Intra‐arterial streptokinase versus intravenous rt‐PA, Outcome 1 Vessel Patency immediately post lysis.

Comparison 1 Intra‐arterial streptokinase versus intravenous rt‐PA, Outcome 2 Asymptomatic Limb salvage at 30 days.

Comparison 1 Intra‐arterial streptokinase versus intravenous rt‐PA, Outcome 3 Amputation at 30 days.

Comparison 1 Intra‐arterial streptokinase versus intravenous rt‐PA, Outcome 4 Death.
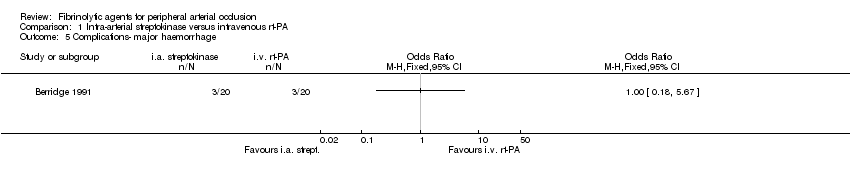
Comparison 1 Intra‐arterial streptokinase versus intravenous rt‐PA, Outcome 5 Complications‐ major haemorrhage.

Comparison 1 Intra‐arterial streptokinase versus intravenous rt‐PA, Outcome 6 Complications‐ minor haemorrhage.
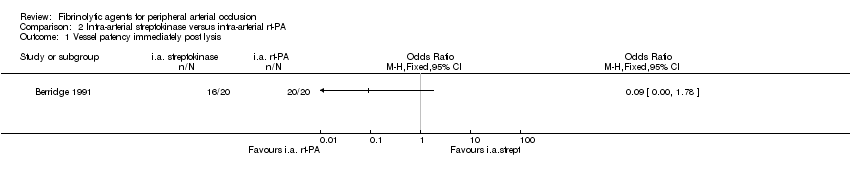
Comparison 2 Intra‐arterial streptokinase versus intra‐arterial rt‐PA, Outcome 1 Vessel patency immediately post lysis.

Comparison 2 Intra‐arterial streptokinase versus intra‐arterial rt‐PA, Outcome 2 Asymptomatic Limb salvage at 30 days.

Comparison 2 Intra‐arterial streptokinase versus intra‐arterial rt‐PA, Outcome 3 Amputation at 30 days.

Comparison 2 Intra‐arterial streptokinase versus intra‐arterial rt‐PA, Outcome 4 Death.

Comparison 2 Intra‐arterial streptokinase versus intra‐arterial rt‐PA, Outcome 5 Complications‐ major haemorrhage.

Comparison 2 Intra‐arterial streptokinase versus intra‐arterial rt‐PA, Outcome 6 Complications‐ minor haemorrhage.
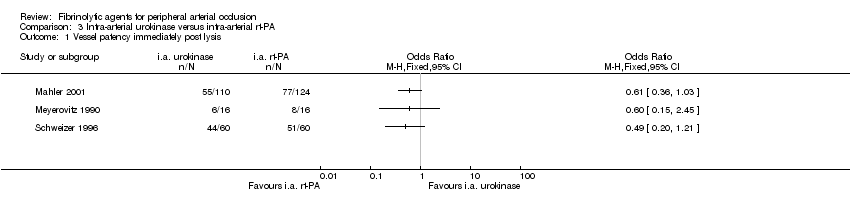
Comparison 3 Intra‐arterial urokinase versus intra‐arterial rt‐PA, Outcome 1 Vessel patency immediately post lysis.
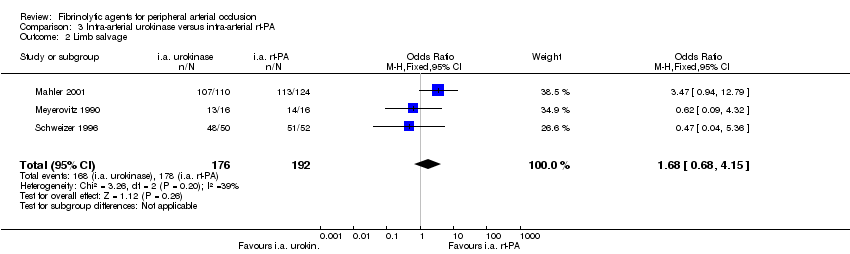
Comparison 3 Intra‐arterial urokinase versus intra‐arterial rt‐PA, Outcome 2 Limb salvage.

Comparison 3 Intra‐arterial urokinase versus intra‐arterial rt‐PA, Outcome 3 Major amputation at 30 days‐6 months.

Comparison 3 Intra‐arterial urokinase versus intra‐arterial rt‐PA, Outcome 4 Death.

Comparison 3 Intra‐arterial urokinase versus intra‐arterial rt‐PA, Outcome 5 Complications ‐ major haemorrhage.
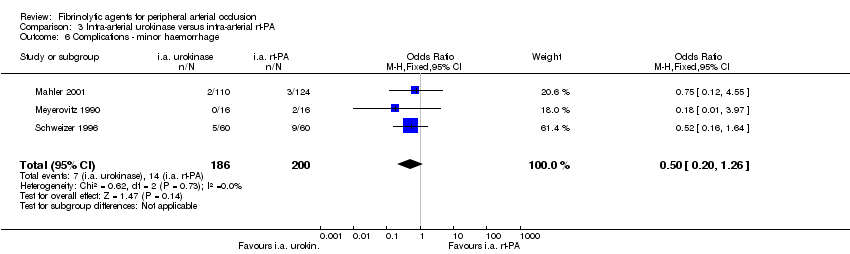
Comparison 3 Intra‐arterial urokinase versus intra‐arterial rt‐PA, Outcome 6 Complications ‐ minor haemorrhage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vessel Patency immediately post lysis Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Asymptomatic Limb salvage at 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Amputation at 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Death Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Complications‐ major haemorrhage Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Complications‐ minor haemorrhage Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vessel patency immediately post lysis Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Asymptomatic Limb salvage at 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Amputation at 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Death Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Complications‐ major haemorrhage Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Complications‐ minor haemorrhage Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vessel patency immediately post lysis Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Limb salvage Show forest plot | 3 | 368 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.68, 4.15] |
| 3 Major amputation at 30 days‐6 months Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Death Show forest plot | 3 | 368 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.24, 2.54] |
| 5 Complications ‐ major haemorrhage Show forest plot | 3 | 298 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.19, 2.40] |
| 6 Complications ‐ minor haemorrhage Show forest plot | 3 | 386 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.20, 1.26] |


