Selective versus routine use of episiotomy for vaginal birth
Information
- DOI:
- https://doi.org/10.1002/14651858.CD000081.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 08 February 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Pregnancy and Childbirth Group
- Copyright:
-
- Copyright © 2017 The Authors. Cochrane Database of Systematic Reviews published by John Wiley & Sons, Ltd. on behalf of The Cochrane Collaboration.
- This is an open access article under the terms of the Creative Commons Attribution‐Non‐Commercial Licence, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Hong Jiang and Xu Qian screened all the searches, assessed risk of bias, and extracted data from included studies. Hong Jiang and Xu Qian drafted the review. Paul Garner provided critical comments on the revised protocol sections, helped structure the review, assess, summarise and synthesise the data, helped write the review, conducted the GRADE assessment. Guillermo Carroli provided critical comments on the review. All authors reviewed and agreed the final version of the review.
Sources of support
Internal sources
-
Centro Rosarino de Estudios Perinatales, Rosario, Argentina.
-
Liverpool School of Tropical Medicine, UK.
-
School of Public Health, Fudan University, China.
External sources
-
UK Aid (grant 5242), UK.
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Hong Jiang received support from the Effective Health care Research Consortium, funded by UK aid from the UK government for the benefit of developing countries (Grant: 5242) ‐ this award was paid to Hong Jiang's institution and was used to support the preparation of this review.
Xu Qian received support from the Effective Health care Research Consortium, funded by UK aid from the UK government for the benefit of developing countries (Grant: 5242) ‐ this award was paid to Xu Qian's institution and was used to support the preparation of this review.
Guillermo Carroli is the principal investigator on a large trial included in this review. Risk of bias assessment, data extraction were carried out by authors independent of GC. PG provided oversight on expression of data from this trial and interpretation of its findings with regard to this potential conflict of interest.
Paul Garner is the Director of the Effective Health Care Research Programme Consortium, a DFID funded research programme that aims to increase the number of decisions in low and middle income countries based on reliable evidence.
Acknowledgements
Authors are thankful to Katrina W Tsang, Luciano Mignini, Qin Liu and Chunyi Gu for their consultancy and technical support during the review writing.
This review is supported by the Effective Health Care Research Consortium, funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242).
As part of the pre‐publication editorial process, this review has been commented on by two peers (an editor and referee who is external to the editorial team), members of Cochrane Pregnancy and Childbirth's international panel of consumers, and the Group's Statistical Adviser.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Feb 08 | Selective versus routine use of episiotomy for vaginal birth | Review | Hong Jiang, Xu Qian, Guillermo Carroli, Paul Garner | |
| 2009 Jan 21 | Episiotomy for vaginal birth | Review | Guillermo Carroli, Luciano Mignini | |
| 1999 Jul 26 | Episiotomy for vaginal birth | Review | Guillermo Carroli, Jose Belizan | |
Differences between protocol and review
We removed Objective 2 of the protocol, "to compare midline and mediolateral episiotomy" since we found it inappropriate to include this objective in the course of writing the review, as the topic 'selective versus routine episiotomy for vaginal birth' and which procedure is used are two different topics. We did look in a subgroup analysis for evidence of a difference in effects depending on the procedure, but there was no obvious pattern. We think it better to carry out another independent review to make this comparison, although we did not find eligible studies comparing these two surgical procedures.
In the protocol, the primary outcome was described as "Severe perineal trauma including, severe vaginal trauma, or severe perineal and vaginal trauma (third‐ or fourth‐degree trauma, irrespective of allocated group, as defined in the background)". We noted during the review that it was a little ambiguous as to where this actually included vaginal trauma, so we altered the descriptor slightly to make this explicit.
In the protocol we included "first or second degree perineal trauma". This outcome is uninformative as it excludes women with severe trauma. The outcome, "any trauma" is also uninformative as the control group expects women to receive an episiotomy, which is in effect "second degree trauma" but would not be reported as such. We therefore dropped this outcome.
Since the previous version of this review, we have changed the title from 'Episiotomy for vaginal birth' to 'Selective versus routine use of episiotomy for vaginal birth' for clarity about the scope of the review.
Since only one trial reported perineal pain measured by visual analogue scale, we also reported pain at different time points by any measure of interest. We think this would be informative for clinical practice.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Episiotomy [adverse effects, methods, standards];
- *Parturition;
- Apgar Score;
- Blood Loss, Surgical;
- Dyspareunia [epidemiology];
- Pain Measurement;
- Parity;
- Perineum [*injuries, surgery];
- Randomized Controlled Trials as Topic;
- Surgical Wound Infection [epidemiology];
- Urinary Incontinence [epidemiology];
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICOs

The rationale commonly used to justify routine episiotomy

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
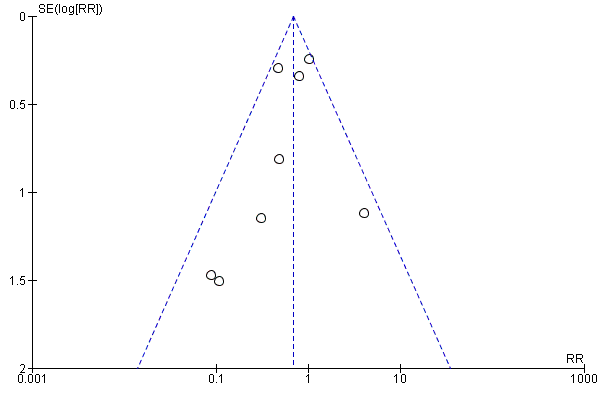
Funnel plot of comparison: 1 Restrictive versus routine episiotomy (planned non‐instrumental), outcome: 1.1 Severe perineal/vaginal trauma

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 1 Severe perineal/vaginal trauma.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 2 Severe perineal/vaginal trauma (grouped by trial implementation success).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 3 Blood loss at delivery (mL).
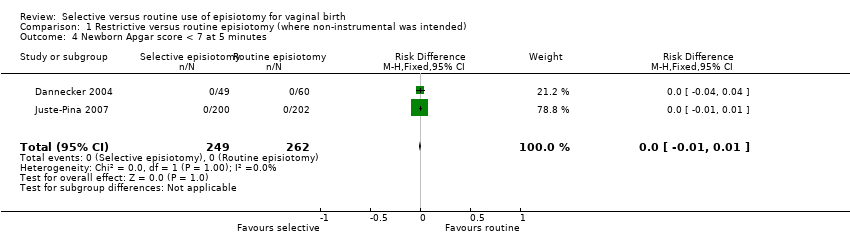
Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 4 Newborn Apgar score < 7 at 5 minutes.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 5 Perineal infection.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 6 Moderate or severe pain (visual analogue scale).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 7 Dyspareunia long term (≥ 6 m).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 8 Genital prolapse long term (≥ 6 m).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 9 Urinary incontinence long term (≥ 6 m).

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 10 Need for perineal suturing.
Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 11 Admission to special care baby unit.

Comparison 1 Restrictive versus routine episiotomy (where non‐instrumental was intended), Outcome 12 Pain at different time points (any measure).

Comparison 2 Restrictive versus routine episiotomy (non‐instrumental, subgroup by parity), Outcome 1 Severe perineal/vaginal trauma.

Comparison 3 Restrictive versus routine episiotomy (non‐instrumental, subgroup midline‐midlateral), Outcome 1 Severe vaginal/perineal trauma.
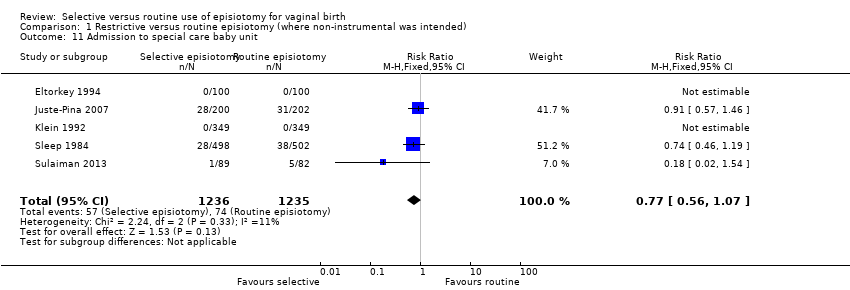
Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 1 Severe perineal/vaginal trauma.

Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 2 Apgar < 7 at 5 minutes.

Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 3 Perineal infection.
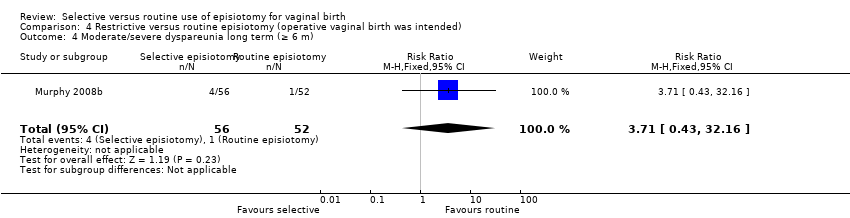
Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 4 Moderate/severe dyspareunia long term (≥ 6 m).
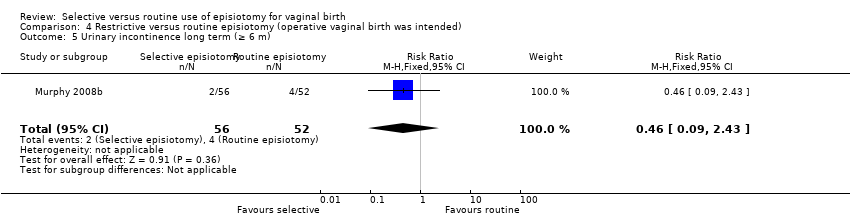
Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 5 Urinary incontinence long term (≥ 6 m).

Comparison 4 Restrictive versus routine episiotomy (operative vaginal birth was intended), Outcome 6 Admission to special care baby unit.
| Selective versus routine episiotomy: all vaginal births where operative vaginal delivery was not anticipated | ||||||
| Patient or population: Women in labour where operative delivery was not anticipated. (Women were above 16 years old and between 28 gestational weeks and full term, with a live singleton fetus, without severe medical or psychiatric conditions, and had vaginal birth.) Intervention: Selective episiotomy (episiotomy rates in the selective group ranged from 8% to 59%). Comparison: Routine episiotomy (episiotomy rates in the routine group ranged from 61% to 100%; episiotomy rate differences between the groups within trials varied from 21% to 91%). | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with routine episiotomy | Risk with selective episiotomy | |||||
| Severe perineal/vaginal trauma | 3.6 per 100 | 2.5 per 100 | RR 0.70 | 5375 | ⊕⊕⊝⊝ due to imprecision and inconsistency | Selective episiotomy compared to routine may reduce severe perineal/vaginal trauma |
| Blood loss at delivery | The mean blood loss at delivery was 278 mL | 27 mL less (95% CI from 75 mL less to 20 mL more) | 336 | ⊕⊝⊝⊝ very low4,5,6 due to risk of bias, imprecision and inconsistency | We do not know if selective episiotomy compared to routine affects blood loss at delivery | |
| Babies with newborn Apgar score < 7 at 5 minutes | 0 per 100 | 0 per 100 | no events | 501 | ⊕⊕⊕⊝ moderate7,8 Due to imprecision | Both selective episiotomy and routine probably has little or no effect on Apgar < 7 at 5 minutes |
| Perineal infection | 2 per 100 | 2 per 100 | RR 0.90 | 1467 | ⊕⊕⊝⊝ Due to imprecision | Selective episiotomy compared to routine may result in little or no difference in perineal infection |
| Women with moderate or severe pain (measured by visual analogue scale) | 45.1 per 100 | 32 per 100 | RR 0.71 | 165 | ⊕⊝⊝⊝ Due to imprecision and indirectness | We do not know if selective episiotomy compared to routine results in fewer women with moderate or severe perineal pain |
| Women with long‐term dyspareunia (≥ 6 months) | 12.9 per 100 | 14.8 per 100 | RR 1.14 | 1107 | ⊕⊕⊕⊝ Due to imprecision | Selective episiotomy compared to routine probably results in little or no difference in women with dyspareunia at > 6 months |
| Women with long‐term urinary incontinence (≥ 6 months) | 32.2 per 100 | 31 per 100 | RR 0.98 | 1107 | ⊕⊕⊝⊝ Due to risk of bias and imprecision | Selective episiotomy compared to routine results may have little or no difference in the number of women with urinary incontinence > 6 months |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 1 for imprecision: confidence intervals range from no important difference to large difference. | ||||||
| Trial | Primigravidae | Follow‐up | |||
| N | per cent (%) | Immediate (< 1 month) | Short‐term (1‐6 months) | Long‐term (≥ 6 months) | |
| 200 | 100 | Discharge & day 7 | No data | No data | |
| 1555/2606 | 60a | Discharge & day 7 | No data | No data | |
| 146 | 100 | Discharge | Several months | A mean follow‐up time of 7.3 months (SD 3.4) | |
| 200 | 100 | Delivery only | No data | No data | |
| 181 | 100 | 4 days | 6 weeks | No data | |
| 98/165 | 59 | 3 days | 3 months | No data | |
| 402 | 100 | No data | 3 months | 3 years 365/402 (91%) | |
| 356/703 | 51 | Discharge | 3 months | No data | |
| 200 | 100 | Discharge | 6 weeks | 1 year | |
| 446 | 100 | Delivery only | N | No data | |
| 420/1000 | 42 | 2 & 10 days | 3 months | 3 years | |
| 209 | 100 | Delivery only | No data | No data | |
| aStratified analysis (primary outcome only) | |||||
| Trial | Selective | Routine | Difference (%) | ||
| n/N | % | n/N | % | ||
| 124/349 | 36 | 198/349 | 57 | 21 | |
| 118/200 | 59 | 169/202 | 84 | 25 | |
| 53/100 | 53 | 83/100 | 83 | 30 | |
| 20/49 | 41 | 46/60 | 77 | 36 | |
| 51/498 | 10 | 258/502 | 51 | 41 | |
| 17/94 | 18 | 49/71 | 69 | 51 | |
| 391/1298 | 30 | 1080/1308 | 83 | 53 | |
| 39/89 | 44 | 82/82 | 100 | 56 | |
| 32/100 | 32 | 100/100 | 100 | 68 | |
| 54/222 | 24 | 223/223 | 100 | 76 | |
| 7/92 | 8 | 89/89 | 100 | 92 | |
| Trial | OVD Included In trial | Total | Included in analysis | Intervention | Control |
| Y | 56/2599 | Y | 24/1302 | 32/1297 | |
| Y | 13/109 | Y | 4/49 | 9/60 | |
| Y | 9/200 | Y | 4/100 | 5/100 | |
| Y | Unknown | Y | 4/92 | Unknown | |
| Y | 20/165 | Y | 10/94 | 10/71 | |
| Unclear | / | / | / | / | |
| Y | 20/703 | Y | Unknown | Unknown | |
| ALL | 200/200 | 101/101 | 99/99 | ||
| Y | 7/445 | Y | 3/222 | 4/223 | |
| Unknown | / | / | / | / | |
| Ali 2004 | Unknown | / | / | / | / |
| Unclear | / | / | / | / |
| Trial | Primary outcome | Outcome related to review primary outcome | Description | Match? |
| Severe perineal trauma | Same | "Extension through the anal sphincter and/or the anal or rectal mucosa (3rd or 4th degree lacerations)" | Matches | |
| Severe perineal trauma | Same | Severe perineal trauma (3rd and 4th degree tear) | Matches | |
| Not specified | Severe perineal trauma | "extension through the anal sphincter or rectal mucosa" | Matches | |
| Not specified | Third‐degree tear | "complete tear including the anal sphincter" | Matches | |
| Not specified | Third‐degree tear | "a complete tear including the anal sphincter, usually extending 2 cm or more up the anal canal" | Matches | |
| Not specified | Third‐degree tear | "one in which the anal sphincter was involved" | Matches | |
| Not specified | Serious case of perineal trauma | "third or fourth degree tear" | Matches | |
| Not specified | Third‐ or fourth‐degree tear | As stated | Matches | |
| Third‐/fourth‐degree tear | Same | Extensive perineal tearing involving the anal sphincter | Matches | |
| Severe laceration to perineal tissues | Same | Third‐degree laceration when the extent of the lesion including the external anal sphincter totally or partially and 4th degree laceration when the rectal mucosa was involved | Matches | |
| Not known | Severe maternal trauma | Extension through the anal sphincter or to the rectal mucosa or to the upper 3rd of the vagina | Matches | |
| Obstetrical anal sphincter injuries | 3rd/4th degree | No further details given | Matches | |
| aMurphy included only women where operative delivery was anticipated and this is described and analysed separately. | ||||
| Trial | Parity | Time assessed | Outcome | Selective n/N (%) | Routine n/N (%) |
| All parities | day 3 | Moderate and severe pain (defined by score categories) | 30/94 (32%) | 32/71 (45%) | |
| Primigravida | day 2 | Average score | Score 1.4, SD 0.8 (N 150) | Score 1.3, SD 0.7 (N 156) | |
| Multigravida | day 2 | Average score | Score 0.9, SD 0.8 (N 156) | Score 0.9, SD 0.7 (N 145) | |
| Primigravida | 1‐5 days | Average score | Score 51, SD 25, 22 (N 49) | Score 69, SD 23, 31 (N 60) |
| Trial | Parameter measured | Collection | Selective n/N (%) | Routine n/N (%) |
| Pain during sex in the last 4 weeks | Questionnaire. Follow up average time of 7.3 months in about 65% of those randomised. | 6/29 (21%) | 13/39 (33%) | |
| Dyspareunia at 3 months; and pain with coitus at 3 years postpartum | Telephone survey 3 months postpartum and interview by telephone at 3 years postpartum. Loss to follow up was 6% in the selective, 5% in the routine group at 3 months; and 8% in the selective, 11% in the routine group at 3 years postpartum. | 3 months postpartum: 42/189 (22%) 3 years postpartum: 20/185 (11%) | 3 months postpartum:67/192 (35%) 3 years postpartum: 15/180 (8%) | |
| Not reported | Collected but not reported | NA | NA | |
| Reported dyspareunia at 3 months postpartum | Self administered postal questionnaire. Follow up rate 66% in selective, and 69% in routine at 3 years postpartum. | 3 months postpartum: 87/394 (22%) 3 years postpartum: 52/329 (16%) | 3 months postpartum: 74/411 (18%) 3 years postpartum: 45/345 (13%) |
| Trial | Parameter measured | Collection | Selective n/N (%) | Routine n/N (%) |
| Urinary incontinence was considered as present whenever a participant gave an answer other than 'never' when replying to "How often do you leak urine involuntarily?" | Questionnaire. Follow‐up average time of 7.3 months in about 65% of those randomised | 13/27 (48%) | 11/41 (27%) | |
| Urinary incontinence at 3 years postpartum | Telephone survey 3 years postpartum. Loss to follow‐up was 8% in the selective, 11% in the routine group at 3 years postpartum | 34/180 (19%) | 49/185 (26%) | |
| Urinary incontinence at 3 months | Questions employing a 4‐point scale | 57/337 (17%) | 60/337 (18%) | |
| Reported urinary incontinence at 3 months after delivery; Reported incontinence of urine at 3 years postpartum | Standardised postal questionnaire administered by mothers at 3 months and 3 years postpartum. Follow‐up rate 62% in selective, and 67% in routine at 3 months postpartum; follow‐up rate 66% in selective, and 69% in routine at 3 years postpartum | 3 months postpartum: 83/438 (19%) 3 years postpartum: 112/329 (34%) | 3 months postpartum: 87/457 (19%) 3 years postpartum: 124/345 (36%) |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 2 Severe perineal/vaginal trauma (grouped by trial implementation success) Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 2.1 Difference in episiotomy rate < 30% | 3 | 1300 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.63, 1.69] |
| 2.2 Difference in episiotomy rate 30% + | 8 | 4877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.38, 0.81] |
| 3 Blood loss at delivery (mL) Show forest plot | 2 | 336 | Mean Difference (IV, Random, 95% CI) | ‐27.16 [‐74.80, 20.49] |
| 4 Newborn Apgar score < 7 at 5 minutes Show forest plot | 2 | 511 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.01, 0.01] |
| 5 Perineal infection Show forest plot | 3 | 1467 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.45, 1.82] |
| 6 Moderate or severe pain (visual analogue scale) Show forest plot | 1 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.48, 1.05] |
| 7 Dyspareunia long term (≥ 6 m) Show forest plot | 3 | 1107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.84, 1.53] |
| 8 Genital prolapse long term (≥ 6 m) Show forest plot | 1 | 365 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.06, 1.41] |
| 9 Urinary incontinence long term (≥ 6 m) Show forest plot | 3 | 1107 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.67, 1.44] |
| 10 Need for perineal suturing Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11 Admission to special care baby unit Show forest plot | 5 | 2471 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| 12 Pain at different time points (any measure) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Any perineal pain at discharge | 2 | 2587 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.25, 2.86] |
| 12.2 Any pain at 10 days | 1 | 885 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.78, 1.27] |
| 12.3 Moderate‐severe pain in first 10 days | 3 | 1127 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.61, 2.12] |
| 12.4 Severe or moderate pain at 3 months postpartum | 1 | 895 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [0.65, 3.49] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 11 | 6177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 1.1 Primiparae | 11 | 4137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.50, 0.93] |
| 1.2 Multiparae | 4 | 2040 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.35, 2.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe vaginal/perineal trauma Show forest plot | 10 | 5977 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.52, 0.94] |
| 1.1 Midline | 2 | 1143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.51, 1.07] |
| 1.2 Mediolateral | 8 | 4834 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.37, 1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severe perineal/vaginal trauma Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.55, 3.07] |
| 2 Apgar < 7 at 5 minutes Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Perineal infection Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.11] |
| 4 Moderate/severe dyspareunia long term (≥ 6 m) Show forest plot | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.71 [0.43, 32.16] |
| 5 Urinary incontinence long term (≥ 6 m) Show forest plot | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.09, 2.43] |
| 6 Admission to special care baby unit Show forest plot | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.68, 6.64] |


