母乳添加脂肪補充劑促進早產兒生長
Abstract
Background
As preterm infants do not experience the nutrient accretion and rapid growth phase of the third trimester of pregnancy, they are vulnerable to postnatal nutritional deficits, including of fat. Consequently, they require higher fat intakes compared to their full term counterparts to achieve adequate growth and development. Human milk fat provides the major energy needs of the preterm infant and also contributes to several metabolic and physiological functions. Although human milk has many benefits for this population, its fat content is highly variable and may be inadequate for their optimum growth and development. This is a 2018 update of a Cochrane Review last published in 2000.
Objectives
To determine whether supplementation of human milk with fat compared with unsupplemented human milk fed to preterm infants improves growth, body composition, cardio‐metabolic, and neurodevelopmental outcomes without significant adverse effects.
Search methods
We used the standard search strategy of Cochrane Neonatal to search the Cochrane Central Register of Controlled Trials (CENTRAL 2018, Issue 1), MEDLINE via PubMed (1966 to 08 February 2018), Embase (1980 to 08 February 2018), and CINAHL (1982 to 08 February 2018). We also searched clinical trials databases, conference proceedings, and the reference lists of retrieved articles for randomised controlled trials and quasi‐randomised trials.
Selection criteria
Published and unpublished randomised controlled trials were eligible if they used random or quasi‐random methods to allocate preterm infants fed human milk in hospital to supplementation or no supplementation with additional fat.
Data collection and analysis
No new randomised controlled trials matching the selection criteria were found but we extracted data from the previously included trial due to changes in review outcomes from when the protocol was first published. Two reviewers independently abstracted data, assessed trial quality, and the quality of evidence at the outcome level using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria. We planned to perform meta‐analyses using risk ratio (RR) for dichotomous data and mean difference (MD) for continuous data, with their respective 95% confidence intervals (CIs). We planned to use a fixed‐effect model and to explore potential causes of heterogeneity via sensitivity analyses.
Main results
One randomised trial involving 14 preterm infants was included. There was no evidence of a clear difference between the fat‐supplemented and unsupplemented groups in in‐hospital rates of growth in weight (MD 0.6 g/kg/day, 95% CI −2.4 to 3.6; 1 RCT, n = 14 infants, very low‐quality evidence), length (MD 0.1 cm/week, 95% CI −0.08 to 0.3; 1 RCT, n = 14 infants, very low‐quality evidence) and head circumference (MD 0.2 cm/week, 95% CI −0.07 to 0.4; 1 RCT n = 14 infants, very low‐quality evidence). There was no clear evidence that fat supplementation increased the risk of feeding intolerance (RR 3.0, 95% CI 0.1 to 64.3; 1 RCT, n = 16 infants, very low‐quality evidence). No data were available regarding the effects of fat supplementation on long‐term growth, body mass index, body composition, neurodevelopmental, or cardio‐metabolic outcomes.
Authors' conclusions
The one included trial suggests no evidence of an effect of fat supplementation of human milk on short‐term growth and feeding intolerance in preterm infants. However, the very low‐quality evidence, small sample size, few events, and low precision diminishes our confidence that these results reflect the true effect of fat supplementation of human milk in preterm infants, and no long‐term outcomes were reported. Further high‐quality research should evaluate the effect on short and long‐term growth, neurodevelopmental and cardio‐metabolic outcomes in the context of the development of multicomponent fortifiers. Optimal dosage, adverse effects, and delivery practices should also be evaluated.
PICOs
Plain language summary
母乳添加脂肪補充劑促進早產兒生長
文獻回顧問題
我們對研究證據進行回顧,以確認在母乳中額外添加脂肪(補充劑)對於早產兒而言,是否可助於生長、體脂肪,肥胖,心臟問題,高血糖和大腦發育且無其他明顯的副作用。
背景
胎兒在第三孕期為生長最快速的時候,同時也於出生前儲存營養。早產兒由於無完整孕期,因此出生時其身體容易缺乏足夠的脂肪量。 因此,與足月嬰兒相比,早產兒需要更高的脂肪攝取量以達到充分的生長及發育。母乳內的脂肪提供約一半的熱量來源,並能促進嬰兒生長及其大腦發育。雖然母乳對於早產兒而言有許多好處,但母乳可能由於其脂肪量不足,而無法促進早產兒達到充分的生長及發育。若以脂肪量不足的母乳哺育的早產兒,可能會對其生長及發育產生不利影響。因此,需額外添加脂肪於母乳中(通常會將少量商業製備的脂肪混合物(例如20毫升)。
研究特性
我們納入了一個證據等級非常低的臨床試驗,其含14位早產兒。此文獻回顧之證據搜集截至2018年2月。
主要成果
對於早產兒而言,在母乳中添加額外脂肪對於其短期體重增加率、身長增加率及頭圍生長率無明顯益處。沒有證據顯示額外脂肪會增加哺餵耐受不良的風險。沒有關於額外添加脂肪對於長期生長,體脂肪,肥胖,高血糖或大腦發育影響的數據。評估副作用的數據也非常有限。
結論
目前尚無足夠的高品質證據證實在母乳中額外添加脂肪對於早產兒之益處與害處,另外尚無長期追蹤的研究報告。 目前額外添加脂肪在母乳的試驗中,其脂肪為綜合強化營養素之其中一部份,未來的試驗應評估脂肪成分對於短期及長期生長,體脂肪,肥胖,高血糖或大腦發育的影響。且應更進一步評估額外添加的脂肪之合適計量及組成、副作用和給予方式。
Authors' conclusions
Summary of findings
| Fat supplementation compared to control for promoting growth in preterm infants | ||||||
| Patient or population: preterm infants | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with control | Risk with Fat supplementation | |||||
| Growth ‐ weight ‐ weight gain (g/kg/day) | The mean weight gain in the unsupplemented human milk group was 15.3 g/kg/day. | MD 0.6 g/kg/day higher | ‐ | 14 | ⊕⊝⊝⊝ | |
| Growth ‐ length ‐ length gain (cm/week) | The mean length gain in the unsupplemented human milk group was 0.8 cm/week. | MD 0.1 cm/week higher | ‐ | 14 | ⊕⊝⊝⊝ | |
| Growth ‐ head circumference ‐ head growth (cm/week) | The mean head growth in the unsupplemented human milk group was 0.9 cm/week. | MD 0.2 cm/week higher | ‐ | 14 | ⊕⊝⊝⊝ | |
| Neurodevelopmental outcomes | ‐ | ‐ | ‐ | ‐ | ‐ | None of the included studies reported on neurodevelopmental outcomes. |
| Duration of hospital admission (days) | ‐ | ‐ | ‐ | ‐ | ‐ | None of the included studies reported on duration of hospital admission. |
| Feeding intolerance | 0 per 1000 | 0 per 1000 | RR 3.00 | 16 | ⊕⊝⊝⊝ | . |
| Necrotising enterocolitis | ‐ | ‐ | ‐ | ‐ | ‐ | None of the included studies reported on necrotising enterocolitis. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: most of the trials lacked methodological details so that we were unable to judge risk of bias. This could have an impact on assessment of growth parameters and possibly the estimate of effect. Single trial. We downgraded one level. 2 Imprecision: few patients and wide confidence intervals, which included meaningful benefit and harm. Single trial. We downgraded two levels. 3 Imprecision: few patients, few events and wide confidence intervals, which include meaningful benefit and harm. Single trial. We downgraded two levels. | ||||||
Background
Description of the condition
Preterm infants are born with inadequate fat stores, due to their being born before the nutrient accretion and rapid growth phase of the third trimester of pregnancy (Robinson 2017). They also have higher nutrient requirements than term infants in the early postnatal period (Fenton 2013). Fat in human milk provides the major energy needs (45% to 55%) of the preterm infant and also contributes to several metabolic and physiological functions paramount to their growth, health, and development (Delplanque 2015). In particular, derivatives of long‐chain polyunsaturated fatty acids (LCPUFA), arachidonic acid (AA), and docosahexaenoic acid (DHA), play key roles in normal immune system functioning as well as brain and retinal development (Delplanque 2015; Hadley 2016; Lapillonne 2014). Thus, insufficient consumption of fat in the preterm infant may have adverse effects on their growth, immune development, neurologic function, and visual acuity (Georgieff 2005; Innis 2003).
Human milk, the preferred enteral nutrition for preterm infants, optimises immunity, visual acuity (Section on Breastfeeding 2012), gastrointestinal function, and neurodevelopmental outcomes in preterm infants (Isaacs 2009; Underwood 2013). In contrast to infant formula, it contains a full array of polyunsaturated fatty acids, including DHA and AA (Moon 2016).
However, in spite of its immense benefits, unsupplemented human milk is nutritionally inadequate for preterm infants for several reasons. Firstly, human milk has insufficient quantities of many nutrients needed for the rapid growth of preterm infants (Su 2014) and its nutrient concentrations fluctuate over time, with fat being the most variable nutrient (Patel 2016). It shows intra‐ and inter‐individual variations (Bhatia 2016), and varies according to maternal diet, time of day, and during a breastfeeding session, with hind milk richer in fat than foremilk (Innis 2014).
Secondly, important reductions in fat concentrations of human milk have been reported during processes of storage, freezing, thawing, and pasteurisation, due to adherence of the disrupted fat globules to container surfaces (Chang 2012; Stocks 1985; Vieira 2011).
Further, breastfeeding initiation and continuation in mothers of preterm infants is not always feasible. Early preterm birth can hinder maternal breast development, delay secretory activation and potentially diminish milk production (Geddes 2013). While these limitations could result in a reliance on donor human milk from mothers who gave birth at term, pasteurisation of donor human milk may inactivate the two endogenous lipases of human milk (lipoprotein lipase and bile salt‐stimulated lipase), thus decreasing lipid absorption and reduce weight gain (Arslanoglu 2013; Peila 2016). Medium‐chain triglyceride (MCT) supplements are sometimes added to donor milk, as these do not require bile salts or pancreatic lipase for digestion and are more easily absorbed than LCPUFA (Kenner 2014). However, this does not provide the high requirements for LCPUFA to optimise brain and retinal development of preterm infants.
A limited supply of fat in preterm infants fed human milk may adversely affect their growth and development. Therefore, additional fat in the form of a supplement may be added to human milk.
Description of the intervention
Enteral fat supplements are available as commercial modular products such as microlipids and medium‐chain triglyceride (MCT) oils (Choi 2016; Yang 2013), a blend of more than one oil including high fat polyunsaturated fatty acid (HF‐PUFA) (Younge 2017) or as multicomponent products like liquid human milk fortifiers (LHMF) (Berseth 2014). They are mixed with human milk and fed enterally to preterm infants once they begin to tolerate breast milk feeds (Berseth 2014). Some of these supplements can also be used via the parenteral route as lipid emulsions (Martin 2015).
Depending on the intended effect, some formulations may contain more than one source of fat supplements that may be combined into the same principal compartment or used together from different compartments. For example, enteral micro lipid and fish oil have recently been successfully combined as a mechanism to reduce intralipid use in a preterm infant with an enterostomy (Yang 2013). Thus, combining different sources of fat supplements may have important maintenance or therapeutic effects. However, the accumulation of certain fatty acids may inhibit the metabolism of others, and cause elevated lipid levels. For example, omega‐3 and omega‐6 lipids compete for the same desaturase enzyme. Thus, a balanced ratio between them is important (Hadley 2016).
How the intervention might work
Paradoxically, in spite of their high need for fat intake per kg body weight, preterm infants present unique challenges that interfere with the delivery of fat (Martin 2015). Preterm infants have low level of activity of pancreatic lipase and bile salt‐stimulated lipase which are normally responsible for a substantial part of fat digestion, micelle formation, and fat absorption (Lindquist 2010). As a result, preterm infants may experience maldigestion and malabsorption of enteral fats, leading to potential intestinal inflammation and injury, loss of energy, and inadequate fat store accumulation (Howles 1999; Martin 2015). Human milk, unlike formula, contains bile salt‐stimulated lipase which enhances the digestion and absorption of milk fat (Martin 2015). Therefore, fat supplementation of human milk is expected to increase fatty acid bioavailability and alleviate dietary deficiency of fat.
Additionally, the unique properties of the different formulations of fat supplements are expected to enhance therapeutic outcomes (Deshpande 2011). For example, MCTs, unlike long‐chain fatty acids, do not require carnitine to enter the mitochondria and so are oxidised rapidly to ketone bodies, making them a quick and readily available source of energy (Longo 2016).
Furthermore, the chain length and saturation of fatty acids impact their absorption (Delplanque 2015). MCTs, whose hydrolysis is independent of the availability of bile and lipase, are more efficiently absorbed than long‐chain fatty acids, making them useful for infants with impaired digestion and absorption of fat, including preterm infants (Martin 2015).
Finally, complications from fat supplementation can also occur. For example, in a study conducted in mice, MCT fortifiers were reported to promote allergic sensitisation and anaphylaxis (Li 2013), while formula supplemented with MCTs is associated with higher osmolality and a higher risk of osmotic diarrhoea (Pereira‐da‐Silva 2008).
Why it is important to do this review
Dietary fat is vital for energy, growth, and long‐term health in preterm infants. However, the previous version of this review found no clear evidence of benefits or harms of fat supplementation of human milk in preterm infants (Kuschel 2000). Interest in fat supplementation of human milk has grown to include not just the digestibility of the fat supplement, but also its quality and role in the visual and neural development of the preterm infant (Koletzko 2014). Thus, it was important to update the review with the most recent trials assessing these effects, including those with LCPUFA supplements.
Objectives
To determine if supplementation of human milk with fat compared with unsupplemented human milk fed to preterm infants improves growth, body composition, cardio‐metabolic and neurodevelopmental outcomes without significant adverse effects.
Methods
Criteria for considering studies for this review
Types of studies
Published and unpublished controlled trials utilising either random or quasi‐random patient allocation were considered for inclusion in this review. Cross‐over trials were excluded.
Types of participants
Preterm infants (< 37 weeks' gestation) receiving enteral feeding of human milk within a hospital setting.
Types of interventions
Human milk with or without additional fat supplementation. Micronutrient and vitamin supplements were allowed in both groups.
Types of outcome measures
The primary and secondary outcomes for this review were aligned with the outcomes of the Cochrane Review Multi‐nutrient fortification of human milk for preterm infants (Brown 2016).
Primary outcomes
-
Growth: weight, length, head circumference, skinfold thickness (WHO 1995), body mass index, and measures of body composition (lean/fat mass) and growth restriction (proportion of infants who remained < 10th percentile for the index population distribution of weight, length, or head circumference). Growth parameters were assessed from birth to hospital discharge, at or after two years’ corrected age, during adolescence, and as adults.
-
Neurodevelopmental outcomes: neurodevelopmental outcomes after 12 months post term included neurological evaluations, developmental scores, and classifications of disability, including auditory and visual disability. We defined neurodevelopmental impairment as the presence of one or more of the following: non‐ambulant cerebral palsy, developmental quotient more than two standard deviations below the population mean, blindness (visual acuity < 6/60) or deafness (any hearing impairment requiring or unimproved by amplification).
Secondary outcomes
-
Duration of hospital admission (days);
-
Feeding intolerance that resulted in cessation or reduction in enteral feeding;
-
Necrotising enterocolitis (NEC);
-
Diarrhoea;
-
Serum bilirubin concentrations;
-
Long‐term measures of cardio‐metabolic health such as insulin resistance, obesity, diabetes, and hypertension.
Search methods for identification of studies
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal search strategy for specialised register).
Electronic searches
We conducted a comprehensive search including: Cochrane Central Register of Controlled Trials (CENTRAL 2018, Issue 1) in The Cochrane Library; MEDLINE via PubMed (1966 to 08 February 2018); Embase (1980 to 08 February 2018); and CINAHL (1982 to 08 February 2018) using search terms unique to the subject of fat supplementation of human milk in neonates, plus database‐specific limiters for RCTs and neonates (see Appendix 1 for the full search strategies for each database). We did not apply language restrictions.
We searched clinical trials registries for ongoing or recently completed trials (clinicaltrials.gov; the World Health Organization’s International Trials Registry and Platform, and the ISRCTN Registry).
Searching other resources
We also searched the reference lists of any articles selected for inclusion in this review in order to identify additional relevant articles. We did not search any additional conference proceedings.
Data collection and analysis
We used the guidelines and standardised methods of the Cochrane Neonatal Collaborative Review Group to assess the methodological quality of the included trials.
Selection of studies
We identified 907 records from the searches for this review. Two authors (EA and JB) independently applied the eligibility criteria to the records identified by the searches. We resolved any disagreements arising through discussions. However, none of the new studies identified were relevant to this review.
Data extraction and management
No new trials were included in the review but, due to changes in our primary and secondary outcomes from the last published protocol (1997), two authors (EA and JB) independently extracted data from the previously included trial. We used a data extraction form which was developed prior to data gathering. Data such as source details, study eligibility, study design, participant characteristics, and intervention and control details were extracted. We planned to resolve conflicts in the data extraction and management process by referral to a third author. The data were then exported into Cochrane’s statistical software, Review Manager 2014 (Review Manager 2014).
Assessment of risk of bias in included studies
Two review authors (EA and JB) independently assessed the risk of bias (low, high, or unclear) of the included trials using the Cochrane ‘Risk of bias’ tool (Higgins 2017) for the following domains:
-
Sequence generation (selection bias)
-
Allocation concealment (selection bias)
-
Blinding of participants and personnel (performance bias)
-
Blinding of outcome assessment (detection bias)
-
Incomplete outcome data (attrition bias)
-
Selective reporting (reporting bias)
-
Any other bias
Any disagreements were resolved by discussion or by a third assessor. See Appendix 2 for a more detailed description of risk of bias for each domain.
Measures of treatment effect
We used the numbers of events in the control and intervention groups of the study to calculate the risk ratio (RR) with 95% confidence intervals (CIs) for dichotomous data. We calculated mean differences (MDs) between treatment groups where outcomes were measured in the same way for continuous data. We did not need to use standardised mean differences (SMD) in this update, although we planned to use it where outcomes from trials were the same but different methods had been used to collect the data. We reported 95% CIs for all outcomes. We did not calculate numbers needed to treat for an additional beneficial outcome (NNTBs) or the numbers needed to treat for and additional harmful outcome (NNTHs) due to insufficient data.
Unit of analysis issues
We did not identify any unit of analysis issues. We planned to undertake analysis at the individual level taking clustering into account as recommended in the Cochrane Handbook for Systematic Reviews of Interventions if we had identified cluster‐randomised trials (Higgins 2017).
Dealing with missing data
We noted levels of attrition. We carried out analyses using an intention‐to‐treat basis, where possible, for all of the outcomes. We analysed all participants, where possible, in the treatment group to which they were randomised, regardless of the actual treatment received. As we had only one included trial, we were unable to conduct sensitivity analyses and were unable to address the potential impact of missing data on the findings of the review.
Assessment of heterogeneity
We planned to assess whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary. We planned to do this by assessing statistical heterogeneity using the Chi2 test and the I2 statistic. An I2 measurement greater than 50% and a low P value (< 0.10) in the Chi2 test for heterogeneity was taken to indicate moderate‐to‐high heterogeneity. Where substantial heterogeneity was detected, we planned to explore possible explanations in sensitivity or subgroup analyses, or both. We planned to take statistical heterogeneity into account when interpreting the results, especially if there was any variation in the direction of effect. We were unable to perform any of these assessments as we included only one trial .
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results. Some types of reporting bias (e.g. publication bias, multiple publication bias, language bias) reduce the likelihood that all studies eligible for a review will be retrieved. If all eligible studies are not retrieved, the review may be biased.
We aimed to conduct a comprehensive search for eligible studies and were alert for duplication of data. We were unable to assess publication bias through the creation of funnel plots as there were insufficient studies for any of the outcomes (10 or more trials required).
Data synthesis
Quality of evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the quality of evidence for the following (clinically relevant) outcomes: growth, neurodevelopment, duration of hospital admission, feeding intolerance that results in cessation or reduction in enteral feeding, and necrotising enterocolitis.
Two authors (EA and JB) independently assessed the quality of the evidence for each of the outcomes above. We considered evidence from randomised controlled trials as high‐quality but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias), consistency across studies, directness of the evidence, precision of estimates, and presence of publication bias. We used the GRADEpro GDT Guideline Development Tool to create a ‘Summary of findings’ table to report the quality of the evidence.
The GRADE approach results in an assessment of the quality of a body of evidence in one of four levels:
-
High: we are very confident that the true effect lies close to that of the estimate of the effect.
-
Moderate: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
-
Low: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect.
-
Very low: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup and sensitivity analyses if moderate‐to‐high heterogeneity was identified. We planned to consider whether an overall summary was meaningful and if it was, we planned to use a random‐effects model to analyse it. We planned to carry out the following subgroup analyses to evaluate differences in outcome between: gestational age subgroups (< 30 versus 30 to < 34 versus 34 to < 37 completed weeks), birth weight subgroups (< 1 kg versus ≥1 kg), male versus female sex; and types of fat supplements (MCT versus other forms). However, there were insufficient data to allow us to conduct any subgroup analyses.
Sensitivity analysis
We planned to conduct sensitivity analysis by examining only those trials considered to have a low risk of bias for allocation concealment and randomisation. We were unable to do this as only one trial was included in the review.
Results
Description of studies
Regarding study details please see: Included studies; Excluded studies.
Results of the search
A search of 1368 records yielded no new trials. However, one trial from the previous review (published in 1999) was included in the 2018 update of this review (Polberger 1989). For a full description of our searches, please see 'Study flow diagram' (Figure 1).

81, Study flow diagram: review update
Included studies
Data were extracted from a full‐text publication for the only trial included in this review (Polberger 1989). This four‐armed randomised controlled trial included 28 randomised preterm infants, of whom 14 fulfilled our predefined criteria. The trial was conducted at two centres in Sweden and was published in English. Details of the included trial are summarised in the table Characteristics of included studies.
Participants
The trial examined preterm infants < 32 gestational weeks and of birth weight < 1500 grams. The infants had no medical problems or major congenital malformations.
Interventions
Standardised rather than targeted fortification was used and infants were randomised to receive either fat (1 gram human milk fat per 100 mL of human milk) or no supplementation. Two other arms of the study evaluated supplementation with protein alone and protein combined with fat, and were excluded from this review. The intervention was commenced once the infants were tolerating enteral feeds at 170 mL/kg/day and was stopped when the infants were breastfed or weighed 2200 grams. Both maternal and donor breast milk were used and supplemental vitamins and minerals (calcium and phosphate) were given to infants in the intervention group.
Comparators
The control group received human milk supplemented with vitamins and minerals (calcium and phosphate).
Outcomes
The trial reported data for our predefined short‐term growth outcomes but no data was reported on long‐term growth, body mass index (BMI), body composition, neurodevelopmental, and cardio‐metabolic outcomes. Of all our secondary outcomes, data were available only for feeding intolerance. Additional data were provided for weight at study end.
Excluded studies
We excluded five full‐text articles (three trials) from this 2018 update . Two trials used interventions that did not meet our predefined criteria (Fewtrell 2011; Makrides 1997), while the other provided data that were not usable Rönnholm 1984. Infants in this latter trial were randomised by alternate allocation to no supplementation, supplementation with protein, supplementation with fat (medium‐chain triglyceride, MCT), or supplementation with both protein and fat. The authors stated that there was no apparent effect from the addition of fat alone and, therefore, combined the groups according to protein supplementation. It was impossible to extract data for the group of infants receiving only fat. See Characteristics of excluded studies for details of exclusions.
Risk of bias in included studies
Overall, we scored all items as unclear risk of bias as there was insufficient methodological detail to make a judgement. See Characteristics of included studies and the 'risk of bias' graph and summary (Figure 2; Figure 3) for details.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We judged random sequence generation and allocation concealment as unclear risk due to insufficient methodological details.
Blinding
We judged performance and detection bias as unclear risk because of lack of information on how blinding was achieved.
Incomplete outcome data
We judged attrition bias as unclear risk because the authors did not report if any differences existed between infants excluded and included in the study. The feeding groups of the excluded infants were also not clarified.
Selective reporting
We judged reporting bias as unclear risk because no details were given as to which were primary and secondary outcomes. We did not view the protocol to ascertain whether the outcomes reported were the only ones collected.
Other potential sources of bias
We judged other potential sources of bias as unclear risk because no details were provided on how the authors resolved differences in sex distribution between the supplemented and unsupplemented groups.
Effects of interventions
1.0 Fat supplementation versus control
1.1 Growth ‐ weight
1.1.1 Weight gain
One randomised controlled trial including 14 infants contributed data (Polberger 1989). Fat supplementation of human milk was not associated with an increase in weight gain compared with unsupplemented human milk (MD 0.6 g/kg/day, 95% CI −2.4 to 3.6; 1 RCT, n = 14 infants, very low‐quality evidence). We downgraded the evidence for risk of bias as there was insufficient methodological information provided to be able to make a judgement. We also downgraded the evidence two levels for imprecision due to the very small sample size and wide confidence intervals spanning across benefits and harms.
1.1.2 Weight at the end of the study
Polberger 1989 reported the weight at the end of the study which was defined as a weight of 2200 grams or when breastfeeding was initiated. There was evidence of a clear difference in weight between the fat‐supplemented and the unsupplemented groups (MD 40.0 g, 95% CI −258.6 to 338.6; 1 RCT, n = 14).
1.2 Growth ‐ length
1.2.1 Length gain
Polberger 1989 contributed data. There was no evidence of a clear difference in length between the fat‐supplemented and the unsupplemented groups (MD 0.1 cm/week, 95% CI −0.08 to 0.3; 1 RCT, n = 14, very low‐quality evidence). We downgraded the evidence for risk of bias as there was insufficient methodological information provided to be able to make a judgement. We also downgraded the evidence two levels for imprecision due to the very small sample size and wide confidence intervals spanning across benefits and harms.
1.3 Growth ‐ head circumference
1.3.1 Head circumference gain
Polberger 1989 contributed data. There was evidence of a clear difference in head growth between the fat‐supplemented and the unsupplemented groups (MD 0.2 cm/week, 95% CI −0.07 to 0.4; 1 RCT, n = 14, very low‐quality evidence). We downgraded the evidence for risk of bias as there was insufficient methodological information provided to be able to make a judgement. We also downgraded the evidence two levels for imprecision due to the very small sample size and wide confidence intervals spanning across benefits and harms.
1.4 Feeding intolerance
Polberger 1989 contributed data. There was no clear evidence that fat supplementation increased the risk of feeding intolerance (RR 3.0, 95% CI 0.1 to 64.3;1 RCT, n = 16 infants, very low‐quality evidence). We downgraded the evidence for risk of bias as there was insufficient methodological information to make a judgement. We also downgraded two levels for imprecision due to the very small sample size, few events and wide confidence intervals.
The study did not evaluate any of our other prespecified primary or secondary outcomes including long‐term growth, BMI, body composition, neurodevelopmental and cardio‐metabolic outcomes.
We were unable to conduct our prespecified subgroup analysis due to insufficient data.
Discussion
Summary of main results
One randomised controlled trial involving 14 preterm infants showed no evidence of an effect of fat supplementation of human milk on in‐hospital rates of growth in weight, length, and head circumference. There was no clear evidence of a difference in the risk of feeding intolerance between the fat‐supplemented and unsupplemented groups. No data were available for the assessment of the effects of fat supplementation on long‐term growth outcomes, BMI, body composition, neurodevelopmental, and cardio‐metabolic outcomes. There were limited data to assess adverse effects.
Overall completeness and applicability of evidence
The only trial included in this review had a very small sample size with methodological flaws that put it at unclear risk of bias in all the 'Risk of bias' domains (Figure 2; Figure 3). The available data were limited and incomplete as some of our outcomes of interest, including long‐term growth, BMI, body composition, neurodevelopmental and cardio‐metabolic outcomes, were not evaluated. Therefore, no conclusions can be drawn on the effects of fat supplementation of human milk fed to preterm infants. Additionally, for the same reasons, no conclusions can be drawn on the applicability of the evidence.
Quality of the evidence
The overall quality of evidence for all our reported outcomes was judged to be of very low‐quality due to a combination of several factors. Firstly, the authors failed to report essential methodological details, including method of randomisation, blinding of study personnel, and outcome assessors. Without such information, it is difficult to adequately judge the risk of bias and quality of evidence. Secondly, the small sample size, few events, and wide confidence intervals, which included possible meaningful benefits and harms, diminished our confidence in the effect estimates.
Potential biases in the review process
We were unable to create funnel plots to assess the potential risk of publication or reporting bias as we had only one trial included in this review. We made every effort to minimise bias by conducting a systematic search of the literature. However, the possibility of missing relevant evidence cannot be excluded. The authors' independent screening of articles and extraction of data in this review also minimised the potential for bias.
Agreements and disagreements with other studies or reviews
To our knowledge, there are no other previous systematic reviews conducted on this topic except for our previous review which included the same single randomised controlled trial published in 2000 and involving 14 preterm infants (Kuschel 2000). We reported similar findings of lack of clear differences between the fat‐supplemented and unsupplemented groups with regards to short‐term rates of weight gain, length gain, head growth, and feeding intolerance.

81, Study flow diagram: review update

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
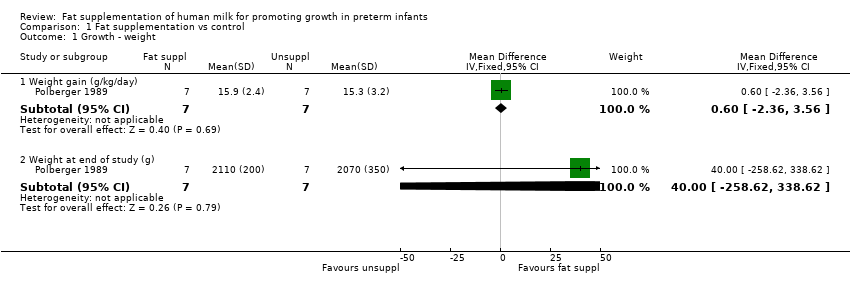
Comparison 1 Fat supplementation vs control, Outcome 1 Growth ‐ weight.

Comparison 1 Fat supplementation vs control, Outcome 2 Growth ‐ length.

Comparison 1 Fat supplementation vs control, Outcome 3 Growth ‐ head circumference.

Comparison 1 Fat supplementation vs control, Outcome 4 Feeding intolerance.
| Fat supplementation compared to control for promoting growth in preterm infants | ||||||
| Patient or population: preterm infants | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with control | Risk with Fat supplementation | |||||
| Growth ‐ weight ‐ weight gain (g/kg/day) | The mean weight gain in the unsupplemented human milk group was 15.3 g/kg/day. | MD 0.6 g/kg/day higher | ‐ | 14 | ⊕⊝⊝⊝ | |
| Growth ‐ length ‐ length gain (cm/week) | The mean length gain in the unsupplemented human milk group was 0.8 cm/week. | MD 0.1 cm/week higher | ‐ | 14 | ⊕⊝⊝⊝ | |
| Growth ‐ head circumference ‐ head growth (cm/week) | The mean head growth in the unsupplemented human milk group was 0.9 cm/week. | MD 0.2 cm/week higher | ‐ | 14 | ⊕⊝⊝⊝ | |
| Neurodevelopmental outcomes | ‐ | ‐ | ‐ | ‐ | ‐ | None of the included studies reported on neurodevelopmental outcomes. |
| Duration of hospital admission (days) | ‐ | ‐ | ‐ | ‐ | ‐ | None of the included studies reported on duration of hospital admission. |
| Feeding intolerance | 0 per 1000 | 0 per 1000 | RR 3.00 | 16 | ⊕⊝⊝⊝ | . |
| Necrotising enterocolitis | ‐ | ‐ | ‐ | ‐ | ‐ | None of the included studies reported on necrotising enterocolitis. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: most of the trials lacked methodological details so that we were unable to judge risk of bias. This could have an impact on assessment of growth parameters and possibly the estimate of effect. Single trial. We downgraded one level. 2 Imprecision: few patients and wide confidence intervals, which included meaningful benefit and harm. Single trial. We downgraded two levels. 3 Imprecision: few patients, few events and wide confidence intervals, which include meaningful benefit and harm. Single trial. We downgraded two levels. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Growth ‐ weight Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Weight gain (g/kg/day) | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐2.36, 3.56] |
| 1.2 Weight at end of study (g) | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 40.0 [‐258.62, 338.62] |
| 2 Growth ‐ length Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Length gain (cm/week) | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.08, 0.28] |
| 3 Growth ‐ head circumference Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Head growth (cm/week) | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.07, 0.37] |
| 4 Feeding intolerance Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |

