Tratamientos tópicos para blefaroqueratoconjuntivitis en niños
References
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Randomised controlled trial (RCT) | |
| Participants | 137 children (80 males) aged 0 to 6 (mean age 2.73 years) with a clinical diagnosis of blepharoconjunctivitis and otherwise in good general health. The study excluded participants if they were using or used recently other anti‐inflammatory agents. The study included only one eye per participant. 126 participants completed the follow‐up. | |
| Interventions | Topical loteprednol/tobramycin combination (34 participants) versus loteprednol alone (35 participants) versus tobramycin alone (34 participants) versus placebo (34 participants). Eye drops were given 4 times a day for 14 days. One participant in the placebo group failed study screening (reason unspecified) and was not included in the safety population. | |
| Outcomes | Visual acuity and assessment of signs of blepharoconjunctivitis at baseline, day 1, day 3 (±1), day 7 (±1) and day 15 (±1). The study reported adverse events (ocular and non‐ocular). | |
| Notes | The study was carried out between June 2008 to May 2010. Bausch & Lomb Global Clinical Programs, Rochester, NY, USA sponsored, designed and conducted the trial. Some trial authors were employees of Bausch & Lomb; they declared this conflict of interest in the publication. Clinical trial registration number: NCT00705159. | |
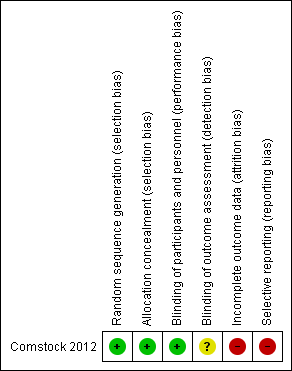
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial used computerised randomisation with a code developed by an independent statistician. |
| Allocation concealment (selection bias) | Low risk | Drugs were packaged identically and labelled according to a computer‐generated randomisation code unique to the study. |
| Blinding of participants and personnel (performance bias) | Low risk | Drugs were packaged in identical bottles. Study investigators were not present during instillation due to differences in the appearance of drops. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Study investigators were not present during instillation due to differences in the appearance of drops but no other details are given regarding masking of outcome assessors to randomisation. |
| Incomplete outcome data (attrition bias) | High risk | The trial authors accounted for losses to follow‐up. The trial authors reported Snellen visual acuities but the numbers of participants able to complete Snellen acuity varied from 33% to 59% across treatment groups. The only comment regarding other visual acuity measures was "Of subjects providing visual behavior responses, 94.5% could fix and follow". |
| Selective reporting (reporting bias) | High risk | Outcomes on trial register were reported on trial register but outcomes on visual acuity and adverse events which were the main focus of the publication were not mentioned on the trials register and visual acuity was not reported fully in the publication. |
Abbreviations: RCT: randomised controlled trial.
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Randomised controlled trial (RCT) but adult participants only. | |
| RCT but adult participants only. | |
| RCT. Publication that compared azithromycin 1.0%/dexamethasone 0.1% combination drop versus azithromycin 1.0% alone or dexamethasone 0.1% alone in the treatment of blepharoconjunctivitis in adults and children. We were unable to obtain the data for the paediatric subgroup despite contacting the trial authors and their industry partners. | |
| RCT. Publication compared gentamicin‐betamethasone ointment versus gentamicin ointment alone, betamethasone ointment alone, or placebo in the treatment of acute blepharoconjunctivitis in adults and children. We were unable to obtain the data for the paediatric subgroup despite contacting the study authors and their industry partners. | |
| RCT but adult participants only. |
Abbreviations: RCT: randomised controlled trial.
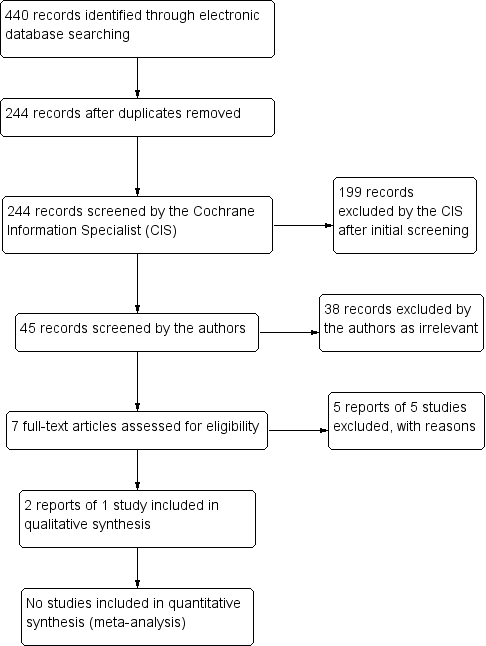
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Topical treatments compared with control for blepharokeratoconjunctivitis in children | ||||||
| Patient or population: children with blepharokeratoconjunctivitis Settings: eye clinic Intervention: topical treatments (antibiotics and/or steroids) Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Certainty (quality) of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo (vehicle) | topical treatments (antibiotics/steroids) | |||||
| Improvement in symptoms, reported by the child or by their parents/carers, preferably measured by a validated tool, at three months (± one month) after start of treatment | ‐ | ‐ | ‐ | 137 (1) | ⊕⊝⊝⊝ | Data on changes in grade of blepharoconjunctivitis measured between baseline and 2 weeks did not suggest any important differences between groups. |
| Elimination of all clinical signs of ocular surface inflammation ('complete success'), preferably measured by a composite grading system, at three months (± one month) after start of treatment | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Improvement of clinical signs of ocular surface inflammation ('partial success'), preferably measured by a composite grading system, at three months (± one month) after start of treatment | ‐ | ‐ | ‐ | 137 (10 | ⊕⊝⊝⊝ | Data on changes in grade of blepharoconjunctivitis measured between baseline and 2 weeks did not suggest any important differences between groups. |
| Change from baseline in best corrected visual acuity in affected eye(s) in logMAR measured with an ETDRS chart at 4 m, or, in younger children, with a Keeler crowded logMAR chart at 3 m, at three months (± one month) after start of treatment | ‐ | ‐ | ‐ | 137 (1) | ⊕⊝⊝⊝ | Limited data in a form that could not be extracted; not statistically significant differences between groups. |
| Uncontrolled or poorly controlled disease progression due to treatment failure, at three months (± one month) after start of treatment | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Adverse effects of medication, at any time during treatment | Ocular adverse events
Non‐ocular adverse events
| 137 (1) | ⊕⊝⊝⊝ | |||
| Quality of life | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Some data on blepharoconjunctivitis grade reported on trials registry but we were unable to estimate a measure of effect for this outcome. 2 Data were not fully reported and we were unable to estimate a measure of effect for change in visual acuity. 3 Very low certainty due to very low numbers of events. | ||||||
| Author, year | Study type | N | Age | Mean/median follow‐up | Mechanical treatment | Systemic (oral) interventions | Topical interventions | Physician‐reported outcomes | Patient‐reported outcomes | Adverse events from condition | Adverse events from treatment |
| Case series | 7 | 6 to 14 years | 6 months | Lid hygiene | Amoxicillin/ clavulanate | Chloramphenicol (PF) drops, chloramphenicol ointment to lids, prednisolone 0.5% (PF) | Eyelid condition, corneal epitheliopathy, stromal defects | Improvement of symptoms | None | None | |
| Case series | 3 | 30 months to 8 years | Variable | Lid hygiene | Azithromycin | Loteprednol 0.2%, CSA 0.05%, | Chalazia, keratitis, corneal ulcer/scar, phlyctenule, MGD | Improvement of itching | None | None | |
| Case series | 16 | 4 to 16 years | Variable | Lid hygiene | Erythromycin (1 participant only) | Azithromycin 1.5%, CSA 2% | Bulbar conjunctival hyperaemia, conjunctival phlycten, corneal inflammation, blepharitis grade | Ocular redness | None | Ocular irritation (redness, burning, stinging) | |
| Case series | 8 | 3.5 to 13 years | 8.3 months | Lid hygiene | Erythromycin suspension 450 mg divided into 3 doses | Prednisolone 0.5% (PF); hydrocortisone acetate 1% ointment nocte | Bulbar conjunctival redness, inferior superficial corneal vascularisation, punctate corneal epithelial staining, inferior subepithelial vascularisation and infiltrate, conjunctival phlyctenules, corneal phlyctenules, circumferential pannus, corneal scar | Red eyes, photophobia, itching, discharge | Corneal scarring and thinning | Stomach disturbance, diarrhoea | |
| Case series | 615 | 7 months to 16 years | Not reported | Lid hygiene | Erythromycin | Topical steroids and antibiotics (not specified) | Outcomes not reported (presenting signs only) | Outcomes not reported (presenting symptoms only) | None | None | |
| Case series | 10 | 6 to 27 years | 4.4 years | Lid hygiene | Azathioprine, mycophenolate mofetil, prednisolone | Steroids (not specified) | Disease remission/ control of inflammation | None | Corneal perforation | none | |
| Case series | 29 | 2 to 12 years | 5.4 months | Warm compresses | Erythromycin, doxycyclin | Prednisolone 1%, dexamethasone 0.1%, antibiotic, fluorometholone, loteprednol etabonate 0.5% | Eyelid inflammation, superficial punctate keratitis, corneal vascularisation, corneal infiltrates, phlyctenules, corneal scarring | None | Amblyopia | Gastrointestinal distress, mouth ulcers (unrelated) | |
| Case series | 27 | 7 months to 15.9 years | 2.3 years | Warm compresses, lid hygiene | Erythromycin, doxycyclin, flaxseed oil | chloramphenicol, ciprofloxacin, gentamicin, prednisolone 1% or 0.5%, fluorometholone 0.1% | Visual acuity, astigmatism | Discomfort, photophobia | Amblyopia | Vaginal candidiasis | |
| Case series | 5 | 4 to 9 years | Not specified | Erythromycin | Lid hyperaemia and swelling, corneal infiltrates | None | None | None | |||
| Case series | 114 | Mean 9.3 years (± 4.2) | 26.4 months | Lid hygiene | Flaxseed oil, erythromycin | Lubricants (hyaluronate, methylcellulose), erythromycin, ciprofloxacin, steroids (dexamethasone 0.1% (PF), loteprednol 0.5%, fluorometholone 0.1%), CSA 0.05% | Visual acuity | None | None reported | None reported | |
| Case series | 51 | Mean 10.2 years (± 3.6) | 58.9 months | Warm compresses, lid hygiene | Antibiotics (erythromycin, amoxicillin/ clavulanate, doxycycline), steroids | Steroids (dexamethasone 1%, prednisolone 0.12 to 1%, fluorometholone 0.1%) , antibiotics (fucidic acid, levofloxacin, tobramycin), CSA 0.5% | Visual acuity | Redness, tearing, blurred vision, pain, irritation, photophobia, white spot, swelling, discharge, itching, rubbing | Corneal perforation | Raised intraocular pressure, cataract, gastrointestinal disturbance | |
| Case series | 44 | 1 to 14 years | 7 years | Lid hygiene | Erythromycin | Chloramphenicol, steroids | Reduction of clinical signs | Redness, watering, itching, grittiness, discharge, photophobia, pain | None reported | None reported | |
| Abbreviations: CSA: ciclosporin | |||||||||||
| Author, year | Study type | N | Age | Mean/median follow‐up | Mechanical treatment | Systemic (oral) interventions | Topical interventions | Physician‐reported outcomes | Patient‐reported outcomes | Adverse events from condition | Adverse events from treatment |
| RCT | 137 | 0 to 6 years | 15 days | None | None | Loteprednol 0.5% , tobramycin 0.3% | Visual acuity | None | None | Eye pain, conjunctivitis, eye discharge, and eye inflammation | |
| RCT | Total 417; 19 children | Not specified | 15 days | None | None | Azithromycin 1%, dexamethasone 0.1% | Complete bacterial eradication from conjunctiva and eyelids, complete resolution of clinical signs | Complete resolution of symptoms | None | Eye disorder, reduced visual acuity, punctate keratitis, blurred vision, conjunctival oedema, discharge, lid oedema, irritation, pain, itching | |
| RCT | Total 71; number of children not specified | 10 to 86 years | 14 to 15 days | None | None | Gentamycin 0.3%, betamethasone 0.1% | Ocular sign score, specific ocular inflammatory signs, bacterial eradication | None | None | Conjunctival hyperaemia | |
| Abbreviations: N: number of participants | |||||||||||
| Follow‐up | Loteprednol Etabonate and Tobramycin | Loteprednol Etabonate | Tobramycin | Vehicle |
| Mean (SD) N | Mean (SD) N | Mean (SD) N | Mean (SD) N | |
| Day 3 | ‐7.32 (3.27) 34 | ‐7.74 (3.90) 34 | ‐5.94 (4.00) 32 | ‐6.58 (3.46) 31 |
| Day 7 | ‐11.03 (3.20) 34 | ‐10.94 (4.69) 34 | ‐9.90 (3.80) 30 | ‐10.03 (4.63) 30 |
| Day 15 | ‐11.41 (3.29) 34 | ‐11.23 (3.98) 35 | ‐10.68 (4.71) 34 | ‐10.30 (5.19) 33 |
| Loteprednol/tobramycin | Loteprednol | Tobramycin | Vehicle | |
| Ocular AEs | 1/34 (eye pain) | 4/35 (eye pain, conjunctivitis, eye discharge, eye inflammation) | 0/34 | 0/33 |
| Non‐Ocular AEs | 2/34 3 AEs (gastroenteritis, pyrexia, bronchiolitis) | 6/35 9 AEs (ear infection, lip swelling, vomiting, URI, varicella, cough, phyarngolaryngeal pain, rash) | 6/34 9 AEs (ear infection, otitis media acute, diarrhea, pyrexia, bronchioltis, URI, nasophayngitis, respirator distress, dermatitis (diaper) ) | 5/33 7 AEs (ear pain, pyrexia, urticaria, bronchioloitis, URI, tonsilitis, dehydration) |
| Abbreviations: AEs: adverse events | ||||