Pruebas diagnósticas no invasivas para la infección por Helicobacter pylori
Appendices
Appendix 1. Glossary
Adenomas: a non‐cancerous growth arising from the glands and has a structure similar to glands
Anaemia: a condition in which there is a deficiency of red cells or of haemoglobin in the blood, resulting in pallor and weariness
Asymptomatic: without symptoms
Atrophic gastritis: chronic inflammation of the stomach lining, leading to loss of cells lining the stomach usually and their replacement with scar tissue and cell types which line the small bowel
Dyspepsia: indigestion
Eradication: removal (of)
Flatulence: passing wind excessively
Gastrectomy: partial removal of stomach
Heterogeneity: (in this context) different results in different studies
Heterogeneity: differences in results between studies
Idiopathic thrombocytopaenia purpura: purpura (purplish spots or patches on the skin and inner lining of the mouth) resulting from bleeding due to a reduction in circulating blood platelets caused by antibodies against platelets
Isotopes: atoms of an element with different numbers of neutrons (a part of atom)
Laryngeal: related to voice‐box (throat)
Lymphoma: is a form of cancer of the lymphocytes, a type of white blood cells, which normally defend the body against harmful micro‐organisms such as bacteria, virus, and fungi
Malignancies: cancers
Meta‐analysis: combining the results of individual studies to provide a single average result
Pathogenic: causing disease
Quartile: each of four equal groups into which a population can be divided
Serology: blood tests to test the presence of antibodies (substances produced by white cells to defend the body against harmful micro‐organisms such as bacteria)
Stool antigen test: a laboratory test of stool to diagnose H plyori infection
Urea breath test: a laboratory test of breath to diagnose H pylori infection
Appendix 2. MEDLINE search strategy
1. exp Helicobacter pylori/ or Helicobacter/
2. (pylori or pyloridis).mp.
3. Helicobacter.mp.
4. HP.mp.
5. Campylobacter.mp.
6. 1 or 2 or 3 or 4 or 5
7. exp Breath Tests/
8. (breath adj3 test).mp.
9. exp Enzyme‐Linked Immunosorbent Assay/
10. (Enzyme‐Linked Immunosorbent Assay or ELISA).mp.
11. exp Blotting, Western/
12. (Western adj1 (blot or blotting or immunoblot or immunoblotting)).mp.
13. Latex Fixation Tests/
14. ("latex agglutination test" or "latex fixation test" or LAT).mp.
15. ((stool or "stool antigen" or feces or faeces or fecal or faecal) adj3 test).mp.
16. 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. 6 and 16
18. exp animals/ not humans.sh.
19. 17 not 18
Appendix 3. Embase search strategy
1. exp Helicobacter pylori/ or Helicobacter/
2. Helicobacter.mp.
3. (pylori or pyloridis or HP).mp.
4. Campylobacter.mp.
5. 1 or 2 or 3 or 4
6. urea breath test/
7. (breath adj3 test).mp.
8. enzyme linked immunosorbent assay/
9. (Enzyme‐Linked Immunosorbent Assay or ELISA).mp.
10.Western blotting/
11. (Western adj1 (blot or blotting or immunoblot or immunoblotting)).mp.
12. latex agglutination test/
13. ("latex agglutination test" or "latex fixation test" or LAT).mp.
14. exp feces analysis/
15. ((stool or "stool antigen" or feces or faeces or fecal or faecal) adj3 test).mp.
16. 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. 5 and 16
18. exp animal/ not exp human/
19. 17 not 18
Appendix 4. Science Citation Index search strategy
#1 TS=(pylori or pyloridis or Helicobacter or HP or Campylobacter)
#2 TS=("breath test" or Enzyme‐Linked Immunosorbent Assay or ELISA or "Western blot" or "Western blotting" or "Western Immunoblot" or "Western Immunoblotting" or ("latex agglutination test" or "latex fixation test" or LAT) or "stool test" or "stool antigen test" or "feces test" or "faeces test" or "fecal test" or "faecal test")
#3 #1 AND #2
Appendix 5. National Institute for Health Research ‐ Health Technology Assessment
Helicobacter pylori and accuracy
Appendix 6. Criteria for assessment of risk of bias and applicability concerns
| Domain 1: Patient selection | Patient sampling | Symptomatic people and asymptomatic people in whom H pylori infection status is sought so that eradication therapy for H pylori can be started |
| Was a consecutive or random sample of patients enrolled? | Yes: If a consecutive sample or a random sample of symptomatic people and asymptomatic people in whom H pylori infection status is sought was included in the study | |
| Was a case‐control design avoided? | Yes: If a cohort of symptomatic people and asymptomatic people in whom H pylori infection status was sought were studied | |
| Did the study avoid inappropriate exclusions? | Yes: If all symptomatic people and asymptomatic people in whom H pylori infection status was sought were included | |
| Could the selection of patients have introduced bias? | Low risk of bias: If 'yes' classification for all the above three questions; high risk of bias: if 'no' classification for any of the above three questions; unclear risk of bias: if 'unclear' classification for any of the above three questions, but without a 'no' classification for any of the above three questions | |
| Patient characteristics and setting | Yes: If all symptomatic people and asymptomatic people in whom H pylori infection status was sought were included | |
| Are there concerns that the included patients and setting do not match the review question? | Low concern: if the patient characteristics and setting were classified as 'yes'; unclear concern: if the patient characteristics and setting were classified as 'unclear'; high concern: if the patient characteristics and setting were classified as 'no' | |
| Domain 2: Index test | Index test(s) | Urea breath test, serology, and stool antigen test |
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes: If the index test was conducted and interpreted without the knowledge of the results of the reference standard | |
| If a threshold was used, was it prespecified? | Yes: if a prespecified threshold was used No: if a prespecified threshold was not used Unclear: if it was not clear whether the threshold used was prespecified | |
| Could the conduct or interpretation of the index test have introduced bias? | Low risk of bias: If 'yes' classification for both questions above; high risk of bias: if 'no' classification for any of the above two questions; unclear risk of bias: if 'unclear' classification for any of the above two questions, but without a 'no' classification for any of the above two questions | |
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern: If the criteria for a positive index test was clearly stated; high concern: if the criteria for a positive index test was not stated | |
| Domain 3: Target condition and reference standard | Target condition and reference standard(s) | Target condition: H pylori infection Reference standard: endoscopic biopsy with histology |
| Is the reference standard likely to correctly classify the target condition? | Yes: If H pylori infection was confirmed by endoscopic biopsy with special stains or immunohistochemical stains Unclear: If the reference standard was not described adequately. Such studies were excluded | |
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes: If the reference standard was interpreted without the knowledge of the results of the index test | |
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk of bias: If 'yes' classification for both questions above; high risk of bias: if 'no' classification for any of the above two questions; unclear risk of bias: if 'unclear' classification for any of the above two questions, but without a 'no' classification for any of the above two questions | |
| Are there concerns that the target condition (as defined by the reference standard) does not match the question? | Considering the inclusion criteria for this review, all the included studies were classified as 'low concern' as anticipated | |
| Domain 4: Flow and timing | Flow and timing | People with H pylori infection may have resolution of infection (usually with treatment) and people without H pylori infection may get infected with H pylori if there is a long delay between the index test and reference standard. An arbitrary two weeks were chosen as acceptable delay between the index test and reference standard |
| Was there an appropriate interval between index test and reference standard? | Yes: If the time interval between index test and reference standard was less than two weeks | |
| Did all patients receive a reference standard? | Yes: If all patients received a reference standard Therefore, all studies included in the review were classified as 'yes' for this item | |
| Did all patients receive the same reference standard? | Yes: If all the patients received the same reference standard Unclear: If this information was not clear | |
| Were all patients included in the analysis? | Yes: If all the patients were included in the analysis, irrespective of whether the results were uninterpretable | |
| Could the patient flow have introduced bias? | Low risk of bias: If 'yes' classification for all the above four questions; high risk of bias: if 'no' classification for any of the above four questions; unclear risk of bias: if 'unclear' classification for any of the above four questions, but without a 'no' classification for any of the above four questions |
Appendix 7. Characteristics of excluded studies
We excluded 1728 references (1727 studies) for the following reasons.
Case‐control study (17): Alarcón‐Rivera 2011; Benjamin 2012; Cao 2012; De Pascalis 1999; Doweck 1997; Dun 2001; Enroth 2002; Figura 1994; Gao 2015; Gerstenecker 1992; Klein 1996; Marshall 1988c; Mattar 1999; Nishizono 1998; Pantoflickova 2000; Roggero 2002; Veijola 2005b
Not a primary research study (147): Abadi 2011; Abut 2006; Adamek 1995; Adamsson 2000; Alpert 1989; Anania 2008; Anonymous 1997; Anonymous 2000; Anonymous 2002a; Anonymous 2002b; Anonymous 2004; Arents 2002; Atherton 1994; Attumi 2011; Barthel 1990; Bateson 1991; Bazzoli 1997b; Bazzoli 1998; Bazzoli 1999; Bellon 2004; Bergmann 1997; Blancas 2004; Blum 1997; Bornschein 2011; Braden 1991; Braden 1992; Braden 2001b; Braden 2007; Braden 2012; Bravos 2000; Breslin 1997; Brown 1993; Calam 1994; Calvet 2015; Canard 2003; Caspary 1995; Chey 2000b; Chiba 1999; Ching 1991b; Ciok 2003; Cirak 2007; Continibali 1991; Corti 2007; Couturier 2014; Cutler 1995b; Cutler 1997; De Argila 2001; De Boer 1995; Dewan 2000; Di Rienzo 2013; Dorta 2005; Drumm 1999; Dyrla 2015; Ebell 1998; Elbast 1999; Elitsur 2005; Falk 1997; Fallone 2000; Farkkila 1996; Ferwana 2015; Fukuda 2002; Fukuda 2003a; Fukuda 2003b; Garcia 1996; Garcia 2006; Gatta 2003a; Gisbert 2000b; Gisbert 2006a; Gisbert 2006b; Gisbert 2006h; Gold 2000; Gold 2014; Gonzalez 2004; Goto 1998; Gottrand 2001; Graham 2000; Graham 2001c; Graham 2010; Guo 2005; Guslandi 2000; Harris 1995; Harris 1998; Hart 1999; Hawtin 1999; Heenan 1989; Hirschl 2005; Ho 2000; Hong 2008; Hoshiya 2001; Hsu 2010; Imperiale 1996; Janssen 2001; Jones 1997b; Kabir 2001; Kalach 1998b; Karakus 2013; Katelaris 1997; Kato 2005b; Kato 2005c; Kato 2010; Laheij 2006; Ling 2013; Malfertheiner 2005; Mana 2000a; Mana 2001b; Megraud 1988; Miftahussurur 2016; Mion 1996; Newell 1989b; Nightingale 1996; Nishikawa 1999; Oderda 1998a; Oderda 2004; Parente 2001; Parente 2002b; Pattison 1996; Payne 2006; Perez 1998; Perri 1995; Perri 2000; Radke 1997; Raedsch 1992; Ratnaraj 2015; Rauws 1987; Rauws 1989b; Satoh 1993; Seo 2004; Seo 2013; Shiba 1998; Snyder 1999; Stirling 1995; Takagi 2002; Tamura 2001; Trevisani 2002; Vaira 1989; Vaira 2000a; Vaira 2000b; Vakil 2000b; Wadstrom 1994; Westblom 1999; Wildgrube 1995; Yakoob 2014; Yamamoto 2008; Zagari 2003; Zhang 2002; Zhelezova 2006; Zhou 2014
Erratum (3): Altindis 2002b; Altindis 2003; Ballam 2000b
Inappropriate population (79)
-
In monitoring (33): Al‐Assi 1999; Balcilar 2012; Bilardi 2002; Bommelaer 2001; Cutler 1996; Fraser 2003; Gisbert 1999c; Hirschl 1996; Houben 1998; Isomoto 2003; Kato 2000a; Kato 2003b; Kato 2005a; Koizumi 2003; Labenz 1997; Makristathis 2000; Mansour‐Ghanaei 2013; Miwa 1998a; Odaka 2002; Oderda 1998b; Osaki 2008; Ploier 1997; Quesada 2006a; Richter 2002; Rollan 1997; Sharma 1999; Shimoyama 2009b; Shimoyama 2011; Sorberg 1997; Thijs 1994; Vaira 1999b; Van't Hoff 2000; Zipser 2000
-
Not in humans (1): Foertsch 2010
-
Only in H pylori negative people (2): Hahn 2000; Urita 2006
-
Only in H pylori positive people (39): Ahmed 2005; Alam 2013; Crabtree 1990; Crabtree 1991a; Crabtree 1991b; Cremonini 2005; Janus 1991; Kopanski 1997; Kryvy 2012; Mirbagheri 2005; Parente 2000a; Parente 2000b; Parente 2002a; Park 2001; Pathak 2012; Perri 1994; Polat 2010; Ren 2010; Savarino 2000b; Shimoyama 1996; Shimoyama 2010; Shirin 2005; Sicinschi 2003a; Slomianski 1994; Slomianski 1995; Sue 1996; Thongbai 2007; Valle 1997; Van der Est 1990; Van der Wouden 1999; Van Zanten 1998; Van Zanten 1999; Van Zwet 1992; Van Zwet 1994; Veijola 2005a; Weingart 2003; Weingart 2004; Yoo 2007; Zagari 2005
-
Only in people with gastrointestinal bleeding (2): Liao 2003; Van Leerdam 2003
-
Selection of patients was based on the results of other H pylori tests (1): Falsafi 2014
-
Includes people who were being monitored for H pylori status (1): Lin 1992
Inappropriate index test (38): Aguilar‐Soto 2004; Alan 2014; Bathe 1996; Boyanova 2003; Busro 2013; Chey 1999b; Chou 1997; Datta 2005; Del Pozo Garcia 2006; Dietz 2001; Elitsur 1999b; El‐Zimaity 1998; Garces 2012; Ho 2004; Ismail 2016; Isomoto 2006; Jolley 2007; Kolts 1993; Koumi 2011; Kuo 2002; Li 1996; Loeb 1997; Niv 1998; Notarnicola 1996; Olsson 1993; Rogge 1995; Sayed 2011; Schilling 2003; Shimada 1994; Smith 2010; Smith 2012; Suto 2000a; Tokunaga 1998; Tokunaga 2000; Urita 2000; Urita 2004b; Urita 2007a
Inappropriate target condition (4): Ang 2007b; Lee 2013; Ploier 1996; Witt 1990
Inappropriate reference standards (1182): Abdulqawi 2012; Abu 2015; Abukhadir 1998; Abu‐Sbeih 2014; Aceti 1989; Adachi 2002; Adamek 1994; Adiloglu 2007; Agha‐Amiri 1999a; Agha‐Amiri 1999b; Agha‐Amiri 2001; Agudo 2009a; Agudo 2009b; Aguemon 2004; Ahuja 1998; Aje 2010; Aksoy 2003; Aktepe 2011; Alavi 1996b; Albrecht 2012; Alcalde 1994; Alemohammad 1993; Al‐Humayed 2008; Ali 1997; Ali 1998; Altindis 2002a; Amendola 2002; Anania 2007; Andersen 1998; Anderson 1993; Andrews 2003; Ang 2007a; Anonymous 1989; Antoine 1995; Antos 2005; Arboleda 2013; Archimandritis 2001; Arents 2001; Arinton 2011; Arita 1982; Arj 2012; Arora 2003; Artiko 2004; Asante 1998; Asfeldt 2004; Ashraf 1999; Atherton 1992; Attallah 2004; Aucher 1998; Auroux 1998; Aziz 2014; Bakka 2002; Ballam 1998; Ballam 2000a; Balon 1997; Baqai 2003; Barbosa 2003; Baryshnikova 2009; Baryshnikova 2012; Baryshnikova 2013; Basso 1999; Bazaz 2005; Bazzoli 1995; Bazzoli 2000; Befrits 1993; Beiki 2005; Bell 1987; Bener 2002; Benito 1999; Bergey 2003; Bermejo 2000a; Bermejo 2000b; Bermejo 2002; Bessede 2011; Best 1992; Best 1994; Bhewa 2007; Bielanski 1996a; Bielanski 1996b; Bielanski 1996c; Bielanski 1997b; Bielanski 1998; Bielanski 1999; Biemond 1997; Billaud 1996; Bjorneklett 1989; Blairon 2009; Blanco 2008; Blanco 2009; Blecker 1993b; Blecker 1993c; Blecker 1993d; Blecker 1993e; Blecker 1993f; Blecker 1994a; Blecker 1994c; Blecker 1994d; Blecker 1995a; Blecker 1995b; Bode 2000; Bode 2001; Bode 2002; Bodger 1999; Bodhidatta 1993; Bolton 1989a; Bolton 1989b; Bonamico 2004; Bongermino 2010; Booka 2005; Borody 2012; Borody 2013; Boudjella 2009; Boukthir 2005; Boyanova 2013; Braden 1993; Braden 1994a; Braden 1994b; Braden 1996; Braden 1999; Braden 2000a; Braden 2000b; Braden 2000c; Braden 2001a; Bravo 1999; Brennan 2015a; Brennan 2015b; Breslin 1998; Breslin 2000; Bretagne 1998; Briedigkeit 1992; Britto 2002; Brmbolic 1997; Bruce 2005; Bruden 2011; Bruning 2002; Brunner 1989; Buchan 2013; Buhling 2004; Burucoa 2013; Cadranel 1998; Cagdas 2012; Caglar 1999; Calvet 1999; Calvet 2002a; Calvet 2002b; Calvet 2002c; Calvet 2003; Calvet 2005; Calvet 2009; Calvet 2010a; Calvet 2010b; Calvo 2013; Camargos 2003; Camorlinga‐Ponce 1998; Campuzano‐Maya 2007; Canete 2002; Canete 2003; Cardenas 2006; Cardenas 2008; Cardinali 2003; Carrasco 1998; Caselli 1999; Casswall 1999; Castro 2004; Castro‐Fernandez 2004; Cave 1999; Chacon 1995; Chang 1999; Chang 2002; Chattopadhyay 2002; Chattopadhyay 2004; Checchi 2000; Chen 1996; Chen 1997; Chen 2000; Chen 2001a; Chen 2001b; Chen 2002a; Chen 2002b; Chen 2003; Cheng 2004; Cherian 2008; Chey 1997a; Chey 1999a; Chey 2000a; Ching 1991a; Ching 1993; Chisholm 2004; Chmiela 2003; Cho 2000; Cho 2003; Choi 2010; Choi 2011; Christie 1996; Chua 2002; Chung 2001a; Chvalova 1990; Clancy 1994; Cockburn 2001; Coelho 1990; Coelho 1997; Coelho 1999; Coelho 2003; Coelho 2009a; Coelho 2009b; Coelho 2011; Cohen 1999; Colaiocco 1999; Connor 1999; Conti‐Nibali 1990; Contreras 2006; Coombs 2001; Corvaglia 1997; Corvaglia 1999; Costa 2001; Crespo 2009; Crispino 2013; Cullen 2002; Cunningham 2010; Cutler 1993; Cutler 1995a; Cutler 1998; Cutler 1999; Da Silva 2010; Dahlberg 1998; Daino 2015; Dan 2013; Danielli 1993; Day 2002; Day 2003; De Angelis 2007; De Bustillo 1998; De Carvalho 2003; De Giacomo 1991; De Laat 2001; De Oliveira 1999; Deankanob 2006; Debongnie 1993; Deguchi 2009; Del Zompo 2014; Delaney 2003; Demiray 2006; Demiray 2012; Demiray‐Gurbuz 2012; Demirturk 2003; Desroches 1997; Dhar 1998; Dhesi 2015; Di Fulvio 2003; Di Mario 2009; Di Mario 2010; Di Silvio 1998; Dill 1989; Dill 1990; Ding 1993; Ding 2000; Dolek 2007; Dominguez 2006; Dominguezmunoz 1995; Domínguez‐Muñoz 1997; Donati 1997; Dondi 2006; Dore 2004; Douraghi 2013; Drew 1988; Drzymala‐Czy 2014; Du 2004; Duan 1994; Duggan 1998; Duggan 1999; Dulbecco 2001; Dulbecco 2003; Dumont 1989; Durdal 2002; Dy‐Limquiaco 2006; Edwards 1997; Elitsur 1997; Elitsur 2004; Elitsur 2009; Ellenrieder 1997; Elnujumi 1991; El‐Nujumi 1996; El‐Nujumi 1998; El‐Zaatari 1995; Endtz 2000; Engberg 2003; Engstrand 1992; Enroth 1997a; Enroth 1997b; Erzin 2004; Erzin 2005; Evans 1989; Everts 1996; Faigel 1996a; Faigel 1996b; Faigel 2000; Fakhrjou 2011; Falaknazi 2010; Fallone 1998; Falsafi 2005; Falsafi 2009; Fanti 2001; Fazulzyanova 2012; Fazzio 1995; Feldman 1995; Felz 1997; Ferrante 1999; Festi 1999; Feteih 2009; Feydt‐Schmidt 2002; Figura 2005; Figura 2014; Finderle 2013; Fontana 2000; Forne 2000; Fox 1989; Fraser 1996b; Frenck 2006; Fry 2005; Fujisawa 2001; Fukuda 1996; Fukuda 2005; Fukuda 2006; Fusconi 1999; Galleguillos 1998; Gallo 2001; Ganga‐Zandzou 2001; Garcia 2000; Garcia‐Diaz 2002; Garza‐Gonzalez 2003; Gatta 2003b; Gatta 2003c; Gatta 2003d; Gatta 2004a; Gatta 2004b; Gatta 2006; Gatta 2010a; Gatta 2010b; Gatta 2011; Gerards 1999; Ghasemian 2005; Ghoshal 2010; Gilger 2002; Gill 2007; Girdalidze 2013; Gisbert 1999a; Gisbert 1999b; Gisbert 2000a; Gisbert 2000c; Gisbert 2000d; Gisbert 2000e; Gisbert 2000f; Gisbert 2000g; Gisbert 2001; Gisbert 2002a; Gisbert 2002b; Gisbert 2002c; Gisbert 2002d; Gisbert 2003a; Gisbert 2003b; Gisbert 2004a; Gisbert 2006c; Gisbert 2006d; Gisbert 2006e; Gisbert 2006f; Gisbert 2006g; Gisbert 2007; Glassman 1990; Glupczynski 1992; Gobert 1989; Goel 2003; Goh 1995; Gomes 2002; Gomes 2005; Gomez 2000; Gomollon 2003; Gonzalez 2007; Gonzalez 2013; Gonzalez‐Cuevas 2001; Good 1991; Goodwin 1987; Gosciniak 1993; Gosciniak 1996; Gosciniak 2000; Gosciniak 2002; Gosciniak 2003; Goto 1995; Graham 1986; Graham 1987; Graham 1996b; Graham 2001a; Graham 2001b; Grino 2001; Grino 2003; Grossi 2000; Guell 2006; Guja 1999; Gulcan 2005; Gupta 2003; Gurbuz 2009; Gutierrez 1999; Gutierrez 2005; Hackelsberger 1998; Haggerty 2005; Hamlet 1995; Hamlet 1999; Han 2006; Hanvivatvong 2004; Hanvivatvong 2006; Harries 1992; Harrison 1998; Hartmann 2003; Hashemi 2008; Hauser 2006; Havlasova 1998; Hawthorne 1999; Hayashi 2003; Heaney 1998; Heanhean 2013; Hegedus 2002; Helvaci 1993; Henze 1988; Henze 1989; Henze 1990; Hidaka 2010; Higazy 2000; Hildebrand 1997; Hino 2004; Hirschl 1991; Hirschl 1993; Ho 1996; Hoang 2006; Hoek 1992; Hollenz 1999; Hooton 2006; Houben 1999; Hu 1995; Hu 2000; Hu 2007; Hu 2011; Huang 1993; Huang 1996; Huang 2000; Huelin 1996; Hung 2002; Hung 2010; Husson 2000; Ibrahim 2012; Ichinose 1998; Ignys 2006; Ilan 1998; Imrie 2001; Iranikhah 2013; Ishihara 2000; Ishizuka 1999; Isomoto 2002; Israeli 2003; Ito 2005; Iwanczak 2005; Jadresin 2000; Jalali 1988; Jensen 1993; Ji 1993; Jiang 2004; Jo 2008; Jo 2014; Johnston 1998; Jonaitis 2007; Jones 1997a; Jones 2007; Juhasz 2000; Juncal 1998; Kajiwara 1997; Kajiwara 1998; Kakinoki 2001; Kaklikkaya 2006; Kalach 1996; Kalach 2005; Kalach 2009; Kalem 2010; Kang 1999; Kannath 2007; Kao 1993; Kaore 2012; Kaptan 2009; Karsligil 2010; Kasho 1996; Kassa 1996; Katelaris 1998; Kato 1997; Kato 1998; Kato 1999; Kato 2000b; Kato 2000c; Kato 2001a; Kato 2001b; Kato 2001c; Kato 2002a; Kato 2002b; Kato 2002c; Kato 2002d; Kato 2002e; Kato 2003a; Kato 2004a; Kato 2004b; Kato 2004c; Kato 2007; Katsuragi 1998; Kaul 1998; Kawai 2008; Kawakami 2002; Kazemi 2011; Kearney 1999; Kearney 2002; Ken 2013; Kesli 2010; Khafri 2005; Khalifehgholi 2013; Kharchenko 2012; Khorovskaya 2003; Kias 2011; Kikuchi 1999; Kim 1996; Kim 1997; Kim 1999; Kim 2001; Kim 2002; Kim 2009; Kim 2012; Kim 2013; Kim 2014; Kindermann 2000; Kindermann 2001a; Kindermann 2001b; Kishkun 2002; Klyucharova 2013; Kobayashi 2002; Kodama 2004; Kodama 2012; Kokkola 2000; Koletzko 1995; Koletzko 2003; Kolho 2002; Kolho 2006; Kolt 1997; Kondo 2000; Konorev 2013; Konstantopoulos 2001; Konturek 1999; Kopacova 1999; Kopacova 2005; Kopanski 1996; Korkmaz 2013; Korkmaz 2015; Korzonek 1997; Kountouras 1996; Kowalski 1990; Kozaiwa 1997; Kozlov 2006; Krausse 2008; Kroser 1998; Krumbiegel 2000a; Krumbiegel 2000b; Kuang 1998; Kubota 2002; Kubota 2003; Kumbhari 2012; Kumbhari 2013; Kuo 2005; Kushch 2009; Kwon 2004; Kwon 2015; Kyrlagkitsis 2007; Labenz 1996; Ladas 2000; Ladas 2002b; Lahaie 1995; Lai 1997; Laine 1999; Langhorst 2002; Larras 2009; Lee 1999; Lee 2000a; Lee 2000b; Lee 2003; Lee 2014; Lee 2015a; Leja 2009; Lelwala 1990; Leodolter 1997; Leodolter 1998a; Leodolter 1998b; Leodolter 1999a; Leodolter 1999b; Leodolter 2000; Leodolter 2001a; Leodolter 2001b; Leodolter 2001c; Leodolter 2002; Leodolter 2003a; Leodolter 2003b; Leodolter 2004; Lepper 2004; Lerang 1998a; Lerang 1998b; Leszczynska 2009; Leung 1998a; Leung 1998b; Leung 1999; Leung 2001; Leunk 1990; Levine 2004a; Levine 2004b; Lew 1999; Lewin‐van 1999; Lewis 1997; Li 1995; Li 2004; Liao 2002; Lie 2012; Lim 2005; Lin 2004a; Lin 2004b; Lin 2004c; Lin 2015; Lindsetmo 2008; Liquornik 1998; Liston 1996; Liu 2002; Lo 2005; Locatelli 2004; Loffeld 1989; Loffeld 1993; Logan 1990; Logan 1991b; Lombardo 1999; Lopez 2001; Lopez 2004; Lopez‐Brea 1998; Lotterer 1991; Lotterer 1993a; Lotterer 1993b; Lozniewski 1996; Lu 2005; Lu 2006; Lucio 1999; Luzza 1995; Luzza 1997; Luzza 2000; Ma 2006; Maaroos 2004; Machado 2004; Machado 2006; MacKay 2003; Madico 1995; Mahmood 2010; Maity 2014; Makristathis 1998; Malaty 1996; Malaty 2000; Malaty 2002; Malfertheiner 1988; Malfertheiner 2002; Mana 2000b; Mana 2005; Manes 2000; Manes 2001; Manes 2005; Marchildon 1996; Marchildon 1999; Marchildon 2003; Marshall 1988a; Marshall 1988b; Marshall 1991; Marusic 2006; Masoero 2000; Matougui 2007; Matsuda 2003a; Matsuda 2003b; Matsukura 1995; Matsukura 2004; Matsuo 2000; Mattar 2014; Mauro 2006a; Mauro 2006b; McColl 2003; McNamara 1999; McNulty 1999; Mediero 2007; Megraud 2000; Megraud 2005; Mehrazma 2014; Meijer 1997; Mendall 1992; Menegatti 1997a; Menegatti 1997b; Metz 1998; Metz 2000; Midolo 1995; Minoli 1998; Mion 1997a; Mion 1997b; Mion 2001; Miwa 1997; Miwa 1998b; Miwa 1999; Miwa 2000; Miwa 2001; Mizukami 1994; Moayyedi 1997; Mock 1999; Mohammadi 2008; Moncayo 2006; Monteiro 2001b; Morales 2002; Moshkowitz 1993; Motta 2009; Moulton‐Barrett 1993; Mowat 1997; Mowat 1998; Mrevlje 2012; Muhsen 2006; Muñoz 1998; Muñoz 1999; Munster 1993; Murakami 2003; Murakami 2011; Murata 2002; Murphy 2015; Myllyniemi 2007; Myllyniemi 2008; Nagahara 2003; Nair 1995; Nakata 1995; Nakata 2004; Nakayama 2004; Navarro 1992; Negayama 1992; Negrini 1992; Newell 1988; Newell 1991; Ng 2002; Ng 2013; Nguyen 2008a; Nguyen 2008b; Nguyen 2010; Nguyen 2013; Ni 2000; Nijevitch 2001; Nilius 2001; Nishikawa 1996; Nishikawa 2000; Noguchi 2007; Nugalieva 2006; Nurgalieva 2003; Nurgalieva 2008; Nysaeter 1992; Obata 2003; Obradovic 2001; Oderda 1989; Oderda 1999; Oderda 2000; Ogunc 2003; Ohara 1995; Ohara 1996; Ohara 1997; Ohara 1998a; Ohara 1998b; Ohara 2004; Ohkura 1998; Ohkura 2000; Oksanen 1997; Oksanen 1998; Oksanen 2001; Okuda 2002; Okuda 2004; Okuda 2005; Okuda 2010; Okuda 2013; Okuda 2014; Olafsson 2012; Oleastro 2000; Oleastro 2002; Oliaro 2000; Omorogbe 2015; Ong 1993; Opekun 2002; Opekun 2006; Ormand 1990; Ortiz‐Olvera 2007; Osman 2014; Osoba 2004; Ou 2013; Ozdemir 2008; Ozturk 2009; Pacheco 2001; Pacheco 2013; Paimela 2006; Palka 2010; Pandya 2014; Pantoflickova 1999; Pantoflickova 2003; Paoluzi 2001; Parejo 1998; Park 2006; Park 2009; Park 2015; Parolova 2012; Patel 1994; Pathak 1992; Pathak 1994; Pathak 2008; Pathak 2011; Pathak 2013; Pathak 2014; Pattison 1997; Pavlitou 1998; Pavlitou 2000; Pawar 2014; Peitz 2000; Peitz 2003; Peitz 2004; Pena 1989; Peng 2000a; Peng 2000b; Peng 2001a; Peng 2001b; Peng 2002; Peng 2003; Peng 2005; Peng 2009; Perets 2014; Perets 2015; Perez 1996; Perezperez 1994; Perna 2002; Perna 2005; Perri 1997a; Perri 1997b; Perri 1998a; Perri 1998b; Perri 1998c; Perri 2002a; Perri 2002c; Perri 2005; Petrovic 2011; Pettersson 2001; Pianko 1999; Pilotto 1999; Pilotto 2000a; Pilotto 2000b; Pilotto 2002; Plebani 1999; Ploier 1995; Pons 2014; Porter 2009a; Porter 2009b; Portorreal 2002; Posteraro 2006; Pourakbari 2011a; Pourakbari 2011b; Pourakbari 2013; Prabakaran 1997; Prell 2009; Prieto 1994; Pronovost 1994; Przyklenk 1990; Pu 2005; Puolakkainen 1997; Puz 2006; Puz 2008; Qibi 2008; Quach 2014; Queiroz 1999; Queiroz 2000; Queiroz 2013; Queralt 2005; Quesada 2006b; Rabbe 1988; Rae 1995; Raguza 2005; Raguza 2010; Rahman 2008; Raju 1994; Ramírez‐Lázaro 2011; Ramírez‐Lázaro 2015; Rao 2001; Rauws 1989a; Rauws 1989c; Raymond 1999; Raymond 2000; Razaghi 2010; Rechcinski 1997; Redéen 2011; Rehnberg 2001; Reilly 1997; Ren 2005; Reynders 2012; Riaz 2011; Riepl 2000; Ritchie 2009; Rocha 1998; Rocha 2002; Rocha 2004; Roma‐Giannikou 2010; Romaozinho 2011; Roth 2001; Rothenbacher 2000a; Rothenbacher 2000b; Rowland 1997a; Rowland 1997b; Sabbi 2005; Sadowski 1998; Saez 2012; Saffari 2003; Salama 1993; Salles‐Montaudon 2001; Salomaa‐Rasanen 2004; Saltik 2001; Saltik 2003; Sanches 2013; Saneian 2013; Sano 2004; Santogade 1990; Sarker 2003; Sastry 1997; Sato 2012; Savarino 1999; Savarino 2000a; Savarino 2001; Savio 1999; Sawada 2001; Scherbakov 2001; Schmitt 1996; Schuman 1995; Schumann 2006; Schwarzer 2007; Sedlackova 1992; Sen 2005; Sen 2011; Serrano 2008; Sfarti 2009; Shaikh 2005; Sharma 1995; Sharma 1997; She 2009; Sheikhian 2007; Shepherd 2000; Sheu 1997; Sheu 1999a; Sheu 1999b; Sheu 2000a; Sheu 2000b; Sheu 2000c; Sheu 2002; Shimizu 2003a; Shimizu 2003b; Shimoyama 2009a; Shimoyama 2015; Shirin 2001; Shirin 2003; Shukla 2012; Sicinschi 2003b; Siddiqui 2010; Silva 2009; Sito 1994; Slade 1999; Slater 2004; Smith 2006; Sobala 1991; Sokucu 2002; Song 2000; Song 2014; Sonmezoglu 2005; Steen 1995; Stege 2010; Sternberg 1997; Stojkovic 2011; Stone 1997; Storskrubb 2005; Stray‐Pedersen 2007; Stuppy 2010; Stuppy 2011; Sudraba 2010; Sudraba 2011; Sugiyama 1991; Sujatha 2013; Sukhanov 2011; Sumona 2009; Sunnerstam 1999; Surveyor 1988; Suto 1997a; Suto 1997b; Suto 1999; Suto 2000b; Suzuki 2010; Syam 2005; Sykora 2002; Sykora 2003; Taha 1992; Taha 1993; Takagi 1993; Takagi 2003; Takahashi 2010; Talebkhan 2009; Talebkhan 2010; Talley 1991; Talley 1992; Talley 1998; Tanahashi 1998; Tanaka 2001; Tanaka 2003; Tanaka 2004; Tanaka 2005; Tanigawa 1996; Taniguchi 1995; Teich 1997; Temelli 2011; Teo 1997; Tepes 2015; Tereshchenko 2014; Tewari 2001; Tham 1993; Tham 1994; Thijs 1995a; Thijs 1995b; Thijs 1996; Thillainayagam 1991; Thomas 1990; Thomas 1999; Tindberg 2001; Tinnert 1998; Tiryaki 2010; Togashi 2006; Tokunaga 2005; Toporowska‐Kowalska 2005; Torres 2001; Toyama 1999; Trautmann 1994; Treiber 2000; Trevisani 1998; Trevisani 1999a; Trevisani 1999b; Tseng 2005; Tu 1999; Tucci 1996; Tummala 2007; Uchida 2011; Ueda 2014; Uematsu 2002; Urita 2002; Urita 2004a; Urita 2004c; Us 2002; Uyub 1994; Vafaeimanesh 2014; Vaira 1996; Vaira 1999a; Vaira 1999c; Vaira 2000c; Vaira 2002; Vaira 2009; Vaira 2010a; Vaira 2010b; Vakil 1999; Vakil 2000a; Valdeperez 2003; Valentine 1991; Valle 2013; Van de Wouw 1995; Van de Wouw 1996; Van de Wouw 1997; Van Den 1991; Van Der Ende 1999; Van Der Hulst 1999; Van der Hulst 1999; Van der Voort 1998; Van der Voort 1999; Van Doorn 2001; Van Leerdam 2002; Vannella 2009; Vargas 2013; Vaz Coelho 2005; Vecsei 2010; Veenendaal 1995; Veijola 2008; Velayos 2012; Veldhuyzen 1990; Veldhuyzen 1991; Vincent 1999; Vinette 2004; Vivas 1993; Von Wulffen 1988b; Von Wulffen 1993; Vyas 1994; Wallace 2006; Wang 1998; Wang 2000; Wang 2001; Wang 2002; Wang 2003; Wang 2015a; Wang 2015b; Watanabe 2001; Watanabe 2013; Weijnen 2001a; Weijnen 2001b; Westblom 1992; Wilcox 1996; Wildner‐Christensen 2002; Wilson 2008; Winiarski 2003b; Winiarski 2003a; Wirtheim 2001; Wisniewska 2002a; Wisniewska 2002b; Wisniewska 2006; Wong 1999; Wong 2000a; Wong 2000b; Wong 2000c; Wong 2001a; Wong 2001b; Wong 2003a; Wong 2003b; Wong 2003c; Wu 1992; Wu 2001a; Wu 2001b; Wu 2003; Wu 2004; Wu 2006a; Wu 2006b; Xia 2000a; Xia 2000b; Xia 2002; Xiao 1991; Yachi 1991; Yakoob 2008; Yamakawa 1993; Yamamoto 1995; Yamamoto 1996; Yamamoto 2000; Yamamoto 2003; Yamamoto 2005; Yamaoka 1998; Yamasaki 2004; Yamashiro 1995; Yan 2010; Yanez 2000; Yang 2005; Yang 2007; Yang 2008a; Yang 2008b; Yang 2015; Yasuda 2009; Ye 2005; Yee 2002; Yilmaz 2006; Yin 2015; Yokota 1990; Yong 2006; Yoshida 1993; Yoshida 2000; Young 1995; Young 1996; Zagari 1998; Zagari 2012; Zalabska 2010; Zambon 2004; Zanetti 2002; Zaremba 1995; Zawadzka‐Gralec 2009; Zhang 1990; Zhang 2007; Zheng 2004; Zhou 1996; Zhu 2002a; Zhu 2002b; Zhukhovitskii 2005; Zubillaga 1997; Zubillaga 1999
Lack of data (256)
-
Insufficient diagnostic test accuracy data (25): Allerberger 1996; Baryshnikova 2014; Bilal 2007; Capurso 2006; Casellas 1999; Chehter 2013; Cinar 2004; De Arruda 2001; Faigel 2001; Folwaczny 1999; Formichella 2012; Goettner 2012; Gonzalez 2003; Groves 1997; Herold 2002; Hilker 1994; Hirschl 1990; Konorev 2014; Mendoza 2006; Neri 1999; Neumann 2010; Neumann 2011; Neumann 2012; Reshetnikov 2007; Urita 2007b
-
No diagnostic accuracy data (42): Abdullah 1997a; Alem 2002; Bazzoli 1994; Bazzoli 1996; Bojko 1997; Brandi 2006; Brennan 1991; Cacoullis 1991; Cai 2010; Caporali 2003; Cevrioglu 2004; Chang 2000; Chiang 2010; Chong 1995; Cremonini 2000; Czkwianianc 1997; Dowlatshahi 2002; Elitsur 2000; Garza‐Gonzalez 2002; Gisbert 1996; Gisbert 2005; Gong 2010; He 1997; Hegedus 2001a; Hegedus 2001b; Herbrink 1988; Iijima 1998; Ilga 2008; Inaba 2002; Jabbari 2009; Jung 2002; Matthews 2000; Matthews 2005; Mitchell 1988; Naruki 1996; Nishi 1998; Oak 2011; Rapoport 2014; Rasheed 2014; Rejchrt 2004; Schaefer 1999; Smith 2009
-
Not a diagnostic test accuracy study of non‐invasive H pylori diagnosis (188): Abdullah 1997b; Adamczyk 2013; Adiloglu 2003; Aguemon 2005; Alavi 1996a; Andersen 1989; Anonymous 1996; Antico 2010; Anwar 2012; Asaka 1988; Asaki 1996; Aulia 2009; Baranskaia 2006; Basinska 2005; Bassler 1992; Bateson 2001; Bauernfeind 1989; Bazzoli 1997a; Bekmen 2008; Bell 1991; Bennedsen 1998; Bennett 2006; Berger 2002; Berker 2003; Berning 2009; Bertschinger 1992; Besherdas 2000; Bielanski 1997a; Bielanski 2000; Bindayna 2006; Birkenfeld 2004; Blashenkov 2013; Bleau 1998; Blecker 1992a; Blecker 1992b; Blecker 1993a; Blecker 1993g; Blecker 1994b; Bode 1998; Bohn 1994; Bolton 1997; Bordin 2013; Braden 1997; Buchvald 1993; Bures 2000; Butler 2000; Buyukbaba‐Boral 2005; Buzas 2001; Buzas 2008; Chalkias 2011; Chang 2003; Chang 2012; Chang 2013; Chen 1994; Chen 2009a; Chen 2009b; Chey 1997b; Cho 2008; Chong 1994; Christensen 1992; Chung 2001b; Churchill 1998; Clayton 1992; Collins 1992; Con 2007; Cooreman 1990; Cullen 1992; Czinn 1991; Datta 2003; Dediste 2003; Demir 2001; Devenish 2005; Djurasinovic 2014; Dmitrienko 2009; Dmitrienko 2011; Donati 2000; Dong 2015; Dore 1997; Dore 2003; Dou 2008; Ebara 2000; Elitsur 1999a; Faulde 1991; Fayaz 2014; Fayed 2008; Floch 2012; Fowora 2012; Fradkin 1997; Franceschi 1999; Fraser 1996a; Fraser 1997; Fraser 1998; Fruehauf 2003; Fukuda 2007; Fukuda 2009; Fusconi 1997; Gangaidzo 1995; Geletneky 1996; Gemignani 2013; Gene 2000; Ghosh 2014; Gisbert 1997; Gobert 1988; Goji 2015; Gomez 2011; Gomez‐Camarasa 2014; Gong 2014; Gonzalez 2012; Gotoh 1997; Grossi 2012; Grotowski 1998; Groves 2002; Guducuoglu 2010; Gunay 2009; Guven 2011; Harde 2008; Harde 2010; Hartman 1992; Hassan 2013; Huijsdens 2004; Hynes 1998; Hynes 2000; Ierardi 2002; Ierfone 2003; Ito 2002; Jaff 2011; Jafri 2010; Jaime 2013; Jain 1999; Jane 1999; Janjetic 2010; Janjetic 2011; Janjetic 2015; Janulaityte 1998; Jarbol 2006; Johansen 2004; Jung 2013; Kessenich 2012; Kist 1999; Klein 1999; Koca 2005; Kokkola 1998; Kopanski 1993a; Kopanski 1993b; Kopanski 2002; Kubo 2001; Lamarque 1996; Lassnig 1988; Lemus 2004; Leodolter 2005; Mahony 1988; Marshall 1999; Massarrat 2012; McColl 1997; Meltzer 2013; Miehlke 1996; Murugesan 2011; Nakagawa 1995; Newell 1989a; Nguyen 2012; Niv 2000; Niv 2003; O'Connor 2010; Perez‐Perez 1997; Perri 2002b; Perrone 2005; Potashov 1996; Presecki 1997; Salih 2013; Sharma 2015; Shimoyama 2014; Shmuely 2007; Shuber 2002; Smith 2011; Stermer 1997; Taylor 1987; Tormo 2013; Van Bohemen 1988; Van Bohemen 1989; Vesna 2005; Von Wulffen 1988a; Von Wulffen 1989; Vorobjova 1991; Werdmuller 1998; Xie 2008a; Xie 2008b; Zhang 2006; Zhou 2000
-
Incorrect data (correct information could not be obtained) (1): Hilker 1996
Appendix 8. Risk of bias and applicability concerns summary for each study included for urea breath test‐13C, urea breath test‐14C, serology and the stool antigen test
Figure 12; Figure 13; Figure 14; Figure 15

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for urea breath test‐13C

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for urea breath test‐14C.
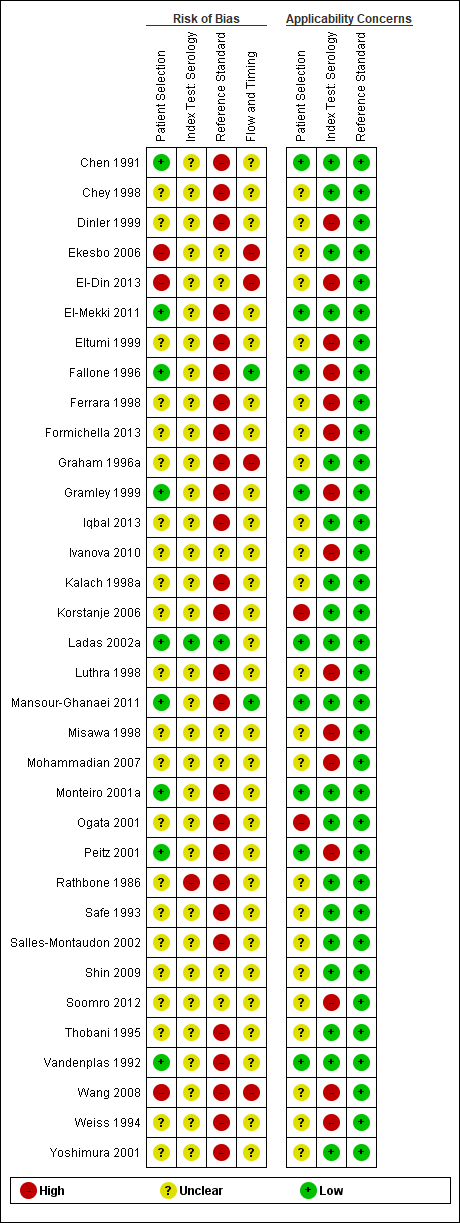
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for serology
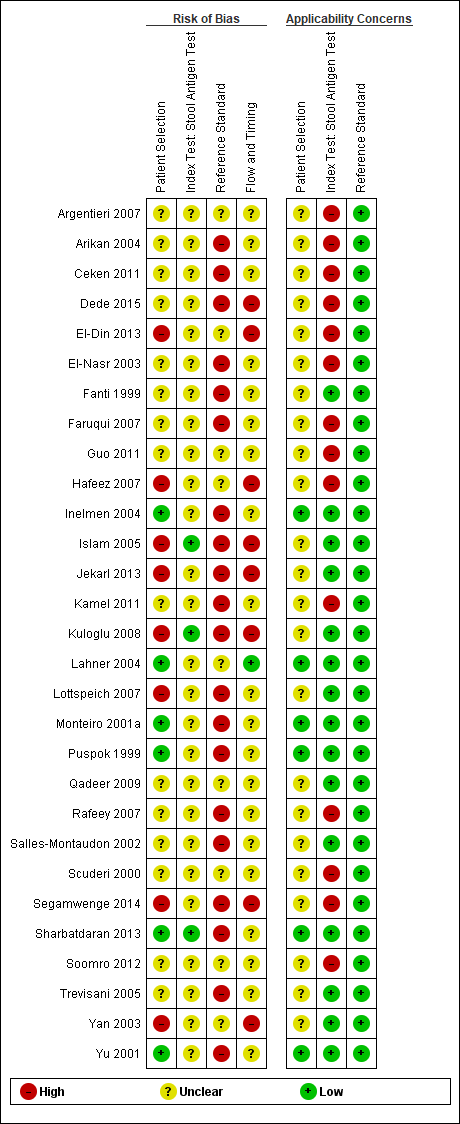
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for the stool antigen test
Appendix 9. Individual study results of test accuracy at other thresholds (grouped by test)
| Study name | Threshold | TP | FP | FN | TN | Sensitivity (95% CI) | Specificity (95% CI) |
| Urea breath test‐13C | |||||||
| DOB > 2.0% (30 minutes) | 12 | 5 | 0 | 62 | 1.00 [0.74, 1.00] | 0.93 [0.83, 0.98] | |
| DOB > 2.5% (30 minutes) | 12 | 2 | 0 | 65 | 1.00 [0.74, 1.00] | 0.97 [0.90, 1.00] | |
| DOB > 3.5% (30 minutes) | 12 | 0 | 0 | 67 | 1.00 [0.74, 1.00] | 1.00 [0.95, 1.00] | |
| DOB > 4.0% (30 minutes) | 12 | 0 | 0 | 67 | 1.00 [0.74, 1.00] | 1.00 [0.95, 1.00] | |
| DOB > 4.5% (30 minutes) | 12 | 0 | 0 | 67 | 1.00 [0.74, 1.00] | 1.00 [0.95, 1.00] | |
| DOB > 5.0% (30 minutes) | 41 | 7 | 13 | 61 | 0.76 [0.62, 0.87] | 0.90 [0.80, 0.96] | |
| DOB > 3.0% (10 minutes) | 84 | 9 | 0 | 89 | 1.00 [0.96, 1.00] | 0.91 [0.83, 0.96] | |
| DOB > 3.0% (20 minutes) | 84 | 7 | 0 | 91 | 1.00 [0.96, 1.00] | 0.93 [0.86, 0.97] | |
| DOB > 3.5% (10 minutes) | 84 | 7 | 0 | 91 | 1.00 [0.96, 1.00] | 0.93 [0.86, 0.97] | |
| DOB > 3.5% (20 minutes) | 84 | 5 | 0 | 93 | 1.00 [0.96, 1.00] | 0.95 [0.88, 0.98] | |
| DOB > 3.5% (30 minutes) | 84 | 5 | 0 | 93 | 1.00 [0.96, 1.00] | 0.95 [0.88, 0.98] | |
| DOB > 4.0% (10 minutes) | 84 | 5 | 0 | 93 | 1.00 [0.96, 1.00] | 0.95 [0.88, 0.98] | |
| DOB > 4.0% (20 minutes) | 84 | 4 | 0 | 94 | 1.00 [0.96, 1.00] | 0.96 [0.90, 0.99] | |
| DOB > 4.0% (30 minutes) | 83 | 4 | 1 | 94 | 0.99 [0.94, 1.00] | 0.96 [0.90, 0.99] | |
| DOB > 4.5% (10 minutes) | 84 | 5 | 0 | 93 | 1.00 [0.96, 1.00] | 0.95 [0.88, 0.98] | |
| DOB > 4.5% (20 minutes) | 84 | 4 | 0 | 94 | 1.00 [0.96, 1.00] | 0.96 [0.90, 0.99] | |
| DOB > 4.5% (30 minutes) | 81 | 4 | 3 | 94 | 0.96 [0.90, 0.99] | 0.96 [0.90, 0.99] | |
| DOB > 5.0% (10 minutes) | 84 | 5 | 0 | 93 | 1.00 [0.96, 1.00] | 0.95 [0.88, 0.98] | |
| DOB > 5.0% (20 minutes) | 84 | 3 | 0 | 95 | 1.00 [0.96, 1.00] | 0.97 [0.91, 0.99] | |
| DOB > 5.0% (30 minutes) | 81 | 4 | 3 | 94 | 0.96 [0.90, 0.99] | 0.96 [0.90, 0.99] | |
| Urea breath test‐14C | |||||||
| CPM > 23 (10 minutes) | 6 | 3 | 1 | 20 | 0.86 [0.42, 1.00] | 0.87 [0.66, 0.97] | |
| CPM > 29 (30 minutes) | 5 | 0 | 2 | 23 | 0.71 [0.29, 0.96] | 1.00 [0.85, 1.00] | |
| CPM > 35 (20 minutes) | 6 | 0 | 1 | 23 | 0.86 [0.42, 1.00] | 1.00 [0.85, 1.00] | |
| CPM > 50 (20 minutes) | 4 | 0 | 3 | 23 | 0.57 [0.18, 0.90] | 1.00 [0.85, 1.00] | |
| CPM > 50 (30 minutes) | 5 | 0 | 2 | 23 | 0.71 [0.29, 0.96] | 1.00 [0.85, 1.00] | |
| Not stated | 64 | 5 | 10 | 25 | 0.86 [0.77, 0.93] | 0.83 [0.65, 0.94] | |
| > 1% excretion (20 minutes) | 19 | 2 | 3 | 14 | 0.86 [0.65, 0.97] | 0.88 [0.62, 0.98] | |
| > 1% excretion (30 minutes) | 15 | 1 | 7 | 15 | 0.68 [0.45, 0.86] | 0.94 [0.70, 1.00] | |
| > 4.7% excretion (10 minutes) | 55 | 2 | 6 | 13 | 0.90 [0.80, 0.96] | 0.87 [0.60, 0.98] | |
| > 4.7% excretion (20 minutes) | 50 | 2 | 11 | 13 | 0.82 [0.70, 0.91] | 0.87 [0.60, 0.98] | |
| > 4.7% excretion (25 minutes) | 52 | 2 | 9 | 13 | 0.85 [0.74, 0.93] | 0.87 [0.60, 0.98] | |
| > 4.7% excretion (5 minutes) | 59 | 3 | 2 | 12 | 0.97 [0.89, 1.00] | 0.80 [0.52, 0.96] | |
| DPM > 100 (10 minutes) | 48 | 5 | 0 | 20 | 1.00 [0.93, 1.00] | 0.80 [0.59, 0.93] | |
| Urea breath test ‐ unknown isotope | |||||||
| Not stated | 33 | 2 | 10 | 54 | 0.77 [0.61, 0.88] | 0.96 [0.88, 1.00] | |
| DOB > 4 per ml (at 5 minute intervals up to 30 minutes) | 10 | 8 | 2 | 8 | 0.83 [0.52, 0.98] | 0.50 [0.25, 0.75] | |
| Serology | |||||||
| Not stated | 128 | 33 | 3 | 123 | 0.98 [0.93, 1.00] | 0.84 [0.77, 0.89] | |
| Two red lines | 115 | 23 | 16 | 133 | 0.88 [0.81, 0.93] | 0.85 [0.79, 0.90] | |
| Not stated | 181 | 13 | 29 | 277 | 0.86 [0.81, 0.91] | 0.96 [0.92, 0.98] | |
| Not stated | 179 | 6 | 31 | 284 | 0.85 [0.80, 0.90] | 0.98 [0.96, 0.99] | |
| ≥44 units | 89 | 10 | 8 | 23 | 0.92 [0.84, 0.96] | 0.70 [0.51, 0.84] | |
| Not stated | 62 | 7 | 22 | 23 | 0.74 [0.63, 0.83] | 0.77 [0.58, 0.90] | |
| Not stated | 44 | 5 | 2 | 53 | 0.96 [0.85, 0.99] | 0.91 [0.81, 0.97] | |
| Not stated | 47 | 1 | 3 | 44 | 0.94 [0.83, 0.99] | 0.98 [0.88, 1.00] | |
| Stool antigen test | |||||||
| Pink red band (5 minutes) | 50 | 4 | 9 | 41 | 0.85 [0.73, 0.93] | 0.91 [0.79, 0.98] | |
| Visual assessment by gastroenterologists | 15 | 4 | 1 | 12 | 0.94 [0.70, 1.00] | 0.75 [0.48, 0.93] | |
| CI = confidence interval; CPM = counts per minute; DOB = delta over baseline; DPM = disintegrations per minute; FN = false negative, FP = false positive; TN = true negative; TP = true positive. For thresholds for urea breath tests, the number of minutes in brackets is the time after administration of urea. | |||||||
Appendix 10. Availability of data on potential sources of heterogeneity
| Characteristic | Test | |||
| Urea breath test C‐13 | Urea breath test C‐14 | Serology | Stool antigen test | |
| Number of studies (H pylori cases/total) | 34 (1526/3139) | 21 (1018/1810) | 34 (2477/4242) | 29 (1311/2988) |
| Reference standard | ||||
| Haemotoxylin and eosin stain | 10 | 7 | 8 | 8 |
| Special histological stains | 7 | 5 | 6 | 9 |
| Immunohistochemical stain | 0 | 0 | 2 | 0 |
| Combination | 17 | 9 | 18 | 12 |
| Participant type | ||||
| Symptomatic | 19 | 13 | 20 | 17 |
| Asymptomatic | 0 | 0 | 1 | 0 |
| Both | 0 | 1 | 1 | 0 |
| Not stated | 15 | 7 | 12 | 12 |
| Recent, current proton pump inhibitor or antibiotic use | ||||
| Yes | 0 | 0 | 0 | 0 |
| No | 18 | 13 | 17 | 19 |
| Both | 2 | 0 | 1 | 2 |
| Not stated | 14 | 8 | 16 | 8 |
| Recruitment type | ||||
| Prospective | 6 | 3 | 3 | 4 |
| Retrospective | 4 | 0 | 2 | 0 |
| Not stated | 24 | 18 | 29 | 25 |
| Publication type | ||||
| Full text | 32 | 21 | 31 | 29 |
| Abstract | 2 | 0 | 3 | 0 |
| Subtype of tests* | ||||
| Serology subtypes | ||||
| ELISA | ‐ | ‐ | 17 | ‐ |
| Latex agglutination test | ‐ | ‐ | 1 | ‐ |
| Western blot | ‐ | ‐ | 3 | ‐ |
| Not stated | ‐ | ‐ | 17 | ‐ |
| Stool antigen subtypes | ||||
| Monoclonal antibody | ‐ | ‐ | ‐ | 2 |
| Polyclonal antibody | ‐ | ‐ | ‐ | 3 |
| Not stated | ‐ | ‐ | ‐ | 24 |
| Risk of bias† | ||||
| Low | 0 | 0 | 0 | 0 |
| High | 32 | 18 | 32 | 27 |
| Unclear | 2 | 3 | 2 | 2 |
*The same study can feature in more than one category depending upon the number of tests included in the study.
†Studies at low risk of bias in all the QUADAS‐2 domains versus those at unclear or high risk of bias.
Appendix 11. Investigation of effect of reference standard on test accuracy
| Test | Special stain | Haemotoxylin and eosin stain | P value* | ||
| Studies; participants (H pylori cases) | DOR (95% CI) | Studies; participants (cases) | DOR (95% CI) | ||
| Urea breath test‐13C | 7; 496 (216) | 59.5 (13.4, 265) | 10; 1154 (623) | 229 (62.3, 842) | 0.30 |
| Urea breath test‐14C | 5; 558 (324) | 123 (33.7, 446) | 7; 428 (269) | 33.1 (10.6, 103) | 0.10 |
| Serology | 6; 1112 (777) | 14.4 (2.98, 69.6) | 8; 813 (464) | 33.5 (7.86, 143) | 0.22 |
| Stool antigen test | 9; 1124 (476) | 33.2 (9.94, 111) | 8; 626 (310) | 33.0 (9.19, 118) | 1.0 |
*P value from likelihood ratio test comparing models with and without the reference standard covariate.
DOR = diagnostic odds ratio.

Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies. For each domain, the numbers shown on the bar represent the number of studies that were scored as high, unclear or low in terms of risk of bias or applicability concern.
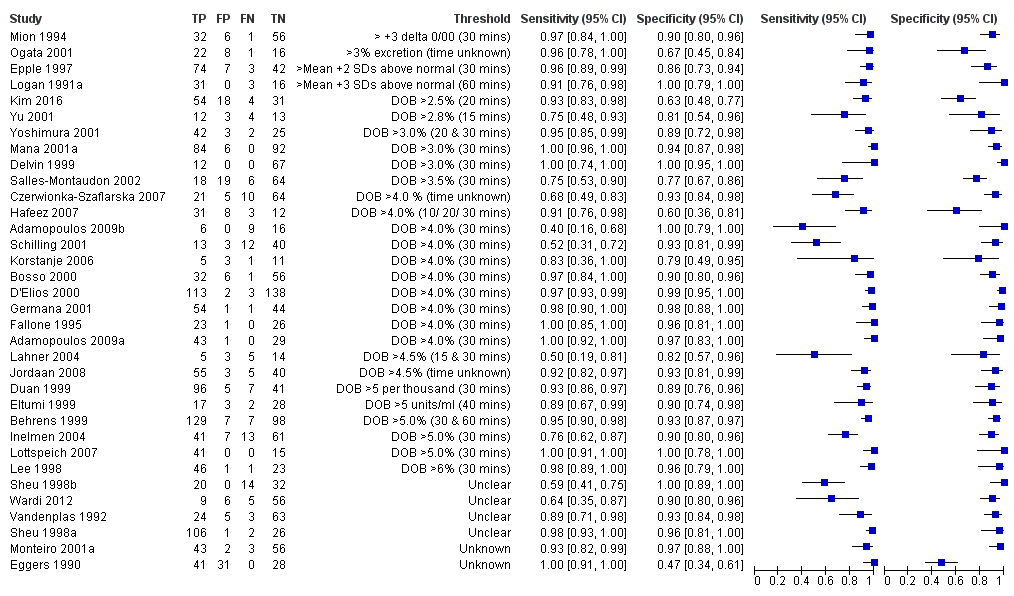
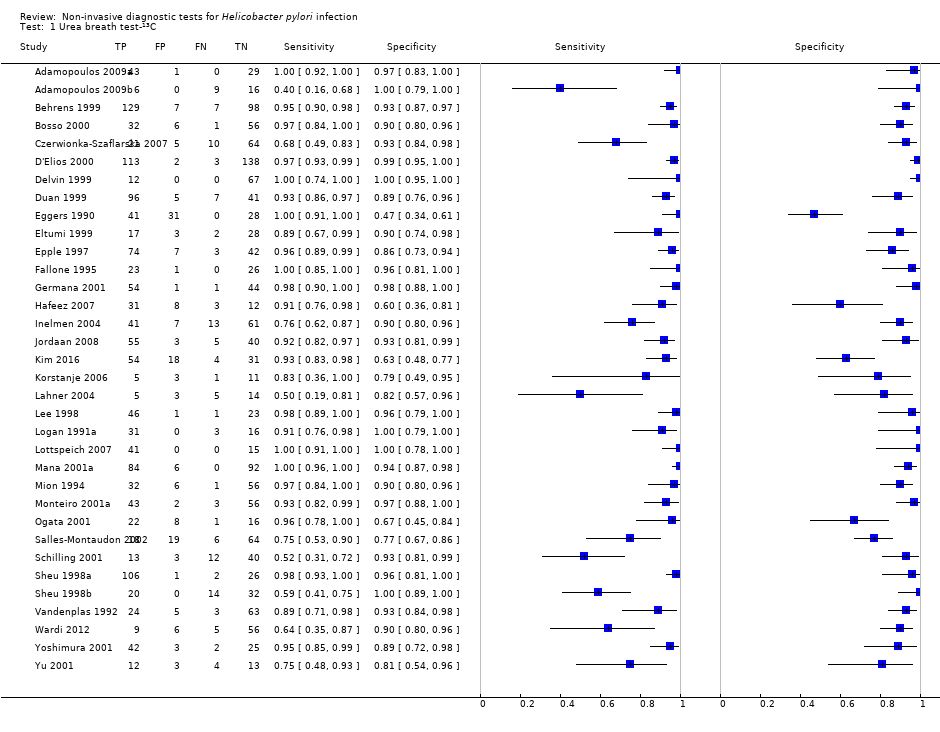
Forest plot of urea breath test‐13C.FN = false negative; FP = false positive; TN = true negative; TP = true positive. The forest plot shows an estimate of sensitivity and specificity from each study and the threshold used. Studies are sorted by threshold, sensitivity and specificity. For threshold, the number of minutes in brackets is the time after administration of urea.

Forest plot of urea breath test‐13C at commonly reported thresholds. FN = false negative; FP = false positive; TN = true negative; TP = true positive. Thresholds are shown in brackets and the number of minutes in brackets is the time after administration of urea.

Forest plot of urea breath test‐14C. FN = false negative; FP = false positive; TN = true negative; TP = true positive. The forest plot shows an estimate of sensitivity and specificity from each study and the threshold used. Studies are sorted by threshold, sensitivity and specificity. For threshold, the number of minutes in brackets is the time after administration of urea.

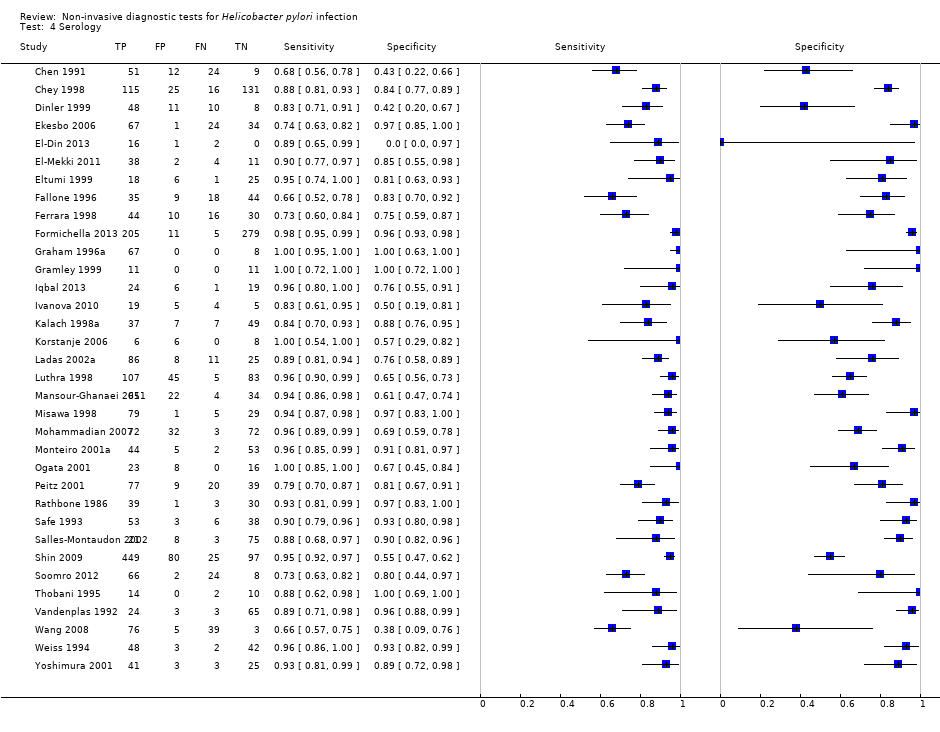
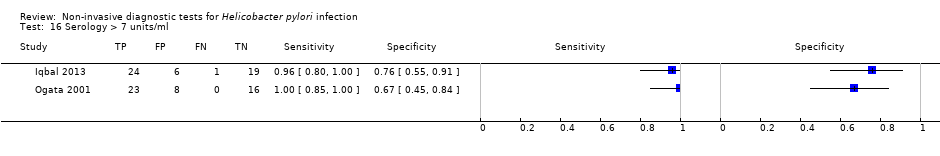
Forest plot of serology. FN = false negative; FP = false positive; SD = standard deviation; TN = true negative; TP = true positive. The forest plot shows an estimate of sensitivity and specificity from each study and the threshold used. Studies are sorted by threshold, sensitivity and specificity. Other threshold is staining of a 120kDa protein (CagA) gel band and/or at least two of five proteins between 28–33 kDa.
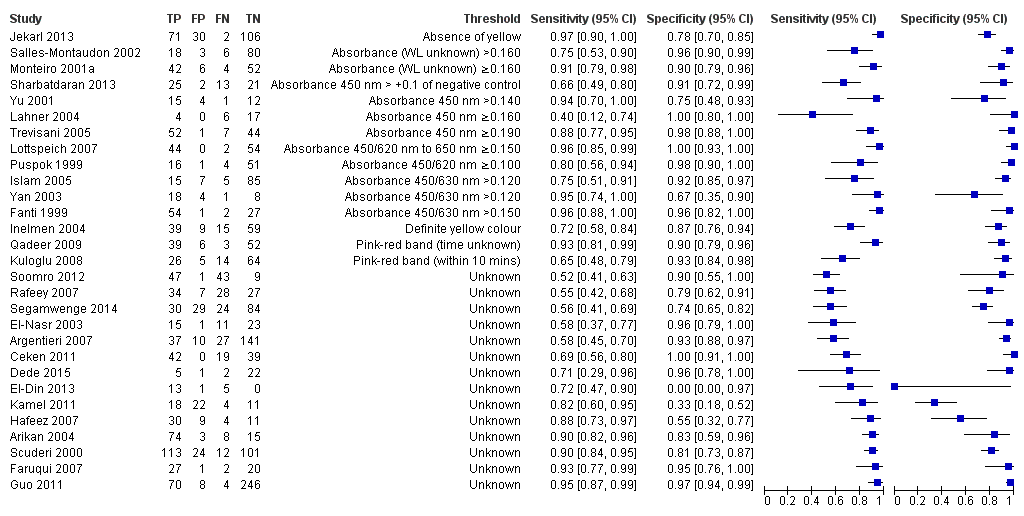
Forest plot of stool antigen test. FN = false negative; FP = false positive; TN = true negative; TP = true positive; WL = wavelength. The forest plot shows an estimate of sensitivity and specificity from each study and the threshold used. Studies are sorted by threshold, sensitivity and specificity.
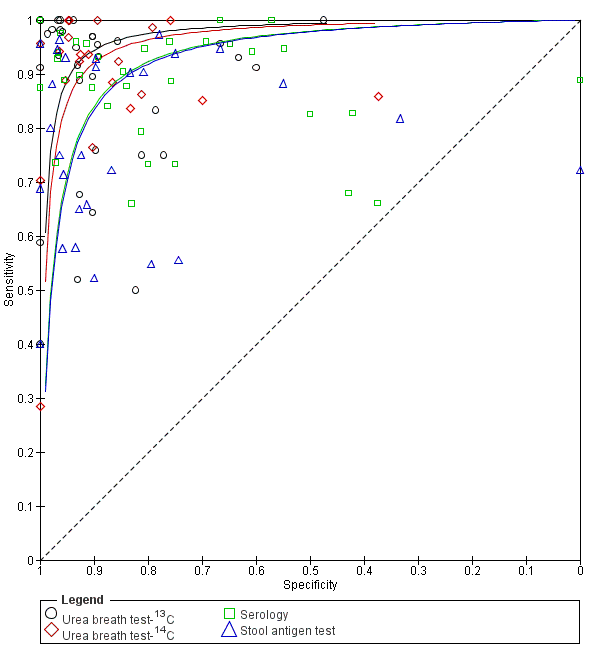
Summary ROC plot of non‐invasive tests for H pylori infection. The SROC curves for the four tests are parallel. The curve for each test is drawn within the range of estimates of specificity from the studies included for the test.

Summary ROC plot of direct comparisons of urea breath test‐13C and serology. Each summary curve was drawn restricted to the range of specificities for each test. The size of each symbol was scaled according to the precision of sensitivity and specificity in the study. A dotted line joins the pair of points for the two tests from each study.
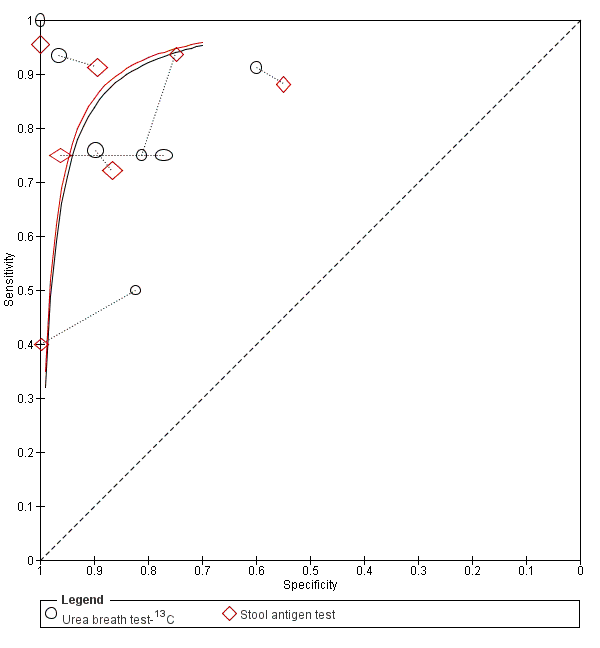
Summary ROC plot of direct comparisons of urea breath test‐13C and stool antigen test. Each summary curve was drawn restricted to the range of specificities for each test. The size of each symbol was scaled according to the precision of sensitivity and specificity in the study. A dotted line joins the pair of points for the two tests from each study.

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for urea breath test‐13C

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for urea breath test‐14C.
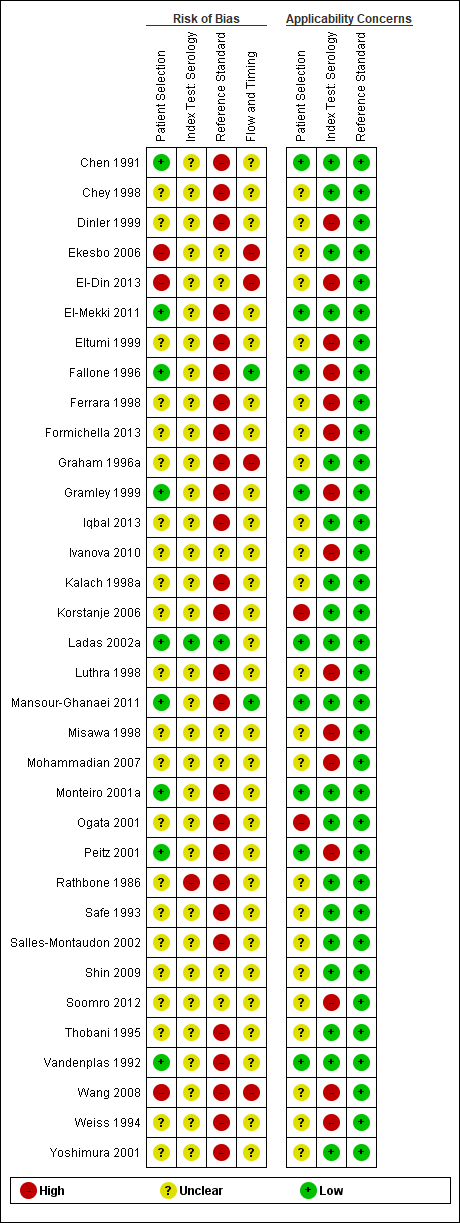
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for serology
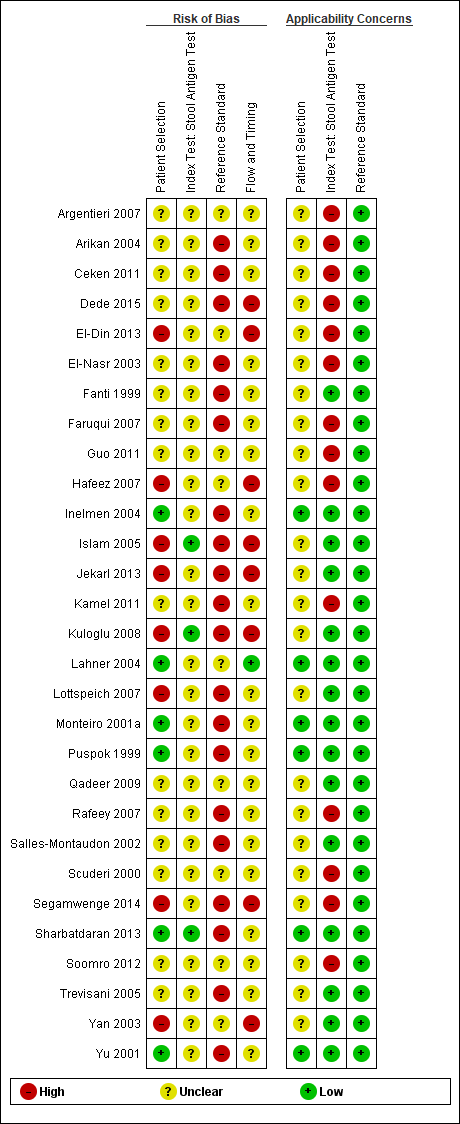
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each study included for the stool antigen test

Urea breath test ‐ Unknown isotope.

Urea breath test‐13C (delta over baseline > 3% (20 minutes)).

Urea breath test‐13C (delta over baseline > 3% (30 minutes)).

Urea breath test‐13C (delta over baseline > 3.5% (30 minutes)).

Urea breath test‐13C (delta over baseline > 4% (10 minutes)).
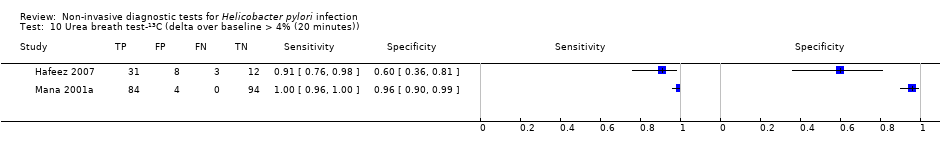
Urea breath test‐13C (delta over baseline > 4% (20 minutes)).

Urea breath test‐13C (delta over baseline > 4% (30 minutes)).

Urea breath test‐13C (delta over baseline > 4.5% (30 minutes)).

Urea breath test‐13C (delta over baseline > 5% (30 minutes)).

Urea breath test‐14C (counts per minute > 50).
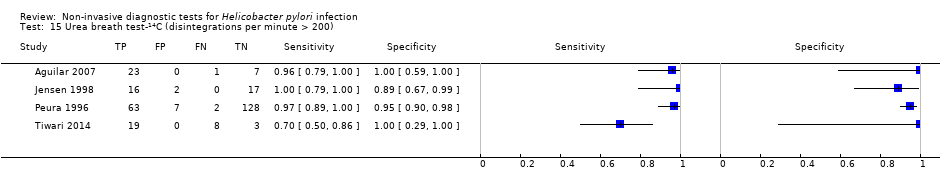
Urea breath test‐14C (disintegrations per minute > 200).
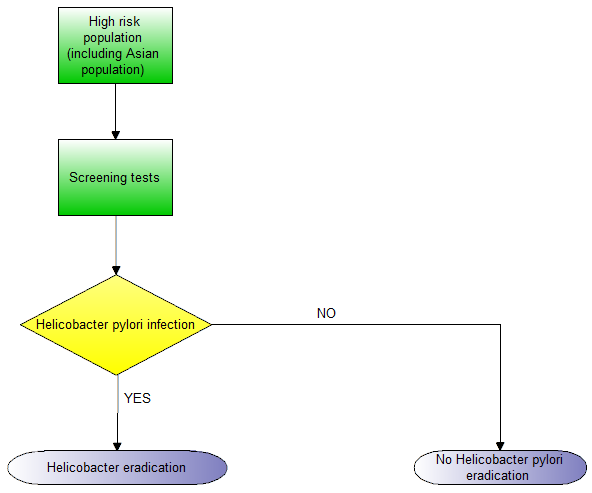
| What is the best non‐invasive test for diagnosis of H pylori infection? | ||||
| Population | Children and adults with gastrointestinal symptoms | |||
| Setting | Primary care setting | |||
| Index tests | Urea breath test‐13C, Urea breath test‐14C, serology, and stool antigen test | |||
| Threshold | Various thresholds were used for each test | |||
| Role and purpose of test | Screening and diagnosis of H pylori | |||
| Reference standard | Endoscopic biopsy with Haemotoxylin & Eosin stain, special stains, or combination of Haemotoxylin & Eosin and special stains | |||
| Quality of evidence | Risk of bias was generally high or unclear with respect to the selection of participants, and the conduct and interpretation of the index tests and reference standard. Applicability concerns were also generally high or unclear with respect to selection of participants | |||
| Limitations | There was heterogeneity in thresholds and reference standards. Studies did not often prespecify or clearly report thresholds used | |||
| Pre‐test probability (prevalence of Helicobacter pylori) | Median (interquartile range) = 53.7% (42.0% to 66.5%) | |||
| Index test | Number of participants (studies) | Diagnostic odds ratio (95% CI) | Sensitivity (95% CI) at fixed specificity of 0.901 | Missed H pylori cases per 1000 people tested (95% CI)2 |
| Urea breath test‐13C | 3139 participants (34 studies) | 153 (95% CI 73.7 to 316) | 0.94 (0.89 to 0.97) | 30 (15 to 58) |
| Urea breath test‐14C | 1810 participants (21 studies) | 105 (95% CI 74.0 to 150) | 0.92 (0.89 to 0.94) | 42 (30 to 58) |
| Serology | 4242 participants (34 studies) | 47.4 (95% CI 25.5 to 88.1) | 0.84 (0.74 to 0.91) | 86 (50 to 140) |
| Stool antigen test | 2988 participants (29 studies) | 45.1 (95% CI 24.2 to 84.1) | 0.83 (0.73 to 0.90) | 89 (52 to 146) |
| Comparison of non‐invasive tests for H pylori infection Based on an indirect comparison of the four tests using all the studies, there was statistical evidence of a difference in diagnostic accuracy (P = 0.024). Direct comparisons were based on few head‐to‐head studies. The ratios of diagnostic odds ratios (95% CI; P value) were 0.68 (95% CI 0.12 to 3.70; P = 0.56) for urea breath test‐13C versus serology (seven studies), and 0.88 (95% CI 0.14 to 5.56; P = 0.84) for urea breath test‐13C versus stool antigen test (seven studies). The 95% confidence intervals of these estimates overlap with those of the ratios of diagnostic odds ratios from the indirect comparison. Data were limited or unavailable for meta‐analysis of other direct comparisons. | ||||
| Conclusions In people with no history of gastrectomy and those who have not recently had antibiotics or proton pump inhibitors, urea breath tests had high diagnostic accuracy while serology and stool antigen tests had lower accuracy to detect H pylori infection. Although susceptible to bias due to confounding, this conclusion is based on evidence from indirect test comparisons as evidence from direct comparisons was based on few studies or was unavailable. It should be noted that studies were generally of poor methodological quality. The thresholds used for the tests were highly variable and there is currently insufficient evidence to recommend specific thresholds for use in clinical practice. | ||||
| 1The sensitivities were estimated along the SROC curves at the median specificity across the studies included for the four tests. 2Based on the sensitivity estimated at the median specificity of 0.90, and the median prevalence of 53.7% from the included studies, the numbers of missed H pylori cases were calculated using a hypothetical cohort of 1000 people suspected of having H pylori infection. The 95% CI for the number of missed cases is from the 95% CI for sensitivity. For a specificity of 0.90 and prevalence of 53.7%, there will be 46 false positives. See Table 3 for results for other values of specificity and prevalence. | ||||
| Threshold | Studies | Number of participants (cases) | Sensitivity (95% CI) | Specificity (95% CI) |
| Urea breath test‐13C | ||||
| Delta over baseline > 3% (20 minutes) | 2 | 254 (128) | 0.98 (0.90 to 1.00) | 0.92 (0.82 to 0.97) |
| Delta over baseline > 3% (30 minutes) | 3 | 333 (140) | 0.99 (0.92 to 1.00) | 0.95 (0.90 to 0.98) |
| Delta over baseline > 3.5% (30 minutes) | 3 | 368 (120) | 0.75 to 1.00 | 0.77 to 1.00 |
| Delta over baseline > 4% (10 minutes) | 2 | 236 (118) | 0.91 to 1.00 | 0.60 to 0.95 |
| Delta over baseline > 4% (20 minutes) | 2 | 236 (118) | 0.91 to 1.00 | 0.60 to 0.96 |
| Delta over baseline > 4% (30 minutes) | 10 | 958 (423) | 0.95 (0.79 to 0.99) | 0.95 (0.87 to 0.98) |
| Delta over baseline > 4.5% (30 minutes) | 3 | 288 (106) | 0.50 to 0.96 | 0.82 to 0.96 |
| Delta over baseline > 5% (30 minutes) | 4 | 601 (315) | 0.95 (0.49 to 1.00) | 0.94 (0.84 to 0.98) |
| Urea breath test‐14C | ||||
| Counts per minute > 50 (10 minutes) | 6 | 471 (231) | 0.89 (0.55 to 0.98) | 0.91 (0.79 to 0.96) |
| Disintegrations per minute > 200 (10 minutes) | 4 | 296 (132) | 0.95 (0.33 to 1.00) | 0.95 (0.80 to 0.99) |
| Serology | ||||
| > 7 units/ml | 2 | 97 (48) | 0.98 (0.74 to 1.00) | 0.71 (0.51 to 0.86) |
| ≥ 300 unit | 2 | 234 (143) | 0.91 (0.82 to 0.96) | 0.86 (0.72 to 0.93) |
| Tests evaluated at the same threshold by more than one study are presented in the table. When there were two or three studies at the same threshold, and little or no heterogeneity was observed in ROC space, estimates of summary sensitivity and summary specificity were obtained by using univariate fixed‐effect logistic regression models to pool sensitivities and specificities separately. When there were two or three studies and we observed heterogeneity, we did not perform meta‐analysis but report the range of the sensitivities and specificities. | ||||
| Index tests | Studies; participants (H pyloripresent) | DOR (95% CI) | Ratio of diagnostic odds ratios (95% CI), P value | ||
| Urea breath test‐13C | Urea breath test‐14C | Serology | |||
| Urea breath test‐13C | 34; 3139 (1526) | 153 (73.7 to 316) | ‐ | ‐ | ‐ |
| Urea breath test‐14C | 21; 1810 (1018) | 105 (74.0 to 150) | 1.45 (0.65 to 3.26), P = 0.36 | ‐ | ‐ |
| Serology | 34; 4242 (2477) | 47.4 (25.5 to 88.1) | 3.22 (1.24 to 8.37), P = 0.017 | 2.22 (1.09 to 4.51), P = 0.028 | ‐ |
| Stool antigen test | 29; 2988 (1311) | 45.1 (24.2 to 84.1) | 3.39 (1.30 to 8.83), P = 0.013 | 2.33 (1.14 to 4.76), P = 0.020 | 1.05 (0.44 to 2.53), P = 0.91 |
| The indirect comparison included all studies that evaluated at least one of the four tests, i.e. all available data. The ratio of diagnostic odds ratios is the diagnostic odds ratio (DOR) of the test in the column divided by the DOR of the test in the row. If the ratio is greater than one, then the test in the column is more accurate than the test in the row; if the ratio is less than one, the test in the row is more accurate than the test in the column. | |||||
| Prevalence (%) | Specificity | False positives1 | Test | Sensitivity (95% CI) | Missed cases (95% CI) |
| 42.0 | 0.79 | 122 | Urea breath test‐13C | 0.98 (0.95 to 0.99) | 10 (5 to 20) |
| Urea breath test‐14C | 0.97 (0.95 to 0.98) | 15 (10 to 20) | |||
| Serology | 0.93 (0.87 to 0.96) | 31 (17 to 54) | |||
| Stool antigen test | 0.92 (0.87 to 0.96) | 32 (18 to 57) | |||
| 53.7 | 0.79 | 97 | Urea breath test‐13C | 0.98 (0.95 to 0.99) | 13 (6 to 26) |
| Urea breath test‐14C | 0.97 (0.95 to 0.98) | 19 (13 to 26) | |||
| Serology | 0.93 (0.87 to 0.96) | 39 (22 to 69) | |||
| Stool antigen test | 0.92 (0.87 to 0.96) | 41 (23 to 72) | |||
| 66.5 | 0.79 | 70 | Urea breath test‐13C | 0.98 (0.95 to 0.99) | 16 (8 to 32) |
| Urea breath test‐14C | 0.97 (0.95 to 0.98) | 23 (16 to 32) | |||
| Serology | 0.93 (0.87 to 0.96) | 49 (27 to 85) | |||
| Stool antigen test | 0.92 (0.87 to 0.96) | 51 (28 to 89) | |||
| 42.0 | 0.90 | 58 | Urea breath test‐13C | 0.94 (0.89 to 0.97) | 23 (12 to 46) |
| Urea breath test‐14C | 0.92 (0.89 to 0.94) | 33 (24 to 46) | |||
| Serology | 0.84 (0.74 to 0.91) | 67 (39 to 110) | |||
| Stool antigen test | 0.83 (0.73 to 0.90) | 70 (41 to 114) | |||
| 53.7 | 0.90 | 46 | Urea breath test‐13C | 0.94 (0.89 to 0.97) | 30 (15 to 58) |
| Urea breath test‐14C | 0.92 (0.89 to 0.94) | 42 (30 to 58) | |||
| Serology | 0.84 (0.74 to 0.91) | 86 (50 to 140) | |||
| Stool antigen test | 0.83 (0.73 to 0.90) | 89 (52 to 146) | |||
| 66.5 | 0.90 | 34 | Urea breath test‐13C | 0.94 (0.89 to 0.97) | 37 (18 to 72) |
| Urea breath test‐14C | 0.92 (0.89 to 0.94) | 53 (38 to 72) | |||
| Serology | 0.84 (0.74 to 0.91) | 106 (62 to 173) | |||
| Stool antigen test | 0.83 (0.73 to 0.90) | 111 (64 to 180) | |||
| 42.0 | 0.96 | 23 | Urea breath test‐13C | 0.86 (0.75 to 0.93) | 57 (30 to 103) |
| Urea breath test‐14C | 0.81 (0.76 to 0.86) | 78 (58 to 103) | |||
| Serology | 0.66 (0.52 to 0.79) | 141 (90 to 204) | |||
| Stool antigen test | 0.65 (0.50 to 0.78) | 146 (93 to 209) | |||
| 53.7 | 0.96 | 19 | Urea breath test‐13C | 0.86 (0.75 to 0.93) | 73 (38 to 132) |
| Urea breath test‐14C | 0.81 (0.76 to 0.86) | 100 (74 to 132) | |||
| Serology | 0.66 (0.52 to 0.79) | 181 (115 to 260) | |||
| Stool antigen test | 0.65 (0.50 to 0.78) | 187 (119 to 267) | |||
| 66.5 | 0.96 | 13 | Urea breath test‐13C | 0.86 (0.75 to 0.93) | 90 (47 to 163) |
| Urea breath test‐14C | 0.81 (0.76 to 0.86) | 124 (92 to 163) | |||
| Serology | 0.66 (0.52 to 0.79) | 224 (142 to 322) | |||
| Stool antigen test | 0.65 (0.50 to 0.78) | 231 (148 to 331) | |||
| 1Average number of participants who are diagnosed with H pylori infection but do not have the infection per 1000 tested. The sensitivities were estimated from the SROC curves at fixed values (lower quartile, median and upper quartile) of specificity from the included studies across all tests. Based on these sensitivities and specificities, and quartiles of prevalence from the included studies (across all tests), the numbers of missed H pylori cases and false positives (i.e. overdiagnosed people) were calculated using a hypothetical cohort of 1000 people suspected of having H pylori infection. | |||||
| Test | Urea breath test‐13C | Urea breath test‐14C | Serology |
| Urea breath test‐13C | ‐ | ‐ | ‐ |
| Urea breath test‐14C | N = 0 | ‐ | ‐ |
| Serology | N = 7 DOR (95% CI) of urea breath test‐13C = 74.8 (95% CI 17.8 to 314) DOR (95% CI) of serology = 111 (95% CI 41.2 to 297) RDORs (95% CI) of urea breath test‐13C versus serology, P value = 0.68 (95% CI 0.12 to 3.70), P = 0.56 | N = 1 | ‐ |
| Stool antigen test | N = 7 DOR (95% CI) of stool antigen test = 53.0 (95% CI 5.34 to 527) RDORs (95% CI) of urea breath test‐13C versus stool antigen test, P value = 0.88 (95% CI 0.14 to 5.56), P = 0.84 | N = 2 | N = 4 |
| DOR = diagnostic odds ratio; N = number of studies; RDORs = ratio of diagnostic odds ratios. Due to paucity of data and substantial heterogeneity observed in ROC space which precluded the use of simpler meta‐analytic models, meta‐analyses were not possible for two test comparisons that had more than one study. For the single study of urea breath test‐14C versus serology (Mansour‐Ghanaei 2011), both tests had similar sensitivity, but specificity was higher for urea breath test‐14C than for serology. The ratio of diagnostic odds ratios is the DOR of the test in the column divided by the DOR of the test in the row. If the ratio is greater than one, then the test in the column is more accurate than the test in the row; if the ratio is less than one, the test in the row is more accurate than the test in the column. | |||
| Test | No. of studies | No. of participants |
| 1 Urea breath test‐13C Show forest plot | 34 | 3139 |
| 2 Urea breath test‐14C Show forest plot | 21 | 1810 |
| 3 Urea breath test ‐ Unknown isotope Show forest plot | 2 | 127 |
| 4 Serology Show forest plot | 34 | 4242 |
| 5 Stool antigen test Show forest plot | 29 | 2988 |
| 6 Urea breath test‐13C (delta over baseline > 3% (20 minutes)) Show forest plot | 2 | 254 |
| 7 Urea breath test‐13C (delta over baseline > 3% (30 minutes)) Show forest plot | 3 | 333 |
| 8 Urea breath test‐13C (delta over baseline > 3.5% (30 minutes)) Show forest plot | 3 | 368 |
| 9 Urea breath test‐13C (delta over baseline > 4% (10 minutes)) Show forest plot | 2 | 236 |
| 10 Urea breath test‐13C (delta over baseline > 4% (20 minutes)) Show forest plot | 2 | 236 |
| 11 Urea breath test‐13C (delta over baseline > 4% (30 minutes)) Show forest plot | 10 | 958 |
| 12 Urea breath test‐13C (delta over baseline > 4.5% (30 minutes)) Show forest plot | 3 | 288 |
| 13 Urea breath test‐13C (delta over baseline > 5% (30 minutes)) Show forest plot | 4 | 601 |
| 14 Urea breath test‐14C (counts per minute > 50) Show forest plot | 6 | 471 |
| 15 Urea breath test‐14C (disintegrations per minute > 200) Show forest plot | 4 | 296 |
| 16 Serology > 7 units/ml Show forest plot | 2 | 97 |
| 17 Serology ≥300 units Show forest plot | 2 | 234 |