Estrategias para mejorar el uso de métodos anticonceptivos posparto: pruebas de estudios no aleatorios
References
References to studies included in this review
Jump to:
References to studies excluded from this review
Jump to:
Additional references
Jump to:
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Location and time frame: rural Upper Egypt (Assiut and Sohag); conducted December 2005 to May 2007. Design: 'Operations research study' within 2 regions with districts assigned to conditions. Described as post‐test panel with non‐equivalent control group. a) selected 2 regions (governorates) b) selected 3 health districts from each region and randomly assigned them to 1 of 3 conditions c) selected 5 rural clinics within each district; clinics with 30 prenatal care visits per month had priority Sample size calculation: To detect difference in contraceptive use at 12 months, 550 needed for each group (55 per clinic). Estimated baseline use 10%; minimal use increase 5%; alpha = 0.05, power 0.8, design effect 1.5, 10% loss to follow up. | |
| Participants | General with N: 1416 pregnant women attending clinic Source: rural clinics (of Ministry of Health and Population) Inclusion criteria: Third trimester (6 to 9 months), low parity (target group: 0 or 1 living child), seeking antenatal care. Exclusion criteria: not specified | |
| Interventions | Study focus: Birth‐spacing message models; effect on knowledge, attitudes, and contraceptive use. Treatment 1: Health services model (HSM): birth spacing messages communicated through services by health workers to women during prenatal and postpartum periods. Included effective use of lactational amenorrhea method (LAM). Educational materials were also used (information, education, and communication (IEC)). Treatment 2: Community awareness model (CAM): communicating messages in HSM plus awareness component through community 'influentials' trained to communicate messages to men. Comparison or control: standard care (unspecified) plus awareness component (IEC) in CAM. | |
| Outcomes | Primary: contraceptive use; use of LAM (4 months postpartum only) Secondary: knowledge of LAM (LAM users only; at 4 months only) Assessment times: Home interviews at 4 months and at 10 to 12 months postpartum. Note: Attitudes about birth spacing were assessed at clinic exit interviews only. Husband's attitudes were reported by women participants. | |
| Notes | Unable to obtain further information from investigator on randomization method or whether analysis accounted for clustering (14 May 2014). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Exposed cohort representativeness | High risk | Low‐parity women (0 or 1 living child) attending prenatal clinic in 1 of 3 health districts. In contrast, community 'influentials' had an average of 4 children. |
| Nonexposed cohort selection | Unclear risk | From same region but different health district than exposed cohort. |
| Exposure ascertainment: method used | Low risk | Checklists included FP services (prenatal, postpartum day 40 and home visits) Prenatal: clinic exit interview to assess services received. Postpartum: home interviews by community workers regarding services received. |
| Comparability of groups: design or analysis | Low risk | Design: From each of 2 regions, 3 health districts assigned to 1 of 3 conditions. Districts matched on socioeconomic characteristics (unspecified), birth rates, and contraceptive prevalence. Analysis: No mention of adjustment for potential confounding. Study groups differed in years married, educational level, and employment status. Study groups did not differ significantly for prior use of contraceptives, but method type was not reported. Analysis methods are limited for 2 clusters per study group. |
| Outcome assessment: method used | Unclear risk | Home interviews by community workers; self‐reported outcomes. |
| Follow‐up length | Low risk | 10 to 12 months |
| Follow‐up adequacy | Low risk | Completed 10‐ to 12‐month interview: > 99% of each group (HSM 546/550; CAM 479/481; control 384/385). |
| Methods | Location and time frame: Edgardo Rebagliati Martins National Hospital in Lima, largest hospital in system. Conducted July 1988 to September 1989. Design: Two maternity wards were randomly selected, one treatment and one control, with 1 cluster per group, Drew 4 subgroups randomly from each monthly cohort for assessment, treatment women and control women at 40 days or at 6 months after delivery. Sample size calculation: no information. | |
| Participants | General with N: 1560 women who gave birth at national hospital Inclusion criteria: no specifics Exclusion criteria: no information | |
| Interventions | Study focus: Increase contraceptive prevalence among postpartum women through family planning counseling and contraceptive provision; determine if intervention could reduce family planning program costs. Treatment: Family planning orientation and provision of contraceptive methods. IUD (TCu380A) inserted immediately after delivery or before discharge; barrier methods offered if no IUD inserted; OCs available if not planning to breast‐feed. Comparison or control: not offered comparable services; reportedly no intervention. | |
| Outcomes | Primary: contraceptive use; pregnancy (self report) Secondary: not applicable Assessment times: 40 days or 6 months after delivery (independent samples); interviewed at home. | |
| Notes | Excluded from analysis: 45 women (sterilized prior to discharge, no education or no living children, or older than 44 years, plus one potential coding error). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Exposed cohort representativeness | Unclear risk | Women who gave birth in a specific facility (access based on residential address); independent samples of women at 40 days and 6 months postpartum. Family planning services were more available in second 6 months of project. New chief doctor, appointed half‐way, was more supportive of postpartum approach. Interviewers gained experience in locating women, so 6‐month sample for experimental group was biased toward women who gave birth in first half of project, and 40‐day sample was biased toward those from second half. Reportedly, weighting samples did not alter comparability of social or demographic characteristics. |
| Nonexposed cohort selection | Low risk | Drawn from same community as exposed cohort; independent samples drawn at 40 days and 6 months postpartum. |
| Exposure ascertainment: method used | Low risk | Presumably study records; intervention provided in hospital. |
| Comparability of groups: design or analysis | High risk | No adjustments noted nor mention of potential confounding. 26 women excluded from analysis ('outliers' were those with no education or living children, or > 44 years). |
| Outcome assessment: method used | Unclear risk | Home interviews; self‐reported outcomes. |
| Follow‐up length | Low risk | 6 months |
| Follow‐up adequacy | High risk | Loss to follow up: 50% (1606 interviewed / 3200 selected); reportedly no difference between study groups. |
| Methods | Location and time frame: Instituto Materno‐Infantil de Pernambuco (IMIP) in city of Recife (Northeast Brazil); early 1990s. Design: 'Semi‐experimental operational study' with different time series for treatment and control. Sample size calculation (and outcome of focus): no information | |
| Participants | General with N: 698 women who gave birth at the institute (IMIP). Source: Teaching institution providing pediatric and obstetric care to low‐income women and children. Inclusion criteria: Treatment group comprised of first 348 women who delivered after intervention started, returned for 40‐day appointment, and volunteered for study. Control group gave birth at IMIP, received traditional counseling (prior to new intervention), and returned to hospital for regular check‐ups (1 year postpartum). Exclusion criteria: had stillbirth or twin pregnancy, would have difficulty breastfeeding, had surgical sterilization approved, or desired pregnancy soon. | |
| Interventions | Study focus: Introduce lactational amenorrhea method (LAM) to postpartum care Treatment: Provided during family planning (FP) counseling of women at prenatal care or those giving birth at IMIP. LAM introduced as contraceptive method during prenatal visits, in maternity hospital after birth, and on 8th‐day postpartum visit. Comparison or control: Traditional FP counseling prior to development of new intervention (did not include LAM); provided during prenatal care, hospitalization, and day 8 postpartum visit. | |
| Outcomes | Primary: contraceptive use by specific method (we also analyzed as modern or traditional (WHO 2013)); pregnancy (presumably self report; no mention of testing or use of records). Secondary: not applicable Assessment times: Treatment group at visits 3, 6, 9, and 12 months postpartum; Comparison group interviewed at one year postpartum only. | |
| Notes | Total Ns for table on contraceptive use were reversed for experimental and control groups (215 versus 350). All other results indicate experimental group had 215 women at 12 months. Control group consisted of 350 women interviewed at 12 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Exposed cohort representativeness | High risk | Gave birth at institution serving low‐income women and returned for 40‐day appointment. |
| Nonexposed cohort selection | High risk | Returned to hospital for regular check‐up at one‐year postpartum. |
| Exposure ascertainment: method used | High risk | Control: unclear whether records or recall of counseling received. Experimental: presumably program records of clinic encounters. |
| Comparability of groups: design or analysis | Low risk | Potential confounders in logistic regression: age, years of schooling, # living children, marital status. |
| Outcome assessment: method used | Unclear risk | Interview at clinic visits; self report |
| Follow‐up length | Low risk | 12 months |
| Follow‐up adequacy | High risk | Loss to follow up: experimental group at 12 months, 133/348 (38%); control interviewed at 12 months. |
| Methods | Location and time frame: conducted in medical center in Taiwan; no time frame specified. Design: Odd‐numbered wards were experimental group and even‐numbered wards were control group. Odd‐numbered wards were divided by 'another' coin flip into group A (wards 1, 3, 5, 7, 11) and B (wards 13, 15, 17, 19, 21, 23). Midway through study, wards chosen for group A were reversed. Ward rooms with double occupancy were assigned as a unit. Assignment reportedly adapted from Sayegh 1976. Sample size calculation (and outcome of focus): not specified | |
| Participants | General with N: 250 women who gave birth in medical center Source: 76‐bed postpartum wards of large medical center and local hospital. Inclusion criteria: delivered single, full‐term healthy baby (gestation age 38 to 42 weeks, body weight > 2500 g, and Apgar score > 8); admitted for < 3 days; no perinatal complications or major chronic illness; married and lived with husband; age 20 to 39 years and could read, write, and speak Chinese. Exclusion criteria: not specified. | |
| Interventions | Study focus: Evaluate effect of postpartum education program on knowledge, attitude, and contraceptive use. Treatment A: Interactive Postpartum Sexual Health Education Program (IPSHEP) included 'interactive pamphlet' plus sexual health education by trained obstetric nurse educator and opportunity for discussion. Treatment B: Interactive pamphlet in 'A' but no individual health education or opportunity for questions. Comparison or control: Routine postpartum education on sexual health included educational talk and pamphlet (same content and printing as in 'A' but no interactive design); staff not trained in interactive education for postpartum women. | |
| Outcomes | Primary: 'effective contraceptive behavior' assessed by effectiveness of method used most often at 2 and 3 months postpartum. Scored from 0 (no use) to 99 (more effective as per WHO definitions, i.e., very effective, moderately effective, less effective). Did not specify what score was used for each category of effectiveness. Secondary: sexual health knowledge and attitudes included contraceptive practice at 3 days and 2 months postpartum Assessment times: 2 and 3 months postpartum | |
| Notes | Unable to obtain further information from investigator on study design or data on contraceptive use by specific method. Routine education: standard deviation (SD) for 'contraceptive effectiveness' at 3 months may be misprint (8 versus 20 to 30 for others). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Exposed cohort representativeness | High risk | Women who gave birth at specific institution, delivered full‐term healthy baby, no complications or chronic disease, lived with husband. |
| Nonexposed cohort selection | Low risk | Same source as exposed cohort |
| Exposure ascertainment: method used | Low risk | Presumably study records; intervention was provided in hospital ward. |
| Comparability of groups: design or analysis | Unclear risk | Analyzed baseline characteristics. Study groups reportedly did not differ significantly except for delivery method (vaginal or cesarean); pretest values for outcomes reportedly did not differ by delivery method. Analysis did not account for assignment by groups, but only 3 groups. |
| Outcome assessment: method used | Unclear risk | Research assistant administered structured questionnaires (tests); self‐reported outcomes. |
| Follow‐up length | Low risk | 3 months |
| Follow‐up adequacy | High risk | Loss to follow up by 3 months: Treatment A 24% (17/70); Treatment B 37% (34/92); Standard care 34% (30/88) |
| Methods | Location and time frame: the Kayseri Maternal and Child Health Hospital, city of Kayseri, Turkey. Conducted from December 1999 to June 2000. Design: Allocation likely to have been alternate. Questionnaire about eligibility criteria was administered to intervention and control groups on alternate days. Intervention provided immediately after the questionnaire. Sample size calculation: 150 women in each group (300 total) to detect 20% increase of contraceptive prevalence (from 60% to 80%), accounting for possible loss to follow up. | |
| Participants | General with N: 260 women who delivered at Kayseri Hospital in December 1999 Exclusion criteria: not specified | |
| Interventions | Study focus: Effect of education on postpartum contraceptive use Treatment: 20‐minute educational session on postpartum family planning, lactation‐contraception relationship, and contraceptive options during this period. Each woman given brochure on 'Postpartum Family Planning.' Control: baseline questionnaire only | |
| Outcomes | Primary: Postpartum contraceptive use, reported as modern or traditional method. Modern (effective) included IUD, OCs, injectable contraceptives, implant (Norplant), tubal ligation, vasectomy, diaphragm and spermicides. Traditional (limited effectiveness) included withdrawal, calendar, and lactation methods. Secondary: not applicable Assessment times: follow up at 6 months. | |
| Notes | Article in Turkish; translation of table headings and study characteristics extracted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Exposed cohort representativeness | Unclear risk | Women who gave birth at specific hospital and could be contacted by telephone. |
| Nonexposed cohort selection | Low risk | Same source as exposed cohort |
| Exposure ascertainment: method used | Low risk | Presumably study records; intervention was provided in hospital |
| Comparability of groups: design or analysis | High risk | Analysis not adjusted for potential confounders. Prior contraceptive use reportedly differed between groups but not analysis not adjusted. |
| Outcome assessment: method used | Unclear risk | Questionnaire administered at clinic during return visit or in home; self‐reported outcome. Grouping of methods as modern (effective) or traditional was inconsistent with WHO 2013 categories. |
| Follow‐up length | Low risk | 6 months |
| Follow‐up adequacy | Low risk | Losses to follow up by 6 months: 8.7% treatment 8.7% (137/150); control 18% (123/150); |
| Methods | Location and time frame: rural areas of Meerut district in Uttar Pradesh (India); intervention from September 2006 to January 2007. Design: Evaluation study; described as 'randomized experimental pre‐ and post‐test design.' District had 12 blocks; randomly assigned 2 blocks to intervention and 2 to comparison. Selected 12 villages with population >= 2000 from each block for inclusion. Sample size calculation: Contraceptive prevalence rate of 10% among women aged <= 24 taken as base value. Needed 541 women in each arm to detect 5% increase in contraceptive use at 9 months postpartum. Estimated 600 to compensate for 10% loss to follow up. | |
| Participants | General with N: 959 women Source: Study villages Inclusion criteria: Had 0 or 1 child, < 25 years old, were 4 to 7 months pregnant. Exclusion criteria: first trimester, reportedly because they rarely mention pregnancy to community workers or go for antenatal care. | |
| Interventions | Study focus: Increase knowledge and use of lactational amenorrhea method (LAM) and postpartum contraception through counseling. Treatment: Educational campaign for enrolled pregnant women and mother‐in‐law or oldest female family member. Included healthy timing and spacing of pregnancy, LAM, postpartum contraception; provided in home. According to investigator, community workers continued with messages postpartum, during routine monthly home visits. Also contacted mothers‐in‐law during antenatal and postpartum periods about postpartum contraception. Intervention included an educational campaign for males in community about maternity care and postpartum contraception. Comparison or control: Government‐run health program (antenatal clinic; home‐based counseling of pregnant women and family about antenatal and postnatal care and family planning; preschool program workers also counseled pregnant and lactating women at home. | |
| Outcomes | Primary: modern contraceptive use; pregnancy (self report) Secondary: change in knowledge of healthy timing and spacing of pregnancy (>= 2 messages); change in knowledge of >=2 spacing methods available in national program. Assessment times: 9 months postpartum; knowledge also at 4 months postpartum. | |
| Notes | Investigator provided additional information about the intervention, including time frame for postpartum contact. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Exposed cohort representativeness | High risk | Low‐parity women (0 or 1 child), < 25years old, living in selected district, block, and village. In contrast, state fertility rate was 3.8. |
| Nonexposed cohort selection | Unclear risk | From same district but different block than that of the exposed (treatment) group. |
| Exposure ascertainment: method used | Low risk | Prenatal: presumably from clinic records of services provided. Postpartum: presumably from community workers' records of home visits and services provided. |
| Comparability of groups: design or analysis | Low risk | Potential confounders included in logistic regression models: study group, education, age, age at initiation of cohabitation, caste, parity. Analysis does not appear to account for assignment of groups. With 2 blocks per study group, analysis methods are limited. |
| Outcome assessment: method used | Unclear risk | Interviews conducted during home visits; self‐reported outcomes. |
| Follow‐up length | Low risk | 9 months |
| Follow‐up adequacy | High risk | Total loss: 20% (238/1197 did not complete all 3 interview rounds) |
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Insufficient outcome data for comparison group: assessed initiation of contraceptive method (from records) by the 30‐ to 40‐day postpartum visit. One‐year data on contraceptive use and pregnancy were available for only 10% of comparison group. | |
| No appropriate comparison group; outcomes by HIV status. Investigator communicated that all women had counseling on various modern methods; did not have material on counseling content. | |
| Two study sites apparently provided the same counseling. Provision of contraceptives differed. One site provided implants and IUDs free of charge, while the other referred women to public clinic that charged small fee. Pills and condoms were free at public clinic. | |
| No apparent postpartum contact; intervention during pregnancy. Outcome was use of family planning services (from records) not contraceptive use. | |
| Intervention not provided within 6‐week postpartum period. Participants could be up to 6 months postpartum. | |
| No follow up; survey during postpartum hospital stay. Outcomes were satisfaction and reported influence of counseling on contraceptive method choice. No data on specific method choice or use. | |
| Pregnant or parenting teens who were not necessarily postpartum. Both groups received the same family planning counseling and referral. Special intervention group also had home visits and case management. | |
| Random assignment to intervention group was noted in the text (not abstract). | |
| No relevant outcome; assessed knowledge, attitudes, and self‐efficacy. | |
| Intervention was provided during third trimester (4 consecutive days). No apparent postpartum education or contact except for assessment of contraceptive continuation at 2 years during home visit. Contraceptive uptake was examined at 7 days postpartum with clinical records. | |
| No comparison intervention or control. Same intervention was provided to all participants, though two locations were used. | |
| Intervention apparently provided during prenatal clinic. Outcome assessment at 6 months postpartum. Trial completion estimated as July 2014. | |
| Pregnant or parenting teens who were not necessarily postpartum. | |
| Assessment time frame appeared insufficient (4 to 9 weeks postpartum). Outcome was 'acceptance' of contraception without type of contraceptive method. Data presented for 37% who returned to clinic by 9 weeks. Those who did not return within 5 weeks were interviewed at home; no data presented. Also, text referred to initiation, maintenance, and switching to safer method but data were insufficient for analysis. | |
| Inadequate information about intervention. Comparison group differed by HIV status as well as type of intervention. | |
| Study groups were based on contraceptive method chosen (immediate subdermal implant (before hospital discharge) versus another contraceptive or no method). Both groups were in the same educational program. | |
| Insufficient outcome data for comparison group: no data on pregnancy or contraceptive use. Only had induced abortions by 2 years for 129 women who did not attend clinics. | |
| Inadequate comparison group. Two service integration models studied: 1) HIV services with family planning, for which postpartum status was not an eligibility criterion; 2) Postnatal care and HIV services with participants who were postnatal (0 to 10 weeks). |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pregnancy by 12 months Show forest plot | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.27, 0.87] |
| Analysis 1.1  Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 1 Pregnancy by 12 months. | ||||
| 2 Use of specific modern methods at 12 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2 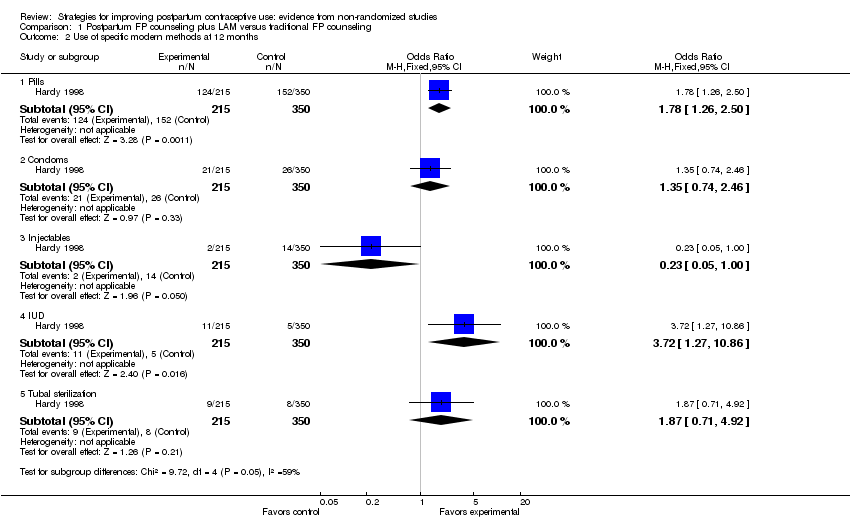 Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 2 Use of specific modern methods at 12 months. | ||||
| 2.1 Pills | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.26, 2.50] |
| 2.2 Condoms | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.74, 2.46] |
| 2.3 Injectables | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.05, 1.00] |
| 2.4 IUD | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.72 [1.27, 10.86] |
| 2.5 Tubal sterilization | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.87 [0.71, 4.92] |
| 3 No contraceptive use at 12 months Show forest plot | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.21, 0.67] |
| Analysis 1.3 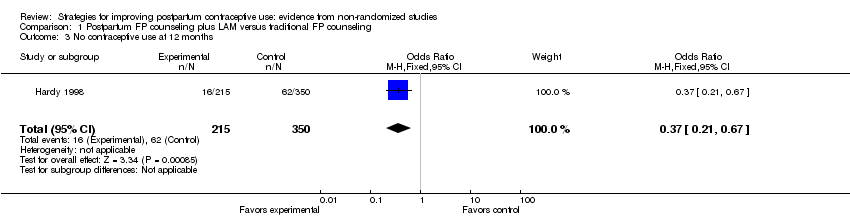 Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 3 No contraceptive use at 12 months. | ||||
| 4 Use of traditional contraceptive methods at 12 months Show forest plot | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.39, 1.41] |
| Analysis 1.4 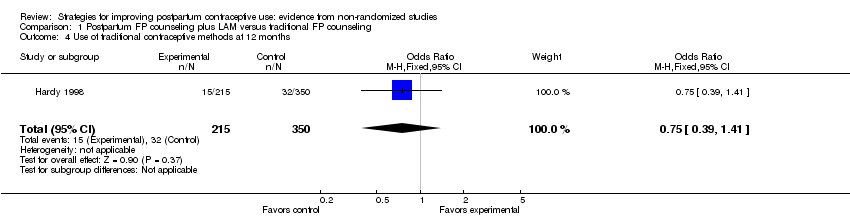 Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 4 Use of traditional contraceptive methods at 12 months. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Contraceptive use (6 months postpartum) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Family planning counseling versus control, Outcome 1 Contraceptive use (6 months postpartum). | ||||
| 1.1 Use of modern contraceptive method | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.77 [1.08, 2.89] |
| 1.2 Use of traditional contraceptive method | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.67, 1.90] |
| 2 No contraceptive use (6 months postpartum) Show forest plot | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.17, 0.64] |
| Analysis 2.2  Comparison 2 Family planning counseling versus control, Outcome 2 No contraceptive use (6 months postpartum). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Effectiveness of contraceptive method used most often (intervention versus pamphlet) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1 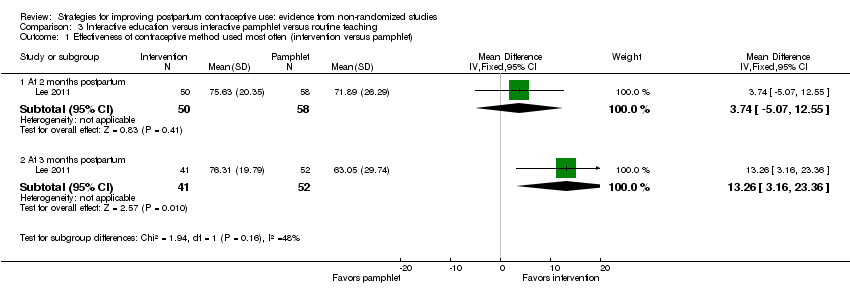 Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 1 Effectiveness of contraceptive method used most often (intervention versus pamphlet). | ||||
| 1.1 At 2 months postpartum | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | 3.74 [‐5.07, 12.55] |
| 1.2 At 3 months postpartum | 1 | 93 | Mean Difference (IV, Fixed, 95% CI) | 13.26 [3.16, 23.36] |
| 2 Effectiveness of contraceptive method used most often (intervention versus routine) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2 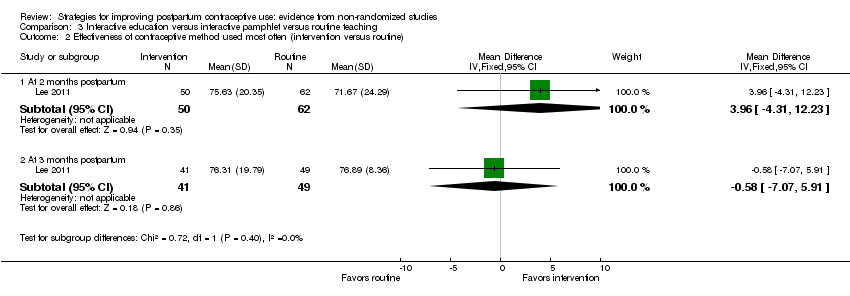 Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 2 Effectiveness of contraceptive method used most often (intervention versus routine). | ||||
| 2.1 At 2 months postpartum | 1 | 112 | Mean Difference (IV, Fixed, 95% CI) | 3.96 [‐4.31, 12.23] |
| 2.2 At 3 months postpartum | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.58 [‐7.07, 5.91] |
| 3 Sexual health knowledge at 2 months postpartum Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.3  Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 3 Sexual health knowledge at 2 months postpartum. | ||||
| 3.1 Intervention versus pamphlet | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.06, 1.02] |
| 3.2 Intervention versus routine | 1 | 112 | Mean Difference (IV, Fixed, 95% CI) | 1.55 [1.13, 1.97] |
| 4 Sexual health attitudes at 2 months postpartum Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.4 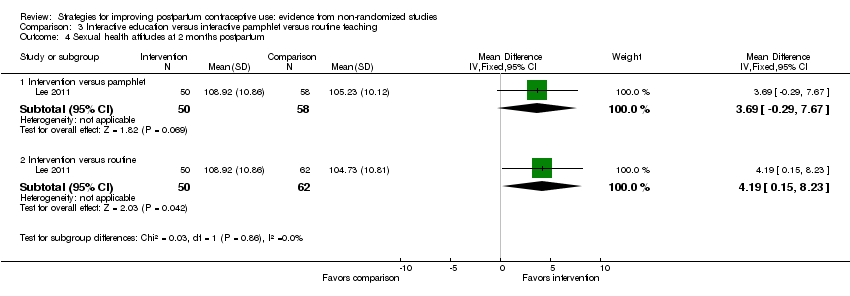 Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 4 Sexual health attitudes at 2 months postpartum. | ||||
| 4.1 Intervention versus pamphlet | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | 3.69 [‐0.29, 7.67] |
| 4.2 Intervention versus routine | 1 | 112 | Mean Difference (IV, Fixed, 95% CI) | 4.19 [0.15, 8.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pregnancy at 6 months postpartum Show forest plot | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.02, 1.87] |
| Analysis 4.1  Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 1 Pregnancy at 6 months postpartum. | ||||
| 2 IUD use postpartum Show forest plot | 1 | 1560 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.82, 3.02] |
| Analysis 4.2 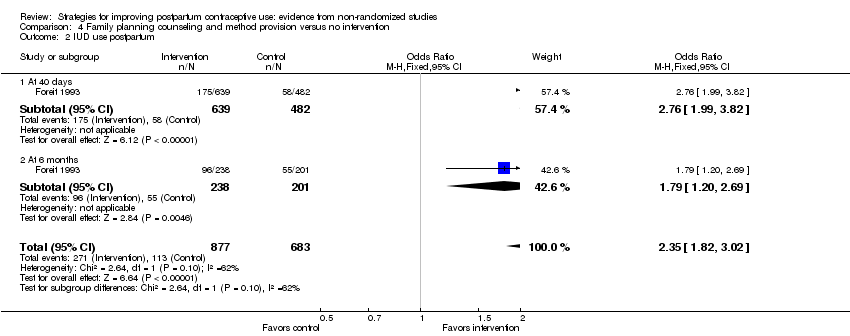 Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 2 IUD use postpartum. | ||||
| 2.1 At 40 days | 1 | 1121 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.76 [1.99, 3.82] |
| 2.2 At 6 months | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.20, 2.69] |
| 3 Other method use postpartum Show forest plot | 1 | 1560 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.91, 1.49] |
| Analysis 4.3  Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 3 Other method use postpartum. | ||||
| 3.1 At 40 days | 1 | 1121 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.93, 1.79] |
| 3.2 At 6 months | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.69, 1.48] |
| 4 No contraceptive method use postpartum Show forest plot | 1 | 1560 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.36, 0.56] |
| Analysis 4.4  Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 4 No contraceptive method use postpartum. | ||||
| 4.1 At 40 days | 1 | 1121 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.34, 0.56] |
| 4.2 At 6 months | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.31, 0.75] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Contraceptive use postpartum (HSM versus standard care) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1 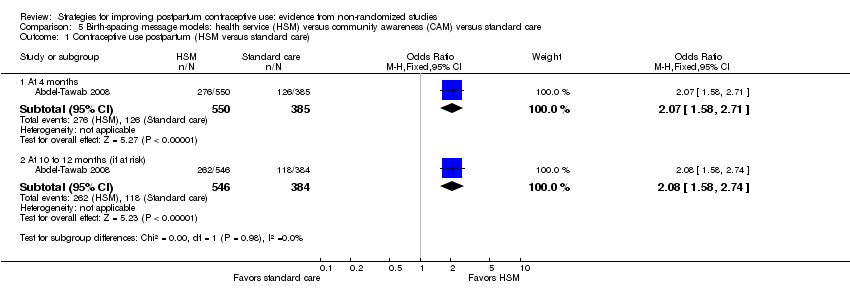 Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 1 Contraceptive use postpartum (HSM versus standard care). | ||||
| 1.1 At 4 months | 1 | 935 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.07 [1.58, 2.71] |
| 1.2 At 10 to 12 months (if at risk) | 1 | 930 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.58, 2.74] |
| 2 Contraceptive use postpartum (HSM versus CAM) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.2  Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 2 Contraceptive use postpartum (HSM versus CAM). | ||||
| 2.1 At 4 months | 1 | 1031 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.40, 2.30] |
| 2.2 At 10 to 12 months (if at risk) | 1 | 1025 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.97, 1.59] |
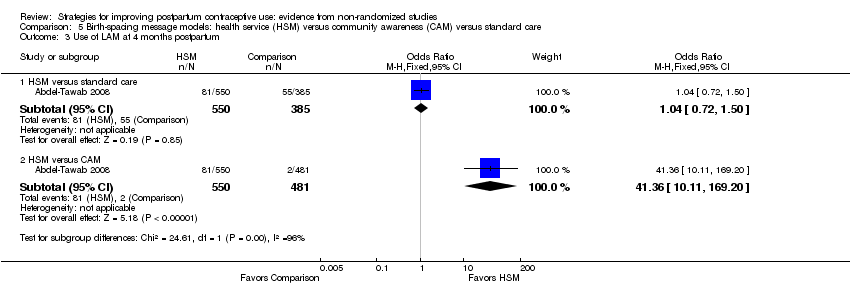
| 3 Use of LAM at 4 months postpartum Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.3 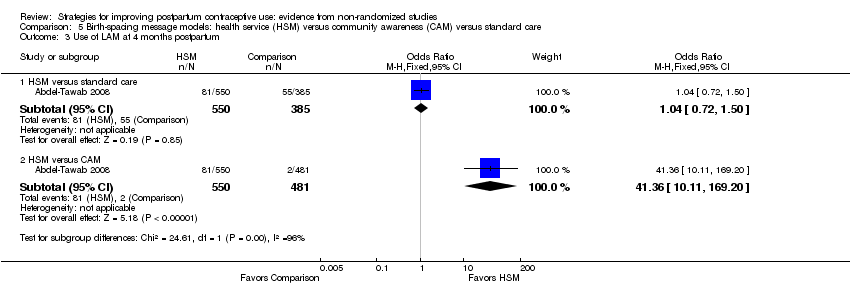 Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 3 Use of LAM at 4 months postpartum. | ||||
| 3.1 HSM versus standard care | 1 | 935 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.72, 1.50] |
| 3.2 HSM versus CAM | 1 | 1031 | Odds Ratio (M‐H, Fixed, 95% CI) | 41.36 [10.11, 169.20] |
| 4 Knowlege of effective LAM use at 4 months postpartum (HSM versus standard care) Show forest plot | 1 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.90 [0.91, 9.26] |
| Analysis 5.4  Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 4 Knowlege of effective LAM use at 4 months postpartum (HSM versus standard care). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
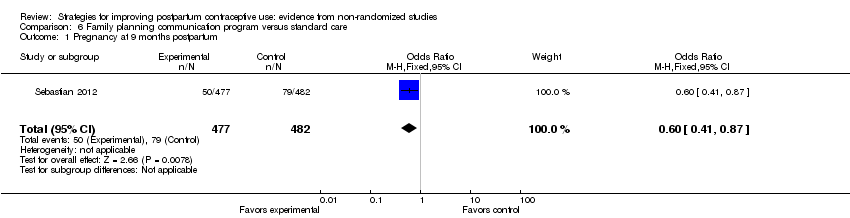
| 1 Pregnancy at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.41, 0.87] |
| Analysis 6.1 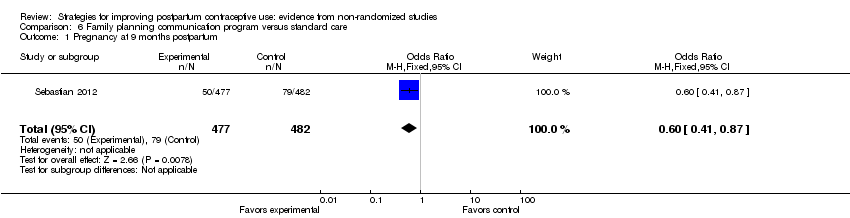 Comparison 6 Family planning communication program versus standard care, Outcome 1 Pregnancy at 9 months postpartum. | ||||
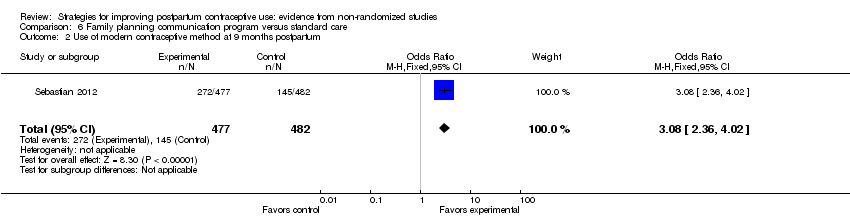
| 2 Use of modern contraceptive method at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [2.36, 4.02] |
| Analysis 6.2 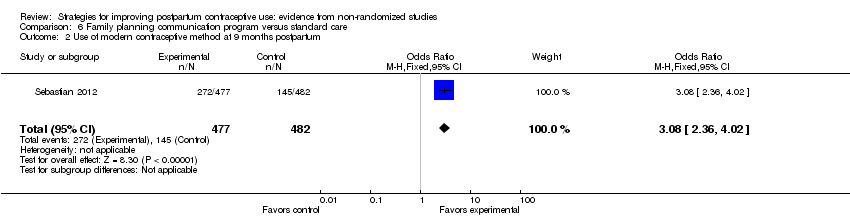 Comparison 6 Family planning communication program versus standard care, Outcome 2 Use of modern contraceptive method at 9 months postpartum. | ||||
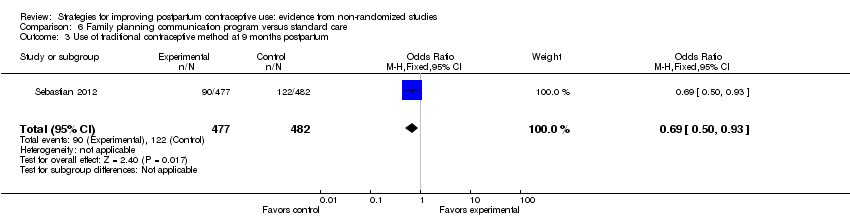
| 3 Use of traditional contraceptive method at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.50, 0.93] |
| Analysis 6.3 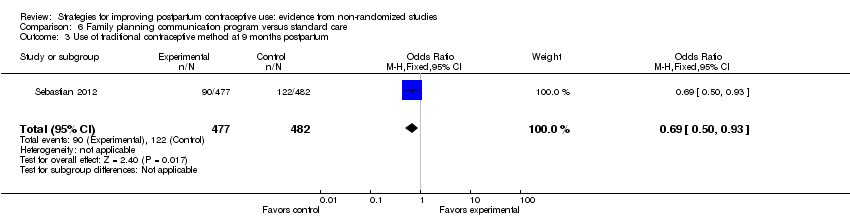 Comparison 6 Family planning communication program versus standard care, Outcome 3 Use of traditional contraceptive method at 9 months postpartum. | ||||
| 4 No contraceptive use at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.30, 0.52] |
| Analysis 6.4  Comparison 6 Family planning communication program versus standard care, Outcome 4 No contraceptive use at 9 months postpartum. | ||||

Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 1 Pregnancy by 12 months.
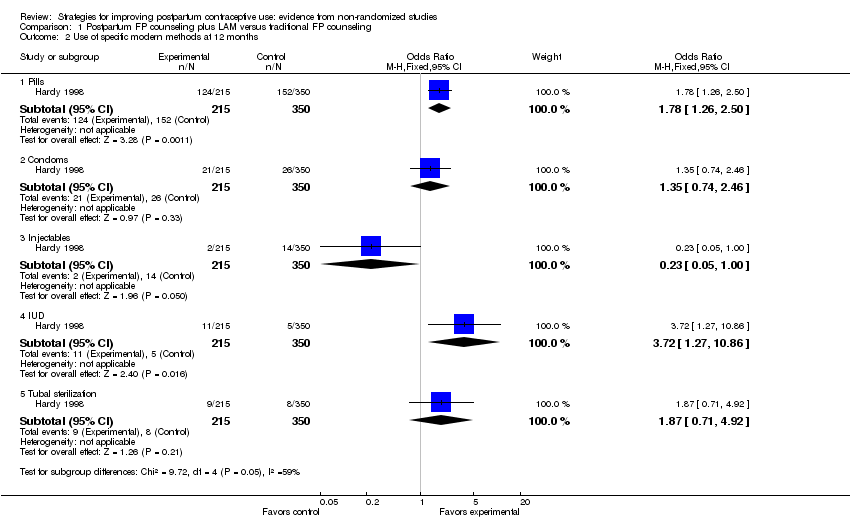
Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 2 Use of specific modern methods at 12 months.
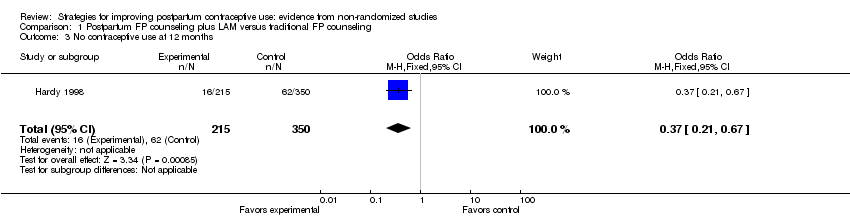
Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 3 No contraceptive use at 12 months.
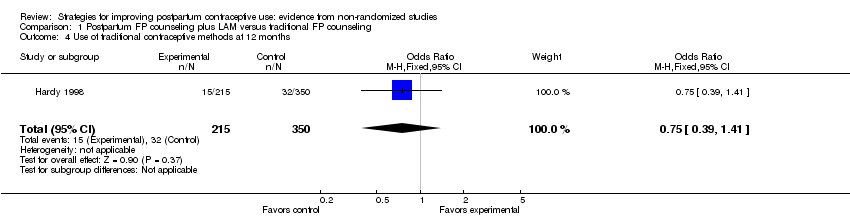
Comparison 1 Postpartum FP counseling plus LAM versus traditional FP counseling, Outcome 4 Use of traditional contraceptive methods at 12 months.

Comparison 2 Family planning counseling versus control, Outcome 1 Contraceptive use (6 months postpartum).

Comparison 2 Family planning counseling versus control, Outcome 2 No contraceptive use (6 months postpartum).
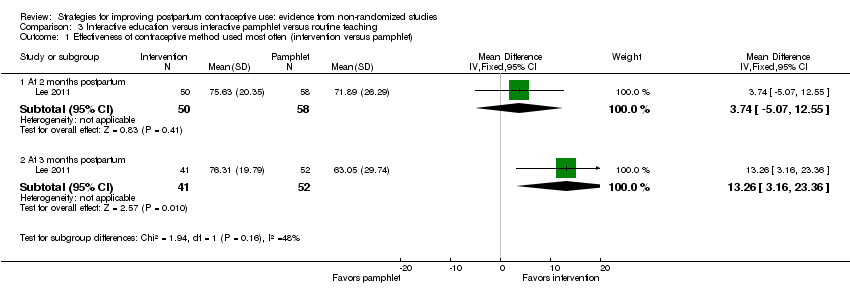
Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 1 Effectiveness of contraceptive method used most often (intervention versus pamphlet).
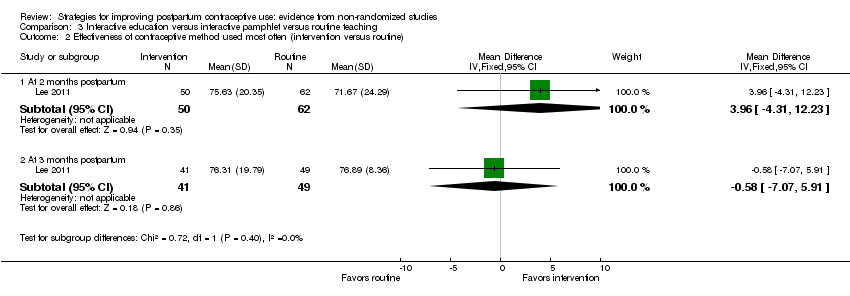
Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 2 Effectiveness of contraceptive method used most often (intervention versus routine).

Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 3 Sexual health knowledge at 2 months postpartum.
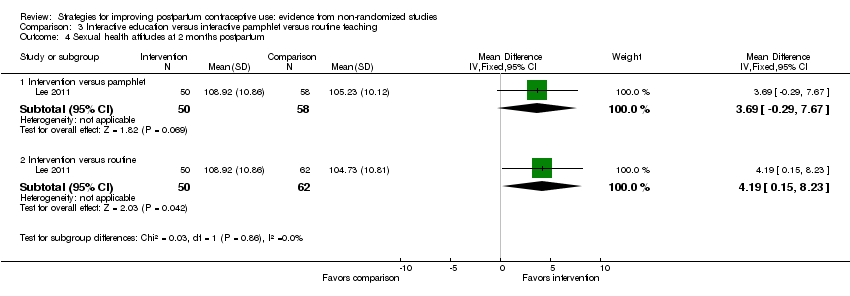
Comparison 3 Interactive education versus interactive pamphlet versus routine teaching, Outcome 4 Sexual health attitudes at 2 months postpartum.

Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 1 Pregnancy at 6 months postpartum.
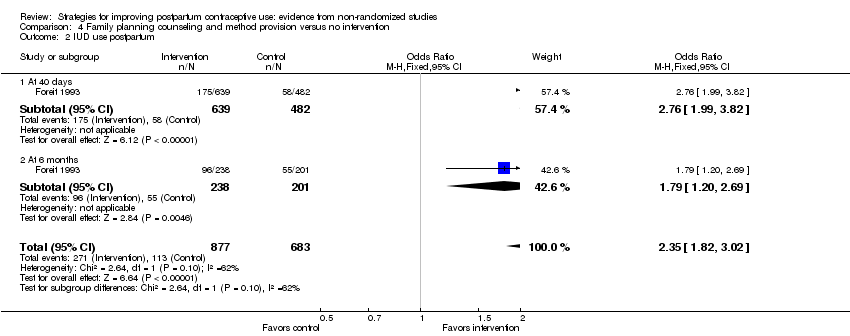
Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 2 IUD use postpartum.

Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 3 Other method use postpartum.

Comparison 4 Family planning counseling and method provision versus no intervention, Outcome 4 No contraceptive method use postpartum.
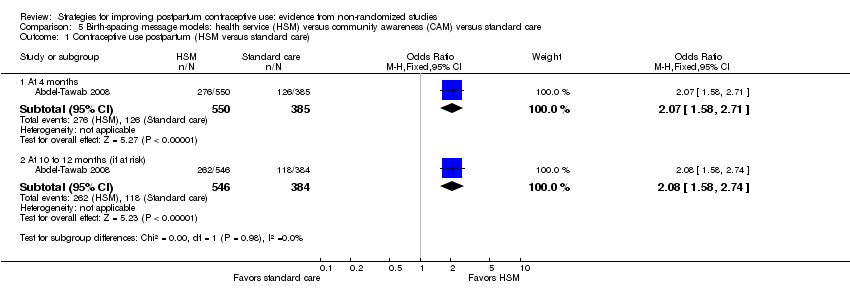
Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 1 Contraceptive use postpartum (HSM versus standard care).

Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 2 Contraceptive use postpartum (HSM versus CAM).
Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 3 Use of LAM at 4 months postpartum.

Comparison 5 Birth‐spacing message models: health service (HSM) versus community awareness (CAM) versus standard care, Outcome 4 Knowlege of effective LAM use at 4 months postpartum (HSM versus standard care).
Comparison 6 Family planning communication program versus standard care, Outcome 1 Pregnancy at 9 months postpartum.
Comparison 6 Family planning communication program versus standard care, Outcome 2 Use of modern contraceptive method at 9 months postpartum.
Comparison 6 Family planning communication program versus standard care, Outcome 3 Use of traditional contraceptive method at 9 months postpartum.

Comparison 6 Family planning communication program versus standard care, Outcome 4 No contraceptive use at 9 months postpartum.
| Study | Curriculum or manual | Provider credentials | Training for intervention | Assessed adherence | Assessed intervention | Fidelity criteria |
| ‐‐‐ | Educators for counseling; physicians for IUD insertion | 5 days for educators on FP; 4 days for physicians on IUD insertion | ‐‐‐ | ‐‐‐ | 2 | |
| Counseling material; leaflet on LAM for participants | ‐‐‐ | Training of all personnel on FP, including LAM as method | ‐‐‐ | ‐‐‐ | 2 | |
| 20‐minute educational session plus pamphlet | Researchers | ‐‐‐ | ‐‐‐ | ‐‐‐ | 2 | |
| Birth‐spacing messages and material for education and communication | Health care (HC) providers (physicians, nurses, Raedat Refiyat (community workers); community leaders | 3 days for HC managers and supervisors as trainers; 3 days for HC providers; 2 days for community leaders | Monthly supervision and monitoring visits by MCH and FP supervisors; checklists for monitoring intervention components. | Clinic exit interview had several knowledge and attitude items. | 5 | |
| Sexual health program (pamphlet) and educator guide booklet | Obstetric nurse educator | ‐‐‐ | ‐‐‐ | Assessed sexual health knowledge and attitudes and contraceptive self‐efficacy. | 3 | |
| Educational materials and counseling aids | Community midwife for antenatal clinic (18 months training); social health activist for counseling in homes (3 weeks training); anganwadi workers for counseling (1 month plus on‐job training) | 1 day for medical and child development officers, who trained community workers over 2 days (with counseling practice) | Supervisors spot‐checked knowledge of women; project staff observed counseling quality and content. | Knowledge assessed at 4 and 9 months postpartum. | 5 | |
| aAssessed participants' understanding and skills regarding the intervention. | ||||||
| Outcome at 12 months postpartum1 | Variable | Reported | Reported | Reported | Odds Ratio | 95% CI |
| Cumulative pregnancy rate | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ |
| Contraceptive use | Having partner | 1.8914 | 0.2020 | <0.0001 | 6.63 | 4.46 to 9.85 |
| Experimental group | 1.1113 | 0.2931 | 0.0002 | 3.04 | 1.71 to 5.40 | |
| >= 2 living children | ‐0.6636 | 0.2670 | 0.0129 | 0.51 | 0.31 to 0.87 | |
| 1Logistic regression model included age, schooling (>= high school), # living children (>= 2), marital state (with partner), study group. | ||||||
| Outcome1 | Variable | Reported adjusted | Reported | Reported |
| Use of modern contraceptive method (9 months postpartum) | intervention group | 3.66 | 2.72 to 4.91 | < 0.01 |
| education >= high school | 1.88 | 1.27 to 2.79 | < 0.01 | |
| caste: other backward‐caste Hindu | 1.60 | 1.07 to 2.38 | < 0.05 | |
| Change in knowledge of >= 2 healthy spacing messages (4 months postpartum)2 | intervention group | 2.07 | ‐‐‐ | < 0.01 |
| age 20 to 24 years | 1.65 | ‐‐‐ | < 0.05 | |
| caste: high‐caste Hindu | 1.93 | ‐‐‐ | < 0.01 | |
| Change in knowledge of >= 2 spacing methods (9 months postpartum)2 | intervention group | 1.96 | ‐‐‐ | < 0.01 |
| baseline value | 1.53 | ‐‐‐ | < 0.05 | |
| education: middle school | 2.07 | ‐‐‐ | < 0.01 | |
| education: >= high school | 3.18 | ‐‐‐ | < 0.01 | |
| 1Logistic regression models did not include LAM use or knowledge because only 0.2% of control‐group women knew about the method. Models included study group, education, age, age at initiation of cohabitation, caste, and parity. Modern methods included pill, condoms, IUD, and sterilization. Models for change in knowledge also included baseline value. | ||||
| NOS criteria for cohort studies | ||||||
| Exposed cohort representativeness | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ |
| Nonexposed cohort selection | ✸ | ‐‐‐ | ✸ | ‐‐‐ | ✸ | ‐‐‐ |
| Exposure ascertainment: method used | ✸ | ‐‐‐ | ✸ | ✸ | ✸ | ✸ |
| Comparability of groups: design or analysis | ‐‐‐ | ✸✸ | ‐‐‐ | ✸ | ‐‐‐ | ✸✸ |
| Outcome assessment: method used | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ | ‐‐‐ |
| Follow‐up length | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ |
| Follow‐up adequacy | ‐‐‐ | ‐‐‐ | ✸ | ✸ | ‐‐‐ | ‐‐‐ |
| Intervention fidelity (>= 4 criteria) | ‐‐‐ | ‐‐‐ | ‐‐‐ | ✸ | ‐‐‐ | ✸ |
| Quality of evidence1,2 | Poor | Very low | Very low | Low | Poor | Low |
| 1Evidence was initially considered moderate quality and then downgraded for 1) no stars for comparability (not controlling for confounding), 2) not meeting >= 4 of remaining 6 NOS criteria, and 3) not having intervention fidelity information for >= 4 categories. Quality grades were moderate, low, very low, or poor. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pregnancy by 12 months Show forest plot | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.27, 0.87] |
| 2 Use of specific modern methods at 12 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Pills | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.26, 2.50] |
| 2.2 Condoms | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.74, 2.46] |
| 2.3 Injectables | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.05, 1.00] |
| 2.4 IUD | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.72 [1.27, 10.86] |
| 2.5 Tubal sterilization | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.87 [0.71, 4.92] |
| 3 No contraceptive use at 12 months Show forest plot | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.21, 0.67] |
| 4 Use of traditional contraceptive methods at 12 months Show forest plot | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.39, 1.41] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Contraceptive use (6 months postpartum) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Use of modern contraceptive method | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.77 [1.08, 2.89] |
| 1.2 Use of traditional contraceptive method | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.67, 1.90] |
| 2 No contraceptive use (6 months postpartum) Show forest plot | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.17, 0.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Effectiveness of contraceptive method used most often (intervention versus pamphlet) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 2 months postpartum | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | 3.74 [‐5.07, 12.55] |
| 1.2 At 3 months postpartum | 1 | 93 | Mean Difference (IV, Fixed, 95% CI) | 13.26 [3.16, 23.36] |
| 2 Effectiveness of contraceptive method used most often (intervention versus routine) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 At 2 months postpartum | 1 | 112 | Mean Difference (IV, Fixed, 95% CI) | 3.96 [‐4.31, 12.23] |
| 2.2 At 3 months postpartum | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.58 [‐7.07, 5.91] |
| 3 Sexual health knowledge at 2 months postpartum Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Intervention versus pamphlet | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.06, 1.02] |
| 3.2 Intervention versus routine | 1 | 112 | Mean Difference (IV, Fixed, 95% CI) | 1.55 [1.13, 1.97] |
| 4 Sexual health attitudes at 2 months postpartum Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Intervention versus pamphlet | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | 3.69 [‐0.29, 7.67] |
| 4.2 Intervention versus routine | 1 | 112 | Mean Difference (IV, Fixed, 95% CI) | 4.19 [0.15, 8.23] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pregnancy at 6 months postpartum Show forest plot | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.02, 1.87] |
| 2 IUD use postpartum Show forest plot | 1 | 1560 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.82, 3.02] |
| 2.1 At 40 days | 1 | 1121 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.76 [1.99, 3.82] |
| 2.2 At 6 months | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.20, 2.69] |
| 3 Other method use postpartum Show forest plot | 1 | 1560 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.91, 1.49] |
| 3.1 At 40 days | 1 | 1121 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.93, 1.79] |
| 3.2 At 6 months | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.69, 1.48] |
| 4 No contraceptive method use postpartum Show forest plot | 1 | 1560 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.36, 0.56] |
| 4.1 At 40 days | 1 | 1121 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.34, 0.56] |
| 4.2 At 6 months | 1 | 439 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.31, 0.75] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Contraceptive use postpartum (HSM versus standard care) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 4 months | 1 | 935 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.07 [1.58, 2.71] |
| 1.2 At 10 to 12 months (if at risk) | 1 | 930 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.58, 2.74] |
| 2 Contraceptive use postpartum (HSM versus CAM) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 At 4 months | 1 | 1031 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.40, 2.30] |
| 2.2 At 10 to 12 months (if at risk) | 1 | 1025 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.97, 1.59] |
| 3 Use of LAM at 4 months postpartum Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 HSM versus standard care | 1 | 935 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.72, 1.50] |
| 3.2 HSM versus CAM | 1 | 1031 | Odds Ratio (M‐H, Fixed, 95% CI) | 41.36 [10.11, 169.20] |
| 4 Knowlege of effective LAM use at 4 months postpartum (HSM versus standard care) Show forest plot | 1 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.90 [0.91, 9.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pregnancy at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.41, 0.87] |
| 2 Use of modern contraceptive method at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [2.36, 4.02] |
| 3 Use of traditional contraceptive method at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.50, 0.93] |
| 4 No contraceptive use at 9 months postpartum Show forest plot | 1 | 959 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.30, 0.52] |


