Renin inhibitors versus angiotensin converting enzyme (ACE) inhibitors for primary hypertension
Information
- DOI:
- https://doi.org/10.1002/14651858.CD012569.pub2Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 22 October 2020see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Hypertension Group
- Copyright:
-
- Copyright © 2020 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Wen Lu Tang formulated the idea for the review, developed the basis for the protocol and was responsible for developing the review.
James M Wright offered expert advice, reviewed the protocol, and contributed to the interpretation of the writing of the review.
Gan Mi Wang took the lead role in searching, identifying and assessing studies, in data extraction and analysis, and in writing up the review.
Liang Jin Li took the executive role in identifying and assessing studies, in data extraction and analysis, and in writing up the review.
Sources of support
Internal sources
-
University of British Columbia, Department of Anesthesiology, Pharmacology & Therapeutics, Canada
infrastructure and salary support
-
Fudan University, China
infrastructure and salary support
External sources
-
No sources of support supplied
Declarations of interest
Gan Mi Wang: None known.
Liang Jin Li: None known.
Wen Lu Tang: None known.
James M Wright: None known.
Acknowledgements
We would like to acknowledge the assistance received from the Cochrane Hypertension Group.
We would like to thank Yu Jie Chen, author of the protocol, for assistance in identifying and assessing studies. We would like to thank Douglas Salzwedel, Information Specialist for Cochrane Hypertension, for designing and conducting the searches, and Ciprian Jauca, Managing Editor for Cochrane Hypertension, for his assistance. We would like to express our gratitude to Dr. Vijaya Musini for the editorial advice.
Version history
| Published | Title | Stage | Authors | Version |
| 2020 Oct 22 | Renin inhibitors versus angiotensin converting enzyme (ACE) inhibitors for primary hypertension | Review | Gan Mi Wang, Liang Jin Li, Wen Lu Tang, James M Wright | |
| 2017 Feb 27 | Renin inhibitors versus angiotensin converting enzyme (ACE) inhibitors for primary hypertension | Protocol | Gan Mi Wang, Liang Jin Li, Yu Jie Chen, Wen Lu Tang, James M Wright | |
Differences between protocol and review
None.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Amides [adverse effects, therapeutic use];
- Angiotensin-Converting Enzyme Inhibitors [adverse effects, *therapeutic use];
- Antihypertensive Agents [adverse effects, *therapeutic use];
- Cardiovascular Diseases [epidemiology];
- Cause of Death;
- Fumarates [adverse effects, therapeutic use];
- Heart Rate [drug effects];
- Irbesartan [therapeutic use];
- Kidney Failure, Chronic [epidemiology];
- Lisinopril [therapeutic use];
- Myocardial Infarction [epidemiology];
- Patient Dropouts [statistics & numerical data];
- Ramipril [therapeutic use];
- Randomized Controlled Trials as Topic;
- Renin [*antagonists & inhibitors];
Medical Subject Headings Check Words
Aged; Female; Humans; Male; Middle Aged;
PICOs

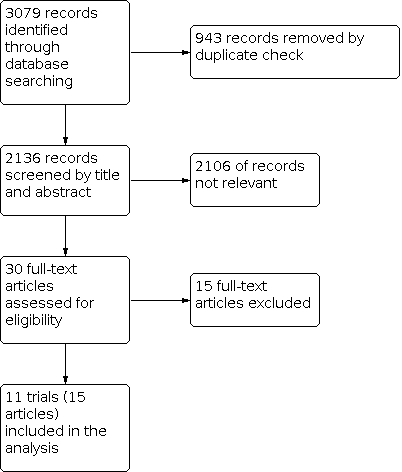
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot of comparison: 1 Renin inhibitors vs. ACE inhibitors, outcome: 1.6 SBP.

Funnel plot of comparison: 1 Renin inhibitors vs. ACE inhibitors, outcome: 1.7 DBP.

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 1: All‐cause mortality

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 2: Fatal or non‐fatal myocardial infarction

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 3: Adverse events

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 4: Fatal or non‐fatal serious adverse events

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 5: Withdrawal due to adverse effects (WDAE)

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 6: SBP

Comparison 1: Renin inhibitors vs. ACE inhibitors, Outcome 7: DBP
| Renin inhibitors compared to ACE inhibitors for primary hypertension | |||||
| Patient or population: people with primary hypertension | |||||
| Outcomes | № of participants | Certainty of the evidence | Relative effect | Anticipated absolute effects* (95% CI) | |
|---|---|---|---|---|---|
| Risk with ACE inhibitors | Risk difference with Renin inhibitors | ||||
| All‐cause mortality | 5962 | ⊕⊕⊝⊝ | RR 1.05 | Study population | |
| 131 per 1000 | 7 more per 1,000 | ||||
| Fatal or non‐fatal myocardial infarction | 957 | ⊕⊝⊝⊝ | RR 0.86 | Study population | |
| 7 per 1000 | 1 fewer per 1000 | ||||
| Adverse events | 6007 | ⊕⊕⊕⊝ | RR 0.98 | Study population | |
| 489 per 1000 | 10 fewer per 1000 | ||||
| Fatal or non‐fatal serious adverse events | 6007 | ⊕⊕⊝⊝ | RR 1.21 | Study population | |
| 27 per 1000 | 6 more per 1000 | ||||
| Withdrawal due to adverse effects (WDAE) | 6008 | ⊕⊕⊝⊝ | RR 0.85 | Study population | |
| 60 per 1000 | 9 fewer per 1000 | ||||
| SBP | 5001 | ⊕⊕⊝⊝ | ‐ | ‐ | MD 1.72 mm Hg lower |
| DBP | 5001 | ⊕⊕⊝⊝ | ‐ | ‐ | MD 1.18 lower |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| aDowngraded due to high risk of source of funding bias. | |||||
| Study ID | N | Follow‐up (weeks) | Mean Age (years) | Co‐morbidity | Intervention | Add‐on drugs | Baseline SBP/DBP (mm Hg) |
|---|---|---|---|---|---|---|---|
| 901 | 36 | T: 72.0 C: 72.2 | Baseline diabetes: aliskiren 21.7%; ramipril 19.6%. | T: Aliskiren 150‐300 mg/day C: Ramipril 5‐10 mg/day | HCTZ 12.5 ‐ 25 mg/day or HCTZ 12.5 ‐ 25 mg/day +amlodipine 5 ‐ 10 mg/day | T: 156.5/85.5 C: 156.6/86.0 | |
| 506 | 8 | T: 60.1 C: 59.8 | NA | T: Aliskiren 150‐300 mg/day C: Ramipril 5‐10 mg/day | None | T: 166.4/89.9 C: 166.3/90.9 | |
| 842 | 26 | T: 53.4 C: 53.1 | Baseline diabetes: aliskiren 10%; ramipril 11.6%. Baseline metabolic syndrome: aliskiren 40.7%; ramipril 43.3%. | T: Aliskiren 150 ‐ 300 mg/day C: Ramipril 5 ‐ 10 mg/day | HCTZ 12.5 ‐ 25 mg/day | T: 151.3/98.8 C: 151.4/98.9 | |
| 7064 | 36.6 months | T: 63.3 C1: 63.3 C2: 63.2 | Heart failure as inclusion criterion; Baseline diabetes: aliskiren 26.8%; enalapril 27.9%; enalapril + aliskiren 28.4% | T: Aliskiren 150 ‐ 300 mg/day C1: Enalapril 5 ‐ 10 mg/day C2: Enalapril 5 ‐ 10 mg/day + Aliskiren 150 ‐ 300 mg/day | Optimal heart failure therapy, including beta blockers, but with the exception of ACE inhibitors | NA Note: Numbers of hypertensive participants at baseline, n(%): T: 1460 (62.4%) C1: 1425 (61.0%) C2: 1447 (61.8%) | |
| 195 | 4 | T1: 52.8 T2: 52.8 C1: 51.5 C2: 53.1 | NA | T1:MK‐8141 250 mg/day T2:MK‐8141 500 mg/day C1: Enalapril 20 mg/day C2: Placebo | None | T1: 150.2/93.8 T2: 149.7/94.2 C1: 150.6/95.1 C2: 151.9/93.6 | |
| 774 | 54 | T: 59.3 C: 59.3 | Baseline diabetes: aliskiren 22.1%; ramipril 25.1%. | T: Aliskiren 150 ‐ 300 mg/day C: Ramipril 5 ‐ 10 mg/day | HCTZ 12.5 ‐ 25 mg/day or HCTZ 12.5 ‐ 25 mg/ay + amlodipine 5 ‐ 10 mg/day | NA | |
| 654 | 9 | T: 53.5 C1: 53.9 C2: 53.4 | NA | T: Aliskiren 150 ‐ 300 mg/day C1: Ramipril 5 ‐ 10 mg/day C2: Irbesartan 150 ‐ 300 mg/day | None | T: 145.5/93 C1:145.8/92.4 C2:145.4/93.0 | |
| 183 | 8 | T: 55.3 C: 55.6 | Baseline diabetes: aliskiren 12.0%; lisinopril 13.8%. Baseline metabolic syndrome: aliskiren 52.8%; lisinopril 58.6% Baseline hypercholesterolemia: aliskiren 16.8%; lisinopril 15.5% | T: Aliskiren 150 ‐ 300 mg/day C: Lisinopril 20 ‐ 40 mg/day | HCTZ 25 mg/day | T: 163.4/108.4 C: 161.7/108.0 | |
| 837 | 8 | T: 60.0 C1: 59.9 C2: 59.5 | Type 1 or 2 diabetes mellitus as inclusion criteria | T: Aliskiren 150 ‐ 300 mg/day C1: Ramipril 5 ‐ 10 mg/day C2: Aliskiren 150 ‐ 300 mg/day+ Ramipril 5 ‐ 10 mg/day | None | T: 157.4/98.4 C1: 155.9/98.2 C2: 156.5/98.4 | |
| 355 | 8 | T1: 73.6 T2: 73.2 T3: 73.0 C: 74.2 | Baseline diabetes: aliskiren 75 mg 13.2%; aliskiren 150 mg 11.9%; aliskiren 300 mg 11.7%; lisinopril 7.0% Baseline metabolic syndrome: aliskiren 75 mg 27.5%; aliskiren 150 mg 22.6%; aliskiren 300 mg 24.5%; lisinopril 23.3% | T1: Aliskiren 75 mg/day T2: Aliskiren 150 mg/day T3: Aliskiren 300 mg/day C: Lisinopril 10 mg/day | None | T1: 160.4/88.0 T2: 160.2/89.3 T3: 160.7/90.1 C: 161.4/88.1 | |
| 1316 | 8 | T1: 52.7 T2: 53.3 T3: 53.8 C: 52.9 | Baseline diabetes: aliskiren 75 mg 10.5%; aliskiren 150 mg 9.6%; aliskiren 300 mg 10.9%; ramipril 5 mg 15.2%. | T1: Aliskiren 75 mg/day T2: Aliskiren 150 mg/day T3: Aliskiren 300 mg/day C: Ramipril 5 mg/day | None | T1: 147.3/98.9 T2: 146.8/98.5 T3: 148.9/98.9 C1: 148.5/98.8 | |
| C: control group; DBP: diastolic blood pressure; HCTZ: hydrochlorothiazide; N: total number of participants randomized in each trial; T: test group; NA: not available; SBP: systolic blood pressure | |||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 All‐cause mortality Show forest plot | 5 | 5962 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.93, 1.18] |
| 1.2 Fatal or non‐fatal myocardial infarction Show forest plot | 2 | 957 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.22, 3.39] |
| 1.3 Adverse events Show forest plot | 10 | 6007 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.93, 1.03] |
| 1.4 Fatal or non‐fatal serious adverse events Show forest plot | 10 | 6007 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.89, 1.64] |
| 1.5 Withdrawal due to adverse effects (WDAE) Show forest plot | 10 | 6008 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.68, 1.06] |
| 1.6 SBP Show forest plot | 9 | 5001 | Mean Difference (IV, Fixed, 95% CI) | ‐1.72 [‐2.47, ‐0.97] |
| 1.7 DBP Show forest plot | 9 | 5001 | Mean Difference (IV, Fixed, 95% CI) | ‐1.18 [‐1.65, ‐0.72] |