Estrategias de transfusión de glóbulos rojos restrictivas versus liberales para los pacientes con neoplasias hematológicas malignas tratados con radioterapia o quimioterapia intensiva, o ambas, con o sin apoyo de células madre hematopoyéticas
Appendices
Appendix 1. CENTRAL search strategy on the 15 June 2016
#1 MeSH descriptor: [Blood Transfusion] this term only
#2 MeSH descriptor: [Blood Component Transfusion] explode all trees
#3 MeSH descriptor: [Erythrocyte Transfusion] this term only
#4 (erythrocyte* or "red cell*" or blood or RBC*) near/5 (transfus* or unit*)
#5 (("red cell*" or RBC* or erythrocyte* or "red blood cell*" or "whole blood" or transfus*) near/5 (trigger* or level* or threshold* or rule* or target* or restrict* or liberal* or reduc* or limit*))
#6 (("red cell*" or blood) near/3 (management or sparing or support or strateg*))
#7 ("allogeneic blood" or (unit* near/2 blood) or "allogenic blood" or (blood near/2 exposure) or "donor blood" or "blood product" or "blood products" or "blood component" or "blood components" or "blood support")
#8 (h*emotransfus* or hypertransfus* or h*emotherap*)
#9 ("red cell*" or "red blood cell*" or RBC* or transfus*):ti
#10 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9
#11 MeSH descriptor: [Hematologic Neoplasms] explode all trees
#12 MeSH descriptor: [Hematologic Diseases] this term only
#13 MeSH descriptor: [Leukemia] explode all trees
#14 MeSH descriptor: [Lymphoma] explode all trees
#15 MeSH descriptor: [Neoplasms, Plasma Cell] explode all trees
#16 MeSH descriptor: [Anemia, Aplastic] explode all trees
#17 MeSH descriptor: [Bone Marrow Diseases] explode all trees
#18 MeSH descriptor: [Thrombocytopenia] explode all trees
#19 (thrombocytop*eni* or leuk*emi* or lymphom* or "aplastic an*emi*" or "refractory an*emi*" or myelodysplas* or myeloproliferat* or myelom* or plasmacytom*)
#20 (lymphogranulomato* or histiocy* or granulom* or thrombocyth*emi* or polycyth*emi* or myelofibros* or AML or CLL or CML or Hodgkin* or nonhodgkin* or reticulos* or reticulosarcom* or MDS or RAEB or "RAEB‐t")
#21 (burkitt* next (lymph* or tumo*r)) or lymphosarcom* or brill‐symmer* or sezary
#22 ((h*ematolog* or blood or "red cell*" or "white cell*" or lymph* or marrow or platelet*) near/3 (malignan* or oncolog* or cancer* or neoplasm* or carcinoma*))
#23 MeSH descriptor: [Antineoplastic Agents] explode all trees
#24 MeSH descriptor: [Remission Induction] explode all trees
#25 MeSH descriptor: [Antineoplastic Protocols] explode all trees
#26 MeSH descriptor: [Stem Cell Transplantation] explode all trees
#27 MeSH descriptor: [Bone Marrow Transplantation] this term only
#28 MeSH descriptor: [Radiotherapy] explode all trees
#29 MeSH descriptor: [Lymphatic Irradiation] this term only
#30 (("bone marrow" or "stem cell*" or "progenitor cell*") near/2 (transplant* or graft* or engraft* or rescu*))
#31 ((h*ematolog* or h*emato‐oncolog*) near/2 patients)
#32 (ASCT or ABMT or PBPC or PBSCT or PSCT or BMT or SCT or HSCT)
#33 #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32
#34 ((consolidat* or induct* or maintenance or conditioning*) near/3 (therap* or treat* or regimen* or patient*))
#35 ((therap* or induc*) near/3 remission*)
#36 ((cytosta* or cytotox*) near/2 (therap* or treat* or regimen*))
#37 ((multimodal* or multi‐modal*) near/3 (treat* or therap*))
#38 (combi* near/2 modalit*)
#39 MeSH descriptor: [Transplantation Conditioning] explode all trees
#40 mini‐tra?splant*
#41 MeSH descriptor: [Transplantation, Homologous] explode all trees
#42 (allograft* or allo‐graft* or allotransplant* or allo‐transplant* or ((allogen* or allo‐gen*) near/5 (transplant* or trasplant* or graft* or rescue*)) or homograft* or homo‐graft* or homotransplant* or homo‐transplant* or homotrasplant* or homo‐trasplant*)
#43 MeSH descriptor: [Transplantation, Autologous] this term only
#44 (autograft* or auto‐graft* or autotransplant* or auto‐transplant* or autotra?splant* or auto‐tra?splant* or (autolog* near/5 (transplant* or graft* or trasplant* or rescu*)))
#45 #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44
#46 #33 or #45
#47 #10 and #46
#
Appendix 2. MEDLINE (Ovid) search strategy on the 15 June 2016
1. BLOOD TRANSFUSION/
2. *BLOOD COMPONENT TRANSFUSION/
3. ERYTHROCYTE TRANSFUSION/
4. ((erythrocyte* or red cell* or blood or RBC*) adj
5 (transfus* or unit*)).tw,kf. 5. ((red cell* or RBC* or erythrocyte* or red blood cell* or whole blood or transfus*) adj3 (trigger* or level* or threshold* or rule* or target* or restrict* or liberal* or reduc* or limit*)).tw,kf.
6. (allogeneic blood or (unit* adj2 blood) or allogenic blood or (blood adj2 exposure) or donor blood or blood product* or bl ood component* or blood support).tw,kf.
7. (h?emotransfus* or hypertransfus* or h?emotherap*).tw,kf.
9. (red cell* or erythrocyte* or transfus* or whole blood or RBC*).ti.
10. BLOOD COMPONENT TRANSFUSION/ not (EXCHANGE TRANSFUSION, WHOLE BLOOD/ or PLASMA EXCHANGE/ or PLATELET TRANSFUSION/ or exp LEUKOCYTE TRANSFUSION/)
11. ERYTHROCYTES/ or (red cell* or red blood cell* or erythrocyte* or RBC*).ti.
12. 10 and 11
13. or/1‐9,12
14. exp Hematologic Neoplasms/ or Hematologic Diseases/
15. exp Leukemia/ or exp Lymphoma/
16. exp Neoplasms, Plasma Cell/
17. exp Anemia, Aplastic/
18. exp Bone Marrow Diseases/
19. exp Thrombocytopenia/
20. (thrombocytopeni* or thrombocytopaeni* or leukemi* or leukaemi* or lymphom* or myelodysplas* or myeloproliferat* or myelom* or plasm??ytom*).tw,kf,ot.
21. (lymphogranulomato* or histiocy* or granulom* or thrombocythemi* or thrombocythaemi* or polycythemi* or polycythaemi* or myelofibros* or AML or CLL or CML or Hodgkin* or nonhodgkin* or reticulosis or reticulosarcom* or MDS or RAEB or RAEB‐t).tw,kf,ot.
22. ((aplastic or refractory) adj an?emi*).tw,kf,t.
23. ((burkitt* adj (lymph* or tumo?r)) or lymphosarcom* or brill‐symmer* or sezary).tw,kf,ot.
24. ((haematolog* or hematolog* or blood or red cell* or white cell* or lymph* or marrow or platelet*) adj3 (malignan* or oncolog* or cancer* or neoplasm* or carcinoma*)).tw,kf,ot.
25. exp Antineoplastic Agents/ or exp Remission Induction/ or exp Antineoplastic Protocols/
26. exp Stem Cell Transplantation/ or Bone Marrow Transplantation/ or exp Radiotherapy/
27. exp Lymphatic Irradiation/
28. (chemotherap* or antineoplast* or anti‐neoplast* or radiotherap* or radio‐therap* or chemoradiotherap* or chemo‐radiotherap* or stem cell* or progenitor cell* or (bone marrow adj2 (transplant* or graft* or engraft* or rescu*))).tw,kf,ot.
29. (ASCT or ABMT or PBPC or PBSCT or PSCT or BMT or SCT or HSCT).tw,kf,ot.
30. ((h?ematolog* or h?ematooncolog* or h?emato‐oncolog*) adj3 patients).tw,kf,ot.
31. (h?ematooncolog* or h?emato‐oncolog*).ti.
32. or/14‐3133. exp Remission Induction/ 34. exp Antineoplastic Protocols/
35. ((consolidat* or induct* or maintenance or conditioning*) adj6 (therap* or treat* or regimen* or patient*)).tw,kf,ot. 36. ((therap* or induc*) adj3 remission*).tw,kf,ot.
37. ((cytosta* or cytotox*) adj2 (therap* or treat* or regimen*)).tw,kf,ot.
38. ((multimodal* or multi‐modal*) adj3 (treat* or therap*)).tw,kf,ot. 39. (combi* adj3 modalit*).tw,kf,ot.
40. or/33‐39
41. Transplantation Conditioning/
42. mini‐tra?splant*.tw.
43. exp Transplantation, Homologous/
44. (allograft* or allo‐graft* or allotransplant* or allo‐transplant* or ((allogen* or allo‐gen*) adj5 (transplant* or trasplant* or graft* or rescue*)) or homograft* or homo‐graft* or homolog* or homotransplant* or homo‐transplant* or homotrasplant* or homo‐trasplant*).tw,kf,ot.
45. Transplantation, Autologous/
46. (autograft* or auto‐graft* or autotransplant* or auto‐transplant* or autotra?splant* or auto‐tra?splant* or (autolog* adj5 (transplant* or graft* or trasplant* or rescue*))).tw,kf,ot.
47. or/41‐46
48. 32 or 40 or 47
49. 13 and 48
50. (201312* or 2014* or 2015*).dc,ed. or ("2013" or "2014" or "2015" or "2016").yr.
51. 49 and 5
Appendix 3. Embase (Ovid) search strategy on the 15 June 2016
1. *Blood Transfusion/
2. Blood Component Therapy/
3. Erythrocyte Transfusion/
4. ((erythrocyte* or red blood cell* or red cell* or blood or RBC*) adj5 (transfus* or unit*)).tw,kf.
5. ((red cell* or RBC* or erythrocyte* or red blood cell* or whole blood or transfus*) adj3 (trigger* or level* or threshold* or rule* or target* or restrict* or liberal* or reduc* or limit*)).tw,kf.
6. (allogeneic blood or (unit* adj2 blood) or allogenic blood or (blood adj2 exposure) or donor blood or blood product* or blood component* or blood support).tw,kf.
7. (h?emotransfus* or h?emotherap* or hypertransfus*).tw,kf.
8. (transfus* or red cell* or red blood cell* or RBC* or whole blood).ti.
9. or/1‐8
10. Hematologic Malignancy/
11. Lymphoma/
12. NonHodgkin Lymphoma/
13. Hodgkin Disease/
14. exp Myeloproliferative Disorder/
15. exp Aplastic Anemia/
16. exp Thrombocytopenia/
17. (thrombocytopeni* or thrombocytopaeni* or leukemi* or leukaemi* or lymphom* or aplast* anemi* or aplast* anaemi* or myelodysplas* or myeloproliferat* or myelom* or plasm??ytom*).tw,kf,ot.
18. (lymphogranulomato* or histiocy* or granulom* or thrombocythemi* or thrombocythaemi* or polycythemi* or polycythaemi* or myelofibros* or AML or CLL or CML or Hodgkin* or nonhodgkin* or reticulosis or reticulosarcom* or MDS or RAEB or RAEB‐t).tw,kf,ot.
19. ((burkitt* adj (lymph* or tumo?r)) or lymphosarcom* or brill‐symmer* or sezary).tw,kf,ot.
20. ((haematolog* or hematolog* or blood or red cell* or white cell* or lymph* or marrow or platelet*) adj3 (malignan* or oncolog* or cancer* or neoplasm* or carcinoma*)).tw,kf,ot.
21. exp Stem Cell Transplantation/
22. exp Bone Marrow Transplantation/
23. exp Chemotherapy/
24. exp Radiotherapy/
25. exp Antineoplastic Agent/
26. exp Immunosuppressive Treatment/
27. Remission/
28. (chemotherap* or antineoplast* or anti‐neoplast* or radiotherap* or radio‐therap* or chemoradiotherap* or chemo‐radiotherap* or stem cell* or progenitor cell* or (bone marrow adj2 (transplant* or graft* or engraft* or rescu*))).tw,kf,ot.
29. (ASCT or ABMT or PBPC or PBSCT or PSCT or BMT or SCT or HSCT).tw,kf,ot.
30. ((haematolog* or hematolog* or haemato‐oncolog* or hemato‐oncolog*) adj2 patients).tw,kf,ot.
31. (malignan* or oncolog* or cancer*).ti.
32. ((consolidat* or induct* or maintenance or conditioning*) adj6 (therap* or treat* or regimen* or patient*)).tw,kf,ot.
33. ((therap* or induc*) adj3 remission*).tw,kf,ot.
34. ((cytosta* or cytotox*) adj2 (therap* or treat* or regimen*)).tw,kf,ot.
35. ((multimodal* or multi‐modal*) adj3 (treat* or therap*)).tw,kf,ot.
36. (combi* adj3 modalit*).tw,kf,ot.
37. Allotransplantation/
38. Autotransplantation/
39. mini‐tra?splant$.tw.
40. (allograft* or allo‐graft* or allotransplant* or allo‐transplant* or ((allogen* or allo‐gen*) adj5 (transplant* or trasplant* or graft* or rescue*)) or homograft* or homo‐graft* or homolog* or homotransplant* or homo‐transplant* or homotrasplant* or homo‐trasplant*).tw,kf,ot.
41. (autograft* or auto‐graft* or autotransplant* or auto‐transplant* or autotra?splant* or auto‐tra?splant* or (autolog* adj5 (transplant* or graft* or trasplant* or rescue*))).tw,kf,ot.
42. or/10‐41
43. 9 and 42
44. limit 43 to dd=20131201‐20151105
Appendix 4. CINAHL (EBSCOhost) search strategy on the 15 June 2016
S1 (MH "Hematologic Neoplasms+")
S2 (MH "Leukemia+")
S3 (MH "Lymphoma+")
S4 (MH "Multiple Myeloma")
S5 TI ( leukemi* or leukaemi* or lymphoma* or myeloma* or plasmacytoma or plasma cell dyscrasia or AML or CLL or CML or Hodgkin* or haematolymphoid* or hematolymphoid* ) OR AB ( leukemi* or leukaemi* or lymphoma* or myeloma* or plasma cell dyscrasia or AML or CLL or CML or Hodgkin* or haematolymphoid* or hematolymphoid* )
S6 TI ( (haematoncolog* or hematoncolog* or haemato‐oncolog* or hemato‐oncolog*) N5 patient* ) OR AB ( (haematoncolog* or hematoncolog* or haemato‐oncolog* or hemato‐oncolog*) N5 patient* )
S7 (MH "Myelodysplastic Syndromes")
S8 myelodysplas* or "bone marrow dysplasia" or preleukemi* or preleukaemi* or dysmyelopoietic or dysmyelopoiesis
S9 refractory N2 (anemia or anaemia)
S10 MDS or RAEB or RAEB‐t
S11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10
S12 (MH "Blood Transfusion")
S13 (MH "Blood Component Transfusion")
S14 (MH "Erythrocyte Transfusion")
S15 (erythrocyte* or red cell* or red blood cell* or RBC*) N5 (transfus* or unit*)
S16 (transfus* or erythrocyte* or red cell* or red blood cell* or RBC*) N5 (trigger* or level* or target* or threshold* or rule* or restrict* or liberal*)
S17 red cell* management or red cell* sparing or red cell* support or red cell* strategy
S18 (red cell* N2 reduc*) or (red cell* N3 requirement*)
S19 hemotransfus* or haemotransfus* or hemotherap* or haemotherap*
S20 TI (red cell* or red blood cell* or erythrocyte* or RBC* or blood)
S21 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20
S22 S11 AND S21
Appendix 5. PubMed search strategy (epublications only) on the 15 June 2016
#1 (((erythrocyte*[TI] OR blood[TI]) AND (unit*[TI] AND trigger*[TI] OR level*[TI] OR threshold*[TI] OR rule*[TI] OR target*[TI] OR restrict*[TI] OR liberal*[TI] OR requir*[TI] OR reduc*[TI] OR limit*[TI])) OR (hemotransfus*[TI] OR haemotransfus*[TI] OR hemotherap*[TI] OR haemotherap*[TI] OR "red cell*"[TI] OR "red blood cell*"[TI] OR RBC*[TI] OR transfus*[TI]))
#2 ((random* OR blind* OR "control group" OR placebo* OR controlled OR cohort* OR nonrandom* OR observational OR retrospective* OR prospective* OR comparative OR comparator OR groups OR trial* OR "systematic review" OR "meta‐analysis" OR metaanalysis OR "literature search" OR medline OR cochrane OR embase) AND (publisher[sb] OR inprocess[sb] OR pubmednotmedline[sb]))
#3 (thrombocytopeni*[TI] OR thrombocytopaeni*[TI] OR leukemi*[TI] OR leukaemi*[TI] OR lymphom*[TI] OR "aplastic anemia"[TI] OR "aplastic anaemia"[TI] OR myelodysplas*[TI] OR myeloproliferat*[TI] OR myeloma[TI] OR lymphogranulomato*[TI] OR histiocy*[TI] OR granulom*[TI] OR thrombocythemi*[TI] OR thrombocythaemi*[TI] OR polycythemi*[TI] OR polycythaemi*[TI] OR myelofibros*[TI] OR AML[TI] OR CLL[TI] OR CML[TI] OR Hodgkin*[TI] OR burkitt*[TI] OR lymphosarcom*[TI] OR brill‐symmer*[TI] OR sezary[TI] OR ((haematolog*[TI] OR hematolog*[TI] OR blood[TI] OR red cell*[TI] OR white cell*[TI] OR marrow[TI] OR platelet*[TI]) AND (malignan*[TI] OR oncolog*[TI] OR cancer*[TI] OR neoplasm*[TI] OR carcinoma*[TI])) OR chemotherap*[TI] OR radiotherap*[TI] OR chemoradiotherap*[TI] OR "stem cell"[TI] OR "stem cells" OR "progenitor cell"[TI] OR "progenitor cells"[TI] OR bone marrow transplant*[TI] OR bone marrow graft*[TI] OR "bone marrow rescue"[TI] OR rituximab[TI] OR antineoplast*[TI] OR anti‐neoplast*[TI] OR ASCT[TI] OR ABMT[TI] OR PBPC[TI] OR PBSCT[TI] OR PSCT[TI] OR BMT[TI] OR SCT[TI] OR HSCT[TI] OR "haematology patients"[TI] OR "hematology patients"[TI] OR "haematological patients"[TI] OR "hematological patients"[TI] OR "hemato‐oncology patients"[TI] OR "haemato‐oncology patients"[TI] OR remission[TI] OR ((consolidat*[TI] OR induct*[TI] OR maintenance[TI] OR conditioning*[TI]) AND (therap*[TI] OR treat*[TI] OR regimen*[TI] OR patient*[TI])) OR ((cytosta*[TI] OR cytotox*[TI]) AND (therap*[TI] OR treat*[TI] OR regimen*[TI])) OR ((multimodal*[TI] OR multi‐modal*[TI]) AND (treat*[TI] OR therap*[TI])) OR (combi*[TI] AND modalit*[TI]) OR (allograft*[TI] OR allo‐graft*[TI] OR allotransplant*[TI] OR allo‐transplant*[TI] OR ((allogen*[TI] OR allo‐gen*[TI]) AND (transplant*[TI] OR trasplant*[TI] OR graft*[TI] OR rescue*)) AND TI OR homograft*[TI] OR homo‐graft*[TI] OR homolog*[TI] OR homotransplant*[TI] OR homo‐transplant*[TI] OR homotrasplant*[TI] OR homo‐trasplant*[TI]) OR (autograft*[TI] OR auto‐graft*[TI] OR autotransplant*[TI] OR auto‐transplant*[TI] OR mini‐transplant*[TI]) OR (autolog*[TI] AND (transplant*[TI] OR graft*[TI] OR trasplant*[TI] OR rescu*[TI]))
#4 #1 AND #2 AND #3
Appendix 6. Transfusion Evidence Library on the 15 June 2016
Clinical Specialty: Haematology, Malignant
Subject Area: Red Cells
Appendix 7. LILACS search strategy on the 15 June 2016
db:("LILACS") AND type_of_study:("cohort" OR "clinical_trials" OR "case_control" OR "systematic_reviews") AND ((leukemi* OR leukaemi* OR lymphoma* OR myeloma* OR plasmacytoma OR plasma cell dyscrasia OR AML OR CLL OR CML OR Hodgkin* OR haematolymphoid* OR hematolymphoid* OR haematolog* OR hematolog* OR ((haematopoietic OR hematopoietic) AND (malignan* OR oncolog* OR cancer* OR neoplas*)) OR haematooncolog* OR hematooncolog* OR haemato‐oncolog* OR hemato‐oncolog* OR myelodysplas* OR bone marrow OR stem cell* OR preleukemi* OR preleukaemi* OR dysmyelopoietic OR dysmyelopoiesis OR refractory anemia OR refractory anaemia OR MDS OR RAEB*) AND (transfus* OR ((erythrocyte* OR red cell* OR red blood cell* OR RBC*) AND (unit* OR trigger* OR level* OR target* OR threshold* OR rule* OR restrict* OR liberal* OR requir* OR reduc* OR limit*)) OR hemotransfus* OR haemotransfus* OR hemotherap* OR haemotherap*))
Appendix 8. INDMED search strategy on the 15 June 2016
(leukemia OR leukaemia OR lymphoma OR myeloma OR plasmacytoma OR Hodgkin OR haematolymphoid OR hematolymphoid OR haematology OR hematology OR myelodysplasia OR marrow OR stem cell OR preleukemia OR preleukaemia OR dysmyelopoietic OR dysmyelopoiesis) AND (transfusion OR red cells OR red blood cells OR RBC OR RBCs OR hemotransfusion OR haemotransfusion OR hemotherapy OR haemotherapy OR hypertransfusion) AND (randomized OR randomised OR randomly OR blind OR blinded OR trial OR cohort OR observational OR control OR controlled OR groups)OR((haematopoietic OR hematopoietic OR haematological OR hematological) AND (malignancyOR oncology OR cancer OR neoplasm)) AND (transfusion OR red cells OR red blood cells OR RBC OR RBCs OR hemotransfusion OR haemotransfusion OR hemotherapy OR haemotherapy OR hypertransfusion) AND (randomized OR randomised OR randomly OR blind OR blinded OR trial OR cohort OR observational OR control OR controlled OR groups)
Appendix 9. KOREAMED search strategy on the 15 June 2016
Limits: ("Clinical Trial" [PT] OR "Comparative Study" [PT] OR "Evaluation Studies" [PT] OR "Meeting Abstract" [PT] OR "Meta‐Analysis" [PT] OR "Multicenter Study" [PT] OR "Practice Guideline" [PT] OR "Randomized Controlled Trial" [PT] OR "Review" [PT] ) AND "Blood Transfusion" [MH] OR transfus* [TI] OR "red cell*" [TI] OR "red blood cell*" [TI
Appendix 10. Web of Science (CPCI‐S) search strategy on the 15 June 2016
#1 TI=(leukemi* OR leukaemi* OR lymphoma* OR myeloma* OR plasmacytoma OR "plasma cell dyscrasia" OR AML OR CLL OR CML OR Hodgkin* OR haematolymphoid* OR hematolymphoid* OR haematolog* OR hematolog* OR haematooncolog* OR hematooncolog* OR haemato‐oncolog* OR hemato‐oncolog* OR myelodysplas* OR "bone marrow" OR "stem cell" OR "stem cells" OR preleukemi* OR preleukaemi* OR dysmyelopoietic OR dysmyelopoiesis OR "refractory anemia" OR "refractory anaemia" OR MDS OR RAEB*) OR TS=(leukemi* OR leukaemi* OR lymphoma* OR myeloma* OR plasmacytoma OR "plasma cell dyscrasia" OR AML OR CLL OR CML OR Hodgkin* OR haematolymphoid* OR hematolymphoid* OR haematolog* OR hematolog* OR haematooncolog* OR hematooncolog* OR haemato‐oncolog* OR hemato‐oncolog* OR myelodysplas* OR "bone marrow" OR "stem cell" OR "stem cells" OR preleukemi* OR preleukaemi* OR dysmyelopoietic OR dysmyelopoiesis OR "refractory anemia" OR "refractory anaemia" OR MDS OR RAEB*)
#2 TI=((haematopoietic OR hematopoietic) AND (malignan* OR oncolog* OR cancer* OR neoplas*)) OR TS=((haematopoietic OR hematopoietic) AND (malignan* OR oncolog* OR cancer* OR neoplas*))
#3 #1 OR #2
#4 TI=(erythrocytes OR red cells OR red blood cells OR RBCs OR transfus* OR hemotransfus* OR haemotransfus* OR hemotherap* OR haemotherap*) OR TS=(erythrocytes OR red cells OR red blood cells OR RBCs OR transfus* OR hemotransfus* OR haemotransfus* OR hemotherap* OR haemotherap*)
#5 TI=(randomi* OR blind* OR trial OR cohort* OR observational* OR control* OR groups) OR TS=(randomi* OR blind* OR trial OR cohort* OR observational* OR control* OR groups)
#6 #3 AND #4 AND #5
)
#9 #7 AND #8
Appendix 11. ClinicalTrials.gov search strategy on the 15 June 2016
Study Type: All
Conditions: blood cancers OR hematological OR nonhodgkin OR leukemia OR lymphoma OR myeloma OR plasmacytoma OR Hodgkin OR haematolymphoid OR hematolymphoid OR myelodysplasia OR preleukemia OR dysmyelopoietic OR dysmyelopoiesis OR "refractory anemia" OR aplastic
Interventions: "red cell transfusion" OR "blood transfusion" OR "red cells" OR RBCs OR "red blood cells"
OR Search Terms: stem cell transplantation OR stem cells OR bone marrow transplantation OR blood cancers OR hematological OR nonhodgkin OR leukemia OR lymphoma OR myeloma OR plasmacytoma OR Hodgkin OR haematolymphoid OR hematolymphoid OR myelodysplasia OR preleukemia OR dysmyelopoietic OR dysmyelopoiesis OR "refractory anemia" OR aplastic Study
Type: All Interventions: "red cell transfusion" OR "blood transfusion" OR "red cells" OR RBCs OR "red blood cells"
Appendix 12. ISRCTN search strategy on the 15 June 2016
("red cell transfusion" OR "blood transfusion" OR "red blood cell transfusion") AND (leukemia OR leukaemia OR lymphoma OR myeloma OR plasmacytoma OR Hodgkin OR haematolymphoid OR hematolymphoid OR haematology OR hematology OR myelodysplasia)
Appendix 13. WHO ICTRP search strategy on the 15 June 2016
Title OR interventions: transfusion OR red cells OR red blood cells OR RBCs
Conditions: blood cancers OR haematological OR nonhodgkin OR leukemia OR lymphoma OR myeloma OR plasmacytoma OR Hodgkin OR haematolymphoid OR hematolymphoid OR myelodysplasia OR preleukemia OR dysmyelopoietic OR dysmyelopoiesis OR refractory anemia OR aplastic anemia
Recruitment Status: ALL
Appendix 14. EUDRACT search strategy on the 15 June 2016
(transfusion OR red cell OR red blood cell) AND (leukemia OR lymphoma OR myeloma OR hematology OR haematology OR haematological OR haematological OR plasmacytoma OR Hodgkin OR haematolymphoid OR hematolymphoid OR myelodysplasia OR preleukemia OR dysmyelopoietic OR dysmyelopoiesis OR refractory anemia)

Study flow diagram for study selection

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 1 All‐cause mortality‐at 31 to 100 days.

Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 2 Mortality due to chemotherapy.

Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 3 Number of participants with any bleeding.
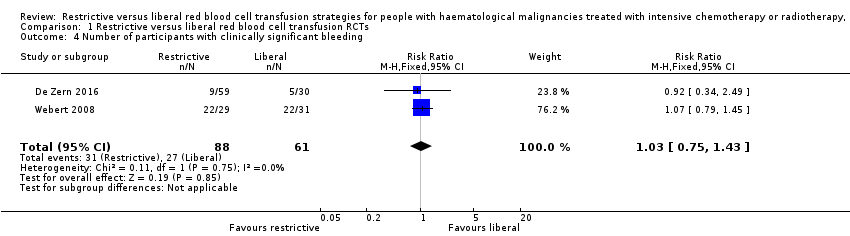
Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 4 Number of participants with clinically significant bleeding.
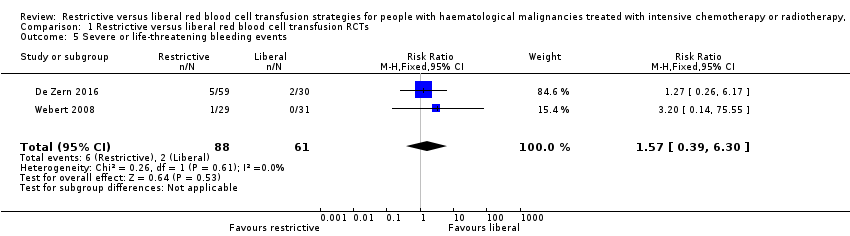
Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 5 Severe or life‐threatening bleeding events.

Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 6 Number of participants with serious infection episodes.

Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 7 Number of participants with VOD.
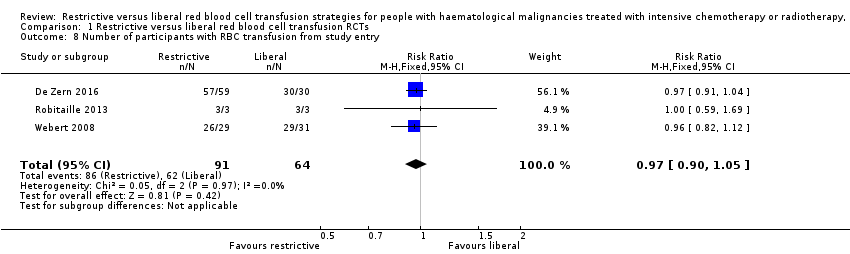
Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 8 Number of participants with RBC transfusion from study entry.
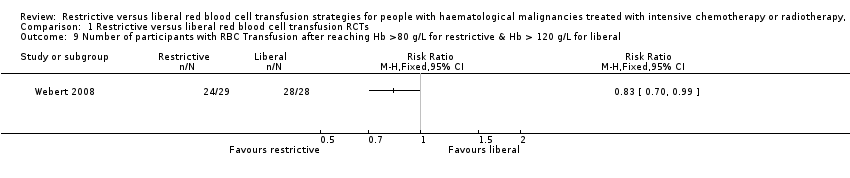
Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 9 Number of participants with RBC Transfusion after reaching Hb >80 g/L for restrictive & Hb > 120 g/L for liberal.
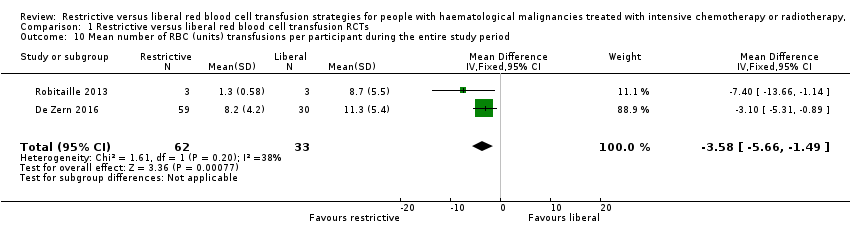
Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 10 Mean number of RBC (units) transfusions per participant during the entire study period.
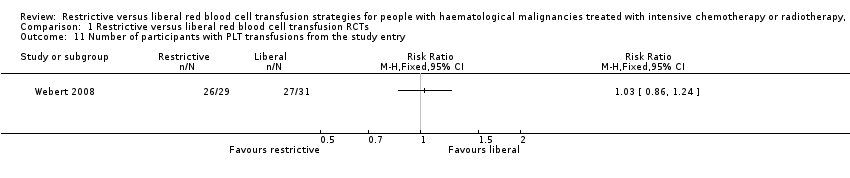
Comparison 1 Restrictive versus liberal red blood cell transfusion RCTs, Outcome 11 Number of participants with PLT transfusions from the study entry.
| Restrictive compared with liberal for people with haematological malignancies treated with intensive chemotherapy or radiotherapy, or both, with or without haematopoietic stem cell support | ||||||
| Patient or population: people with haematological malignancies treated with intensive chemotherapy or radiotherapy, or both, with or without haematopoietic stem cell support | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Risk with liberal red blood cell transfusion RCTs | Risk with Restrictive | |||||
| All‐cause mortality at 31 to 100 days | Study population 61 per 1000 | 15 per 1000 (1 to 163) | RR 0.25 (0.02 to 2.69) | 95 (2 RCTs) | ⊕⊕⊝⊝ LOW1 | |
| Quality of life | Liberal group: median 4.5 (IQR: 3.6 to 5) Restrictive: median 4.8 (IQR: 4 to 5.2)a | 89 (1 RCT) | ⊕⊕⊝⊝ VERY LOW2,3,4 | |||
| Number of participants with any bleeding | Study population 639 per 1,000 | 595 per 1000 | RR 0.93 | 149 | ⊕⊕⊝⊝ | |
| Number of participants with clinically significant bleeding | Study population 443 per 1,000 | 456 per 1000 | RR 1.03 | 149 | ⊕⊕⊝⊝ | |
| Serious infections | Study population 400 per 1,000 | 492 per 1000 (296 to 816) | RR 1.23 | 89 (1 RCT) | ⊕⊝⊝⊝ VERY LOW2,3,4 | |
| Length of hospital admission (days) | Liberal: median 36 days (IQR: 29.2 to 44) Restrictive: median: 35.5 days (IQR: 31.2 to 43.8) | 89 (1 RCT) | ⊕⊕⊝⊝ LOW2,3 | |||
| Hospital readmission rate ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1The level of evidence was downgraded by 2 due to imprecision. aThis is a ten‐point scale with a score of zero indicating no fatigue and a score of ten indicating the worst possible fatigue. The median fatigue scare was similar for both groups; P = 0.53. Interquartile range: IQR | ||||||
| Restrictive compared with liberal for people with haematological malignancies treated with intensive chemotherapy or radiotherapy, or both, with or without haematopoietic stem cell support | ||||||
| Patient or population: people with haematological malignancies treated with intensive chemotherapy or radiotherapy, or both, with or without haematopoietic stem cell support | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Risk with liberal red blood cell transfusion RCTs | Risk with Restrictive | |||||
| All‐cause mortality at 31 to 100 days | Liberal: 1 death (46 participants) Restrictive: 1 death (38 participants) | 84 | ⊕⊝⊝⊝ | Mean 31 days follow‐up | ||
| Quality of life ‐ not reported | ‐ | ‐ | ‐ | ‐ | ||
| Number of participants with any bleeding ‐ not reported | ‐ | ‐ | ‐ | ‐ | ||
| Number of participants with clinically significant bleeding | Liberal: 8 (46 participants) Restrictive: 3 (38 participants) | 84 | ⊕⊝⊝⊝ | The study authors reported that there was no significant difference between the two groups. | ||
| Serious infections ‐ not reported | ‐ | ‐ | ‐ | ‐ | ||
| Length of hospital admission ‐ not reported | ‐ | ‐ | ‐ | ‐ | ||
| Hospital readmission rate ‐ not reported | ‐ | ‐ | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1The level of evidence was downgraded by 1 due to imprecision. | ||||||
| Transfusion Risk | Frequency in the UK (units transfused) ( Bolton‐Maggs 2014) | Frequency in low income countries ( WHO 2015 ) |
| ABO incompatible red cell transfusion | 3.7 in 1 million (10 cases per 2663488 transfusions) | unknown |
| Transfusion‐related acute lung injury | 0.4 in 1 million (10 cases per 2663488 transfusions) | unknown |
| Transfusion associated circulatory overload | 34.1 in 1 million (91 cases per 2663488 transfusions) | unknown |
| Transfusion transmitted infection | Frequency in high income countries | Frequency in low income countries |
| HIV | 2 in 100,000 (IQR 0.4 in 100,000 to 20 in 100,000) | 850 in 100,000 (IQR 480 in 100,000 to 2000 in 100,000) |
| HBV | 20 in 100,000 (IQR 8 in 100,000 to 24 in 100,000) | 3590 in 100,000 (IQR 2010 in 100,000 to 6080 in 100,000) |
| HCV | 20 in 100,000 (IQR 0.4 in 100,000 to 22 in 100,000) | 1070 in 100,000 (IQR 630 in 100,000 to 1690 in 100,000) |
| IQR=interquartile range | ||
| Risk of Bias | Assessment | Support for judgement |
| Selection (one star each, maximum four stars) | 2 stars | |
| Representativeness of the exposed cohort | 0 stars | This study only included participants with AML as opposed to all patients with haematological malignancies |
| Selection of the non‐exposed cohort | 0 star | Participants in the control were from a second haematology centre, but there was no information to reassure that this cohort was drawn from the same community as exposed cohort |
| Ascertainment of exposure | 1 star | Secondary analyses from HOVON 29, prospective randomised controlled trial |
| Demonstration that outcome of interest was not present at start of study | 1 stars | The primary outcome and other outcomes were defined and were based on events that occurred after the study started |
| Comparability of cohort on design and analyses (maximum of two stars) Recognition of at least 75% of the main potential confounding factors (2 stars) Recognition of 50% to 75% of the main potential confounding factors (1 star) | 0 stars | < 50% of potential cofounders considered and sex, age and AML type were adjusted for in the multiple regression model. There was no discussion on previous severe bleeding, use of anticoagulation, use of radiotherapy in addition to chemotherapy, previous cardiovascular disease, previous alloimmunisation or performance status |
| Outcome (one star each, maximum of four stars) | 2 stars | |
| Assessment of outcome | 0 stars | Not described |
| Was follow‐up long enough for outcomes to occur? | 1 star | Yes, 31 days from chemotherapy |
| Adequacy of follow‐up of cohorts | 0 star | Reported for all, except unclear for infection, mean Hb during follow‐up, total number of platelet/red blood cell units received |
| Follow‐up equal between groups for primary and secondary outcomes? | 1 star | Follow‐up not significantly different |
| Additional concerns | None | |
| Overall assessment | 4 stars | |
| AML = acute myeloid leukaemia | ||
| Study | No. of participants received RBC transfusion during the study period | Mean no. RBC units transfusions/participant during study period | Number of participant‐days with RBC transfusions | Proportion of participant‐days with RBC transfusions | Mean Hb within first +100 days: | Number of RBC units per transfusion | Interval between RBC transfusions (mean) (days) |
| RCTs | |||||||
| Restrictive: 57/59 Liberal: 30/30 | Restrictive: mean 8.2 (SD 4.2) Liberal: mean 11.3 (SD 5.4) | NR | NR | Restrictive: mean 33.6 (SD 1.4) Liberal: mean 33.2 (SD 2.0) | NR | NR | |
| Restrictive: 3/3 Liberal: 3/3 | Restrictive: (mean 1.3 [SD 0.58]; median 1 [range 1 to 2; SE 0.33]) Liberal: (mean 8.7 [SD 5.5]; median 9 [range 3 to 14; SE 3.2]) | NR | NR | Restrictive: [mean pre transfusion Hb 69 g/L (range 69 g/L to 70 g/L) no SD] Liberal: [mean pre transfusion Hb 106 g/L (range 118 g/L to 132 g/L) no SD] | NR | NR | |
| Restrictive: 26/29 (24/29 from when Hb ≥80 g/L) Liberal: 29/31 (28/28 from when Hb ≥ 120g/L) | NR | Restrictive: 75 (70/467 days of observation once reached target Hb) Liberal: 113 g/L (72/410 days of observation once reached target Hb) | Restrictive: 0.151 (0.150 after study Hb threshold reached) Liberal: 0.233 (0.176 after study Hb threshold reached) [RR 1.56; 95% CI 1.16 to 2.10] [RR 1.18: 95% CI 0.90 to 1.54; once study Hb threshold reached]a | NR | NR | NR | |
| NRS | |||||||
| NR | Restrictive: mean 9.6 (SD 3.9); Median 9 (SE 0.6); Range 3 to 21 Liberal: mean 10.8 (SD 2.9); Median 11.0 (SE 0.4); Range 6 to 21 | NR | NR | Restrictive: Age < 25 Hb 7.5 (n = 3); 25‐50 yrs Hb 8.0 (n = 22); Age 50‐70 years Hb 8.3 (n = 13) Liberal: Age < 25 years Hb 8.8 (n = 3); 25‐50 years Hb 9.3 (n = 32); 50‐70 years Hb 9.5 (n = 11) | Restrictive: Mean 1.3 (SD 0.5); Median 1.0 (SE 0.03); range 1‐4 Liberal: Mean 1.82 (SD 0.4); Median 2 (SE 0.03); Range 1‐5 | Restrictive: 3.1 days (No SD) Liberal: 3 days (No SD) | |
| CI = confidence interval Trial HB: Restrictive ≥ 80g/L and Liberal ≥ 120g/L aData analysed by study authors, reported as relative risks derived from adjusted Cox regression models, allowing for repeated measures. | |||||||
| Study ID | Number of PLTs transfused per participant | Number of participant‐days with PLT transfusions | Proportion of participant‐days with RBC transfusions | Interval between PLT transfusions (mean & SD)(days) | Number of PLT units per transfusion (mean & SD) (units) | Nmber of PLT transfusion per participant |
| RCTs | ||||||
| NR | NR | NR | NR | NR | Restrictive: median:9 (IQR: 5.5 to 12.5) Liberal; median: 9 (IQR: 7 to 12) | |
| NR | NR | NR | NR | NR | NR | |
| Restrictive: 26/29 from study entry, 26 from when target Hb reached Liberal: 27/31 from study entry; 26 from when target Hb reached | Restrictive: 124 from study entry; 122 from Hb 80 g/L to 100 g/L Liberal: 0.265 from study entry; 0.283 from when Hb > 120 g/L | Restrictive: 0.249 from study entry; 0.261 from when Hb 8‐10 Liberal: 0.265 from study entry; 0.283 from when Hb > 12 [RR 1.06; 95% CI 0.74 to 1.52] [RR 1.02: 95% CI 0.73 to 1.44; once study Hb threshold reached]a | NR | NR | NR | |
| NRS | ||||||
| Restrictive: Mean 7.5 (SD 3.8); median 7 (SE 0.6); range 2 to 18 Liberal: Mean 8.5 (SD 4.9); median 7 (SE 0.7); range 2 to 30 P > 0.05 | NR | NR | Restrictive: 4 days (No SD) Liberal: 3.8 days (No SD) | Restrictive: Mean 1.1 (SD 0.4); median 1 (SE 0.03); range 1 to 4 Liberal: Mean 1.2 (SD 0.5); Median 1 (SE 0.03); range 1 to 4 | NR | |
| aData analysed by study authors, reported as relative risks derived from Cox regression models. IQR = Interquartile range | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All‐cause mortality‐at 31 to 100 days Show forest plot | 2 | 95 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.02, 2.69] |
| 2 Mortality due to chemotherapy Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Number of participants with any bleeding Show forest plot | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.73, 1.18] |
| 4 Number of participants with clinically significant bleeding Show forest plot | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.75, 1.43] |
| 5 Severe or life‐threatening bleeding events Show forest plot | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.39, 6.30] |
| 6 Number of participants with serious infection episodes Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Number of participants with VOD Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected | |
| 8 Number of participants with RBC transfusion from study entry Show forest plot | 3 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.90, 1.05] |
| 9 Number of participants with RBC Transfusion after reaching Hb >80 g/L for restrictive & Hb > 120 g/L for liberal Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10 Mean number of RBC (units) transfusions per participant during the entire study period Show forest plot | 2 | 95 | Mean Difference (IV, Fixed, 95% CI) | ‐3.58 [‐5.66, ‐1.49] |
| 11 Number of participants with PLT transfusions from the study entry Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

