18F PET s florbetapirom u ranoj dijagnostici Alzheimerove demencije i drugih demencija u osoba s umjerenim kognitivnim oštećenjem (MCI)
References
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Study characteristics | |||
| Patient sampling |
| ||
| Patient characteristics and setting |
| ||
| Index tests |
After a training session, three nuclear medicine physicians with no access to clinical information, independently rated each PET image for amyloid burden based on successive levels of florbetapir retention from 0 to 4 as follows: (0) None: predominantly white matter tracer retention with no appreciable cortical gray matter retention above cerebellar grey matter levels; (1) Low: evidence of increased tracer retention above cerebellar grey levels in 1 or 2 cortical grey regions; (2) Low‐moderate: either (a) predominantly white matter pattern, but at least 2 cortical regions with increased retention relative to cerebellar grey, or (b) predominantly a cortical gray matter pattern, with most cortical areas mildly positive relative to cerebellum; (3) Moderate‐high: specific cortical retention generally greater than or equal to white matter retention and at least one cortical area with greatly increased retention relative to cerebellar grey; (4) High: Specific cortical uptake greater than or equal to white matter background and multiple cortical areas with greatly increased retention relative to cerebellar grey.
The visual reads were used to classify each data set as either visually positive for Aβ or visually negative for Aβ Visual rating scores of 2 to 4 were considered positive and 0 to 1 were considered negative.
| ||
| Target condition and reference standard(s) |
| ||
| Flow and timing |
| ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Was the PET scan interpretation done by a trained reader physician? | Yes | ||
| Was there a clear definition of a positive result? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Was the study free of commercial funding? | No | ||
| High | |||
| Study characteristics | |||
| Patient sampling |
| ||
| Patient characteristics and setting |
Nine of the participants were women, two of them were Aβ (+), and two of four men were Aβ (+) at baseline. APOE ϵ4 carrier: not reported MMSE: the mean MMSE was 28 (range 24 to 30); for those considered as in the Aβ (+) group, the mean was 26.5 (range 24 to 29) and 28 (range 25 to 30) for those in the Aβ (‐) group. Years of education: seven participants were reported having studied after high school: two of them were Aβ (+) and five were Aβ (‐); for those six having studied at high school or with less education, two were Aβ (+) and four were Aβ (‐), respectively.
| ||
| Index tests |
After a training session, three nuclear medicine physicians with no access to clinical information, independently rated each PET image for amyloid burden based on successive levels of florbetapir retention from from 0 (no amyloid) to 4 (high levels of cortical amyloid). The median of the three visual scores was used to dichotomize participants into Aβ (‐) (score, 0 to 1 point) and Aβ (+) (score, 2 to 4 points). | ||
| Target condition and reference standard(s) |
| ||
| Flow and timing |
| ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Was the PET scan interpretation done by a trained reader physician? | Yes | ||
| Was there a clear definition of a positive result? | Unclear | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the study free of commercial funding? | No | ||
| High | |||
| Study characteristics | |||
| Patient sampling |
| ||
| Patient characteristics and setting |
| ||
| Index tests |
The reader was trained using an online electronic training tool produced by the company who produced the tracer, and the reader was blinded to all clinical data and any other imaging test of each participant.
The threshold used was a SUVR > 1.11 determined at baseline.(Landau 2012, Landau 2013). | ||
| Target condition and reference standard(s) |
Unclear whether clinicians conducting follow‐up were aware of the ¹⁸F‐florbetapir PET scan results. | ||
| Flow and timing |
Number included in analysis: MCI
| ||
| Comparative | |||
| Notes | Dr Schreiber kindly sent the ADNI identification code for each MCI participant (mail received 04/07/2017). | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Was the PET scan interpretation done by a trained reader physician? | Yes | ||
| Was there a clear definition of a positive result? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the study free of commercial funding? | Yes | ||
| Low | |||
Aβ: Amyloid Beta
ADD: Alzheimer's disease dementia
ADNI: Alzheimer's Disease Neuroimaging Initiative
APOE ϵ4: Apolipoprotein E4
CDR: Clinical dementia rating
CIND: Cognitive impairment not dementia
CT: Computed tomography
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.)
FN: False negative
FP: False positive
MBq: Megabecquerel
MCI: Mild cognitive impairment
mCi: Millicurie
MMSE: Mini‐mental state examination
MPRAGE: Magnetization‐Prepared Rapid Gradient‐Echo
NINCDS‐ADRDA: National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association
PET: Positron emission tomography
ROI: Region of interest
SUVR: Standardised uptake value ratio
T: Tesla
TN: True negative
TP: True positive
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| MCI diagnosis at baseline was not made with any of our accepted definitions by protocol for MCI participants. Dr Altomare kindly responded to some questions regarding the method of his study (mail received 16/06/2017). | |
| Not having data for constructing a 2 x 2 table. The study was focused on the development of neuropsychiatric symptoms and not on Alzheimer's disease or dementia progression. | |
| Not having data for constructing a 2 x 2 table. The study was focused on longitudinal quantitative analyses of 18F‐florbetapir PET and their association with progression of dementia. | |
| Not having data for constructing a 2 x 2 table. The study was focused on testing the effects of different reference regions and atrophy‐based partial volume effects on the discriminatory power and longitudinal performance of amyloid PET. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the relationship between regional distributions of brain fibrillar amyloid deposition, neurodegenerative biomarkers in CSF (CSF Aβ 1‐42, t‐tau, p‐tau) and cognitive function (ADAS‐cog) at 24 months follow‐up. | |
| Not having data for constructing a 2 x 2 table. The study compared the power of template‐based cerebellar, pontine, and cerebral white matter reference regions to track 24‐month florbetapir standardized uptake value (SUV) ratio (SUVR) changes; and to relate those changes to 24‐month clinical declines | |
| Not having data for constructing a 2 x 2 table. The study was focused in the diagnostic potential of FDG PET, florbetapir, PiB and CSF biomarkers in monitoring the progression from mild cognitive impairment (MCI) to Alzheimer’s disease (ADD) and cognitively normal (NC) to MCI in a longitudinal study | |
| Not having data for constructing a 2 x 2 table. The study was focused on examining different approaches to amyloid‐PET quantification and a longitudinal analyses of Aβ deposition. | |
| The study focused on the evaluation of brain amyloidosis (ELBA) with a new method on imaging of the 18F‐florbetapir PET scan. We did not include this study because we preferred to include the Schreiber study for the following reasons:
| |
| Not having data for constructing a 2 x 2 table. The study was focused in evaluate five different test strategies for integrating use of florbetapir and FDG PET information to predict rates of cognitive and functional decline over 2 years. | |
| Not having data for constructing a 2 x 2 table. The study was focused on investigating whether different translocator protein genotypes influenced cognitive function, amyloid load, and disease progression over time. | |
| Not having data for constructing a 2 x 2 table. The study was focused on evaluating the 18F‐florbetapir PET and the relationship with cognitive decline in the oldest‐old. | |
| Not having data for constructing a 2 x 2 table. The study was focused on trying to define trajectories of cognitive and functional decline, and characteristics associated with distinct trajectories, using Growth Mixture Modeling. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the estimation of longitudinal change in Aβ burden over 2 years. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the evaluation of native space compared to SPM template methods and a variety of possible SUVR reference regions with highest longitudinal change in the SUVR at 24 months. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the 18F‐florbetapir PET longitudinal evaluation in cognitively normal, MCI, and ADD participants, examining characteristics of normal individuals with subthreshold florbetapir retention and the influence of reference region selection on estimated trajectories across the entire range of amyloid measurements. | |
| This study was focused on comparing participants with amyloid beta negative MCI and participants with ADD enrolled in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) with their Aβ amyloid positive counterparts on a number of clinical, neuropsychological, and biomarker characteristics with an average available follow‐up time for longitudinal cognitive measurements of 1.4 + 0.8 years. The conversion rate in those MCI participants with PET negative was 11% and the conversion in those with PET positive was 45%. We did not include this study, and we preferred Schreiber 2015 to be included for the following reasons:
| |
| Not having data for constructing a 2 x 2 table. This study was focused in the correlation between florbetapir and FDG PET and cognition measured by MMSE at follow‐up. | |
| Not having data for constructing a 2 x 2 table. This study was focused on evaluating the florbetapir status at baseline and different cognitive composite measures at 36 months. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the relationship between regional distributions of brain fibrillar amyloid deposition, neurodegenerative biomarkers in brain (FDG) and CSF (tau), brain structural change, and cognitive function at 24‐month follow‐up. | |
| Not having data for constructing a 2 x 2 table. The study was focused on evaluating the 18F‐florbetapir PET and the relationship with cognitive decline at follow‐up. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the regional effects of amyloid retention measured by the 18F‐florbetapir PET scan on the rate of hypometabolism measured by FDG PET scan over the follow‐up. | |
| This study was focused on comparing the diagnostic test accuracy with CSF Aβ42 and the 18F‐florbetapir PET scan in three different groups, healthy controls, Alzheimer's disease dementia, and MCI (progressive vs stable MCI) participants. We did not include this study, as we preferred Schreiber 2015 to be included for the following reasons:
| |
| Not having data for constructing a 2 x 2 table. This study was focused in determine the extent to which CSF and 18F‐florbetapir PET contribute independent diagnostic information in AD studies, and to determine the nature and degree of pathology in discordantly classified individuals in healthy controls, ADD patients, and MCI participants. | |
| Not having data for constructing a 2 x 2 table. The study was focused on testing if CSF and amyloid beta PET scan biomarkers were independently related to other Alzheimer's disease markers, and to examine individuals who were discordantly classified by these two biomarker modalities with a follow‐up for up to three years. | |
| Not having data for constructing a 2 x 2 table. The study was focused on relationships in a large number of brain regions in MCI participants with cognitive evaluations for up to three years with Logical Memory delayed recall and Rey Auditory Verbal Learning Test delayed recall. | |
| Not having data for constructing a 2 x 2 table. The study was focused on MCI participants and 18F‐florbetapir at baseline and follow‐up for up to three years with cognitive evaluations with MMSE, ADAS11 and CDR sum of boxes. | |
| Not having data for constructing a 2 x 2 table. The study was focused on comparing neurodegeneration in 18F‐florbetapir accumulators and nonaccumulators based on a 24‐month assessment. | |
| Not having data for constructing a 2 x 2 table. The study was focused on MCI participants that had longitudinal evaluation with the 18F‐florbetapir PET scan over two years and different methods to establish the PET positivity. | |
| Not having data for constructing a 2 x 2 table. The study was focused on neuropsychological and clinical decline in participants with MCI and if they were associated with brain amyloid‐beta deposition and tau hyperphosphorylation. | |
| The study was focused on amnestic MCI individuals and whether the synergism between Aβ aggregation and tau hyperphosphorylation could determine the progression from amnestic MCI to ADD dementia. We did not include this study because we preferred the Schreiber study to be included for the following reasons:
Dr Pascoal kindly responded to some questions regarding the method of his study and provided the ADNI identification code of the participants (mail received 16/06/2017). | |
| Not having data for constructing a 2 x 2 table. The study was focused on the evaluation of the correlation of florbetapir SUVR with cognitive change from baseline to month 24 in MCI and cognitively normal participants, PET PiB, and CSF amyloid and tau levels. | |
| Not having data for constructing a 2 x 2 table. The study was focused on the comparative assessment of two‐year change in amyloid deposition, glucose metabolism, and hippocampal atrophy in healthy controls, MCI and ADD participants. | |
| Not having data for constructing a 2 x 2 table. The study was focused on evaluating the effect of reference tissue normalization in a test–retest 18F‐florbetapir SUVR study using different reference regions and evaluating the correlation between 18F‐florbetapir PET and concurrent CSF Aβ1–42 levels in a MCI cohort over the course of 2 years. | |
| Not having data for constructing a 2 x 2 table. The study was focused on evaluating cognitive decline measured by ADAS‐cog in participants with negative and positive 18F‐florbetapir PET scan imaging with a clinical follow‐up of 18 months. | |
| Not having data for constructing a 2 x 2 table. The study was focused on comparing penalized regression analysis, with more classical unregularised regression models in respect to predicting conversion from MCI to ADD in 127 MCI subjects who had a clinical follow‐up between 6 and 31 months. | |
| Not having data for constructing a 2 x 2 table. The study was focused on determining the association between CSF and PET amyloid biomarkers (cross‐sectional and longitudinal measures) and comparing the cut‐offs for these measures. | |
| Not having data for constructing a 2 x 2 table. The study was focused on characterising MCI participants separated into four groups according to their abnormal amyloid‐beta 42 levels and abnormal hippocampal volume or hypometabolism using fluorodeoxyglucose PET and the conversion rate at 24 months. | |
| The study was focused on exploring the contribution of different neuroimaging modalities in their predictive power and characterised the sensitive biomarkers from each modality. We did not include this study, as we preferred the Schreiber study to be included for the following reasons:
|
Aβ: Amyloid Beta
ADAS11: Alzheimer's disease assessment scale‐11
ADAScog: Alzheimer's Disease Assessment Scale‐Cognitive subscale
ADD: Alzheimer's disease dementia
ADNI: Alzheimer's Disease Neuroimaging Initiative
CDR: Clinical dementia rating
CSF: Cerebrospinal fluid
ELBA: Evaluation of brain amyloidosis
FDG: Fluorodeoxyglucose
MCI: Mild cognitive impairment
MMSE: Mini‐mental state examination
PET: Positron emission tomography
PiB: Pittsburgh compound B
SPM: statistical parametric mapping
SUV: Standardised uptake value
SUVR: Standardised uptake value ratio
Characteristics of ongoing studies [ordered by study ID]
Jump to:
| Trial name or title | Clinical and neuroimaging study on preclinical Alzheimer's disease |
| Target condition and reference standard(s) | Estimation of progression rate at 36 months of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir, PET PiB, 18F‐flutemetamol |
| Starting date | 2016 |
| Contact information | Hiroshi Mori |
| Notes |
| Trial name or title | FluoroAv45 Imaging Research‐in Alzheimer's Disease (FAIR‐AD) |
| Target condition and reference standard(s) | Cogitive decline after 2 years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2009 |
| Contact information | vincent.camus@univ‐tours.fr |
| Notes |
| Trial name or title | Multi‐modal Neuroimaging in Alzheimer's Disease (IMAP) |
| Target condition and reference standard(s) | Cognitive decline over three years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2008 |
| Contact information | Vincent de La Sayette, University Hospital, Caen |
| Notes |
| Trial name or title | Multi‐modal Neuroimaging in Alzheimer's Disease (IMAP+) |
| Target condition and reference standard(s) | Cognitive decline over three years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2012 |
| Contact information | Vincent de La Sayette, University Hospital, Caen |
| Notes |
| Trial name or title | A Study of Brain Aging in Vietnam War Veterans (DOD‐ADNI) |
| Target condition and reference standard(s) | Cognitive decline over one year of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2012 |
| Contact information | Michael W. Weiner, University of California, San Francisco |
| Notes |
| Trial name or title | Can the Assessment of the Subhippocampal Region Contribute to the Detection of Early Diagnosis of Alzheimer's Disease? A Validation Study Using PET With florbetapir (AV‐45) |
| Target condition and reference standard(s) | Cognitive decline over two years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2011 |
| Contact information | Bernard Belaiguesa, Assistance Publique Hopitaux De Marseille |
| Notes |
| Trial name or title | Longitudinal Study of Brain Amyloid imaGing in MEMENTO (MEMENTOAmyGing) |
| Target condition and reference standard(s) | Cognitive decline over two years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir and 18F‐flutemetamol |
| Starting date | 2014 |
| Contact information | Genevieve Chene, CIC‐EC7 ‐ ISPED ‐ CHU de Bodeaux |
| Notes |
| Trial name or title | Amyloid and Glucose PET Imaging in Alzheimer and Vascular Cognitive Impairment Patients With Significant White Matter Disease (MITNEC C6) |
| Target condition and reference standard(s) | Cognitive decline over two years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2014 |
| Contact information | Maryam Niapour, [email protected] |
| Notes |
| Trial name or title | Alzheimer's Disease Imaging With PET/MRI ‐ Beta‐amyloid |
| Target condition and reference standard(s) | Assessing the diagnosis of a participant at one year of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir |
| Starting date | 2014 |
| Contact information | James O'Donnell, [email protected] |
| Notes |
| Trial name or title | Alzheimer's Disease Neuroimaging Initiative 3 (ADNI3) Protocol |
| Target condition and reference standard(s) | Rate of progression to MCI or dementia due to ADD, reference standard not specified |
| Index and comparator tests | 18F‐florbetapir and 18F‐florbetaben |
| Starting date | 2016 |
| Contact information | Paul Aisen, Director, Alzheimer's Therapeutic Research Institute, University of Southern California |
| Notes |
ADD:Alzheimer's disease dementia
MCI: Mild cognitive impairment
PET: Positron emission tomography
PiB: Pittsburgh Compound B
Data
Presented below are all the data for all of the tests entered into the review.
| Test | No. of studies | No. of participants |
| 1 MCI to ADD by visual assessment from 2 to less than 4 years of follow‐up Show forest plot | 1 | 47 |
| Test 1  MCI to ADD by visual assessment from 2 to less than 4 years of follow‐up. | ||
| 2 MCI to ADD by visual assessment from 1 to less than 2 years follow‐up Show forest plot | 1 | 401 |
| Test 2  MCI to ADD by visual assessment from 1 to less than 2 years follow‐up. | ||
| 3 MCI to ADD by SUVR at 1 to less than 2 years follow‐up Show forest plot | 1 | 401 |
| Test 3 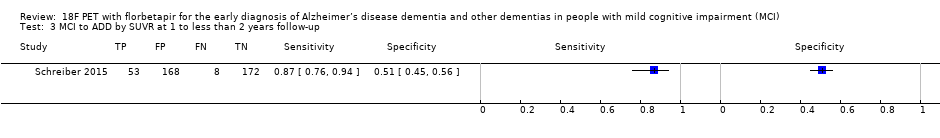 MCI to ADD by SUVR at 1 to less than 2 years follow‐up. | ||
| 4 MCI to any form of dementia Show forest plot | 1 | 5 |
| Test 4  MCI to any form of dementia. | ||

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study

Forest plot of tests: 1 MCI to ADD by visual assessment from 2 to less than 4 years of follow‐up, 2 MCI to ADD by visual assessment from 1 to less than 2 years follow‐up, 3 MCI to ADD by SUVR at 1 to less than 2 years follow‐up, 4 MCI to any form of dementia.

MCI to ADD by visual assessment from 2 to less than 4 years of follow‐up.

MCI to ADD by visual assessment from 1 to less than 2 years follow‐up.
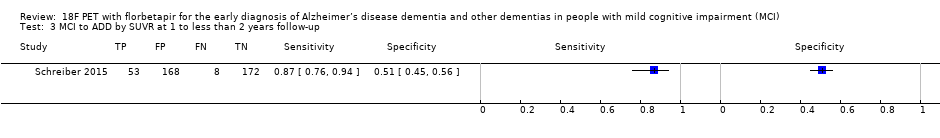
MCI to ADD by SUVR at 1 to less than 2 years follow‐up.

MCI to any form of dementia.
| What is the diagnostic accuracy of 18F‐florbetapir PET amyloid biomarker for predict progression to ADD, any other form of dementia (non‐ADD) or any form of dementia in people with MCI? | |||||||
| Descriptive | |||||||
| Patient population | Participants diagnosed with MCI at time of performing the test using any of the Petersen criteria or Winblad criteria or CDR = 0.5 or any 16 definitions included by Matthews (Matthews 2008). | ||||||
| Sources of referral | Not reported (n = 2) Mixed (memory clinics, newspaper ads, radio, and other public media campaigns) (n = 1) | ||||||
| MCI criteria | ADNI criteria, CDR 0.5 criterion was included (n = 2) CIND (cognitive impairment not dementia) (Matthews 2008) (n = 1) | ||||||
| Sampling procedure | Unclear (n = 3) | ||||||
| Prior testing | The only testing prior to performing the 18F‐florbetapir PET amyloid biomarker was the application of diagnostic criteria for identifying participants with MCI | ||||||
| Settings | Community and institutionalised (n = 1) Not reported (n = 2) | ||||||
| Index test | 18F‐florbetapir PET | ||||||
| Threshold prespecified at baseline | Yes (n = 3) | ||||||
| Threshold interpretation | Visual (n = 3) Quantitative (n = 1) | ||||||
| Threshold | Visual:
SUVR (Standardised Uptake Volume ratio):
| ||||||
| 18F‐florbetapir retention region | Global cortex (n = 1) | ||||||
| Reference Standard | Alzheimer’s disease dementia: NINCDS‐ADRDA (n = 1) Unclear (n = 1) Any form of dementia: DSM‐IV criteria for dementia (n = 1) | ||||||
| Target condition | Progression from MCI to Alzheimer’s disease dementia or any other forms of dementia (non‐ADD) or any form of dementia | ||||||
| Included studies | Prospectively well‐defined cohorts with any accepted definition of MCI (as above). Three studies (N = 458 participants) were included. Number of participants included in analysis: 453. | ||||||
| Quality concerns | The participant selection and reference standard QUADAS‐2 domain: unclear risk of bias. The index test domain: low risk of bias in all three included studies. The flow and timing domain: high risk of bias in the two included studies. Unclear concerns about applicability in the reference standard domain in all three included studies. | ||||||
| Limitations | Limited investigation of heterogeneity and sensitivity analysis due to insufficient number of studies. We were unable to evaluate progression from MCI to any other form of dementia (non‐ADD) due to lack of included studies. | ||||||
| Test | Studies | Cases/Participants | Sensitivity | Specificity | Consequences in a cohort of 100 | ||
| Proportion converting1 | Missed cases2 | Overdiagnosed2 | |||||
| Alzheimer's disease dementia | |||||||
| 18F‐florbetapir by visual assessment from one to less than two years of follow‐up | 1 | 61/401 | 89% (95% CI 78% to 95%) | 58% (95% CI 53% to 64%) | 15 | 2 | 36 |
| 18F‐florbetapir by quantitative assessment from one to less than two years of follow‐up | 1 | 61/401 | 87% (95% CI 76% to 94%) | 51% (95% CI 45% to 56%) | 15 | 2 | 42 |
| 18F‐florbetapir by visual assessment from two to less than four years of follow‐up | 1 | 9/47 | 67% (95% CI 30% to 93%) | 71% (95% CI 54% to 85%) | 19 | 6 | 23 |
| Any form of dementia | |||||||
| 18F‐florbetapir by visual assessment from one to less than two years of follow‐up | 1 | 3/5 | 67% (95% CI 9% to 99%) | 50% (95% CI 1% to 99%) | 60 | 20 | 20 |
| Investigation of heterogeneity and sensitivity analysis: The planned investigations were not possible due to the limited number of studies available for each analysis. | |||||||
| Conclusions:18F‐florbetapir PET scan is not an accurate test for detecting progression from MCI to Alzheimer’s disease dementia or any form of dementia. The strength of the evidence was weak because of considerable variation in study methods, unclear methodological quality due to poor reporting, and high risk of bias due to possible conflict of interest. There is a need for conducting studies using standardised 18F‐florbetapir PET scan methodology in larger populations. | |||||||
| 1. Proportion converting to ADD or any form of dementia in each included study. 2. Missed and overdiagnosed numbers were computed using the proportion converting to the target condition. | |||||||
| Test | No. of studies | No. of participants |
| 1 MCI to ADD by visual assessment from 2 to less than 4 years of follow‐up Show forest plot | 1 | 47 |
| 2 MCI to ADD by visual assessment from 1 to less than 2 years follow‐up Show forest plot | 1 | 401 |
| 3 MCI to ADD by SUVR at 1 to less than 2 years follow‐up Show forest plot | 1 | 401 |
| 4 MCI to any form of dementia Show forest plot | 1 | 5 |


