Amitriptilina para la fibromialgia en adultos
Appendices
Appendix 1. Methodological considerations for chronic pain
There have been several recent changes in how the efficacy of conventional and unconventional treatments is assessed in chronic painful conditions. The outcomes are now better defined, particularly with new criteria for what constitutes moderate or substantial benefit (Dworkin 2008); older trials may only report participants with 'any improvement'. Newer trials tend to be larger, avoiding problems from the random play of chance. Newer trials also tend to be of longer duration, up to 12 weeks, and longer trials provide a more rigorous and valid assessment of efficacy in chronic conditions. New standards have evolved for assessing efficacy in neuropathic pain, and we are now applying stricter criteria for the inclusion of trials and assessment of outcomes, and are more aware of problems that may affect our overall assessment. To summarise some of the recent insights that must be considered in this new review:
-
Pain results tend to have a U‐shaped distribution rather than a bell‐shaped distribution. This is true in acute pain (Moore 2011a; Moore 2011b), back pain (Moore 2010d), and arthritis (Moore 2010c), as well as in fibromyalgia (Straube 2010); in all cases average results usually describe the experience of almost no‐one in the trial. Data expressed as averages are potentially misleading, unless they can be proven to be suitable.
-
As a consequence, we have to depend on dichotomous results (the individual either has or does not have the outcome) usually from pain changes or patient global assessments. The Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) group has helped with their definitions of minimal, moderate, and substantial improvement (Dworkin 2008). In arthritis, trials of less than 12 weeks duration, and especially those shorter than eight weeks, overestimate the effect of treatment (Moore 2010c); the effect is particularly strong for less effective analgesics, and this may also be relevant in neuropathic‐type pain.
-
The proportion of patients with at least moderate benefit can be small, even with an effective medicine, falling from 60% with an effective medicine in arthritis to 30% in fibromyalgia (Moore 2009; Moore 2010c; Moore 2013b; Moore 2014b; Straube 2010; Sultan 2008). A Cochrane review of pregabalin in neuropathic pain and fibromyalgia demonstrated different response rates for different types of chronic pain (higher in diabetic neuropathy and postherpetic neuralgia and lower in central pain and fibromyalgia) (Moore 2009). This indicates that different neuropathic pain conditions should be treated separately from one another, and that pooling should not be done unless there are good grounds for doing so.
-
Individual patient analyses indicate that patients who get good pain relief (moderate or better) have major benefits in many other outcomes, affecting quality of life in a significant way (Moore 2010b; Moore 2014a).
-
Imputation methods such as last observation carried forward (LOCF), used when participants withdraw from clinical trials, can overstate drug efficacy especially when adverse event withdrawals with drug are greater than those with placebo (Moore 2012b).
Appendix 2. MEDLINE (via OVID) search strategy
-
exp PAIN/
-
exp PERIPHERAL NERVOUS SYSTEM DISEASES/
-
exp SOMATOSENSORY DISORDERS/
-
FIBROMYALGIA/ or exp MYOFASCIAL PAIN SYNDROMES/ or POLYMYALGIA RHEUMATICA/
-
((pain* or discomfort*) adj10 (central or complex or rheumat* or muscl* or muscul* or myofasci* or nerv* or neuralg* or neuropath*)).mp.
-
(fibromyalgi* or fibrosti* or FM or FMS).mp.
-
((neur* or nerv*) adj6 (compress* or damag*)).mp.
-
1 or 2 or 3 or 4 or 5 or 6 or 7
-
Amitriptyline/
-
(am?tr?pt?lin* or amitriptyliini).mp.
-
9 or 10
-
8 and 11
-
randomized controlled trial.pt.
-
controlled clinical trial.pt.
-
randomized.ab.
-
placebo.ab.
-
drug therapy.fs.
-
randomly.ab.
-
trial.ab.
-
groups.ab.
-
or/13‐20
-
exp animals/ not humans.sh.
-
21 not 22
-
23 and 12
Appendix 3. EMBASE (via OVID) search strategy
-
exp chronic pain/
-
exp peripheral neuropathy/
-
exp somatosensory disorder/
-
fibromyalgia/ or exp myofascial pain/ or rheumatic polymyalgia/
-
((pain* or discomfort*) adj10 (central or complex or rheumat* or muscl* or muscul* or myofasci* or nerv* or neuralg* or neuropath*)).mp.
-
(fibromyalgi* or fibrosti* or FM or FMS).mp.
-
((neur* or nerv*) adj6 (compress* or damag*)).mp.
-
1 or 2 or 3 or 4 or 5 or 6 or 7
-
amitriptyline/
-
(am?tr?pt?lin* or amitriptyliini or Tryptomer or Elavil or Tryptizol or Laroxyl or Sarotex or Lentizol or Endep).mp.
-
9 or 10
-
8 and 11
-
random*.ti,ab.
-
factorial*.ti,ab.
-
(crossover* or cross over* or cross‐over*).ti,ab.
-
placebo*.ti,ab.
-
(doubl* adj blind*).ti,ab.
-
assign*.ti,ab.
-
allocat*.ti,ab.
-
RANDOMIZED CONTROLLED TRIAL.sh.
-
DOUBLE‐BLIND PROCEDURE.sh.
-
CROSSOVER PROCEDURE.sh.
-
13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
-
12 and 23
Appendix 4. CENTRAL search strategy
-
MeSH descriptor Pain explode all trees
-
MeSH descriptor Peripheral Nervous System Diseases explode all trees
-
MeSH descriptor Somatosensory Disorders explode all trees
-
MeSH descriptor Fibromyalgia, this term only
-
MeSH descriptor Myofascial Pain Syndromes explode all trees
-
MeSH descriptor Polymyalgia Rheumatica explode all trees
-
((pain* or discomfort*) and (central or complex or rheumat* or muscl* or muscul* or myofasci* or nerv* or neuralg* or neuropath*)):ti,ab,kw
-
(fibromyalgi* or fibrosti* or FM or FMS):ti,ab,kw
-
((neur* or nerv*) and (compress* or damag*)):ti,ab,kw
-
(1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9)
-
MeSH descriptor Amitriptyline
-
(am?tr?pt?lin* or amitriptyliini or Tryptomer or Elavil or Tryptizol or Laroxyl or Sarotex or Lentizol or Endep).ti,ab,kw
-
11 or 12
-
10 and 13
-
Limit 14 to CENTRAL
Appendix 5. Summary of outcomes in individual studies: efficacy
| Study | Treatment (taken at night, unless stated) | Pain outcome | Other efficacy outcome |
| Amitriptyline 25 mg = 13 | VAS PI reduced in all groups compared with baseline, but no statistically significant difference between groups | No significant differences between groups on any of the measures: fatigue, sleep, QoL | |
| Amitriptyline 50 mg = 27 | Global impression of change ‐ moderate or marked at 9 weeks Placebo = 10/32 Placebo = 5/32 | No difference in tender points, but improved sleep with amitriptyline | |
| Amitriptyline 25 mg = 84 | Significant improvers (50% improvement in pain, sleep, fatigue, global, myalgic score, 4 of 6): Placebo = 8/42 No difference for change in mean pain score (from graph): Placebo dropped 69 to 54 mm | No significant end of trial difference for sleep, fatigue, global, tender points | |
| Amitriptyline 25 mg = 22 Placebo = 20 Cross‐over | Significant improvers (50% improvement in pain, sleep, fatigue, global, myalgic score, 4 of 6) Amitriptyline = 6/22 Placebo = 0/22 VAS pain at 8 weeks (mean ± SD) Amitriptyline = 5.1 ± 3.2 | Significant difference for sleep, patient global, fatigue, but not tender points | |
| Amitriptyline 25 mg daily = 21 Melatonin 10 mg daily = 21 Amitriptyline 25 mg + melatonin 10 mg daily = 21 | Mean PI in last 24 h during last week of treatment (100 mm VAS) vs before treatment | No significant difference observed between groups in the numbers of analgesic used in last week of treatment, sleep quality and number of tender points | |
| Amitriptyline 25 mg = 24 Placebo = 22 | Responder (at least 50% improvement pain and or global) at 8 weeks: Placebo = 0/22 VAS pain (mean ± SD) Amitriptyline baseline 3.8 ± 2.4 | Major changes in patient global, tender point count and score, sleep, fatigue, and stiffness | |
| Balanced assignment quoted, but actual numbers in each group not given Therefore we assume: Placebo = 16 (Also included naproxen 2 x 500 mg and amitriptyline + naproxen treatment arms) | VAS pain at 6 weeks (mean, from graph): Placebo = about 7.4 | End of trial ‐ significant benefit for amitriptyline versus placebo for fatigue, sleep, and patient global assessment, but not tender points | |
| Amitriptyline 25 mg = 21 Placebo = 19 Cross‐over | VAS pain at 6 weeks (mean ± SD) Placebo = 82 ± 17 | Apparent significant results, probably amitriptyline versus placebo, for pain, FIQ, sleep, and global, but not fatigue or tender points | |
| Amitriptyline 25 mg = 42 Placebo = 45 Titration to max 37.5 mg A, 600 mg M | VAS (mean ± SD) Placebo baseline 5.7 ± 2.3 | General health, sleep fatigue tender points, and clinician severity all improved with amitriptyline and placebo, but no obvious between group difference, except perhaps sleep |
AE: adverse effect; d: day; FIQ: Fibromyalgia Impact Questionnaire; QoL: quality of life; SD: standard deviation; VAS: visual analogue scale
Appendix 6. Summary of outcomes in individual studies: adverse events and withdrawals
| Study | Treatment (taken at night, unless stated) | Adverse events | Withdrawals |
| Amitriptyline 25 mg = 13 | Not reported | All cause: | |
| Amitriptyline 50 mg = 27 | Patients with ≥ 1 AE: Placebo = 4/32 "minor side effects" ‐ mostly drowsiness and xerostomia | Total: | |
| Amitriptyline 25 mg = 84 | Patients with ≥ 1 AE: Amitriptyline = 80/84 Placebo = 26/42 | Total: Amitriptyline = 14/84, Cyclobenzaprine = 24/82, Placebo = 14/42 | |
| Amitriptyline 25 mg = 22 Placebo = 20 Cross‐over | Not reported | 2 withdrawals after first period A (not drug‐related) | |
| Amitriptyline 25 mg daily = 21 Melatonin 10 mg daily = 21 Amitriptyline 25 mg + melatonin 10 mg daily = 21 | Minor Amitriptyline + melatonin not reported Amitriptyline + melatonin not reported | AE: Amitriptyline 2/21 No other withdrawals reported | |
| Amitriptyline 25 mg = 24 Placebo = 22 | Amitriptyline = 7/24 (3 dry mouth, 2 digestive symptoms, 1 vertigo, 2 neuro‐psychic symptoms) Placebo = 0/22 | 1 in amitriptyline due to AE | |
| Balanced assignment quoted, but actual numbers in each group not given. Therefore we assume: Placebo = 16 (Also included naproxen 2 x 500 mg, and amitriptyline + naproxen treatment arms) | 8 patients (across groups) complained of side effects but did not discontinue medication (dry mouth, dyspepsia, diarrhoea) | Amitriptyline = 1 (lost to follow‐up) Placebo = 1 (AE ‐ epigastric distress) | |
| Amitriptyline 25 mg = 21 Placebo = 19 Cross‐over | Not reported | 12/31 did not complete Placebo = 1 (AE) | |
| Amitriptyline 25 mg = 42 Placebo = 45 Titration to max 37.5 mg amitriptyline, 600 mg moclobemide | Patients with ≥ 1 AE: Placebo = 36/45 (fatigue, headache) | Withdrawals: Placebo = 15/45 (7 LoE, 5 AE, 3 other) |
AE: adverse effect; LoE: lack of efficacy; SAE: serious adverse effect

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Amitriptyline versus placebo, outcome: 1.1 Third‐tier efficacy.
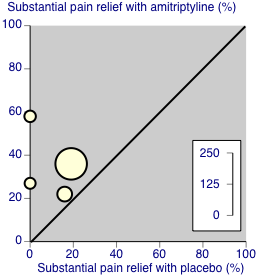
Third‐tier evidence: substantial pain relief

Comparison 1 Amitriptyline versus placebo, Outcome 1 Third‐tier efficacy.

Comparison 1 Amitriptyline versus placebo, Outcome 2 At least 1 adverse event.

Comparison 1 Amitriptyline versus placebo, Outcome 3 All‐cause withdrawal.

Comparison 1 Amitriptyline versus placebo, Outcome 4 Adverse event withdrawal.

Comparison 1 Amitriptyline versus placebo, Outcome 5 Lack of efficacy withdrawal.
| Amitriptyline compared with placebo for fibromyalgia | ||||||
| Patient or population: adults with fibromyalgia Settings: community Intervention: amitriptyline 25 to 50 mg daily Comparison: placebo | ||||||
| Outcomes | Probable outcome with intervention | Probable outcome with placebo | NNT or NNH and/or relative effect (95% CI) | No of Participants | Quality of the evidence | Comments |
| At least 50% reduction in pain or equivalent (substantial) | 360 in 1000 | 110 in 1000 | RR 2.9 (1.7 to 4.9) NNT 4.1 (2.9 to 6.7) | 4 studies, 275 participants | Very low | Small number of studies and participants |
| At least 30% reduction in pain or equivalent (moderate) | no data | |||||
| Adverse event withdrawals | 80 in 1000 | 90 in 1000 | RR 1.03 (0.49 to 2.2) NNTp not calculated | 4 studies, 298 participants | Very low | Small number of studies and participants |
| Serious adverse events | none reported | |||||
| Death | none reported | |||||
| GRADE Working Group grades of evidence | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Third‐tier efficacy Show forest plot | 4 | 275 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.88 [1.69, 4.91] |
| 1.1 Fibromyalgia | 4 | 275 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.88 [1.69, 4.91] |
| 2 At least 1 adverse event Show forest plot | 4 | 318 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [1.29, 1.84] |
| 3 All‐cause withdrawal Show forest plot | 7 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.53, 1.11] |
| 4 Adverse event withdrawal Show forest plot | 4 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.49, 2.16] |
| 5 Lack of efficacy withdrawal Show forest plot | 3 | 272 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.19, 0.95] |


